Clinical Genotyping of Lung Cancer
in the Era of Personalized Medicine
Laura J. Tafe, MD
Assistant Professor of Pathology
Assistant Director, Molecular Pathology
CTOP Retreat May 23, 2014
Overview
• Overview of molecular workflow
• NGS 50 gene panel experience
• Mass spec ALK project
Histology matters
Lung Cancer Histology
Adenocarcinoma
Squamous cell
carcinoma
Large cell
carcinoma
Small cell
carcinoma
Any primary lung cancer with adenocarcinoma histology
May be mixed (ADC-SQC, ADC-SCLC)
No pure SQC, SCLC or neuroendocrine
Poorly differentiated tumors should be tested
Pre-analytical Workflow
Molecular testing ordered by
surgical pathologist
2 H&E and 10 USS
MG Pathologist review of H&E for adequacy
and % tumor
1 H&E and 2 USS to FISH lab
to hold for additional
testing as needed
(rearrangements by FISH)
DNA extracted from USS in
molecular laboratory for PCR
NGS (Analytical) Workflow
Sample
Preparation
Library
Preparation
Emulsification
and Enrichment
DNA Extraction
-minimum tumor
cellularity: 10%
-8 unstained slides
PCR
AmpliSeq
HotSpot Cancer
Panel
• 201 amplicons
• 50 genes
• Require 10ng
DNA
Emulsification PCR
Clonal amplification of
DNA on Ion Spheres
(ISP’s)
DNA
Quantification
PicoGreen Method
Sequencing and
Data Analysis
318 IonChip
Majority of amplicon
coverage >500X
•
Variant Calling
Ion Torrent Variant
Caller Plugin
Reference genome:
hg19
•
ISP’s quantification
•
Enrichment of ISP’s with
DNA
FuPa Treatment
•
•
Barcode Adaptor
Ligation
Data Annotation, Review
and Sign-out
Library
Quantification and
Pooling
(qPCR)
Total time: ~9h
Hands on time:
~3h
Total time: ~8h
Hands on time:
~4h
Day 1-2
Day 3-4
Reporting
Golden Helix SVS
Software
Variant Call Summary
Variant Prediction
Total time: ~7h
Hands on time: ~1h
Day 5
Total time: ~14h
Hands on time: ~5h
Courtesy of F. de Abreu
Day 6-7
Ion Torrent Technology
• Simple, robust, scalable and cost effective.
Low cost+, convenient,
single use device.
Easy, automatic fluid connections.
Match the size of the Ion chip to your
application.
AmpliSeq Cancer Hotspot Panel v2
Single pool of primers
• 207 Primer Pairs
• 50 Genes
• 10 ng input DNA
Targets genomic "hot spots“
1 year: ~ 500 clinical samples
+ ~ 100 research samples
Weekly run: ~ 20 samples
TAT: 7 days (samples in the
lab)
ABL1
EGFR
GNAS
KRAS
PTPN11
AKT1
ERBB2
GNAQ
MET
RB1
ALK
ERBB4
HNF1A
MLH1
RET
APC
EZH2
HRAS
MPL
SMAD4
ATM
FBXW7
IDH1
NOTCH1
SMARCB1
BRAF
FGFR1
IDH2
NPM1
SMO
CDH1
FGFR2
JAK2
NRAS
SRC
CDKN2A
FGFR3
JAK3
PDGFRA
STK11
CSF1R
FLT3
KDR
PIK3CA
TP53
CTNNB1
GNA11
KIT
PTEN
VHL
Post-analytical Workflow
Analysis Pipeline:
Variant-Calling and Annotation
Run Variant
Caller Version
4.0
Upload VCF
File to Golden
Helix SVS
(Version 7.7.8)
and Annotate
Variants
FILTER
Non-Coding
Variants
FILTER
Synonymous
Variants
FILTER
<5% SNVs
<20%INDELS
Review
Remaining
Variants in IGV,
FILTER
Homopolymeric
Variants and
Sequencing
Artifacts
Variant calls and annotation:
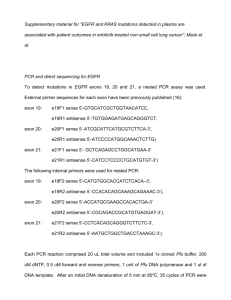
• Initially filtered to remove non-coding and synonymous mutations.
• Golden Helix then used to annotate and help predict pathogenicity.
• All reported variants received sufficient coverage and were of high
enough frequency to be annotated as true variants.
Report
Remaining
Variants To
Clinicians
EGFR Exon 21 p.L858R (c.2573T>G)
EGFR Exon 19
18bp deletion
Example report
INDICATION FOR STUDY: Lung, right (CT-guided needle core biopsy): Adenocarcinoma
SPECIMEN ANALYZED: Cytology or surgical #, Block #
Analysis: Examination of DNA extracted from formalin-fixed paraffin-embedded tumor tissue for somatic mutation
analysis.
Results:
The following gene variants were identified in the submitted tissue:
CLINICALLY ACTIONABLE:
BRAF:
NORMAL
EGFR:
MUTATION
KRAS:
NORMAL
PIK3CA:
NORMAL
NOT CLINICALLY INDICATED:
TP53
c.421C>T
c.2573T>G p.L858R
p.R141C
Exon 21
Exon 4
Interpretation: After review of the pathology report and slides, the specimen (N-14-00257, Block A2) was selected
for mutation analysis from a panel of 50 genes. The results of this test indicate that tumor cells comprising 25.0%
of the tissue specimen analyzed were normal for BRAF, KRAS and hotspots in 46 other genes. A p.L858R activating
mutation was detected in exon 21 of the EGFR gene suggesting that this patient may benefit from anti-EGFR
therapy. In addition, a mutation of unknown clinical significance was detected in the TP53 gene. Therapeutic
options related to the presence or absence of mutations should be carefully assessed. Availability of other
therapeutic indications and clinical trials may be possible.
For additional information on reported variants please visit:
http://www.mycancergenome.org/content/disease/lung-cancer
203 non-squamous NSCLC cases
on Ion Torrent AmpliSeq Hotspot
Panel v2
(May 2013 – May 2014)
Specimen types tested
Resection: 24%
Cell Block: 33%
Consult: 13%
Needle Core: 30%
Types of Mutations
QNS: 8%
Wild Type: 13%
Actionable: 48%
VUS: 31%
EGFR
KRAS
BRAF
ERBB2 ins
PIK3CA
Most Frequent Mutations
Other: 16%
KRAS: 30%
STK11: 10%
EGFR: 12%
TP53: 32%
Other = Mutations in 32 additional genes were seen in 1-7 cases each
Uncommon mutations
• EGFR
– 2 – Exon 20 insertion (1%)
– 3 – Exon 18 (1.5%)
– 3 – T790M (1.5%)
• BRAF
– 7 mutations (only 3 - V600E) (3%)
• ERBB2
– 2 – exon 20 insertion (1%)
• PIK3CA
– 9 mutations (4%)
Limitations of AmpliSeq
• CNVs
• Structural variants (rearrangements/translocations)
• mRNA
Quantification of ALK from Formalin-Fixed Paraffin-Embedded
Non-small Cell Lung Cancer (NSCLC) Tissue by Mass Spectrometry
Christopher P. Hartley 1, Wei-Li Liao2, Jon Burrows2,
Todd Hembrough2, and Laura J. Tafe1
1Department of Pathology, Dartmouth-Hitchcock Medical Center,
Lebanon, NH and 2OncoPlex Diagnostics, Rockville, MD
Selected Reaction Monitoring (SRM) - MS
ALK exons
SRM peptide
(outside KD)
5’ NH2
3’ COOH
Wang R et al. Clin Cancer Res 2012;18:4725-4732
11 samples from 10 patients
(6 with ALK rearrangement)
Heterozygous Single Nucleotide Point Mutation in ALK for DH9
(ALK kinase domain: 1116-1392, peptide 1417D P E G V P P L L V S Q Q AK1431 is C-terminal to the KD)
Heterozygous (T in one allele and G in the other)
C0483-T2LR-C (DH9)
Heterozygous G/T results in DPEGVPPLLVQQAK (WT) from one allele and
DPEGVPPLLVSQ*AK (Q to stop codon*) in the second allele introducing a
stop codon (p.Q1429X) within the MS targeted peptide (missing aa 14291620).
Homozygous (G in both alleles)
C0481-T2LR-C (DH1)
Homozygous G results in DPEGVPPLLVQQAK (WT) from both DNA alleles.
Crizotinib resistance in ALK-positive
lung cancer
Shaw. JCO. 2013. 31(8):1105-1111
Hypothesis: Missing 192aa might alter
the function of the ALK fusion protein
and response to ALK inhibitors
Stage
68
Smoking hx
Non-smoker (3 pyr;
40 yrs prior)
Progression free
survival
pT2a N2
7 mos + (?)
NED - lost to f/u
M
54
Never smoker
pT2a pN2
14 mos
NED
DH3
F
49
pT1a N2
19 mos
DH4
M
76
stage 4
12 mos
NED
AWD -Stable brain
met
DH5/6
M
62
pT2b pN1
no crizotinib tx
NED
DH9
M
65
Never smoker
Former (stopped 40 pyr)
Never smoker
(second hand
smoke exposure
22 yrs)
Smoker
(quit 1 yr ago)
pT2 pN1
4 mos
AWD
DH#
M/F
Age at dx
DH1
F
DH2
Status
Conclusions
• The Ion Torrent Ampliseq technology:
Successfully performed on small biopsy / cytology
specimens
Requires very little input DNA (10ng)
• Mass Spectrometry proteomic techniques are
complementary to molecular analysis and
have potential to identify clinically meaningful
biomarkers