WPW 1998 - UCSF Department of Anesthesia and Perioperative Care
advertisement

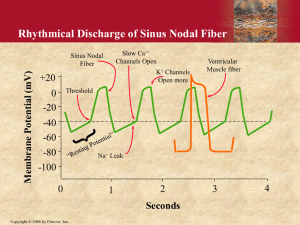
Wolff-Parkinson-White Syndrome William A. Shapiro, M.D. UCSF Department of Anesthesia September 24, 2005 E-mail: ShapiroB@anesthesia.ucsf.edu Wolff-Parkinson-White (WPW) syndrome is the most common electrocardiographic (ECG) abnormality of pre-excitation and, it is associated with very specific, clearly identifiable arrhythmias. My goal is to assist with the anesthetic management of patients with WPW by helping you decide whether or not the cardiac rhythm seen at any time during surgery is a routine part of anesthesia, or is one of the arrhythmias known to occur in patients with WPW. I will provide a formula for rapid interpretation of the tachycardias associated with WPW so that effective therapy, when indicated, can be chosen first. A glossary of frequently used terms is provided immediately preceding the bibliography. Bold and underlined sentences are designed to help with important points. In 1930, Wolff, Parkinson and White1 described a series of patients in whom the resting surface electrocardiogram (ECG) showed a short P-R interval. All these patients experienced paroxysmal bouts of tachycardia. The explanation for both the ECG findings in sinus rhythm and the arrhythmias seen in WPW was first proposed by Wolferth2 in 1933 and later confirmed histologically.3 This abnormality of cardiac conduction consists of an electrically conductive tissue bridge which connects the atrium to the ventricle and allows impulses originating in the sinus node to bypass the normal pathway through the AV node and produce ventricular activation over the alternate pathway. Normally, the cardiac impulse originates in the sinus node and is conducted via internodal pathways to, then through, the AV node (AVN), down the His Purkinje system, ultimately causing activation of the ventricular myocardium, first at the apex, resulting in cardiac contraction which propels blood from the apex of the heart toward the base and out through the aortic and pulmonic valves. Each sinus impulse is conducted down through the AV node and cannot return to reactivate the atria (through sites other than the AV node) because of the fibrous annulus, nonconductive tissue separating atria from ventricle at all points except the AV node. In addition, the impulse also cannot return via the AV node to reactivate the atria because, normally, the retrograde AV node refractory period exceeds the retrograde impulse conduction time (see glossary). In this way, the normal heart protects itself from reentrant arrhythmias either through the AV node or directly from any part of the ventricular muscle back into the atria. Definition of Pre excitation: Pre excitation exists when in relation to atrial events, all or part of the ventricular muscle is activated by the atrial impulse sooner than would be expected if the impulse reached the ventricles only by way of the normal A-V conduction system. Wolff-Parkinson-White Syndrome The clinical significance of the pre-excitation syndrome is related to: 1. The high frequency of arrhythmias with which they are associated. 2. The bizarre ECG patterns which make additional ECG analysis impossible. 3. The cardiac anomalies with which they may be associated. As described earlier, in WPW there is an electrically conductive, histologically distinct tissue bridge connecting atrial muscle directly to ventricular myocardium. This anomolous pathway, often referred to as a bypass tract (BT) is located apart from the AV node and allows impulses originating in the sinus node to activate the ventricle by bypassing the AV node. The clinical importance of this tissue bridge is that there are now two pathways (the AVN and the BT) for electrical impulses to travel from atria to ventricle and vice versa. Because both the AVN and the BT can conduct impulses in either direction, circus movement (reentrant) tachycardias are now possible. A multitude of other accessory bypass pathways are theoretically possible. The socalled Mahaim fibers are His-ventricular bypass tracts while the Lown-Ganong-Levine (LGL) syndrome is associated with atrio-His fibers which bypass the AV node. The ECG characteristics of each pre excitation syndrome is predicted by the location of the bypass tract. Since Mahaim fibers take off after the cardiac impulse has passed through the AV node, the PR interval will have a normal contour and duration. The wide QRS complex associated with Mahaim bypass tracts is a result of early ventricular activation which occurs because the cardiac impulse activates the ventricle prematurely; that is, before it would ordinarily pass down the right and left bundle branches over the normal pathway. Since LGL fibers bypass the AV node, and insert directly into the His bundle, the ECG pattern associated with this syndrome shows a short P-R interval and a narrow QRS complex. In 1975 a nomenclature4 was proposed to explain and predict virtually any theoretical possibility of ventricular pre excitation. For purposes of explaining how pre-excitation syndromes lead to arrhythmias, I will discuss the genesis and treatment of arrhythmias associated with the WPW syndrome. The 12 Lead Surface ECG Pattern in Patients with WPW In patients with WPW, the sinus node impulse reaches the AVN and the BT at approximately the same time. The result of its passage through both structures produces a 12 lead ECG which typically shows a short P-R interval (less than .12 sec), a slurred initial QRS upstroke(delta wave) and a wide QRS complex (greater than .12 sec). When the BT conducts impulses in only the retrograde direction, it is referred to as a concealed BT, and is only “uncovered” during reentrant tachycardias since theses patients with a concealed BT will not have a delta wave during sinus rhythm. The incidence of premature atrial contractions (PAC’s) is higher in people with WPW. The reason for the higher incidence of PAC’s is unknown, however PAC’s are important in the genesis of arrhythmias in this patient population. 2 Wolff-Parkinson-White Syndrome Prevalence, Natural History, and Associated Cardiac Abnormalities Looking at ECG's alone, the reported incidence of classic WPW ranges from .1 to 3.1 per 5 1000 . In children, the prevalence rates quoted in the literature ranges between .4 and 5 per 1000. The quality of life and life expectancy of children discovered to have ECG evidence of WPW, but who do not experience arrhythmias, appears to be normal. Some children discovered to have arrhythmias associated with WPW find that their symptoms decrease as they grow older. Others still, appear to “outgrow” their arrhythmias altogether. 6 Studies in adults show a decreasing number of people with ECG evidence of WPW with increasing age. This does not imply that sudden death is associated with WPW, since, as with some children with WPW, adults too can “outgrow” this entity. WPW is occasionally associated with structural heart disease and when it is, the incidence of both symptomatic arrhythmias (morbidity) and sudden death (mortality) is higher. The cardiac structural abnormality most often associated with WPW is Ebstein's anomaly (abnormal morphogenesis of the tricuspid valve). This is most frequently associated with WPW bypass tracts located between the right atria and ventricle. Left sided bypass tracts are only rarely associated with mitral valve abnormalities. THE TWO TACHYCARDIAS ASSOCIATED WITH WPW7 Introduction The electrical properties of conduction velocity and the refractory period will be different over the AVN and the BT. One important difference in conduction properties between the bypass tract (BT) and the AV node is that as the frequency of impulses bombarding the BT is increased, the ability to conduct those impulses through the BT is also increased. Conversely, as the frequency of impulses hitting the AV node is increased, there is an upper limit (usually around 180 beats/minute) of the number of impulses that can be conducted through the AV node per minute. It is this electrical property of AV nodal tissue which normally prevents atrial fibrillation from achieving dangerously rapid ventricular rates. Therefore, as the sinus rate increases in a patient with WPW, the short PR interval, and slurred QRS upstroke(delta wave) become more prominent. While the majority of people with ECG evidence of WPW will not have structural heart disease, 40 - 80% will experience an arrhythmia. There are two types of arrhythmias associated with WPW. 1. Narrow complex Supraventricular Tachycardia (SVT) The most common arrhythmia associated with WPW is a regular tachycardia (120-220 beats/min) with a narrow QRS complex. This arrhythmia is usually infrequent, short in duration when it occurs, and sometimes without symptoms, particularly in infants and 3 Wolff-Parkinson-White Syndrome children. Studies in adults reveal that when the rate of SVT exceeds 180 bpm, about 50% of those affected have symptoms of chest pain, congestive heart failure (manifested by SOB and/or pulmonary edema), or syncope. Initiation of this narrow complex SVT usually begins with a PAC. Because of the electrical properties of the BT, the PAC is blocked in the BT. However, because of different conduction and refractory properties of the AV node, the premature beat finds the AV node capable of conduction. Therefore, the PAC, which was just blocked in the BT, is now conducted to the ventricles through the AV node. Since this beat (produced by the PAC) is conducted down the AV node, it will have a narrow QRS complex. This beat, which has activated the ventricles via the AV node, now finds it possible to return to the atria via retrograde conduction over the BT. Perpetuation of this circus movement (reentry) will produce a sustained tachycardia. If the onset of this arrhythmia is captured and recorded on the ECG, the following characteristics would be seen: A. Sinus rhythm with a narrow PR interval and a delta wave, then... B. A premature atrial contraction (PAC) followed by a long PR interval. C. The PAC beat now proceeds through the AVN producing a narrow QRS complex (without a Delta wave). D. The narrow QRS complex is closely followed by a P wave which is inverted in leads in which the P wave was upright during sinus rhythm. The atria, AV node, ventricle, and the ABT are all necessary elements in this reentrant loop. 2. Irregularly irregular wide complex tachycardia The other arrhythmia encountered in WPW is atrial fibrillation with conduction to the ventricle over the BT resulting in a wide QRS complex in almost every beat. In patients with WPW, it is this abnormal rhythm (atrial fibrillation) which is most potentially life threatening, since ventricular rates up to 300 or more beats/min can occur with atrial fibrillation. In fact, in any patient who is having what appears to be an irregularly irregular ventricular tachycardia at rates of > 220 beats/min, the diagnosis of WPW with conduction over the ABT should be strongly suspected. This occurs because of the fundamental difference in conduction properties between the BT and the AV node. As the frequency of impulses bombarding the BT is increased, the ability to conduct those impulses is also increased. This creates the potential for very rapid ventricular rates, making this form of atrial fibrillation so very dangerous. In summary, there are two distinct tachycardias associated with WPW. One is a regular narrow QRS complex tachycardia. The second is an irregularly irregular wide QRS complex tachycardia (atrial fibrillation). Both use the bypass tract for their perpetuation, while only the narrow QRS complex regular tachycardia is a reentrant arrhythmia. PAC’s usually initiate the onset of either arrhythmia. 4 Wolff-Parkinson-White Syndrome 5 ANESTHETIC MANAGEMENT There are no cookbook recipes. Electrophysiologic information about WPW and the associated arrhythmias has been well known in cardiology, but slow to appear in the anesthesia literature. In 19688 and 19789, case reports of one case each lead to generalized speculation about which anesthetic agents might be contraindicated. In 197910, anesthesia for surgical interruption of the BT in 13 symptomatic patients again focused on the anesthetic techniques, without offering suggestions based on the patient’s arrhythmia history, or the effects of anesthetic agents on the electrical properties of the BT and the AV node. By 1989, the emphasis changed when Lubarsky11 reported on 2 patients with WPW and discussed the specific arrhythmias and their treatment. More recent publications by Chang12,13 and Sharpe14,15 offer information on the effects of anesthetic agents on the electrical properties of AVN and BT conduction. Preoperative Assessment History -- Patients who do not experience arrhythmias preoperatively appear not to be at increased risk to have their first arrhythmia during anesthesia and surgery. If a patient with a baseline 12 lead ECG showing WPW experiences arrhythmias preoperatively, it is important to ascertain which one. Is it the regular, narrow QRS complex type, or is it the irregularly irregular wide QRS complex form. Once it is established that the patient experiences arrhythmias, one should identify inciting events, such caffeine or exercise, and also define the treatment known to terminate them. Obviously, triggering agents are best avoided preoperatively whenever possible and perhaps sedatives prescribed for some patients. While most arrhythmias are short and non sustained, some patients will have been taught carotid sinus massage or other vagal maneuvers to terminate their arrhythmias. Others may have implanted pacemakers which they activate themselves to terminate undesirable arrhythmias. If so, the patient can demonstrate how to activate these devices should that be necessary during anesthesia and surgery. Since WPW may be associated with structural cardiac abnormalities, questions related to exercise tolerance can help quantify cardiac reserve, or reveal cardiac limitation if the exist. Physical exam -- This should emphasize valvular problems. Murmurs do not normally exist in WPW unless they are associated with valvular abnormalities. Such valvular abnormalities should be searched for, identified, or their suspected presence eliminated. Chronic Antiarrhythmic Medication--In patients with WPW having non cardiac surgery, antiarrhythmic therapy shown to be effective preoperatively, should be continued up to and including the day of surgery. Wolff-Parkinson-White Syndrome 6 INTRAOPERATIVE MANAGEMENT Patients with WPW, but without structural heart disease or exercise limitation, need only be evaluated with standard monitors during surgery. Invasive monitoring or TEE should be reserved for patients with depressed LV function, or for surgery when these monitors are typically used. The most common clinical question during surgery will relate to the cardiac rhythm and whether or not it is sinus tachycardia or one of the arrhythmias known to be associated with WPW. TREATMENT OF INTRAOPERATIVE ARRHYTHMIAS IN PATIENTS WITH WPW Narrow Complex Regular Rhythm Since this tachycardia is a reentrant arrhythmia which involves the atrium, AV node, ventricle and the accessory bypass tract, it could theoretically be attacked pharmacologically at any of these sites. Practically speaking, the largest treatment experience is involves drugs and/or maneuvers that effect the AV node. Carotid sinus massage (CSM), or other vagal maneuvers can be tried first. Drugs that affect the AV node by slowing conduction through can be effective if vagal maneuvers fail. Adenosine is the drug of first choice. Neosynephrine, which both raises blood pressure and often produces a reflex vagal effect on the AV node can, at least theoretically, be a good choice. Verapamil and beta blockers are faster acting than digitalis, all of which have been quite successful in terminating this arrhythmia and restoring sinus rhythm. If pharmacologic therapy fails, or makes the blood pressure worse, cardioversion will always work. Irregularly Irregular Wide Complex Rhythm (Atrial Fibrillation) Since all (or almost all) of the impulses produced by atrial fibrillation are being conducted down the bypass tract to activate the ventricle, drugs which predominantly affect conduction over this muscle bridge are the treatment of choice. While lidocaine may rarely slow conduction over the BT, procainamide or quinidine work best. These agents work by slowing conduction and prolonging refractoriness through the bypass tract thus decreasing the ventricular rate. Defibrillation is often necessary to restore sinus rhythm. Procainamide or quinidine can also be used to suppress PAC's so that sinus rhythm is not soon followed by a PAC which initiates another bout of symptomatic atrial fibrillation. Pharmacologic agents which slow conduction through the AV node are contraindicated during atrial fibrillation because these drugs will preferentially increase conduction over the ABT resulting in faster ventricular rates. Wolff-Parkinson-White Syndrome 7 HOW TO DISTINGUISH SINUS TACHYCARDIA FROM THE ARRHYTHMIAS ASSOCIATED WITH WPW During anesthesia and surgery there may be times when sinus tachycardia is the expected result of either anesthetic or surgical manipulation or the effect of a pharmacologic agent administered to the patient. Quick and easy determination of the type of tachycardia in this patient population is necessary to determine whether or not, for instance, to deepen the anesthesia or begin therapy to terminate an unwanted tachycardia. Measurement of the blood pressure during any tachycardia will often direct immediate attention to treatment even before the underlying mechanism of the tachycardia is identified. A simple method to determine the type of tachycardia in any patient with WPW is outlined in table 1. Once the arrhythmia is identified, treatment can then be chosen accordingly. Remember, sinus rhythm in patients with WPW has a delta wave, and, the faster the sinus rate, the larger the delta wave. Therefore, sinus tachycardia in patients with WPW is a regular tachycardia in which a delta wave and a widened QRS complex is associated with each beat. The faster the sinus rate, the larger the delta wave. And like any other sinus tachycardia, this one too has a gradual onset; that is, the onset is not abrupt. They "warm up" and "slow down" over time. Both supraventricular tachycardias associated with WPW most often have an abrupt onset since generally (though not always) they are initiated by an atrial premature beat. As described earlier, one tachycardia has a regular narrow QRS complex in a patient who moments earlier exhibited a delta wave with every beat. The other tachycardia is rapid and irregularly irregular and has a widened QRS complex associated with every beat. TABLE 1 Sinus Tachycardia Narrow Complex SVT Atrial Fibrillation ONSET DELTA WAVE QRS COMPLEX REGULAR Gradual Sudden Sudden Yes No Yes Wide Narrow Wide Yes Yes No Treatment Blood pressure determination should guide initial therapy. If the blood pressure is inadequate, cardioversion or defibrillation is the treatment of choice regardless of the arrhythmia present. Sinus tachycardia, as it so often occurs in the operating room, is treated as in any other patient. Deepening the anesthesia, usually by increasing the concentration of an inhalation agent or administering narcotics, will decrease the heart rate. As always, whenever it is determined that slowing the sinus rate is indicated, beta blocking agents are the preferred treatment. Narrow complex SVT or atrial fibrillation treatment has been outlined above. Wolff-Parkinson-White Syndrome Summary: 8 Pre excitation abnormalities of cardiac conduction produce conditions which make possible the initiation of certain arrhythmias. WPW is the most common of the pre excitation syndromes. These syndromes may occasionally be associated with structural heart disease and varying degrees of pump failure. Preoperative management of these patients should include continuation of successful antiarrhythmic therapy. Intraoperative management of tachycardias depends on the specific arrhythmia present. Hemodynamic compromise whenever caused by an arrhythmia (reentrant or otherwise) should be treated with cardioversion or defibrillation. The pharmacologic agent or maneuver chosen to treat an arrhythmia should be determined after analyzing the ECG, paying particular attention to the rhythm (regular or irregular), the QRS duration (narrow or wide), and the temporal relationship of the P wave to the QRS complex. Recent electrophysiologic information suggests that some of our commonly used anesthetic agents effect the electrical properties of conduction and refractoriness in some parts of the heart. While these effects are important for evaluation of these structures by cardiologists, these effects do not appear to promote arrhythmias during surgery. To date, no anesthetic agent or anesthetic technique has been shown better or worse than any other in patients with WPW. GLOSSARY Normal Sinus Rhythm -- Normal sinus rhythm results from the initiation of an electrical signal (the cardiac impulse) by cells of the sinus node at a rate appropriate to the age and state of activity of the individual, and then the propagation of that signal in an orderly manner through the atria, A-V junction, ventricular specialized conducting system and the ventricular myocardium. Arrhythmia-- An arrhythmia reflects either abnormally rapid or slow impulse initiation by the sinus node, or interruption of the sinus rhythm by impulses originating from some other site in the heart, either for short of long periods of time. Pre excitation -- Pre excitation exists when, in relation to atrial events, all or part of the ventricular muscle is activated by the atrial impulse sooner than would be expected if the impulse reached the ventricles only by way of the normal A-V conduction system. Reentry -- A reentrant rhythm uses the substrate of cardiac tissue electrophysiologic inhomogeneity to produce and sustain an arrhythmia. Three fundamental conditions are required for the initiation and maintenance of a reentrant arrhythmia. 1. At least two functional distinct pathways that are joined proximally and distally to form a closed circuit of conductive pathways. 2. Unidirectional block in one pathway. Wolff-Parkinson-White Syndrome 9 3. Slowed conduction down the unblocked pathway allowing time to recover retrograde excitability in the blocked pathway. Refractoriness -- The response of a tissue to the introduction of premature stimuli. 1. Effective refractory period of cardiac tissue is the longest coupling interval between the basic drive and the premature impulse that fails to propagate through that tissue. 2. Relative refractory period is the longest coupling interval between the basic drive and the premature impulse that results in prolonged conduction of the premature impulse relative to that of the basic drive. REFERENCES 1. Wolff L, Parkinson J, White PD: Bundle branch block with a short P-R interval in healthy young people prone to paroxysmal tachycardia. American Heart Journal 5:685-, 1930 2. Wolferth CC, Wood FC: The mechanism of production of short P-R intervals and prolonged QRS complexes in patients with presumably undamaged hearts: Hypothesis of an accessory pathway of auriculoventricular conduction (bundle of Kent). The American Heart Journal 8(3):297-312, 1933 3. Becker AE, Anderson RH, Path MRC, Durrer D, Wellens HJJ: The Anatomic substrates of WolffParkinson-White syndrome: A clinicopathologic correlation in seven patients. Circulation 57(5):870879, 1978 4. Anderson RH, Becker AE, Brechenmacher C, Davies MJ, Rossi L: Ventricular pre-excitation. A proposed nomenclature for its substrates. European Journal of Cardiology 3:27-36, 1975 5. Averill KH, Fosmoe RJ, Lamb LE: Electrocardiographic findings in 67,375 asymtomatic subjects. IV. Wolff-Parkinson-White syndrome. The American Journal of Cardiology :108-129, 1960 6. Mantakas ME, McCue CM, Miller WW: Natural history of Wolff-Parkinson-White syndrome discoverd in infancy. The American Journal of Cardiology 41:1097-1103, 1978 7. Gallagher JJ, Svenson RH, Sealy WC, Wallace AG: The Wolff-Parkinson-White syndrome and the preexcitation dysrhythmias. Medical Clinics of North America 60(1):101-123, 1976 8. Hannington-Kiff JG: The Wolff-Parkinson-White syndrome and general anaesthesia. British Journal of Anaesthesia 40:791-795, 1968 9. van der Starre PJA: Wolff-Parkinson-White syndrome during anesthesia. Anesthesiology 48:369-372, 1978 10. Sadowski AR, Moyers JR: Anesthetic management of the Wolff-Parkinson-White syndrome. Anesthesiology 51(6):553-556, 1979 11. Lubarsky D, Kaufman B, Turndorf H: Anesthesia unmasking begign Wolff-Parkinson-White syndrome. Anesthesia and Analgesia 68:172-174, 1989 Wolff-Parkinson-White Syndrome 12. Chang R-KR, Stevenson WG, Wetzel GT, Shannon K, Baum VC, Klitzner TS: Effects of isoflurane on electrophysiologic measurements in children with Wolff-Parkinson-White syndrome. PACE , 1995 13. Chang R-KR, Wetzel GT, Shannon K, Stevenson WG, Baum VC, Klitzner TS: Age- and anesthesiarelated changes in accessory pathway conduction in children with Wolff-Parkinson-White syndrome. The American Journal of Cardiology 76:1074-1076, 1995 14. Sharpe MD, Dobkowski WB, Murkin JM, Klein G, Guiaudon G, Yee R: The electrophysiologic efects of volatile anesthetics and sufentanil on the normal atrioventricular conduction system and accessory pathways in Wolff-Parkinson-White syndrome. Anesthesiology 80:63-70, 1994 15. Sharpe MD, Dobkowski WB, Murkin JM, Klein G, Yee R: Propofol has no direct effect on sinoatrial node function or on normal atrioventricular and accessory pathway conduction in Wolff-ParkinsonWhite syndrome during alfentanil/midazolam anesthesia. Anesthesiology 82:888-895, 1995 10