1 ADVANTAGES AND DISADVANTAGES OF VARIOUS

52
A D V A N T A G E S A N D D I S A D V A N T A G E S
O F V A R I O U S A P P R O A C H E S T O B E N I G N M A S S E S
O F M A M M A R Y G L A N D S
Benign affections are the most common pathology of mammary glands.
These diseases are usually considered as pre-tumorous conditions, on which backgrounds breast cancer may develop. However with this pathological state no thorough statistical observation is carried out as it is done with cancer. The number of publication on this topic is significantly fewer than of those devoted to oncological diseases of the mammary gland.
Nevertheless the problem exists and occupies a significant part of work of mammology departments, centers and oncology dispensaries. According to data of
V.E. Savello et al. (2000), the number of women with pathological processes of benign character needing to be observed and treated 25–30 times exceeds the number of women with breast cancer.
There are various surgical approaches to benign masses in mammary glands.
1. Sectoral resection (SR) – removal of the tumour with the surrounding tissues
(part of the skin and subjacent tissue up to the fascia of pectoral muscle, stepping from 1 to 2–3 cm back from the tumour). Cosmetic defect after this kind of surgery is rather considerable. Surgical scar deforms the gland and can be seen during all life of the patient.
2. Resection from projection approach (RPA) – skin incision is situated in the area of projection of the tumour on the skin of the mammary gland and is oriented in radial direction or concentrically, parallel to areola.
3. We have suggested the resection from extra-projection approach (REPA) within which skin incision is made aside from the tumour projection on the skin of the mammary gland, in the area where it would be less noticeable: para-areolarly or submammary (The method of surgical treatment of benign masses of the mammary
53 gland: Pat. 2381752. Rus. Federation МКИ 3 А 61 В 17/00 / Kuklin I.A.; applicant and patent holder State Establishment Scientific Center of Reconstructive and
Restorative Surgery ESSC SB RAMS. – N 2008112644/14 (013674); appl.
01.04.08; publ. 20.02.10, Bul. N 5. – 1 p.).
Suggested method of extra-projection approach to benign masses of mammary glands
The approach is planned in such a way that skin incision is situated lower tumour projection – this is necessary for postoperative outflow of wound discharge and reducing the possibility of infiltrate formation. If the process is localized in upper quadrants then para-areolar incision is performed, in lower quadrants – submammary.
Prior the surgery the marking is made (Fig. 1). First is done in the standing position of the patient. Then it is specified on the lying patient, when the position is horizontal like on surgical table. In some cases, especially with large breasts and localization of the tumour in exterior quadrants of the gland the surgery is more convenient to perform with the position lying on one side or with the cushion put under the back from one side. The marking is made of the tumour projection on the skin, of the future incision coinciding with the fold or the edge of areola.
Before the anesthesia the tumour is fixed through the skin by an injection needle. This is made to prevent the introduced solution to press the tumour back into the tissues and in order there is a clear indicator of tumour localization in infiltrated tissues (Fig. 2).
54
Fig. 1. Marking of extra-projection approach along submammary fold.
Fig. 2.
Fixation of the tumour by an injection needle.
55
Anesthesia is performed with 2% solution of lidocaine with addition of adrenaline 0.01% with 1 ml per 1 l of the solution. First the place of incision is anaesthetized with formation of “lemon skin”. Then hypoderm is infiltrated towards the tumour and entering behind it for 1.5–2 cm. It is more rational to make in from the points situated on the ends of the future incision. Further through the puncture behind the tumour from the opposite side of the incision deeper tissues around the tumour are anaesthetized.
The incision is performed through skin and hypoderm till the a nterior leaf of superficial fascia (Fig. 3).
Fig. 3.
View of anterior leaf/folium of superficial fascia.
In this layer subcutaneous canal is formed which reaches the tumour and goes further beyond it. Then mosquito forceps are introduced into the canal, and the anterior leaf of superficial fascia above the tumour is bluntly drawn back. If fibroadeboma is large (more then 1.5 cm), it is extirpated with
“mosquito”, the surgeon’s finger draws the tumour aside, and forceps’ branches are expand in the space between the tumour and surrounding tissues. With the small size of the tumour (less than 1.5 cm) it is delivered with the help of towel clip and carefully removed (Fig. 4).
56
Fig. 4. The tumour is delivered with the towel clip.
After hemostasis is performed subcutaneous canal is drained by the strip of glove rubber.
Two layers of sutures are placed on skin: with resorbable material (Vicryl) on the lower skin layers and upper subcuticular suture with monofilamentous material
(Prolene, Etilone) (Fig. 5).
When placing the dressing it’s important to place a cushion of pelot type on the skin in the projection of subcutaneous canal. Circular compressive bandage is placed on the chest (Fig. 6).
57
Fig. 5. Subcuticular suture.
Fig. 6. Placing of the pelot in projection of subcutaneous canal.
58
The clinical example 1. Removal of the tumour of the right mammary gland from extra-projection approach.
Patient Zh., 26 y.o. Admitted with complaints about the mass in the right mammary gland, which she discovered herself 3 month ago.
The examination revealed the following. The mammary glands are of normal shape. There’s no discharge from mamillae. Periphery lymphatic nodes are not enlarged. The left mammary gland has no peculiarities. In the right gland in superior-exterior quadrant rounded movable mass is detected, up to 1 cm in diameter, of solid consistence, not painful.
Ultrasound breast examination conclusion: in superior-exterior quadrant of the right mammary gland a fibroadenoma is detected with the size 1,1 × 1,0 × 0,8 cm.
After thin-needle aspiration biopsy epithelial ductal hyperplasia is revealed.
The diagnosis is made: fibroadenoma of the right mammary gland.
The patient underwent a surgery – oncotomy of the tumour of the right mammary gland from extra-projection approach.
Taking into consideration the localization of the tumour the para-areolar approach was chosen. Preoperative marking was done. With intravenous anesthesia after fixation of the tumour to surrounding tissues of the mammary gland with the injection needle local anesthesia was additionally performed. Then above the anterior leaf of superficial fascia subcutaneous canal was formed. The tumour was delived with the towel clip and removed. After hemostasis was performed subcutaneous canal was drained with the strip of glove rubber.
Postoperative period had no peculiarities. Morphological findings No. 5786-
88/06 tumour of the right mammary gland 0.8 × 1.3 cm has a structure of intracanalicular fibroadenoma.
Patient was examined in 1 and 3 months after the surgery. Mammary glands had no peculiarities. Tumour masses were not detected. Postoperative scar is situated along the edge of the areola, of good quality, is merely seen (Fig. 7).
59
Fig. 7. Patient Zh., 26 y.o. The scar 3 months after the surgery.
The patient is satisfied with the achieved result.
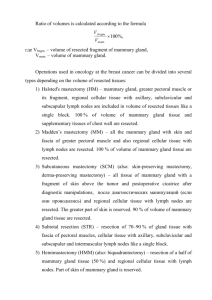
We assessed the method we has suggested with traditional approaches to the benign masses of mammary glands (sectoral resection, projection approach) according to duration of surgery, postoperative complications, and also according to aesthetical acceptability of postoperative results.
Our survey included 124 patients with the most common benign masses of mammary glands.
60
Table 1
Comparative characteristics of patients with benign masses of mammary glands depending on the surgical approach to the mass
Number of patients
Age
Characteristics
( M ± m , years) n
SR
%
37
57,3 ± 1,
2
P
SR –RPA
<
0,001
RPA n %
42
46,6 ± 1,
1
P
RPA –REPA
<
0,001
38,6
P
SR n
45
7
REPA
± 1,
–REPA
%
< 0,001
Tumour localization
Left mammary gland 23 62,2 29 69,1 32 71,1
Right mammary gland
Duration of surgery
(M ± m , min)
14 37,8 13 30,9 13
35,9
6
± 1, 35,8 ± 1,
2
41,9 ± 1,
1
P
SR –RPA
= 0,86
P
RPA –REPA
<
0,001
P
SR –REPA
28,9
< 0,002
Postoperative complications
Infiltrates
Suture line disruption
Suppuration
1
1
2,7
2,7
3
1
7,1
2,4
6
0
13,3
0
1 2,7 1 2,4
P
SR –RPA
= 0,66
χ 2 = 1,58
P
SR –REPA
= 0,19
χ 2 = 4,81
0 0
P
RPA –REPA
= 0,66
χ 2 = 1,60
Table 2
Expert evaluation of aesthetic results after various approaches for surgical treatment of benign masses of mammary glands
Type of approach
SR
RPA
REPA
Evaluation
Me [25% –75%]
2 [2 –3]
3 [2 –4]
5 [4 –5]
Groups of comparison
Mann – Whitney test
Z p
SR – RPA 4,988 <0,001
RPA - REPA 11,824 <0,001
With the help of method of expert evaluation it was defined that the best aesthetic result is achieved after application of extra-projection approach – median
61
= 5 [4–5] grades. More discreet estimation was given to the aesthetic results after sectoral resection (SR) and resection from projection approach (RPA) – 2 [2–3] и 3
[2–4] grades correspondingly. Established difference between SR and RPA, SR and
REPA, RPA and REPA is statistically significant in all cases, р < 0,001.
Thus, the suggested extra-projection approach (REPA) despite of greater labour-intensity and duration of the surgery does not increase the number of postoperative complications, but at the same time significantly improves aesthetic results of the surgical treatment. All this gives us the grounds to recommend to use the resection from extra-projection approach (REPA) in most cases of surgical treatment of benign masses of mammary glands.
Fig. 8. Scar after sectoral resection 3.5 months after the surgery.
62
Fig. 9. Scar after sectoral resection 5 months after the surgery.
63
Fig. 10. Scar after resection from projection approach 6 months after the surgery.
Fig. 11. Scar after resection from projection approach 3 months after the surgery.
64
Fig. 12. Scar after resection from extra-projection approach 6 months after the surgery.