Pascotto Sample
advertisement

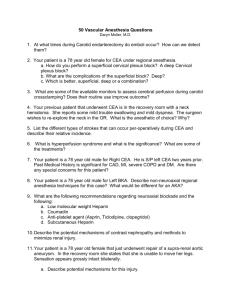
Pascotto Sample 1 SURGEON: Robert D Pascotto, MD ASSISTANT: Dan Beitelschies, PA DATE OF PROCEDURE: 10/14/2004 PREOPERATIVE DIAGNOSIS: Critical aortic stenosis with associated bicuspid valve. POSTOPERATIVE DIAGNOSIS: Critical aortic stenosis with associated bicuspid valve. PROCEDURE PERFORMED: Aortic valve replacement utilizing a 25-mm Carbomedics mechanical prosthesis. ANESTHESIA: General endotracheal anesthesia. OPERATIVE FINDINGS: At the time of operation the patient had a bicuspid densely calcified aortic valve. Once this was excised, the annulus accepted a 25-mm sizer and a Carbomedics valve as previously discussed with the patient was implanted. The patient was weaned from cardiopulmonary bypass without difficulty. PROCEDURE DESCRIPTION: After satisfactory general endotracheal anesthesia was accomplished, the patient was prepped and draped in the customary fashion. A median sternotomy incision was made and the sternum was split and the pericardium was entered. The patient received heparin intravenously. Aortic cannulation as well as single two-stage venous cannulae was inserted and cardiopulmonary bypass was initiated. While the patient was being cooled to 26 degrees centigrade, aortic crossclamp was applied and the patient received 1500 cc of cold blood cardioplegia retrograde. Throughout the cross-clamp period, the patient received intermittent doses of cold blood cardioplegia retrograde into the coronary sinus every 15 minutes. Antegrade cardioplegia was not delivered as the patient did have associated mild aortic insufficiency. An oblique incision was made on the proximal aspect of the ascending aorta and the above-described densely calcified bicuspid valve was appreciated. The valve was excised with great care taken not to allow any spicules of calcium to fall within the left ventricular cavity. Once he valve was excised, the annulus was debrided of a significant amount of calcification. The calcification extended onto the anterior leaflet of the mitral valve. Once this was accomplished, the annulus accepted a 25-mm sizer and a Carbomedics mechanical prosthesis as previously discussed with the patient was selected. Seventeen (17) horizontal mattress sutures of #2-0 Ethibond were then placed with pledgets through the aortic annulus with the pledgets on the ventricular side. Subsequently they were placed through the sewing ring of the valve and the valve sat within the annulus quite satisfactorily. The sutures were secured. The leaflets opened without difficulty and the coronary ostia, that is, both the right and left coronary ostia were visualized and were not encumbered by the valve at all. The aortotomy was then closed in two layers with a running horizontal mattress suture of #4-0 Prolene followed by an over-and-over suture of #4-0 Prolene. Prior to closure of the annular aortotomy, the patient was placed in a steep Trendelenburg position and the de-airing procedure was accomplished in the customary fashion. While retrograde blood cardioplegia was being delivered, the aortic tack was also utilized. Once this was accomplished, the aortotomy was closed and the aortic cross clamp was released after 101 minutes. The rewarming process was continued. This took a while as the patient was overweight. Once the patient was at 37.5 degrees Centigrade and in normal sinus rhythm, she was weaned from cardiopulmonary bypass after a 136-minute average flow of 4.0 liters per minute. Post-bypass transesophageal echocardiogram performed by Dr. Clark from Anesthesia demonstrated good ventricular function. No significant air on the left side of the heart. There was no perivalvular leak and the valve leaflets opened and closed without difficulty. The patient was then decannulated, the purse string sutures secured and heparin reversed with protamine sulfate. Right ventricular pacing wires were placed. The sternum was then approximated with wires after platelet gel was applied. Customary closure was accomplished and a subcuticular closure for the skin. Dry sterile dressings were applied and the patient went to the open-heart recovery unit in satisfactory condition. Pascotto Sample 2 SURGEON: Robert D Pascotto, MD ASSISTANT: Dan Beitelschies, PA. DATE OF PROCEDURE: 11/26/2004 PREOPERATIVE DIAGNOSIS: Unstable angina pectoris secondary to critical multivessel coronary artery disease with totally occluded left anterior descending, status post large anterior myocardial infarction in the distant past, moderately severe left ventricular dysfunction. POSTOPERATIVE DIAGNOSIS: Unstable angina pectoris secondary to critical multivessel coronary artery disease with totally occluded left anterior descending, status post large anterior myocardial infarction in the distant past, moderately severe left ventricular dysfunction. PROCEDURE PERFORMED: Four vessel coronary artery bypass graft surgery (SVG-distal RCA, left radial- obtuse marginal, SVG-diagonal, LIMALAD). ANESTHESIA: General endotracheal anesthesia. OPERATIVE FINDINGS: At the time of operation, the patient's heart had a fibrous scarring around it. As noted above, he had a totally occluded left anterior descending with critical multivessel coronary artery disease. The patient had an intraoperative transesophageal echocardiogram performed by Dr. Ralph Gregg and demonstrated trivial mitral regurgitation that was trivial to mild immediately after termination of cardiopulmonary bypass. The patient went to the open heart recovery unit in satisfactory condition. PROCEDURE DESCRIPTION: After satisfactory general endotracheal anesthesia was accomplished the patient was prepped and draped in the customary fashion. A concomitant incision was made overlying the chest and the left leg. The left saphenous vein was dissected out endoscopically for its full length. The vein was removed from its bed, prepared in the customary fashion, and a layered closure was accomplished in the two small incisions of the leg. The left radial artery was harvested in the customary fashion and incision was made from the wrist to the elbow crease. A pulse oximeter was placed on the index finger of the left hand. It had an excellent wave form as well as 100% saturation prior, during and after the radial artery was harvested. A layered closure was accomplished. A median sternotomy incision was made and the sternum was split. The left internal mammary was dissected out and after heparin was administered, dissected distally, flow was checked and noted to be satisfactory. The pericardium was entered. Aortic cannulation as well as a single, two-stage venous cannula was then inserted and cardiopulmonary bypass was initiated. While the patient was being cooled to 28 degrees centigrade aortic cross-clamp was applied and the patient received 1000 cc of cold blood cardioplegia antegrade. Throughout the crossclamp the patient received intermittent doses of cold blood cardioplegia both antegrade into the aortic root as well as antegrade through the grafts. The distal anastomosis was performed in the following fashion: A reverse segment of the saphenous vein was sutured end-to-side to the distal right coronary artery. The left radial was placed to the obtuse marginal, a second segment of vein to the diagonal and lastly, the left internal mammary artery to the left anterior descending. #7-0 Prolene was used for the construction of the four distal anastomoses. The aortic cross-clamp was released a partial occluding clamp was placed on the ascending aorta and a three proximal anastomoses were performed with #5-0 Prolene. The proximal anastomotic sites were marked with washers. All the areas were checked and with the heart being placed right ventricularly, the patient was weaned from cardiopulmonary bypass without difficulty and with satisfactory hemodynamics. All areas were checked. Hemostasis being achieved, the patient was decannulated, pursestring sutures secured and heparin reversed with protamine sulfate. A left pleural tube, which was a $19 French Blake drain was placed. Two anterior mediastinal tubes were placed. The sternum was approximated with wires. Customary closure was accomplished in a subcuticular closure for the skin. Dry sterile dressings were applied and the patient went to the open-heart recovery unit in satisfactory condition. Pascotto Sample 3 SURGEON: Robert D Pascotto, MD ASSISTANT: Dan Beitelschies, PA DATE OF PROCEDURE: 11/21/2004 PREOPERATIVE DIAGNOSIS: 1. Cardiogenic shock secondary to acute anterior wall myocardial infarction with severe left ventricular dysfunction, pulmonary edema and congestive heart failure with: 2. Severe left main disease. 3. Severe triple-vessel disease. 4. History of hypertension. 5. History of hyperlipidemia. 6. Possible history of diabetes mellitus. POSTOPERATIVE DIAGNOSIS: 1. Cardiogenic shock secondary to acute anterior wall myocardial infarction with severe left ventricular dysfunction, pulmonary edema and congestive heart failure with: 2. Severe left main disease. 3. Severe triple-vessel disease. 4. History of hypertension. 5. History of hyperlipidemia. 6. Possible history of diabetes mellitus. PROCEDURE PERFORMED: 1. Five-vessel coronary artery bypass graft surgery (saphenous vein graft-diagonalleft anterior descending sequential graft, saphenous vein graft-first obtuse marginal-second obtuse marginal sequential graft sequential graft, saphenous vein graft-posterior descending artery) - salvage procedure. ANESTHESIA: General anesthesia. OPERATIVE FINDINGS: After the induction of anesthesia, the patient became more hypotensive and required more pressors. Therefore, cardiopulmonary bypass was instituted without taking down the left internal mammary artery. Upon entering the pericardium, the patient had an infarcted anterior wall with some thinning of the area and collaterals over the left anterior descending, compatible with a previously occluded left anterior descending. All vessels were satisfactory targets for grafting except for the left anterior descending, which was a diffusely diseased vessel and which accepted only the 1-mm probe. The patient came off of cardiopulmonary bypass with the use of the previously placed intraaortic balloon that was placed by Dr. Lee in the catheterization laboratory as well as multiple pressors. He was then taken to the intensive care unit in critical condition. PROCEDURE DESCRIPTION: After satisfactory general endotracheal anesthesia was accomplished, in actuality, the patient had been intubated in the catheterization laboratory because of severe pulmonary edema. In actually, we opened both hemithoraces and he had 1450 cc of pleural fluid in the right hemithorax and 1100 cc of pleural fluid in the left hemithorax, compatible with congestive heart failure. The patient was rapidly prepped and draped in the customary fashion. After the induction of anesthesia, the patient became more hypotensive and required more pressors. Therefore, cardiopulmonary bypass was rapidly instituted without taking down the left internal mammary artery. The pericardium was entered and aortic cannulation as well as a single two-stage venous cannula were inserted and cardiopulmonary bypass was initiated. While the patient was being cooled to 26 degrees centigrade, the coronary arteries were dissected out. A left ventricular vent was inserted through the right superior pulmonary vein as the left heart was dilated from his ischemic cardiomyopathy. A cannula was placed in the coronary sinus for delivery of retrograde blood cardioplegia. The aortic cross-clamp was applied and the patient received 800 cc of cold blood cardioplegia antegrade and another 200 cc of cold blood cardioplegia retrograde into the coronary sinus. Throughout the cross-clamp period, the patient received intermittent doses of cold blood cardioplegia both retrograde into the coronary sinus as well as antegrade in the aortic root as well as antegrade through the grafts. The distal anastomosis was performed in the following fashion: A reverse segment of the saphenous vein was sutured end-to-side to the posterior descending artery. A second segment of reverse vein was sutured end-to-side to the second obtuse marginal and then transversely side-to-side to the first obtuse marginal. A third segment was placed longitudinally side-to-side to the diagonal and end-to-side to the left anterior descending. #7-0 Prolene was used for the construction of the five distal anastomoses. The aortic cross-clamp was released after 68 minutes and then a partial occluding clamp was placed on the ascending aorta and the three proximal anastomoses were performed during the rewarming process. #5-0 Prolene was used for the construction over the proximal anastomotic sites. The sites were marked with washers. Temporary atrial and ventricular pacing wires were placed and with the patient at 38 degrees Centigrade, he had been cooled to 26 degrees, the patient was weaned from cardiopulmonary bypass, AV sequentially paced with the utilization of intraaortic balloon as well as Inocor, epinephrine and Levophed. After a period of observation after the completion of the cardiopulmonary bypass, the patient was decannulated. A purse string suture was secured. It should be appreciated that retrograde warm blood had been delivered right after the institution of cardiopulmonary bypass as well as after the cross-clamp was applied to more adequately perfuse the myocardium while the proximal anastomoses were being constructed. Also, cardioplegia was being given antegrade utilizing an Octopus cardioplegia delivery system into the grafts. Cardiopulmonary bypass was initiated as noted after 132 minutes. All areas were checked. Hemostasis being achieved, the patient was decannulated, a purse string suture secured and heparin reversed with protamine sulfate. A pleural tube was placed into each hemithorax and two anterior mediastinal tubes. The sternum was approximated with wires. Customary closure was accomplished and a subcuticular closure for the skin. It should be appreciated that the left saphenous vein was dissected out for its full length and that was also closed in layers and staples for the skin. Dry sterile dressings were applied and the patient went to the open-heart recovery unit in critical condition.