Periph_nerves_reflex..
advertisement

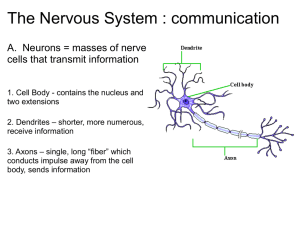
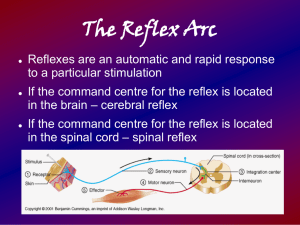
Periph_nerves_reflexes_notes.doc WCR 2015 (See Marieb & Hoehn ch. 13) Sensory Receptors Convert physical stimulus into nerve impulses Basic structure and mode of activation Classify by stimulus type that they’re most responsive to, or by location, or by structure: By stimulus type: mechano-, thermo-, photo-, chemo-, nociBy location: extero-, intero-, proprioBy structure: Simple (unencapsulated, etc); complex (“special” senses) Adaptation – more in some than in others; for example, nociceptors don’t adapt much Peripheral nerves have afferent & efferent fibers, small blood vessels, connective tissue wrapper, subdivided into fascicles, each fascicle with many axons Cranial Nerves For each of the 12 cranial nerves, know: Name Motor, sensory, or both Function Symptoms that might be present if nerve is damaged (as discussed in class) Spinal nerves Spinal nerves: C1-C8(!), T1-T12, L1-L5, S1-S5, C0 Dermatomes: skin region with sensory innervation from one spinal nerve; overlap some Shingles: Due to varicella zoster virus (which also causes chicken pox), can erupt decades after chicken pox. Rash follows a dermatome since virus lives in and along a single spinal nerve on one side Spinal nerve ramus organization Dorsal & ventral rami (plural of ramus) Dorsal & ventral roots Be able to explain the path taken by motor outputs and sensory inputs as they go between periphery (on dorsal or ventral part of the body) and the spinal cord, or vice versa. Rami communicantes (communicating ramuses): At thoracic levels there are also the communicating rami which have autonomic nerve fibers going to/from the sympathetic trunk ganglia, which run vertically just outside the vertebral column on either side. More in the autonomic chapter. Spinal nerve distribution Plexus = network of nerve fibers outside the CNS 4 major plexuses formed by ventral rami at different spinal levels Cervical Plexus C1 – C5 Innervation to some neck & shoulder muscles & skin Phrenic nerve (to diaphragm) = most important output Brachial Plexus C4 – T1 Supplies muscles & skin of upper limb and shoulder Branches include: 1. Axillary 2. Musculocutaneous 3. Radial 4. Median 5. Ulnar Radial, median, & ulnar nerves innervate forearm and hand muscles and skin; median nerve runs through carpal tunnel. Also see details of motor & sensory functions of musculocutaneous and axillary nerves. Lumbar Plexus L1-L4 Innervates parts of genitals, skin & muscles of hip and parts of thigh and leg (hip adductors, knee extensors) Branches include: 1. Femoral nerve 2. Obturator nerve Sacral Plexus L4-S4 Innervates parts of genitals, skin & muscles of hip and leg (hip abductors, knee flexors (hamstrings), muscles below the knee) Branches include: 1. Sciatic nerve: longest and largest-diameter nerve in the body. Sciatic nerve gives rise to a. Tibial nerve b. Common fibular (common peroneal) nerve 2. Superior & inferior gluteal Reflexes Neural reflex organization Circuit organization: diverging, converging, reverberation (feedback, good for rhythm generation) Processing: serial or parallel or both Reflex = rapid automatic response to stimulus Steps 1. Receptor activation by stimulus 2. Sensory neuron activation 3. Central processing in CNS (brain or SC) 4. Motor neuron activation 5. Response of peripheral effector (e.g. muscle) Stretch reflex Sensor = muscle spindle, responds to muscle stretch by generating action potentials on afferent neuron Muscle spindle is innervated by gamma motor neuron Muscle stretch causes more action potentials to be generated by the “sensors”: the muscle spindles. This causes activation of motor neurons going to that same muscle. This helps a muscle maintain its length relatively constant even when load on it changes quickly. Also, the antagonist muscle is inhibited. Monosynaptic, ipsilateral. Patellar reflex: An example of a stretch reflex Tap patellar tendon to activate stretch reflex in fibers of quadriceps femoris. Normal response: quick mild knee extension. Tests femoral nerve and descending control of spinal reflexivity. Golgi tendon reflex Sensor = Golgi tendon organ, similar to a muscle spindle in that stretch activates it Does the opposite of what the muscle stretch reflex does: inhibits activity in the muscle attached to lengthening tendon, and activates antagonist muscle. Polysynaptic, ipsilateral Flexor (withdrawal) & crossed extensor reflexes Flexor (withdrawal) reflex Initial stimulus is sudden pain which causes flexion of ipsilateral limb muscles to pull limb away from source of pain. Ipsilateral extensors are simultaneously inhibited. Polysynaptic, ipsilateral Crossed extensor reflex Present in weight bearing limbs. Initial stimulus is sudden pain. This activates the (ispilateral) flexor reflex (see above), and causes extension of contralateral limb. Contralateral limb flexors are simultaneously inhibited. Helps to maintain balance if one steps on sharp object, stubs toe, etc.: straighten out and stiffen the opposite leg to prevent falling. Polysynaptic, contralateral Superficial Reflexes Plantar reflex Sometimes called Babinski reflex, although purists object to that usage. Used by clinicians to test spinal cord integrity and corticospinal connections Stimulus: draw a blunt object along the lateral aspect of the plantar surface (sole) of foot, from heel to toe. “Negative” Babinski sign: toes flex down in response to stimulus. “Positive” Babinski sign: toes fan out & flex upward in response to stimulus. Adults and children over 1 y.o.: negative is normal. Infants < 1 y.o.: positive Babinski sign is normal. Positive Babinski in an adult suggests damage to brain centers or descending pathways.