Anterior Communicating Arterial Aneurysm Report
advertisement

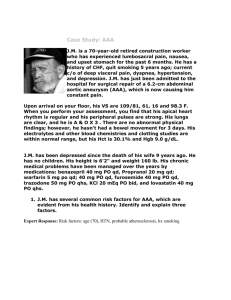
CASE STUDY Anterior Communicating Arterial Aneurysm Stent- Assisted Coil Embolization By Jessica Birt ABSTRACT This case study is about a 67 year old man who came into the ECU and a brain tumor was found. After his tumor resection an incidental cerebral aneurysm was found on a follow-up post resection CT. After a few weeks of monitoring the aneurysm the patient had a stent-assisted coil embolization of the aneurysm, which was very successful. TABLE OF CONTENTS PATIENT HISTORY…………………………………………………………1 PROCEDURES MRI……………………………………………………………………1&5 CT…………………………………………………………………….2&3 ANGIO……………………………………………………………………4&6 PROGNOSIS…………………………………………………………………7 DISCHARG…………………………………………………………………..8 PATIENT HISTORY A 67 year old man with chronic back, leg and feet pain came into the Emergency Care Unit at the VA hospital September 9, 2006. He is on disability for back injury and takes chronic opiate pain medications as an outpatient. He lives with his wife independently in a home in Oregon and the reason for his unscheduled visit to the ECU was due to a progressive worsening memory loss and personality changes. These changes were noticed by his wife and had been insidious in onset. In the months before admittance to the ECU, he was also experiencing constant nausea associated with a bad taste in his mouth and a general unsteadiness of his gait. He denied any specific headaches, focal weakness, or vomiting. The symptoms prompted his visit to the ECU September 9, 2006 and a MRI scan was performed of his head (Medical Records). PROCEDURES MRI- The MRI scan was done with and without contrast media. They used Gadolinium contrast and performed sagittal T1, axial T1, T2, gradient-echo, DWI, coronal FLAIR, and post-Gadolinium axial, coronal, and sagittal T1 scans from the foramen magnum to the vertex. The findings showed a 4.2 x 3 x 2.5 cm partially enhancing mass in the right lateral ventricle, which displaced the septum pellucidum into the left lateral ventricle ( See pictures dated MRI 09-09-06). MRI 09-09-06 PRE-TUMOR RESECTION The heterogeneous enhancement had corresponding signs of hemorrhage on the gradient-echo. There were no signs of hydrocephalus (Report case# 5967). The patient was scheduled for surgery to remove the tumor on October 4, 2006. On October 3, 2006 the patient came back to the hospital for surgery and had another MRI performed which was stereotactic for surgery. He also had a pre-op chest xray done which is routine. October 4, 2006 he underwent an interhemispheric craniotomy and transcallosal resection of his intraventricular tumor (Medical Records). The core biopsy indicated that it was a benign low-grade ependymal neoplasm most consistent with mixed ependymoma/subependymoma (Surgical Pathology). He did have some postoperative issues which showed on the CT that was done the same day after his surgery. CT- The CT of his head was done without contrast using 2mm axial images. It showed that they successfully removed the mass and expected postoperative hemorrhage did occur in the region of the surgical bed. He also had expected postoperative pneumocephalus and a ventriculostomy tube was placed (Report case# 3382). (See Pictures dated CT 10-04-06) The patient was left with attention/memory deficits as well as mild left-sided neglect and urinary incontinence after the surgery. He had to go to rehab after recovery from surgery before he was discharged (Medical Records). October 6, 2006 he had another routine chest x-ray and CT to r/o hydrocephalus. 5 mm axial images were reconstructed through the brain without contrast and were compared to the previous CT scan. There was a decrease in postoperative pneumocephalus. This CT did however, have an incidental finding which was on image 11 case #4317(See CD pictures dated CT 10-06-06). It showed a nodular density slightly anterior to the region of the third ventricle measuring 6 x 3 mm and was of uncertain significance. Close attention to this area on follow-up exams was suggested to evaluate for stability of this finding (Report case# 4317). CT 10-06-06 ANEURYSM CT 10-06-06 VENTRICULOSTOMY TUBE & HEMORRHAGE The next follow-up CT was done on October 8, 2006 using axial 5mm thick images obtained without IV contrast. The round density was seen again on the CT in the location of the anterior cerebral artery representing an aneurysm. After retrospective reviewing the MRI images taken on October 3, 2006, it was clear that it was an artery aneurysm. An arterial aneurysm is an out pouching of an artery. It is a localized widening (dilation) of an artery, vein, or the heart. At the area of the aneurysm there is typically a bulge and the wall is weakened and may rupture (MedicineNet.com). The aneurysm in this patient was a cerebral aneurysm and could potentially burst causing death (Neil- Angio Tech). The findings were discussed with neurosurgery and angiography would be the next step (Report case# 40). Another routine chest x-ray and CT was performed on October 9, 2006. It was just a follow-up and findings were unchanged from previous scan. On October 11, 2006 a CT using 5mm images were taken for status of post-removal of the ventriculostomy drain. Findings were negative for hydrocephalus or any new hemorrhage. The same day he had two more CT’s for follow-ups with and without contrast using non-ionic iodinated media and 1mm helical images. The aneurysm was noted as stable. He also had a routine chest x-ray (Reports case#’s 1832, 1911, 1910, 2743). On the 14th of October he had another routine f/u CT which was compared to the 11th scans. No changes were seen (Report case# 5312). Routine chest x-rays were performed on the 17th and 18th. No unusual findings were noted. On October 20, 2006 another f/u CT was performed with no significant changes (Report case# 6434). ANGIO-Angiography was performed on October 25, 2006 for assessment and evaluation of the arterial aneurysm. Surgical catheterization of the right common femoral artery was accessed using a 19-gauge open-needle. A 0.035 Benson guide wire was used along with a 5-French Davis catheter to reach the selective arteries within the neck and head. The findings were as expected; ~ 7mm smoothly marginated anterior communicating artery aneurysm which is rather symmetrically involving the origins of both the left and right A2 anterior cerebral arteries and is not ruptured (Report case #3674+, See Report for full description & pictures dated 10-25-06 Pre coils ). 3D IMAGE OF CEREBRAL ANEURYSM 10-25-06 The patient was admitted to rehab on the 26th with the goal of returning home with his wife. On the first of November the patient was discharged from rehab and was scheduled for a f/u CT on November 14, 2006. This CT was done axial noncontrast scans from the foramen magnum to vertex. Everything looked the same from previous compared exams, and the aneurysm was stable and further assessment through angiography was recommended (Report case# 1608). MRI- Again on the 5th of December, the patient had another MRI for a f/u on the tumor resection and to assess the aneurysm. The MRI sequences were obtained through the brain using sagittal T1, axial T1, axial T2, coronal FLAIR, postcontrast (Gadolinium) axial and coronal T1. The findings indicated a reduction in size of the right lateral ventricular mass status post partial resection. MRI 12-05-06 POST-TUMOR RESECTION (COMPARE TO MRI 09-09-06) The aneurysm was again assessed showing same consistency (Report case# 1834). Angiography was again suggested for treatment of the aneurysm with coils. December 11, 2006 the patient returned to the hospital and was admitted for coiling and embolization of his aneurysm. The reason for this procedure is to keep the aneurysm from growing which could lead to rupture and death. The coils that are put into the aneurysm will block the blood flow to the aneurysm keeping it the same size (Neilangio tech). There are risks involved such as bursting the aneurysm, infection, bleeding, death, which were discussed with the patient during his consent. Regarding the patients prior craniotomy, the doctors asked him how he was doing and the patient stated that he was doing well. He denied any headaches, nausea, vomiting, visual changes, or any focal deficits. According to his wife, he does have continuous problems with short-term memory difficulties and also problems with bed wetting at night. He is able to ambulate with the help of a cane and seems to be increasing his level of activity (Discharge Summary). ANGIO- On the 12th of December the patient was prepped for his coiling and embolization of his aneurysm. The procedure is one that the Portland VA has never been able to perform because the lack of appropriate equipment. Because of some remodeling and upgrades the doctors were able to perform this special procedure at the Portland VA instead of OHSU for the first time in history. The Portland VA hospital is now the only VA center in the country that has a lab that can perform this procedure (Neil-Angio tech). The patient was given a general anesthetic before the procedure began and was pretreated with Plavix and aspirin. The puncture site was sterilized and sterile drapes were placed over the patient. The doctors used a 19-gauge open needle and a 0.035 Benson guidewire to surgically catheterize the right common femoral artery. A 6-French Shuttle sheath was placed over the guidewire into the thoracic aorta also for constant arterial monitoring. Then the placement of a coaxial 6.5 French JB 1 catheter was introduced with a 0.035 Glidewire, and selective catheterization of the left internal carotid artery was performed. Preliminary diagnostic cerebral arteriography in the AP, lateral, magnified views, and with 3D spin angiography was performed. (Reports case #1588+) See Pre-Coil pictures dated 12-12-06. After preliminaries were performed, coaxial placement of an SL-10 microcatheter with a Fast Dasher Guidewire was placed. Selective catheterization began with an ipsilateral A1 arterial segment through the anterior communicating artery aneurysm to the contralateral A2 arterial segment. After that, an over-the-guidewire exchange for a 3mm diameter x 20mm length Neuroform self-expanding stent was positioned across the aneurysm neck from ipsilateral A1 segment, to contralateral A2 arterial segment. Recatheterization of ipsilateral A1 segment, into the anterior communicating artery aneurysm was performed with the SL-10 microcatheter and Transend Guidewire. After everything was in place, the Neuroform stent was deployed across the neck of the aneurysm, which trapped the microcatheter within the aneurysm lumen. Next was the embolization of the aneurysm which took multiple GDC bare platinum coils; a 7mm framing coil followed by numerous Ultrasoft 0.010 coils. These completely filled the aneurysm blocking off blood flow to it. The microcoils were packed generally tight filling the aneurysm full enough to block blood flow, but not enough to burst it. The catheters were removed and follow-up intracranial arteriography in the AP/Lateral, magnified views, and spin 3D angiography was performed showing no evidence of prolapse of the coil into the native parent artery (Report case# 1588+). PROGNOSIS The final pictures showed successful stent-assisted coil embolization of anterior communicating artery aneurysm. The doctor noted that it was an excellent angiographic result without any complications. The right common femoral artery was assessed and closed using a StarClose device. This entire procedure was performed under fluoroscopy and room time was ~2.5 hours. 175 cc nonionic contrast was used to perform the procedure (Report case #+1588) (See report for full description). PRE-COILS 12-12-06 POST-COILS 12-12-06 POST-COILS 12-12-06 (COMPARE TO 3D IMAGE ON 10-25-06) DISCHARGE The patient was transferred to the SICU where he was observed overnight and received anticoagulation therapy for 24 hours after the procedure (Medscape.com). He remained neurologically intact and was discharged to home on 12-13-06 in stable condition. A follow-up angiogram will be performed in six months to access the coils (Discharge summary). Works Cited “Arterial Aneurysm”, Retrieved January 22, 2006 from www.MedicineNet.com. “Coil Embolization”, Retrieved January 22, 2006 from www.Medscape.com Discharge Summary from Portland VA Medical Records from Portland VA Pathology Report from Portland VA Radiologist Reports from Portland VA