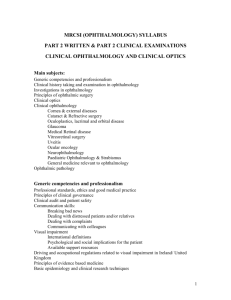
OphthalALL
advertisement

1. Common visual field defects have causes as follows: DEFECT CAUSE Bitemporal hemianopia Pituitary adenoma Arcuate scotoma Glaucoma (all types) Central scotoma Macular degeneration, optic neuritis Homonymous hemianopia Lesion in optic tract or stroke (clot) in posterior cerebral artery Ring scotoma Retinal disorder (Retinitis pigmentosa) 2. SLE can cause: - retinal vasculitis (exudates and haemorrhages), - episcleritis - conjunctivitis - optic neuritis - secondary Sjogrens syndrome Rheumatoid arthritis can cause: - scleritis and episcleritis - scleritis can lead to eye perforation (scleromalacia perforans) - secondary Sjogrens syndrome Behcet’s disease can cause: - acute and recurrent anterior or posterior uveitis - retinal vasculitis and vitritis Reiter’s syndrome can cause: - conjunctivitis - uveitis Juvenile chronic arthritis (AFP+) can cause: - anterior uveitis - cataract/glaucoma/macular degeneration occur more commonly (chronic) In addition: IBD anterior uveitis Psoriatic arthritis uveitis and conjunctivitis Ankylosing spondylitis uveitis Sarcoidosis recurrent/chronic granulomatous anterior uveitis and “mutton-fat” keratic precipitates in association with granulomatous inflammation 3. Topical steroids have the following ocular effects: - glaucoma (especially LOCAL administration) by increased intraocular pressure - cataracts (especially SYSTEMIC administration) - exacerbation of infections (especially HSV) 4. Orbital cellulitis is usually associated with an infection in the paranasal air sinus. It leads to conjunctivitis, eyelid swelling, proptosis and reduced ocular movement. It may be accompanied by systemic indicators of infection like malaise or pyrexia. Causative organisms are Haemophilus influenzae and Streptococcus pneumoniae and anaerobes. It may be rapidly progressive and needs to be treated quickly to avoid visual loss, orbital abscess formation and intracranial spread. Cavernous sinus thrombosis (CST) is usually a late complication of an infection of the central face or paranasal sinuses. Effective treatment of orbital cellulitis can reduce the incidence of cavernous sinus thrombosis. 5. Painless loss of vision occurs with: - retinal detachment - retinal arterial occlusion - retinal venous occlusion - amaurosis fugax - cataract - arteritic and non-arteritic ischemic optic neuropathy - open angle glaucoma Keratitis tends to be painful and is caused by viral (HSV, VZV, adenovirus) or bacterial (Staph aureus/epidermidis, Strep pneumoniae, enterobacter (E.coli, Proteus, Klebsiella), Pseudomonas aeruginosa) or parasite (Acanthamoeba) infection. 6. Diabetic retinopathy is categorized into three grades: Background Microaneurysms Dot-blot haemorrhages Oedema and exudates Preproliferative Cotton wool spots Venous beading, loops Proliferative Neovascularization at disc (NVD) and elsewhere (NVE) The seriousness increases as we go from background to pre-proliferative to proliferative, as do the likelihood of advanced disease complications (see below). The macula can also be affected by oedema, microaneurysms, exudates and haemorrhages and thus is called diabetic maculopathy. In advanced disease, complications include: - iris rubeosis (new vessels in iris- can cause vascular glaucoma) - vitreous haemorrhage - retinal detachment Retinal changes occur in types 1 and 2 diabetics. 7. The uveal tract includes the ciliary body, iris and choroids. It is present at birth. The ciliary body produces aqueous humor for the anterior chamber, and drains the fluid via the trabecular meshwork and the Canal of Schlemm. Ankylosing spondylitis causes anterior uveitis, as do all other seronegative arthropathies. Carbonic anhydrase is found in the ciliary body, where aqueous humor is made. Inhibition of carbonic anhydrase can be used to decrease secretion of aqueous humor. This is a common therapy in glaucoma (acetazolamide). 8. Amblyopia, defined as poor vision due to abnormal visual experience early in life (before 9), affects approximately 3% of the population and carries a projected lifetime risk of visual loss of at least 1.2 per cent. Amblyopia is the impairment of vision without detectable organic lesion of the eye. The most common cause is strabismus (squint), but other causes include: - alcohol - arsenic - nutritional deficiency - quinine - reflex (results from peripheral irritation) - trauma - tobacco (caused by ingestion) - uremic If strabismus develops in the sensitive period (up to 7-8) the brain responds by refusing to see the image from deviating eye. This prevents diplopia but also causes lazy eye to form. It is usually treated by: - correcting refractive error (glasses) - reversing amblyopia (occlude good eye, forcing amblyopic eye to fix and see) - Orthoptic management - Surgery Amblyopia is usually painless. 9. Palsy of CNIII leads to divergence (looking “down and out”), ptosis and pupil dilation. Third nerve palsies are separated into “medical” and “surgical” causes. Since pupillomotor fibers in CNIII have a difference blood supply from the rest of the nerve, microvascular disorders like diabetes usually cause papillary sparing. Surgical causes, like aneurysm of posterior communicating artery, DO involve the pupil. Oculomotor nerve palsies may be congenital, as both unilateral and bilateral congenital oculomotor nerve palsies have been decribed, alone AND in conjunction with other neurological abnormalities. Pilocarpine is a parasympathetico-mimetic, causing contraction of ciliary muscle and constrictor pupillae. A palsy would have the opposite effect, given the CNIII has parasympathetic outflow from the cilary ganglion. 10. Errors in refraction require correction. Hypermetropia involves the image being focused behind the eye. A convex lens is used to focus the image onto the back of the eye. It is caused by an abnormally small eyeball or a lens that can’t sufficiently focus. It can be complicated by acute glaucoma (have to overconverge to focus on eye-ball, bringing lens more spherical making posterior attachment to iris more likely). Myopia involves the image being focused in front of the eye. A concave lens is used to focus the image onto the back of the eye. It is caused by an abnormally large eyeball. High myopia predisposes to retinal detachment, glaucoma (open angle as ciliary body drainage insufficient), cataracts, chorioretinal atrophy and macular choroidal neovascularization. It is generally agreed that both myopia and hypermetropia are congenital and unalterable except by glasses or surgery. In childhood, esotropia (convergent squint) is often a result of hypermetropia (child overconverges as they focus on near objects). Exotropia is often the result of myopia (child stares into distance). 11. Temporal giant cell arteritis is an arterial ischemic optic neuropathy. It causes scalp tenderness (pain?) with inflammatory swelling of temporal arteries, jaw claudication and elevated ESR and CRP. There is an RAPD (relative afferent pupil defect) and swollen optic disc (haemorrhage and cotton wool spots) with altitudinal field loss. Systemic steroids must be given for several years to prevent relapse. It is most common in elderly. NON-arteritic ischemic optic neuropathy has no sign of inflammation and is associated with atherosclerosis, hypertension, smoking and diabetes. 12. Corneal abrasions cause pain and watering, and blurred vision. Corneal abrasions are demonstrated with flourescein drops and blue light-dye pools green in defect. Trauma, UV light can cause. Conventional treatment consists of chloramphenicol with cyclopegic (cyclopentolate 1% or homatropine 2%) for comfort, occlusive padding for a day, followed by 4 times a day chloramphenicol ointment for 4-7 days. They usually heal by themselves with this treatment, unless a foreign body is present or infection persists. 13. The normal pupil is slightly nasal to the center of the cornea. It’s size is determined by a balance of the sphincter muscle and the dilator muscle. The dilator muscle is innervated by the sympathetic trunk. The postganglionic fibres arise from the superior cervical ganglion and the neurotransmitter is noradrenaline. The sphincter muscle is innervated by the parasympathetic system via the oculomotor nerve (CN III) through the Edinger Westphal nucleus. Horner’s syndrome causes abruption of sympathetic outflow and thus inhibits dilation (and thus constricts affected pupil). A palsy of the oculomotor nerve causes paralysis of the sphincter which causes dilation. Pilocarpine is a parasympatheticomimetic and thus increases sphincter muscle activity. Glaucoma causes iris ischaemia which causes it to be weak and unreactive. An oval, enlarged, and unreactive pupil results. Optic neuritis causes a relative afferent pupillary defect. 14. Retrobulbar neuritis is a type of optic neuritis between the eye and the brain. It’s symptoms are similar to optic neuritis: - blurred or dimmed vision - central scotoma - pain with eye movement - eye tender to touch or pressure - complete blindness in affected eye Chronic open angle glaucoma is painless. However, acute closed angle glaucoma is painful. Iridocyclitis (acute) also known as anterior uveitis, is painful. It can be caused by HSV, VZV, Fuchs cyclitis, trauma and systemic causes (Ankylosing spondylitis, Reiters, Behcets, sarcoidosis, IBD, Psoriasis, Juvenile chronic arthritis). Central retinal vein and central retinal artery occlusions are both painless. Corneal erosion is painful. Symptoms include: - severe pain (especially after awakening) - blurred vision - foreign body sensation - dryness and irritation - tearing, redness and photophobia 15. Herpes simplex can cause: - superficial keratitis (heals without scarring) - deep keratitis (heals WITH scarring) - anterior uveitis (iris, ciliary body) - dendritic ulcers (so called because of branching pattern) It is often recurrent and needs treatment from topical acyclovir. Topical steroids exacerbate this condition, turning a corneal ulcer into an amoeboid ulcer. 16. Opthalmic herpes zoster: Primary infection conjunctivitis + dendritic ulcer Secondary infection ANY ocular or ajoining (adnexal) structures Dermatomal skin rash Conjunctivitis, keratitis, anterior uveitis COMMON Scleritis and episcleritis MAY occur Herpes zoster may be associated with post-herpetic neuralgia. 17. Ptosis is a drooping of the upper eyelid. It can be caused by: - Horner’s Sympathetic nerve palsy. Since Muller’s muscle is supplied by sympathetic system, a ptosis arises. Other symptoms include constricted pupil and anhydrosis - Age-related - trauma - myasthenia gravis (presumably cause of fatigue of levator palpebrae) - CN III nerve palsy (dilated pupil, “down and out“ eye) occurs as a result of levator palpebrae being supplied by CN III. ** CN7 does NOT cause ptosis as it supplies orbicularis oculi which CLOSES the eyelids. 18. Diplopia also known as double vision, can be caused by: - incomitant squint: - neurological: - paralysis of CN III, IV or VI - CNS disease (ophthalmoplegia) - muscular: - myasthenia gravis - mechanical restriction: - thyroid eye disease - orbital wall fracture - orbital tumor - “pseudotumor” - surgical overcorrection of squint - decompensation of latent squint - spectacle problems Monocular diplopia: - disorders of the cornea or lens: - keratoconus - cataract - lens dislocation 19. Uveitis can be caused by: - viruses (HSV, VZV, adenovirus) - trauma - Fuchs heterochromic cyclitis (heterochromia [color diff between two iris], fine keratic precipitates (KPs)), leading to glaucoma and cataracts. - Systemic (IBD, TB, sarcoidosis, JIA, Behcets, Reiters, ankylosing spondylitis, Psoriasis) 20. Commonly used drugs with ocular complications include: DRUG Ocular complication Amiodarone Verticillata (vortex pattern on cornea) Lens opacities Ant. Ischemic optic neuropathy Gold, chlorpromazine Pigmented inclusions in conjunctiva/lids Antihistamines/B-blockers TCA, anxiolytics Dry eyes Chloroquine/chlorpromazine, Gold, NSAIDs, steroids amiodarone Lenticular deposits/keratopathy Sulphonamides, metronidazole Thiazides, Acetazolamide Refractive error Ethambutol, isoniazid Reduced acuity, visual field defects, color vision disturbance Chloramphenicol Optic neuritis/retrobulbar neuritis Isotretinoin/sulphonamides, salicylates Antineoplastic agent Conjunctivitis/blepharitis Ethambutol Optic neuritis 21. Viral conjunctivitis is commonly caused by Adenovirus and herpes virus. Discharge is watery, but nightime discharge causes stickiness in the conjunctiva. Follicles representing grains of rice are seen (bacterial=papillae/”velvet” while virus=follicle/”rice”). Corneal erosion is common and corneal ulceration should be excluded. Secondary iritis can also occur. Pre-auricular lymph node involvement is common. Swelling can expand to the ear. Viral infection usually settles without treatment within two weeks. Topical agents like acyclovir are effective against HSV. Symptoms can be aided by vasoconstrictor/antihistamine combinations. 22. Atropine blocks parasympathetic activity and thus causes dilation Morphine use causes pin-point pupils Pilocarpine is a parasympatheticomimetic pupil constriction CN VII and CN VI have no effect on pupils 23. Congenital nasolacrimal duct blockage presents with recurrent mucocele, noninfected swelling of the lacrimal sac or to lacrimal gland infection (dacrocystitis). Is usually resolves itself but if it doesn’t, can be cured by probing at 9 months. ACQUIRED forms of nasolacrimal duct obstruction can be treated with a bypass (dacrocystorhinostomy). Congenital forms arise because of aberrant development of the first pharyngeal arch, and is not associated with a specific genetic inheritance. 24. Dysthyroid disease: infiltration of the orbital tissues and extraocular muscles by edema and inflammatory cells cause: - proptosis, diplopia and muscle weakness Other symptoms include: - lid retraction and lid lag - exophthalmos - optic nerve compression Proptosis can be unilateral or bilateral Strabismus is usually horizontal Exposure of the cornea can cause inflammation (exposure keratitis) 25. Rheumatoid arthritis tends NOT to cause anterior uveitis. It DOES cause scleritis and episcleritis. While viral conjunctivitis may cause anterior uveitis, it is usually adenovirus and not HSV that is the causative agent. 26. Retinoblastoma is the most common primary malignant intraocular tumor to affect children (1 in 20,000). Age of onset is 18 months and family history occurs in about 6% in autosomal dominant fashion (Chr 13). Hereditary forms may cause bilateral retinoblastomas. Leukocoria is usually the presenting sign. Retinoblastoma can cause strabismus and secondary glaucoma. Retinoblastoma’s are treated by enucleation (removal of eye) or by radiotherapy/chemotherapy in small lesions. Prognosis is determined by the optic nerve invasion. Survival is 90% at 3 years. 27. Oculomotor nerve palsies may be caused by aneurysm of the posterior communicating cerebral artery. This is considered a neurosurgical emergency. Oculomotor nerve supplies levator palpebrae and thus a palsy can result in ptosis. Palsy causes the eye to look “down and out.” Palsy can be caused by microvascular disease; this is considered a “medical” palsy as it can be caused by hypertension, diabetes, etc. This type of CN III palsy is associated with papillary sparing. CN III carries parasympathetic innervation to sphincter pupillae; a palsy would cause dilation (mydriasis). 28. The chief cause of optic neuritis is demyelination. Less commonly, viral infections, vasculitis (SLE) or drugs (esp ethambutol) can cause. Clinically, it presents with rapidly progressive loss of vision (central scotoma) in one eye with pain on eye movement. On examination, - central scotoma - relative afferent papillary defect Atypically, the other eye may become involved. Recovery usually occurs spontaneously after few weeks, even without treatment. At 5 years, the risk of developing MS is 60%. Visual evoked responses are often abnormal. VERs can be used to evaluate optic nerve damage, even in asymptomatic patients. 29. Hypermetropia predisposes to glaucoma (acute angle) because of overcompensation near response. Retinal detachment occurs as a complication in HyPOmetropia (near sighted), as does glaucoma, cataracts, choroidoretinal atrophy and macular choiroidal neovascularization. Abnormal development of the anterior chamber angle is the usual cause of congenital glaucoma. The presenting sign is USUALLY buphthalmos, since the infant eyeball can enlarge enormously with increased intraocular pressure. The three classic signs are photophobia, epiphora (tearing) and blepharospasm (eyelid spasm). Tears contain secretory IgA antibodies. Most disease processes of the optic nerve cause early change in visual acuity, but papilloedema causes LATE loss of acuity. Blurring is more common in the early stages. The cornea is composed of three layers, from outside to inside, the epithelium, the stroma and the endothelium. Epithelium can regenerate but involvement of the stroma or endothelium in corneal disease causes scarring. Corneal guttata (age-related) and Fuchs endothelial dystrophy (progressive) represent two processes that cause corneal endothelial cell loss. Decompensation can lead to oedema, loss of transparency and loss of vision. 30. Rubeosis iridis is the neovascularization of the iris, leading to occlusion of the anterior chamber angle and predisposing to glaucoma. Causes may include: - diabetic retinopathy - central retinal vein occlusion - retinal artery occlusion - radiation retinopathy - sickle cell retinopathy - chronic uveitis - chronic retinal detachment Laser photocoagulation to the central retina can improve rubeosis iridis. The central retina is where neovascularization mostly takes place (macular area). 31. Leukocoria can be caused by: - retinoblastoma - cataracts - toxocara granuloma - advanced retinopathy of prematurity - vitreous maldevelopment - retinal dysplasias - corneal opacity 32. Binocular vision is vision in which both eyes are used together. The word binocular comes from two Latin roots, bin for two, and oculus for eye. Having two eyes confers at least four advantages over having one. First, it gives a creature a spare eye in case one is damaged. Second, it gives a wider field of view. For example, a human has a horizontal field of view with one eye of about 150 degrees and with two eyes of about 180 degrees. Third, it gives binocular summation in which the ability to detect faint objects is enhanced (improved acuity). Fourth it can give stereopsis in which parallax provided by the two eyes' different positions on the head give precise depth perception. Such binocular vision is usually accompanied by singleness of vision or binocular fusion, in which a single image is seen despite each eye's having its own image of any object. The optic disc is the area of blind spot. It has no neuroreceptors in one eye but the other eye is sensitive and thus binocular vision can compensate for the blind spot. 33. Primary open angle glaucoma presents with increased intraocular pressure, optic disc cupping and peripheral visual field loss. Headache, eye pain and visual acuity problems do NOT occur. A cup:disc ratio of 0.6 in one eye, or a difference of 0.2 between eyes, is suggestive of glaucoma. An increasing cup: disc ratio is indicative of progressive disease. Average cup:disc ratio is under 0.4. The normal optic disc has nerve fibers (pink because of vascular perfusion), an area without nerve fibers (WHITE optic disc cup). As nerve fibers are lost or damaged, proportion of pink rim diminished and the cup enlarges. The blind spot corresponds to the area in front of the optic nerve head, where no photoreceptors are present. Since glaucoma causes death of nerve fibers, this area would (in theory) actually get smaller (it doesn’t though. It stays pretty much the same size cause there still aren’t any photoreceptors over the area replacing the dead nerve fibers). 34. Diabetes causes: - diabetic retinopathy (background, preproliferative, proliferative). - maculopathy - cataracts - glaucoma (primary open angle) - vitreous hemorrage and tractional retinal detachment - microvascular disease CN palsies (esp. CN III) strabismus This is a PARALYTIC squint Non-paralytic squints are caused by persistence of childhood squint or local muscle imbalance 35. The cornea and sclera form the outer wall of the eyeball. The cornea consists of a stroma sandwiched between a multilayered epithelium and an inner monolayer of endothelial cells. The stroma is 90% of the thickness, composed of collagen and extracellular matrix. There are few cells and no blood vessels. The cornea is avascular; its nutrition comes from diffusion from blood vessels at limbus, from aqueous humor and from tear film. The cornea is transparent because of the specialized arrangement of collagen fibrils in the stroma, kept in a state of dehydration. Dehydration is accomplished by the endothelium, which pumps ions from stroma into anterior chamber. While epithelial cells can regenerate, endothelial cells can NOT, so when endothelial cells are lost, the ability to pump ions and keep stroma dehydrated is lost, and thus corneal opacities occur, called corneal decompensation or bullous keratopathy. Normal aging, Fuchs heterochromic dystrophy and cataract surgery can all cause endothelial cell loss. 36. Cataracts can be caused by: Ocular factors Blunt or perforating trauma High myopia Recurrent uveitis Topical steroid use Ionising radiation Excessive UV exposure IR irradiation Systemic factors: Diabetes Steroid therapy Atopy Galactosemia HyPOcalcemia Dystrophia myotonica 37. Strabismus in a one year old is most commonly caused by hypermetropia. Other causes (less common) include myasthenia, myopathy, nerve palsies, cerebral palsy, hydrocephalus, any other cause of central or peripheral neurological deficit (including intracranial tumor and retinoblastoma). 38. The commonest adult intraocular tumor is the choroidal melanoma, a malignant melanoma of the choroids. 39. Enucleation is the closest parallel to traumatic loss of an eye. With that in mind, the complications of an enucleation procedude include: - loss of depth perception (stereoscopic vision) - loss of part of visual field to the side of the eye lost, when looking straight ahead. The loss is from about 180 to 150 degrees. Visual acuity in the remaining eye is maintained. The pupil reacts the same except consensual reflex is obviously absent (cause the eye is gone…). 40. Amblyopia is a defect in visual acuity not caused by organic disease, that occurs in the sensitive period of eye development (before age 8). Common causes include: - cataracts (sensory deprivation leads to lazy eye) - strabismus - central or peripheral CNS disorders affecting CN III, IV or VI can lead to strabismus and thus amblyopia - birth trauma, illness and family history, maternal infection - anisometropia (refractive power of one eye differs from the other). Since refractive errors commonly present with amblyopia (hypermetropiaconvergent and myopia divergent) Since maturity onset diabetes doesn’t (generally) occur before age 8, it can not cause amblyopia. 41 75. Sudden loss of vision can be caused by: - migraine - ischemic optic neuropathy (includes temporal arteritis) - raised intracranial pressure (papilloedema) - retinal vein occlusion - retinal artery occlusion - retinal detachment - foreign body - macular hemorrhage - acute glaucoma - optic neuritis - medications for erectile dysfunction Gradual vision loss can be caused by - cataract - medication (steroids, chloroquine, tamoxifen) - diabetic retinopathy - glaucoma - retinoblastoma - macular degeneration - retinitis pigmentosa Chlamydial conjunctivitis (serotypes A-C) can cause conjunctivitis leading to corneal ulceration and scarring. This may cause blindness in a chronic course (not sudden). 76. Floaters are more likely to develop as we age and are more common in people who are very nearsighted, have diabetes, or who have had a cataract operation. There are other, more serious causes of floaters, including infection, inflammation (uveitis), hemorrhaging, retinal tears, and injury to the eye. Sometimes a section of the vitreous pulls the fine fibers away from the retina all at once, rather than gradually, causing many new floaters to appear suddenly. This is called a vitreous detachment, which in most cases is not sightthreatening and requires no treatment. However, a sudden increase in floaters, possibly accompanied by light flashes or peripheral (side) vision loss, could indicate a retinal detachment. A retinal detachment occurs when any part of the retina, the eye's light-sensitive tissue, is lifted or pulled from its normal position at the back wall of the eye. A retinal detachment is a serious condition and should always be considered an emergency. If left untreated, it can lead to permanent visual impairment within two or three days or even blindness in the eye. Those who experience a sudden increase in floaters, flashes of light in peripheral vision, or a loss of peripheral vision should have an eye care professional examine their eyes as soon as possible. For people who have floaters that are simply annoying, no treatment is recommended. On rare occasions, floaters can be so dense and numerous that they significantly affect vision. In these cases, a vitrectomy, a surgical procedure that removes floaters from the vitreous, may be needed. A vitrectomy removes the vitreous gel, along with its floating debris, from the eye. The vitreous is replaced with a salt solution. Because the vitreous is mostly water, you will not notice any change between the salt solution and the original vitreous. This operation carries significant risks to sight because of possible complications, which include retinal detachment, retinal tears, and cataract. Most eye surgeons are reluctant to recommend this surgery unless the floaters seriously interfere with vision. I could find no relation between temporal arteritis, or optic neuritis, and floaters. 77. Age-related macular degeneration (ARMD) See question 86 for more complete explanation of ARMD. Regarding the parts to this question unanswered in the explanation for question 86, Once dry AMD reaches the advanced stage, no form of treatment can prevent vision loss. However, treatment can delay and possibly prevent intermediate AMD from progressing to the advanced stage, in which vision loss occurs. The National Eye Institute's Age-Related Eye Disease Study (AREDS) found that taking a specific high-dose formulation of antioxidants and zinc significantly reduces the risk of advanced AMD and its associated vision loss. Slowing AMD's progression from the intermediate stage to the advanced stage will save the vision of many people. People who are at high risk for developing advanced AMD should consider taking the formulation. You are at high risk for developing advanced AMD if you have either: 1. Intermediate AMD in one or both eyes. 2. Advanced AMD (dry or wet) in one eye but not the other eye AMD is detected during a comprehensive eye exam that includes: - Visual acuity test: This eye chart test measures how well you see at various distances. - Dilated eye exam. Drops are placed in your eyes to widen, or dilate, the pupils. Your eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of AMD and other eye problems. After the exam, your close-up vision may remain blurred for several hours. - Tonometry. An instrument measures the pressure inside the eye. Numbing drops may be applied to your eye for this test. Your eye care professional also may do other tests to learn more about the structure and health of your eye. During an eye exam, you may be asked to look at an Amsler grid. The pattern of the grid resembles a checkerboard. You will cover one eye and stare at a black dot in the center of the grid. While staring at the dot, you may notice that the straight lines in the pattern appear wavy. You may notice that some of the lines are missing. These may be signs of AMD. (See Amsler grid.) If your eye care professional believes you need treatment for wet AMD, he or she may suggest a fluorescein angiogram. In this test, a special dye is injected into your arm. Pictures are taken as the dye passes through the blood vessels in your retina. The test allows your eye care professional to identify any leaking blood vessels and recommend treatment. 78, Patients with ectropion have a sagging lower eyelid that leaves the eye exposed and dry. It is caused by a lack of tone of the delicate muscles that hold the lid taut against the eye. Excessive tearing (epiphora) is common with ectropion. BCC’s do not metastasize. SCC’s however, can readily metastasize. Molluscum contagiosum is a disease caused by a poxvirus of the Molluscipox virus genus that produces a benign self-limited papular eruption of multiple umbilicated cutaneous tumors. This common viral disease is confined to the skin and mucous membranes. Transmission requires direct contact with infected hosts or contaminated fomites. It is generally thought to infect humans exclusively, but there are a few isolated reports of Molluscum contagiosum occurring in chickens, sparrows, pigeons, chimpanzees, kangaroos, a dog, and a horse. The infection is found worldwide and has a higher incidence in children, sexually active adults, and those who are immunodeficent. A chalazion forms when the meibomian gland becomes blocked. If the gland ruptures through the tarsal plate, granulation tissue results. Acne rosacea and chronic blepharitis are 2 predisposing skin and eyelid conditions that affect true incidence. Dry eye syndrome may be another associated factor. Males more commonly are affected, possibly from increased androgenic hormone and associated skin changes arising from that hormone's effect. Chalazia are more common in adults than in children. A chalazion is usually a painless swelling on the eyelid that has been present for weeks to months. Patients may seek medical attention when a chalazion causes impaired vision, double vision, discomfort, or pain or becomes inflamed and painful, or infected. To conservatively manage chalazia, apply warm compresses for 15 minutes (4 times per day on outpatient basis). More than 50% of chalazia resolve with conservative treatment. Defer steroid injections and surgical drainage to an ophthalmologist or plastic surgeon. Recognize that injection and removal of chalazia may create cosmetic morbidity (see below). Ophthalmology texts indicate that topical or systemic antibiotics are not necessary. Refer patients for follow-up care with an ophthalmologist after 2 weeks if conservative management does not completely resolve the chalazion. 79. A cataract is an opacification of the lens. Congenital cataracts usually are diagnosed at birth. If a cataract goes undetected in an infant, permanent visual loss may ensue. Not all cataracts are visually significant. If a lenticular opacity is in the visual axis, it is considered visually significant and may lead to blindness. If the cataract is small, in the anterior portion of the lens, or in the periphery, no visual loss may be present. Unilateral cataracts are usually isolated sporadic incidents. They can be associated with ocular abnormalities (eg, posterior lenticonus, persistent hyperplastic primary vitreous, anterior segment dysgenesis, posterior pole tumors), trauma, or intrauterine infection, particularly rubella. Bilateral cataracts are often inherited and associated with other diseases. They require a full metabolic, infectious, systemic, and genetic workup. The common causes are hypoglycemia, trisomy (eg, Down, Edward, and Patau syndromes), myotonic dystrophy, infectious diseases (eg, toxoplasmosis, rubella, cytomegalovirus, and herpes simplex [TORCH]), and prematurity. Visual morbidity may result from deprivation amblyopia, refractive amblyopia, glaucoma (as many as 10% post surgical removal), and retinal detachment. Metabolic and systemic diseases are found in as many as 60% of bilateral cataracts. An irregular red reflex is the hallmark of visual problems. If an irregular red reflex is detected at the initial screening, this is usually an indication that a congenital cataract might be present and an ophthalmology consultation is warranted. Cataract surgery is the treatment of choice and should be performed when patients are younger than 17 weeks to ensure minimal or no visual deprivation. Most ophthalmologists opt for surgery much earlier, ideally when patients are younger than 2 months, to prevent irreversible amblyopia and sensory nystagmus in the case of bilateral congenital cataracts. The delay in surgery is because of glaucoma. Since glaucoma occurs in 10% of congenital cataract surgery, many surgeons delay the cataract surgery. Of persons with unilateral cataracts, 40% develop vision of 20/60 or better. Of persons with bilateral congenital cataracts, 70% develop vision of 20/60 or better. I would suggest that this data implies that unilaterally cataracts have a poor prognosis. Also, I found an editorial in BMJ that read “Some might protest that visual results are notoriously poor after surgery for a unilateral congenital cataract. Why drag the family and child through all the turmoil required for the treatment of infantile cataracts for, at best, a "spare eye"? The answer is simple: two eyes are better than one.” I’m guessing this implies that it’s generally agreed that unilateral congenital cataract has a poor prognosis The prevalence of congenital cataracts in unilateral and bilateral cataracts has been studied in UK and Australia, where the rates found that MOST (90-95%) hereditary congenital cataracts are bilateral and about 50-65% of sporadic congenital cataracts are bilateral. In total, 34% (UK) and 42% (Australia) of ALL congenital cataracts are unilateral. Treatment of Chlamydial infections is with oral tetracycline or erythromycin. Cataracts can cause strabismus, and esotropia (manifest strabismus) is most common. 80. Cataracts can be caused by: Ocular factors include: - trauma - high myopia - recurrent uveitis - steroid use (topical) - radiation (UV/IR/ionising) Systemic factors include: - age - diabetes mellitus - Drugs: - steroids - amiodarone - miotics - phenothiazines - atopy - galactosemia - hypocalcemia - Diseases: - Down’s syndrome - Lowe’s syndrome - Dystrophia myotonica I don’t think Penicillin can cause cataracts; in fact it’s used in post-cataract antibiotic prophylaxis against infection. I couldn’t find anything online or in BNF suggesting it would. Phacoemulsification has gained in popularity in recent years, and is now the preferred form of cataract removal. Although this procedure has been available to us for a long time, recent advances and refinements in machine and microsurgical instruments have made it safer and more effective than previously. The technique of phacoemulsification utilizes a small incision. The tip of the instrument is introduced into the eye through this small incision. Localized high frequency waves are generated through this tip to break the cataract into very minute fragments and pieces, which are then sucked out through the same tip in a controlled manner. A thin 'capsule' or shell is left behind after cleaning up of the entire opaque cataract. In a conventional surgery the incision required is larger (10-12 mm) and requires stitches for closing. This larger incision takes 6-8 weeks to heal. Moreover, the stitches can cause distortion of the normal curvature of the cornea (the clear part of eye) and thus lead to astigmatism and blurred vision because of this. The replacement of a lens with opacity (cataract) with a prosthetic lens, as is done in cataract surgery, usually means loss of accommodation since the implanted lens is rigid. However, recent advances have made an accommodating intraocular lens called Crystalens available. Given this is a recent advance, loss of accommodation is still typical after surgery. Causes of leucocoria in children include: - cataract - retinoblastoma - toxocara granuloma - advanced retinopathy of prematurity - corneal opacity - Coat’s disease - vitreous development 81. Optic neuritis causes central scotoma, as does macular degeneration. Arcuate scotorma is caused by glaucoma. Pituitary adenoma most commonly produces a bitemporal hemianopia Cerebral vascular accident can cause homonymous hemianopia. Cataracts present with difficulty seeing at night, haloes around lights, and being sensitive to glare. 82. Basal cell carcinomas, while being locally invasive and destructive, do not metastasize. Scarring on the outside of the eye causes ectropion while conjunctival scarring causes entropion. Aging is the major cause of both entropion and ectropion. By “around eye” are we to mean the skin or the conjunctiva? Since I assume it includes both, it MAY cause entropion or ectropion. A capillary hemangioma develops after birth and usually resolves by school age. Treatment with steroids may rarely be needed to prevent amblyopia. Malignant eyelid tumors are: - 85-90% BCC - 5% SCC - 1-5% sebaceous cell carcinoma (arises from glands) - 1% MM Congenital ptosis can partially or completely cover the pupil and thus obscure vision, inhibit normal vision, and cause amblyopia. Yes, a child should be observed whether or not the visual axis is obscured-without it being obscured the risks are minimal. 83. Conjunctivitis is split into infective or non-infective conjunctivitis. Of the infective causes, there is bacterial conjunctivitis, viral conjunctivitis and chlamydial condunctivitis (serotypes A-C trachoma, serotypes D-K STD young adult subacute follicular conjunctivitis. Bacterial conjunctivitis papillae/velvet…purulent discharge Viral conjunctivitis follicles/rice…watery discharge Chlamydial conjunctivitis A-C: entropion, dry eye, corneal ulceration, Scarring, blindness D-K: subacute follicular…watery discharge Conjunctival follicles are germinal centers containing B cells mostly (so A is true). Mutton-fat keratic precipitates forming translucent rings with opaque centers in the anterior chamber, and occurring in uveitis. Since uveitis can occur in several granulomatous conditions (TB/Sarcoidosis/Syphilis), I’m guessing this is true. Vernal and atopic keratoconjunctivitis refer to a spectrum of chronic allergic conjunctivitis occurring especially in atopic patients. IgE mediates atopia and thus mediates vernal conjunctivitis. Allergic conjunctivitis can be rapidly relieved by topical cromoglycate. Vernal or chronic allergic conjunctivitis can also be treated with sodium cromoglycate, but often steroids are also needed. 84. Astigmatism occurs when the light is focused onto different planes depending on it’s origin. Correction requires a lens. An excimer laser is used to correct refractive errors. A YAG laser is used for posterior capsulotomy or peripheral iridotomy. Argon and KRYPTON are the (SUPERMAN) lasers cause they can almost do everything! They can be used in diabetic maculopathy, retinal/iris neovascularization, retinal breaks, destroy neovascular membrane on choroids, laser trabeculoplasty. I wish I were a Krypton laser. Corneal inflammation is primarily viral, and of the viruses, herpes simplex 1 is the major cause (with VZV and adenovirus contributing also) Dendritic ulcers are branching patterned, and affect the epithelium (in which case heals without scar) or stroma (some degree of scarring will occur). They are caused by HSV or VZV. Keratoconus (kehr-a-toh-KOH-nus) is a non-inflammatory condition in which the center of the cornea progressively thins and develops a cone-shaped bulge that blurs and distorts vision. A normal cornea is round, with even curvature like that of a sphere. But with keratoconus, the curvature is irregular and too steep, like the narrow end of an egg. Corneal grafting, medically known as epikeratophakia, consists of an eye surgeon grafting a layer of corneal epithelial (surface or skinlike) cells from the patient's own cornea in the upper layer around the central cone to build up and flatten the slope of the cornea. The success rate compares to that of corneal transplants (90%), but it offers the advantage of not requiring donated tissue. 85. Subluxation of the lens is associated with. - trauma (most common cause) - hereditary causes: - autosomal dominant (chromosome 15) - ectopia lentis et pupillae (autosomal recessive condition of asymmetric pupils, displaced opposite direction to lens dislocation) - Systemic condition: - Marfans (fibrillin-1 defect) - homocystinuria - Weil-Marchesani syndrome (rare) - sulfite oxidase deficiency (extremely rare) - hyperlysinemia (very extremely rare) VERY rare systemic: - Ehlers-Danlos (collagen defect) - Refsum syndrome (increased phytanic acid causing polyneuritis, nerve deafness, night blindness, cardiomyopathy, ataxia…autosomal recessive) - Sturge-Weber syndrome (trigeminal port wine stain + seizures) - Pierre-Robin syndrome - primary ocular disorders: - congenital glaucoma/buphthalmos - syphilis - chronic uveitis - retinitis pigmentosa - intraocular tumor - high myopia Ectopia lentis causes refractive problems and secondary glaucoma. Partial dislocation tends to be more symptomatic. Anterior lenticonus is considered a characteristic sign of Alport’s syndrome. Lenticonus is a condition whereby the central part of the front surface of the lens of the eye has a much steeper curvature than normal and bulges forwards in a blunted cone. Compare keratoconus (cone shaped curvature to cornea, getting sharper as years go on). Both keratoconus and lenticonus are non-inflammatory conditions of thinning of the central core of the cornea or the lens, respectively. Cataract surgery is the treatment of choice for congenital cataracts and should be performed when patients are younger than 17 weeks to ensure minimal or no visual deprivation. Most ophthalmologists opt for surgery much earlier, ideally when patients are younger than 8 weeks, to prevent irreversible amblyopia and sensory nystagmus in the case of bilateral congenital cataracts. The delay in surgery is because of glaucoma. Since glaucoma occurs in 10% of congenital cataract surgery, many surgeons delay the cataract surgery. The limbus is the scleral-corneal junction. The limbus has many functions including nourishment of the peripheral cornea (supplies oxygen), mitotic capacity for corneal epithelial healing, immunosurveillance of the eye surface, and hypersensitivity reactions. It also contains the pathways of aqueous humor outflow and is therefore involved in regulation of intraocular pressure. 86. According to the American Eye Institute: AMD (age-related macular degeneration) is the leading cause of vision loss in Americans 60 years of age and older. The dry form is much more common. More than 85 percent of all people with intermediate and advanced AMD combined have the dry form. However, if only advanced AMD (implies visual loss) is considered, about twothirds of patients have the wet form. Because almost all vision loss comes from advanced AMD, the wet form leads to significantly more vision loss than the dry form. All people who have the wet form had the dry form first Now, what’s the difference between the wet and dry forms? The dry form is also known as the non-exudative form. There is atrophy of retinal pigment epithelial change in photoreceptor outer segments. The dry form causes: - drusen (small discrete yellowish deposits; they do NOT cause visual loss by themselves) - RPE atrophy and photoreceptor degeneration - gradual central visual field loss The wet form is also known as the exudative form because it includes neovascularization from choroids (vascular) to the retina. These new blood vessels tend to be very fragile and often leak blood and fluid. The blood and fluid raise the macula from its normal place at the back of the eye. Damage to the macula occurs rapidly. Given that wet AMD arises from dry AMD and drusen are present in dry AMD, it would be sensible to think that wet AMD also has drusen as a common feature. However, the lone picture in the text of the retina shows that the neovascularization can obscure the visualization of drusen, so while we know it has to be there as a result of wet AMD arising from dry AMD, it can’t be seen…Any ideas? I’ll put false… 87. Retinal artery occlusion typically cause severe painless visual loss. Arterial occlusion can involve the central artery itself or one of its branches. The most common cause is embolus from the carotid artery. If an embolus passes within the retinal vasculature, it can cause transient rather than permanent visual loss, but a stationary embolus produces retinal failure beyond the point of obstruction. It may be asymptomatic if the embolus is far from the macula, but central arterial occlusions present with sudden onset of severe monocular loss of vision. A marked relative afferent pupillary defect is almost always present in central, and often present in branch retinal arterial occlusions. A couple weeks may pass before a “cherry-red spot” is seen. (highly vascular choroid seen through the ischemic retina). NEOVASCULARIZATION is UNCOMMON in retinal arterial occlusion. Flame/dot/blot hemorrhages are present in retinal vein occlusion but not in retinal artery occlusion. In a retinal artery occlusion, changes visible on fundoscopy include: - retinal arteriole thinning - white/opaque retina (devoid of glistening appearance) - cherry-red spot (due to vascularized choroids visible through white retina) - cotton wool spots - emboli visible in arterioles While giant cell arteritis usually causes ischemic optic neuropathy, it can sometimes lead to emboli and retinal artery occlusion, and thus must be considered. 88 and 89. Retinal vein occlusion can occur centrally (central retinal vein) or a tributary (“branch” retinal vein occlusion). Thrombosis occurs in the vessel lumen, because of hyperviscosity or vessel wall inflammation. Arteriovenous crossing points are common sites of branch retinal vein occlusions. Clinically, patients are middle-ages or elderly, and present with sudden painless loss of vision with or without a relative afferent pupillary defect. Fundoscopy flame/dot/blot hemorrhage, cotton wool spots, swollen optic disc, macular edema Complications of retinal vein occlusion: - macular edema - neovascularization of iris and retina (treat with laser) - neovascular glaucoma (occurs in ischemic areasiris rubeosis severe painful glaucoma) Ischemic retinal vein occlusion, as a rule, presents with sudden painless loss of vision. The branch retinal vein occlusion tends to cause visual loss in the area supplied by the branch and thus total loss of vision is very uncommon. Retinal vein occlusion is divided into TWO types, ischemic retinal vein occlusion (presents with sudden painless loss of vision) or non-ischemic retinal vein occlusion (~70% total, usually asymptomatic). Non-ischemic retinal vein occlusions may develop to ischemic retinal vein occlusions (1/3 of cases within 4 years); however, on their own they do not cause ischemia and thus no neovascularization is found. Treatment of areas of macular edema with argon laser can improve visual acuitywhether it’s in the majority of cases or not (as it is in diabetes) I’m not sure. 90. Giant cell arteritis is an inflammatory granulomatous arteritis of large arteries, occurring as a systemic disease in the elderly. It presents with severe headaches, scalp tenderness (combing hair is painful), jaw claudication while eating, and sudden painless temporary or permanent visual loss. Investigations will show a raised CRP, raised ESR, pathognomonic temporal artery biopsy. However, neither a low ESR nor a negative biopsy exclude the diagnosis. Giant cell arteritis requires immediate high dose corticosteroids to reduce risk of irreversible visual loss and other focal ischemic lesions. Bilateral blindness is a risk if untreated. Duration of therapy is 12-36 months for 75% of patients and may need to be longer in 25% of patients. GCA typically involves inflammation of the aortic arch and its branches, but almost any artery of the body as well as some veins may be affected occasionally. The inflammation tends to involve the arteries in a segmental or patchy manner, although long portions of arteries may be involved. The likely determinant of arterial susceptibility to GCA is the presence and/or quantity of internal elastic lamina within the vessel wall. For example, intracranial cerebral vasculature is not affected in GCA because these vessels lack an internal elastic lamina. Visual symptoms are present in about 33% of patients; 40-50% are transient (amaurosis fugax and diplopia) and 50-60% are permanent. Regarded as one of the more serious complications of GCA is the onset of blindness from involvement of the ophthalmic artery. Permanent visual loss may be partial or complete and may occur without warning; about 50% are unilateral and 50% are bilateral. Varied visual symptoms including blurring of vision, diplopia, and loss of vision occur in 36-60% of patients. Rarely, the inflammatory process may weaken the aortic wall, leading to localized aneurysm formation, aortic annular dilatation, and aortic regurgitation. Narrowing or occlusion of the branch vessels of the thoracic aorta (clinically referred to as aortic arch syndrome) may be found in 9-14% of cases, producing symptoms similar to those of Takayasu arteritis (decreased upper extremity pulses and blood pressure, arm or leg claudication, Raynaud phenomenon, transient ischemic attacks, coronary ischemia, and abdominal angina). Aortic aneurysms, aortic regurgitation, and aortic dissection occur less commonly. Evans and colleagues reported aortic aneurysms occurring in 15% of patients at a median of 6 years after the GCA initially was diagnosed. Two thirds were thoracic aortic aneurysms, with the majority located in the ascending aorta. Almost 33% developed symptomatic aortic regurgitation. Involvement of major vessels (aorta) predisposes patients to higher risks for death. In Evans and colleagues' report, 50% of those with thoracic aortic aneurysms died suddenly from aortic dissection. The most common cause of vision loss is AION. Examination of the fundus may reveal optic disc edema, with or without splinter hemorrhages along the disc margin. Arteritic AION, as in GCA, typically presents with a chalky white edematous optic disc. Automated visual field testing typically reveals an inferior altitudinal defect, inferior nasal sectorial defect, or central scotoma. Other important vascular ophthalmic presentations of GCA include posterior ischemic optic neuropathy, central retinal artery occlusion, branch retinal artery occlusion, and choroidal ischemia. Given retinal vein occlusion is nowhere on the emedicine.com list, I’m saying false. Just for interest sake, the types or vasculitides (cool word…repeat the last part loudly as frequently as possible without laughing) include: - small-vessel (Wegener’s granulomatosis, Churg-Strauss, Henoch-Schonlein purpura, cryoglobinemic vasculitis) - medium vessel (Polyarteritis nodosa, Kawasaki’s disease) - large vessel (Temporal arteritis, Takayasu’s arteritis) 91. Diabetic retinopathy is NOT the commonest cause of blindness in 25-75 year age group. The most common registrable cause is age-related macular degeneration, but prevalence of bilateral visual impairment is about 30%, and 75% of these have remediable problems (30% cataract, 8% macular degeneration). Application of an ocular laser is the chief treatment in diabetic retinopathy, once diabetic control and hypertensive control have been maximized. In areas of macular edema, laser reduces leakage and improves resorption of retinal edema. Treatment of preproliferative retinopathy remains controversial, but severe changes warrant prophylactic laser application. It can be assumed then that background retinopathy should not be treated with laser. The laser is targeted at ischemic areas to reduce neovascular stimulus. Most laser therapy can be performed as out-patient procedure using topical anesthesia. (I’ll assume “global” means to the globe which I’ll assume is the effect of topical anesthesia?). While macular edema does occur in proliferative retinopathy, the classic lesions for the three types of diabetic retinopathy are as follows: Background dot-blot hemorrhage, exudates, edema, microaneurysms Preproliferative cotton wool spots (swollen axonal endings), IRMAs (IntraRetinal Microvascular Anomalies), venous beeding Proliferative NVD and NVE (new vessels at disc or elsewhere) 92. Acids coagulate proteins so tend not to penetrate the eye. Alkalis, however, cross cell membranes, penetrating conjunctiva and cornea and passing deep into eye. Corneal opacification, glaucoma and cataract can result. An orbital blow out fracture always presents with a history of blunt ocular trauma. Blow-out fracture is usually caused by a large, low-velocity object like a fist or ball. Patient may present with pain, local tenderness and diplopia. Complaints of intense pressure feeling or eye swelling may also be reported. Signs include: - edema of lid tissues - restriction of vertical movement - orbital crepitus (subcutaneous emphysema)palpate bony rim and air “pops” “emphysema”=a pathological collection of air in tissues or organs. - hypoesthesia of ipsilateral cheek (entrapped infraorbital nerve) - epistaxis (communication between orbit and maxillary sinus - proptosis at first (swelling pushes eye forward at first) - enophthalmic (eye drops down and back as swelling subsides) Blow-out fracture may result in cases of abrupt trauma to the eye by any object >5cm in diameter. Because the orbital rim is very strong, the forces of blunt trauma are reflected back, compressing the eye and creating a tremendous increase in pressure within the orbit. Since the larger bones which comprise the orbit contain sinuses, the orbital walls are at great risk for fracture; should the trauma be of sufficient force, these walls can literally "blow out." The medial wall (ethmoid bone) is occasionally affected. But most commonly, the orbital floor (the superior aspect of the maxillary bone) sustains the damage. In cases of floor fractures, the eye may partially drop down into the maxillary sinus, causing enophthalmos and entrapment of the inferior rectus or inferior oblique muscle. This entrapment leads to a tethering effect, resulting in a limited downgaze ability and, more notably, an inability toward upgaze in the affected eye. While this situation can be surgically corrected in the early stages, prolonged entrapment leads to fibrosis of the muscle(s) and permanent motility impairment. Associated medial wall fractures may induce damage to the medial rectus muscle and/or the lacrimal apparatus, but this is uncommon. Any penetrating eye injury requires Xray or CT scan and ophthalmological referral. The consequences of failure to identity a foreign body are major and include intraocular infection (short-term), retinal detachment (medium-term) and siderosis (long-term). Siderosis involves the deposition of toxic ferrous ions into retina (permanent visual loss), iris (heterochromia) and trabecular meshwork (glaucoma). Blunt or perforating trauma can each cause cataract. Cataracts caused by blunt trauma classically form stellate/rosette-shaped posterior axial opacities that may be stable or progressive, whereas penetrating trauma with disruption of lens capsule forms cortical changes that may remain focal if small or may progress rapidly to total cortical opacification. So: BLUNT trauma posterior subcapsular cataract PERFORATING trauma cortical cataract 93. Retinal detachment refers to separation of the inner layers of the retina from the underlying retinal pigment epithelium (RPE, choroid). The choroid is a vascular membrane containing large branched pigment cells sandwiched between the retina and sclera. Separation of the sensory retina from the underlying RPE occurs by the following 3 basic mechanisms: Rhegmatogenous: A hole, tear, or break in the neuronal layer allowing fluid from the vitreous cavity to seep in between and separate sensory and RPE layers Traction: Traction from inflammatory or vascular fibrous membranes on the surface of the retina, which tether to the vitreous Exudative: Exudation of material into the subretinal space from retinal vessels such as in hypertension, central retinal venous occlusion, vasculitis, or papilledema The most common worldwide etiologic factors associated with RD are myopia (ie, nearsightedness), aphakia (absence of lens in eye), pseudophakia (ie, cataract removal with lens implant), and trauma. Approximately 40-50% of all patients with detachments have myopia, 30-40% have undergone cataract removal, and 10-20% have encountered direct ocular trauma. Traumatic detachments are more common in young persons, and myopic detachment occurs most commonly in persons aged 25-45 years. Although no studies are available to estimate incidence of RD related to contact sports, specific sports (eg, boxing and bungee jumping) have an increased risk of RD. Systemic diseases associated with retinal detachment include the following: o o Diabetes Tumors (eg, breast cancer, melanoma) o o o o o Angiomatosis of the CNS Sickle cell disease Leukemia Eclampsia Prematurity Symptoms of retinal detachment include flashing lights (photopsia), floaters and vision loss (patient won’t notice until central vision affected). Detachments anterior to the equator of the eye can’t be observed using visual field testing. Other patients present when central vision is lost, which may represent retinal detachment involving the macula (central retina). Because the macula is responsible for central vision, these patients have a less favorable prognosis than patients with a peripheral retinal detachment. The duration of retinal detachment is critical to the prognosis, i.e., the longer the detachment, the worse the prognosis. Patients with macular detachment for even one day have reduced postoperative visual acuity, i.e., preoperative acuity correlates with postoperative acuity. Eighty-five to 90% of patients with preoperative acuity of 20/30 or better will have postoperative acuity of 20/30 or better. Overall, retinal detachment surgery is successful in reattaching the retina in more than 90% of cases. Posterior scleritis is quite rare, but usually presents with poor or double vision, severe pain, proptosis (forward displacement of the eye), uveitis (inflammation inside the eye), and limitation of eye movement. An exudative retinal detachment (fluid under the retina) may cause severe visual loss. 94. With increasing age (particularly after 40), deformability of the lens reduces, accommodation begins to fail and the point of closest focus falls further and further from the eye. This phenomenon is called presbyopia and is corrected by a convex lens (reading glasses). Myopia (short-sightedness) occurs cause the eye is too big or the lens convexity excessive, leading to the focus in front of the retina. It is corrected by a concave (aka divergent) lens. Hypermetropia (far-sightedness) occurs cause the eye is too small or the lens convexity too small, leading to the focus behind the retina. It is corrected by a convex (aka convergent) lens. Hypermetropia predisposes to a convergent squint, which can be corrected by hypermetropic spectacles. 95. The etiological basis of proptosis can be traumatic, inflammatory, vascular, infectious, or neoplastic. In adults, thyroid orbitopathy is the most common cause of unilateral and bilateral exophthalmos. Infectious: - orbital cellulitis - mucormycosis - concurrent sinus disease Inflammatory: - thyroidopathy - orbital inflammation (pseudotumor, benign orbital inflammation) Vasculitis: Neoplastic: - Wegeners - Churg-Strauss - lacrimal gland tumors - lymphoma/leukemia - meningioma - glioma Trauma Vascular: - orbital arteriovenous malformation or venous malformation Pseudoproptosis: - buphthalmos - contralateral enophthalmos - ipsilateral lid retraction (may be caused by CN VII palsy, but this isn’t a TRUE proptosis). 96. Kayser-Fleisher refers to “Keyser-Fleisher rings,” copper deposite in the iris that are seen in Wilson’s disease. Argyll-Robertson pupils are seen in syphilis, and refer to bilateral “light-near dissociation” secondary to disruption of the internuncial neurons in the pre-tectal nucleus. It causes “prostitute’s pupils” to form- they accommodate (“near”) but don’t react (“light”). Weill-Marchesani syndrome is a rare, genetic disorder characterized by short stature; an unusually short, broad head (brachycephaly) and other facial abnormalities; hand defects, including unusually short fingers (brachydactyly); and distinctive eye (ocular) abnormalities. These typically include unusually small, round lenses of the eyes (spherophakia) that may be prone to dislocating (ectopia lentis) as well as other ocular defects. Due to such abnormalities, affected individuals may have varying degrees of visual impairment, ranging from nearsightedness (myopia) to blindness. Researchers suggest that WeillMarchesani syndrome may have autosomal recessive or autosomal dominant inheritance. Hudson-Stahli line refers to a line in the corneal epithelium commonly seen in the junction between the middle and lower third cornea. It is often seen in the elderly and causes no symptoms and is of clinical significance (this is according to emedicine.com…this begs the question why the HELL do we have to learn it?). Holmes-Adie pupil refers to damage to the postganglionic parasympathetic fibres in the orbit, causing poor reaction to light and to accomodation. Diagnosis is with 0.1% pilocarpine. Other cute papillary abnormalities to know about are Horner’s and Marcus-Gunn (relative afferent papillary defect, causes include optic neuritis, retinal detachment, severe “wet” macular degeneration). 97. Causes of lid retraction include - thyroid eye disease (most common cause) - ocular surgery (overcorrected ptosis or squint) - Ocular: - contralateral ptosis - myopia - Neurological:- hydrocephalus - dorsal mid-brain syndrome - congenital - systemic: - cirrhosis - Cushings - COPD - SVC syndrome - medications: - lithium - steroids Please don’t ask me to explain this as I have found no satisfactory explanation for any of them really… Facial nerve causes closure of the eyelids by it’s innervation of orbicularis oculi. This muscle contains a palpebral part, which can gently close the lids, and a orbital part which tightly closes them. Levator palpebrae superioris is a thin flat muscle of the superior eyelid, supplied by oculomotor nerve, and elevates superior eyelid. Oculomotor nerve palsies commonly cause lid retraction and “down and out” eyes… 98. The syringing in the question describes the caloric test. This uses differences in temperature to diagnose ear nerve damage as a cause of dizziness or vertigo. Damage to the vestibular portion of the nerve of the inner ear (acoustic nerve) is a common cause of vertigo. Cold water is placed in the ear canal with a bulb syringe. This should cause nystagmus. This test is then repeated using warm water, and then cold and warm water are done in the opposite ear. The nystagmus should occur in the opposite direction (towards the warm water then slowly away, rather than away from the water and slowly back). The injection of cold water should move the eyes away and injection of warm water move eyes toward, the ear injected. Injection of cold water into the right ear should cause horizontal nystagmus to the left. BOTH eyes will move to the left, so uniocular nystagmus (E), vertical nystagmus (D) and convergence nystagmus (C) are all false, as are A and B. 99. Myopia, or “short sighted” implies that the image is focusing in front of the retina, usually because of hyperrefraction or an enlarged eyeball. Hypermetropia, on the other hand, or “far-sightedness” implies that the image is focusing behind the retina (image goes too “far” before focusing). This results from inadequate refraction of the lens or an eyeball that is too small (bet ya my daddy’s eyeball is bigger than yer daddy’s eyeball!). To correct myopia, a concave lens is needed, while in hypermetropia, a convex lens is needed. Errors of refraction are best treated using spectacles or contact lenses. Of course, we already learned that contact lens wearing can predispose us to getting acanthamoeba keratitis. Atropine is a parasympathetic antagonist, causing disruption of the parasympathetic stimulation of constrictor pupillae (via CN III), and thus pupil dilatation. Being myopic does not disrupt this pathway and thus the pupils will still dilate. Exophoria is the turning out of the eye when it is covered. Esophoria is the turning in of the eye when it is covered. They are otherwise known as latent squints. Primary exotropia is associated with myopia. Convergent squints (esotropias and esophorias) are non-refractive if they present early but can be due to hypermetropia when they present later in childhood. Thus I say this is true. 100. Endocrine exophthalmos refers thyroid eye disease. This can result in bulging of the eyes, retraction of the lids, double vision, decreased vision, and ocular irritation. This is often associated with abnormalities in thyroid gland function (either too much thyroid (Graves' disease) or too little (Hashimoto's thyroiditis)). The eye findings of thyroid orbitopathy may be independent of treatment of your thyroid abnormalities and may not resolve in spite of the fact that the thyroid is now "controlled." These symptoms may be present even if your thyroid has no apparent problems. The inferior rectus, superior rectus, lateral rectus and medial rectus, are most frequently involved. These muscles originate behind the eye at the peak of the eye socket and attach to the eye just behind the cornea (the clear portion of the eye overlying the colored part of the eye). The muscles cannot be seen on the surface as they are covered by a thin layer of tissue (the conjunctiva) but may become visible as the blood vessels over their anterior portion become very prominent. The immune system singles out the fibroblasts, support cells within the muscles causing the muscles to enlarge. With muscle enlargement the globe (eyeball) is pushed forward leading to the characteristic "stare." In addition, the muscles become stiff and the upper lid tends to retract, pulling away from the colored portion of the eye. The eyes may become red due to difficulty closing as well as increased prominence of the blood vessels. If the muscles get large enough, they may press on the optic nerve causing damage to the nerve (necessitating steroids or surgery to decompress the nerve). Upper lid elevation, particularly when looking down, is very characteristic of thyroid orbitopathy. The eyes frequently bulge forward and the blood vessels on either side of the pupil tend to become dilated. The lids often don't close completely at night and there is resistance to pushing the globes posteriorly within the orbit. The pupils may not react normally and the eyes may be limited in their movement. Pressure inside the eye may be high particularly while looking in one direction. Eye symptoms include: - proptosis (unilateral or bilateral) - swelling of eyelids/conjunctiva - diplopia (because of proptosis and infiltration of recti) - decreased vision - red/swollen conjunctiva (chemosis) - exposure of cornea (secondary to proptosis) causing ulceration - increase in intraocular pressure causing glaucoma - optic nerve compression causing severe or total visual loss. Surgery to cause ptosis can be done to assure the upper lid covers the cornea more appropriately. Causes of ptosis include: - Horner’s (thanks to Muller’s muscle) - Myasthenia gravis - Trauma - CN III palsy - Post eye surgery 101. Subluxation of the lens is also known as lens dislocation or ectopia lentis. It is caused by: - trauma (most common cause) - hereditary causes: - autosomal dominant (chromosome 15) - ectopia lentis et pupillae (autosomal recessive condition of asymmetric pupils, displaced opposite direction to lens dislocation) - Systemic condition: - Marfans (fibrillin-1 defect) - homocystinuria - Weil-Marchesani syndrome (rare) - sulfite oxidase deficiency (extremely rare) - hyperlysinemia (very extremely rare) VERY rare systemic: - Ehlers-Danlos (collagen defect) - Refsum syndrome (increased phytanic acid causing polyneuritis, nerve deafness, night blindness, cardiomyopathy, ataxia…autosomal recessive) - Sturge-Weber syndrome (trigeminal port wine stain + seizures) - Pierre-Robin syndrome - primary ocular disorders: - congenital glaucoma/buphthalmos - syphilis - chronic uveitis - retinitis pigmentosa - intraocular tumor - high myopia Ectopia lentis causes refractive problems and secondary glaucoma. Partial dislocation tends to be more symptomatic. 102. The presentation of a patient with symptoms of increased intracranial pressure and papilledema is a clinical emergency. Although this scenario may be the harbinger of a brain mass, other clinical entities should be considered. A significant number of patients presenting in the above fashion are diagnosed with the syndrome of pseudotumor cerebri. Although idiopathic intracranial hypertension, pseudotumor cerebri, and benign intracranial hypertension are synonymous with this diagnosis, the preferred term is idiopathic intracranial hypertension. The diagnostic criteria include the following: symptoms and signs restricted to those of elevated intracranial pressure; normal findings on neuroimaging studies, excluding nonspecific findings of raised intracranial pressure; and increased cerebrospinal fluid pressure with a normal composition. The disease commonly occurs in women who are overweight (ie. None of the lovely women reading this). The role of obesity in this disorder is unclear. Obesity has been proposed to increase intra-abdominal pressure, which, in turn, raises cardiac filling pressures. This rise in pressure leads to impeded venous return from the brain (due to the valveless venous system that exists from the brain to the heart) with a subsequent elevation in intracranial venous pressure. If not treated appropriately, chronic interruption of the axoplasmic flow of the optic nerves with ensuing papilledema due to this pressure may lead to irreversible optic neuropathy. If this disorder presents in an individual who is not overweight, ruling out associated risk factors is necessary. Risk factors include Systemic diseases: - Lyme disease - anemia, HTN, - MS - Reyes syndrome - sarcoidosis - SLE - thrombocytopenic purpura - pregnancy - restriction of venous drainage from head Exogenous substances (the list is so extensive…here are the ones which I can spell…): - amiodarone - antibiotics (penicillin, tetracycline, nalidixic acid) - carbidopa - levodopa - corticosteroids (being ON them or coming off them…) - danazol - growth hormone - indomethacin (the NSAID) - lead - OCP - oxytocin - lithium - phenytoin - vitamin A 103. Since men of medicine began studying the human body, anatomists and pathologists have been intrigued by the mysterious, gelatinous substance filling the eyeball. Vitreous body comprises four fifths of the globe, averaging 4 mL in an adult. Vitreous is 99% water, with collagen and hyaluronic acid comprising the remaining 1%. These components give vitreous its specific gel-like form. (for those of you still reading, that last paragraph was TOTALLY a copy and paste job). Vitreous hemorrhage is defined as the presence of extravasated blood within the space outlined by the zonular fibers and posterior lens capsule anteriorly, the nonpigmented epithelium of the ciliary body laterally, and the internal limiting membrane of the retina (lamina limitans interna) posteriorly and posterolaterally. Vitreous has firm attachments to 3 important areas of the inner eye. First, at the most anterior portion and termination of the retina (ie, ora serrata), a circular band approximately 4 mm wide forms the vitreous base. This is the strongest of all attachments and maintains its strength throughout life. Any traction of this area is transmitted to the adjacent peripheral retina. The second attachment is at the circular zone of the optic nerve head. This area progressively weakens with age and can separate with posterior vitreous detachment (PVD). As a result, one often can observe a feathery ring (ie, Weiss ring) following PVD. The third area of firm attachment occurs to the retina along the course of the major retinal vessels. Vitreous traction along the vessels may lead to partialthickness retinal breaks (ie, retinal pits) or full-thickness breaks with a bridging vessel. Tractional forces, whether traumatic or from pathologic vascularization of the retina, result in hemorrhage into the vitreous. Causes of vitreous hemorrhage include: 90% of cases from: - proliferative diabetic retinopathy posterior vitreous detachment (with or without retinal tears and/or detachment) - ocular trauma (shaken baby syndrome) Less common causes include: - retinal vein occlusion proliferative sickle cell retinopathy retinal microaneurysm age-related macular degeneration subarachnoid hemorage (Terson syndrome) The complications of vitreous hemorrhage include hemosiderosis bulbi (The vitreous contains 13 times more iron-binding proteins relative to the serum) with photoreceptor toxicity, glaucoma, severe floaters, and myopic shift in infants. Laser photocoagulation is contraindicated in vitrous hemorrhage- the blood gets in the way of the laser beam! If laser photocoagulation is wanted, wait til the blood clears, or perform a vitrectomy, then do the laser photocoagulation. Ghost cell glaucoma can occur after vitreous hemorrhage when the residual deformed red blood cells gain access to the anterior chamber and clog the trabecular meshwork resulting in increased intraocular pressure. "Ghost cells" are rigid, denatured RBCs with Heinz bodies seen inside the cells. Ghost cell glaucoma usually follows trauma to the eye (blunt or penetrating). The rbc in the posterior eye die, then 2-4 weeks passes while they pass to the anterior chamber, clog up the trabecular meshwork, then raise intraocular pressure, causing glaucoma. 104. Infection in the orbit is usually associated with infection in a paranasal sinus. Clinically, we see: - proptosis - reduced ocular movement - redness and swelling of eyelids may meningitis (does rapidly so IV antibiotics immediately!) Infective organisms: - Haemophilus influenzae - Streptococcus pneumoniae - anaerobes Orbital cellulitis occurs in the following 3 situations: (1) extension of infection from the periorbital structures, most commonly from the paranasal sinuses, but also from the face, globe, and lacrimal sac; (2) direct inoculation of the orbit from trauma or surgery; and (3) hematogenous spread from bacteremia. The medial orbital wall is thin and not only perforated by numerous blood vessels and nerves, but it also has numerous other defects (Zuckerkandl dehiscences). Ethmoid sinusitis is the most common cause of orbital cellulitis in all age groups and aerobic bacteria are the organisms most frequently responsible. Orbital cellulitis is more common in children than in adults. Median age of children hospitalized with orbital cellulitis is 7 years. Carotid-cavernous fistulas (CCFs) are abnormal communications between the carotid arterial system and the venous cavernous sinus. Most often, CCFs are broadly classified as either direct or indirect, as depicted on angiograms. Further classification is based on their etiologic and hemodynamic qualities. Clinical manifestations of CCFs frequently involve ophthalmologic abnormalities. CCFs can develop either because of trauma or spontaneous causes. Traumatic CCFs may occur after head injuries in which the intracavernous carotid artery is torn. These head injuries range from minor falls to severe penetrating wounds. In addition, iatrogenic causes resulting from endovascular therapy may contribute to traumatic CCFs. Spontaneous CCFs usually result from a ruptured carotid aneurysm; however, some have hypothesized that these fistulas may be congenital arteriovenous connections that open spontaneously in the setting of collagen vascular disease, atherosclerotic disease, hypertension, or childbirth. Signs and symptoms of CCFs can be correlated with the specific anatomy of the cavernous sinus. Because the sinus directly communicates with the ophthalmic veins, an abnormal shunt between the sinus and carotid artery can transmit arterial pressure to these veins. Concurrently, arterial perfusion to the globe is decreased. Both events lead to orbital manifestations (90% direct CCF loss of vision without treatment). Palsies involving cranial nerve III, VI, and/or VII may also be evident from mass effect in the cavernous sinus. CCFs are most frequently found in young men and in women who are postmenopausal. Orbital pseudotumor (OP) or idiopathic non-specific orbital inflammation is a non-infectious acute inflammation of the orbits, that presents with orbital swelling or a mass. It is usually unilateral, but it may be bilateral as it was in this case. It is uncommon in children but it has been reported in children as young as 3 months of age. OP may present as proptosis, eye pain, ptosis, lid edema, conjunctivitis with or without chemosis (swelling of the conjunctiva) and limitation of extraocular movements. Fever, headaches and eye discharge may be found. Orbital involvement is generally unilateral and recurrences may occur. Sometimes one can palpate a mass above the temple or under the orbital rim. Autoimmune disorders have been associated with this condition. After an imaging diagnosis is made, a biopsy may be necessary to rule out leukemia or lymphoma. The histopathology of orbital pseudotumor shows polymorphic lymphocytic and plasmacytic infiltrates with eosinophilia. Corticosteroids are the mainstay of therapy. Once started, the symptoms quickly resolve as they did in our case. In fact, the response to steroids is so pathognomonic, that the diagnosis is often made retrospectively based on the response. Capillary hemangiomas are one of the most common benign orbital tumors of infancy. They are benign endothelial cell neoplasms that are typically absent at birth and characteristically have rapid growth in infancy with spontaneous involution later in life. This is in contrast to another known group of childhood vascular anomalies, vascular malformations. Vascular malformations, such as lymphangiomas and arteriovenous malformations, are present at birth and are characterized by very slow growth with persistence into adult life. Females outnumber male patients with hemangiomas by a ratio of 3:1. Patients usually present with a unilateral, superonasal, eyelid, or brow lesion. It typically blanches with pressure, unlike the lesions seen with port-wine stains. The mass lesion may be sufficient to cause a ptosis of the involved eyelid. Alternatively, if the lesion extends posteriorly in the orbit, proptosis and visual loss may be present. Clinical signs of a capillary hemangioma include: Systemic: - hemolytic anemia - thrombocytopenia - nasopharyngeal obstruction Ophthalmic: - occlusion of visual axis - optic nerve compression - severe proptosis - anisometropia Dermatological: - erosion of epidermis - infection - cosmetic disfigurement Cavernous hemangiomas are the most common intraorbital tumors found in adults. These benign, vascular lesions are slow growing and can manifest as a painless, progressively proptotic eye. Most of these tumefactions are exceedingly unilateral. Bilateral cases have been reported but are rare. 105. Any orbital structure can give rise to a primary benign or malignant tumor, and the orbit may be involved in secondary spread from adjacent or distant sites. Primary tumors include: - Cavernous hemangioma - Meningiomas (sphenoid or optic nerve sheath most often) - Lacrimal gland tumors Lymphoma (is there anywhere this tumor ISNT found?) In kids there are a few tumors seen more often: - dermoid cysts (upper nasal or upper temporal orbit) - capillary hemangioma (develop soon AFTER birth, usually regress spontaneously by school age, but may need local steroid treatment to prevent amblyopia). Since this develops soon after birth, both statements are false. It is, however, benign. - optic nerve glioma (usually with neurofibromatosis) rhabdomyosarcoma (“may mimic orbital cellulitis”) Rhabdomyosarcoma is the most common malignant orbital tumor of childhood. The average age of onset is about 6 years. These tumors generally grow very rapidly and produce proptosis (forward displacement) of the eye. They may destroy bone and enter adjacent sinuses. A biopsy is required to confirm the diagnosis, but the tumor cannot usually be excised due to its infiltrative nature. Once the diagnosis is made, prompt radiation and chemotherapy is usually given. Optical ciliary shunt vessels are abnormal blood vessels on the optical disc, directing blood from retina to choroid. It is commonly seen in central retinal vein occlusion where the prognosis is dictated by reestablishment of patency of the venous system by recanalization, dissolution of clot, or formation of optociliary shunt vessels. Central retinal vein occlusion has been associated with several conditions, including: Systemic vascular disease: - HTN, DM Blood dyscrasias: - Polycythemia vera, lymphoma, leukemia Clotting disorders: - Hypercoaguability (including OCP) Multiple myeloma/cryoglobinemia Syphilis and sarcoidosis Autoimmune disease Exercise and alcohol consumption decrease risk of CRVO 106. Conjunctivitis can be infective or non-infective. Infective causes are bacterial, chlamydial or viral. Non-infective causes are acute allergic, chronic allergic, superior limbic keratoconjunctivitis, and cicatrial/bullous conjunctivitis. INFECTIVE conjunctivitis includes bacterial conjunctivitis. Organisms responsible for bacterial conjunctivitis include: - Staphylococcus aureus/epidermidis - Streptococcus pneumoniae - Haemophilus influenzae - Neisseria gonorrheae (unlike otherspenetrates corneal epithelium and causes keratitis) Bacterial conjunctivitis papillae (velvet like) appearance (remember “papillae/pus” for bacterial Viral conjunctivitis follicles (rice-like) According to a Norwegian study of 6763 swabs obtained over a period of four years (2001 to 2004), bacterial conjunctivitis was found with a predominance of Staphylococcus aureus (87.2%) followed by Streptococcus pneumoniae (4.7%) and gram negative rods (E.coli + Klebsiella spp. + Pseudomonas spp.) in 8.1% swabs 107. Corneal epithelium is usually well protected from microorganism entry, but bacteria can reach the stroma (past the epithelium) in the following predisposing factors: - contact lens wear - corneal trauma - herpetic keratitis - corneal exposure - corneal anesthesia - immunosuppression (steroids) - Chronically compromised ocular surface (dry eye, blepharitis, endothelial failure as occurs in Fuchs endothelial dystrophy or cornea guttata) Usually bacterial infection is seen with purulent conjunctivitis, a corneal ulcer and corneal opacity. Vision is reduced. The infection can spread to the inner eye (endophalmitis), leading to blindness. Intraocular infection is suggested by a hypopnon (white cells in anterior chamber). This requires urgent admission. Causative organisms of bacterial keratitis include: - Staph aureus and Staph epidermidis - Strep pneumoniae - Enterobacter (E.coli/Proteus/Klebsiella) - Pseudomonas aeruginosa Enterobacter belong in your bum and thus are not considered “normal” flora of the eye, unless you have an ano-ocular fistula (aka the anatomical equivalent of a finger).(I just made that up…awesome…). That being said, the staphs and streps ARE normal flora, so this may simply be a matter of knowing what they mean by “usually.” Acanthamoeba is a protozoal corneal infection causing severe unrelenting keratitis, unresponsive to antibiotic treatments. It is particularly associated with contact lens use and can grow in many contact lens solutions. Stromal keratitis occurs and intense ocular pain (disproportionate to signs). Treatment is prolonged. 108.Band keratopathy is the subepithelial deposition of calcium in the interpalpebral region. It arises secondary to chronic intraocular inflammation (including chronic uveitis, rheymatoid disease) or in association with systemic hypercalcemia (hyperparathyroidism). Symptoms of band keratopathy - reduced vision (central cornea involved) - gritty sensation (irregular overlying epithelium) Renal failure is most often associated with hyPOcalcemia and hyPERphosphatemia, so renal failure wouldn’t increase the likelihood of band keratopathy. Incidentally, risk of CATARACTS increases with hyPOcalcemia, so in theory renal failure would increase risk for cararacts. I don’t know if it’s calcium phosphate that is deposited or some other calcium salt. I will assume it’s calcium phosphate and thus this is true. 109. Mooren’s ulcer is a chronic ulceration of the marginal cornea having a serpiginous (wavy indented margin), usually bilateral formation. It is seen in the elderly and is of unknown aetiology. Sounds like this is true. 110. Causes of cataracts can be separated into ocular factors and systemic factors. Ocular factors include: - trauma - high myopia - recurrent uveitis - steroid use (topical) - radiation (UV/IR/ionising) Systemic factors include: - age - diabetes mellitus - Drugs: - steroids - amiodarone - miotics - phenothiazines - atopy - galactosemia - hypocalcemia - Diseases: - Down’s syndrome - Lowe’s syndrome - Dystrophia myotonica 111. Uveitis is inflammation of the uveal tract, which includes the iris, ciliary body and choroid. Inflammation confined to the anterior segment of the eye (in front of iris), is referred to as iritis or anterior uveitis, that involving ciliary body is referred to as intermediate uveitis and inflammation of the choroids is termed posterior uveitis. If all three regions are involved then the term pan-uveitis is used. Uveitis causes red eye, pain, blurred vision, photophobia and floaters. Each symptom is determined by the location of the inflammation so photophobia and pain are common in iritis while floaters are seen in posterior uveitis. Uveitis is commonly encountered with: - ankylosing spondylitis (don’t forget HLA B-27) - arthritis (rheumatoid and seronegative like Reiters, JCA, etc) - IBD (can cause erythema nodosum) - sarcoidosis (can cause erythema nodosum) - TB (can cause erythema nodosum) - syphilis - toxoplasmosis - Behcet’s syndrome (“VASCULitiS”=Vasculitis, Arthritis, Skin lesions (erythema nodosum, papulopustular lesions), Colitis, Ulcers (oral) and UVEITIS, hLa-B51 association, Steroids treat) - lymphoma and viruses (HSV, CMV, HIV) - psoriatic arthropathy 112. Acquired primary open angle glaucoma (POAG) is the most common type of glaucoma, affecting 1% over 40 and 10% over 80. Twenty years after diagnosis, virtually all Type 1 and about 60% of Type 2 diabetics will have retinopathy detectable on examination. Does this make it 80% chance for diabetes if you don’t specify the type? I’d be willing to say true. After 30 years, 30% Type 1 and 3% Type 2 will have proliferative disease. The stages in diabetic retinopathy include background (dot-blot hemorages, exudates, edema, microaneurysms), preproliferative (cotton wool spots, venous beading, IRMA=intraretinal microvascular anomalies), proliferative (new vessels at disc (NVD) or new vessels elsewhere (NVE)). Remember that advanced disease of the retina can cause iris rubeosis, vitreous hemorage and retinal detachment. Retinoblastoma is the most common primary malignant intraocular tumor to affect children, with a frequency of 1 in 20,000. Presentation is usually at about 18 months. Family history can be found in about 6% of the tumors, transmitted on chromosome 13 as autosomal dominant trait with 80% penetrance. Retinoblastoma can grow beneath and elevate the retina, and may cause strabismus and secondary glaucoma. Retinitis pigmentosa can be autosomal dominant (4-7/100,000), autosomal recessive (4-5/100,000) or X-linked dominant (1-4/100,000), meaning a total prevalence of retinitis pigmentosa of 9-16 per 100,000, or 1 per 6000-10000. This is fairly close to 4000 and given the constant need to make things sound more common and serious in medicine, let’s say true. I have no reason to believe that females are impacted more by angle closure glaucoma. I’d say this is false. 113 and 114. Muscle Origin Insertion Superior rectus Inferior rectus Lateral rectus Medial rectus Superior oblique Common tendinous ring Common tendinous ring Common tendinous ring Common tendinous ring Body of sphenoid bone Inferior oblique Anterior floor orbit Nerve CN III (Oculomotor) Sclera Sclera Sclera Sclera Through fibrous ring, changes direction, inserts into sclera deep to superior rectus sclera deep to lateral rectus CN IV (Trochlear) CN VI (Abducent) Muscle supplied Superior rectus, inferior rectus, medial rectus Inferior oblique Sphincter pupillae and ciliary muscle Superior oblique Lateral rectus Muscle Superior rectus Inferior rectus Medial rectus Lateral rectus Inferior oblique Superior oblique Eye moves Up (elevation) and in (adduction) Down (depression) and in (adduction) In (adduction) Out (abduction) Up (elevation) and out (abduction) Down (depression) and out (abduction)