Vagus nerve stimulator-induced apneas and hypopneas in a child
advertisement

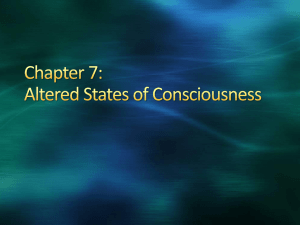
Vagus nerve stimulator-induced apneas and hypopneas in a child with refractory seizures Running title: Vagal nerve stimulators and apneas Fuzhan Parhizgar a, Karen Rogers b, Daniel Hurst b, Kenneth Nugent a and Rishi Raj a,* a Department of Internal Medicine, Texas Tech University Health Sciences Center, Lubbock, TX, USA b Department of Pediatrics, Texas Tech University Health Sciences Center, Lubbock, TX, USA * Corresponding author: Rishi Raj, M.D. Department of Internal Medicine, Texas Tech University Health Sciences Center, 3601 4th Street, Stop 9410, Lubbock, Texas 79430, USA Tel.: +1 806 743 3155; Fax: +1 806 743 3148; E-mail: rishi.raj@ttuhsc.edu. Received: 29 March 2011 Revised: 13 May 2011 Accepted: 7 July 2011 1 Abstract. Vagal nerve stimulators (VNS) can decrease seizure frequency in pediatric patients with refractory seizure disorders. However, vagal nerve stimulation can cause apneas and hypopneas during sleep, especially in patients with undiagnosed obstructive sleep apnea. We currently care for a young boy with cerebral palsy and refractory seizures. His mother noted intermittent noisy breathing and pauses in breathing at night following VNS implantation. An overnight sleep study revealed very abnormal sleep architecture and an apnea-hypopnea event rate of nine per h (18 per h when supine). After a review of the management options, the VNS was disabled. A repeat sleep study demonstrated improved sleep architecture and a reduced number of apneas and hypopneas (overall and supine event rate 1.7 per h). Management options in these patients include changing the VNS parameters, the use of positive airway pressure therapy, and discontinuing the VNS device. Keywords: Vagal nerve stimulator, apnea, hypopnea, seizures 2 1. Introduction Vagal nerve stimulators (VNS) can reduce the frequency of seizures to varying degrees in patients with epilepsy [1]. Patients implanted younger than 12 yr, patients with tuberous sclerosis, and Lennox-Gastaut patients may have better outcomes with VNS treatment [1]. However, VNS can change the respiratory pattern in patients and can induce or aggravate sleep apnea. We report a patient who had an increase in apneas and hypopneas after VNS implantation and discuss the management options. 2. Case report The patient, a 5-year-old boy with cerebral palsy, started having seizures at 20 mo of age. He was developmentally delayed and had a vocabulary span of five words at 20 mo. Electroencephalography done during these seizure episodes showed generalized, frontal and central spike and spike wave activity. The seizure frequency increased to 20 times per day. Eventually his seizures were refractory to combination medical therapy. No other etiology for his seizures was uncovered despite an extensive evaluation, including multiple genetic and metabolic tests. The patient was finally treated with zonisamide, valproate, and clorazepate and had a VNS implanted. This therapeutic regimen improved seizure control, but he continued to have seizures at the rate of one event every one to two weeks. On a follow up visit, the mother reported intermittent noisy breathing and pauses in breathing during the night. These symptoms were new and were not present before the VNS was placed. No excessive daytime somnolence or behavioral changes were reported by the mother. Physical examination was unremarkable except for findings consistent with his underlying diagnosis of cerebral palsy. No stridor or difficulty breathing were noted during the physical examination. The patient was referred for a diagnostic polysomnography for suspected obstructive sleep apnea (OSA). The montage employed consisted of electroencephalography (F4-M1, C4-M1, F3-M2, C3-M2, O2-M1, O1-M2), electro-oculography (E1-M2, E2-M2), electromyography 3 (EMG) (submental, mental), snoring (microphone), nasal and oral airflow (thermistor), chest and abdominal respiratory effort, pulse oximetry, single lead electrocardiography, limb EMG, and body position (manual). Computerized polysomnography recording equipment (BioLogic Sleep Scan V. 2.03.05. Natus, San Carlos, CA) was used to record the polysomnography. The study was scored per the criteria set forward by the American Academy of Sleep Medicine in 2007 [2]. This sleep study demonstrated OSA/hypopnea with an overall apnea-hypopnea index (AHI) of 9.0 and a supine AHI of 18.0. Sleep efficiency was 63%. Sleep stage distribution for the night was 37% stage W (wakefulness), 1.5% stage N1 (non-rapid eye movement [NREM] 1), 17.5% stage N2 (NREM 2), 44.0% stage N3 (NREM 3) and 0% stage R (rapid eye movement [REM]). Sleep onset latency was prolonged at 92 min. Hypopnea events coincided with VNS impulses, which could clearly be seen on the EMG channel (Fig. 1). The sleep technician reported “stridorous vocalizations” which coincided with the vagal nerve stimulations. The VNS impulses occurred approximately every 150 sec and lasted approximately 35 sec. Subtle decrease in airflow was noted during wakefulness, but during sleep every single VNS impulse was associated with significant decrease in flow without any change in thoracic or abdominal movements. Most impulses were not associated with arousals or desaturation. No apnea/hypopnea events independent of the VNS impulses were noted. These events (mostly hypopneas) were more severe in the supine position and were partially relieved when the patient was placed in a lateral position. Various therapeutic options were considered for treating the patient’s OSA. Positive airway pressure therapy was considered less than an ideal solution because of behavioral and compliance issues. The patient had already had a tonsillectomy and adenoidectomy in the past for non-sleep related issues, and other surgical therapy was considered too invasive. It was decided to cautiously discontinue the VNS and closely monitor the patient for recurrent seizure activity. The VNS was disabled, and the patient was scheduled for another sleep 4 study. The mother reported disappearance of the apnea events and near complete disappearance of the noisy breathing during the night. Repeat diagnostic polysomnography revealed snoring but no “stridorous vocalizations”. Sleep onset and REM onset were within normal limits. Sleep efficiency had increased to 96.4%. Sleep stage distribution for this repeat sleep study was 3.6% stage W (wakefulness), 0% stage N1 (NREM 1), 33.2% stage N2 (NREM 2), 47.0% stage N3 (NREM 3) and 16.2% stage R (REM). The AHI was 1.7 with one central, five obstructive, and seven hypopneic events. The patient spent the entire night in supine position, and the supine AHI was 1.7 as well. The patient’s seizure frequency and severity did not change after discontinuing the VNS, but seizure control has been incomplete during the last 2 yr, even with the addition of lacosamide. 3. Discussion VNS therapy can induce apneas and hypopneas in patients without OSA and can increase the number in patients with OSA. However, information on the frequency and severity of these sleep disordered breathing events is limited. Hsieh et al. [3] studied nine epileptic pediatric patients (13.9 ± 4.6 yr old) with VNS using polysomnography during their sleep. Sleep efficiency was reduced, and sleep latency and REM latency were increased. The average apnea-hypopnea index was 14.4 ± 19.4 per h, and the arousal index was 31.8 ± 39.4 per h. The mean oxygen saturation was 96.7% ± 1.1%, and they had 10 ± 9 desaturation episodes per h. Eight patients had snoring or loud breathing during sleep. Six patients had an AHI ≥ 5; these patients had 8.3 ± 11.3 central apneas per h, 73.3 ± 61.5 obstructive hypopneas per h, and 18.8 ± 26.9 obstructive apneas per h. One patient had a high event rate when supine (180 events per h), and one had a high event rate when in REM sleep (15 per h). There was no correlation between the respiratory event rate and body mass index. This study reports the highest AHI observed in these patients and demonstrates that children can have clinically significant OSA associated with VNS therapy. One of these patients had an AHI of 37 after 5 VNS placement. Repeat polysomnography in this patient with the VNS turned off showed that her AHI had decreased from 37 to 10 [3]. Treatment options for these patients include changing the VNS parameters, positive airway pressure therapy, and turning off the VNS device. VNS operational parameters can influence the AHI in patients with VNSs. A cycling time of 300 sec is a common but not universal setting for most VNS [4]. Since most obstructive events are related to vagal stimulation in these patients and more severe sleep-disordered breathing is associated with the shorter cycling time, increasing the cycling time to 300 sec in patients with shorter cycling times will likely improve the sleep-disordered breathing in these patients [4,5]. Stimulation frequency also affects the severity of airflow obstruction and can be adjusted in patients with OSA/hypopnea related to VNS. Airflow obstruction and obstructive events related to VNS are highest at a device setting of 30 Hz, are less at 20 Hz, and are virtually non-existent at 10 Hz [6]. Both lowering the frequency and increasing the cycle time have been recommended by the manufacturer to potentially prevent worsening of OSA during VNS therapy. In patients with severe sleep-disordered breathing related to VNS in whom other therapeutic options are either ineffective or not tolerated, taping the magnet over the stimulator during sleep might be an alternative to deactivating the stimulator completely. The authors are unaware of any published literature on the effectiveness of the VNS when it is on only for a portion of the day, but it seems reasonable to speculate that vagal nerve stimulation for approximately 16 h in a 24-h period is more effective than no stimulation at all. VNS related sleep-disordered breathing events also depend on patient related factors. The AHI is often higher in the supine position and positional therapy could be used as an adjunct in these patients [4]. Hsieh et al. [3] and Marzec et al. [4] reported that continuous positive airway pressure (CPAP) was effective in treating sleep disordered breathing events in two patients with VNS. However, Ebben et al. [7] noted that CPAP titration with the device turned on was difficult and that 6 CPAP decreased but did not eliminate sleep disordered breathing events. This patient had an AHI of 82.3 during diagnostic polysomnography with the VNS on; the AHI was 0.4 with the VNS off and 13 with CPAP and the VNS on [7]. The patient reported by Hsieh had an AHI of 37 after VNS placement [3]. This AHI dropped to 10 after switching off the VNS and to 0.8 with CPAP and the VNS on [3]. In summary, VNS frequently can cause sleep apnea or exacerbate sleep apnea in patients with a preexisting diagnosis. These patients should routinely be checked for signs and symptoms of sleep disturbance before and after implantation of VNS, followed by a sleep study if clinically indicated. Treatment should be individualized, and therapeutic options consist of continuous positive airway pressure therapy, adjusting the VNS parameters and discontinuation of VNS. 7 References [1] Milby AH, Halpern CH, Baltuch GH. Vagus nerve stimulation in the treatment of refractory epilepsy. Neurotherapeutics 2009;6(2):228-37. [2] Iber C, Ancoli-Israel S, Chesson A, Quan SF; authors for the American Academy of Sleep Medicine. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. Westchester IL: American Academy of Sleep Medicine; 2007. [3] Hsieh T, Chen M, McAfee A, Kifle Y. Sleep-related breathing disorder in children with vagal nerve stimulators. Pediatr Neurol 2008;38(2):99-103. [4] Marzec M, Edwards J, Sagher O, Fromes G, Malow BA. Effects of vagus nerve stimulation on sleep-related breathing in epilepsy patients. Epilepsia 2003;44(7):930-5. [5] Gschliesser V, Hogl B, Frauscher B, Brandauer E, Poewe W, Luef G. Mode of vagus nerve stimulation differentially affects sleep related breathing in patients with epilepsy. Seizure 2009;18(5):339-42. [6] Malow BA, Edwards J, Marzec M, Sagher O, Fromes G. Effects of vagus nerve stimulation on respiration during sleep: a pilot study. Neurology 2000;55(10):1450-4. [7] Ebben MR, Sethi NK, Conte M, Pollak CP, Labar D. Vagus nerve stimulation, sleep apnea, and CPAP titration. J Clin Sleep Med 2008;4(5):471-3. 8 Figure Legend Fig. 1. A 300 sec representative epoch from the first polysomnography. Chin electromyography (green) shows artifacts corresponding to the vagal nerve stimulator (VNS) stimulation (labeled “VNS On”). Hypopnea events corresponded precisely with the periods of VNS activation and comprised nearly all sleep disordered breathing events during this study. These disappeared after the VNS was inactivated.