Aseptic Processing Operation
advertisement
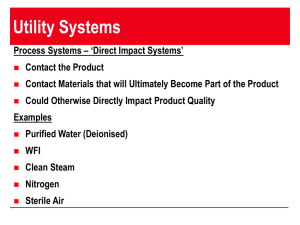
Seminar on Aseptic Processing operation by Ranjith Kumar kankala. M.Pharm (I sem) Department of Pharmaceutics BLUE BIRDS COLLEGE OF PHARMACY Affiliated to Kakatiya university Warangal 2009 Schedule (contents) Introduction to aseptic processing, Aseptic Processing vs. Terminal Sterilization contamination: Sources and control, Microbial environmental monitoring Microbiological testing of air and water Characterization of aseptic process, Media and incubation conditions. Conclusion References Aseptic Processing Aseptic Processing is the processing of drug components ( drug product, containers, excipients, etc.) in a manner that makes impossible of microbiological contamination of the final sealed product. “Sepsis is a serious medical condition characterized by a whole-body inflammatory state caused by infection.” Progression of Symptoms Fever Decreased Blood Pressure Rapid Breathing and Heart Rate Skin Lesions Spontaneous Blood Clotting Organ Failure Death Causes of sepsis Sterile drug manufacturers should have a keen awareness of the public health implications of distributing a non-sterile product. Poor cGMP conditions at a manufacturing facility can ultimately pose a life-threatening health risk to a patient.” Asepsis is the practice to reduce or eliminate contaminants (such as bacteria, viruses, fungi, and parasites) from entering the field to prevent infection. Ideally, a field is "sterile" — free of contaminants — a situation that is difficult to attain. However, the goal is elimination of infection. Producing drug products by Terminal sterilization Aseptic processing Product containers are filled and Drug product, container, and sealed under high-quality environmental conditions designed to minimize contamination, but not to guarantee sterility. Product in its final container is subject to a sterilization process such as heat or irradiation. closure are subject to sterilization separately, and then brought together. Because there is no process to sterilize the product in its final container, it is critical that containers be filled and sealed in an extremely high –quality environment. Terminal Sterilization Drug Product Container / Closure Excipiants Sterilization Process Sterile Drug Product ! Aseptic Processing Drug Produc t Sterilization Process Container Sterilization Process Sterile Drug Product Sterile Container Closur e Sterilization Process Sterile Closure Excipient Sterilization Process Sterile Excipient Aseptic Processin g Sterile Final Product Can use multiple sterilization processes each optimized for the individual component Contaminating agents Bacteria, virus, fungi and other viable microbes cause a serious contamination. Bacterial spores and endotoxins Non viable Particles like dust, fibers, or other material are suspended in the air and may contaminate product. Humans and bacteria Over 200 different species of bacteria are found associated with humans. Bacteria are found in the intestines, eyes, nares, mouth, hair and skin. Dry skin can have 1000’s of microbes / mm2 ! Staphylococcus epidermidis Scanning EM. CDC. Sources of Contamination: Personnel born contaminants Poor or improper Sanitization: Procedures deficient, or poorly executed Air born contaminants. Inadequate HEPA seal (over 90% vials contaminated) Velocity through HEPA Filters: Variable velocities between filters. Inadequate laminar flow resulted. Low or undetectable velocity at work surface. Mechanical failure of filling tank; main pump failure; cooling system leaks at joints. Control 1st step – eliminating the source of contamination ! 2nd Step - Reduce the Risk of contamination through: Sterile barriers Surface monitoring Aseptic technique Gowning (sterile barrier) If people are a major source of contamination we avoid contaminating the product while we process it. Surface Monitoring Touch or Contact plates - RODAC Plates (Replicate Organism Detection and Counting) Swabs Aseptic Technique (skill) Contact sterile materials only with sterile instruments: Operators should not contact sterile products, containers, closures, or critical surfaces with any part of their gown or gloves Keep the entire body out of the path of unidirectional airflow Approach a necessary manipulation in a manner that does not compromise sterility of the product What’s wrong with this picture? CORRECT Unidirectional airflow The operator should never come between the air source and the product. pressure differential b/n critical area from external environment (17.5-50 Pa) www.ors.od.nih.gov/ds/pubs/bsc/graphics/fig3.gif Horizontal airflow Vertical airflow Disinfectants ISOPROPYL ALCOHOL (70%) Powerful disinfectant Effectively kills bacteria and fungi Mode of action: denatures proteins, dissolves lipids and can lead to cell membrane disintegration. But does not inactivate spores! e.g., phenols, Alcohols, Aldehydes etc., Sporicidal agents Glutaraldehyde Formaldehyde sodium hypochlorite Iodine and iodophors Peroxygens Ethylene oxide P- Propiolactone Isolators Advantage: No direct contact between operator & product. Microbial Environmental Monitoring: Identification Microbial identification should extend to the species level. Routine traditional techniques phenotypic and biochemical. Genotypic techniques are suggested for failure investigations. Identifying Microbes Phenotypic technique Gram Stain Biochemical Assays Reduction of Tetrazolium Violet Staphylococcus xylosus Genotypic Methods Use DNA sequence (often ribosomal RNA genes rDNA) to identify organism Faster, and more accurate then traditional biochemical and phenotypic techniques QC Micro: Identifying Microbes Genotype Based Assay: PCR: Polymerase Chain Reaction Endotoxin Testing Endotoxin: a pyrogenic (fever inducing) substance (e.g. lipopolysaccharide) present in the bacterial cell wall. Endotoxin reactions range from fever to death. LAL Assay (Limulus amoebocyte lysate) ENDOTOXIN LIMIT FOR WFI IS 0.25 EU/ml Extremely heat stable – recommended conditions for inactivation are 180 0 C for 3 hours. Microbiological testing of water Universal solvent ,Used as Vehicle and used to rince and cleaning of apparatus Water should also be tested for presence of coliforms and/or pseudomonads if appropriate (may cause biofilm) Water should be tested using R2A agar (low nutrient for the recovery of water borne organisms) incubated for at least 5 days at 30-35°C Sampling procedures should follow those used in production Microbiological testing of air Compressed Air/Nitrogen/CO2 Air sampling should be done and tested for the presence of non-viables and viables by exposure to the environment. Pressure control orifices should be used to provide a steady stream of air. Fall out plate Slit sampler (slit-to-agar sampler) Slit Sampler (New Brunswick Scientifics Model STA-230 Slit-to-Agar Air Sampler.) Characterization of aseptic process The four pillars of a robust * aseptic process Personnel training & monitoring Environmental monitoring Facilities design Media fills Personnel Training & Monitoring Avoiding contamination means knowing the potential sources of contamination Personnel Equipment Air/liquids Drug product Containers/closures Outside environment Anything Brought in contact with, or in the vicinity of, the product is a potential source of contamination! Environmental Monitoring The goal of the environmental monitoring program is to provide meaningful information on the quality of the aseptic processing environment during production as well as environmental trends. Environmental Monitoring Sampling 7. Critical (processing) areas 6. 8. Sampling of adjacent classified areas (aseptic corridors, gowning rooms, etc) will provide trend data and may help identify sources of contamination. 4. 3. 5. 13. 10. 9. 12 . 11. 2. 1. Facilities: General Clean room Design HEPA/ULPA filters on ceiling Exhaust vents on floor Airlocks and interlocking doors to control air balance Seamless and rounded floor to wall junctions Readily accessible corners Floors, walls, and ceilings constructed of smooth hard surfaces that can be easily cleaned Limited equipment, fixtures and personnel Layout of equipment to optimize comfort and movement of operators Facilities: Clean room Classification FS209 ISO 14644-1 Cleanroom Cleanroom classification classification ≥0.5um particles/m3 Viable Microbes (cfu/m3) Ave Airflow Velocity (fpm) Air changes/hr 100,000 8 3,520,000 100 5-10 5-48 10,000 7 352,000 10 10-15 60-90 1000 6 35,200 7 25-40 150-240 100 5 3,520 1 40-80 240-480 Facilities: Clean room Classification Class 10,000 clean room Class 100 clean room http://www.americancleanrooms.com/am/photogallery_08.html Facilities: HEPA Filters High Efficiency Particulate Air filters Minimum particle collection efficiency: 99.97% for 0.3µm diameter particles. Disposable Filter made of pleated borosilicate glass http://people.deas.harvard.edu/~jones/lab_arch/nano_facilities/hepa.gif Media Fill test Used to validate the aseptic process Use microbial growth media instead of drug product-any contamination will result in microbial growth. It doesn’t provide a direct relation for sterility but gives an adequate evaluation for operational processing steps. Media and Incubation conditions Soybean casein digest medium (SCD) Fluid thioglycollate medium (FTM) for anerobes Inoculated with < 100 cfu challenge At least 14 days incubation 30-35°C for SCD, 20-25°C for FTM temperatures should be monitored product produces suspension, flocculation or deposit in media, suitable portions (2-5%) should be transferred to fresh media, after 14 days, and incubated for a futher 7 days Theoretical Evaluation Whyte mathematical model contamination is due to air borne microbes Cont rate (c) = 0.0032.d2.A.t d = equivalent particle diameter A= area of container opening (cm2) t = time (sec) PostScript (conclusion) The challenge in aseptic processing is always personnel: As a source of microbial and Particle contamination. As a brake on the implementation of Improved technology. REFERENCES Encyclopedia of pharm.technology RUSSELL A. D.. Bacterial Spores and Chemical Sporicidal Agents. clinical microbiology reviews. 3(2): 99-119 (1999) . http://www.fda.gov/cber/gdlns/steraseptic.pdf http://www.emedicinehealth.com/images/4453 http://pathmicro.med.sc.edu/fox/lps.jpg http://micro.med.harvard.edu/faculty/rudner.html ThanQ