Acquisition of clinical specimens. Colorectal cancer(CRC) were
advertisement
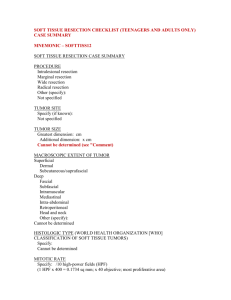
Acquisition of clinical specimens. Colorectal cancer(CRC) were obtained from archived tissue samples derived from patients with CRC who underwent surgical treatment at The First Affiliated Hospital of Zhengzhou University, China from January, 2003 through December, 2012. CRC was diagnosed according to the 2007 WHO Classification of Tumors of the colorectal cancer. All tumors were staged on the basis of the pathologic tumor-node-metastasis classification of the International Union Against Cancer [22]. The selection criteria were as follows: 1) the subject presented with a diagnosis of colorectal cancer and no history of other tumors; 2) the subject had complete demographic and clinical data, such as age, gender, clinical manifestations, tumor size, extent of resection, adjuvant therapy, and date of relapse and/or death; 3) the subject underwent evaluation by enhanced head MRI scanning for tumor relapse or progression after surgery at least once every six months. Written informed consent of the patients was provided by their legal surrogates to permit surgical procedures and use of resected tissues. This study was approved by the Specialty Committee on Ethics of Biomedicine Research, Zhengzhou University of China. Human tissue acquisition and use in this study complied with the National Regulations on the Use of Clinical Samples in China. Collection of clinical information and follow up. Data was collected by review of the clinical history. Information was recorded including the patient’s characteristics (e.g., gender, age), relevant symptoms or history, tumor characteristics (e.g., size, boundary, whether or not associated with a cystic change or evidence of necrosis), extent of resection, post-surgical treatment protocol (e.g., whether the patient took assistant radiotherapy or chemotherapy), overall survival time and progression-free survival time, or miR-145 and RAD18 expression status (e.g., high levels or low expression levels). For analysis, a patient's age was stratified into ≥60 or less than 60 years. The extent of resection was classified as gross total resection, subtotal resection (i.e. greater than 95% of the enhancing tumor was resected), and partial resection. The tumor size was described by mean tumor diameter (MTD, defined as the geometric mean of 3 diameters on MRI scan), and sorted into ≥4 cm and <4 cm. The follow-up was conducted by telephone or direct correspondence. Postsurgical treatment, including adjuvant radiotherapy and chemotherapy, was fully discussed with the patient or their relatives. The time of tumor relapse or death was verified by the patient or their relatives, by medical recording, or by thesocial security record. Overall survival (OS) was calculated in months from the date of diagnosis to the time of death, regardless of cause. Progression free survival (PFS) was defined as the period from the initial date of diagnosis to the time of tumor progression by MRI, or to the time of death of the patient from CRC. Apoptosis assay. Apoptosis was measured using the Apoptosis Detection Kit I (BD Biosciences, Mountain View, CA). As a standard, 1 x 106/ml cells per treatment condition were fixed and stained with 5ul Annexin-V-FITC (BD PharMingen) and 5µl propidium iodide (Sigma). Flow-cytometric analysis was performed for 1 x 104 cells and analyzed by FACScan (Becton Dickinson, NJ) using a single laser emitting excitation light at 488 nm. Data was analyzed by CellQuest software (Becton Dickson, San Jose, CA). Immunocytochemistry and in situ hybridization. Immunohistochemical staining was performed using anti-RAD18 antibody (Santa Cruz Biotechnology, 1:50 dilution). In situ hybridization was performed using a miRNA-145 probe from Exiqon (miRCURY LNA detection probe 5ʹ-DIG (digoxigenin)-labelled). Detection of the probe was carried out using digoxigenin antibody (21H8; 1:200, ab420, Abcam), LSAB2 System-HRP (K0672, Dako) and liquid DAB+ Substrate Chromogen System (K3468, Dako) according to the manufacturer’s instructions.