Hemiparesis/Hemiplegia
advertisement

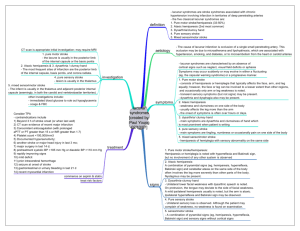
Hemiparesis/Hemiplegia Examination “This man has a left hemiparesis, please examine him” For this, examine the UL and LL Locate o Brainstem Weber’s syndrome (III and contralateral hemiplegia) Millard-Gubler (VI and VII and contralateral hemiplegia; usually a/w contralateral loss of proprioception and light touch as the medial lemniscal damage) o Subcortical – lacunar; a/w UMN VII Pure motor (50%) Pure sensory (5%) Mixed motor and sensory (35%) Ataxic hemiparesis (10%) Dysarthria clumsy hand syndrome (rare) o Cortical signs Do abbreviated version Gaze preference, sensory and visual neglect, hemianopia and dysphasia if dominant lobe involved Causes or risk factors o Pulse, Carotid bruit, murmur o Dyslipidaemia stigmata (xanthelasma, xanthomas, thickened TA) o DM dermopathy o Tar stains o Bruising, telangiectasia Function and complications o Upper limb o Gait o Pressure sores, NG, urinary catheter Request o BP o Urine dipstick o Fundoscopy for papilledema (to rule out SOL which is a possible differential) Presentation Sir, this patient has got a left hemiparesis as evidenced by State the UL and LL findings State the level of the lesion and justify as above Mentioned the causes as above Mention the functional status and complications Questions What are your differential diagnoses? Vascular o Ischaemic (80%) Intracranial thrombosis Extracranial embolism – heart, extracranial arteries, paradoxical Lacunar strokes – small vessel disease from DM or hypt as a result of lipohyalinosis Dissection o Haemorrhagic (Intracerebral, SDH, SAH) Space occupying lesion Infective – abscess, meningoencephalitis Seizures Toxic-metabolic – Hypoglycaemia, HypoNa What are the 4 neuroanatomic stroke syndromes? Anterior cerebral artery - affect frontal lobe function, producing altered mental status, impaired judgment, contralateral lower extremity weakness and hypoesthesia, and gait apraxia. Middle cerebral artery (MCA) - contralateral hemiparesis, contralateral hypoesthesia, ipsilateral hemianopsia (blindness in one half of the visual field), and gaze preference toward the side of the lesion. Agnosia is common, and receptive or expressive aphasia may result if the lesion occurs in the dominant hemisphere. Since the MCA supplies the upper extremity motor strip, weakness of the arm and face is usually worse than that of the lower limb. Posterior cerebral artery occlusions affect vision and thought, producing homonymous hemianopsia, cortical blindness, visual agnosia, altered mental status, and impaired memory. Vertebrobasilar artery occlusions are notoriously difficult to detect because they cause a wide variety of cranial nerve, cerebellar, and brainstem deficits. These include vertigo, nystagmus, diplopia, visual field deficits, dysphagia, dysarthria, facial hypoesthesia, syncope, and ataxia. Loss of pain and temperature sensation occurs on the ipsilateral face and contralateral body. In contrast, anterior strokes produce findings on one side of the body only. How would you investigate? Confirm the diagnosis o Imaging – CT or MRI if posterior stroke (Diffusion-weighted imaging) For diagnosis and type For complications eg hydrocephalus Blood Ix o FBC – polycythemia o Coagulation profile o Biochemical – HypoNa ECG – AF, MI (60% a/w with AF or MI) CXR – Enlarged mediastinum suspicious of a dissection 2D echo (cardioembolic course) Carotid ultrasound scan (significant stenosis - >70%) and transcranial doppler Young patient – young stroke work up (10) o ANA, dsDNA, ESR o Protein C, S o Anti Thrombin III o Factor V leiden or APC resistance o Anticardiolopin IgM/IgG o Homocystine o VDRL What are the limitations of CT brain? Unable to visualise the posterior fossa structures such as the brainstem and the cerebellum Maybe normal up to 6 hours of onset o After 6 hours – hypodense area o Early signs on CT (5) – loss of grey-white differentiation, insular ribbon sign, sulcal asymmetry, hyperdense MCA sign and obscuration of the LN MRI – Diffusion weighted imaging which has a high sensitivity – looked for hyperintense signal How would you manage? Multidisciplinary approach Education and counselling PT/OT and ST – speech and swallowing, caregiver training, prevention of bed sores Medications o Antiplatelets (Aspirin, persantin, Clopidogrel, Ticlid) o Anticoagulation Correct risk factors o Hypertension o Hyperlipidaemia o Diabetes mellitus Surgical o Intracranial bleeds o Hydrocephalus How would you manage the patient acutely? Airway, breathing and circulation Control BP if bleed otherwise allow high BP in ischaemic stroke up to 220/120 Treat fever Control of blood sugar Determine if bleed or ischemic If ischaemic stroke, assess for possibility of reperfusion therapy ie National Institute of Health Stroke Scale (NIHSS) using alteplase ie recombinant tissue plasminogen activator; within 3 hours and important to note inclusion and exclusion criteria. Treat complications o Seizures o Raised intracranial pressure (Hyperventilation, elevate the head, mannitol)