All- - Vanderbilt University
advertisement
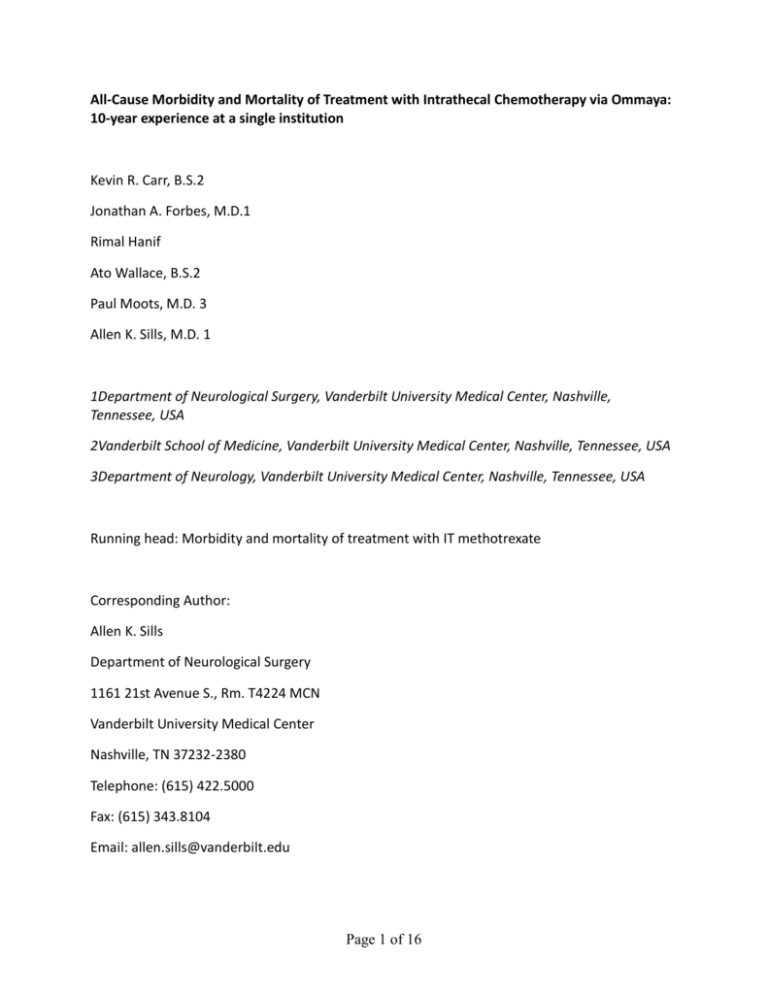
All-Cause Morbidity and Mortality of Treatment with Intrathecal Chemotherapy via Ommaya: 10-year experience at a single institution Kevin R. Carr, B.S.2 Jonathan A. Forbes, M.D.1 Rimal Hanif Ato Wallace, B.S.2 Paul Moots, M.D. 3 Allen K. Sills, M.D. 1 1Department of Neurological Surgery, Vanderbilt University Medical Center, Nashville, Tennessee, USA 2Vanderbilt School of Medicine, Vanderbilt University Medical Center, Nashville, Tennessee, USA 3Department of Neurology, Vanderbilt University Medical Center, Nashville, Tennessee, USA Running head: Morbidity and mortality of treatment with IT methotrexate Corresponding Author: Allen K. Sills Department of Neurological Surgery 1161 21st Avenue S., Rm. T4224 MCN Vanderbilt University Medical Center Nashville, TN 37232-2380 Telephone: (615) 422.5000 Fax: (615) 343.8104 Email: allen.sills@vanderbilt.edu Page 1 of 16 Reprint Requests: Allen K. Sills Department of Neurological Surgery 1161 21st Avenue S., Rm. T4224 MCN Vanderbilt University Medical Center Nashville, TN 37232-2380 Telephone: (615) 422.5000 Fax: (615) 343.8104 Email: allen.sills@vanderbilt.edu Key words: morbidity, mortality, treatment with intrathecal methotrexate, CNS lymphoma Page 2 of 16 All-Cause Morbidity and Mortality of Treatment with Intrathecal Methotrexate via Ommaya: 10-year experience at a single institution Background: Individual studies have described both the medical morbidity of treatment with intrathecal methotrexate and the surgical morbidity of Ommaya placement. However, information regarding the all-cause morbidity of intrathecal treatment with methotrexate following Ommaya placement is lacking. Methods: The authors retrospectively studied complications associated with Ommaya insertion and subsequent intraventricular methotrexate therapy in patients with various CNS neoplasms over a 10 year period. In total, 65 patients were treated with intraventricular methotrexate chemotherapy using an Ommaya reservoir and intraventricular catheter system. Surgical morbidity of Ommaya insertion and medical morbidity related to intrathecal methotrexate therapy were assessed. Results: Regarding surgical complications, 9 out of 65 (15.4%) patients suffered infection of the Ommaya, 3 of whom required hardware removal. 3 out of 66 (4.5%) patients suffered an intracranial hemorrhage as a result of surgery—fatal in one (1.5%). In total, 12 of 65 patients (18.5%) experienced some form of surgical morbidity. Regarding medical complications, 8 out of 65 (12.3%) patients experienced acute chemical arachnoiditis. Another 4 of 65 (6.2%) patients experienced sub acute myelopathy of the central nervous system and 8 (12.3%) suffered from chronic leukencephalopathy. No episodes of acute fulminant brain edema were recorded. In total, 15 of 65 patients (23.0%) experienced some form of medical morbidity. Conclusions: Altogether 30 of 65 (46%) patients experienced significant complication(s) as a result of Ommaya reservoir insertion and/or subsequent intrathecal methotrexate therapy. This information should prove useful for practitioners considering the risk-benefit analysis of Page 3 of 16 permanent reservoir insertion for intrathecal methotrexate therapy in patients with various CNS neoplasms. Page 4 of 16 Introduction The Ommaya catheter is an indwelling ventricular access device commonly used for intrathecal chemotherapy, precluding the need for repeated intrathecal punctures. Although an Ommaya reservoir is the preferred route of intrathecal methotrexate administration, achieving significantly higher ventricular drug concentrations, Ommaya placement is associated with attendant surgical morbidity (Bleyer, Poplack et al 1978). Specifically, surgical morbidity can include device malfunction, device, infection, and intracranial hemorrhage. Reasons for high rate of infection with Ommaya reservoir include: 1) myelosuppression secondary to chemotherapy administration; 2) many patients suffering from hematologic malignancies are severely immunocompromised. Surgical morbidity as a result of Ommaya placement is well characterized by various studies highlighted in Table 1. Surgical complications secondary to Ommaya implantation: a literature study Author/year Total Complications Infection Hemorrhage Death (Lishner, Perrin et al. 1990) 11/106 (10.3%) 10/106 (9.4%) 2/106 (1.9%) -- (Sandberg, Bilsky et al. 2000) 10/107 (9.3%) 2/107 (1.8%) 3/107 (2.8%) 2/107 (1.8%) (Chamberlain, Kormanik et al. 1997) 19/120 (15.8%) 9/120 (45%) -- -- (Schlegel, Pels et al. 2001) 5/20 (25%) Page 5 of 16 (Greenfield and Schwartz 2008) 3/20 (15%) Table 1. Surgical complications secondary to Ommaya implantation: a literature study Methotrexate is a potent chemotherapeutic agent that is widely used as monotherapy or multitherapy for CNS tumors, including primary CNS lymphoma and leptomeningeal dissemination. While this chemotherapeutic agent has found favor as the primary treatment agent for several CNS tumors, it occasionally is associated with significant neurotoxicity. Methotrexate toxicity usually manifests subacutely, within one to two weeks after administration. Patients often present with stroke-like symptoms, such as sensory deficits, paresis, and aphasia, with resolution of clinical and radiological findings within one week to a month of presentation (Agarwal, Vijay et al. 2011; Tufekci, Yilmaz et al. 2011) . Occasionally patients can present with acute neurological deficits, within one to two hours following administration—often associated with confusion, disorientation and/or seizures. These symptoms, though acute, usually resolve completely with dexamethasone and folinic acid (Tufekci, Yilmaz et al. 2011). Medical morbidity secondary to intrathecal methotrexate is described in various studies, listed in Table 2. Medical complications associated with intrathecal methotrexate administration: a literature study Author/year Leukoencephalopathy Myelopathy Death (Schlegel, Pels et 2/20 (10%) --al. 2001) (Chamberlain, 1/120 Kormanik et al. 2/120 (1.7%) -(0.83%) 1997) (Greenfield and 3/20 (15%) --Schwartz 2008) (Weigel, Senn et 1/3 (33.3%) -2/3 (66.7%) al. 2004) Table 2. Medical Complications associated with intrathecal methotrexate administration: a literature study Individual studies have described either medical morbidity of treatment with intrathecal methotrexate or surgical morbidity of Ommaya placement. To the authors’ knowledge, this is Page 6 of 16 the first study to report all-cause surgical and medical morbidity and mortality of intrathecal treatment with methotrexate following Ommaya placement. Methods Morbidity/Mortality Assessment: Surgical morbidity as a result of Ommaya placement was classified as (1) infectious (2) hemorrhagic and (3) death suffered from the operation. Medical morbidity secondary to methotrexate administration occurring within a window of causality was stratified as (1) acute chemical arachnoiditis, (2) sub-acute myelopathy (3) chronic leukencephalopathy (4) fulminant brain edema and (5) other. The treatment window was defined as two months following placement of Ommaya reservoir and initiation of intrathecal methotrexate adminstration. Acute chemical arachnoiditis was diagnosed in patients with a combination of headaches, fever, nuchal rigidity, or back pain. Subacute myelopathy describes patients who presented with myelopathy of the long fiber tracts, with clinically associated paraparesis or paraplegia. The categorization of chronic leukencephalopathy was reserved for patients who presented with confusion, irritability, somnolence, ataxia, dementia, seizures or coma. Fulminant brain edema is a radiologic classification for clinically significant bulbar or brainstem deficits. Patient Population: The study highlighted a cohort of 65 patients recorded from 2001-2011 who received intrathecal methotrexate therapy via an Ommaya reservoir catheter at the Vanderbilt University Medical Center. There were 30 (46.1%) females and 35 (53.9%) males. Patients’ ages ranged from 4 months to 78 years old, with an average age of 42 years and a median age of 43 years. 13 patients were older than 60 years at the time of operation. As previous studies have suggested a link between methotrexate toxicity and ventricular obstruction secondary to tumor morphology, patients were retrospectively stratified using physical tumor characteristics into one of three groups: (1) bulky tumors suggestive of CSF blockage, (2) intra-axial tumors without the likelihood of occlusion, or (3) CNS lesions in the absence of intra-axial tumors (Table 3). Bulky tumors were characterized by the presence of intracerebral lesions along the ventricular foramina. These lesions were assessed based on their likelihood of causing hydrocephalus secondary to CSF flow obstruction. Of the patients assessed, 8 had bulky tumors suggestive of possible obstruction, 14 had intracranial tumors not indicative Page 7 of 16 of possible obstruction and the rest (43) showed no evidence of intra-axial CNS lesions. Radiologic assessment was made via magnetic resonance imaging studies obtained at the Vanderbilt University School of Medicine. Tumor Characteristics Total Male Female Intra-axial bulky 8 | 11.3% 5 3 tumor Intra-axial none15 | 21.1 % 6 8 bulky tumor None intra-axial 43 | 60.56 % 24 19 tumor Total 35 30 Table 3. Tumor characteristics based on radiographic likelihood to cause CSF obstruction Of the patients identified 20(30.8%) patients had a primary diagnosis of acute lymphocytic leukemia, 11 patients hadlarge B cell lymphoma [LBCL], 3 had Burkett’s lymphoma, 5 had acute myelogenous leukemia, while the remaining patients presented with either carcinomatous meningitis, chronic myelogenous leukemia or other lesions (Table 4). Age Range Diagnosis Large B Cell Lymphoma Acute myelogenous leukemia (AML) Acute lymphocytic leukemia (ALL) Metastatic carcinomatous meningitis Burkett’s lymphoma Male Female 41-78 34-61 8 3 3 2 4 ms – 64 11 9 36-70 1 8 30-59 3 0 *Other 9 8 Total 35 30 Table 4. Age, sex and Primary diagnosis of patient population receiving intrathecal MTX via and ommaya reservoir. [* Other includes, Anaplastic T Cell leukemia, Mantle Cell lymphoma, Follicular Celllymphoma, Medulloblastoma, NK T Cell lymphoma Treatment: Prior to placement of Ommaya catheter, patients were induced with general anesthesia and prepped and draped in the usual fashion. Following incision and burr hole placement, the Page 8 of 16 intrathecal catheter was introduced into the lateral ventricles using intraoperative navigation. The reservoir was subsequently connected and placed with a subgaleal pocket. Patients presented to the Medical Center with various diagnoses in varied states of advancement. Intrathecal treatment regimens were thus stratified per their presenting diagnoses and comorbidities. Of the cohort assessed patients either received methotrexate monotherapy or multitherapy.29 patients (44.6%) received methotrexate only, with the majority, 55% receiving additional chemotherapy agents. Additional chemotherapy included, among others, CystosineArabinoside, Depocyt ®, Vincristine, Xeloda®, ICE ®, ESAP®, RICE® multitreatments. The median number of intrathecal chemotherapy administration was 2, with only 3 patients receiving ≥2 treatments during the period of study. Medical morbidity was assessed similarly for both groups, multitherapy defined as Intrathecal Methotrexate administration in addition to any other agent administered within the window of time associated with methotrexate morbidity. Results 12 of 65 patients (18.5%) experienced some form of surgical morbidity from Ommaya placement—9 patients (13.8%) suffered infection of the Ommaya device, 3 of whom required hardware removal. 3 (4.6%) patients suffered an intracranial hemorrhage, fatal in 1 (1.5%) (Table 5). 3 patients had both surgical and medical complications as a result of the treatment and 5 patients had at least two medical or surgical complications. Of the patients found to have infections, 2 patients developed hemorrhages. Surgical morbidity associated with intrathecal Ommaya implantation Age Male Female Range Hemorrhage 31-48 2 1 Infection 28-64 6 3 Table 5. Of the patients presenting with surgical morbidity, 75% were due to infections Page 9 of 16 One death due to surgical intervention was reported in our study, a 48-year-old Caucasian male with a diagnosis of multiple myeloma with CNS involvement. The patient prior to surgical intervention had presented with enlarging plasmacytomas with left sided gaze palsy and headaches. Head CT showed significant clivus involvement of his lesions with severe right carotid canal erosion. Subsequent to Ommaya implantation the patient developed intracerebral hemorrhages identified by multiple Ommaya taps and postoperative CT. The patient became obtunded, and developed intermittent apnea and worsening respiratory acidosis and died four days after insertion of Ommaya reservoir. There were 9 reported cases of infections related to Ommaya reservoir implantation. 50% of the cases were due to coagulase negative staphylococcus. One infected patient died while receiving treatment after developing a subarachnoid hemorrhage identified on CT. Blood samples were found to have grown Capnocytophaga species and Stomatococcusmucillaginosis and he was unsuccessfully treated with IV levofloxacin, cefipime and metronidazole for a concomitantClostridium difficile gastrointestinal infection. Only 3 (33.3%) patients required Ommaya shunt removal due to their infections, as the rest of the patients had resolution of infection with antibiotics. Infectious complications due to Ommaya implantation Patient Diagnosis Number/Age 1/42 Mantle Cell Lymphoma 2/40 CML 3/28 ALL 4/64 LBCL 5/31 ALL Organism Management Outcome Coagulase Negative Staphylococcus Coagulase Negative Staphylococcus Coagulase Negative Staphylococcus Propionibacterium Acnes IV Vancomycin + po Rifampin Resolved IV Vancomycin Resolved IV Vancomycin, Cefipime,Levaquin & ommaya removal Po Rifampine, Levaquin Resolved Capnocytophaga Species, StomatococcusMu cillaginosus IV Levaquin, Cefipime, Metronidazole Died Page 10 of 16 Resolved 6/64 Primary CNS Lymphoma 7/44 8/54 NK Cell Lyphoma TALL 9/52 ALL 10/38 ALL Coagulase Negative Staphylococcus None identified IV Vancomycin Resolved IV Levaquin, Vancomycin Resolved MRSA IV Vancomycin, Zyvoxx&ommaya removal IV Cefipime, Vancomycin&ommaya removal IV vancomycin, polevaquin Resolved Coagulase Negative Staphylococcus Streptococcus alpha Transferred Resolved Table 6. Coagulase negative staphylococcus was the primary agent for infectious complications Of the 65 patients in our cohort, 18 (27.6%) developed some medical morbidity due to treatment intervention. 8 (12.3%) patients developed acute chemical arachnoiditis, 4 (6.2%) developed subacute myelopathy, and 8 (12.3%) developed chronic leukoencephalopathy (Table 7). None of the patients developed fulminant brain edema. One patient developed both characteristics of subacute myelopathy and chronic leukencephalopathy, while another developed acute chemical arachnoiditis and subacute myelopathy some time later. The average age however for patient who developed at least some medical morbidity was slightly higher than the total cohort at 48.9 years old. Medical morbidity associated with intrathecal methotrexate administration Age range Acute chemical arachnoiditis Subacute Myelopathy Fulminant brain edema Chronic leukencephalopathy Male Female 26-70 5 3 26-65 -- 3 0 1 0 4-65 4 4 Table 7. Medical morbidity associated with intrathecal methotrexate administration Page 11 of 16 Of the cohort, nine (9), 13.8% patients who received intrathecal methotrexate chemotherapy in addition to some other chemical treatment developed medical morbidity. Additionally, nine (9) patients developed chemical morbidity secondary to intrathecal methotrexate administration alone. Of that patients with chemical multitherapy who developed chemical morbidity 44.4% was due to acute chemical arachnoiditis and 22.2% presented with symptomas consistent with sub-acute myelopathy. Twenty seven (27) patients, 41.5% of the cohort received multitherapy without documented medical complications. Patient Number 1 Treatments Medical Complications Taxotere Chronic Leukencephalopathy Intrathecal Methotrexate 2 Intrathecal Depocyt Acute Chemical Arachnoiditis Intrathecal Methotrexate 3 Intrathecal Methotrexate Acute Chemical Arachnoiditis Vincristine Daunomycin 4 ECOG Trial ® [Methotrexate, Chronic Leukencephalopathy Procarbazine, Vincristine, Rituximab] Temodar, Rituxan Intrathecal Methotrexate 5 Intrathecal Methotrexate Sub-Acute Myelopathy Vincristine 6 Intrathecal methotrexate Acute Chemical Arachnoiditis Cystosine Arabinose, Cyclophosphamide 7 Intrathecal Methotrexate Acute Chemical Arachnoiditis Cyclophosphamide 8 Intrathecal Methotrexate Chronic Leukencephalopathy Temozolamide 9 Intrathecal Methotrexate Sub-Acute Myelopathy Topotecan Table 7. The majority of chemical complications associated with chemical multitherapy were acute chemical arachnoiditis Discussion This is the first study to report all-cause morbidity and mortality of intrathecal treatment with methotrexate following Ommaya placement. While the intrathecal administration of methotrexate via the Ommaya reservoir is an improvement over lumbar access (Bleyer and Poplack 1979), the morbidity associated with chemotherapy administration via Ommaya is Page 12 of 16 nonetheless substantial. Several studies have documented a rate of surgical complications due to Ommaya placement similar to that found in our study. In a series of 20 patients with primary CNS lymphoma, 19 (95%) of whom underwent Ommaya placement for intraventricular chemotherapy with several agents, 4 (21.0%) patients suffered infection of Ommaya reservoir (Schlegel, Glasmacher et al 2001). In another study of 120 patients undergoing Ommaya reservoir placement for treatment of leptomeningeal metastases, 2 patients (2%) had malpositioned catheters, 6 (5%) developed unidirectional catheter obstruction, 2 (2%) developed delayed pressure necrosis of the skin overlying the Ommaya reservoir, and 4 (3%) developed Staphylococcus epidermidis meningitis related to Ommaya reservoir placement. In all, 14 patients (12%) developed surgical complications related to Ommaya placement, of whom 6 patients (6%) underwent replacement of Ommaya reservoir. 5 (4%) additional patients suffered from Staphylococcus epidermidis meningitis more than 30 days after Ommaya placement; therefore, these infections were not considered surgical complications of Ommaya placement and were instead believed to be secondary to iatrogenic introduction of bacteria during chemotherapy administration via the Ommaya reservoir. Of the 9 patients who developed bacterial meningitis, the first 2 underwent replacement of Ommaya reservoir in addition to antibiotic therapy, while the remaining 7 were successfully treated with intravenous and intraventricular vancomycin in conjunction with oral rifampin. Therefore, antibiotic treatment without surgical replacement of Ommaya reservoir appears to be an effective method to prevent reoperation. Similarly, in our cohort, 6 of 9 patients (66%) with infection secondary to Ommaya placement were treated with antibiotics alone and did not require replacement of Ommaya device (Chamberlain, Kormanik et al 1987). Similarly, in our cohort, there were 9 (13.8%) patients who sustained an infection due to Ommaya implantation. The majority of our cases were found to be due to coagulase-negative Staphylococcus species, and 6 of 9 (75%) patients were treated with antibiotics alone. In both of the previous two studies, the surgical morbidity is significantly higher than that found by (Sandberg, Bilsky et al. 2000), who demonstrated a 9.3% surgical complication rate. In the cohort of 107 patients, intrathecal Ommaya implantation was assisted in 72.6% of patients by intraoperative fluoroscopic guidance. No such assistance was utilized in our study. Nonetheless, there still is significant morbidity associated with the technical aspect of the reservoir’s implantation with even the utilization of frameless stereotaxy in patient populations, (Greenfield and Schwartz 2008) producing 13.3% and 6.6% infection and hemorrhage rates, lrespectively. Methotrexate is a potent chemotherapeutic agent and is widely used to treat leptomeningeal dissemination and primary CNS lymphoma (PCNSL). In a series of 20 patients with primary CNS lymphoma, 19 (95%)of whom underwent Ommaya placement for intraventricular chemotherapy with methotrexate among other agents, 9 (45%) patients developed Page 13 of 16 neurotoxicity believed to be methotrexate induced. 2 (10%) patients developed fully reversible transient encephalopathies, 1 (5%) developed subacute encephalopathy that resolved over months, and 6 (30%) developed leukoencephalopathy, of whom 4 patients suffered no cognitive impairment, 1 suffered severe cognitive impairment, and 1 died (Schlegel, Glasmacher et al 2001). In a case report of 3 patients with PCNSL, severe complications related to intrathecal methotrexate administration were described, including 2 patients who died secondary to fulminant brain edema and 1 patient who developed severe dementia, gait disturbance and urinary incontinence due to leukoencephalopathy (Weigel, Senn et al 2003). Since bulky disease was present in all three patients, the authors surmised that CSF flow abnormalities may have been present, even though no CSF flow studies were performed. Impaired CSF clearance exposes normal brain tissue to toxic drug concentrations. There are data to show that all patients with bulky leptomeningeal metastasis have impaired CSF flow studies. In addition, standard cross-sectional imaging did not identify CSF flow disturbances in up to 70% of patients. Therefore, CSF flow studies performed prior to intrathecal drug administration may be considered of prognostic significance. None of the patients receiving methotrexate in our series died due to methotrexate toxicity or developed fulminant brain edema. The most common complication was chemical arachnoiditis, which is common with intrathecal chemotherapy and may be treated with concurrent administration of corticosteroids. A significant proportion of our patients had bulky tumor burden and likely had impaired CSF flow contributing to methotrexate toxicity. Therefore, in the future patients with bulky tumor burden may benefit from CSF flow studies to determine suitability for intrathecal chemotherapy. In order to prevent neurotoxicity secondary to intrathecal methotrexate in patients with bulky intracranial tumors, alternate treatment strategies may be proposed. High-dose intravenous methotrexate alone provided therapeutic CSF concentrations, yet a lower cumulative concentration when compared to intrathecal methotrexate administration, and was successfully used in the treatment of PCNSL. Additionally, a case-controlled retrospective study matching patients treated with systemic methotrexate with or without intrathecal methotrexate found no difference in survival, disease control, or neurotoxicity. Therefore, high-dose intravenous methotrexate may preclude the need for intrathecal methotrexate and for Ommaya reservoir placement with regard to reducing neurotoxicity secondary to intrathecal methotrexate and surgical morbidity secondary to Ommaya placement. Limitations Page 14 of 16 This study is limited in that it is a retrospective analysis. Assessment of overall morbidity and mortality significantly after the post-operative phase was limited due to high rates of patient loss to follow-up. Additionally, treatment of various cancers demonstrated great variability in chemotherapeutic regimen. Conclusion Intrathecal MTX administration via Ommaya reservoir for the treatment of CNS tumors continues to present with significant morbidity. Though this treatment modality presents significant advances in intrathecal chemotherapy administration, there is much room for improvement of post-operative morbidity and mortality. Page 15 of 16 References: Agarwal, A., K. Vijay, et al. (2011). "Transient leukoencephalopathy after intrathecal methotrexate mimicking stroke." Emerg Radiol18(4): 345-347. Bleyer, W. A. and D. G. Poplack (1979). "Intraventricular versus intralumbar methotrexate for central-nervous-system leukemia: prolonged remission with the Ommaya reservoir." Med Pediatr Oncol6(3): 207-213. Chamberlain, M. C., P. A. Kormanik, et al. (1997). "Complications associated with intraventricular chemotherapy in patients with leptomeningeal metastases." J Neurosurg87(5): 694-699. Greenfield, J. P. and T. H. Schwartz (2008). "Catheter placement for Ommaya reservoirs with frameless surgical navigation: technical note." Stereotact Funct Neurosurg86(2): 101105. Lishner, M., R. G. Perrin, et al. (1990). "Complications associated with Ommaya reservoirs in patients with cancer. The Princess Margaret Hospital experience and a review of the literature." Arch Intern Med150(1): 173-176. Mechleb, B., F. Khater, et al. (2003). "Late onset Ommaya reservoir infection due to Staphylococcus aureus: case report and review of Ommaya Infections." J Infect46(3): 196-198. Bleyer WA, Poplack DG, Simon RM. (1978). "Concentration x time methotrexate via a subcutaneous reservoir: a less toxic regimen for intraventricular chemotherapy of central nervous system neoplasms." Blood51: 835-42. Sandberg, D. I., M. H. Bilsky, et al. (2000). "Ommaya reservoirs for the treatment of leptomeningeal metastases." Neurosurgery47(1): 49-54; discussion 54-45. Schlegel, U., H. Pels, et al. (2001). "Combined systemic and intraventricular chemotherapy in primary CNS lymphoma: a pilot study." J Neurol Neurosurg Psychiatry71(1): 118-122. Tufekci, O., S. Yilmaz, et al. (2011). "A rare complication of intrathecal methotrexate in a child with acute lymphoblastic leukemia." Pediatr Hematol Oncol28(6): 517-522. Weigel, R., P. Senn, et al. (2004). "Severe complications after intrathecal methotrexate (MTX) for treatment of primary central nervous system lymphoma (PCNSL)." Clin Neurol Neurosurg106(2): 82-87. Page 16 of 16