SSAT Exchange Placement 2012: Buenos Aires, Argentina
advertisement

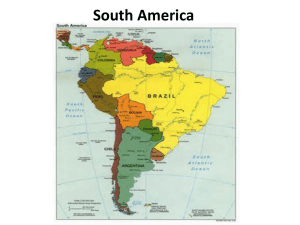
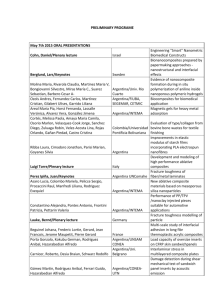
SSAT Exchange Placement 2012: Buenos Aires, Argentina Dr Padmasayee Papineni, SpR Infectious Diseases/GUM I had the opportunity to take part in a two-week clinical exchange placement funded by St Stephens’ AIDS Trust at Helios Salud, San Telmo, Buenos Aires, Argentina in March 2012, under the supervision of Dr Isabel Cassetti. Argentina is a country located in South America with a total population of around 40 million, with 92% of the population living in urban areas. The life expectancy is 76 years and the gross domestic product per capita is US $8500. The prevalence of HIV for the country is 5 per 1000 adults aged 15-49 years (compared with a global average of 8 per 1000 adults). Estimates of epidemiological data from 2009 indicate that the number of people living with HIV is 110,000 [range 88,000 140,000], with women aged 15 and over accounting for 36,000. The number of annual AIDS deaths is 2,860 and the number of new HIV infections per year is 7,488. Helios Salud has the largest HIV cohort in Argentina, with approximately 4000 patients. It is 70% government funded, and the rest paid through the health maintenance organisation or insurance of the patient. The clinic provides many services, including a dentist, gynaecologist, psychiatrist, and dieticians as well as a day hospital where patients can receive intra-venous therapies. The clinic also runs a number of clinical trials. The majority of patients are heterosexual (70%). A few patients are children and adolescents who acquired HIV through vertical transmission. 25% of the patients are co-infected with hepatitis C and 6% with hepatitis B (seropositivity for hepatitis B is 38%). Overall adherence to antiretroviral therapy is about 90%. The majority of the patients I saw in consultations were clinically asymptomatic. The clinical dilemmas faced by the clinicians included many of the ones we face at Chelsea and Westminster Hospital, with management of chronic health conditions, including diabetes, dyslipidaemia, and alcohol excess. This extended role of the HIV physician as the general practitioner of the patient is seen both in our unit in London and Helios Salud. In addition, management of drug interactions and side effects associated with anti-retroviral therapy including lipodystrophy and rash was important. I noted that patients were more willing to disclose their status to their family, and involve their partners and family in their HIV care compared with our patients in the UK. I visited Laoratorio FUNCEI, where Marina Gutierrez, the biomedical scientist in virology, explained to me that the lab is the largest private lab in Argentina, and performs HIV viral loads daily. The set-up was similar to virology laboratories in UK hospitals, with the same techniques used such as Taqman. All the tests are done in-house, and the services provided included integrase resistance testing and testing for HLA B5701 for abacavir hypersensitivity. I also had the opportunity to visit Hospital Muñiz, a public hospital that has a history steeped in infectious diseases, having faced major epidemics that have affected Argentina over time, including yellow fever, dengue, measles and hantavirus. I spent time with Dr Tomas Orduna, consultant in tropical medicine and his team. The buildings and surrounding grounds of the hospital are beautiful, but it is clear that a lack of government funding has led to poor maintenance. The hospital acts as a referral centre for the whole of Argentina, as it specialises in tropical medicine. The hospital has 300 in-patient beds and also sees a large number of tuberculosis patients in the out-patient department. The wards are mainly open bays (see photograph above), which accounts for a lack of privacy and poses infection risks. Many of the patients are immigrant workers from Bolivia and Paraguay. The case mix of medical conditions was very varied, including aspergilloma post tuberculosis, ocular herpes zoster, adrenal insufficiency (with the differential diagnoses for the cause being tuberculosis, parcoccoidodomycosis, or histoplasmosis), muco-cutaneous leishmaniasis, and lung fibrosis secondary to paracoccidomycosis. The patients with HIV had advanced disease with very low CD4 counts and wasting syndrome. Patient consent obtained As the hospital acts as a tertiary centre, patients who live in the Northern provinces of Argentina where mucocutaneous leishmanisasis is endemic would travel to the hospital for diagnosis and treatment. The photograph above is a lesion on the arm of a twenty-year old farmer who lived near Salta, who attended for biopsy. To gain insight by making a comparison to a private hospital, I also visited Centro Medico CEMIC under the supervision of Dr Pablo Bonvehi, Consultant in Infectious Diseases. I joined the resident Dra. Fernanda on her ward round. The patient mix was similar to hospital-acquired infectious diseases in the UK, with caring for patients with endocarditis, device infections, post-operative infections, bone and joint infections and patients post bone marrow transplantation. It was inspiring to witness how closely all the hospital teams worked and communicated with each other. I not only learnt a lot about HIV and infectious diseases care in Argentina, but also appreciated the opportunity to experience the culture and warmth of the people, and I would like to thank all those involved in giving me this experience and also recommend it to others. Dr Padmasayee Papineni References: http://www.unaids.org/en/regionscountries/countries/argentina/ Accessed 29/3/12. http://www.who.int/gho/countries/arg.pdf Accessed 27/3/12.