Obstetric haemorrhage in women who refuse blood transfusion
advertisement
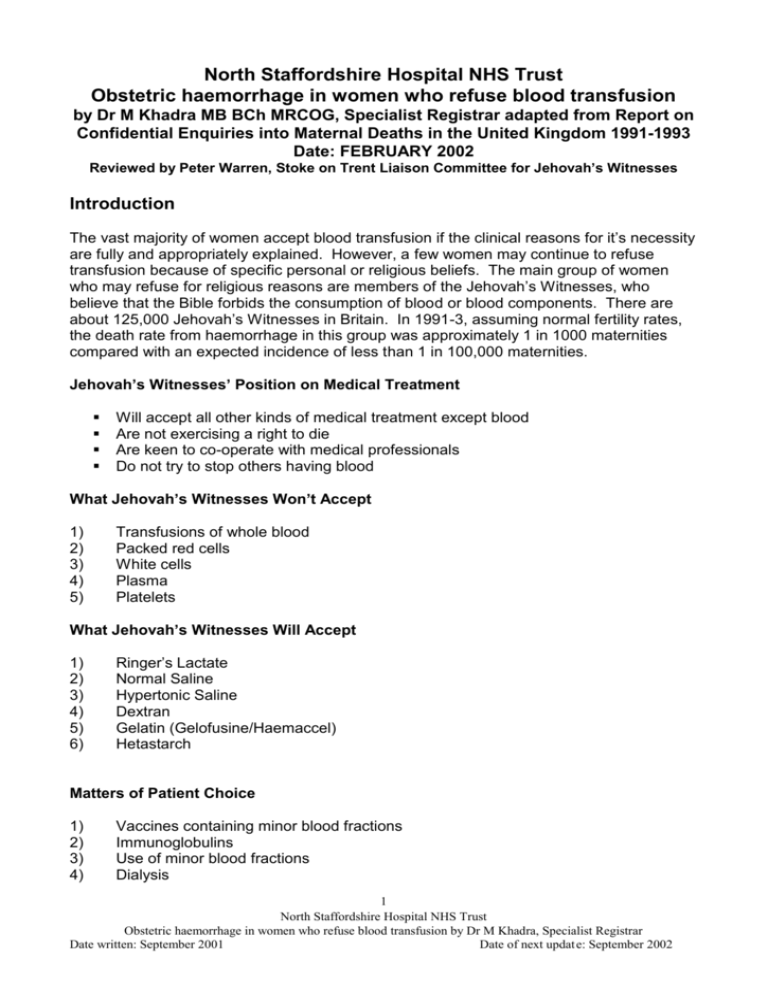
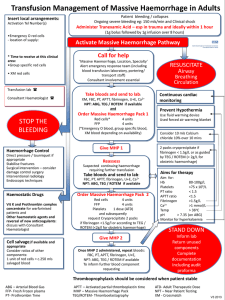
North Staffordshire Hospital NHS Trust Obstetric haemorrhage in women who refuse blood transfusion by Dr M Khadra MB BCh MRCOG, Specialist Registrar adapted from Report on Confidential Enquiries into Maternal Deaths in the United Kingdom 1991-1993 Date: FEBRUARY 2002 Reviewed by Peter Warren, Stoke on Trent Liaison Committee for Jehovah’s Witnesses Introduction The vast majority of women accept blood transfusion if the clinical reasons for it’s necessity are fully and appropriately explained. However, a few women may continue to refuse transfusion because of specific personal or religious beliefs. The main group of women who may refuse for religious reasons are members of the Jehovah’s Witnesses, who believe that the Bible forbids the consumption of blood or blood components. There are about 125,000 Jehovah’s Witnesses in Britain. In 1991-3, assuming normal fertility rates, the death rate from haemorrhage in this group was approximately 1 in 1000 maternities compared with an expected incidence of less than 1 in 100,000 maternities. Jehovah’s Witnesses’ Position on Medical Treatment Will accept all other kinds of medical treatment except blood Are not exercising a right to die Are keen to co-operate with medical professionals Do not try to stop others having blood What Jehovah’s Witnesses Won’t Accept 1) 2) 3) 4) 5) Transfusions of whole blood Packed red cells White cells Plasma Platelets What Jehovah’s Witnesses Will Accept 1) 2) 3) 4) 5) 6) Ringer’s Lactate Normal Saline Hypertonic Saline Dextran Gelatin (Gelofusine/Haemaccel) Hetastarch Matters of Patient Choice 1) 2) 3) 4) Vaccines containing minor blood fractions Immunoglobulins Use of minor blood fractions Dialysis 1 North Staffordshire Hospital NHS Trust Obstetric haemorrhage in women who refuse blood transfusion by Dr M Khadra, Specialist Registrar Date written: September 2001 Date of next updat e: September 2002 5) 6) 7) Intra-operative cell salvage Haemodilution Organ transplant Massive obstetric haemorrhage is often unpredictable and can become life threatening in a short time. In most cases, blood transfusion can save the woman’s life and very few women refuse blood transfusion in these circumstances. If it is thought likely that a woman may do so, the management of massive haemorrhage should be considered in advance. The management of women refusing blood transfusion Consent and Communication Booking/Antenatal period 1) At the booking clinic, all women are normally asked their religious beliefs, and should also be asked if they have any objections to blood transfusion. If a woman is a Jehovah’s Witness or likely to refuse blood transfusion for other reasons, this should be noted in the case notes. She should be asked if she is willing to receive blood transfusion if necessary, and her reply should be noted and consent obtained. 2) If she asks about the risks of refusing blood transfusion, she should be given all relevant information. This must be done in a non-confrontational manner. She would be advised that if massive haemorrhage occurs, there is an increased risk that hysterectomy will be required (see para 23-24), and the woman and her partner should be offered the opportunity to read and discuss the treatment guidelines in this Annexe. 3) If she decides against accepting blood transfusion in any circumstances, she should be booked for delivery in a unit which has all facilities for prompt management of haemorrhage, including hysterectomy as outlined in this Annexe. 4) The woman’s blood group and antibody status should be checked in the usual way and the haemoglobin and serum ferritin should be checked regularly. Haematinics should be given throughout pregnancy to maximise iron stores. 5) An ultrasound scan should be carried out to identify the placental site. 6) Blood storage should not be suggested to pregnant women, as the amounts of blood required to treat massive obstetric haemorrhage are far in excess of the amount that could be donated during pregnancy. 7) If any complications are noted during the antenatal period, the Consultant Obstetrician must be informed. Haemorrhage 2 North Staffordshire Hospital NHS Trust Obstetric haemorrhage in women who refuse blood transfusion by Dr M Khadra, Specialist Registrar Date written: September 2001 Date of next updat e: September 2002 8) The woman should be kept fully informed about what is happening. Information must be given in a professional way, ideally by someone she knows and trusts. If standard treatment is not controlling the bleeding, she should be advised that blood transfusion is strongly recommended. Any patient is entitled to change her mind about a previously agreed treatment plan. 9) The doctor must be satisfied that the woman is not being subjected to pressure from others. It is reasonable to ask the accompanying persons to leave the room for a while so that the doctor (with a midwife or other colleague) can ask her whether she is making her decision of her own free will. 10) If she maintains her refusal to accept blood or blood products, her wishes should be respected. The legal position is that any adult patient (i.e. 18 years old or over) who has the necessary mental capacity to do so is entitled to refuse treatment, even if it is likely that refusal will result in the patient’s death. No other person is legally able to consent to treatment for that adult or to refuse treatment on that person’s behalf. However, unlike adults, the refusal of a competent person aged 16-17 may in certain circumstances be over-ridden by either a person with parental responsibility or a court.(1) 11) The staff must maintain a professional attitude. They must not lose the trust of the patient or her partner as further decisions - for example, about hysterectomy - may have to be made. 12) If, in spite of all care, the woman dies, her relatives require support like any other bereaved family. 13) It is very distressing for staff to have to watch a woman bleed to death while refusing effective treatment. Support should be promptly available for staff in these circumstances. 3 North Staffordshire Hospital NHS Trust Obstetric haemorrhage in women who refuse blood transfusion by Dr M Khadra, Specialist Registrar Date written: September 2001 Date of next updat e: September 2002 General medical management Labour 14) The Consultant Obstetrician should be informed when a woman who will refuse blood transfusion is admitted in labour. Consultants in other specialities need not be alerted unless complications occur. 15) The labour should be managed routinely, by experienced staff. 16) Oxytocics should be given when the baby is delivered. The woman should not be left alone for at least an hour after delivery. 17) If caesarean section is necessary, it should be carried out by a Consultant Obstetrician if possible. 18) The majority of pregnancies will end without serious haemorrhage. When the mother is discharged from hospital, she should be advised to report promptly if she has any concerns about bleeding during the puerperium. Haemorrhage 19) The principle of management of haemorrhage in these cases is to avoid delay. Rapid decision-making may be necessary, particularly with regard to surgical intervention. 20) If unusual bleeding occurs at any time during pregnancy, labour or the puerperium, the Consultant Obstetrician should be informed and the standard management should be commenced promptly. The threshold for intervention should be lower than in other patients. Extra vigilance should be exercised to quantify any abnormal bleeding and to detect complications, such as clotting abnormalities, as promptly as possible. 21) Consultants in other specialties, particularly anaesthetics and haematology, are normally involved in the treatment of massive haemorrhage. When the patient is a woman who has refused blood transfusion, the Consultant Anaesthetist should be informed as soon as possible after abnormal bleeding has been detected. The Consultant Haematologist should also be informed, even though the options for treatment may be severely limited. Intensive care may need to be warned. 22) Dextran should be avoided for fluid replacement because of its possible effects on haemostasis. Intravenous crystalloid and artificial plasma expanders such as Haemaccel should be used. Albumin can be useful and requires consent. 4 North Staffordshire Hospital NHS Trust Obstetric haemorrhage in women who refuse blood transfusion by Dr M Khadra, Specialist Registrar Date written: September 2001 Date of next updat e: September 2002 Surgical Haemorrhage 23) Hysterectomy is normally the last resort in the treatment of obstetric haemorrhage, but with such women delay may increase the risk. The woman’s life may be saved by timely hysterectomy, though even this does not guarantee success. 24) When hysterectomy is performed the uterine arteries should be clamped as early as possible in the procedure. Subtotal hysterectomy can be just as effective as total hysterectomy, as well as being quicker and safer. In some cases there may be a place for internal iliac artery ligation. 25) The timing of hysterectomy is a decision for the consultant on the spot. When making this decision it may be helpful to note that the shortest time from delivery to death recorded in these Reports was in 1985-7, when a woman died within 3 hours of delivery with a haemoglobin concentration of 3.4g/dl. Survival without hysterectomy has been recorded with a haemoglobin concentration of 4.9g/dl (2). APPENDIX CARE PLAN FOR WOMEN IN LABOUR REFUSING A BLOOD TRANSFUSION (as referred to in the RCOG News (October 2000) of the Royal College of Obstetricians and Gynaecologists) Please ensure that the consultant obstetrician is aware a Jehovah’s Witness is being admitted in labour. All such patients should have the third stage of labour actively managed with oxytocic drugs together with early cord clamping and controlled cord traction after placental separation. Do not leave the patient alone for the first hour after delivery. Risk factors predisposing to postpartum haemorrhage If the patient has any of the risk factors below, an IV infusion of Syntocinon should be considered after delivery of the baby Previous history of bleeding, post or antepartum haemorrhage Multiple pregnancy and/or 4 children Large baby (>3.5kg) Prolonged labour (especially when augmented with syntocinon Polyhydramnios Difficult operative delivery Actively haemorrhaging: First steps: Establish IV colloid infusion e.g. Haemaccel or Gelofusine. Give oxygen. Consider CVP line. Catheterise & monitor urine output. Give oxytocic drugs first, then exclude retained products of conception or trauma (this could save time). Proceed with bimanual uterine compression. A useful emergency measure to buy time is aortic compression, using a fist just above the umbilicus directed back against the spine. Slow but persistent blood loss requires action. Anticipate coagulation problems. Involve consultant anaesthetist and haematologist. Keep patient fully informed. Proceed with following strategies if bleeding continues: 5 North Staffordshire Hospital NHS Trust Obstetric haemorrhage in women who refuse blood transfusion by Dr M Khadra, Specialist Registrar Date written: September 2001 Date of next updat e: September 2002 Syntometrine marginally more effective than oxytocin alone. If patient is hypertensive, use oxytocin, 10U IV, not 5U. Oral Misoprostol 600μg (prostalgnadin E1 analogue). Use when unresponsive to oxytocin and ergometrine (3). Intrauterine Misoprostol 800μg (4 tablets, has been successfully used when unresponsive to oxytocin and carboprost (4). Rectal Misoprostol (1000μg) rapid absorption and control of haemorrhage reported, avoids oral problems (5). Does not appear to cause hypertension. Carboprost (Hemabate) 250μg/ml IM, can be repeated after 15min. Direct intramyometrial injection is faster (less hazardous at open operation). If not available, use 1 or 2 Gemeprost pessaries (Beacon Pharmaceuticals) in the uterus (6;6). Aprotinin (Trasylol) 2,000,000 U followed by 500,000 U/hr or tranexamic acid (Cyklokapron) 1gm IV x 3 daily (7);(8);(9). Both agents are fibrinolytic inhibitors used to control serious haemorrhage including PPH, have been used in combination. Recombinant factor VIIa (Novoseven) 90μg/kg, provides site specific thrombin generation. Successfully used to treat 5 reported cases of uncontrollable bleeding associated with DIC, in one case following caesarean section (10). Experience with this drug is limited. Should only be used in lifethreatening bleeding under consultant guidance. Expert advice available from local Haemophilia Comprehensive Care Centre or Novo Nordisk 24-hour medical advice line: 0845 600 5055 (with emergency delivery). Uterine packing (11) or intrauterine balloon catheter (6). Purpose-designed 500 ml J-SOS Bakri balloon available (Cook [UK] Ltd Ted. 01462 473100). Embolisation or ligation of internal iliac artery or bilateral mass ligation of uterine arteries and veins (6). B-Lynch brace suture (12);(13). Simple surgical technique to control massive haemorrhage. Has been used to avoid hysterectomy. Hysterectomy, subtotal hysterectomy can be just as effective, also quicker and safer (8). Consider blood salvage if surgical blood loss anticipated (blood salvage with leucocyte depletion fillers also reported as potential life-saving technique during caesaean section). Post haemorrhage For severe anaemia, give oxygen and use erythropoietin 300 U/kg x 3 per week subcutaneously, without delay (14);(15). Shortens lag period of erythropoiesis and accelerates haemoglobin recovery. Dosage for renal anaemia (50 U/kg), ineffective for severe blood loss anaemia (14). Iron supplementation essential. Oral iron is slow and unreliable, use IV iron sucrose (Venofer) which is not associated with anaphylaxis, 200mg x 3 per week 6 North Staffordshire Hospital NHS Trust Obstetric haemorrhage in women who refuse blood transfusion by Dr M Khadra, Specialist Registrar Date written: September 2001 Date of next updat e: September 2002 (8);(14);(15). Augment with vitamin B-12 and folic acid. Consider elective ventilation on intensive care unit. Hyperbaric oxygen therapy is an option in life-threatening anaemia (8);(16) – contact Hospital Information Services for Jehovah’s Witnesses Tel: 020 8906 2211 (his@wtbts.org.uk) References and sources: 1 Department of Health. Reference Guide to consent for examination or treatment. 2001. London, Department of Health. 2 Reid MF, Nohr K, Birks RJS. Eclampsia and haemorrhage in a Jehovah's Witness. Anaesthesia 1986; 41:324-325. 3 El-Refaey H, O'Brien P, Morafa W, Walder J, Rodeck C. Use of oral misoprostol in the prevention of postpartum haemorrhage. Br J Obstet Gynaecol 1997; 104:336-339. 4 Adekanmi OA, Purmessur S, Edwards G, Barrington JW. Intrauterine misoprostol for the treatment of severe recurrent atonic secondary postpartum haemorrhage. Br J Obstet Gynae 2001; 108:541-542. 5 O'Brien P, El-Refaey H, Gordon A, Geary M, Rodeck CH. Rectally administered misoprostol for the treatment of postpartum hemorrhage unresponsive to oxytocin and ergometrine. A descriptive study. Obstet Gynaecol 1998; 92:212-214. 6 Drife J. Management of primary postpartum haemorrhage. Br J Obstet Gynaecol 1997; 104:275-277. 7 Valentine S, Williamson P, Sutton D. Reduction of acute haemorrhage with aprotinin. Anaesthesia 1993; 48:405-406. 8 Department of Health. The treatment of obstetric haemorrhage in women who refuse blood transfusion. Report on confidential enquiries into maternal deaths in the United Kingdom 1991-1993. London: HMSO, 1996: 44-47. 9 Alok KA, Hagen P, Webb JB. Tranexamic acid in the management of postpartum haemorrhage. Br J Obstet Gynaecol 1996; 103:1250-1251. 10 Moscardo F. Successful treatment of severe intra-abdominal bleeding associated with disseminated intravascular coagulation using recombinant activated factor VII. Br J Haematol 2001; 113:174-176. 11 Maier RC. Control of postpartum hemorrhage with uterine packing. Am J Obstet Gynaecol 1993; 169(2 (1)):317-323. 12 B-Lynch C, Coker A, Lawal AH, Abu J, Cowen MJ. The B_Lynch surgical technique for the control of massive postpartum hemorrhage: an alternative to hysterectomy? Five cases reported. Br J Obstet Gynaecol 1997; 104:372-375. 7 North Staffordshire Hospital NHS Trust Obstetric haemorrhage in women who refuse blood transfusion by Dr M Khadra, Specialist Registrar Date written: September 2001 Date of next updat e: September 2002 13 Ferguson JEI, Bourgeois FJ, Underwood PB. B-Lynch suture for postpartum hemorrhage. Obstet Gynaecol 2000; 95(6(2)):1020-1022. 14 Buscuttil D, Copplestone A. Management of blood loss in Jehovah's Witnesses. BMJ 1995; 311:1115-1116. 15 Breymann C, Richter C, Huttner C, Huch R, Huch A. Effectiveness of recombinant erythropoietin and iron sucrose vs iron therapy only, in patients with postpartum anaemia and blunted erythropoiesis. Europ J Clin Invest 2000; 30:154-161. 16 McLoughlin PL, Cope TM, Harrison JC. Hyperbaric oxygen therapy in the management of severe acute anaemia in a Jehovah's Witness. Anaaesthesia 1999; 54:891-895. 8 North Staffordshire Hospital NHS Trust Obstetric haemorrhage in women who refuse blood transfusion by Dr M Khadra, Specialist Registrar Date written: September 2001 Date of next updat e: September 2002