Diagnostic Right Ventricle
advertisement
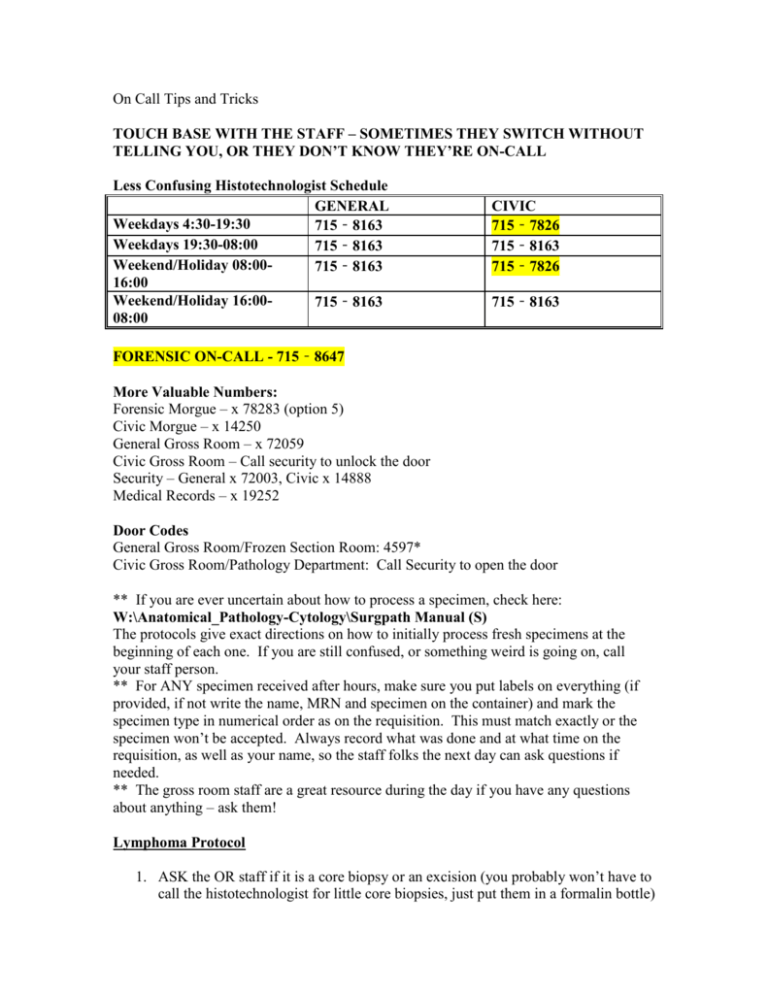
On Call Tips and Tricks TOUCH BASE WITH THE STAFF – SOMETIMES THEY SWITCH WITHOUT TELLING YOU, OR THEY DON’T KNOW THEY’RE ON-CALL Less Confusing Histotechnologist Schedule GENERAL Weekdays 4:30-19:30 715‐8163 Weekdays 19:30-08:00 715‐8163 Weekend/Holiday 08:00715‐8163 16:00 Weekend/Holiday 16:00715‐8163 08:00 CIVIC 715‐7826 715‐8163 715‐7826 715‐8163 FORENSIC ON-CALL - 715‐8647 More Valuable Numbers: Forensic Morgue – x 78283 (option 5) Civic Morgue – x 14250 General Gross Room – x 72059 Civic Gross Room – Call security to unlock the door Security – General x 72003, Civic x 14888 Medical Records – x 19252 Door Codes General Gross Room/Frozen Section Room: 4597* Civic Gross Room/Pathology Department: Call Security to open the door ** If you are ever uncertain about how to process a specimen, check here: W:\Anatomical_Pathology-Cytology\Surgpath Manual (S) The protocols give exact directions on how to initially process fresh specimens at the beginning of each one. If you are still confused, or something weird is going on, call your staff person. ** For ANY specimen received after hours, make sure you put labels on everything (if provided, if not write the name, MRN and specimen on the container) and mark the specimen type in numerical order as on the requisition. This must match exactly or the specimen won’t be accepted. Always record what was done and at what time on the requisition, as well as your name, so the staff folks the next day can ask questions if needed. ** The gross room staff are a great resource during the day if you have any questions about anything – ask them! Lymphoma Protocol 1. ASK the OR staff if it is a core biopsy or an excision (you probably won’t have to call the histotechnologist for little core biopsies, just put them in a formalin bottle) 2. Call the histotechnologist on call (remember to ask the clinician which campus to go to….yes I’ve forgotten this) 3. Either go to the OR (you can ask the surgeon to observe the excision – quite often they will give you more tissue if you need it, and ask for extra labels) or to the ACC desk to pick up the specimen, and bring it to the gross room (code 4597*). It’s better to pick up the specimen from the OR yourself to be safe (this goes for any specimen, actually). Remember to cover the specimen to discourage nosey/easily freaked out people, and wear gloves. 4. Measure, describe and write down your observations (mention if the specimen was received fresh or *gasp* already in formalin). Size in three dimensions for lymph node, amount of attached soft tissue. Describe the cut surface appearance homogeneous, nodular, hemorrhagic, necrotic, fibrotic, colour, and/or necrosis. For cores, give the length and diameter of the smallest fragment and of the largest fragment. 5. If there is a lot of tissue, bisect it on the longitudinal axis, save the majority for formalin fixation, and small (pinky-fingernail-sized sections) for snap-frozen and flow cytometry. The tissue priority is: A) Formalin fixation B) Snap-frozen C) Flow cytometry 6. If you are waiting for the histotechnologist, put the remaining pieces in a petri dish with a little saline (you can leave at this point as long as the technologist knows where to find the tissue) 7. Put all cores through for formalin fixation for diagnosis, no matter how many cores are received. 8. Go home. Frozen Section 1. Ask the following – Where, When will the tissue be ready, What is it? 2. Call your staff (if your staff person is unavailable or not answering, you can try the residents’ room to ask if there are any other staff around willing to cover. Otherwise, you have to call the Department Chief – Dr. Burns) 3. Call the histotechnologist (try not to make calls on the road – be safe, and I’ve been ticketed before…the “I’m a doctor” riff doesn’t work) 4. Wear scrubs. Sometimes you’ll have to go to the OR, especially at the Civic, and it saves time and effort 5. Proceed as per regular frozen section protocols 6. Go home. Breast – Mastectomy 1. Check with the gross room staff during the day to identify any late breast cases 2. If you’re aware of a late breast case, keep track of it. Call the OR if you haven’t heard anything. Check the ACC, Lab Receiving and Gross Room. Remember – you only have 1 HOUR to process the specimen and put it in formalin; don’t wait. 3. Check the time the specimen was removed by the OR on the requisition. If it’s not there, CALL the OR to confirm the time. 4. Write the time the specimen was received in Pathology on the requisition 5. Ink the resected margins (all the fat, leave the skin alone) 6. Orient the specimen (usually with sutures; if you can’t orient it, call the surgeon), and describe any lesions you might see (especially on the skin) 7. Sharpen the knife 8. With the skin facing down, slice in 1cm sections, from deep to superficial and medial to lateral, down close to the skin but not through it. You can use a folded wet paper towel to hold the specimen steady. Aren’t you glad you sharpened the knife? 9. The tumour must be exposed. If you don’t see it, check Oacis for radiological details. If it’s a neo-adjuvant case, you might see a lot of fibrotic white tissue – section it as best as you can. 10. Place folded pieces of paper towel between each section to maximize formalin exposure. 11. Put the specimen in a white bucket with formalin and RECORD THE TIME on the requisition. 12. If it’s a really big specimen, use one of the larger, reusable plastic containers used for cassettes. 13. Go home. Breast – Lumpectomy 1. Check the time the specimen was removed by the OR on the requisition. If it’s not there, CALL the OR to confirm the time. 2. Write the time the specimen was received in Pathology on the requisition 3. If the specimen is received in a Dubin container (blue circular container with a clear lid full of grid holes), note the location of the tumour as indicated by radiology on the requisition. Place the pins in the correct grid hole (as far through and as straight as possible). Carefully remove the clear lid (use the little tabs on the side), keeping the pins in place. Ink the specimen and slice in 0.5cm intervals, deep to superficial, lateral to medial, while keeping the slices attached along the superficial surface. Place folded pieces of paper towel between each section to maximize formalin exposure. Place the specimen in formalin. RECORD THE TIME. 4. If the breast is received inked in multiple colours, confirm that the margins agree with the legend on the requisition, and the laterality of the specimen. If the orientation is in question, call the OR (or your staff if you need to) to confirm. Slice in 0.5cm intervals, deep to superficial, lateral to medial, while keeping the slices attached along the superficial surface. Place folded pieces of paper towel between each section to maximize formalin exposure. Place the specimen in formalin. RECORD THE TIME. 5. If the breast is oriented with sutures, confirm the orientation with the laterality on the requisition. If the orientation is in question, call the OR (or your staff if you need to) to confirm. Slice in 0.5cm intervals, deep to superficial, lateral to medial, while keeping the slices attached along the superficial surface. Place folded pieces of paper towel between each section to maximize formalin exposure. Place the specimen in formalin. RECORD THE TIME. 6. Go home. *If the breast is not inked, then ink it in either green followed by acetic acid, or black ink. Total Mesorectal Excision/TME (you won’t get many of these) 1. Record the time received in Pathology on the requisition 2. Assess for “completeness” A) Complete - bulky mesorectum, smooth surface, no tearing, and no coning. If there are defects they have to be no deeper than 5mm. B) Nearly Complete - moderate bulk of mesorectum, irregular surface, moderate coning, defects deeper than 5mm but no visible muscularis propria. Note: Levator muscles may be seen at their insertion in lower rectum-upper anal canal and this should not be considered a defect. C) Incomplete - little bulk of mesorectum, very irregular surface, defects down to muscularis propria, moderate to marked coning. 3. Ink the resection margins – they aren’t covered with a nice, shiny peritoneum. They look ragged and bare (see below) **If the specimen is incomplete, call your staff person. It’s also helpful to take a picture of the specimen.** Anterior Posterior 4. Check the requisition or Oacis for the location of the tumour. Open the specimen anteriorly from proximal to distal, then place wet paper towel loosely on the mucosal surface. If the tumour is located on the anterior surface, open to within 1 cm of the tumour and place wet paper towel in the lumen. Put the specimen in a bucket with formalin. 5. Go home. Lungs 1. ALWAYS check the requisition/OACIS to see if the lung is infectious (it’s good practice to use an N95 mask for all fresh specimens in case of TB – top shelf, first bench). If infection is suspected but not diagnosed, consider culturing the lesion (you can speak to your friendly neighbourhood microbiologist down the hall or on-call), and WORK IN THE FUME HOOD (in the back room of the gross room). 2. Weigh and measure the specimen uninflated, and record this on the requisition. 3. For a lobectomy/pneumonectomy, remove the bronchial stapled margin carefully, then take the first resection margin just underneath. Place the margin in an unlabelled cassette. Mark this down on the requisition, as well as the time it was done. 4. Inflate the lung with formalin using a large syringe and the metal syringe adapters (these are found in empty formalin bottles, usually on the shelf at the first bench on your right. The gold one is the best). Be sure to inflate the whole lobe by selectively inflating through the different segmental bronchi. 5. If you get a small, stapled wedge resection or a lesion is obstructing the bronchus, use a syringe with a large bore needle (blue stacking containers on shelf at the first bench) and inject the formalin into the lung parenchyma directly. Make sure the entire lung is inflated as much as possible. 6. Place the specimen and cassette (if margins submitted) in a bucket with formalin. 7. Go home. Neuropathology (Frozen Section) 1. These always occur at the Civic 2. During the week, there is a Neuropathologist on-call (either Dr. Woulfe or Dr. Jansen) – they are the staff person you need to speak with when there is a frozen section for neuropathology. You still have to contact the histotechnologist. 3. On weekends or days when no neuropathologist is listed on the schedule, you can try your on-call staff person if they are comfortable with neuropathology specimens. If not, or if the clinician specifically asks for a neuropathologist, contact Dr. Woulfe, Dr. Jansen or Dr. Michaud for assistance (in that order). Autopsy 1. We don’t do autopsies after hours during the week (repeat that) 2. The Forensics Unit handles both the hospital cases and the forensics cases on Saturday. For residents, hospital cases take priority. 3. On holidays, hospital autopsies may need to be done in order to prevent backlog the following week. For example, on Easter Monday, if there is a hospital case, the PAs will page you in the morning (if not, call the forensic morgue). Your regular staff person is responsible for handling the case with you. 4. Biohazard cases (see below) are not to be done on holidays for safety reasons. A) Proven HIV infection. B) Fever of unknown origin. C) Hepatitis of unknown origin, Hepatitis A, B and C. D) Dementia of unknown origin or suspected slow virus disease (e.g. Creutzfeldt-Jacob Disease) E) Tuberculosis, active form. Random Calls We don’t do autopsies in the middle of the night. We will be happy to perform an autopsy during regular working hours or on Saturdays. We do not transport bodies in our cars (the funeral home does this – yes, I’ve been asked to do this) If you get called about transporting a body around the hospital, refer them to Security If you get called about a Forensic case, don’t ask questions – tell them to call the Forensic Pathologist on-call. Formalin bottles can be obtained in the ORs You can put a rush on a case in PowerPath the next morning (General tab, lower right corner, Priority pull-down tab). Usually the clinician will give you a reason, if not – ASK. If it isn’t anything urgent, politely explain that RUSHing a case is not appropriate (i.e. “The patient is acutely deteriorating and we need a diagnosis” vs. “I just want to know what this is, looks cool”) Always verify proper labelling of a specimen. If a specimen is mislabelled, call the clinician to fix it. The Weird and Wonderful These are cases that will rarely, if ever, be encountered. Diagnostic Right Ventricle 1. Go to the Heart Institute catherization lab (basement level) and ask the nice lady at the front desk for the specimen. 2. Bring the specimen to the gross room at the Civic 3. Examine the specimen: - if there are 3 or less pieces, place all in formalin - if there are 4 pieces, cut one piece in half and place in gluteraldehyde (black-topped vial) for EM, place the rest in formalin - if there are 5 pieces, cut one piece in half and place one half in gluteraldehyde and the other half should be submitted for freezing (the histotechnologist must be called for this) - if there are more than 5 pieces, you have plenty to submit for both EM and freezing - Document all on the requisition form, as well as the time 4. Leave the specimen in the gross room for the PAs the next morning. 5. Go home. *Gluteraldehyde can be obtained in the morgue, the fridge in the back room of the gross room, or the histotechnologist can give you some from the frozen section room. Fetus/Placenta If you have any doubts, place the fetus in the fridge and inform your staff person the next day – this is your safest option. If the fetus is less than 500 grams or 20 weeks gestation, it will be treated as a regular surgical specimen. A filled-out CON 20 form should accompany the specimen. Make sure the disposal method (Hospital or Funeral Home) section has been filled out. If there are any discrepancies, call the floor. A stillbirth is a fetus greater than 500 grams or equal to or greater than 20 weeks gestation. If an autopsy is requested, an autopsy consent form must be filled out. If a fetus/baby needs to be transported or released, the people to call are security and medical records. Medical records should be able to tell you if the body can be released. DO NOT transport the body to CHEO yourself if asked; call security and they’ll do it. For regular body transport to a funeral home, it works like a regular autopsy: medical records gets the OK and then the funeral directors pick up the body. Heart Valves 1. 2. 3. 4. 5. 6. 7. 8. 9. Dr. Veinot already knows about it, don’t call him Pick up the specimen at the Cardiac Operating Room Ensure it has been delivered in STERILE SALINE Turn on the UV light in the fume hood for 10 minutes to sterilize before handling the specimen Call Microbiology and ask if they want/already have a sample for culture Take a picture Under sterile conditions (in the flow hood, the sterile utensils are in the cabinets under the fumehood on the left side), open the sterile jar, take a small bit of thrombus/vegetation and place in the sterile jar, carefully add the infected saline. The rest can be placed in formalin and treated as a surgical specimen. All valves that are not infected should be placed in formalin Go home. Department-Wide Fan-Out Procedure – this happens once every 5 years or so, and I hope it never happens to you. If so, you will be paged by the hospital and told to “initiate the department-wide fan-out procedure, please refer to your fan-out procedure manual”. This is a safety procedure in case of a disaster; each department is required to reach certain contact people within their department to advise them of the procedure in a phone-tree fashion. You are responsible for immediately contacting each person (or their alternate) and saying “I’m initiating the departmentwide fan-out procedure”. You also need to record the time each person was contacted. If you get a busy signal, try the alternate. You have to keep trying until you reach one of them. It’s a miserable job. The list is kept hidden somewhere….I just called Dr. Burns and he gave me the numbers.