ETIOLOGY OF HEARING LOSS IN CHILDREN - Paediatrie
advertisement

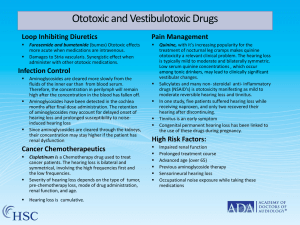
ETIOLOGY OF HEARING LOSS IN CHILDREN Nongenetic Causes HEARING LOSS IN CHILDREN Nancy J. Roizen MD Department of Pediatrics, University of Chicago Pritzker School of Medicine, and Section of Developmental and Behavioral Pediatrics, Chicago, Illinois Address reprint requests to Nancy J. Roizen, MD Department of Pediatrics, MC 900 5841 South Maryland Avenue Chicago, IL 60637 The identification of a specific cause of hearing loss in children facilitates optimal management. When a specific cause of a child's hearing loss is identified, parents are usually relieved. In many of the disorders associated with hearing loss, other organ systems are involved, and frequently hereditary factors are present. [61] In the article by Grundfast on the genetic causes of hearing loss, identification of the various hereditary causes and genetic counseling are discussed. Grundfast notes that a specific diagnosis (e.g., Usher syndrome) can allow the anticipation of associated complications and their appropriate management. Occasionally, medical or surgical intervention may be needed (e.g., syphilis). Therefore, knowledge of a specific cause facilitates habilitation planning and family planning. The frequency of the various causes of hearing loss in children has changed over the past 30 years and will probably continue to change as newborn hearing screening becomes available to all children and as we develop more ways to prevent hearing loss. The greatest victories in the arena of prevention of hearing loss in children have been in the infectious diseases. Congenital rubella has become almost nonexistent in the United States with the introduction of the vaccine. With the introduction of the Haemophilus influenzae B vaccine, the bacterial meningitis that has been responsible for most meningitis-induced hearing loss has been enormously decreased. These advances have resulted in hereditary causes and neonatal intensive care unit (NICU) graduates contributing most children with hearing loss. In addition, cytomegalovirus (CMV) remains a common cause of hearing loss in children. [42] In this article, the many nongenetic causes of hearing loss are discussed. The article focuses on the most common causes of nongenetic hearing loss in 50 children and attempts to place them in the context of the changes in the major causes of hearing loss over the past few decades. NEONATAL INTENSIVE CARE UNIT GRADUATES Over the past 25 years, NICU graduates have increased in percentage of infants with hearing loss. In the 1960s and early 1970s, the proliferation of NICUs had not occurred, and low birth weight and perinatal factors accounted for perhaps 2% of the children with hearing loss [42] ; however, with the introduction of effective ventilation for respiratory distress syndrome in the early 1970s, a whole group of medically complex, at-risk children who had hearing loss were surviving. In the next decade, approximately 13% of children with hearing loss had been of low birth weight, whereas 4% had perinatal causes, thereby increasing the percentage of children with hearing loss who were NICU graduates to 17%. In the next decade (1983-1992), the percentage of children with hearing loss identified by NICU admission increased further, with 19% of children being of low birth weight and 8% having perinatal factors. How much of the increase in the percentage of children with hearing loss being identified with a NICU stay is related to the increased survival in infants of lower and lower birth weights, and how much is caused by the decrease during this 25-year period of rubella and meningitis as major causes of hearing loss in infants remains unclear. The category of NICU graduates easily identifies a group of children who are at risk for hearing loss for a variety of reasons. Of the 10 indicators repeatedly stated by the Joint Committee on Infant Hearing [37] as associated with the category of sensorineural or conductive hearing loss at birth through age 28 days, four specifically relate to NICU graduates' experience. These include (1) birth weight less than 1500 g; (2) hyperbilirubinemia at a serum level, requiring exchange transfusion; (3) Apgar scores of 0 to 4 at 1 minute or 0 to 6 at 5 minutes; and (4) mechanical ventilation lasting 5 days or longer. In addition, two more indicators are related to risks frequently found in NICU graduates: (1) ototoxic medications including, but not limited to, the aminoglycosides, used in multiple courses or in combination with loop diuretics and (2) bacterial meningitis. Also, children with in utero infections, such as CMV, rubella, herpes, syphilis, and toxoplasmosis; craniofacial anomalies, including those with morphologic abnormalities of the pinna and ear canal; or syndromes known to be associated with sensorineural or conductive hearing loss, such as children with Down syndrome, are frequently admitted to NICUs for associated health problems. NICU graduates have been exposed to unique health experiences: those medical conditions for which they required intensive care; the NICU experience, with the necessary, but potentially ototoxic, interventions and complications thereof; and the possible potentiating effects that these factors together may produce on the inner ear. In addition, children with sensorineural hearing loss who are NICU graduates have complex neurologic and other health problems. The lower the birth weight, the more likely a child will have neurosequelae, hearing loss or visual impairment, asthma, and cognitive impairment. [56] Most studies designed to determine the cause of hearing loss in NICU graduates have found that the main associated factors include hypoxia, hyperbilirubinemia, exposure to ototoxic medications, and illness. The significance of the various causes in the pathogenesis of sensorineural hearing loss is not fully understood, and controversy remains regarding their respective roles. Studies that have tried to identify specific causes for hearing loss found with increased 51 frequency in NICU graduates have been complicated by multiple factors. Frequently, studies have identified their subjects by starting with what is determined to be a high-risk group, such as children with a gestational age of less than 36 weeks. Many of the studies have been retrospective in design and of small numbers of children. Frequently, the definition of hearing loss has varied from study to study, making comparisons difficult. Many of the studies have not included all of the children admitted to the NICU. Hypoxia Most studies of the cause of hearing loss in NICU graduates have identified hypoxia to be a factor. In different studies, hypoxia has been defined differently. Hypoxia might be defined as apnea, [1] [4] a difficult delivery, [71] a history of duration of ventilation, [5] a lower Apgar score at 5 minutes, or a more frequently documented P O2 of less than 50 mm Hg. Bergman and colleagues [5] identified 36 children with a sensorineural hearing loss of less than 55 dB bilaterally in their NICU follow-up program, which included all infants of less than 1500 g birth weight or with neonatal seizures. Significant neonatal predictors of hearing loss in high-risk premature infants were prolonged respirator care, high serum bilirubin concentration, and hyponatremia. Eavey and colleagues [20] compared 23 patients identified between 1974 and 1986 with a sensorineural hearing loss of greater then 35 dB bilaterally and believed to include all patients identified during these years from the NICU population, with 17 infants serving as normal hearing controls. They performed univariate and multivariate analysis, examining 65 prenatal, perinatal, and NICU factors considered related to possible hearing loss. They found that a history of ventilation was the only factor associated with hearing loss ( p = 0.0023). Salamy and colleagues [68] studied prospectively 12 infants with sensorineural hearing loss from a group of 224 very low birth weight ( 1500 g) infants requiring NICU care. Salamy and colleagues [68] found that the infants with hearing loss had a P O2 less than 50 mm Hg more frequently than the control infants ( p < 0.01). They concluded that reliance on risk factors was an inadequate clinical method to select a patient for a hearing test, and that each NICU survivor deserved audiometric evaluation. In a study of risk factors of sensorineural hearing loss, Borradori and colleagues [7] compared eight children with sensorineural hearing loss with a control group retrospectively matched for similar birth weight and gestation to identify clinical risk factors. The study group all presented with severe respiratory distress syndrome, required prolonged mechanical ventilation (11-55 d), and all had none or several pneumothoraces. No significant differences were found in the incidence of perinatal asphyxia, hyperbilirubinemia, hyaline membrane disease, or persistent fetal circulation. The children with hearing loss were more likely to have pneumothoraces ( p = 0.0001), bronchopulmonary dysplasia ( p = 0.002), and renal failure ( p < 0.002). Borradori and colleagues [7] went on to identify a second control group with similar major perinatal complications, including respiratory distress syndrome, need for ventilation, and pneumothorax. The analyses of arterial blood gases and blood pressure did not reveal any statistical differences; however, the duration of mechanical ventilation ( p = 0.0001) and the length of NICU stay ( p = 0.005) were higher in the study group. Simmons [71] found that the NICU graduates with hearing loss had a higher incidence of certain factors than controls, including a difficult delivery by a factor of 3.8 and an Apgar score of 6 or less at 5 minutes by a factor of 7.9. Simmons' [71] findings are supported by an analysis of 290,737 births in Utah, [22] where they found that 52 the cutoffs of an Apgar score of 0 to 4 at 1 minute and 0 to 6 at 5 minutes were better indicators of possible hearing loss than were the previous criteria of a 5-minute Apgar score of 0 to 3. Persistent Pulmonary Hypertension and Extracorporeal Membrane Oxygenation In relation to the problem of hypoxia and associated sensorineural hearing loss (SNHL), two situations deserve special attention: persistent pulmonary hypertension (PPHN) and extracorporeal membrane oxygenation (ECMO). Persistent pulmonary hypertension or persistent fetal circulation occurs as a result of failure of the circulatory adaptation at birth with the high pulmonary vascular resistance present in utero continuing and causing right-to-left shunting at the levels of both the foramen ovale and ductus arteriosus. Persistent pulmonary hypertension is primarily a disorder of full-term infants and associated with severe hypoxemia. Although a recent follow-up study by Marron and colleagues [55] found none of 27 children with PPHN to have SNHL, most follow-up studies of this population have found an increased prevalence of SNHL of 20% to 53%. [30] [41] [70] In infants with PPHN, Hendricks-Munoz and Walton [30] found that infants with hearing loss were more likely to have alkalosis, a longer duration of ventilation, and to use furosemide, whereas Sell and colleagues [70] found a correlation between PPHN and maternal insulin-dependent diabetes. Of interest is a report by Kawashiro and colleagues [41] that 8 of 10 children who developed hearing loss after discharge from the NICU had PPHN, and 6 of the 8 had required ECMO. During that period, a total of 25 cases of PPHN had been treated, and 32% exhibited SNHL on follow-up. Desai and colleagues [14] found SNHL in 12 (15%) of 80 ECMO-treated children. The children with hearing loss did not differ with regard to neonatal clinical variables from those without hearing loss, but 7 of the 12 with hearing loss had normal initial neonatal brain stem auditory evoked potentials (BAEPs). These findings suggest that children who have been treated with ECMO and children with PPHN are at increased risk for late-onset hearing loss and need special monitoring. Hyperbilirubinemia Along with hypoxia, hyperbilirubinemia is the factor most frequently associated with sensorineural hearing loss in NICU graduates. In the presence of hyperbilirubinemia, specific aberrations appear in brain stem responses (ABRs). These aberrations disappear after exchange transfusion and the establishment of a normal bilirubin level. [45] [64] Most studies of NICU graduates include mainly low birth weight children and sick children; consequently, the level of bilirubinemia that is likely to be associated with a sensorineural hearing loss would be lower than with a preterm infant. Although a bilirubin level of 14 mg/dL is frequently cited as a level that places NICU graduates at increased risk for hearing loss, a specific toxic level of bilirubin elevation in premature infants cannot be defined because so many variables affect the dynamics of bilirubin binding to albumin and the degree of entry into the central nervous system. Acidosis, hypothermia, hypoxia, and low serum albumin concentration may increase the "neurotoxicity" of bilirubin, either by increasing the unbound portion of bilirubin or by increasing its access to the brain. DeVries and colleagues [15] found that in children with hyperbilirubinemia, adverse perinatal factors, such 53 as acidosis, a longer mean duration of hyperbilirubinemia (48 h versus 24 h), and lower birth weight, were associated with an increased risk for SNHL. Anagnostakis and colleagues [4] found hyperbilirubinemia (> 14 mg/dL) and apneic spells with bradycardia and cyanosis and hypothermia (temperature < 34.5°C) to be associated with hearing loss ( p < 0.001). In a study of 56 children of less than 1000 g birth weight, Doyle and colleagues [18] found that four children with SNHL had significantly higher maximum concentrations of bilirubin in the newborn period and required more intensive care. In his study of a group of NICU graduates with a birth weight of up to 1500 g or neonatal seizures, Bergman and colleagues [5] found that maximum serum bilirubin levels were one of several independent predictors of hearing loss and that a negative correlation was found with the number of exchange transfusions. Simmons [71] found that the incidence of hyperbilirubinemia was 2.5 times greater in children with SNHL. Ototoxic Medications The NICU population is more likely to be exposed to ototoxic medications than possibly any other group of children. The medications frequently used in the NICU and associated with SNHL include aminoglycosides, such as gentamycin and kanamycin, and diuretics, such as furosemide. The degree to which ototoxic medications used in the NICU contribute to the increased incidence of SNHL in this population is unclear. Several studies of the factors associated with SNHL in NICU graduates have not found the use of aminoglycosides in the NICU to be a significant predictor of SNHL. [5] [23] [68] Borradori and colleagues [7] found ototoxicity closely related to a prolonged administration and higher total doses of ototoxic drugs, particularly aminoglycosides and furosemide. Studies of furosemide in the neonatal period, especially with greater amounts of administration for longer durations and in combination with aminoglycosides, are associated with an increased risk for hearing loss. [68] MENINGITIS Between 1966 and 1992, meningitis was the cause of hearing loss in 6% to 13% of the children who had hearing loss. From 1966 to 1972, meningitis accounted for 6% of the cases of hearing loss, and from 1973 to 1982, meningitis increased to the point that it accounted for 13% of the cases of hearing loss in children. This was probably not necessarily caused by an increase in the number of cases of meningitis but probably by the extraordinary decrease in cases of rubella with the introduction of the rubella vaccine. Introduction of the first vaccine for H. influenzae type B (HIB) in 1985 resulted in a dramatic decrease in the incidence of invasive bacterial disease, including meningitis. The incidence of hospital admissions for meningitis decreased from 34 per 100,000 in 1982 to 1 per 100,000 children birth to 4 years of age in 1992. [51] During 1983 to 1992, the incidence of meningitis decreased and accounted for 7% of cases of hearing loss. [42] Bacterial meningitis has been the leading cause of acquired SNHL in children. Serial recordings of BAEP beginning within 48 hours of admission have shown the early occurrence of hearing loss, with a possible recovery or worsening occurring during the first 2 weeks with no cases of "late" deafness or "late" recovery. [40] [81] The number of days of illness before hospitalization and institution of antibacterial treatment has not been shown to correlate with the development of SNHL. [16] Some studies have indicated that the SNHL that complicates menin 54 gitis tends to be a defect isolated from other neurologic sequelae of meningitis, [24] whereas other studies have shown a high correlation with severe neurologic deficits. [16] Clinical and experimental research indicates that the hearing loss after meningitis is caused by cochlear damage by ototoxic drugs used to treat the meningitis or to direct damage to the cochlea by the meningitis. [26] By the 1970s, advances in antibiotic therapy resulted in decreased mortality rates from bacterial meningitis. Presently, for all types of bacterial meningitis, the mortality rate is 5% to 10%. [13] Significant morbidity, which was most frequently SNHL, has continued to be a problem. In a study of 185 cases of bacterial meningitis in children, Dodge and colleagues [16] found that overall 10.3% of the patients had persistent bilateral or unilateral SNHL, with Streptococcus pneumoniae having the highest incidence (31%), followed by Neisseria meningitidis (10.5%) and H. influenzae (6%). Introduction of cephalosporins, which have better access to the central nervous system, has improved outcomes. In addition, specifically in H. influenzae, studies of treatment early in the course of the meningitis with dexamethasone have demonstrated decreased hearing loss and neurologic sequelae. [13] The efficacy of dexamethasone in the treatment of pneumococcal or meningococcal meningitis has not been demonstrated [83] ; however, the Red Book [13] states that dexamethasone should be considered. In the past, H. influenzae was the infecting organism in most cases of bacterial meningitis in children and has therefore been studied the most. H. influenzae meningitis was complicated by SNHL in 9% to 18% of cases of H. influenzae meningitis [50] [78] with additional neurologic morbidity (e.g., blindness, seizures, cerebral palsy, or mental retardation) in 4% to 9%. S. pneumoniae not only has had the highest frequencies of SNHL but also has high mortality rates (17%-42%) [29] [31] [82] and neurologic morbidity in 12% to 13% [29] [82] of children. In one study of 80 children with meningitis caused by N. meningitidis, 8% of infections were fatal, and 9% developed an SNHL. [21] Little is reported about hearing loss in children with fungal infections, but Nadol [59] reported 3 children out of 7 children with fungal meningitis developed SNHL. There have been no studies of the sequelae of viral meningitis that have reported SNHL. [87] Clearly, all children with bacterial or fungal meningitis need to be evaluated for hearing loss; however, Fortnum and Hull [24] found in a survey of pediatricians in the United Kingdom that 10.6% did not routinely refer all children with meningitis for an evaluation of their hearing. Although gram-negative enteric bacillary meningitis accounts for only 3.6% of bacterial meningitis, the organisms are associated with a high mortality rate and devastating neurologic sequelae. In a survey of gram-negative enteric bacillary meningitis from 1969 to 1989 at Parkland Hospital, [79] the most frequent organism causing gram-negative enteric bacillary meningitis was Escherichia coli, accounting for 53% of cases, with the remainder being caused by Klebsiella enterobacter (16%), Citrobacter diversus (9%), Salmonella sp. (9%), and other gram-negative enteric bacilli less frequently encountered (13%). Most frequently, the infected children were neonates, with 50% ( n = 49) being term and 24% ( n = 23) being preterm, whereas 18% ( n = 18) were 1 to 3 months of age, and 8% ( n = 8) were more than 3 months of age. Predisposing problems included surgical problems, especially neural tube defects and urinary tract anomalies. The mortality rate was high (17%), and central nervous system sequelae, such as cerebral palsy, hydrocephalus, seizures, severe mental and neurologic damage requiring constant care, developmental delay with most being in the range of severe mental retardation, and hearing loss, were found in 61% of survivors. Seventeen percent of children had an SNHL. The literature on tuberculous meningitis comes from the early 1960s, when treatment included intramuscular and intrathecal streptomycin. The reported 55 incidence of SNHL in children who had tuberculous meningitis varied between 5% [52] and 37%, [49] with some researchers reporting an additional 15% incidence of high-frequency loss. Ototoxic treatment may have contributed to the high incidence of SNHL. CONGENITAL INFECTIONS Cytomegalovirus Cytomegalovirus infection occurs in 0.2% to 2.2% of all newborns, making it the most common intrauterine infection in humans. One third of pregnant women are seronegative for CMV; 2.5% to 6.8% of these women become infected during pregnancy, and 24% transmit the infection to their fetuses. [73] Of the women who are seropositive, 3.4% transmit CMV to their fetuses. [74] [92] Up to 10% of children with congenital CMV infection exhibit systemic and neurologic symptoms at birth, and 61% of these children develop SNHL. [65] Fowler [25] prospectively evaluated 307 children with documented asymptomatic congenital CMV infection and found that 22 (7.2%) had SNHL. Among the children with hearing loss, further deterioration of hearing occurred in 50.5%, and delayed-onset SNHL was observed in 18.2% of children with a median age of 27 months but as old as 60 months of age. In addition, fluctuating SNHL was documented in 22.7% of children with hearing loss. Eleven of the children had unilateral losses, and 12 of the ears had a severe to profound hearing loss. The authors speculated that more children with asymptomatic CMV would probably develop late-onset hearing loss and recommend that children with congenital CMV have continued monitoring of their hearing status. A prospective study of 108 children with congenital CMV infection indicated that children with congenital CMV represented approximately 12% of all children with congenital SNHL. [62] Herpes Simplex Infection Neonatal herpes simplex virus (HSV) infection is a rare but potentially fatal disease that occurs in 1 in 2500 to 1 in 10,000 pregnancies. [74] Infections are usually caused by exposure to the HSV type 2 (HSV-2) during delivery and rarely caused by in utero exposure to HSV-2 by maternal viremia. [86] Ninety-seven percent of children with HSV-2 present in the first 3 weeks of life with disseminated infection, encephalitis, or localized infection. The children with disseminated infection or encephalitis have high mortality rates (85% and 32%, respectively). [27] The neurologic impairment, including hearing loss, is found in most children with the disseminated presentation, 40% of the children with encephalitic presentation, and 25% of children with infection confined to the skin, mouth, or eyes. [85] Hutto and colleagues [33] reported on 13 infants who had clinical manifestations of intrauterine HSV infection, including skin lesions and scars, chorioretinitis, microcephaly, hydranencephaly, and microphthalmia. Two infants died, whereas 6 of the remaining 12 children had severe neurologic sequelae, including mental retardation, seizures, and three were blind and hard of hearing. Congenital Rubella The classic triad of congenital rubella includes congenital heart disease, vision problems, and SNHL. Before the development of the rubella vaccine, 0.1% 56 to 0.4% of children were born with congenital rubella, but since the introduction of the vaccine, congenital rubella has become rare. Sixty percent of newborns with congenital rubella have subclinical infections in the neonatal period, but 71% of these children go on to develop manifestations of infection within the next 5 years. Hearing loss is the most common permanent manifestation and affects 68% to 93% of children with congenital rubella. The SNHL is most frequently profound and bilateral, effects all frequencies equally, and is progressive in some cases. Central auditory imperception (an inability to respond to sound on a cortical basis) can complicate the evaluation and remediation of hearing loss. [3] Children with congenital rubella also have psychomotor retardation (17-63%, depending on how it is defined), cerebral palsy (50%), cataracts (50%) and other visual disorders, and seizures (6%). [66] Congenital Syphilis Since 1986, the prevalence of congenital syphilis, which is approximately 0.005% of live births, or 0.4% of the children of mothers with syphilis, has increased in parallel with an increased incidence of primary and secondary syphilis in the adult population. [34] One third to two thirds of newborns with congenital syphilis are asymptomatic. Hearing loss is one of the late manifestations of congenital syphilis and occurs after 2 years of age. The hearing loss results from persistent, active disease with ongoing inflammation and scarring. In 3% of children with congenital syphilis, SNHL develops in the first to fourth decades in association with vertigo and beginning in the high frequencies and progressing. [66] Congenital Toxoplasmosis A mass screening of 330,000 pregnant women revealed a seroconversion rate of 1 in 10,000. The overall rate of transmission of Toxoplasma to the fetus is 33%. At birth, 90% of the babies with congenital toxoplasmosis are asymptomatic. Educationally significant hearing loss has been reported in 10% to 15% of children with congenital toxoplasmosis. [58] In a group of 30 children with congenital toxoplasmosis treated at birth with pyrimethamine and sulfonamide preparations, McGee and colleagues [58] reported no development of hearing loss. Prenatal Toxic Syndromes Hearing loss has been described in association with prenatal exposure to alcohol, trimethadione, and methyl mercury, as well as prenatal iodine deficiency. Fetal alcohol syndrome includes growth retardation, dysmorphic facial features, and developmental and behavioral disorders, including mental retardation, attention deficit hyperactivity disorder, and language delays. Although not reported to be a common feature of fetal alcohol syndrome, 14 children with fetal alcohol syndrome unselected for hearing loss and referred for otolaryngology evaluation were found to have a high prevalence of conductive and sensorineural hearing loss. Thirteen of the children (93%) had clinically significant histories of bilateral recurrent serous otitis media, and four (29%) had bilateral sensorineural hearing loss. [10] Abnormalities have been found in the offspring of children 57 whose mothers have had seizures treated with trimethadione. The children have been reported to have mental deficiency, prenatal onset growth deficiency, facial dysmorphology, septal defects of the heart and tetralogy of Fallot, and occasionally hearing deficits. [39] The sources of methyl mercury exposure during pregnancy can include fish from contaminated water, flour made from methyl mercury-treated seed grain, or meat eaten from animals reared on such seed grain. Prenatal exposure usually leaves permanent sequelae of all gradations. The fetus may exhibit poor growth, microcephaly, aberrant muscle tone, hearing loss, and blindness. [39] Severe iodine deficiency during gestation has been shown to result in fetal iodine deficiency, which is characterized by mental deficiency, SNHL, spastic diplegia, strabismus, and nystagmus. OTITIS MEDIA, HEARING LOSS, AND DEVELOPMENTAL SEQUELAE Otitis media has its peak incidence in children who are 6 months to 18 months of age. After every episode, fluid persists in the middle ear for weeks to months. Conductive hearing loss usually accompanies the fluid, with a median loss of 25 dB. [43] The conductive hearing loss is reversed with the resolution of the middle ear effusion. Although not common, permanent SNHL has been described in association with otitis media. There continues to be concern but no resolution about the sequelae of the fluctuating hearing loss associated with otitis media. Hubbard and colleagues [32] studied 24 children with cleft palate and aggressive treatment to maintain ventilation in the middle ear with controls who presumably had had continuous middle ear effusion for the first few years of life. He found mean verbal, performance, and full-scale IQs were normal in both groups and not significantly different. On the other hand, the Greater Boston Otitis Media Study Group evaluated 207 children followed prospectively from birth until age 7 years. They found that the more time spent with middle ear effusion during the first 3 years of life, the lower the full-scale, performance, and verbal Wechsler Intelligence Scale for Children-Revised (WISC-R) IQ scores and the lower the scores in mathematics and reading on the Metropolitan Achievement Test. [77] OTOTOXIC MEDICATIONS AND SUBSTANCES Hearing loss from ototoxic medications, such as gentamycin, and toxic substances, such as lead, are an infrequent and preventable cause of SNHL in children. These substances may permanently injure or destroy the hair cells of the cochlea, resulting in an SNHL. Exposure to some drugs causes irreversible SNHL, whereas other drugs cause hearing loss that is reversible once the drug is stopped. In some instances, the ototoxic effects may not develop for up to 6 months after exposure. [90] With drugs excreted by the kidney, increase of drug levels to the ototoxic range is more likely to be complicated by hearing loss. [9] There appears to be both idiosyncratic and genetic susceptibility to ototoxic drugs. [36] The hearing impairment caused by drugs is usually bilateral, symmetric, and of varying severity. Hearing loss is usually progressive, with the high frequencies affected first. The ingestion of ototoxic drugs by pregnant women can result in hearing loss of prenatal origin. The period in gestation when the use of ototoxic medications is most likely to cause damage to the auditory system is in the first trimester, especially in the sixth and seventh weeks. In hearing loss secondary 58 to exposure to ototoxic drugs, otologic anomalies have included aplasia of the inner ear, outer and inner hair cell damage, middle ear anomalies, absence of the VIIth and VIIIth nerves, dysplasia of the organ of Corti, and a decreased number of ganglion cells. Prenatal use of ototoxic medications has been believed to cause conductive hearing loss as a result of ossicular malformation of the middle ear. NOISE-INDUCED HEARING LOSS Although the phenomenon of noise-induced hearing loss (NIHL) has been appreciated for more than 100 years, most of the interest has focused on hazardous noise in the occupational environment. NIHL accounts for a small percentage of the hearing loss in children but is a preventable cause of hearing loss. The audiometric configuration classified as NIHL has a decreased sensitivity of at least 15 dB at any or all of the frequencies 3000, 4000, or 6000 Hz, as well as an improved threshold of at least 10 dB at 8000 Hz. With continued exposure to loud sounds, the classic notch-type configuration has been observed [2] to evolve into a nonspecific high-frequency hearing loss with gradual disappearance of the characteristic audiometric notch with continued exposure to loud sounds. Exposure to potentially injurious sounds may result in a temporary threshold shift (TTS), acoustic trauma, or NIHL. Moderate exposure to potentially damaging sounds may initially cause a TTS with associated subtle anatomic changes, such as swelling of hair cells and the afferent fibers under the inner hair cells, vascular spasm, and metabolic exhaustion. [48] What may begin as a TTS can gradually become an NIHL with repeated exposure. A period of exposure to an intense, short-duration noise greater than 140 dB peak sound pressure level, such as an explosion may produce an immediate, severe, and permanent hearing loss exemplifying acoustic trauma. With acoustic trauma, the organ of Corti may actually be displaced from the basilar membrane, and swollen degenerating hair cells and swollen nerve fibers and endings may be seen at the edges of the lesion. [8] The evidence that fetuses and newborns exposed to excessive noise may suffer SNHL is unclear. In a retrospective study of children 4 to 10 years of age, the children born to women who were exposed consistently to occupational noise in the range of 85 to 95 dB during pregnancy were more likely to have a high-frequency hearing loss. [47] Other studies have been inconsistent in relation to exposure to excessive noise and congenital malformations. [38] [46] [93] Several studies have shown an increased risk of shortened gestation in women exposed to noise. [53] [54] [57] [69] In one study, women exposed to 80 dB for an 8-hour shift were at increased risk for preterm delivery (relative risk, 1.6). [54] Other studies have found no increase in preterm births or were inconclusive. [28] [60] [63] [93] Studies of decreased birth weight and an association with noise exposure have also been inconsistent. Many studies have documented the continuous noise exposure associated with NICUs varies from 60 dB to 80 dB, [8] with intense short duration noise from such things as the closing of the metal cabinet doors (90 dB) and dropping the head of the mattress (120 dB). [12] Of the many studies that have documented hearing loss in NICU graduates, three have investigated the synergism of aminoglycosides and noise exposure with conflicting results. [4] [18] [75] [89] Winkel and colleagues [89] found that all five cases of children with moderate to severe sensorineural hearing loss had been exposed to kanamycin and kept in an incubator. Stennert and colleagues [75] found that 52% of 56 incubator-treated children with 59 normal hearing had minor changes on their audiograms, suggestive of noise-induced cochlear lesions. Conversely, Anagnostakis and colleagues [4] assessed the hearing of 98 preterm NICU graduates when they were 6.5 years of age and found no association with duration of incubator care or exposure to aminoglycosides of conventional ventilation. Children and adolescents have many opportunities for exposure to loud noises and the development of noise-induced hearing loss. Riding for 2 hours on a snowmobile with exposure to sound pressure levels of 105 dB to 136 dB [6] or being present at a rock concert, where sound levels of 105 dB to 115 dBA are quite common [11] have been observed to cause a TTS. Adolescents actively involved in farm work or children exposed for extended periods of time to noisy machinery, such as tractors, which produce sound levels of 95 dBA or greater at full throttle, are at risk. Impulse noises, such as gunfire or firecrackers, are characterized by very high sound intensity levels and short duration. The initial acoustic pulse of a gun discharge may have a peak sound level from 132 dB to 179 dB, with the potential for immediate and permanent NIHL. [84] A study by Brookhauser and colleagues [8] described a population of 114 children and adolescents with NIHL, which provides information of the probable exposures that caused the hearing loss and the types of hearing loss seen. His study group had a striking preponderance of males over females (90.3% to 9.7%) compared with 58.6% males in the entire data base of the Boys Town National Research Hospital. Twenty-six percent of the losses were identified before 10 years of age, and 75% before 16 years of age. Hearing losses were asymmetric (having a difference in thresholds between ears of 15 dB or greater in one or more of the frequencies between 3000 and 8000 Hz) in 71% of the population, including 86% of the children exposed to high levels of pulse noise from fireworks and firearms. Losses attributed to high levels of continuous noise, such as music, recreational vehicles, and power tools or equipment showed less of a tendency toward asymmetry (55%). Of the 94 children, 24 children had an unspecified noise source, with the remaining sources being fireworks or firearms (29), music (11), power tools or equipment (7), recreational vehicles (4), and multiple sources (19). HEAD TRAUMA Although conductive, sensorineural, and mixed hearing losses have been reported as a complication of head trauma in children, few prospective studies have shown hearing loss in children who suffered head injuries. Zimmerman and colleagues [94] studied 50 children 2 to 17 years of age admitted to the neurosurgical service of a children's hospital for head trauma following a fall (52%), an automobile accident (22%), being struck by an automobile (16%), and assault (10%). Audiologic evaluations generally performed within 24 to 48 hours of admission revealed hearing loss in 50% of the children, with 32% being conductive, 16% high-frequency sensory, and 2% mild mid-frequency loss. All of the patients with temporal bone fractures had conductive hearing losses, but the presence of skull fault fracture did not correlate with the presence, type, or degree of hearing loss. In addition, no correlation was found between either cause of injury, loss of consciousness, or Glasgow Coma Scale scores, and the presence, type, or degree of hearing loss. By the 6- to 8-month follow-up, all eight children with conductive hearing loss and temporal bone fractures had regained their hearing. The children with conductive hearing loss without temporal bone fractures were lost to follow-up, and of the six children with the 60 high-frequency SNHL who came for follow-up, five showed complete resolution. The one patient with the mild mid-frequency hearing loss had no change in hearing loss but originally had a pattern typical of congenital abnormalities. Dorman [17] studied 40 patients aged 6 to 16 years who had minor head injuries defined by a loss of consciousness from head injury. SNHL was sustained in 25%, with half in the lower frequencies and half in the high frequencies but none greater than 30 dB. At follow-up 6 months later, none of the hearing losses persisted. OTHER CAUSES OF HEARING LOSS Mumps Mumps is a systemic disease characterized by swelling of the salivary gland. Approximately one third of infections, however, do not cause clinically apparent salivary gland swelling. Encephalitis occurs rarely, and permanent sequelae are uncommon. Complications include orchitis, which rarely results in sterility, arthritis, renal involvement, thyroiditis, mastitis, pancreatitis, and hearing loss. With the introduction of the measles, mumps, and rubella (MMR) vaccine, the incidence of mumps infections has decreased to 1500 cases per year, with the highest rates being in 5- to 9-year-olds. [13] Hearing loss from mumps is rare. In a group of 40,000 students enrolled in special education programs for children with hearing loss, only 0.6% of the cases were caused by mumps. [35] Yanagita and Murahashi [91] reviewed 95 cases (98 ears) of mumps deafness. The age of onset of deafness was less than 9 years in most patients, and no cases of hearing improvement were observed. Other diseases in which the complication of SNHL has been reported include infectious mononucleosis, [88] Kawasaki disease, [76] pertussis, [9] and scarlet fever. Hearing loss from tuberculosis may be a complication of tuberculous middle ear and mastoid disease [72] or meningitis. Measles (rubeola) complicated by acute encephalomyelitis may result in SNHL. [44] Hypothyroidism Congenital hypothyroidism increases the risk for hearing loss in children. Rovet and colleagues [67] retrospectively studied 101 children followed longitudinally to evaluate newborn screening for hypothyroidism. Of seventy-five children who had previously had their hearing tested, 15 (20%) had hearing loss: 5 were conductive, 2 unilateral, and 3 bilateral; 9 sensorineural (1 unilateral, 8 bilateral; 1 child had bilateral sensorineural and conductive losses). The hearing loss was mild (21-40 dB) in 10 cases, moderate (41-55 dB) in 2 cases, and moderately severe (56-70 dB) in 3 cases. The children with hearing loss differed from the children without hearing loss in age of treatment onset (22 vs 14 days) but not in disease severity or duration. EVALUATION OF THE ETIOLOGY OF HEARING LOSS Every child with hearing loss is entitled to an evaluation to determine the cause of the hearing loss. The medical evaluation includes the basics of a good pregnancy, labor, delivery history, medical history, family history, and physical 61 examination followed by indicated laboratory tests. A history of meningitis, a NICU experience, or family members with hearing loss are helpful in pointing to a cause but are not always present. If the medical evaluation is negative, the most likely cause may be genetic or perhaps a congenital infection, and further evaluation in these directions is warranted. The identification of a cause is important for planning a habilitation plan, for knowing the prognosis, for medical monitoring because so many syndromes have associated disorders, and for family planning. References 1. Abramovich SJ, Gregory S, Slemick M, et al: Hearing loss in very low birthweight infants treated with neonatal intensive care. Arch Dis Child 54:421, 1979 Abstract 2. Alberti PW: Clinical criteria: Noise or not? Presented at the NIH Consensus Development Conference, January 1990, p 27 3. Ames MD, Plotkin SA, Winchester RA, et al: Central auditory imperception: A significant factor in congenital rubella deafness. JAMA 213:419, 1970 Citation 4. Anagnostakis D, Petmezakis J, Papazissis G, et al: Hearing loss in low birth-weight infants. Am J Dis Child 136:602, 1982 Abstract 5. Bergman I, Hirsch RP, Fria TJ, et al: Cause of hearing loss in high-risk premature infant. J Pediatr 106:95, 1985 Abstract 6. Bess FH, Poyner MA: Snowmobile engine noise and hearing. Arch Otolaryngol 95:45, 1972 Citation 7. Borradori C, Fawer CL, Buclin T, et al: Risk factors of sensorineural hearing loss in preterm infants. Biol Neonate 7:1, 1997 Abstract 8. Brookhouser PE, Worthington DW, Kelly WJ: Noise-induced hearing loss in children. Laryngoscope 102:645, 1992 Abstract 9. Catlin FJ: Prevention of hearing impairment from infection and ototoxic drugs. Arch Otolaryngol 111:377, 1985 Abstract 10. Church MW, Gerkin KP: Hearing disorders in children with fetal alcohol syndrome: Findings from case reports. Pediatrics 82:147, 1988 Abstract 11. Clark WW: Noise exposure and hearing loss from leisure activities. Presented at the NIH Consensus Development Conference, January 1990, p 55 12. Committee on Environmental Health American Academy of Pediatrics: Noise: A hazard for the fetus and newborn. Pediatrics 100:724, 1997 Full Text 13. Committee on Infectious Diseases American Academy of Pediatrics Antimicrobials on Related Therapy: In 1997 Red Book, ed 24. Elk Grove Village, American Academy of Pediatrics, 1997, p 620 14. Desai S, Kollros PR, Graziani LJ, et al: Sensitivity and specificity of the neonatal brainstem auditory evoked potential for hearing and language deficits in survivors of extracorporeal membrane oxygenation. J Pediatr 13:233, 1997 Full Text 15. de Vries LS, Lary S, Dubowitz LMS: Relationship of serum bilirubin levels to ototoxicity and deafness in high-risk low-birth-weight infants. Pediatrics 76:351, 1985 Abstract 16. Dodge PR, Davis H, Feigen RD, et al: Prospective evaluation of hearing impairment as a sequela of acute bacterial meningitis. N Engl J Med 311:869, 1984 Abstract 17. Dorman EB: Hearing loss in minor head injury. N Z Med J 95:454, 1982 Abstract 18. Doyle LW, Keir E, Kitchen WH, et al: Audiologic assessment of extremely low birth weight infants: A preliminary report. Pediatrics 90:744, 1992 Abstract 19. D'Souza SW, McCartner E, Nolan M, et al: Hearing, speech, and language in survivors of severe perinatal asphyxia. Arch Dis Child 56:245, 1981 Abstract 20. Eavey RD, do Carmo C, Bertero M, Thornton AR, et al: Failure to clinically predict NICU hearing loss. Clin Pediatr 34:138, 1995 Abstract 21. Edwards MS, Baker CJ: Complications and sequelae of meningococcal infections in children. J Pediatrics 99:540, 1981 22. Eichwald J, Mahoney T: Apgar scores in the identification of sensorineural hearing loss. J Am Acad Audiol 4:133, 1993 Abstract 62 23. Finitzo-Hieber R, Mc Cracken GH, Brown KC: Prospective controlled evaluation of auditory function in neonates given netilmicin or amikacin. J Pediatr 106:129, 1985 Abstract 24. Fortnum HM, Hull D: Is hearing assessed after bacterial meningitis? Arch Dis Child 67:1111, 1992 Abstract 25. Fowler KB, McCollister FP, Dahle AJ, et al: Progressive and fluctuating sensorineural hearing loss in children with asymptomatic congenital cytomegalovirus infection. J Pediatr 130:624, 1997 Full Text 26. Francois M, Laccourreye, Huy ETB, et al: Hearing impairment in infants after meningitis: Detection by transient evoked otoacoustic emissions. J Pediatr 130:712, 1997 Full Text 27. Freij BJ, Sever JL: Herpes virus infections in pregnancy: Risks to embryo, fetus, and neonate. Clin Perinatol 15:208, 1988 28. Harlikainen AI, Sorri M, Anttonen H: Effects of occupational noise on the course and outcome of pregnancy. Scand J Work Environ Health 20:444, 1994 Abstract 29. Haslam RHA, Allen JR, Dorsen MM, et al: The sequelae of group B B-hemolytic streptococcal meningitis in early infancy. Am J Dis Child 131:845, 1977 Abstract 30. Hendricks-Munoz KD, Walton JP: Hearing loss in infants with persistent fetal circulation. Pediatrics 81:650, 1988 Abstract 31. Horn KA, Zimmerman RA, Knostman JD, et al: Neurological sequelae of group B streptococcal neonatal infection. Pediatrics 53:501, 1974 Citation 32. Hubbard TW, Paradise JL, McWilliams BJ, et al: Consequences of unremitting middle-ear disease in early life otologic, audiologic, and developmental findings in children with cleft palate. N Engl J Med 312:1529, 1985 Abstract 33. Hutto C, Arvin A, Jacobs R, et al: Intrauterine herpes simplex virus infections. J Pediatr 110:97, 1987 Abstract 34. Ikeda MK, Jenson HB: Evaluation and treatment of congenital syphilis. J Pediatr 117: 843, 1990 35. Jensema C: Children in educational programs for the hearing impaired, whose impairment was caused by mumps. J Speech Hear Dis 40:164, 1975 36. Johnsonbaugh RE, Drexler HG, Light IJ, et al: Familial occurrence of drug-induced hearing loss. Am J Dis Child 127:245, 1974 Citation 37. Joint Committee on Infant Hearing: Joint Committee on Infant Hearing 1994 Position Statement. Pediatrics 95:152, 1995 Full Text 38. Jones FN, Tauscher J, Jones KL (ed): Residency under an airport landing pattern as a factor in teratism. Arch Environ Health 33:10, 1978 Abstract 39. Jones KL: Fetal trimethadione syndrome. In Jones KL (ed): Smith's Recognizable Patterns of Human Malformation, ed 5. Philadelphia, WB Saunders, 1997, p 564 40. Kaplan SL, Catlin FI, Weaver T, et al: Onset of hearing loss in children with bacterial meningitis. Pediatrics 73:575, 1984 Abstract 41. Kawashiro N, Tsuchihashi N, Koga K, et al: Delayed post-neonatal intensive care unit hearing disturbance. Int J Pediatr Otorhinolaryngol 34:35, 1996 Abstract 42. Kile JE: Identification of hearing impairment in children: A 25-year review. InfantToddler Intervention 3:155, 1993 43. Klein JO: Otitis media. In Katz SL, Gershon AA, Hotez PJ (eds): Krugman's Infectious Diseases of Children, ed 10. St. Louis, Mosby, 1998, p 302 44. Krugman S, Katz SL, Gershon AA, et al: Measles. In Krugman S, Katz SL, Gershon AA, et al: Infectious Diseases of Children, ed 9. St. Louis, Mosby, 1992, p 223 45. Kuriyama M, Tomiwa K, Konishi Y, et al: Improvement in auditory brainstem response of hyperbilirubinemic infants after exchange transfusions. Pediatr Neurol 2:127, 1986 Abstract 46. Kurppa K, Rantala K, Nurminen T, et al: Noise exposure during pregnancy and selected structural malformations in infants. Scand J Work Environ Health 15:111, 1989 Abstract 47. Lalande NM, Hetu R, Lambert J: Is occupational noise exposure during pregnancy a risk factor of damage to the auditory system of the fetus? Am J Ind Med 70:427, 1986 Abstract 48. Liberman MC: Biological Bases of Acoustic Injury. Presented at the NIH Consensus Development Conference, January 1990, p 21 49. Lincoln EM, Sordillo SVR, Davies PA: Tuberculous meningitis in children. J Pediatr 57:778, 1960 50. Lindberg J, Rosenhall U, Nylen O, et al: Long-term outcome of Haemophilus influenzae meningitis related to antibiotic treatment. Pediatrics 60:1, 1977 Abstract 63 51. Liptak GS, McConnochie KM, Roghmann KJ, et al: Decline of pediatric admissions with Haemophilus influenzae type b in New York State, 1982 through 1993: Relation to immunizations. J Pediatr 130:923, 1997 Full Text 52. Lorber J: Long-term follow-up of 100 children who recovered from tuberculous meningitis. Pediatrics 28:778, 1961 53. Luke G, Mamolle N, Keith L, et al: The association between occupational factors and preterm birth: A United States Nurses' study. Am J Obstet Gynecol 173:849, 1995 Full Text 54. Mamelle N, Laumon B, Lazar P, et al: Prematurity and occupational activity during pregnancy. Am J Epidemiol 119:309, 1984 Abstract 55. Marron M-J, Crisafi MA, Driscoll JM Jr, et al: Hearing and neurodevelopmental outcome in survivors of persistent pulmonary hypertension of the newborn. Pediatrics 90:392, 1992 Abstract 56. McCormick MC, Brooks-Gunn J, Workman-Daniels K, et al: The health and developmental status of very low-birth-weight children at school age. JAMA 267:2204, 1992 Abstract 57. McDonald AD, McDonald JC, Armstrong B, et al: Prematurity and work in pregnancy. Br J Ind Med 45:56, 1988 Abstract 58. McGee T, Wolters C, Stein L, et al: Absence of sensorineural hearing loss in treated infants and children with congenital toxoplasmosis. Otolaryngol Head Neck Surg 106:75, 1992 Abstract 59. Nadol JB: Hearing loss as a sequela of meningitis. Laryngoscope 88:739, 1978 Abstract 60. Nurminen T, Kurppa K: Occupational noise exposure and course of pregnancy. Scand J Work Environ Health 15:117, 1989 Abstract 61. Paparella MM, Fox RY, Schachern PA: Diagnosis and treatment of sensorineural hearing loss in children. Otolaryngol Clin North Am 22:51, 1989 Abstract 62. Peckham CS, Stark O, Dudgeon JA, et al: Congenital cytomegalovirus infection: A cause of sensorineural hearing loss. Arch Dis Child 62:1233, 1987 Abstract 63. Peoples-Sheps MD, Siegel E, Suchipdran CM, et al: Characteristics of maternal employment: Effects on low birthweight. Am J Public Health 81:1007, 1991 Abstract 64. Perlman M, Fainmesser P, Sohmer H, et al: Auditory nerve-brainstem evoked responses in hyperbilirubinemic neonates. Pediatrics 72:658, 1983 Abstract 65. Ramsay MEB, Miller E, Peckham CS: Outcome of confirmed symptomatic congenital cytomegalovirus infection. Arch Dis Child 66:1068, 1991 Abstract 66. Roizen NJ, Johnson D: Congenital infections. In Capute AJ, Accardo PJ (eds): Developmental Disabilities in Infancy and Childhood, ed 2. Baltimore, Paul H. Brookes, 1996, p 175 67. Rovet J, Walker W, Bliss B, et al: Long-term sequelae of hearing impairment in congenital hypothyroidism. J Pediatr 128:776, 1996 Full Text 68. Salamy A, Eldredge L, Tooley WH: Neonatal status and hearing loss in high-risk infants. J Pediatr 114:847, 1989 Abstract 69. Schell LM: Environmental noise and human prenatal growth. Am J Phys Anthropol 56:63, 1981 Abstract 70. Sell EJ, Gaines JA, Gluckman C, et al: Persistent fetal circulation neurodevelopmental outcome. Am J Dis Child 139:25, 1985 Abstract 71. Simmons FB: Patterns of deafness in newborns. Laryngoscope 90:448, 1980 Abstract 72. Skolnic PR, Nadol JB Jr, Baker AS: Tuberculosis of the middle ear: Review of the literature with an instructive case. Rev Infect Dis 8:403, 1986 Abstract 73. Stagno S, Whitley RJ: Herpesvirus infections of pregnancy. Part II. Herpes simplex, virus and varicella-zoster virus infections. N Engl J Med 313:1327, 1985 Citation 74. Stagno S, Pass RF, Cloud G, et al: Primary cytomegalovirus infection in pregnancy: Incidence, transmission to fetus, and clinical outcome. JAMA 256:1904, 1986 Abstract 75. Stennert E, Schultz PJ, Vollrath M, et al: The etiology of neurosensory hearing defects in preterm infants. Arch Otorhinolaryngol 221:171, 1978 Abstract 76. Sundel RP, Newburger JW, McGill T, et al: Sensorineural hearing loss associated with Kawasaki disease. J Pediatr 117:371, 1990 Abstract 77. Teele DW, Klein JO, Chase C, et al: Otitis media in infancy and intellectual ability, school achievement, speech, and language at age 7 years. J Infect Dis 162:685, 1990 Abstract 78. Tejani A, Dobias B, Sambursky J: Long-term prognosis after H. influenzae meningitis: Prospective evaluation. Dev Med Child Neurol 24:338, 1982 Abstract 64 79. Unhanand M, Mustafa MM, McCracken GH, et al: Gram-negative enteric bacillary meningitis: A twenty-one-year experience. J Pediatr 122:15, 1993 Abstract 80. Vartiainen E, Karjalainen S, Karja J: Auditory disorders following head injury in children. Acta Otolaryngol (Stockh) 99:529, 1985 Abstract 81. Vienny H, Despland PA, Lutschg J, et al: Early diagnosis and evolution of deafness in childhood bacterial meningitis: A study using brainstem auditory evoked potentials. Pediatrics 73:579, 1984 Abstract 82. Wald ER, Bergman I, Taylor HG, et al: Long-term outcome of group B streptococcal meningitis. Pediatrics 77:217, 1986 Abstract 83. Wald ER, Kaplan SL, Mason EO, et al: Dexamethasone therapy for children with bacterial meningitis. Pediatrics 95:21, 1995 Full Text 84. Ward WD: Impulse/impact vs continuous noise. Presented at the NIH Consensus Development Conference, January 1990, p 47 85. Whitley R, Hutto C: Neonatal herpes simplex virus infections. Pediatr Rev 7:119, 1985 86. Whitley R, Arvin A, Prober C, et al: Predictors of morbidity and mortality in neonates with herpes simplex virus infections. N Engl J Med 324:450, 1991 Abstract 87. Wilfert CM, Thompson RJ, Sunder TR, et al: Longitudinal assessment of children with enteroviral meningitis during the first three months of life. Pediatrics 67:811, 1981 Abstract 88. Williams LL, Lowery HW, Glaser R: Sudden hearing loss following infectious mononucleosis: Possible effect of altered immunoregulation. Pediatrics 75:1020, 1985 Abstract 89. Winkel S, Bonding P, Larsen PK, et al: Possible effects of kanamycin and incubation in newborn children with low birth weight. Acta Paediatr Scand 67:709, 1978 Abstract 90. Wong D, Shah CP: Identification of impaired hearing in early childhood. Can Med Assoc J 121:529, 1979 Abstract 91. Yanagita N, Murahashi K: A comparative study of mumps deafness and idiopathic profound sudden deafness. Arch Otorhinolaryngol 243:197, 1986 Abstract 92. Yow MD, Williamson DW, Leeds LJ, et al: Epidemiologic characteristics of cytomegalovirus infection in mothers and their infants. Am J Obstet Gynecol 158:1189, 1988 Abstract 93. Zhang J, Cai WW, Lee DJ: Occupational hazards and pregnancy outcomes. Am J Ind Med 21:397, 1992 Abstract 94. Zimmerman WD, Ganzel TM, Windmill IM, et al: Peripheral hearing loss following head trauma in children. Laryngoscope 103:87, 1993 Abstract MD Consult L.L.C. http://www.mdconsult.com Bookmark URL: /das/journal/view/N/10575693?ja=136911&PAGE=1.html&ANCHOR=top&source=HS,MI