Peripheral Arterial Thrombolysis Guidelines
advertisement
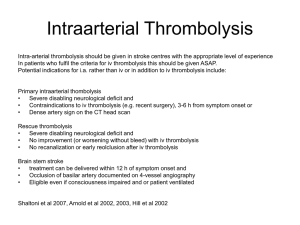
PORTSMOUTH HOSPITALS NHS TRUST NURSING GUIDELINES Peripheral Arterial Thrombolysis Guidelines. Issue 2. 04.01.2010 TITLE Peripheral Arterial Thrombolysis Guidelines Manager / committee responsible DEPARTMENT OF VASCULAR SURGERY, QAH Date issued 04.01.2010 Version 2 Review date December 2010 Equality impact assessment has been applied to this guideline C.M BOWNASS (Vascular Nurse Specialist) Author C.M. BOWNASS (Vascular Nurse Specialist) Ratified by Professional Advisory Committee – September 2007 Amendments record: January 2010: This guideline has had its review date extended from June 2008 to December 2010. No other changes other than issue number and issue date. Contents: 1. Introduction 2. Status 3. Purpose 4. Scope/Audience 5a) Definitions and Indications 5b) Contra-Indications to using alteplase (rt-PA) 6.1 Clinical Practice Guideline 6.2 Process 7. Supporting Evidence 8. Duties and Responsibilities 9. Training: Competency Statement: Peripheral Arterial Thrombolysis Appendices: APPENDIX 1: Information for Patients undergoing Peripheral Arterial Thrombolysis Control Date: 05/02/16 Page 1 of 14 PORTSMOUTH HOSPITALS NHS TRUST NURSING GUIDELINES Peripheral Arterial Thrombolysis Guidelines. Issue 2. 04.01.2010 1. Introduction Guideline for management of peripheral arterial thrombolysis within the Vascular Unit, QAH 2. Status Clinical guideline 3. Purpose The purpose of this guideline is to assist nursing and medical staff, in the use of intra-arterial thrombolysis to obtain safe and effective care for patients. It is not designed to restrict or limit professional judgement and decision-making. This area of practice will be evaluated and the guideline reviewed whenever there is a change in circumstances or annually. 4. Scope/Audience This guideline applies to all PHT staff involved in the administration of arterial thrombolysis 5a) Definitions and Indications ARTERIAL THROMBOLYSIS Insertion of a catheter under x-ray vision and usually via the femoral artery to infuse fibrinolytic agent – e.g. .Alteplase (i.e rt-PA or Actilyse) directly into an arterial clot (thrombus). RECOMBITANT TISSUE TYPE PLASMINOGEN ACTIVATOR ALTEPLASE (RT-PA), rt-PA is a synthetic version of this naturally occurring protein and is potentially fibrin specific, that is, it works only at the site of recent thrombus deposition, rather than having a generalised systemic effect. Other lysis agents include streptokinase, tenecteplase, reteplase but alteplase is currently the only drug in use for arterial thrombolysis in P.H.T. FIBRINOLYSIS (LYSIS) This is the dissolution of a blood clot’s fibrin network; it occurs naturally when proteins released by damaged tissues activate the plasma enzyme PLASMINOGEN into the active plasma enzyme PLASMIN. INDICATIONS FOR INFUSION Arterial occlusion of recent onset involving native artery, by-pass graft or dialysis access fistula. The most suitable lesions for lysis are 10-20 cm in length, are acutely occluded, and have good run-off vessels distally. A common site for lysis is the femoral-popliteal artery. The intra-arterial system is generally comprised of a sheath into e.g. the femoral artery, and a longer arterial catheter inserted via the sheath. Consultation between radiologist and vascular surgeon re appropriateness of procedure and immediate back up from a vascular surgery team is essential because of the potential complications of lysis. Where possible, lysis is started early in the working day and as a planned procedure. 5b) Relative contra-indications to using rt-PA (Senior medical clinician to determine patient’s suitability for peripheral arterial thrombolysis) Ischaemic neurological abnormality/stroke Severe liver disease, including hepatic failure, oesophageal varices and active hepatitis Recent haemoptysis, G.I. bleed, gross haematuria Coagulation defects Control Date: 05/02/16 Page 2 of 14 PORTSMOUTH HOSPITALS NHS TRUST NURSING GUIDELINES Peripheral Arterial Thrombolysis Guidelines. Issue 2. 04.01.2010 Recent surgery/trauma, including dental extractions in past 3 months Severe uncontrolled arterial hypertension Open wounds Recent childbirth Patients receiving oral anti-coagulants e.g. warfarin sodium Neoplasm with increased bleeding risk Bacterial endocarditis These factors increase the risk of haemorrhage. Complications of alteplase (rt –PA) Haemorrhage – can be minor e.g. from around the catheter site (approx 40%) or major e.g. a retroperitoneal haematoma (approx. 9% and requiring blood transfusion 1). Cerebral Vascular Accident CVA – (1-2% risk of intra-cranial haemorrhage) Allergy/anaphylaxis Renal Failure Distal emboli (approx 4 % - these may break off from the dispersing thrombus and shower down the limb causing ischaemic pain. Small clots will be dissolved by the continuation of lysis 1) Reperfusion injury (2% - restoring blood flow to ischaemic tissues may lead to systemic inflammatory response and multi-organ dysfunction 1) Control Date: 05/02/16 Page 3 of 14 PORTSMOUTH HOSPITALS NHS TRUST NURSING GUIDELINES Peripheral Arterial Thrombolysis Guidelines. Issue 2. 04.01.2010 6.1 Clinical Practice Guideline WARD PREPARATION OF PATIENT Action Preparation as for Trans Femoral Angiogram - see check list Ward visit by X-Ray nurse /Ward nurse who has completed Peripheral Arterial Thrombolysis Competency to: meet and assess the patient explain preparation and procedure explain the aftercare answer any questions X-ray nurse to supply check list and any specific instructions – e.g. care of diabetics Ward staff and X-ray nurse to ensure that patient’s details are correct clotting studies (I.N.R. and A.P.T.R.) have been requested, are available and are satisfactory blood has been taken for urea & electrolytes, group and save a consent form has been signed by the patient patient has a wide bore IV cannula When peripheral arterial thrombolysis is performed out of hours or is unplanned, it is essential that ward staff are notified as soon as possible. All peripheral arterial patients should where possible be nursed on E2 (i.e. the vascular ward). E2 ward must assess and address ward and nursing skill mix in order to provide close supervision of the patient and a safe standard of care. Rationale 1, 3, 4, To allay anxiety, assess patient’s ability to tolerate the procedure and provide reassurance To promote patient safety To ensure all relevant clinical information is available, that the patient is medically stable (renal and coagulation function assessed) and the risk of complications is minimised. To ensure that the patient understands the procedure and gives valid consent For I.V. access/analgesia In order that appropriate arrangements are made for equipment and that transfer to the ward is a safe and smooth process This is a high risk procedure and nursing staff should be familiar with protocols and potential complications (many other areas nurse peripheral arterial thrombolysis patients on ITUs or HDUs). PROCEDURE Action Initially as for T.F.A. i.e. explain procedure and table controls (e.g. table movement) explain and give sedation if appropriate insert wide bore peripheral IV cannula, if not already done prepare and drape skin, give local anaesthetic- usually a femoral approach incise skin and insert needle insert guide wire remove needle insert introducer sheath insert arterial catheter through sheath remove guide wire Control Date: 05/02/16 Rationale To reduce anxiety and prepare patient for intensity of procedure and post-procedure care For administration of IV fluids, as required To reduce risk of infection To provide pain relief during procedure Page 4 of 14 PORTSMOUTH HOSPITALS NHS TRUST NURSING GUIDELINES Peripheral Arterial Thrombolysis Guidelines. Issue 2. 04.01.2010 FOR PERIPHERAL ARTERIAL THROMBOLYSIS Action catheter re-positioned until tip is situated proximal to or within thrombus first dose of alteplase (rt-PA) is given in X-ray. Further doses may be given in succession before the patient returns to the ward catheter secured e.g. with suture/opsite light dressing applied Ward staff notified patient is to receive alteplase (rt-PA). 1. Refer to Drug Therapy Guideline) X-ray nurse to prepare Heparinised Saline. (Unless prescribed otherwise, add heparin 5000 units to 500ml sodium chloride 0.9%). Run this through a volumetric infusion pump. A second volumetric pump will also be required for the alteplase (rt-PA) infusion. 2. If sheath in situ, prepare Heparinised Saline (as above), connect to side arm of catheter sheath as marked and set infusion rate (25 ml per hour, unless directed otherwise, refer to Drug Therapy Guidelines). 3. Prepare alteplase (rt-PA) solution as per prescription and prime infusion set and volumetric pump (refer to Drug Therapy Guidelines) Label lines as either “Arterial catheter” or “Sheath” Rationale To achieve optimal results and maximise concentration of alteplase (rt-PA) in thrombus To prevent slippage or accidental pulling of the arterial line To facilitate inspection of the puncture site To prevent delays in commencement of rt-PA and/or possible occlusion of the lines Volumetric pumps improve accuracy of drug administration, i.e. rate, dosage To prevent platelet aggregation/embolus formation along the length of the sheath 3 For easy identification of lines Prior to connection, X-ray nurse should draw back on arterial catheter (via 3-way tap on connecting tube) using a 20 ml syringe. Connect alteplase (rt-PA) line to main arterial catheter, as marked, and set infusion rate (25 ml per hour, unless directed otherwise and depending on body weight); modify according to instructions. Have available 10-20 ml sodium chloride 0.9% in a sterile syringe 4. Ensure patient stays on strict bed rest throughout alteplase (rt-PA) therapy, is nursed flat with only 2 pillows and that there is minimal moving of patient. If arterial catheter tip is positioned in arm artery, elevate arm on pillow; if lower limb use bed cradle If patient has difficulty with passing urine whilst flat, insert a urinary catheter. 5. Cover catheter entry site with a light gauze dressing, but do not seal the dressing down. To ensure line is not blocked and is free of clots. N.B. the arterial catheter may be on the opposite side to the side being treated). Access from the ipsilateral side may be restricted by previous surgery or the site of the occlusion. Control Date: 05/02/16 To flush catheter if line blocks. A sterile syringe is used to minimise risk of introducing infection. To prevent dislodgement of arterial sheath and catheter For comfort and to limit range of movement To reduce necessity for patient to change position. To enable continued inspection of line and early recognition of bleeding. Page 5 of 14 PORTSMOUTH HOSPITALS NHS TRUST NURSING GUIDELINES Peripheral Arterial Thrombolysis Guidelines. Issue 2. 04.01.2010 PATIENT’S TRANSFER TO WARD Action On collecting the patient from Xray, the Ward Nurse & Xray Nurse should check the following: Catheter site Labelling of the Arterial Catheter and Sheath That both Volumetric pumps are working and the drug administered, solution, rate etc All documentation has been completed Any specific instructions noted and then accompanies patient back to the ward. CARE OF THE PATIENT RECEIVING ALTEPLASE rt-PA Action Rationale To ensure safe hand-over of patient to ward staff Rationale 1. Patient nursed in OBSERVATION BAY To allow close observation and monitoring of patient 2. Assess cardio-vascular function by monitoring patient’s Pulse andTo enable deviations (i.e. tachycardia, hypotension, Blood Pressure, Respirations ½ hourly for 4 hours, then hourly if bleeding, allergic reaction or shock) to be stable. Record temperature 4 hourly. established quickly and complications to be treated promptly Complete MEWS score as per protocol Observe arterial catheter insertion site hourly for peri – catheter bleeding, haematoma, line disconnection Monitor patient for abdominal pain, restlessness, back pain. 3. If major bleeding does occur, apply firm, direct pressure to puncture site, discontinue lysis, summon help and treat for shock as necessary. If peri-catheter bleeding occurs, apply light gauze dressing and direct, digital pressure. IF BLEEDING CONTINUES: Contact medical staff Keep patient nil by mouth 4. Monitor patient for other potential bleeding complications, e.g. intra-cranial (causing strokes), renal tract (causing haematuria) and GI Tract (causing oral and/or rectal bleeding). If severe systemic or intra-cranial bleeding occurs, discontinue peripheral arterial thrombolysis and seek urgent medical assistance 5. Check limb/foot hourly as for Trans Femoral Angiogram i.e warmth, colour, movement, swelling, function and evidence of embolic “trash” etc. Bleeding may be visible or concealed causing e.g. retro-peritoneal haematoma, and occur at any time during the period of lysis 1 To control bleeding and prevent formation of haematoma 3. Patient may require surgical intervention to close the puncture site and secure haemostasis Medical staff will assess need to contact Interventional Radiologist Distant haemorrhagic complications may occur due to altered anti-coagulant status 5. Haemorrhage may be due to lysis of pre-existing blood clots acting as “plugs” To assess effectiveness of rt-PA, level of action, worsening of ischaemia or compartment syndrome . Lysis is contra-indicated if there is total limb anaesthaesia, paralysis, swollen or tense muscles Mark foot pulses with skin marker and record presence/absence of pulses. or persistent skin discolouration 3 6. Check infusion pump hourly throughout procedure to ensure pump is running and there is adequate volume of infusion fluid 7. Monitor patient’s pain level (see MEWS chart); ensure adequate analgesia is prescribed and administer as appropriate. Oramorph or IV morphine may be indicated and should be titrated to pain. Control Date: 05/02/16 To ensure infusion runs continuously and there is no back-bleeding Clot lysis may cause distal embolisation and transient pain. Page 6 of 14 PORTSMOUTH HOSPITALS NHS TRUST NURSING GUIDELINES Peripheral Arterial Thrombolysis Guidelines. Issue 2. 04.01.2010 Action 8. Administer I.V. fluids as prescribed and maintain an accurate fluid balance chart Rationale Contrast medium is nephro-toxic, especially in patients with compromised renal function. Monitoring diuresis aids with renal assessment 5 9. If patient scheduled for theatre (e.g. for embolectomy) or outcomeTo of ensure safe pre-operative preparation of patient treatment is uncertain, keep nil by mouth, otherwise patient can eat and drink as desired. 10. If any problems occur, nursing staff should refer to the on call doctor without delay or directly to senior medical staff as necessary To ensure help is sought immediately and from the most appropriate staff 11. At pre-arranged interval (e.g. 12-24 hours) and based on clinical evidence, a repeat angiogram is carried out. To monitor extent of re-perfusion, to advance the arterial line further into the remaining thrombus or as a basis for surgery 3 12. Exercise caution with administering IM Injections during the period of Alteplase (rt –PA) affects clotting mechanism and may peripheral arterial thrombolysis and give only under specific medical cause excessive bleeding after venepuncture etc.4 instruction. If venepuncture or intra-arterial punctures are necessary, then observe the site for potential bleeding. FOLLOWING ALTEPLASE (rt-PA) INFUSION -Switch off alteplase (rt-PA) infusion as directed by medical staff. Replace To prevent platelet aggregation/embolus formation along alteplase (rt-PA) with heparinised saline (see above) at 25ml/hr the length of the arterial catheter 3 N.B. patient may therefore be having heparinised saline - If sheath in situ, continue proximal infusion of heparinised saline via both the sheath and the catheter. - Do not remove arterial catheter until consultation with Radiologist. If patient attends X-ray for repeat angiogram, X-Ray staff may remove arterial catheter but will leave sheath in situ for removal by the ward staff (or as per instructions). Patient may require further lysis, angioplasty or surgical intervention. -Loosen adhesive dressing over arterial line and withdraw catheter as instructed through haemostatic valve on the catheter introducer sheath. Ensure sheath and dressing are still secure So that sheath is not dislodged until lytic effect is reduced. - Do not remove sheath until alteplase rt-PA has been switched off for one hour Half life of alteplase (rt-PA) is about 5 minutes 3 - Check direction of sheath insertion (from notes). Remove stitch / adhesive dressing. So that line is removed and pressure applied in appropriate direction -When removing sheath, apply manual compression for 10 minutes by the clock, but do not obliterate the pulse To achieve effective haemostasis whilst ensuring that the distal circulation is not compromised. -Continue to observe the surrounding tissue for bleeding or bulging and if this occurs apply a further 5 minutes of pressure (more if necessary). -Apply a light pressure dressing Further compression may be needed to ensure bleeding has ceased and to reduce risk of false aneurysm formation. To enable regular inspection of puncture site -Following successful haemostasis- wait at least an hour before commencing heparin therapy -Do not mobilise the patient for 6 hours following removal of the catheter and then follow protocol for care of patient following Trans-femoral arteriogram To reduce risk of reactionary bleeding from puncture site. -Commence IV heparin infusion as indicated To maintain anti-coagulation Control Date: 05/02/16 Page 7 of 14 PORTSMOUTH HOSPITALS NHS TRUST NURSING GUIDELINES Peripheral Arterial Thrombolysis Guidelines. Issue 2. 04.01.2010 6.2) Process Prescription and Dose Administration For preparation and Pharmaceutical Particulars of Alteplase, refer to Drug Therapy Guidelines on PHT Intranet site Infusions will be prepared by: Radiologist/Doctor Registered nurse / practitioner competent in Intravenous (IV) therapy and competent at Level 3 - 4 of Peripheral Arterial Thrombolysis protocol (see Training and Competency Levels) Infusions will be set up by: Radiologist/Doctor Registered nurse / practitioner competent in Intravenous (IV) therapy and competent at Level 3 - 4 of protocol Infusions will be changed by: Radiologist/ Doctor Registered nurse / practitioner competent in Intravenous (IV) therapy and competent at Level 3 - 4 of Peripheral Arterial Thrombolysis protocol Prior to administration of alteplase (rt-PA) the Radiologist will complete the patient’s prescription chart in relation to the bolus dose and the maintenance dose to be administered on the ward. The prescription will include: a) drug and concentration b) rate in ml/hour NB Prescribed settings MUST NOT be altered by ward staff without discussion with the prescribing Radiologist or medical doctor Alteplase may be re-constituted in x-ray for a bolus dose and the remaining solution returned to the ward, for infusion via volumetric pump Acute pain can be a common problem with peripheral thrombolysis. Patients should be boarded for analgesia (e.g. Oramorph) prior to the procedure and its effectiveness titrated against their pain. Peripheral arterial thrombolysis will be stopped when it is clinically safe and appropriate to do so. Equipment 2 volumetric pumps infusion pumps and giving sets Any syringes made up by medical or nursing staff should be discarded every 24 hours. Observations to include Refer to the MEWS observation record chart; in addition * Arterial catheter site ½ hourly – for puncture site bleeding, peri-catheter haematoma, * Limb observations ½ hourly. – for colour, temperature, calf muscle tenderness, function * Dosage information 1 hourly (Recorded from pump) Patient Information A patient information sheet is available (local adaptation of Royal College of Radiologists template). However peripheral arterial thrombolysis is sometimes an emergency procedure with minimal time for discussion about the care and issues involved. See Appendix. Control Date: 05/02/16 Page 8 of 14 PORTSMOUTH HOSPITALS NHS TRUST NURSING GUIDELINES Peripheral Arterial Thrombolysis Guidelines. Issue 2. 04.01.2010 7. Supporting Evidence 1 BEARD J. & GAINES P.2006 Vascular and Endovascular Surgery, Elsevier Saunders, Philadelphia 2 DOUGHERTY Lisa & LISTER Sara (2004) The Royal Marsden Hospital Manual of Clinical Nursing Practice Blackwell Publishing Ltd; Oxford 3 EARNSHAW J. & GREGSON R. 1994 Practical Peripheral Arterial Thrombolysis, Butterworth Heinemann: Oxford 4 KESSEL DO, BERRIDGE DC &ROBERTSON I (2005) Infusion Techniques for peripheral arterial thrombolysis The Cochrane Collaboration, John Wiley 5 SHEILA MURRAY (Ed.) 2001 Vascular Disease, Nursing and Management, Whurr; London 6 WORKING PARTY ON THROMBOLYSIS IN THE MANAGEMENT OF LIMB ISCHAEMIA (2003) Thrombolysis in the management of Lower Limb Peripheral Arterial Occlusion Journal of Vascular and Interventional Radiology 8. Duties and Responsibilities It is the responsibility of all clinical staff involved in the administration of arterial thrombolysis to follow the recommendations of this guideline. It is the responsibility of the Radiologists, Diagnostic Imaging Modern Matron, Vascular Consultants and Vascular Ward Sister to ensure that systems exist to enable staff to receive the training they require. Control Date: 05/02/16 Page 9 of 14 PORTSMOUTH HOSPITALS NHS TRUST NURSING GUIDELINES Peripheral Arterial Thrombolysis Guidelines. Issue 2. 04.01.2010 9. TRAINING COMPETENCY STATEMENT: PERIPHERAL ARTERIAL THROMBOLYSIS Competency indicators 1st level Demonstrates the ability to: 1) Assist a competent practitioner in the care of a patient undergoing peripheral arterial thrombolysis 2) Prepare patient for procedure, using Transfemoral Arteriogram (TFA) Guideline 3)Ensure patient remains on strict bed-rest and close supervision. Assist patient with basic personal care whilst on bed rest ( e.g. hygiene needs, elimination, nutrition) 4) Record vital signs– as per MEWS chart. 5) Recognize and report deviations to a senior nurse 6) Inform senior nurse of alarm signals on volumetric pump Competency indicators 2nd level All of Level 1 plus demonstrates the ability to 1) Assist a competent (level 3) practitioner in the administration of peripheral arterial thrombolysis 2) Explain pre and post- procedure care to patients 3) Describe the applications and complications of peripheral arterial thrombolysis 4) Practise the correct procedures for drug administration a) can counter-check preparation and commencement of arterial infusions b) administer analgesia as prescribed and monitor effectiveness c) completed (PHT) IV drug administration competency to level 2 5) Critically observe the ischaemic limb and monitor changes in colour temperature and presence of pulses 6) Monitor the integrity of the catheter entry site (usually the groin) 7) On removal of arterial line, apply manual compression to puncture site (only under supervision of level 4 practitioner), Control Date: 05/02/16 Competency indicators– 3rd level All of Levels 1 & 2 plus demonstrates the ability to 1) Describe in detail the principles and complications of peripheral arterial thrombolysis 2) Prepare, connect and administer peripheral arterial thrombolysis according to prescription 3) Flush arterial line using safe, sterile technique 4) Assess effectiveness of lysis on patient’s ischaemic limb 5) Recognize and take appropriate action to avoid complications 6) Report to medical staff on progress and concerns re lysis 7) Remove arterial line on completion of lysis 8) Support nursing staff in caring for patients undergoing lysis and assist Level 4 practitioner with teaching and supervision of the protocol Page 10 of 14 Competency indicators – 4th level All of levels 1, 2 & 3 plus demonstrates 1) expert knowledge of the principles and indications for peripheral arterial thrombolysis 2) expert knowledge of the management and safe administration of peripheral arterial thrombolysis 3) provision of education to medical and nursing staff in all aspects of peripheral arterial thrombolysis 4) provision of patient centred information to patients and their carers regarding peripheral arterial thrombolysis PORTSMOUTH HOSPITALS NHS TRUST NURSING GUIDELINES Peripheral Arterial Thrombolysis Guidelines. Issue 2. 04.01.2010 Education/resources to support achievement of the above competencies Ward induction As Level 1, plus As Level 2, plus As Level 3, plus Experience of caring for angiography patients, Observation of angiogram procedure Evidence of reflective practice on management of peripheral arterial thrombolysis Assessment by member of Senior medical staff Trust Medication policy. Peripheral arterial thrombolysis guideline, Resource folder Pharmacy Guidelines on the administration of Alteplase on the PHT intranet site To be assessed by Level 4 competent practitioner Competency maintained through Continuous Professional Development Training/Competency assessment/ and updating in use of volumetric pumps To be assessed by Level 3 or 4 competent practitioner To verify competence please ensure that you have the appropriate level signed as a record of achievement in the boxes below Level 1 Level 2 Level 3 Level 4 Date: Date: Date: Date: Signature of assessor: Signature of assessor: Signature of assessor: Signature of assessor: Print Name: Control Date: 05/02/16 Print Name Print Name Page 11 of 14 Print Name: PORTSMOUTH HOSPITALS NHS TRUST NURSING GUIDELINES Peripheral Arterial Thrombolysis Guidelines. Issue 2. 04.01.2010 APPENDIX 1: Information for Patients undergoing Thrombolysis CRPLG/12 - Last updated 30th June 2000 Introduction This leaflet tells you about the procedure known as Thrombolysis, explains what is involved and what the possible risks are. It is not meant to be a substitute for informed discussion between you and your doctor, but can act as a starting point for such a discussion. If you are having thrombolysis done as a pre-planned procedure, then you should have plenty of time to discuss the situation with your own GP, your consultant and the radiologist who will be doing the thrombolysis. However, it is more likely that you need the thrombolysis as an emergency, in which case there may be less time for discussion, but none the less you should have had sufficient explanation before you sign the consent form. What is Thrombolysis? Thrombolysis means breaking up blood clots. Once a clot starts to form in a blood vessel, it may carry on getting bigger until the whole vessel is blocked. While an operation may be necessary to remove the clot, it is also possible to dissolve the clot by injecting a special "clot busting" drug into the artery, directly into the clot. This can lead to a great improvement in blood flow, and make an operation unnecessary. Why do I need Thrombolysis? Your doctors know that there is a problem with part of your circulation. You are likely to have had an angiogram, a special x-ray examination of the blood vessels, which has shown a blockage in an artery. If nothing is done about the situation, then severe and permanent damage will result, and amputation may be necessary. While the blockage could need treatment with surgery, in your case it has been decided that thrombolysis is the best way of proceeding. Who has made the decision? The doctors in charge of your case, and the radiologist doing the thrombolysis, will have discussed the situation, and feel that this is the best treatment option. However, you will also have the opportunity for your opinion to be considered, and if, after discussion with your doctors, you do not want the procedure carried out, then you can decide against it. Who will be doing the Thrombolysis? A specially trained doctor called a Radiologist. Radiologists have special expertise in using x-ray equipment, and also in interpreting the images produced. They need to look at these images while carrying out the procedure. What are the risks and complications? Thrombolysis is a very safe procedure, but there are some risks and complications that can arise. There may occasionally be a small bruise or haematoma around the site where the needle has been inserted, and this is quite normal. If this becomes a large bruise, then there is the risk of it getting infected, and this would then require treatment with antibiotics. Very rarely, some damage can be caused to the artery by the catheter and this may need to be treated by surgery or another radiological procedure. Clot busting drugs have to be very powerful in order to work, and consequently there is a risk that bleeding will occur elsewhere. For example, if you have a duodenal ulcer, it is possible that this might start bleeding. If this happened, it would be necessary to treat it in the usual way, perhaps with a blood transfusion. However, the risks associated with not treating your blocked artery are felt to be greater than the risks of bleeding elsewhere. Sometimes the blood clot may be so extensive that the clot-busting drug simply cannot dissolve it all away. In these cases, it may be that surgery will be required to relieve the blockage. Despite these possible complications, the procedure is normally very safe, and is carried out with no significant side effects at all. Where will the procedure take place? Control Date: 05/02/16 Page 12 of 14 PORTSMOUTH HOSPITALS NHS TRUST NURSING GUIDELINES Peripheral Arterial Thrombolysis Guidelines. Issue 2. 04.01.2010 Generally in the x-ray department, in a special "screening" room, which is adapted for specialised procedures. How do I prepare for thrombolysis? You need to be an in-patient in the hospital. You will probably be asked not to eat for four hours beforehand, though you may be allowed to drink some water. You may receive a sedative to relieve anxiety. You will be asked to put on a hospital gown. As the procedure is generally carried out using the big artery in the groin, you may be asked to shave this area. If you have any allergies, you must let your doctor know. If you have previously reacted to intravenous contrast medium, the dye used for kidney x-rays and CT scanning, then you must also tell your doctor about this. What actually happens during thrombolysis? The procedure starts off in exactly the same way as an angiogram, and if you have already had this performed, you will know what to expect. You will lie on the x-ray table, generally flat on your back. You need to have a needle put into a vein in your arm, so that the radiologist can give you a sedative or painkillers. Once in place, this needle will not cause any pain. You may also have a monitoring device attached to your chest and finger, and may be given oxygen through small tubes in your nose. The radiologist needs to keep everything as sterile as possible, and may wear a theatre gown and operating gloves. The skin near the puncture site, probably the groin, will be swabbed with antiseptic, and then most of the rest of your body covered with a theatre towel. The skin and deeper tissues over the artery will be anaesthetised with local anaesthetic, and then a needle will be inserted into the artery. Once the radiologist is satisfied that this is correctly positioned, a guide wire is placed through the needle, and into the artery. Then the needle is withdrawn allowing the small plastic tube, or catheter, to be placed over the wire and into the artery. The radiologist will use the x-ray equipment, and small amounts of contrast medium to make sure that the catheter, still on the wire, is moved into the right position, very close to the blockage in the artery. Then the wire will be withdrawn and the clot busting, or thrombolytic, drug injected down the catheter and into the blood clot. The radiologist will check progress by injecting contrast to show how much the clot has dissolved. Although sometimes all the clot is dissolved at the first attempt, generally the catheter has to be left in the artery and attached to an infusion pump, so that injection of the clot busting drug can be continued over the next few hours, or days. Will it hurt? Some discomfort may be felt in the skin and deeper tissues during injection of the local anaesthetic. After this, the procedure should not be painful. The radiologist and other staff looking after you can give you additional painkillers through the needle in your arm, if necessary. You will be awake during the procedure, and able to tell the radiologist if you feel any pain, or become uncomfortable in any other way. As the dye, or contrast medium, passes around your body, you may get a warm feeling, which some people can find a little unpleasant. However, this soon passes off and should not concern you. How long will it take? Every patient's situation is different, and it is not always easy to predict how complex or how straightforward the procedure will be. Sometimes thrombolysis does not take very long, perhaps half an hour. On other occasions the procedure may be more involved, and take rather longer, perhaps over an hour. As a guide, expect to be in the x-ray department for about an hour and a half. What happens afterwards? You will be taken back to your ward on a trolley. Nurses on the ward will carry out routine observations, such as taking your pulse and blood pressure, to make sure that there are no untoward effects. They will also look at the puncture site to make sure there is no bleeding from it. You need to stay in bed for as long as the catheter stays in the artery. Control Date: 05/02/16 Page 13 of 14 PORTSMOUTH HOSPITALS NHS TRUST NURSING GUIDELINES Peripheral Arterial Thrombolysis Guidelines. Issue 2. 04.01.2010 The radiologist needs to check on progress, and will arrange for you to come back to the x-ray department the next day, or the day after. By injecting a small amount of contrast medium, or dye, down the catheter it is possible to tell how much of the clot has dissolved. The radiologist may also use a special balloon, on a different catheter, to try and open up a narrowed artery, and improve blood flow even more. What happens next? This all depends on where the blockage was, and how successful the thrombolysis has been. In many cases, no further procedure is necessary. In some cases the artery may be so narrowed that an operation is required to permanently improve the blood supply. Most patients will be started on Aspirin, or blood thinning drugs, anticoagulants, to improve blood flow in their arteries, and to try and limit the chance of a similar condition occurring again. Finally... Some of your questions should have been answered by this leaflet, but remember this is only a starting point for discussion about your treatment with the doctors looking after you. Do satisfy yourself that you have received enough information about the procedure, before you sign the consent form. Thrombolysis is considered a very safe procedure, designed to improve your medical condition and save you having a larger operation. There are some slight risks and possible complications involved, and although it is difficult to say exactly how often these occur, they are generally minor and do not happen very often. © The Royal College of Radiologists, July 2000. Permission is granted to modify and/or re-produce this leaflet for purposes relating to the improvement of health care provided that the source is acknowledged and that none of the material is used for commercial gain. The material may not be used for any other purpose without prior consent from the College. Legal Notice Please remember that this leaflet is intended as general information only. It is not definitive, and the RCR and the BSIR cannot accept any legal liability arising from its use. We aim to make the information as up to date and accurate as possible, but please be warned that it is always subject to change. Please therefore always check specific advice on the procedure or any concerns you may have with your doctor. This leaflet has been prepared by the British Society of Interventional Radiology (BSIR) and the Clinical Radiology Patients' Liaison Group (CRPLG) of the Royal College of Radiologists. Board of the Faculty of Clinical Radiology The Royal College of Radiologists. July 2000 Control Date: 05/02/16 Page 14 of 14