Neuropathic Pain Conditions
advertisement
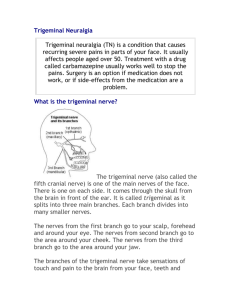
Neuropathic Pain Conditions Neuropathic pain refers to pain is no longer a result of an initial injury or inciting event, but is rather from a lesion or dysfunction of the nervous system. In essence, the nervous system becomes transformed, and the pain signal is generated from this transformation. Such pain is a result of a change in the individual’s physiology, and is not simply a result of a localized physical injury or problem. Neuropathic pain is best treated in a multidisciplinary manner, utilizing a combination of medication, mindfulness, exercise and psychotherapy when needed. As the pain can become chronic and relentless, the multidisciplinary treatment helps to address the multitude of physical, emotional and social problems that may result with such conditions. Complex Regional Pain Syndrome (Reflex Sympathetic Dystrophy) Complex regional pain syndrome (formerly known as reflex sympathetic dystrophy) is a severe pain syndrome with associated autonomic nervous system dysfunction. The autonomic nervous system controls such functions as blood flow, sweat pattern and skin color. The hallmark of complex regional pain syndrome is: There is an initial injury or inciting event that necessitates immobilization Persistent pain that is disproportionate to the initial injury or inciting event Evidence at some time of autonomic dysfunction in the region of the pain, for example, abnormal sweating, a change in hair growth, brittle nails, or a change in skin color or temperature The absence of another medical condition that accounts for the other criteria noted above Because the pain of complex regional pain syndrome is disproportionate to the initial injury, some physicians will incorrectly assume that the pain is psychosomatic, or is a factitious (not real) medical condition. However, there is ample scientific evidence that complex regional pain syndrome is a true neuropathic pain condition, and ultimately results from a change in the manner that pain signals are processed in the brain and spinal cord. Treatment should be multi-disciplinary. Therapeutic injections are sometimes useful early in the course of this condition. The most commonly performed therapeutic injections for this condition are know as sympathetic blocks. In sympathetic blocks, a pain medicine interventionalist places a needle in the region of the sympathetic nerves (along the spine) and injects enough medication to anesthetize these nerves, without affecting the sensory and motor nerves. In a successful sympathetic block, the pain and autonomic nerve dysfunction will abate, and the patient can then be treated with aggressive physical therapy. However, not all patients with complex regional pain syndrome respond to these blocks, which does not necessarily mean that the diagnosis is incorrect. Because pain is sometimes so severe, physical therapy can only be performed following some type of pain relief. Besides the sympathetic blocks, medications are often used, and this may include a combination of anti-convulsant and anti-depressant medication, coupled with analgesics, including opioid medication. For refractory pain, spinal cord stimulator and/or morphine pump placement may be considered. It is important to try to provide pain relief and to begin movement of the affected body region. Prolonged immobilization can lead to more permanent changes in the affected limb, which complicates long-term management. Psychological and social support are extremely important in the overall management of complex regional pain syndrome. Pain can be relentless, and this can lead to a cascade of a breakdown in one’s inner sense of hope and support, as well as within the family, social and work environment. In addition, certain psychological and behavioral techniques teach individuals how to turn inward, and in doing so, how to listen to and regulate the body’s pain response and physiology. Post-Herpetic Neuralgia Post-herpetic neuralgia is pain that develops after shingles. In essence, shingles is a localized reactivation of the chicken pox virus (herpes zoster) along a single nerve root. The virus can remain dormant in part of the nerve root for many years, and can reactivate during times of physical or emotional duress. Following the typical chicken pox eruption, individuals can develop severe pain along the same nerve. Sometimes, the pain precedes the vesicle eruption. Pain can be severe, sharp, burning and lancinating, and sometimes the affected region is hypersensitive even to light touch. Treatment options include localized pain patches, such as a Lidoderm (5% lidocaine) or capsaicin patch. Medications are often necessary, and include anti-depressant or anticonvulsant medications, sometimes with narcotic analgesics as needed. A localized nerve block can also be performed, and repeated as necessary. Fibromyalgia Fibromyalgia is a pain syndrome in which individuals develop several areas of trigger point tenderness. Although some definitions state that there must be 12 such trigger points in typical areas such as the joints, neck and low back, others believe that the diagnosis can be made without mandating a minimum number of specific tender areas. Some individuals present with a more diffuse muscle pain, and with this in mind, fibromyalgia is sometimes considered a more diffuse continuum of myofascial pain. Whereas myofascial pain occurs in one region of the body, fibromyalgia is more diffuse. The cause of fibromyalgia is not certain, although it is likely to represent a type of neuropathic pain, which means that fibromyalgia results from dysfunction of the nervous system. Because it presents as an arthritis-like condition, it is prudent to first rule out an underlying rheumatological or auto-immune condition. There are many other fibromyalgia theories, ranging from thyroid related causes to nutrition to a latent virus to an undefined auto-immune condition. Many individuals present with a spectrum of symptoms besides pain, including insomnia, chronic fatigue, vulnerability to infection and decreased memory and cognition. Treatment should be multi-disciplinary, and should address the individual’s physical, emotional, social and nutritional health. Medications include anti-depressant, anticonvulsant and analgesic medications. Exercise, coupled with mindfulness meditation, is extremely important. Group therapy and cognitive-behavioral strategies are often helpful. With all treatment, it is extremely important to feel validated that this is a real physical condition. However, it is equally important to understand the mind-body continuum in multi-disciplinary treatment. Cancer Pain Individuals who suffer with cancer may have pain secondary to spread of cancer along bones, nerves or internal organs. Sometimes, opioid medications are sufficient for pain management. Other times, opioid medications are coupled with anti-depressant or anticonvulsant medication. Group therapy and cognitive-behavioral strategies may be extremely beneficial in helping individuals to cope. For refractory pain, therapeutic injections or nerve blocks may be attempted. Morphine pump placement is indicated if there is intolerance to oral opioid medications. Trigeminal Neuralgia Trigeminal neuralgia is a type of facial pain that results from activation of the trigeminal nerve, which is the nerve that supplies sensation to the face. Sometimes an entire onehalf of the face is affected, and other times, an area along the jaw, cheek or forehead is affected. Pain is typically electric or lancinating, and lasts for seconds to minutes. Individuals may suffer with multiple attacks per day, sometimes triggered by eating, drinking or talking. Trigeminal neuralgia can result from compression of the trigeminal nerve by a tortuous blood vessel, or from another medical condition such as multiple sclerosis. Most times, there is no identifiable cause. The most effective treatment is usually an anti-convulsant medication, which calms down the repeated firing of the nerve. If medications do not work, then a therapeutic injection into the ganglion of the nerve can be performed. For more refractory pain, other treatments include gamma radiation or nerve decompression by a neurosurgeon.