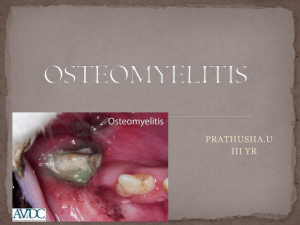
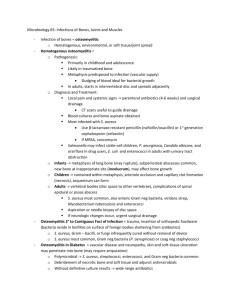
Osteomyelitis Dr.Adnan Al Bursh Consultant orthopedic surgery Head of orthopedic department Shifa medical complex Gaza-palestine • Infection of bone characterized by progressive inflammatory destruction and apposition of new bone. • Essential to diagnose specific organism with biopsy and cultures. • Treatment is often a combination of culture-directed antibiotics and surgical debridement of nonviable tissue. • Epidemiology • incidence – the exact incidence is unknown • location – spine and ribs in dialysis patients – medial or lateral clavicle in IV drug abusers – foot and decubitus ulcers in diabetics • risk factors – – – – – – recent trauma or surgery immunocompromised patients illicit IV drug use poor vascular supply systemic conditions such as diabetes and sickle cell peripheral neuropathy • Pathophysiology • mechanism of spread – hematogenous • originated or transported by blood – may be due to bacterial or viral systemic illness • most common etiology in children • vertebrae are the most common hematogenous site in adults • S. aureus is the most common organism – contiguous-spread • associated with previous surgery, trauma, wounds, or poor vascularity • can be bacterial (most common), mycobacterial, or fungal in nature – direct-inoculation • penetrating injuries • open fractures • surgical contamination. Osteomyelitis Organism Table Age group Most common organisms Newborns (younger than 4 mo) S. aureus, Enterobacter species, and group A and B Streptococcus species Children (aged 4 mo to 4 y) S. aureus, group A Streptococcus species, Kingella kingae, and Enterobacter species Children, adolescents (aged 4 y to adult) S. aureus (80%), group A Streptococcus species, H. influenzae, and Enterobacter species Adult S. aureus and occasionally Enterobacter or Streptococcus species Associated conditions • orthopaedic manifestations – septic arthritis – abscess • medical conditions – – – – – – immunosuppression dialysis IV drug use diabetes poor nutrition vascular disease • Prognosis despite surgical debridement and long-term antibiotics, recurrence rate of chronic osteomyelitis in adults is 30% • poor prognosis in patients with major nutritional or systemic disorders Unusual Osteomyelitis Organism Table Organism Patient characteristic Salmonella Sickle cell anemia patients (S. aureus is still most common) Pseudomonas IV drug use with AC or SC joint infection or puncture wound through rubber soled shoes Bartonella HIV/AIDS patient following cat scratch or bite Fungal osteomyelitis Immunosuppressed, long-term IV medications, or parentarel nutrition Tuberculosis Manifestations include Potts disease Classification •Timing classification • acute • within 2 weeks • subacute • within one to several months • chronic • after several months Cierny-Mader Classification of Osteomyelitis Anatomic Location Stage I Medullary Stage 2 Superficial Stage 3 Localized Stage 4 Diffuse Presentation •History • duration • prior treatments • characterize host • immunocompromised •Symptoms • pain • fever • more common in acute osteomyelitis •Physical exam • vital signs • fever, tachycardia, and hypotension suggest sepsis • inspection • erythema, tenderness, and edema are commonly seen • draining sinus tract • more common in chronic osteomyelitis • if able to probe bone through sinus, chronic osteomyelitis is present • motion • limp and/or pain inhibition with weight-bearing or motion may be present • assess the joints above and below the area of concern • neurovascular • assessment of vascular insufficiency locally or systemically Imaging. • Radiographs – recommended views • orthogonal plain radiographs of the affected extremity – findings • acute – imaging findings lag behind by 2 weeks • chronic – bone lucency, sclerotic rim, osteopenia, periosteal reaction, and lysis around hardware – sequestrum: devitalized bone that serves as a nidus for infection – involucrum: formation of new bone around an area of bony necrosis – sensitivity and specificity is variable sequestrum • CT – indications • assist in diagnosis and surgical planning by identifying necrotic bone – sensitivity and specificity may be affected by hardware artifact. • MRI • indications – assists in the diagnosis and surgical planning – best test for diagnosing early osteomyelitis and localizing infection • views – T2 sequences will show bone and soft tissue edema • findings – penumbra sign • dark central abscess with bright internal wall and dark external sclerotic rim • sensitivity and specificity – if negative rules out osteomyelitis – if positive may overestimate the extent of osteomyelitis penumbra sign • Nuclear medicine. • gallium scan • Laboratory analysis • leukocyte count (WBC) – only elevated in 1/3 of acute osteomyelitis • erythrocyte sedimentation rate (ESR) – usually elevated in both acute and chronic osteomyelitis (90%) • a decrease in ESR after treatment is a favorable prognostic indicator • C-reactive protein – most sensitive test with elevation in 97% of cases • decreases faster than ESR in successfully treated patients • blood cultures – often negative, but may be used to guide therapy for hematogenous osteomyelitis • Microbiology – sinus tract cultures • not reliable for guiding antibiotic therapy – culture of bone • gold-standard for guiding antibiotic therapy • Histology – acute osteomyelitis • live osteocytes with numerous acute inflammatory cells (neutrophils) – chronic osteomyelitis • no nuclei in osteocytes with fibrosis of marrow and chronic inflammatory cells (lymphocytes) Differential •Key differential • benign tumor • biopsy all infection, cultures all tumors • malignant tumor • biopsy all infection, cultures all tumors • healing fracture treatment • Goals • success in the treatment is dependent on various factors – patient factors • immunocompetence of patient • nutritional status – injury factors • the severity of the injury infection location. • metaphyseal infections heal better than mid-diaphyseal infections . – other factors affecting prognosis and treatment include: • residual foreign materials and/or ischemic and necrotic tissues • inappropriate antibiotic coverage • lack of patient cooperation or desire Nonoperative Treatment • suppressive antibiotics – indications • when operative intervention is not feasible • hyperbaric oxygen therapy – indications • can be used as adjunct in refractory osteomyelitis Operative treatment • irrigation and debridement followed by organism specific antibiotics – indications • • • • acute osteomyelitis that fails to improve on IV antibiotics subacute osteomyelitis abscess formation chronic osteomyelitis – draining sinus • amputation – indications • chronic infection with pervasive wound or bone damage that is unable to be salvaged complication • • • • Persistence or extension of infection Amputation Sepsis Malignant transformation – incidence • 1% in chronic osteomyelitis • most commonly squamous cell carcinoma (Marjolin's ulcer) – risk factors • chronic draining sinus – treatment • wide surgical resection Marjolin's ulcer Septic Joint Septic Arthritis Septic Joint/Septic Arthritis • Inflammation of a synovial membrane with purulent effusion into the joint capsule. Followed by articular cartilage erosion by bacterial and cellular enzymes. • Usually monoarticular • Usually bacterial – Staph aureus – Streptococcus – Neisseria gonorrhoeae Septic Joint- Etiology • Direct invasion through penetrating wound, intra-articular injection, arthroscopy • Direct spread from adjacent bone abcess • Blood spread from distant site Septic Joint- Location • Knee- 40-50% • Hip- 20-25%* – *Hip is the most common in infants and very young children • Wrist- 10% • Shoulder, ankle, elbow- 10-15% Septic Joint- Risk Factors • • • • • • • • Prosthetic joint Joint surgery Rheumatoid arthritis Elderly Diabetes Mellitus IV drug use Immunosupression AIDS Septic Joint- Signs and Symptoms • • • • • • • • Rapid onset Joint pain Joint swelling Joint warmth Joint erythema Decreased range of motion Pain with active and passive ROM Fever, raised WCC/CRP, positive blood cultures Septic Joint- Treatment • Diagnosis by aspiration – Gram stain, microscopy, culture – Leucocytes >50 000/ml highly suggestive of sepsis • Joint washout in theatre • IV Abx 4-7 days then orally for another 3 weeks • Analgesia • Splintage Septic Joint- Complications • • • • • • • Rapid destruction of joint with delayed treatment (>24 hours) Growth retardation, deformity of joint (children) Degenerative joint disease Osteomyelitis Joint fibrosis and ankylosing Sepsis Death