Elevated serum levels of autoantibodies against high
advertisement

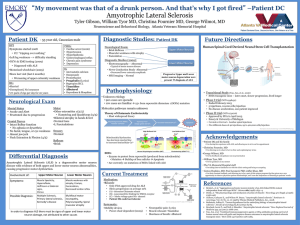
Molecular Biomarkers for Amyotrophic Lateral Sclerosis Chi-Shin Hwang1, Chia-Hung Hsieh2, Guan-Ting Liu2,3, Si-Yi Chen3,4, Johnannes SchengMing Tschen4,5, Hao-Teng Chang2,3,6* 1 Department of Neurology, Taipei City Hospital, Zhongxiao Branch, Taipei, Taiwan, Republic of China; 2Graduate Institute of Basic Medical Science and Ph.D. Program for Aging, and 3Graduate Institute of Molecular Systems Biomedicine, Taichung, Taiwan, Republic of China; 6China Medical University Hospital, Taichung, Taiwan, Republic of China; 4Master Programs of Life Science, College of Life Sciences, National Chung Hsin University, Taichung, Taiwan, Republic of China; 5Biotechnology Department, Ming Dao University, Taichung, Taiwan, Republic of China. *Corresponding author: Dr Hao-Teng Chang, Graduate Institute of Molecular Systems Biomedicine, College of Medicine, China Medical University, No. 91, Hsueh-Shih Road, Taichung, 40402, Taiwan, Republic of China. Tel: +886-4-22052121 ext. 7721; Fax: +886-4-22333641; E-mail: htchang@mail.cmu.edu.tw 1 Abstract Amyotrophic lateral sclerosis (ALS) is a complicated and devastating neurodegenerative disease. To date, its diagnosis is still mainly based on clinical symptoms and electromyographic findings. High rates of misdiagnosis and delayed diagnosis are the major hurdles in ALS treatment. Thus, searching for biomarkers to improve clinical diagnosis of ALS is a highly desirable goal. Here we review current potential biomarkers derived from the various pathogenic mechanisms of ALS, including those involved in oxidative stress, synaptic excitotoxicity, neuroinflammation and the autoimmune response. Oxidative stress results from genetic mutation or an increase in protein aggregation, synaptic excitotoxicity arising from elevated levels of glutamate and D-serine, and the neuroinflammation occurring from elevated levels of inflammatory molecules and cytokine receptors. Some of these biomarkers could be used for monitoring the disease progression and to assess effectiveness of treatment for ALS. We conclude that neuroinflammation plays a crucial role in ALS, which may lead to a better understanding of this devastating disease and ultimately to a cure. In addition, the identification of new biomarkers would undoubtedly provide critical insights into the pathogenesis of ALS. Keywords: amyotrophic lateral sclerosis , biomarker , pathogenesis and autoantibody . 2 1. INTRODUCTION Amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease or motor neuron disease, is the most common adult-onset neuromuscular degenerative disease in humans. Its underlying pathology is characterized by selective loss of motor neurons in the spinal cord, brainstem, and cerebral cortex (1). ALS usually progresses rapidly and leads to total paralysis concomitant with respiratory failure within 2 to 5 years from diagnosis. Although ALS was previously considered to be solely a central nervous system motor disease, it is now recognized as a multi-system neurodegenerative disease with various extra-motor involvements (2-4). The worldwide annual incidence of ALS is 1 to 2 per 100,000 people (5). Approximately 10% of ALS cases are familial ALS (FALS), resulting from genetic inheritance (6); the remaining cases are attributed to sporadic ALS (SALS), where the cause(s) is less understood. Although a cure for ALS does not exist, disease progression can be ameliorated. Survival rates can be improved by early diagnosis followed by early intervention, including medications such as Riluzole (7), multi-disciplinary care (8), the use of noninvasive positivepressure ventilation and percutaneous endoscopic gastrostomy tube feeding (9-11). Traditionally, diagnosis of ALS is made according to neurologist’s comment primarily based on clinical symptoms and electrophysiological findings using techniques that have been available since the turn of the nineteenth century (12, 13). An average misdiagnosis rate of 10% has been reported (14, 15). In addition, the average delay between onset of symptoms and confirmation of diagnosis can be as long as 13 to 18 months (16). Searching for novel biomarkers to improve the timeliness and accuracy of the clinical diagnosis of ALS is therefore a high priority. For discovery of biomarkers in diagnosis or the treatment, omics approaches have been established well, such as genomics, transcriptomics, proteomics, metabolomics and even gene-gene and/or protein-protein interaction. A systems biology approach for identifying the 3 metabolite biomarkers was established by Wang (17). This system was developed for comparing the different levels of serum metabolites after the acupuncture treatments using linear programming based feature selection method. Authors specifically analyzed the high throughput metabolome derived from the sera of subjects with acupuncture in different acupoints. A small set of metabolites can be predicted and selected as acupuncture biomarkers. In addition, the information of transcriptome and protein-protein interaction could be combined for identifying the disease candidate genes (18). The gene expression profiles could show the gene transcriptional levels and the protein-protein interaction information could further explain the real cellular biological behaviors. Through the combination of these two datasets, Liu and colleagues identified 34 early phase candidates for gastric cancer. Since biomarker discovery is much important for diagnosis and disease treatment, here we provide an overview of current researches regarding the biomarkers of ALS. 2. REVIEW OF ALS BIOMARKERS As shown in Table 1, many types of molecules, including amino acids, organic chemicals, genes and proteins, would be discovered as biomarkers for ALS. Some biomarkers have also been correlated with the disease mechanisms, such as glutamate and Dserine inducing the excitotoxicity of post synapsis, the mutants of Cu/Zn superoxide dismutase (SOD1) inducing the neuronal death due to protein aggregation and reactive oxygen species (ROS), transforming growth factorwe generated a subcellular localization of these biomarkers and saw that the cellular biomarkers were distributed in nucleus, cytosol, mitochondria, membrane and extracellular area (Figure 1). Generally, a disease would occur if a protein is located at the wrong site with the wrong amount and/or at the wrong time. Two of the inflammatory related molecules, heat shock proteins (HSPs) and high-mortality group box 1 (HMGB1), would be released into 4 plasma and discovered as ALS biomarkers. These protein biomarkers will be introduced in the following sections. Table 1. Selected studies of potential blood biomarkers for ALS Biomarkers Amino acids Cu/Zn superoxide dismutase (SOD1) Fibronectin Hyaluronic acid Interleukin 6 Plasma transforming growth factor-beta 1 4-Hydroxy-2,3-nonenal Monocyte chemoattractant protein-1α Angiogenin Interleukin 13-positive T cells Insulin-like growth factor (IGF) and insulinlike growth factor-binding protein (IGFBP) Low- to high-density lipoprotein ratio Phosphorylated axonal neurofilament H subunit Heat shock proteins High-mortality group box 1 TAR DNA-binding protein 43 (TDP-43) (RNA-binding protein FUS) FUS Description Increased levels of tyrosine Decreased levels of large neutral amino acids; no change in glutamate Increased levels of glutamate and serine; decreased levels of other amino acids 21q22.1 missense mutations Decreased levels Increased levels Increased levels: 73% sensitive, 91% specific Increased levels Increased levels Increased levels (not vs ND) Increased levels Increased levels (CD4-positive and CD8positive vs HC) Increased levels of total IGF and decreased levels of IGFBP (not vs ND) Increased levels Increased levels References (19) (20) Increased levels Increased inflammatory and neurodegenerative processes (33) Genetic mutations Genetic mutations (35) (35) (21) (22) (23) (24) (25) (26) (27) (27) (28) (29) (30) (31) (32) (34) 5 Figure 1. The subcellular distribution of the ALS biomarkers. The ROS will induce the activation of NF-B and regulate the gene expression. The danger signals, HSPs and HMGB1 can be released into sera of patients of ALS and may induce the neuroinflammation. The SOD1 is a mitochondrial protein whose SOD1-G93A mutant has been developed as an ALS mouse model. The TDP-43 and FUS are nuclear proteins for regulating the gene expression. The membrane RAGE is a receptor for danger signals and the soluble RAGE lower levels of RAGE observed in ALS patients. 2.1. Oxidative Stress and Copper/Zinc-Dependent Superoxide Dismutase 1 (SOD1) Mutations in ALS Mutations in the gene encoding copper/zinc-dependent superoxide dismutase 1 (SOD1) contribute to the disease process in FALS, and this accounts for about 20% of FALS cases (22). These mutations lead to an increase in oxidative stress owing to SOD1 dysfunction. SOD1 is a constitutively expressed homodimer that converts superoxide to hydrogen peroxide and water. More than 100 mutations in human SOD1 have been 6 discovered (36, 37). Most of these mutations do not affect SOD1 activity (38). However three mutants, SOD1-G93A, SOD1-G85R and SOD1-G37R, that have been transduced into mice induce symptoms of motor neurodegeneration (39-41), although the mechanism by which this occurs remains unclear. The common features of the toxic SOD1-G93A and SOD1G37R mutants are protein aggregation and high levels of reactive oxygen species in mitochondria of motor neurons (42). Despite this, there are several reasons why the loss of SOD1 activity may not be relevant to ALS: (a) SOD1 knockout mice do not present symptoms of motor neuron dysfunction (43); (b) levels of SOD1 activity do not correlate with the disease in mice or humans (44); and (c) an increase in SOD1 activity in the ALS mouse model does not accelerate or slow disease onset (45). Therefore, although SOD1 mutations may contribute to ALS, they probably are not the only cause. 2.2. Excitotoxicity from Increased Levels of Synaptic Neurotransmitters It has been known for some time that synapses contain high levels of the neurotransmitter glutamate, which excites N-methyl-D-aspartic acid (NMDA) signaling via post-synaptic NMDA receptors (46). In the ALS mouse model and in humans with ALS, the glutamate level in the brain is higher than normal (47). Riluzole is the only drug approved by the U.S. Food and Drug Administration for slowing ALS disease progression (48, 49), and it is thought to act by preventing stimulation of glutamine receptors, thereby reducing the effect of excess glutamine. Another important molecule that is involved in FALS pathogenesis is the enzyme D-amino acid oxidase (DAO), which regulates the levels of D-serine — a neurotransmitter involved in activating NMDA receptors (50). In 2010, Belleroche et al. discovered a unique missense mutation in the DAO gene that encoded DAOR199W in a family with a strong inheritance of ALS. The same group also demonstrated ubiquitin aggregation and cytotoxicity in a DAOR199W-transfected motor neuron cell line (51). This discovery provided crucial evidence that dysfunction of DAO may result in increased D-serine levels 7 and lead to over-excitation, and ultimately increased excitotoxicity, at the postsynaptic site (52). 2.3. Neuroinflammation Mitchell et al. recently reported an ALS biomarker panel from the cerebrospinal fluid (CSF) of patients with ALS that included molecules that promote inflammation and blood vessel formation (53). They suggested that a number of inflammatory responses occur in the central nervous system of ALS patients, and these biomarkers may reflect the levels of neuroinflammation (53). Oxidative stress (54) and heat shock proteins (33) (HSPs) are also thought to play an important role in the development of ALS. The HSPs belong to a family of stress proteins associated with the general cellular stress response, and they are part of the larger group of damage-associated molecular pattern (DAMP) molecules (55). Levels of cytoprotective HSPs usually increase when motor neurons encounter oxidative stress (56, 57). It was found that chaperoning activity of HSPs decreases in the lumbar spinal cord but increases or remains unchanged in clinically unaffected tissues of SOD1-G93A transgenic mice (58). The high mobility group box 1 (HMGB1) protein, a DAMP molecule, is a non-histone chromosomal protein. HMGB1 is involved in maintaining nucleosome structure, and it regulates transcription through the activation of DNA recombination and repair. It has also been found to be a late mediator of endotoxemia and sepsis (59-61). When inflammation is induced, HMGB1 is released from the activated macrophages and triggers the release of proinflammatory mediators that cause cell death. HMGB1 is overexpressed in the spinal cord of SOD1-G93A transgenic mice (34). In addition, other HMGB1-related molecules, such as Toll-like receptor 2 (TLR-2), TLR-4, and receptor for advanced glycation end product (RAGE), were also found at elevated levels by the studies using immunohistochemical staining (34, 62). Both HSPs and HMGB1 belong to the class of DAMPs released by damaged cells, and they may bind TLRs, thereby activating the inflammatory responses. 8 In addition, unpublished data from our laboratory has revealed that the serum levels of autoantibodies against HSP60, HSP70, and HMGB1 in ALS patients were 1.64-, 1.37-, and 3.00-fold higher, respectively, than those in age-matched control subjects. This discovery suggests that serum autoantibodies against HSP60, HSP70, and HMGB1 may serve as biomarkers for ALS diagnosis. Furthermore, we found that the serum levels of autoantibody against HMGB1 correlated well with the severity of ALS. This means that the serum levels of HMGB1 may be a promising biomarker for monitoring ALS disease progression. In 2003, Ilzecka and Stelmasiak reported that annexin-V autoantibodies could be detected in the CSF and sera of ALS patients but not in that of controls (63). They also found that annexin-V autoantibodies were detected only in ALS patients with bulbar onset and short disease duration. Thus, autoantibodies may be involved in the pathogenesis of ALS and may be related to its progression. Levels of HSPs decrease prior to, and increase after, symptom onset in motor neurons of SOD1-G93A transgenic mice (64). This discovery suggests that disease occurrence may correlate with overexpression of HSPs. ALS is a progressive disease, however, motor neurons are damaged at very early stages of disease (65), HSPs are continuously released into the extracellular space and subsequently enter the bloodstream (66). This may lead to induction, amplification, and release of specific autoantibodies against the HSPs by activated B cells. RAGE, a membrane-bound receptor, belongs to the immunoglobulin-like superfamily, and it binds to ligands such as HMGB1, AGE, amyloid fibrils, and S100 (67). In Alzheimer’s disease, increased levels of membrane-bound RAGE correlate well with disease severity (68, 69). Soluble RAGE (sRAGE) is the serum polypeptide released by cleavage of membrane-bound RAGE, and it neutralizes inflammatory factors such as HMGB1 and AGE to reduce inflammatory symptoms (70). A recent report found that blood levels of sRAGE are lower in ALS patients (71). The decrease of sRAGE in ALS may explain neuronal death 9 caused by DAMP molecules (72, 73). DAMP molecules and their receptors may therefore play an important role in the pathogenic mechanisms of ALS, and neuroinflammation may likewise play an important role in ALS onset or progression. 2.4. Other Candidate Biomarkers for ALS The TAR DNA-binding protein 43 (TDP-43) was found in the neuron inclusion bodies in FALS patients. In 2008, Screedharan et al. reported that a single nucleotide polymorphism in TDP-43, encoding TDP-43M337V, induces aggregation of poly-ubiquitins and causes neuronal damage (74). It has also been reported that the amount of TDP-43 is elevated in the CSF of ALS patients (75). In addition, Miana-Mena et al. reported that transthyretin levels are lower in ALS patients, particularly those with SALS (76). The extent of post-translational modification of transthyretin, however, was higher in patients with ALS compared to that of healthy controls (77). This result indicates that non-genetic factors may also be involved in ALS pathogenesis. 2.5. Bioinformatics Databases for ALS Biomarkers As mentioned in section 2.1 and 2.4, SOD1 and TDP-43 have been discovered as important ALS biomarkers. Till now, more than 100 mutations on SOD1 are identified and most of the TDP-43 mutations are located at the C-terminus except Ala90Val and Asp169Gly mutations. In this section, we will introduce two ALS databases which collect all SNP mutants of these two ALS biomarkers. ALSOD, Amyotrophic Lateral Sclerosis Online Database, is a database collecting all SNPs of ALS biomarkers, including SOD1, ALS2, ALS3, TDP-43 and the other 17 ALS related genes. It also includes patient information aiming for correlating the genotype of biomarkers and the phenotype of patients with ALS (78). Originally, ALSOD collected 97 individual ALS cases and now the database has collected 609 cases. This database is comprehensive for ALS biomarker studies. The other database, PRO-MINE, is an analytic tool for TDP-43 mutations (79). This database collected all SNPs of TDP-43 gene. Since TDP-43 is not only for ALS, but also occurs in Front 10 Temporal Lobar Degeneration and Alzheimer Disease, this database was generated for studying the neurodegenerative diseases. Besides the collection of TDP-43 SNPs, the analytic tool can also predict the biological function of mutant TDP-43. This prediction tool makes biologists to design the wet lab experiments for studying the relationship between mutant TDP-43 and the neurodegenerative diseases. CONCLUSIONS ALS is a complex disease of the central nervous system, and identifying even a single biomarker for the diagnosis or the monitoring of disease progression has proved elusive. Researchers have been vigorously searching for serum biomarkers of ALS for many years, yet no biomarker has been proved to be effective and convenient for clinical use. With the recent progress of biomedical techniques, researchers are vigorously developing new potential biomarkers according to the various pathogenic mechanisms of ALS. With the identification of new biomarkers, the pathogenesis of ALS will be understood more clearly in the near future. Acknowledgments This work was supported by an award from the National Science Council of Taiwan (NSC100-2627-B-039-002 to H.-T. Chang) and an award from the Taiwan Department of Health Clinical Trial and Research Center of Excellence (DOH101-TD-B-111-004). Conflict of interest: The authors declare that they have no conflict of interest. References 1. Mitchell JD, Borasio GD. Amyotrophic lateral sclerosis. Lancet. 2007 Jun 16;369(9578):2031-41. 2. Hayashi H, Kato S. Total manifestations of amyotrophic lateral sclerosis. ALS in the totally locked-in state. J Neurol Sci. 1989 Oct;93(1):19-35. 11 3. Dettmers C, Fatepour D, Faust H, Jerusalem F. Sympathetic skin response abnormalities in amyotrophic lateral sclerosis. Muscle Nerve. 1993 Sep;16(9):930-4. 4. Oey PL, Vos PE, Wieneke GH, Wokke JH, Blankestijn PJ, Karemaker JM. Subtle involvement of the sympathetic nervous system in amyotrophic lateral sclerosis. Muscle Nerve. 2002 Mar;25(3):402-8. 5. Worms PM. The epidemiology of motor neuron diseases: a review of recent studies. J Neurol Sci. 2001 Oct 15;191(1-2):3-9. 6. Kunst CB. Complex genetics of amyotrophic lateral sclerosis. Am J Hum Genet. 2004 Dec;75(6):933-47. 7. Miller RG, Mitchell JD, Lyon M, Moore DH. Riluzole for amyotrophic lateral sclerosis (ALS)/motor neuron disease (MND). Cochrane Database Syst Rev. 2007(1):CD001447. 8. Traynor BJ, Alexander M, Corr B, Frost E, Hardiman O. Effect of a multidisciplinary amyotrophic lateral sclerosis (ALS) clinic on ALS survival: a population based study, 1996-2000. J Neurol Neurosurg Psychiatry. 2003 Sep;74(9):1258-61. 9. Cudkowicz M, Qureshi M, Shefner J. Measures and markers in amyotrophic lateral sclerosis. NeuroRx. 2004 Apr;1(2):273-83. 10. Miller RG, Jackson CE, Kasarskis EJ, England JD, Forshew D, Johnston W, et al. Practice parameter update: The care of the patient with amyotrophic lateral sclerosis: drug, nutritional, and respiratory therapies (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2009 Oct 13;73(15):1218-26. 11. Andersen PM, Borasio GD, Dengler R, Hardiman O, Kollewe K, Leigh PN, et al. EFNS task force on management of amyotrophic lateral sclerosis: guidelines for diagnosing and clinical care of patients and relatives. Eur J Neurol. 2005 Dec;12(12):921-38. 12. Brooks BR, Miller RG, Swash M, Munsat TL. El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord. 2000 Dec;1(5):293-9. 13. Radunovic A, Mitsumoto H, Leigh PN. Clinical care of patients with amyotrophic lateral sclerosis. Lancet Neurol. 2007 Oct;6(10):913-25. 14. Davenport RJ, Swingler RJ, Chancellor AM, Warlow CP. Avoiding false positive diagnoses of motor neuron disease: lessons from the Scottish Motor Neuron Disease Register. J Neurol Neurosurg Psychiatry. 1996 Feb;60(2):147-51. 15. Traynor BJ, Codd MB, Corr B, Forde C, Frost E, Hardiman O. Amyotrophic lateral sclerosis mimic syndromes: a population-based study. Arch Neurol. 2000 Jan;57(1):109-13. 16. Chio A, Cucatto A, Calvo A, Terreni AA, Magnani C, Schiffer D. Amyotrophic lateral sclerosis among the migrant population to Piemonte, northwestern Italy. J Neurol. 1999 Mar;246(3):175-80. 17. Wang Y, Wu QF, Chen C, Wu LY, Yan XZ, Yu SG, et al. Revealing metabolite biomarkers for acupuncture treatment by linear programming based feature selection. BMC Syst Biol. 2012;6(S1):S15. 18. Liu X, Liu ZP, Zhao XM, Chen L. Identifying disease genes and module biomarkers by differential interactions. Journal of the American Medical Informatics Association : JAMIA. [Research Support, Non-U.S. Gov't]. 2012 MarApr;19(2):241-8. 19. Patten BM, Harati Y, Acosta L, Jung SS, Felmus MT. Free amino acid levels in amyotrophic lateral sclerosis. Annals of neurology. 1978 Apr;3(4):305-9. 12 20. Camu W, Billiard M, Baldy-Moulinier M. Fasting plasma and CSF amino acid levels in amyotrophic lateral sclerosis: a subtype analysis. Acta neurologica Scandinavica. [Research Support, Non-U.S. Gov't]. 1993 Jul;88(1):51-5. 21. Ilzecka J, Stelmasiak Z, Solski J, Wawrzycki S, Szpetnar M. Plasma amino acids percentages in amyotrophic lateral sclerosis patients. Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. [Comparative Study]. 2003 Nov;24(4):293-5. 22. Rosen DR, Siddique T, Patterson D, Figlewicz DA, Sapp P, Hentati A, et al. Mutations in Cu/Zn superoxide dismutase gene are associated with familial amyotrophic lateral sclerosis. Nature. [Comparative Study Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. 1993 Mar 4;362(6415):59-62. 23. Ono S, Imai T, Shimizu N, Nakayama M, Mihori A, Kaneda K, et al. Decreased plasma levels of fibronectin in amyotrophic lateral sclerosis. Acta neurologica Scandinavica. 2000 Jun;101(6):391-4. 24. Ono S, Imai T, Tsumura M, Takahashi K, Jinnai K, Suzuki M, et al. Increased serum hyaluronic acid in amyotrophic lateral sclerosis: relation to its skin content. Amyotroph Lateral Scler Other Motor Neuron Disord. 2000 Jun;1(3):2138. 25. Ono S, Hu J, Shimizu N, Imai T, Nakagawa H. Increased interleukin-6 of skin and serum in amyotrophic lateral sclerosis. J Neurol Sci. 2001 Jun 15;187(1-2):2734. 26. Houi K, Kobayashi T, Kato S, Mochio S, Inoue K. Increased plasma TGFbeta1 in patients with amyotrophic lateral sclerosis. Acta neurologica Scandinavica. 2002 Nov;106(5):299-301. 27. Simpson EP, Henry YK, Henkel JS, Smith RG, Appel SH. Increased lipid peroxidation in sera of ALS patients: a potential biomarker of disease burden. Neurology. [Evaluation Studies Research Support, Non-U.S. Gov't]. 2004 May 25;62(10):1758-65. 28. Cronin S, Greenway MJ, Ennis S, Kieran D, Green A, Prehn JH, et al. Elevated serum angiogenin levels in ALS. Neurology. [Research Support, Non-U.S. Gov't]. 2006 Nov 28;67(10):1833-6. 29. Shi N, Kawano Y, Tateishi T, Kikuchi H, Osoegawa M, Ohyagi Y, et al. Increased IL-13-producing T cells in ALS: positive correlations with disease severity and progression rate. Journal of neuroimmunology. [Research Support, Non-U.S. Gov't]. 2007 Jan;182(1-2):232-5. 30. Hosback S, Hardiman O, Nolan CM, Doyle MA, Gorman G, Lynch C, et al. Circulating insulin-like growth factors and related binding proteins are selectively altered in amyotrophic lateral sclerosis and multiple sclerosis. Growth hormone & IGF research : official journal of the Growth Hormone Research Society and the International IGF Research Society. [Comparative Study]. 2007 Dec;17(6):472-9. 31. Dupuis L, Corcia P, Fergani A, Gonzalez De Aguilar JL, Bonnefont-Rousselot D, Bittar R, et al. Dyslipidemia is a protective factor in amyotrophic lateral sclerosis. Neurology. [Research Support, Non-U.S. Gov't]. 2008 Mar 25;70(13):1004-9. 32. Boylan K, Yang C, Crook J, Overstreet K, Heckman M, Wang Y, et al. Immunoreactivity of the phosphorylated axonal neurofilament H subunit (pNF-H) in blood of ALS model rodents and ALS patients: evaluation of blood pNF-H as a 13 potential ALS biomarker. Journal of neurochemistry. [Research Support, Non-U.S. Gov't]. 2009 Dec;111(5):1182-91. 33. Brown IR. Heat shock proteins and protection of the nervous system. Annals of the New York Academy of Sciences. [Research Support, Non-U.S. Gov't Review]. 2007 Oct;1113:147-58. 34. Lo Coco D, Veglianese P, Allievi E, Bendotti C. Distribution and cellular localization of high mobility group box protein 1 (HMGB1) in the spinal cord of a transgenic mouse model of ALS. Neuroscience letters. [Comparative Study Research Support, Non-U.S. Gov't]. 2007 Jan 22;412(1):73-7. 35. Mackenzie IR, Rademakers R, Neumann M. TDP-43 and FUS in amyotrophic lateral sclerosis and frontotemporal dementia. Lancet Neurol. [Comparative Study Research Support, Non-U.S. Gov't Review]. 2010 Oct;9(10):995-1007. 36. Mandler RN, Anderson FA, Jr., Miller RG, Clawson L, Cudkowicz M, Del Bene M. The ALS Patient Care Database: insights into end-of-life care in ALS. Amyotroph Lateral Scler Other Motor Neuron Disord. [Comparative Study Research Support, Non-U.S. Gov't]. 2001 Dec;2(4):203-8. 37. Bromberg MB, Anderson F, Davidson M, Miller RG. Assessing health status quality of life in ALS: comparison of the SIP/ALS-19 with the ALS Functional Rating Scale and the Short Form-12 Health Survey. ALS C.A.R.E. Study Group. Clinical Assessement, Research, and Education. Amyotroph Lateral Scler Other Motor Neuron Disord. [Research Support, Non-U.S. Gov't]. 2001 Mar;2(1):31-7. 38. Bowling AC, Barkowski EE, McKenna-Yasek D, Sapp P, Horvitz HR, Beal MF, et al. Superoxide dismutase concentration and activity in familial amyotrophic lateral sclerosis. Journal of neurochemistry. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. 1995 May;64(5):2366-9. 39. Babb TL, Mathern GW, Leite JP, Pretorius JK, Yeoman KM, Kuhlman PA. Glutamate AMPA receptors in the fascia dentata of human and kainate rat hippocampal epilepsy. Epilepsy research. [Research Support, U.S. Gov't, P.H.S.]. 1996 Dec;26(1):193-205. 40. Gurney ME. Transgenic-mouse model of amyotrophic lateral sclerosis. The New England journal of medicine. [Comment Letter]. 1994 Dec 22;331(25):1721-2. 41. Ripps ME, Huntley GW, Hof PR, Morrison JH, Gordon JW. Transgenic mice expressing an altered murine superoxide dismutase gene provide an animal model of amyotrophic lateral sclerosis. Proceedings of the National Academy of Sciences of the United States of America. [Research Support, U.S. Gov't, P.H.S.]. 1995 Jan 31;92(3):689-93. 42. Dal Canto MC, Gurney ME. Neuropathological changes in two lines of mice carrying a transgene for mutant human Cu,Zn SOD, and in mice overexpressing wild type human SOD: a model of familial amyotrophic lateral sclerosis (FALS). Brain research. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. 1995 Apr 3;676(1):25-40. 43. Reaume AG, Elliott JL, Hoffman EK, Kowall NW, Ferrante RJ, Siwek DF, et al. Motor neurons in Cu/Zn superoxide dismutase-deficient mice develop normally 14 but exhibit enhanced cell death after axonal injury. Nature genetics. [Comparative Study Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S. Research Support, U.S. Gov't, P.H.S.]. 1996 May;13(1):43-7. 44. Borchelt DR, Lee MK, Slunt HS, Guarnieri M, Xu ZS, Wong PC, et al. Superoxide dismutase 1 with mutations linked to familial amyotrophic lateral sclerosis possesses significant activity. Proceedings of the National Academy of Sciences of the United States of America. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. 1994 Aug 16;91(17):8292-6. 45. Bruijn LI, Houseweart MK, Kato S, Anderson KL, Anderson SD, Ohama E, et al. Aggregation and motor neuron toxicity of an ALS-linked SOD1 mutant independent from wild-type SOD1. Science. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. 1998 Sep 18;281(5384):1851-4. 46. Burger PM, Mehl E, Cameron PL, Maycox PR, Baumert M, Lottspeich F, et al. Synaptic vesicles immunoisolated from rat cerebral cortex contain high levels of glutamate. Neuron. [Research Support, Non-U.S. Gov't]. 1989 Dec;3(6):715-20. 47. Spreux-Varoquaux O, Bensimon G, Lacomblez L, Salachas F, Pradat PF, Le Forestier N, et al. Glutamate levels in cerebrospinal fluid in amyotrophic lateral sclerosis: a reappraisal using a new HPLC method with coulometric detection in a large cohort of patients. J Neurol Sci. 2002 Jan 15;193(2):73-8. 48. Lacomblez L, Bensimon G, Leigh PN, Guillet P, Meininger V. Dose-ranging study of riluzole in amyotrophic lateral sclerosis. Amyotrophic Lateral Sclerosis/Riluzole Study Group II. Lancet. [Clinical Trial Comparative Study Multicenter Study Randomized Controlled Trial]. 1996 May 25;347(9013):1425-31. 49. Waibel S, Reuter A, Malessa S, Blaugrund E, Ludolph AC. Rasagiline alone and in combination with riluzole prolongs survival in an ALS mouse model. J Neurol. [Comparative Study Research Support, Non-U.S. Gov't]. 2004 Sep;251(9):1080-4. 50. Pollegioni L, Piubelli L, Sacchi S, Pilone MS, Molla G. Physiological functions of D-amino acid oxidases: from yeast to humans. Cellular and molecular life sciences : CMLS. [Research Support, Non-U.S. Gov't Review]. 2007 Jun;64(11):1373-94. 51. Mitchell J, Paul P, Chen HJ, Morris A, Payling M, Falchi M, et al. Familial amyotrophic lateral sclerosis is associated with a mutation in D-amino acid oxidase. Proceedings of the National Academy of Sciences of the United States of America. 2010 Apr 20;107(16):7556-61. 52. Wake K, Yamazaki H, Hanzawa S, Konno R, Sakio H, Niwa A, et al. Exaggerated responses to chronic nociceptive stimuli and enhancement of Nmethyl-D-aspartate receptor-mediated synaptic transmission in mutant mice lacking D-amino-acid oxidase. Neuroscience letters. 2001 Jan 5;297(1):25-8. 15 53. Mitchell RM, Freeman WM, Randazzo WT, Stephens HE, Beard JL, Simmons Z, et al. A CSF biomarker panel for identification of patients with amyotrophic lateral sclerosis. Neurology. [Research Support, Non-U.S. Gov't]. 2009 Jan 6;72(1):14-9. 54. Miana-Mena FJ, Gonzalez-Mingot C, Larrode P, Munoz MJ, Olivan S, FuentesBroto L, et al. Monitoring systemic oxidative stress in an animal model of amyotrophic lateral sclerosis. J Neurol. 2010 Nov 25. 55. De Maio A. Extracellular heat shock proteins, cellular export vesicles, and the Stress Observation System: A form of communication during injury, infection, and cell damage : It is never known how far a controversial finding will go! Dedicated to Ferruccio Ritossa. Cell Stress Chaperones. 2010 Oct 21. 56. Mailhos C, Howard MK, Latchman DS. Heat shock protects neuronal cells from programmed cell death by apoptosis. Neuroscience. 1993 Aug;55(3):621-7. 57. Kalmar B, Burnstock G, Vrbova G, Urbanics R, Csermely P, Greensmith L. Upregulation of heat shock proteins rescues motoneurones from axotomyinduced cell death in neonatal rats. Exp Neurol. 2002 Jul;176(1):87-97. 58. Bruening W, Roy J, Giasson B, Figlewicz DA, Mushynski WE, Durham HD. Up-regulation of protein chaperones preserves viability of cells expressing toxic Cu/Zn-superoxide dismutase mutants associated with amyotrophic lateral sclerosis. Journal of neurochemistry. 1999 Feb;72(2):693-9. 59. Thomas JO, Travers AA. HMG1 and 2, and related 'architectural' DNAbinding proteins. Trends Biochem Sci. 2001 Mar;26(3):167-74. 60. Brezniceanu ML, Volp K, Bosser S, Solbach C, Lichter P, Joos S, et al. HMGB1 inhibits cell death in yeast and mammalian cells and is abundantly expressed in human breast carcinoma. FASEB J. 2003 Jul;17(10):1295-7. 61. Yuan F, Gu L, Guo S, Wang C, Li GM. Evidence for involvement of HMGB1 protein in human DNA mismatch repair. J Biol Chem. 2004 May 14;279(20):20935-40. 62. Casula M, Iyer AM, Spliet WG, Anink JJ, Steentjes K, Sta M, et al. Toll-like receptor signaling in amyotrophic lateral sclerosis spinal cord tissue. Neuroscience. 2011 Apr 14;179:233-43. 63. Ilzecka J, Stelmasiak Z. Anti-annexin V antibodies in the cerebrospinal fluid and serum of patients with amyotrophic lateral sclerosis. Neurological sciences : official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. 2003 Nov;24(4):273-4. 64. Maatkamp A, Vlug A, Haasdijk E, Troost D, French PJ, Jaarsma D. Decrease of Hsp25 protein expression precedes degeneration of motoneurons in ALS-SOD1 mice. Eur J Neurosci. 2004 Jul;20(1):14-28. 65. Perry JJ, Shin DS, Tainer JA. Amyotrophic lateral sclerosis. Adv Exp Med Biol. 2010;685:9-20. 66. Taylor DM, Tradewell ML, Minotti S, Durham HD. Characterizing the role of Hsp90 in production of heat shock proteins in motor neurons reveals a suppressive effect of wild-type Hsf1. Cell Stress Chaperones. 2007 Summer;12(2):151-62. 67. Bucciarelli LG, Wendt T, Rong L, Lalla E, Hofmann MA, Goova MT, et al. RAGE is a multiligand receptor of the immunoglobulin superfamily: implications for homeostasis and chronic disease. Cellular and molecular life sciences : CMLS. 2002 Jul;59(7):1117-28. 68. Wang MY, Ross-Cisneros FN, Aggarwal D, Liang CY, Sadun AA. Receptor for advanced glycation end products is upregulated in optic neuropathy of Alzheimer's disease. Acta Neuropathol. 2009 Sep;118(3):381-9. 16 69. Lue LF, Yan SD, Stern DM, Walker DG. Preventing activation of receptor for advanced glycation endproducts in Alzheimer's disease. Curr Drug Targets CNS Neurol Disord. 2005 Jun;4(3):249-66. 70. Zhang H, Tasaka S, Shiraishi Y, Fukunaga K, Yamada W, Seki H, et al. Role of soluble receptor for advanced glycation end products on endotoxin-induced lung injury. Am J Respir Crit Care Med. 2008 Aug 15;178(4):356-62. 71. Ilzecka J. Serum-soluble receptor for advanced glycation end product levels in patients with amyotrophic lateral sclerosis. Acta neurologica Scandinavica. 2009 Aug;120(2):119-22. 72. Babu GN, Kumar A, Chandra R, Puri SK, Kalita J, Misra UK. Elevated inflammatory markers in a group of amyotrophic lateral sclerosis patients from northern India. Neurochem Res. 2008 Jun;33(6):1145-9. 73. Moreau C, Devos D, Brunaud-Danel V, Defebvre L, Perez T, Destee A, et al. Elevated IL-6 and TNF-alpha levels in patients with ALS: inflammation or hypoxia? Neurology. 2005 Dec 27;65(12):1958-60. 74. Sreedharan J, Blair IP, Tripathi VB, Hu X, Vance C, Rogelj B, et al. TDP-43 mutations in familial and sporadic amyotrophic lateral sclerosis. Science. 2008 Mar 21;319(5870):1668-72. 75. Noto Y, Shibuya K, Sato Y, Kanai K, Misawa S, Sawai S, et al. Elevated CSF TDP-43 levels in amyotrophic lateral sclerosis: specificity, sensitivity, and a possible prognostic value. Amyotroph Lateral Scler. 2011 Mar;12(2):140-3. 76. Miana-Mena FJ, Piedrafita E, Gonzalez-Mingot C, Larrode P, Munoz MJ, Martinez-Ballarin E, et al. Levels of membrane fluidity in the spinal cord and the brain in an animal model of amyotrophic lateral sclerosis. Journal of bioenergetics and biomembranes. [Research Support, Non-U.S. Gov't]. 2011 Apr;43(2):181-6. 77. Ryberg H, An J, Darko S, Lustgarten JL, Jaffa M, Gopalakrishnan V, et al. Discovery and verification of amyotrophic lateral sclerosis biomarkers by proteomics. Muscle Nerve. 2010 Jul;42(1):104-11. 78. Wroe R, Wai-Ling Butler A, Andersen PM, Powell JF, Al-Chalabi A. ALSOD: the Amyotrophic Lateral Sclerosis Online Database. Amyotroph Lateral Scler. [Research Support, Non-U.S. Gov't]. 2008 Aug;9(4):249-50. 79. Pinto S, Vlahovicek K, Buratti E. PRO-MINE: A bioinformatics repository and analytical tool for TARDBP mutations. Human mutation. [Research Support, NonU.S. Gov't]. 2011 Jan;32(1):E1948-58. 17