PDF hosted at the Radboud Repository of the Radboud University
Nijmegen
The following full text is a publisher's version.
For additional information about this publication click this link.
http://hdl.handle.net/2066/91314
Please be advised that this information was generated on 2015-01-31 and may be subject to
change.
Persistent m edically unexplained sym ptom s
in primary care
The patient, the doctor and the consultation
T im C. o ld e H artm an
Colophon
This thesis has been prepared by the D epartm ent of Prim ary and C om m unity Care of the Radboud U niversity Nijmegen
Medical Centre, the Netherlands. The Departm ent of Prim ary and Com m unity Care participates in the N etherlands School
of Prim ary Care research (CaRe), w hich has been acknowledged by the Royal N etherlands Academy of Arts and Sciences
(KNAW) in 1995.
Design:
Joost Perik
Photo W aal Bridge:
Edw in H obert (ww w .edw inenleonie.nl)
Penrose triangle:
by Oscar Reutersvärd, 1934
Layout:
Joost Perik
Digital version of thesis:
Tables:
Joost Perik, by an idea of Fons v an Bindsbergen
QR-code:
Lea Peters
Print:
Ipskam p Drukkers, Enschede (w w w .ipskam pdrukkers.nl)
ISBN:
978-94-91211-99-7
Financial support
This thesis w as made possible by grants of:
-
ZonM w (the N etherlands O rganization for H ealth Research and Developm ent, grant no. 920-03-339)
-
D epartm ent of Prim ary and C om m unity Care, R adboud U niversity Nijmegen Medical Centre
-
SBOH, em ployer of general practitioner trainees
SBCH—
ZonMw
Nijmegen, 2011
Copyright
© T.C. olde H artm an, Nijmegen, the N etherlands, 2011. All rights reserved. No part of this book m ay be reproduced or
transm itted in any form, by print, photo print, microfilm or otherwise, w ithout prior w ritten perm ission of the holder of the
copyright.
Niets uit deze uitgave m ag w orden verm enigvuldigd e n /o f openbaar gemaakt door m iddel van druk, fotokopie,
microfilm, of w elke andere wijze dan ook, zonder schriftelijke toestem m ing van de auteur.
Persistent m edically unexplained symptoms
in primary care
The patient, the doctor and the consultation
E en w etenschap p elijk e p ro ev e op h et gebied v a n de
M edische W eten sch ap p en
Proefschrift
te r v erkrijg in g v a n de g raa d v a n doctor
aa n de R ad b o u d U n iv ersiteit N ijm egen
op gezag v a n de rector m agnificus prof. m r. S.C.J.J. K ortm ann,
volgens b eslu it v an h et college v an decanen
in h et o p en b a ar te v e rd e d ig e n op d o n d e rd a g 13 o k to b er 2011
om 13.00 u u r precies
door
Tim Christian olde Hartman
g eboren op 13 m a a rt 1977
te Alm elo
Promotor:
Copromotoren:
D hr. prof. dr. C. v a n W eel
D hr. dr. P.L.B.J. Lucassen
D hr. dr. H .C.A.M . v a n Rijswijk
Manuscriptcommissie:
M w . prof. dr. A.E.M. Speckens (voorzitter)
D hr. prof. dr. B.G. v a n E ngelen
D hr. prof. dr. C.F. D ow rick (U niversity of L iverpool, Liverpool)
Paranimfen:
D hr. drs. H.J. M eijerink
M w . dr. L.J.A. H assink-F ranke
Contents
Chapter 1
G eneral In tro d u c tio n
8
based on H uisarts W et. 2007;50(1):11-5
T he p a tien t
Chapter 2
C hronic fun ctio n al som atic sym ptom s: a single sy ndrom e?
26
B r J Gen Pract. 2004;54(509):922-7
Chapter 3
M edically u n ex p lain e d sy m p to m s, so m atisatio n d iso rd er an d
42
h ypochondriasis: course a n d p rognosis. A system atic review
J Psychosom Res. 2009;66(5):363-77
Chapter 4
The d o cto r-p atien t relatio n sh ip fro m th e p ersp ectiv e of p atien ts
68
w ith p ersisten t m edically u n ex p lain e d sy m p to m s. A n interview
stu d y
subm itted
T he doctor
Chapter 5
E xplanation an d relations. H ow do g eneral p ractitio n ers deal
86
w ith p atien ts w ith p ersisten t m edically u n ex p lain ed sym ptom s:
a focus g ro u p stu d y
B M C Fam Pract. 2009;10:68
T he co n su lta tio n
Chapter 6
'W ell doctor, it is all a b o u t h o w life is lived': cues as a tool in
106
th e m edical co n sultatio n
M e n t H ealth Fam M ed. 2008;5:183-7
Chapter 7
H ow p atien ts an d fam ily p h y sician s co m m u n icate ab o u t
p ersisten t m edically u n ex p lain e d sym ptom s. A q u alitativ e
stu d y of v ideo -reco rd ed co n su ltatio n s
P atient Educ Couns. 2011; A p r 7. [Epub ahead o f print]
116
S tartin g p o in ts for im p r o v in g m an a g em en t
Chapter 8
E xperts' opin io n s o n th e m a n ag em en t of m edically u n ex p lain e d
136
sym p to m s in p rim a ry care. A q u alitativ e analysis of n arrativ e
review s a n d scientific ed itorials
Fam Pract. 2011;28(4):444-455
Chapter 9
E xplanatory m odels of m edically u n ex p lain e d sym ptom s: a
162
qualitative analysis of the literatu re
M e n t H ealth Fam M ed. 2010;7:223-31
Chapter 10
M edically u n ex p lain e d sy m p to m s in fam ily m edicine: d efin in g
180
a research agenda. P roceedings fro m W O N C A 2007
Fam Pract. 2008;25(4):266-71
Chapter 11
G eneral D iscussion
196
Summary / Samenvatting
218
Dankwoord
234
List of publications
242
Curriculum Vitae
252
10 I Chapter 1
M edicine is n o t o nly a science; it is also an art. I t does n o t consist o f com pounding pills and plasters; it
deals w ith the very processes o f life, w hich m u st be understood before they m ay be guided. (Paracelsus (c.
1493-1541))
General introduction | 11
Background
P hysical sy m p to m s su ch as h eadach e, back pain , dizzin ess a n d fatig u e are com m o n in the
general p o p u latio n . Tw o th ird s of m en a n d fo u r fifth of w o m en re p o rt a t least on e physical
sy m p to m in th e last tw o w eeks.1;2H o w ev er m o st p eo p le do n o t contact pro fessio n al m edical care
for these sy m p to m s.3;4W hen peo p le contact th eir G eneral P ractitio n er (GP) for th ese sy m p to m s
80% rem a in restricted to one d o cto r-p atien t contact,5 su g g estin g th a t m o st of these sy m p to m s
are transient.
In ab o u t 25-50% of all sym p to m s p rese n ted in p rim a ry h ea lth care, no evidence can be fo u n d for
an u n d e rly in g physical disease, an d sh o u ld be co n sid ered as m edically u n ex p lain e d sy m p to m s
(MUS).6;7 In specialist care these p ercen tag es are ev en higher, ra n g in g fro m 30-70%.8;9 MUS
u su ally d isa p p ea r sp o n ta n eo u sly in th e course of tim e or as a consequence of th e p hysician's
m anagem ent. A recent D u tch s tu d y fo u n d th a t o nly 2.5% of th e p atien ts in g eneral practice
p rese n tin g w ith m edically u n ex p lain e d sy m p to m s m eet criteria for ch ronicity.“ H o w ev er, this
m inority rep rese n t a maj or p ro b lem in h ea lth care for th e fo llo w in g reasons:
a. p atien ts w ith persisten t MUS suffer fro m th eir sy m p to m s, are fu n ctio n ally im p aired , a n d
are at risk for poten tially h arm fu l a d d itio n a l te stin g a n d treatm ent;
b. these p atien ts are a b u rd e n for th e h ea lth care sy stem as th ey are resp o n sib le for high,
often unnecessary, h ea lth care costs;
c. p atien ts w ith persisten t MUS are often d issatisfied w ith th e m edical care th ey receive
d u rin g th eir illness;
d. these p atien ts often cause feelings of fru stra tio n an d irritatio n in th eir physicians; an d
e. th e suitability, applicability a n d effectiveness of specific in te rv en tio n s to w ard s p atien ts
w ith persisten t MUS in p rim a ry care are lim ited.
The p roblem s described above are at the basis of the stu d ies re p o rte d in th is thesis, w h ich
to g eth er aim ed at g aining m ore in sig h t into th e care p atien ts w ith p ersis ten t MUS expect
(the patient), th e w ay G Ps experience th e care th ey d eliv er for th ese p atien ts (the doctor) a n d the
care G Ps deliver d u rin g en co u n ters w ith these p atien ts (the consultation) in o rd er to g u id e n ew
in te rv en tio n strategies for these patients.
Confusing terms
D efinitions in literature
In the scientific literatu re there is d iscu ssio n a n d d ebate for the b est te rm to describe physical
com plaints of p atien ts w h e n the aetiology is unclear. L ipow ski d efin ed som atisation as the
tendency to experience a n d com m unicate psychological d istress in the fo rm of som atic
1
12 I Chapter 1
sym p to m s th a t th e p a tie n t m isin te rp rets as signifying serio u s physical illness.11 In DSM-IV
som atisation disorder is defin ed as a histo ry of m an y ph y sical co m p lain ts (four p a in sym ptom s,
tw o g astro in testin al sym ptom s, one sexual sy m p to m a n d one p seu d o n eu ro -lo g ical sym ptom )
b eg in n in g before th e age of 30 th a t occur o ver a p erio d of sev eral years. E scobar in tro d u c e d the
concept of abridged som atisation, a con stru ct for less severe fo rm s of so m atisatio n ch aracterized
by fo u r or m ore u n ex p lain e d physical sy m p to m s in m en an d six or m o re u n ex p lain e d physical
sym p to m s in w om en.12 In fu n ctio n a l som atic syndrom es a set of u n ex p lain e d sy m p to m s is
clustered into a syndrom e. In th is w ay each m edical specialty h as his o w n fu n ctio n al som atic
syndrom e. For exam ple C hronic F atigue S y n d ro m e (CFS) in in tern al m edicine, Irritable Bowel
S y ndrom e (IBS) in g astroenterology an d F ibrom yalgia (FM) in rh eu m ato lo g y . In N ijm egen the
te rm chronic nervous fu n ctio n a l somatic sym ptom s h as b een d ev elo p ed .13 P atien ts m eet this
diagnostic category w h e n th ey rep e ate d ly p rese n t ph y sical sy m p to m s th a t rem a in m edically
u n ex p lain e d after ad e q u ate exam ination, in co m b in atio n w ith th e (presu m ed ) presen ce of
psychosocial p roblem s or psychological distress. This d iagnostic category has b ee n in c lu d ed in
th e C o n tin u o u s M orbidity R egistry (CMR) sy stem w h ich w as in tro d u c ed by th e N ijm egen
D ep a rtm en t of Fam ily M edicine in 1971.13-16T o o u r k n o w led g e, th e CM R is th e only classification
system w ith a se p arate category for p atien ts w ith p ersisten t MUS. In a fu rth e r elab o ratio n of
chronic n erv o u s-fu n ctio n al sym ptom s, th e th eo ry of 'som atic fixation' w as dev elo p ed . Somatic
fixa tio n is th e consequence of co n tin u o u s o n e-sid ed em p h asis on th e som atic aspects of
sy m p to m s a n d h ea lth p roblem s resu ltin g in p eo p le beco m in g m o re an d m o re e n tan g led in and
d e p e n d e n t of h ea lth care.17;18This th eo ry explicitly ack n o w led g es th e role of th e p h y sician in the
d ev elo p m en t of p ersisten t MUS.
Which term w ill w e use in this thesis?
A n u m b e r of term s a n d definition s are u se d for p ersisten t sy m p to m s w ith o u t obvious
pathology. Som atisation has b een criticized, as it su g g ests th a t ph y sical sy m p to m s o rig in ate from
psychosocial distress. F u rth erm o re th is te rm assu m es p ath o g en ic p rocesses a n d tendencies,
such as illness b eh av io u r, o n th e p a rt of th e p atien t, w ith o u t co n sid erin g at all th e role of the
physician.19 C oncerning fu n ctio n a l somatic syndrom es, research ers arg u e th a t th e existing
definitions of these in d iv id u a l sy n d ro m es are of lim ited v alu e because: (1) th e su b stan tial
overlap b etw e en the in d iv id u a l sy n d ro m es a n d (2) th e sim ilarities b etw een th e m o u tw eig h the
differences.20F u rtherm ore, th e re is som e co n fu sio n reg a rd in g its core concept as it m ay refer to a
fun ctio n al distu rb an ce of org an s or th e b ra in sy stem s or it m ay refer to th e fu n ctio n of sym p to m s
w ith in the fra m ew o rk of seco n d ary gain.21 This also ap p lies for th e te rm chronic nervousfu n ctio n a l som atic sym ptom s. It has b een criticized for su g g estin g (1) th e tran slatio n of m ental
distress into physical sym ptom s, (2) th e im p licatio n th a t p atien ts h o ld o n to som atic a ttrib u tio n
of sym ptom s, a n d (3) a 'function' of th e sy m p to m s in ex p ressin g psychological d istress.22
H ow ever, a lth o u g h doctors m ay th in k th e te rm 'functional' is pejorative, p atien ts do n ot
General introduction | 13
perceive it as such.23 The te rm p ersistent m edically unexplained sym ptom s h as g ain ed p o p u la rity
d u rin g recent y ears am o n g general p ractitio n ers. A lth o u g h it defines p atien t's sy m p to m s by
w h a t they are n ot, rath e r th a n b y w h a t th ey are, an d a lth o u g h it reflects dualistic th in k in g , this
te rm is p u re ly descriptive an d th e m o st n e u tra l as it does n o t in d icate an u n d erly in g causal
m echanism or in te rp re tatio n .24H ow ev er, it has n eg ativ e co n n o tatio n s for p atien ts.23
These v ario u s term s a n d definitions reflect th e d ifficulties in th e concept of u n ex p lain e d bodily
com plaints w h ich is n o t u n equivocally d efined.25 A s a consequence of co n cep tu al problem s
d o cto r-p atien t com m unication a n d sy m p to m ex p lan atio n d u rin g co n su ltatio n is h am p ered .23
F urth erm o re, it com plicates research in th is p o p u la tio n as a a p p ro p ria te selection of th e stu d y
p o p u la tio n , a accurate definition of reference sta n d a rd s a n d a u sefu l d efin itio n of outcom e
m e asu res are lacking.26
In the light of the foregoing, w e d ecid ed to use th e te rm persisten t m edically unexplained sym ptom s
(p ersistent MUS) in this thesis, because w e th in k th is is th e m o st n e u tra l te rm a n d because this
te rm is w id ely accepted in to d a y 's scientific co m m u n ity a n d in p rim a ry ca re.
The patient, the doctor and the consultation
In 1979 researchers of the d e p a rtm e n t of Fam ily M edicine of th e R ad b o u d U n iv ersity N ijm egen
M edical C entre in th e N eth e rlan d s sta rte d a stu d y of som atic fixation.17This stu d y cu lm in ated in
th e book ' To heal or to harm. The prevention o f somatic fixa tio n in general practice' by R ichard G rol et
al.18 The concept of som atic fixation co nnected a th eo ry of h ea lth a n d illness w ith c o n su ltatio n
skills. Som atic fixation assum es a ten d en cy w ith in p atien ts to p ersisten tly experience
sym ptom s, freq u en tly as a consequence of psychological problem s. P atien ts w h o are inclined
to w ard s som atic fixation also te n d to in a d eq u a te h elp seeking b eh a v io u r a n d d ep en d en ce on
h ea lth care professionals. The re su lt of th ese ten d en cies is th a t th e p a tie n t focuses o n his or her
b o d y an d denies the relatio n b etw e en b o d ily sy m p to m s a n d psychosocial problem s.
A ccording to th a t theory, th e G P has p o w erfu l tools to p re v e n t som atic fixation an d w ith it
p ersisten t MUS. These tools - co n su ltatio n an d co m m u n icatio n skills - com p rise a goal-oriented
a n d system atic ap p ro ach , effective m a n ag em en t of th e d o cto r-p atien t relatio n sh ip an d
ad e q u ate tre a tm e n t of b o th som atic a n d psychosocial sy m p to m s. H o w ev er, d esp ite th e u se of
these tools, a sm all gro u p of p atien ts en d s u p w ith p ersisten t MUS. R esearch o n th e m an ag em en t
by G Ps of those functionally im p a ired an d su fferin g p atien ts an d reg a rd in g th e care these
p atien ts expect is still lim ite d .
14 I Chapter 1
E laborating o n the theory of som atic fixation a n d th e role of th e p atien t, th e d octor an d the
co n su ltatio n w e w ill (1) explore the k n o w led g e reg a rd in g th e p ro b lem s arisin g w h e n G Ps m eet
p atien ts w h o have d evelo p ed p ersisten t MUS in daily practice, a n d (2) in d icate k n o w led g e gaps
reg a rd in g the care G Ps deliver a n d the care p atien ts expect w h e n en c o u n te rin g w ith p ersisten t
MUS.
The patient
P atients w ith p ersisten t MUS often h av e the feeling th a t doctors do n o t ackn o w led g e the
legitim acy of th eir sym ptom s, a n d th a t th ey co n stan tly h av e to o p p o se th eir doctor's
skepticism .27 M any p atien ts feel th a t th eir doctors label th em as 'psychological cases'.28;29
F u rtherm ore, p atien ts have th e feeling th a t G Ps d o n 't take th e m serio u sly because G Ps o ften tell
th e m 'it is n o th in g ' or 'you do n o t have a disease'.27;30'33
P atients w ith distin ct fun ctio n al sy n d ro m es are o ften dissatisfied w ith the m edical care th ey
receive d u rin g their illness.28;34 They sense th e n ee d to fig h t to gain reco g n itio n a n d acceptance
fro m th e ir GP. O ften, these p atien ts co n sid er th eir d octor in co m p eten t an d them selv es as
experts reg a rd in g their o w n sym ptom s.35P atien ts w ith p ersisten t MUS u se strateg ies to keep u p
m edical atten tio n w h e n they m eet an atm o sp h ere of d istru st in the co nsultation. These include
so m atizin g (i.e. p ersistin g in b odily explanations), claim ing u n d e r cover (i.e. referrin g to other
au th o rities such as TV or a n eig h b o u r w h o is a doctor), an d p le ad in g (crying a n d begging) to
catch th e d octor's interest.32;36
Which care do patients with persistent MUS expect?
The freq u en tly ex pressed dissatisfactio n by p atien ts w ith th e m edical care received d u rin g
illness m ig h t o rig in ate fro m the m ism atch b etw e en w h a t p atien ts w a n t a n d w h a t th ey actually
receive fro m their GP. A nalysis of v id e o ta p e d co n su ltatio n s sh o w ed th is m ism atch clearly
d u rin g th e initial p rese n tatio n of MUS in p rim a ry care. Salm on et al. sh o w ed th a t p atien ts w ith
MUS w ish to have a convincing, legitim atin g a n d e m p o w erin g ex p lan atio n for th eir sym p to m s
w hich, u n fo rtu n a te ly , is n o t given by th e ir GP.37-40 F u rth erm o re th ey in d icated th a t th ey w a n t
m ore em otional s u p p o rt fro m th eir G P.30 H o w ev er, research to w ard s preferen ces of p atien ts
w ith persisten t MUS reg a rd in g th e care th ey expect a n d receive in p rim a ry care is still lacking.
The doctor
R esearch p o in te d o u t th a t d octors o ften experience p atien ts w ith p ersisten t MUS as difficult to
m anage.27;41 F urth erm o re, th ey indicate th a t effective m a n ag em en t strateg ies are lacking.42 In
fact, m a n y GPs th in k th a t p ersisten t MUS are asso ciated w ith p erso n ality or psychiatric
diso rd ers.4443 F u rtherm ore, m an y doctors re g a rd p ersisten t MUS as a n ex p ressio n of
psychological distress w ith p atien ts failing to see th e co n n ectio n b etw e en th e physical
General introduction | 15
sym p to m s a n d the psychological distress.'41;44 A ccording to m an y G Ps, th e physical sy m p to m s
are n o t the real problem .44In ad d itio n , m an y d octors rem a in skeptical ab o u t ph y sical sy m p to m s
th a t can n o t be explained b y a physical disease.45 C o m p ared w ith p atien ts w ith 'real' diseases,
p atien ts w ith p ersisten t MUS do n o t h av e m u c h p restig e in th e m edical arena.46 In fact, research
has sh o w n th a t doctors' ju d g m e n ts re g a rd in g th e in ten sity of p ain felt by p atien ts is associated
w ith th e presence o r absence of su p p o rtin g m edical evidence.47W h en th e re is objective m edical
evidence for th e pain, doctors w ere m o re inclined to accept th e p atien t's claim reg a rd in g th e p ain
intensity. F urth erm o re, doctors te n d to believe th a t th ere is inco n g ru en ce b etw een the
p rese n tatio n of MUS a n d th e actual b u rd e n in th is case.45
W h en facing p atien ts w ith p ersisten t MUS, m an y G Ps feel p re ssu riz e d to offer som atic
interv en tio n s.44148This feeling of b ein g p re ssu riz e d has b een w id ely a ttrib u te d to p atien ts' belief
th a t sy m p to m s are cau sed by physical disease a n d to th eir rejection of psychological help .42;49
In conclusion, G Ps' subjective feelings of b ein g p ressu riz ed for som atic in te rv en tio n s as w ell as
G Ps' skepticism reg a rd in g p ersisten t MUS h elp s to ex p lain th eir d issatisfaction w ith
con su ltatio n s w ith p atien ts w ith p ersisten t MUS an d th e w id e sp re a d labelling of th em as
'heartsink' or 'difficult' patien ts.42;50-53 H o w ev er, d esp ite th is fru stra tio n a n d skepticism , m any
G Ps believe th a t p atien ts w ith p ersisten t MUS sh o u ld be m a n ag e d in p rim a ry care as p ro v id in g
reassurance, counselling a n d acting as a 'gatekeeper' to p re v e n t in a p p ro p ria te in v estig atio n s are
c o n sid ered im p o rta n t roles for G P m an ag em en t.42
How do GPs experience the care they deliver fo r these patients ?
A s can be expected fro m the afo rem en tio n ed difficulties w ith p atien ts w ith p ersisten t MUS, GPs
experience difficulties in th e ir m a n ag em en t of these p atien ts. P rev io u s stu d ies rev ealed th a t
these difficulties are m ainly associated w ith th e co m m u n icatio n a n d th e d o cto r-p atien t
relatio n sh ip w ith these p atien ts.27;45;54-59H o w ev er, m o st stu d ies d id n o t focus specifically o n GPs'
experiences of th e care th ey d eliver to p atien ts w ith p ersisten t MUS. A s p atien ts w ith p ersisten t
MUS w ill keep atte n d in g th e consu ltin g h o u rs of th eir G Ps w ith th eir sy m p to m s, G Ps h av e to
fin d strategies to specifically deal w ith th e co m m u n icatio n a n d th e d o cto r-p atien t relatio n sh ip
d u rin g th e enco u n ters w ith these chronic p atien ts. U n fo rtu n ately , h o w ev er, k n o w led g e ab o u t
these strategies an d G Ps ' experiences, w h ich are b u ilt o ver tim e d u rin g th e co n tin u in g pro cess of
GPs' h ea lth care delivery for these patien ts, is still lacking.
The consultation
A n u m b e r of stu d ies reg a rd in g the d o cto r-p atien t co m m u n icatio n d u rin g co n su ltatio n s w ith
MUS p atien ts h ave b een p u b lish ed .38* 61The resu lts of these stu d ies are im p o rta n t because th ey
d em o n strate th a t G Ps com m unicate w ith MUS p atien ts m ore p o o rly th a n p rev io u sly th o u g h t.
^
16 I Chapter 1
In contrast to con su ltatio n s w ith p atien ts w ith ex p lain ed sy m p to m s, G Ps d id explore the
sym ptom s, feelings, concerns, o pinio n s an d expectations of th e p a tie n t less ad eq u ately in
consultations w ith p atien ts w ith MUS. It seem s th a t th e d o cto r-p atien t co m m u n icatio n in
p atien ts w ith MUS is less p atien t-c en tred co m p ared to p atien ts w ith ex p lain ed sym ptom s.
A lth o u g h p atien t-c en tred com m unicatio n is of m ajor im p o rtan ce, th e resu lts d em o n strate d th at
doctors co m m unicated in a d eq u a tely in precisely those co n su ltatio n s w h ere p atien t-cen tred
com m unication is m o st d esired a n d ad v a n ta g eo u s.38
These stu d ies also sh o w ed th a t p atien ts w ith MUS d id n o t req u e st som atic in te rv en tio n s m ore
fre q u en tly th a n p atien ts w ith m edically ex p lain ed sym ptom s. A d d itio n ally , p atien ts w ith MUS
d id n o t ask for an ex p lan atio n or req u ire reassu ran ce m o re often th a n p atien ts w ith m edically
ex plained sym ptom s. These fin d in g s refu te th e GPs' subjective feeling of b ein g p ressu rized . The
only difference b etw e en p atien ts w ith ex p lain ed sy m p to m s a n d p atien ts w ith u n ex p lain e d
sy m p to m s w as th a t p atien ts w ith MUS d esired m o re em otional s u p p o rt fro m th e ir G P.60
H ow ever, G Ps w ere less em pathic to w a rd th ese patien ts. F u rth erm o re, in co n su ltatio n s w ith
patien ts w ith MUS, G Ps are m ore inclined to offer a p resc rip tio n th a n th a t p atien ts ask ed for a
presc rip tio n them selves (70% v ersu s 58%). Sim ilar resu lts w ere fo u n d w ith resp ect to p ro p o sals
for ad d itio n a l tests (35% v ersu s 13%) a n d su g g estio n s for referrals (20% v ersu s 14%).
D u rin g m o st consultations (m ore th a n 95%) w ith p atien ts w ith MUS, p atien ts in d ic ated one or
m ore psychosocial problem s. F urth erm o re they su g g e sted th a t the problem (s) m ay cause or
influence th eir sym ptom s. H ow ever, m o st G Ps do n o t seem to resp o n d to these cues.62;63
What care do GPs deliver during encounters with patients with persistent MUS ?
D octor-patient com m u n icatio n in p atien ts w ith MUS is a com plex p h en o m en o n . M ost stu d ies
described above stu d ie d th e d o cto r-p atien t in teractio n d u rin g th e initial p rese n tatio n of MUS
an d d id n o t focus o n p atien ts w ith persisten t MUS.38;60-61 H o w ev er, in g eneral m o st of th e tim e
MUS are tran sien t a n d im prove w ith o u t fu rth e r in te rv en tio n s after one or tw o consultations.
W hen sy m p to m s evolve into a chronic a n d d isab lin g co n d itio n (i.e. persisten t MUS), encounters
as w ell as d o cto r-p atien t com m unicatio n becom e m ore com plicated. H o w ev er, k n o w led g e of
th e d o cto r-p atien t com m u n icatio n in p atien ts w ith p ersistent MUS is still lacking.
Rationale for this thesis
As d escribed above, there is alread y su b stan tial k n o w led g e re g a rd in g the problem atic
interactio n w h e n G Ps m eet p atien ts d u rin g th e p rese n tatio n of MUS. H o w ev er m ost of this
research d id n o t focus specifically o n p a tie n t w ith persisten t MUS. The initial p rese n tatio n of
General introduction | 17
MUS does n o t rep rese n t a large p ro b lem for h ea lth care, as m ost of th ese sy m p to m s are tran sien t
an d have a good prognosis. The m ain p ro b lem w ith MUS p atien ts rises w h e n th ese sy m p to m s
develop to w ard s a chronic co n d itio n in w h ich p atien ts p ersisten tly p rese n t MUS to th eir GP.
From this p o in t o n th e G P has to fin d a w ay to m an ag e these p atien ts in o rd er to im p ro v e
patien ts' subjective w ell-being, sy m p to m red u c tio n a n d q u ality of life, to p re v e n t p o ten tial
h arm fu l investigations a n d referrals, a n d to p re v e n t G Ps o w n dissatisfactio n a n d fru stra tio n
•l1 these
l1
L* L 7;38;64;65
w ith
patients.
To im prove th e q u ality of care for p atien ts w ith persisten t MUS, w e n ee d in sig h t in to th e care G Ps
deliver an d the care p atien ts expect. This w ill lead to a b etter u n d e rs ta n d in g of strateg ies for the
m a n ag e m en t of p atien ts w ith p ersisten t MUS by GPs. F u rth erm o re, giv en th e lim ited
suitability, applicability a n d effectiveness of specific in te rv en tio n s in p rim a ry care (such as a n ti­
d ep ressan ts, cognitive b eh av io u ral th e ra p y a n d re a ttrib u tio n th erap y ) for p atien ts w ith
p ersiste n t M US,66-70 k n o w le d g e
of p a tie n ts o p in io n s, G Ps' v ie w s a n d d o c to r-p a tie n t
com m unication m ig h t gu id e n ew in te rv en tio n strateg ies for p atien ts w ith persisten t MUS in
p rim a ry care a n d enhance th e satisfactio n of G Ps as w ell as p atien ts w h ile en c o u n te rin g daily GP
practice.
Objectives of this thesis
T he aim of th is thesis w as to o b ta in m o re in sig h t in w h a t h ap p e n s w h e n G Ps en c o u n ter p atien ts
w ith persisten t MUS a n d w h ic h p roblem s th e n arise. Specifically w e w ere in te reste d in th e care
G Ps d eliver a n d th e care p atien ts expect w h e n v isitin g th e G P w ith persisten t MUS. T herefore, w e
d esig n ed a s tu d y to ev alu ate the three essential p a rts in th e care for th ese p atients: th e p atient,
th e doctor a n d th e consultation.
R eg ard in g the p a tien t w e aim ed to an sw er th e fo llo w in g research questions:
1. W h at are the characteristics of p atien ts w h o p rese n t p ersisten t MUS in p rim a ry care?
2. W h at is the course of MUS a n d w h ich facto rs influence its course?
3. W h at are patien ts' opin io n s ab o u t en co u n ters in w h ich th ey p rese n t p ersisten t MUS?
R eg ard in g the doctor w e aim ed to an sw er the fo llo w in g research questions:
1. W h at are G Ps' p ercep tio n s ab o u t en co u n ters w ith p atien ts w ith p ersisten t MUS?
R eg ard in g their consultations w e aim ed to an sw er th e fo llo w in g research questions:
1. H ow do G Ps talk to p atien ts w ith p ersisten t MUS d u rin g en co u n ters in w h ich p atien ts
p rese n t p ersisten t MUS?
18 I Chapter 1
W e fu rth e rm o re s tu d ie d th e literatu re aim in g to fin d sta rtin g p oints fo r im proving the m anagem ent
of p atien ts w ith p ersisten t MUS. W e th erefo re aim ed to an sw er th e fo llo w in g research
questions:
1. W hat are, according to experts in th e field, im p o rta n t a n d effective elem ents in the
trea tm e n t of MUS in p rim a ry care?
2. W hich explan ato ry m odels for MUS are describ ed in th e literatu re?
Outline of this thesis
The patient
In C h ap ter 2 w e p rese n t d ata ab o u t co m orbidity, referrals, d iagnostic tests, a n d h o sp ital
ad m issions over a p erio d of 10 y ears p rio r to th e diag n o sis chronic fu n ctio n al som atic sy m p to m s
in fo u r general practices p articip a tin g in th e C o n tin u o u s M o rb id ity R egistry (CMR) of the
u n iv ersity of N ijm egen.
C h ap ter 3 contains a system atic review a n d best-ev id en ce sy n th esis of th e literatu re on the
course of MUS, so m atisatio n diso rd er, h y p o ch o n d riasis, a n d rela ted p ro g n o stic factors.
C h ap ter 4 includes patien ts' opin io n s ab o u t en co u n ters in w h ich th ey p rese n t p ersisten t MUS.
A s w e consider the d o cto r-p atien t relatio n sh ip as a key factor in th e m a n ag em en t of p atien ts
w ith p ersisten t MUS, w e specifically ex p lo red p atien ts' o p in io n s ab o u t th e d o cto r-p atien t
relationship.
The doctor
C h ap ter 5 describes GPs' percep tio n s a b o u t en co u n ters w ith p atien ts w ith p ersisten t MUS. W e
focused o n percep tio n s a b o u t explain in g MUS to p atien ts a n d G Ps' p ercep tio n s ab o u t how
relatio n sh ip s w ith these p atien ts evolve o ver tim e in daily practice.
The consultation
C h ap ter 6 describes a co n su ltatio n w ith a p a tie n t w ith u n ex p lain e d p alp ita tio n s d u rin g
v a c u u m in g w hich ch an g ed m y perso n al co m m u n icatio n skills d u rin g en co u n ters w ith p atien ts
w ith p ersisten t MUS.
C h ap ter 7 p ro v id es insig h ts in how G Ps talk to p atien ts w ith p ersisten t MUS d u rin g th eir
encounters. W e focused p rim a rily on G Ps' ex p lo ratio n of p atien ts' sy m p to m s an d p ro b lem s and
G Ps d istrib u tio n of th e available tim e o n d ifferen t stages in th e p ersisten t MUS consultations.
Starting points for improving the management
In C h ap ter 8 w e p rese n t th e resu lts of a q u alitativ e analysis of n arrativ e rev iew s an d scientific
edito rials to explore experts opin io n s reg a rd in g effective m a n ag em en t strateg ies for p atien ts
w ith MUS.
General introduction | 19
C h ap ter 9 p ro v id es an overview of ex p lan ato ry m odels (i.e. m o d els of ex p lain in g th e n a tu re of
th e sym ptom s) of MUS described in th e scientific literatu re th a t m ay be of u se in daily general
practice.
C h ap ter 10 contains th e resu lts of a sy m p o siu m a n d w o rk sh o p o n MUS in p rim a ry care h eld a t
th e W onca W orld C onference 2007 in S ingapore. D u rin g th is m eetin g w e fo cu sed o n detecting
k n o w ledge g aps in MUS a n d establish in g p rio rities in MUS research.
In C h ap ter 11 th e resu lts of this thesis are critically rev iew ed , a n d reco m m en d atio n s for clinical
practice, m edical ed u c atio n an d fu tu re research are given.
1
20 I Chapter 1
Reference List
1
H o u tv ee n JH. D e d o k ter k an n iets v in d en . A m sterdam : U itgeverij B ert Bakker; 2009.
2
K roenke K, S pitzer RL. G en d er differences in th e rep o rtin g of physical a n d so m ato fo rm
3
G reen LA, F ryer GE, Jr., Y aw n BP, L anier D, D ovey SM. The ecology of m edical care
4
v a n de L isdonk EH. E rvaren en aan g eb o d e n m o rb id iteit in de h u isartsp rak tijk . Thesis.
sym ptom s. P sychosom M ed 1998; 60(2):150-155.
revisited. N Engl J M ed 2001; 344(26):2021-2025.
N ijm egen: K atholieke U n iversiteit N ijm egen, 1985.
5
v a n d er L inden M, W estert G, de Bakker D, Schellevis F. T w eede N atio n ale S tu d ie n aa r
ziekten en v errich tin g en in de h u isartsp rak tijk : k lach ten en a a n d o en in g en in de b ev o lk in g
en in de h u isa rtsp ra k tijk (Second N atio n al S urvey of m o rb id ity a n d in te rv en tio n s in general
practice: sy m p to m s a n d diseases in th e p o p u la tio n ). 2004.
Ref Type: R eport
6
P eveler R, K ilkenny L, K inm on th AL. M edically u n ex p lain e d ph y sical sy m p to m s in
p rim a ry care: a co m p ariso n of self-rep o rt screen in g q u estio n n aires an d clinical op in io n . J
Psychosom Res 1997; 42(3):245-252.
7
Barsky AJ, Borus JF. S om atizatio n a n d m ed icalizatio n in th e era of m a n ag e d care. JAMA
1995; 274(24):1931-1934.
8
N im n u a n C, H o to p f M, W essely S. M edically u n ex p lain e d sym ptom s: an epidem iological
stu d y in seven specialities. J P sychosom Res 2001; 51 (1):361-367.
9
Reid S, W essely S, C rayford T, H o to p f M. M edically u n ex p lain e d sy m p to m s in fre q u en t
a tten d e rs of secondary h ea lth care: retro sp ectiv e co h o rt stu d y . BMJ 2001; 322(7289):767.
10 V erhaak PF, M eijer SA, V isser AP, W olters G. P ersisten t p rese n tatio n of m edically
u n ex p lain e d sy m p to m s in general practice. Fam P ract 2006; 23(4):414-420.
11 L ipow ski ZJ. S om atization: the concept an d its clinical ap plication. A m J P sy ch iatry 1988;
145(11):1358-1368.
12 E scobar JI, G old in g JM, H o u g h RL, K arno M, B urnam M A, W ells KB. S o m atizatio n in the
com m unity: relatio n sh ip to disability an d u se of services. A m J Public H ea lth 1987;
77(7):837-840.
13 v a n W eel-B aum garten EM. D epression: th e lo n g -term perspective. A fo llo w -u p s tu d y in
general practice. Thesis. N ijm egen: R ad b o u d U n iv ersity N ijm egen M edical C entre, 2000.
14 v a n W eel C. V alid atin g long te rm m o rb id ity recording. J E pidem iol C o m m u n ity H ealth
1995; 49 S u p p l 1:29-32.
15 v a n W eel C, de G rau w WJ. Fam ily practices reg istra tio n n etw o rk s co n trib u ted to p rim a ry
care research. J C lin E pidem iol 2006; 59(8):779-783.
16 v a n W eel C. The C o n tin u o u s M orb id ity R eg istratio n N ijm egen: b ac k g ro u n d a n d h isto ry of a
D u tch general practice database. E ur J G en P ract 2008; 14 S u p p l 1:5-12.:5-12.
General introduction | 21
17 v an Eijk JT, G rol R, H u y g en FJ, M esker P, M esker-N iesten J, v a n M ierlo G et al. The fam ily
doctor a n d the p rev e n tio n of som atic fixation. Fam ily System s M edicine 1983;
1:5-15.
18 G rol R. To heal or to harm . The p rev e n tio n of som atic fix atio n in G eneral Practice. L ondon:
Royal College of G eneral P ractitioners; 1981.
19 K irm ayer LJ, Robbins JM. T hree form s of so m atizatio n in p rim a ry care: p revalence, co­
occurrence, a n d sociodem ograph ic characteristics. J N erv M ent Dis 1991;
179(11):647-655.
20 W essely S, N im n u a n C, S harpe M. F unctional som atic syndrom es: one or m any? L ancet
1999; 354(9182) :936-939.
21
C reed F, G u th rie E, Fink P, H en n in g sen P, Rief W , S h arp e M et al. Is th e re a b etter te rm th a n
"m edically u n ex p lain e d sym ptom s"? J P sychosom Res 2010; 68(1):5-8.
22 de W aal MW , A rnold IA. S om atoform d iso rd ers in g eneral practice. E pidem iology,
tre a tm e n t a n d com orbidity w ith d ep ressio n a n d anxiety. Thesis. L eiden: U niversiteit
L eiden, 2006.
23 Stone J, W ojcik W, D urran ce D, C arso n A, L ew is S, M acK enzie L et al. W h at sh o u ld w e say to
p atien ts w ith sym p to m s u n ex p lain e d by disease? The "num ber n e e d e d to offend". BMJ
2002; 325 (7378):1449-1450.
24 de W aal MW , A rn o ld IA, E ekhof JA, v a n H em ert AM. S om atoform d iso rd ers in general
practice: prevalence, fun ctio n al im p a irm en t a n d co m o rb id ity w ith anxiety a n d d ep ressiv e
disorders. Br J P sychiatry 2004; 184:470-6.:470-476.
25 v a n B okhoven MA. Blood test o rd erin g for u n ex p lain e d co m p lain ts in g eneral practice. The
feasibility of a w atch fu l w aitin g ap p ro ach . Thesis. M aastricht: M aastrich t U niversity, 2008.
26 v a n B okhoven MA, K och H , v a n d er WT, D in an t GJ. Special m eth o d o lo g ical challenges
w h e n s tu d y in g th e diagnosis of u n ex p lain e d co m p lain ts in p rim a ry care. J C lin E pidem iol
2008; 61(4):318-322.
27 M a lteru d K. S ym ptom s as a source of m edical know ledge: u n d e rs ta n d in g m edically
u n ex p lain e d d iso rd ers in w om en. F am M ed 2000; 32(9):603-611.
28 Page LA, W essely S. M edically u n ex p lain e d sym ptom s: exacerb atin g factors in th e doctorp a tie n t encounter. J R Soc M ed 2003; 96(5):223-227.
29 K ouyanou K, P ither CE, R abe-H esketh S, W essely S. A co m p arativ e s tu d y of iatrogenesis,
m ed icatio n abuse, a n d psychiatric m o rb id ity in chronic p a in p atien ts w ith a n d w ith o u t
m edically explained sym ptom s. P ain 1998; 76(3):417-426.
30 P eters S, S tanley I, Rose M, S alm on P. P atien ts w ith m edically u n ex p lain e d sym ptom s:
sources of p atien ts' a u th o rity a n d im plications for d em an d s o n m edical care. Soc Sci M ed
1998; 46(4-5):559-565.
31 S alm on P, P eters S, S tanley I. P atien ts' p ercep tio n s of m edical ex p lan atio n s for so m atisatio n
disorders: q u alitativ e analysis. BMJ 1999; 318(7180):372-376.
22 I Chapter 1
32 Johansson EE, H am b erg K, L in d g ren G, W estm an G. "I've b een crying m y w ay "--qualitative
analysis of a gro u p of fem ale patien ts' co n su ltatio n experiences. Fam P ract 1996; 13(6):498503.
33 N ettleto n S, W att I, O 'M alley L, D uffey P. U n d e rsta n d in g th e n arrativ es of p eo p le w h o live
w ith m edically u n ex p lain e d illness. P atien t E duc C o u n s 2005; 56(2):205-210.
34 D eale A, W essely S. P atients' percep tio n s of m edical care in chronic fatig u e sy n d ro m e. Soc
Sci M ed 2001; 52(12) :1859-1864.
35 S alm on P. P atients w h o p rese n t ph y sical sy m p to m s in th e absence of ph y sical pathology: a
challenge to existing m odels of d o cto r-p atien t interaction. P atien t E duc C o u n s 2000;
39(1):105-113.
36 W ern er A, M a lte ru d K. It is h a rd w o rk b eh a v in g as a credible patien t: en co u n ters b etw een
w o m en w ith chronic p a in a n d th e ir doctors. Soc Sci M ed 2003; 57(8):1409-1419.
37 Ring A, D ow rick C, H u m p h ris G, Salm on P. Do p atien ts w ith u n ex p lain e d physical
sy m p to m s p ressu rise g eneral p ractitio n ers for som atic treatm en t? A q u alitativ e stu d y . BMJ
2004; 328(7447):1057.
38 E pstein RM, S hields CG, M e ld ru m SC, Fiscella K, C arroll J, C arney PA et al. P hysicians'
responses to patien ts' m edically u n ex p lain e d sy m p to m s. P sychosom M ed 2006; 68(2):269276.
39 D ow rick CF, R ing A, H u m p h ris GM , S alm on P. N o rm alisatio n of u n ex p lain e d sy m p to m s
by general practitioners: a functio n al typology. Br J G en P ract 2004; 54(500):165-170.
40
Coia P, M orley S. M edical reassu ran ce a n d p atien ts' responses. J P sychosom Res 1998;
45(5):377-386.
41 W oivalin T, K rantz G, M a n ty ra n ta T, R ingsberg KC. M edically u n ex p lain e d sym ptom s:
percep tio n s of physicians in p rim a ry h ea lth care. F am P ract 2004; 21 (2) :199-203.
42 Reid S, W hooley D, C rayford T, H o to p f M. M edically u n ex p lain e d sym ptom s--G P s'
attitu d e s to w ard s their cause a n d m an ag em en t. F am P ract 2001; 18(5):519-523.
43 S harpe M, M ayou R, W alker J. Bodily sym ptom s: n ew ap p ro ach es to classification. J
P sychosom Res 2006; 60(4) :353-356.
44 W ilem an L, M ay C, C h ew -G raham CA. M edically u n ex p lain e d sy m p to m s a n d th e p ro b lem
of p o w er in the p rim a ry care consultation: a q u alitativ e stu d y . F am P ract 2002; 19(2):178182.
45 A sbring P, N a rv a n e n AL. Ideal v ersu s reality: p h y sician s p ersp ectiv es o n p atien ts w ith
chronic fatig u e sy n d ro m e (CFS) an d fibrom yalgia. Soc Sci M ed 2003; 57(4):711-720.
46 A lbum D, W estin S. D o diseases h av e a p restig e hierarchy? A su rv ey am o n g p h y sician s an d
m edical stu d en ts. Soc Sci M ed 2008; 66(1):182-188.
47 Tait RC, C hibnall JT. P hysician ju d g m e n ts of chronic p a in patien ts. Soc Sci M ed 1997;
45(8):1199-1205.
General introduction | 23
48
A rm stro n g D, Fry J, A rm stro n g P. D octors' p ercep tio n s of p ressu re fro m p atien ts for
referral. BMJ 1991; 302(6786):1186-1188.
49 G o ld b erg DP, B ridges K. Som atic p rese n tatio n s of p sychiatric illness in p rim a ry care
setting. J P sychosom Res 1988; 32(2):137-144.
50 G arcia-C am payo J, S anz-C arrillo C, Yoldi-E lcid A, L opez-A ylon R, M o n to n C. M an ag em en t
of som atisers in p rim a ry care: are fam ily doctors m o tiv ated ? A u st N Z J P sy ch iatry 1998;
32(4):528-533.
51 H a rtz AJ, N oyes R, B entler SE, D am iano PC, W illard JC, M om any ET. U n ex p lain ed
sy m p to m s in p rim a ry care: p ersp ectiv es of d o cto rs a n d p atien ts. G en H o sp P sy ch iatry 2000;
22(3):144-152.
52 S teinm etz D, T abenkin H. The 'difficult p atien t' as p erceiv ed by fam ily physicians. Fam
P ract 2001; 18(5):495-500.
53 M athers N, Jones N , H an n a y D. H ea rtsin k p atients: a s tu d y of th eir g eneral p ractitio n ers. Br
J G en P ract 1995; 45(395):293-296.
54 W alker EA, U n u tze r J, K aton WJ. U n d e rsta n d in g a n d carin g for th e d istre ssed p a tie n t w ith
m u ltip le m edically u n ex p lain e d sy m p to m s. J A m B oard Fam P ract 1998;
11(5):347-356.
55 Lin EH, K aton W , V on K orff M, B ush T, L ipscom b P, R usso J et al. F ru stra tin g patients:
physician a n d p a tie n t p erspectives am o n g d istressed h ig h u sers of m edical services. J G en
In tern M ed 1991; 6(3):241-246.
56 W alker EA, K aton WJ, K eegan D, G a rd n e r G, S ullivan M. P red icto rs of p h y sician fru stra tio n
in the care of p atien ts w ith rh eu m ato lo g ical com plaints. G en H o sp P sychiatry 1997;
19(5):315-323.
57 L u n d h C, S egesten K, B jorkelund C. To be a helpless helpoholic--G Ps' experiences of w o m en
p atien ts w ith non-specific m uscu lar pain. Scand J P rim H ea lth C are 2004; 22(4):244-247.
58 S m ith S. D ealing w ith the difficult p atien t. P o stg rad M ed J 1995; 71(841):653-657.
59 H a h n SR, T hom pson KS, W ills TA, S tern V, B u d n er NS. The difficult d o cto r-p atien t
relationship: so m atization, p erso n ality a n d psy ch o p ath o lo g y . J Clin E pidem iol 1994;
47(6):647-657.
60 S alm on P, Ring A, D ow rick CF, H u m p h ris GM. W h at do g eneral practice p atien ts w a n t
w h e n th ey p rese n t m edically u n ex p lain e d sy m p to m s, an d w h y do th e ir doctors feel
p ressu rized ? J P sychosom Res 2005; 59(4):255-260.
61 Ring A, D ow rick CF, H u m p h ris GM , D avies J, S alm on P. The so m atisin g effect of clinical
consultation: W hat p atien ts a n d doctors say a n d do n o t say w h e n p atien ts p rese n t m edically
u n ex p lain e d physical sym ptom s. Soc Sci M ed 2005; 61 (7):1505-1515.
62 C egala DJ. A s tu d y of doctors' a n d p atien ts' co m m u n icatio n d u rin g a p rim a ry care
consultation: im plications for com m u n icatio n training. J H ea lth C o m m u n 1997;
2(3):169-194.
24 I Chapter 1
63 Salm on P, D ow rick CF, Ring A, H u m p h ris GM. V oiced b u t u n h e a rd agendas: q u alitativ e
analysis of the psychosocial cues th a t p atien ts w ith u n ex p lain e d sy m p to m s p rese n t to
general p ractitioners. Br J G en P ract 2004; 54(500):171-176.
64 L ucassen P, olde H a rtm a n TC, B orghuis MS. Som atische fixatie. Een n ie u w lev en v o o r een
o u d begrip. H u isa rts en W etenschap 2007; 50(1):11-15.
65 S m ith GR, Jr., M onson RA, Ray DC. P atien ts w ith m u ltip le u n ex p lain e d sym ptom s. Their
characteristics, functional health , a n d h ea lth care u tilization. A rch In tern M ed 1986;
146(1):69-72.
66 K roenke K. Efficacy of tre a tm e n t for so m ato fo rm disorders: a rev iew of ran d o m ized
co ntrolled trials. P sychosom M ed 2007; 69(9):881-888.
67 S u m ath ip ala A. W hat is the ev idence for th e efficacy of trea tm e n ts for so m ato fo rm
disorders? A critical review of p rev io u s in te rv en tio n stu d ies. P sychosom M ed 2007;
69(9):889-900.
68 M orriss R, G ask L, D ow rick C, D u n n G, P eters S, R ing A et al. R an d o m ized trial of
rea ttrib u tio n o n psychosocial talk b etw e en d o cto rs an d p a tie n ts w ith m edically
u n ex p lain e d sym ptom s. P sychol M ed 2010; 40(2) :325-333.
69 M orriss R, D ow rick C, S alm on P, P eters S, D u n n G, R ogers A et al. C luster ran d o m ised
controlled trial of train in g practices in re a ttrib u tio n for m edically u n ex p lain e d sym ptom s.
Br J P sychiatry 2007; 191:536-42.:536-542.
70 M ultidisciplinary g uideline m edically u n ex p lain e d sy m p to m s a n d so m ato fo rm d iso rd e rs].
T rim bos In s titu u t/N e th e rla n d s In stitu te of M ental H ea lth an d A d d ictio n , editor. 2009.
H o u ten , L adenius C om m unicatie BV.
Ref Type: R eport
General introduction | 25
28 I Chapter 2
Abstract
Background.
Reliable lo n g itu d in al d a ta of p atien ts w ith fu n ctio n al som atic sy m p to m s in
g eneral practice are lacking.
Aim.
T o identify distinctive featu res in p atien ts w ith chronic fu n ctio n al som atic sym ptom s,
an d to determ in e w h e th e r these sy m p to m s su p p o rt th e h y p o th esis of th e existence of specific
som atic syndrom es.
Design.
O bservational stu d y , w ith a co m p ariso n co n tro l group.
Setting.
Four p rim a ry care practices affiliated w ith th e U n iv ersity of N ijm egen in The
N etherlands.
Methods.
O ne h u n d re d an d eig h ty -tw o p atien ts d ia g n o sed b etw e en 1998 a n d 2002 as
h av in g chronic fun ctio n al som atic sy m p to m s an d 182 controls m atch ed by age, sex,
socioeconom ic statu s, a n d practice w ere in clu d ed . D ata on co m orbidity, referrals, diagnostic
tests, a n d h o sp ital adm issio n s over a p erio d of 10 y ears p rio r to th e diag n o sis w ere collected.
M edication use a n d n u m b e r of visits to th e g eneral p ractitio n er (GP) w ere extracted fro m the
m o m en t co m p u teriz ed reg istratio n w as started.
Results.
In th e 10 y ears before th e d iag n o sis chronic fu n ctio n al som atic sy m p to m s,
significantly m ore p atien ts th a n controls p rese n t fu n ctio n al som atic sy m p to m s in at least tw o
b o d y system s, a n d u se d m ore som atic a n d psy ch o tro p ic d ru g s. T hey v isit th e G P tw ice as m uch,
statistically h a d significantly m ore p sychiatric m o rb id ity , a n d w ere referred m o re often to
m ental h ea lth w o rk e rs a n d som atic specialists. The n u m b e r of p atien ts u n d e rg o in g diagnostic
tests w as higher for p atien ts w ith chronic fu n ctio n al som atic sy m p to m s th a n for controls, b u t
h o sp ital ad m issions rates w ere equal.
Conclusion.
P atients w ith chronic fu n ctio n al som atic sy m p to m s h av e a g reat d iv ersity of
fun ctio n al som atic sym ptom s. They u se m o re som atic a n d p sy ch o tro p ic d ru g s th a n controls in
th e y ears before diagnosis. M oreover, th ey sh o w h ig h rates of referrals an d psychiatric
m orbidity. The div ersity of sym p to m s of p atien ts w ith chronic fu n ctio n al som atic sy m p to m s
su p p o rts th e concept th a t sym p to m s do n o t cluster in w ell-d efin ed d istin ct syndrom es.
T herefore, p atien ts w ith chronic fu n ctio n al som atic sy m p to m s sh o u ld p referab ly n o t be
classified into m edical su bspecialty syndrom es.
Chronic functional somatic symptoms: a single syndrome? | 29
Introduction
M edically u n ex p lain e d sym p to m s are com m on, a n d acco u n t for one in five n ew co n su ltatio n s in
p rim a ry care.1;2In 20-25% of all p rim a ry care visits, no serio u s m edical (that is, organic) cause is
fo u n d to ex p lain th e p atien t's p rese n tin g sy m p to m , an d 20-40% of th e p atien ts seen by m edical
specialists do n o t receive a clear diag n o sis.3;4 The p rese n ted sy m p to m s are th e n referred to as
'm edically unex p lain ed ' or 'functional'.5 F unctional, or rath e r m edically u n ex p lain ed , som atic
sym p to m s are ran k e d second o n th e list of th e 10 m o st com m on physical sy m p to m s in p rim ary
care an d have a n incidence rate of 70 p e r 1000 p a tie n t y ears in th e N e th e rla n d s.6
A lth o u g h an occasional v isit to the general p ractitio n er (GP) for a fu n ctio n al som atic sy m p to m
seem s n atu ra l, rep e ate d consultations because of these sy m p to m s rep rese n t a serio u s problem .
P atients w h o do this are often d iag n o sed as h av in g 'chronic fu n ctio n al som atic sym ptom s'.
Psychological d istress or psychosocial p ro b lem s are p re su m e d to b e th e u n d e rly in g cau ses.7As
such, diag n o sin g chronic fun ctio n al som atic sy m p to m s req u ires th e p a tie n t to rep eated ly
p rese n t physical sy m p to m s th a t rem a in m edically u n ex p lain e d after ad e q u ate exam ination,
an d indications, fro m the patien ts' p erso n al circum stances of p re su m e d psychosocial p roblem s
or psychological distress.
A s p atien ts w ith chronic functional som atic sy m p to m s are fu n ctio n ally im p aired , h av e h ig h
rates of com orbid psychiatric disorders, a n d are at risk of u n n ecessary d iagnostic p ro ced u res
an d treatm en ts, 1;4;<M1a correct d iagnosis is of p a ra m o u n t im p o rtan ce. H o w ev er, m o st research on
this topic has b ee n p erfo rm ed either o n u n selected p o p u la tio n -b ase d sam p les,12^3or in selected
patien ts referred to seco n d ary care.14;15 M oreover, m o st of th ese stu d ies m ake use of
q u estio n n aires in w h ich p atien ts h av e to recall a v arie ty of sy m p to m s ex istin g for a considerable
am o u n t of tim e.10;16;17This m e th o d has b een sh o w n to p ro d u ce u n stab le resu lts in w h ich lifetim e
sym p to m s p rese n t a t baseline are n o t rem em b ered a t fo llo w -u p .18 R esearch o n p atien ts from
p rim a ry care settings in w h o m th e diag n o sis h a d b een m ad e o n reliable lo n g itu d in al d ata is
generally lacking.
M oreover, th e re is considerable d ebate re g a rd in g th e q u estio n of w h eth e r fu n ctio n al som atic
sym p to m s cluster in w ell defin ed distin ct sy n d ro m es, su ch as fib rom yalgia, chronic fatig u e
syndrom e, or ten sio n headache, or w h eth e r th ese specific som atic sy n d ro m es are largely an
artefact of m edical sp ecilization.7;19In th is d ebate reliable d ata o n p rim a ry care p atien ts are also
n ee d ed , w h ereas m o st research on th is topic is p erfo rm ed in referred p o p u la tio n s2“21
concentrating o n specific sy m p to m s,22-24 or in co m m u n ity sa m p le s25 u sin g q u estio n n aires in
w h ich inconsistencies of recall m ay h av e a g reat effect o n th e assessm en t of th e u ltim ate
diagnosis.1826 The aim s of th is stu d y , therefore, are to explore w ith lo n g itu d in al data:
30 I Chapter 2
• h o w an d how often p atien ts w ith chronic fu n ctio n al som atic sy m p to m s p rese n t to their
G P a n d oth er m edical in stitution s,
• w h e th e r p atien ts w ith chronic fu n ctio n al som atic sy m p to m s in d e ed p rese n t m ore
functional som atic sy m p to m s in th e y ears before th e diagnosis,
• if sy m p to m s p rese n ted b y p atien ts w ith chronic fu n ctio n al som atic sy m p to m s su p p o rt
the existence of specific som atic syndrom es.
Methods
Continuous Morbidity Registration database
This s tu d y uses d ata fro m the C o n tin u o u s M o rb id ity R eg istratio n (CMR) d atab ase, a project of
th e d e p a rtm e n t of Fam ily M edicine of th e U n iv ersity of N ijm egen th e N eth e rlan d s.27-30 This
project w as sta rted in 1971 in fo u r practices in a n d a ro u n d N ijm egen31an d m o n ito rs a p o p u la tio n
of ap p ro x im ately 12 000 patien ts, rep rese n tativ e of th e D u tch p o p u la tio n w ith re g a rd to age an d
sex. E very episode of illness seen by, or re p o rte d to, th e G P is reg istered as so o n as it is
estab lish ed u sin g an ad a p te d v ersio n of th e E-list.32 D iagnoses an d codes are co rrected w h en
necessary. O ver m an y years, m o n th ly m eetin g s of all G Ps in v o lv ed are h eld to discuss
classification problem s, to m o n ito r th e a p p licatio n of d iagnostic criteria, a n d to discuss co ding
p roblem s of h y p o th etical case histories. As w ell as m edical d ata, th e fo llo w in g in fo rm atio n is
available: age, sex, socioeconom ic sta tu s (low, m id d le a n d high), a n d m arital statu s. In the
b eg in n in g th e reg istra tio n w as p erfo rm ed o n th e m edical chart; since 1994 a co m p u terized
reg istra tio n has b een used.
Patients with chronic functional somatic symptoms
W e selected all p atien ts fro m the CMR d atab ase in w h o m chronic fu n ctio n al som atic sym p to m s
w ere d iag n o sed for the first tim e b etw e en 1998 a n d 2002 (n = 182). For a p erio d of 10 y ears before
this diagnosis, th e follow ing variab les h ad b een collected: sociod em o g rap h ic characteristics;
m orb id ity data; a n d d a ta o n referrals, d iagnostic tests, a n d h o sp ital adm issions. U se of m edical
facilities w as assessed by the n u m b e r of contacts w ith th e GP. D ata on m ed icatio n use co u ld be
extracted fro m w h e n co m p u teriz ed reg istra tio n sta rted , a n d m ed icatio n d ata w ere tran sfo rm ed
in to th e p re sc rib e d
d a ily
d o se b y u sin g th e A n a to m ic a l T h e ra p e u tic a l C h em ical
C lassificatio n /D efin ed D aily D oses (A T C /D D D ) system .33As a pro x y of som atic m o rb id ity , w e
assessed three p rev a len t categories of chronic d iso rd ers (diabetes m ellitus, asth m a /c h ro n ic
obstru ctiv e p u lm o n a ry disease [COPD], an d card io v ascu lar diseases) a n d th ree p rev alen t
categories of self-lim iting d iso rd ers (skin d iso rd ers, m usculoskeletal, a n d airw ay) in o rd er to
stu d y th e h y p o th esis th a t p atien ts w ith chronic fu n ctio n al som atic sy m p to m s are at risk for
som atic m o rb id ity .37
Chronic functional somatic symptoms: a single syndrome? | 31
W e allocated the reg istered functional som atic sy m p to m s to specific b o d y system s; for exam ple,
g astro in testin al or m usculoskeletal, as described by E scobar et al.10 Irritab le b o w el sy n d ro m e
an d h y p erv e n tila tio n sy n d ro m e, som etim es re g a rd e d as m edically u n ex p lain e d sy m p to m s, are
n o t in c lu d ed in this study.
Controls
For each p a tie n t w ith chronic fun ctio n al som atic sy m p to m s, a control m atch ed b y age, sex,
socioeconom ic sta tu s, a n d practice w as d ra w n fro m th e CMR p o p u latio n . The o nly exclusion
criterion in th e control g ro u p w as the diag n o sis chronic fu n ctio n al som atic sy m p to m s. P atients
w h o w ere controls h a d to have h a d at least one reg istered ep iso d e of illness d u rin g th e p erio d
they h a d b een o n th e practice list. For controls, th e sam e in fo rm atio n as describ ed for p atien ts
w ith chronic fun ctio n al som atic sy m p to m s w as o b tain ed fro m 1990-2000.
Statistical methods
O u r analysis p rim arily in v o lv ed co m p arin g p atien ts w ith chronic fu n ctio n al som atic sy m p to m s
w ith th eir m atch ed controls. S tatistical analyses w ere co n d u cted u sin g SPSS 9.0. D escriptive
statistics w ere calculated for all variables. The d a ta o n specific b o d y sy stem s w ere an aly sed
u sin g explo rato ry factor analysis, a n d th e n sim p lified by v arim ax ro tation. The j 2 te st an d
stu d e n t's t-test w ere u se d for co m p arin g m eans of co n su ltatio n s an d m ed icatio n use in b o th
groups. O d d s ratio s (ORs) a n d 95% confidence in terv als (CIs) w ere u se d as th e m ain
m easu rem en t for associations, p articu larly w ith reg a rd to fu n ctio n al som atic sy m p to m s,
com orbidity, referrals, diagnostic tests a n d h o sp ital adm issions. All P -values are tw o-tailed.
Results
Characteristics of subjects
O f the 182 in c lu d ed p atien ts w ith chronic fu n ctio n al som atic sy m p to m s in c lu d ed in th e stu d y ,
141 (77.5%) w ere w om en; th e m ean age of all p atien ts w as 42.0 y ears (range = 10-85 years). M ost
subjects w ere of low (44.5%) or m id d le (42.9%) socioeconom ic class.
Functional somatic symptoms
The incidence rate of p atien ts w ith chronic fu n ctio n al som atic sy m p to m s w as 3.5 p er 1000
p a tie n t years, w h ereas th e p revalence of p atien ts k n o w n to h av e chronic fu n ctio n al som atic
sym p to m s is established o n 68.8 p er 1000 p a tie n t years.
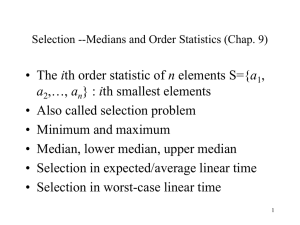
The p rese n ted fun ctio n al som atic sy m p to m s in v ario u s b o d y sy stem s in p atien ts a n d controls is
d isp lay ed in T able 1. For each sy m p to m g ro u p , p atien ts an d controls differ significantly
32 I Chapter 2
Table 1. Distribution of functional somatic symptoms in the various body systems (n = 182)
Pseu d o n eu ro lo g ical
Patients (%)
Controls (%)
Odds ratio (95% CI)‘
54 (29.7)
13 (7.1)
5.5 (2.8 to 11.1)
G astro in testin al
69 (37.9)
15 (8.2)
6.8 (3.6 to 13.1)
M usculoskeletal
58 (31.9)
6 (3.3)
13.7 (5.5 to 36.5)
C ard io resp irato ry
74 (40.7)
16 (8.8)
7.1 (3.8 to 13.5)
H ead ach e a n d o th er p a in
80 (44.0)
15 (8.2)
8.7 (4.6 to 16.6)
Pseu d o p sy ch iatric
150 (82.4)
48 (26.4)
13.1 (7.7 to 22.4)
O thers
66 (36.3)
10 (5.5)
9.8 (4.6 to 12.2)
U nknow n
67 (36.8)
0 (0)
aStatistical significant difference between patients and controls.
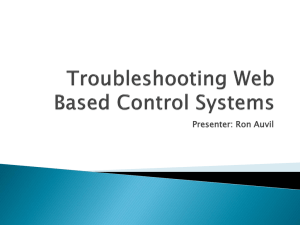
(P<0.05). It is rem arkable th a t m an y p atien ts h a d sy m p to m s in v ario u s b o d y sy stem s - a fin d in g
th a t is su p p o rte d by the factor analysis (Figure 1) - as it is often co n sid ered th a t th e re are a
n u m b e r of w ell-d efin ed distin ct fun ctio n al som atic sy n d ro m es, clu sterin g a ro u n d physical
sym p to m s of one b o d y system . M oreover, factor analysis su g g ests th at, o n th e one han d ,
gastrointestinal, ca rd io resp irato ry , a n d p seu d o p sy ch iatric sy m p to m s are lin k ed an d , o n the
Figure 1. Symptom diversity in patients with chronic functional somatic symptoms and their matched controls
controls
patients
number of affected body systems
Chronic functional somatic symptoms: a single syndrome? | 33
other, th a t pseu d o n eu ro lo g ical sym pto m s, m u scu lo sk eletal sy m p to m s, a n d h ead ach e a n d other
pain, are lin k ed w ith each other. S ignificantly m o re p atien ts th a n controls p rese n ted sy m p to m s
in tw o or m ore b o d y system s (87.9 v ersu s 19.8%; OR = 29.5, 95% CI = 16.0 to 54.9). O f all the
patien ts, 25 % p rese n ted sym p to m s in fo u r or m o re b o d y sy stem s.
H alf of th e p atien ts h a d th ree or m ore ep iso d es of fu n ctio n al som atic sy m p to m s before he or she
w as d iag n o sed as h av in g chronic functio n al som atic sy m p to m s; 25% of th e p atien ts h ad five or
m ore episodes before chronic fun ctio n al som atic sy m p to m s w ere d iagnosed.
Comorbidity: somatic and psychiatric
P atients w ith chronic fun ctio n al som atic sy m p to m s h ad significantly m ore psychiatric
d iso rd ers in co m p ariso n w ith controls (OR = 2.4) (Table 2). P atien ts d id n o t h av e a m u c h higher
rate of chronic a n d self-lim iting som atic co m orbidity, a n d th ey h a d o nly slig h tly m o re episodes
of self-lim iting airw ay p roblem s th a n controls.
Consultations, referrals, diagnostic tests and hospital adm issions
The n u m b e r of consultations in p atien ts w ith chronic fu n ctio n al som atic sy m p to m s is
significantly h ig h er (n = 9.8 v ersu s n = 4.2, P<0.001), as th e n u m b e r of subjects referred for
diagnostic te stin g (n = 156 v ersu s n = 140, OR = 1.8). The n u m b e r of hom e visits w as eq u al in b o th
groups. A b o u t th ree -q u a rters of p atien ts h a d b een referred to som atic specialists, com p ared
w ith ab o u t half of th e controls. A bo u t o n e-th ird of th e p atien ts h a d b een referred to m ental
h ea lth sources co m p ared w ith less th a n 10% in controls. H o sp ital ad m issio n s w ere th e sam e.
T hese d a ta are o u tlin ed in T able 2.
Medication use
The resu lts reg a rd in g m ed icatio n use are d etailed in Table 3. W e fo u n d th a t p atien ts w ith
chronic functional som atic sym ptom s u se d a significant m o re som atic m ed icatio n (2.6 v ersu s
1.5, P<0.001) a n d p sychotropic d ru g s (0.4 v ersu s 0.05, P<0.001) p er y ear co m p ared w ith controls.
The n u m b e r of p atien ts u sin g a n tid ep ressan ts a n d b en zo d iazep in es is statistically d ifferen t in
b o th g ro u p s (35.6% v ersu s 5.9%; 52.5% v ersu s 12.7% respectively, P<0.001).
In p atien ts u sin g m edication, an tid ep ressan ts w ere u sed for a m ean of 20 days a year an d
b en z o d ia ze p in es for 9 d ays a y ear co m p ared w ith 5 a n d 4 days, respectively, in controls.
H ow ever, these fin d in g s do n o t reach statistical significance. M oreover, th ere is no difference in
p rescrib ed daily dose for p atien ts a n d controls.
34 I Chapter 2
Table 2. Number of consultations, comorbidity, referrals, diagnostic tests, and hospital admissions in patients
and controls (n = 182)
<0.001b
0.53
00
C o m o rb id ity (n [%])
Som atic chronic:
D iabetes M ellitus
A sth m a/C O P D
C ard io v ascu lar
P-value
\o
CM
LO
fN
00
Os
G P consultations in one y e ara
(mean [range])
Practice visits
H om e visits
0.2 (0-3.5)
Controls
LO
o
<N
Patients
0.3 (0-7.1)
Odds ratio (95% CI)
-
5 (2.7)
20 (11.0)
16 (8.8)
4 (2.2)
10 (5.5)
8 (4.4)
-
1.3 (0.3 to 5.7)
2.1 (0.9 to 5.0)
2.1 (0.8 to 5.5)
Som atic self-lim iting:
Skin
M usculoskeletal
A irw ay
96 (52.7)
130(71.4)
136 (74.7)
82 (45.1)
115(63.2)
113 (62.1)
-
1.4 (0.9 to 2.1)
1.5 (0.9 to 2.3)
1.8 (1.1 to 2.9)b
Psychiatric0
41 (22.5)
20 (11.0)
-
2.4 (1.3 to 4.4)b
R eferrals (n [%])
Somatic: M edical
Somatic: P a ra m e d ic a l
M ental H ealth
130 (71.4)
129 (70.9)
59 (32.4)
97 (53.3)
87 (47.8)
15 (8.2)
-
2.2 (1.4 to 3.5)b
2.6 (1.7 to 4.2)b
5.3 (2.8 to 10.3)b
D iagnostic teste (n[%])
156 (85.7)
140 (76.9)
-
1.8 (1.0 to 3.2)b
H osp ital ad m issio n s (n [%])
Som atic
Psychiatric
57 (31.3)
1 (0.5)
51 (28.0)
1 (0.5)
-
1.2 (0.7 to 1.9)
-
1.0
an = 118: one general practice did not use the computerised registration, so consultation could not be established in this practice.bStatistically significant
difference between patients and controls P<0.05. Including schizophrenia, depression, psychoses, hysteria, phobia, neuroses, post-traumatic stress
disorder, alcoholism, use of street drugs. Including physiotherapist, dietician. Including hematological tests, x-ray examinations, ultrasonography,
electrocardiography.
Discussion
Strengths and limitations of this study
The stre n g th of th e p rese n t stu d y is th a t th e p atien ts w h o w ere in c lu d ed w ere those w ho
consu lted th eir GP, irrespective of th e p rese n ted sy m p to m s. T herefore, a th resh o ld of relevance
of the sy m p to m s for th e p a tie n t w as estab lish ed an d w e w ere able to analyse all sym p to m s
presen ted . M ost p o p u la tio n -b ase d stu d ies assess all sy m p to m s irresp ectiv e of th e p erceived
n ee d for help.10;16;17 M oreover, in p o p u la tio n -b ase d stu d ies, in te rv iew in g p atien ts rep eated ly
does n o t lead to a consistent classification of so m ato fo rm d iso rd ers,18w h ereas o u r classification
of th e p rese n ted m o rb id ity is b ased on v ery stable d ata,29;34 in w h ich lo n g itu d in al research is
allow ed an d recall bias w ill n o t occur.
Chronic functional somatic symptoms: a single syndrome? | 35
Table 3. Medication use in patients and controlsa (n = 118)
Odds ratio
(95% CI)
Patients
Controls
P-value
N u m b e r of som atic m ed icatio n p e r y e ar (mean [range])
N u m b e r of psych o tro p ic d ru g s p e r y ear (mean [range])
2.6 (0-18.0)
0.4 (0-9.0)
1.5 (0-7.5)
0.05 (0-0.62)
<0.001b
<0.001b
-
N u m b e r of p atien ts u sin g psych o tro p ic d ru g s (n [%])
A ntid ep ressan ts
B enzodiazepines
O thers
42 (35.6)
62 (52.5)
3 (2.5)
7 (5.9)
15 (12.7)
3 (2.5)
-
7.5 (3.1to18.9)b
5.8 (3.0to11.1)b
1.0
19.5 (1.9-297.0)c 5.0 (1.62-91.7)d
8.9 (0.4-322.5)c 4.2 (1.1-90.8)d
3.8 (0.2-25.1)d
34.3 (1.7-58.2)
-
-
0.76 (0.20-1.37)c 0.77 (0.13-2.00)d
0.62 (0.06-1.50)c 0.61 (0.20-1.54)d
0.51 (0.25- 0.75) 0.31 (0.25-0.40)d
-
-
D ays of p sy chotropic d ru g use p e r y e ar (median
[range])
A ntid ep ressan ts
B enzodiazepines
O thers
P rescribed d a ily d ose (mean [range])
A ntid ep ressan ts
B enzodiazepines
O thers
an = 118: one general practice di not use the computerised registration, so medication could not be established in this practice. bStatistically ignificant
difference between patients and controls P<0.05. cFor patients with antidepressants, benzodiazep nes and other psychotropic drugs, n = 42 62, and 3,
respectively. dFor controls with ntidepressants, benzodiazepines and other psychotropic drugs, n ==7, 15 and 3, respectively.
The lim itations of the stu d y are the retro sp ectiv e u se of d ata in existing m edical reco rd s a n d the
possible in terd o cto r v aria tio n of th e diag n o sis of chronic fu n ctio n al som atic sy m p to m s.35 The
in terd o cto r v aria tio n is p artly a consequence of n o t h av in g explicitly sta te d criteria for chronic
fun ctio n al som atic sy m p to m s in the CMR. This subjectivity w ill p ossibly alw ay s exist because
d iag n o sin g chronic fun ctio n al som atic sy m p to m s rem ain s an in te rp re tatio n of th e sym ptom s,
an d is influenced by forek n o w led g e a n d context.27H o w ev er, it is k n o w n fro m th e literatu re th a t
th e G P's ju d g e m e n t o n so m atisatio n seem s v alid in daily practice. M oreover, ad d itio n al
v alid atio n of clinical ju d g e m e n t is possible th ro u g h lo n g itu d in al fo llo w -u p .36The subjectivity of
th e diagnosis a n d th e d o cto r-p atien t relatio n sh ip also m ake im p o rta n t co n trib u tio n s to the
genesis an d persistence of fun ctio n al som atic sy m p to m s.37 The d octor's k n o w led g e of the
p atien t's com plaints is an im p o rta n t issue a n d is asso ciated w ith a b etter outcom e.
O f all variables described, only consult freq u en cy is d irectly lin k ed w ith th e diag n o sis of chronic
fun ctio n al som atic sym p to m s - as such, th e h ig h er freq u en cy of G P visits w as to be ex pected a
p rio ri.38
36 I Chapter 2
Summary of main findings
This is th e first observational s tu d y u sin g lo n g itu d in al d a ta d escrib in g p atien ts in w h o m
consu ltin g th e G P for functional som atic sy m p to m s h as becom e a reg u la r w ay of presen tin g .
D u rin g th e 10 y ears before th e d iagno sis of chronic fu n ctio n al som atic sy m p to m s is estab lish ed
by the G P, p atien ts consult th eir G P tw ice as m uch, u se m u c h m o re som atic an d psychotropic
m edication, have m ore psychiatric m o rb id ity an d are m o re often referred to m en tal h ealth
w o rk e rs th a n controls. D u rin g these 10 years, th e n u m b e r of d iagnostic tests is slightly h ig h er in
p atien ts an d th e n u m b e r of h o sp ital ad m issio n s is eq u al in co m p ariso n w ith controls. P atients
w ith chronic functional som atic sy m p to m s are m o re likely to p rese n t sy m p to m s in tw o or m ore
b o d y system s an d they p rese n t a hig h er n u m b e r an d g reater d iv ersity of sy m p to m s to th e GP
th a n control p atients. G Ps in th is s tu d y ap p e ar to classify p atien ts as h av in g chronic fu n ctio n al
som atic sym p to m s after th ree episo d es of p rese n tin g w ith fu n ctio n al som atic sym ptom s.
Comparison with the existing literature
The fin d in g th a t p atien ts could be reco g n ized as h av in g chronic fu n ctio n al som atic sy m p to m s
after they h a d experienced th ree episo d es of fu n ctio n al som atic sy m p to m s p rese n ted in tw o or
m ore b o d y system s, is an im p o rta n t one. F un ctio n al som atic sy m p to m s are often recognized
after h av in g excluded o th e r possible diagnosis. This m ay be associated w ith u n n ecessary and
p ossibly h arm fu l diagnostic strategies a n d m ay p ro m o te som atic fixation. E arly id en tificatio n of
these p atien ts co u ld p re v e n t som atic fixation, a n d enables th e G P to m odify h is /h e r
p ro ceed in g s.39 A d d itionally, this fin d in g w as co n firm ed u sin g factor analysis an d sh o w s th a t
fun ctio n al som atic sy m p to m s prob ab ly do n o t clu ster in w ell defined specific som atic
syndrom es. It also suggests th a t sy m p to m v aria tio n is g reat in th ese patients.
The concept of p atien ts w ith functional som atic sy n d ro m es p rese n tin g sy m p to m s in m an y body
system s h as also b ee n su p p o rte d b y recen t stu d ies.20T herefore, th e existence op specific som atic
sy n d ro m es sh o u ld be challenged. W ith a b ro ad -b ase d ap p ro ach , th e G P m ig h t be the
a p p ro p ria te p ractitio n er to diagnose a n d trea t these p atien ts by e m p h asizin g th e bio m ed ical as
w ell as th e psychosocial factors in v o lv ed in sy m p to m p ro d u c tio n a n d p erc ep tio n .40
The fin d in g th a t p atien ts w ith chronic fu n ctio n al som atic sy m p to m s d id n o t h av e a h ig h er rate of
chronic a n d self-lim iting som atic com o rb id ity is rem ark ab le because it is sta te d in th e literatu re
th a t so m atisatio n w ith m ore fre q u en t ex am in atio n m ay increase th e chance for chronic diseases
to be d iscovered.36W e fo u n d th a t m o re fre q u en t co n su ltatio n d id n o t lead to m o re d iag n o sed
chronic a n d self-lim iting diseases in p atien ts w ith chronic fu n ctio n al som atic sym ptom s.
The diagnosis chronic functional som atic sy m p to m s is n o t rec o rd e d as su ch in th e DSM-IV
classification. It no d o u b t exists as p a rt of th e sp e ctru m so m ew h ere b etw e en so m atisatio n
Chronic functional somatic symptoms: a single syndrome? | 37
diso rd er a n d som atoform d iso rd er n o t o th erw ise specified. The co n d itio n resem bles the
concept of 'ab rid g ed som atizatio n ',10 b u t is n o t b ased o n th e n u m b e r of sy m p to m s. Both
'ab rid g ed so m atization' an d chronic fu n ctio n al som atic sy m p to m s p resu m e u n d erly in g
psychological distress. The prevalence of so m atisatio n d iso rd er acco rd in g to th e DSM-IV in
p rim a ry care is low because of th e strin g e n t c rite ria “141 O n th e o th er h an d , less severe fo rm s of
som atizatio n have a m ajor im pact o n q u ality of life a n d o n th e use of h ea lth services, a n d are
m ore prevalent.
Implications for further research and clinical practice
P atients w ith chronic functional som atic sy m p to m s m ay b e co n sid ered as p ersisten t
com plainers a n d consequently labelled as 'difficult' patien ts. The co n d itio n m ay in d e ed reflects
a greater p ro p en sity to com plain; h ow ever, as is a p p a re n t fro m th e excess of psychiatric
com orbidity, p atien ts w ith chronic fu n ctio n al som atic sy m p to m s also have m ore reaso n to
com plain. W ith re g a rd to these patien ts, it seem s th a t c o n su ltin g th e G P for fu n ctio n al som atic
sy m p to m s h as becom e a reg u la r w ay of p resen tin g , b u t it m ig h t also be th a t p atien ts w h o a tten d
m ore often are at h ig h er risk of b ein g co n sid ered as chronic fu n ctio n al som atic sym ptom s.
M oreover, the diagnosis m ig h t relate to fru stra te d d o cto rs as a consequence of lack of
u n d e rsta n d in g , or failures in th e com m u n icatio n b etw e en d octor an d patient.
C hronic fun ctio n al som atic sym p to m s are a m ajor cause of m o rb id ity a n d d eserve fu rth er
in v estig atio n to estim ate the im portan ce of the d o cto r-p atien t relatio n sh ip , the feasibility of
treatm en ts, a n d th e u n d e rsta n d in g of th e aetiology of fu n ctio n al sy m p to m s to id en tify p atien ts
w h o are likely to becom e p ersisten t co m p lain ers a n d d ev elo p th e b eh a v io u ral p a tte rn of p atien ts
w ith chronic fun ctio n al som atic sym ptom s.
Also, th e o verlap of chronic functional som atic sy m p to m s w ith th e v ario u s DSM-IV diagnoses
sh o u ld be stu d ied . This is im p o rta n t becau se th e v alid ity of th e classification of m en tal d iso rd ers
is useful, b u t also questionable.42 T hin k in g in n a rro w sy n d ro m es m ig h t h in d e r an ap p ro p ria te
in te rp re tatio n of th e p atien t's syndrom es.
P atients rep e ate d ly p rese n tin g functio n al som atic sy m p to m s to the G P in tw o or m ore b o d y
system s, p articu la rly w h e n com bined w ith psychological co m plaints, sh o u ld be re g a rd e d as
ca n d id a tes for the diagnosis of chronic fu n ctio n al som atic sy m p to m s. It seem s th a t the
p rese n ted functional som atic sy m p to m s are p a rt of a single sy n d ro m e an d th a t sy m p to m
v aria tio n is g reat in these patients. T herefore, th e G P, w h o is co n sid ered as b ein g k now ledgeable
ab o u t u n d e rly in g psychosocial pro b lem s, sh o u ld diag n o se, treat, an d accom pany these
patients.
38 I Chapter 2
Acknowledgements
W e are g rateful to the G Ps an d practice n u rse s for b ein g able to carry o u t o u r research w o rk in
th eir CMR practices, a n d w e w o u ld like also to th a n k A n k d e Jonge an d V ivien M offat for
review in g the m anuscript.
Chronic functional somatic symptoms: a single syndrome? | 39
Reference List
1
K roenke K, M angelsdorff AD. C om m on sy m p to m s in am b u lato ry care: incidence,
ev aluation, th e ra p y , an d outcom e. A m J M ed 1989; 86(3):262-266.
2
Bridges KW, G o ld b erg DP. Som atic p rese n tatio n of DSM III p sychiatric d iso rd ers in
p rim a ry care. J P sychosom Res 1985; 29(6) :563-569.
3
Bass C e. Som atisation: P hysical S ym p to m s a n d Psychological d iso rd er. O xford: Blackwell;
1990.
4
Barsky AJ, Borus JF. S om atizatio n a n d m ed icalizatio n in th e era of m a n ag e d care. JAMA
5
T rim ble MR. F unctional diseases. Br M ed J (Clin Res Ed) 1982; 285(6357):1768-1770.
6
v a n de L isdonk EH, v a n d e n Bosch WJ, H u y g en FJA, L agro-Janssen ALM. P sychische en
1995; 274(24):1931-1934.
P sychiatrische stoornissen. Z iekten in de h u isartsp rak tijk . N ijm egen: E lsev ier/B u n g e; 1999.
101-121.
7
Barsky AJ, B orus JF. F unctional som atic sy n d ro m es. A n n In tern M ed 1999; 130(11):910-921.
8
K aton WJ, W alker EA. M edically u n ex p lain e d sy m p to m s in p rim a ry care. J C lin P sychiatry
1998; 59 S u p p l 20:15-21.
9
S m ith GR, Jr., M onson RA, Ray DC. P atien ts w ith m u ltip le u n ex p lain e d sy m p to m s. Their
characteristics, functional health , a n d h ea lth care u tilization. A rch In tern M ed 1986;
146(1):69-72.
10 Escobar JI, W aitzkin H , Silver RC, G ara M, H o lm an A. A b rid g ed som atization: a s tu d y in
p rim a ry care. P sychosom M ed 1998; 60(4):466-472.
11 K aton W , V on K orff M, Lin E, L ipscom b P, R usso J, W ag n er E et al. D istressed h ig h utilizers
of m edical care. DSM-III-R diag n o ses a n d tre a tm e n t needs. G en H o sp P sy ch iatry 1990;
12(6):355-362.
12 Escobar JI, G old in g JM, H o u g h RL, K arno M, B urnam M A, W ells KB. S o m atizatio n in the
com m unity: relatio n sh ip to disability a n d use of services. A m J Public H ea lth 1987;
77(7):837-840.
13 F ink P. The use of h o sp italizatio n s by p ersisten t so m atizin g p atien ts. Psychol M ed 1992;
22(1):173-180.
14 G o ld in g JM, S m ith GR, Jr., K ashner TM. D oes so m atizatio n d iso rd er occur in m en? Clinical
characteristics of w o m en an d m en w ith m u ltip le u n ex p lain e d som atic sy m p to m s. A rch G en
P sychiatry 1991; 48(3):231-235.
15 K roenke K, A rrin g to n ME, M an g elsd o rff AD. The p revalence of sy m p to m s in m edical
o u tp a tie n ts a n d th e ad eq u acy of th erap y . A rch In tern M ed 1990; 150(8):1685-1689.
16 d eG ruy F, C olum bia L, D ickinson P. S o m atizatio n d iso rd er in a fam ily practice. J Fam P ract
1987; 25(1):45-51.
40 I Chapter 2
17 F eder A , O lfson M, G am eroff M, F uentes M, Shea S, L an tig u a RA et al. M edically
un ex p lain e d sy m p to m s in an u rb a n g eneral m edicine practice. P sychosom atics 2001;
42(3):261-268.
18 S im on GE, G ureje O. S tability of so m atizatio n d iso rd er a n d so m atizatio n sy m p to m s am o n g
p rim a ry care p a tie n ts. A rch G en P sy ch iatry 1999; 56(1):90-95.
19 W essely S, N im n u a n C, S harpe M. F unctional som atic syndrom es: o ne or m any? L ancet
1999; 354(9182):936-939.
20 N im n u a n C, R abe-H esketh S, W essely S, H o to p f M. H ow m an y fu n ctio n al som atic
syndrom es? J P sychosom Res 2001; 51 (4) :549-557.
21 N im n u a n C, H o to p f M, W essely S. M edically u n ex p lain e d sym ptom s: an epidem iological
s tu d y in seven specialities. J P sychosom Res 2001; 51 (1):361-367.
22 W essely S, C halder T, H irsch S, W allace P, W rig h t D. Psychological sy m p to m s, som atic
sym ptom s, an d psychiatric d iso rd er in chronic fatig u e a n d chronic fatig u e sy ndrom e: a
prosp ectiv e stu d y in th e p rim a ry care setting. A m J P sy ch iatry 1996; 153 (8) :1050-1059.
23 F u k u d a K, D obbins JG, W ilson LJ, D u n n RA, W ilcox K, S m allw ood D. A n epidem iologic
s tu d y of fatigue w ith relevance for th e chronic fatig u e sy n d ro m e. J P sy ch iatr Res 1997;
31(1):19-29.
24 H ickie I, L loyd A, H adzi-P avlovic D, P ark er G, Bird K, W akefield D. C an th e chronic fatigue
sy n d ro m e be defined by d istinct clinical featu res? Psychol M ed 1995; 25 (5) :925-935.
25 K om aroff AL, Fagioli LR, D oolittle TH, G an d ek B, G leit M A, G u erriero RT et al. H ealth
sta tu s in p atien ts w ith chronic fatig u e sy n d ro m e a n d in g eneral p o p u la tio n a n d disease
co m p ariso n groups. A m J M ed 1996; 101 (3):281-290.
26 F einstein AR, Josephy BR, W ells CK. Scientific a n d clinical p ro b lem s in indexes of
fun ctio n al disability. A n n In tern M ed 1986; 105(3) :413-420.
27 W eel-B aum garten EM, v a n d en Bosch WJ, v a n d en H o o g en HJ, Z itm an FG. The v alid ity of
th e diagnosis of d ep ressio n in general practice: is u sin g criteria for diag n o sis as a ro u tin e the
answ er? Br J G en P ract 2000; 50(453):284-287.
28 W eel-B aum garten E, v a n d en Bosch WJ, v a n d en H o o g en HJ, Z itm an FG. T en y ear fo llo w -u p
of d ep ressio n after d iagnosis in general practice. Br J G en P ract 1998; 48(435) :1643-1646.
29 v a n W eel C. V alidating long te rm m o rb id ity recording. J E pidem iol C o m m u n ity H ealth
1995; 49 S u p p l 1:29-32.
30 v a n W eel C, S m ith H , Beasley JW. Fam ily practice research n etw o rk s. E xperiences fro m 3
countries. J F am P ract 2000; 49(10) :938-943.
31 v a n W eel C, v a n d en Bosch WJ, v a n d en H o o g en HJ, S m its AJ. D ev elo p m en t of resp ira to ry
illness in childhood--a lo n g itu d in al stu d y in g eneral practice. J R Coll G en P ract 1987;
37(302):404-408.
32 Eim erl TS. O rg an ized curiosity. A p ractical ap p ro ac to th e p ro b lem of k eep in g reco rd s for
research p u rp o ses in general practice. J Coll G en P ract 1960; 3:246-252.
Chronic functional somatic symptoms: a single syndrome? | 41
33 W orld H ea lth O rganisation: G uid elin es for ATC classification a n d D DD assignm ent. N o rsk
M edisinaldepot, Oslo; 1996.
34 v a n d en Bosch WJ, H u y g en FJ, v a n d e n H o o g en HJ, v an W eel C. M o rb id ity in early
childhood: differences b etw e en girls a n d boys u n d e r 10 y ears old. Br J G en P ract 1992;
42(362):366-369.
35 R eid S, C rayford T, R ichards S, N im n u a n C, H o to p f M. R ecognition of m edically
u n ex p lain e d sym ptom s--do docto rs agree? J P sychosom Res 1999; 47(5) :483-485.
36 Schilte AF, P ortegijs PJ, B lankenstein A H , K n o ttn eru s JA. S o m atisatio n in p rim a ry care:
clinical ju d g e m en t a n d sta n d a rd ise d m e asu rem en t co m p ared . Soc P sy ch iatry Psychiatr
E pidem iol 2000; 35(6):276-282.
37 S tew art M A, M cW hinney IR, Buck CW. The d o c to r/ p a tie n t relatio n sh ip a n d its effect u p o n
outcom e. J R Coll G en P ract 1979; 29(199):77-81.
38 de G rau w WJ, v a n d en H o ogen HJ, v a n de L isd o n k EH, v a n G erw en W H , v a n W eel C.
C ontrol g ro u p characteristics a n d stu d y outcom es: em p irical d ata fro m a stu d y o n m o rtality
of p atien ts w ith ty p e 2 diabetes m ellitus in D u tch g eneral practice. J E pidem iol C om m unity
H ea lth 1998; 52 S u p p l 1:9S-12S.
39 G rol R. To heal or to harm . The p rev e n tio n of som atic fixation in G en eral Practice. L ondon:
Royal College of G eneral P ractitioners; 1981.
40 K aton W , S ullivan M, W alker E. M edical sy m p to m s w ith o u t id en tified pathology:
relatio n sh ip to psychiatric disord ers, ch ild h o o d a n d a d u lt trau m a, an d p erso n ality traits.
A n n In tern M ed 2001; 134(9 P t 2):917-925.
41 K aton W , Lin E, V on K orff M, R usso J, L ipscom b P, B ush T. S om atization: a sp e ctru m of
severity. A m J P sychiatry 1991; 148(1):34-40.
42 K endell R, Jablensky A. D istin g u ish in g b etw e en th e v alid ity a n d u tility of psychiatric
diagnoses. A m J P sychiatry 2003; 160(1):4-12.
44 I Chapter 3
Abstract
Objective.
To stu d y the course of m edically u n ex p lain e d sy m p to m s (MUS), so m atisatio n
d iso rd er a n d h y p o ch o n d riasis an d rela ted p ro g n o stic factors. K now ledge of p ro g n o stic factors
in p atien ts p rese n tin g p ersisten t MUS m ig h t im p ro v e o u r u n d e rsta n d in g of th e n atu ralistic
course an d the identification of p atien ts w ith a h ig h risk of a chronic course.
Methods.
A com prehensive search of M edline, PsycInfo, CIN A H L an d EMBASE w as
p erfo rm ed to select stu d ies focusin g o n p atien ts w ith MUS, so m atisatio n d iso rd er an d
h y p o ch o n d riasis an d assessing prog n o stic factors. S tu d ies fo cu sin g o n p atien ts w ith sin g le­
sy m p to m u n ex p lain e d d iso rd er or distinctive fu n ctio n al som atic sy n d ro m es w ere excluded. A
best-evidence sy nthesis for th e in te rp re tatio n of resu lts w as used.
Results.
O nly six stu d ies o n MUS, six stu d ies o n h y p o ch o n d riasis, a n d one stu d y on
a b rid g e d som atisatio n co u ld be inclu d ed . A p p ro x im ately 50 to 75% of th e p atien ts w ith MUS
im prove, w h ereas 10 to 30% of p atien ts w ith MUS d eterio rate. In p atien ts w ith h y p o ch o n d riasis
recovery rates v ary b etw e en 30% to 50%. In stu d ies o n MUS a n d h y p o ch o n d riasis w e fo u n d
som e evidence th a t the n u m b e r of som atic sy m p to m s a t baseline influences th e course of these
conditions. F urth erm o re, th e seriousn ess of th e co n d itio n at b aselin e seem ed to influence the
p rognosis. C om orbid anxiety an d d ep ressio n do n o t seem to p red ic t th e course of
h y po chondriasis.
Conclusions.
D ue to the lim ited n u m b e rs of stu d ies a n d th e ir h ig h h etero g en eity , th e re is a
lack of rig o ro u s em pirical evidence to id en tify rele v an t p ro g n o stic factors in p atien ts p resen tin g
p ersisten t MUS. H ow ever, it seem s th a t a m o re serio u s co n d itio n at baseline is asso ciated w ith a
w o rse outcom e.
Course and prognosis, a systematic review | 45
Introduction
M edically u n ex p lain e d sy m p to m s (MUS) are com m o n in p rim a ry care.1In 25-50% of all p rim a ry
care visits, n o som atic cause is fo u n d to ex p lain th e p atien t's p rese n tin g sy m p to m s.2 It is
generally believed th a t p ersisten t p rese n tatio n of MUS is a chronic an d d isab lin g d iso rd er.3
H ow ever, in m an y p atien ts MUS are tran sien t an d h av e a g o o d p rognosis. A recen t D u tch stu d y
fo u n d th a t only 2,5% of th e atten d ees in g eneral p ractice p rese n tin g w ith su ch sy m p to m s m eet
criteria for chronicity.4
In a recent review , researchers sta te d th a t in p o p u la tio n -b ase d a n d p rim a ry care sam ples, MUS
is th e com m on characteristic of the D S M -IV a n d IC D -10 so m ato fo rm d iso rd ers in clu d in g
so m atisatio n an d h y p o ch o n d riasis.5-7 S om atisatio n is ch aracterized by rec u rren t an d fre q u en t
p rese n tatio n of MUS w h ereas h y p o ch o n d riasis is ch aracterized by excessive w o rry ab o u t illness
an d th e belief of h av in g an u n d ia g n o sed ph y sical d ise ase.
D espite the low p revalence of p ersisten t MUS, it rep rese n ts a serio u s p ro b lem in p rim ary care.
P atients are functionally im p aired , hav e h ig h rates of co m o rb id p sychiatric d iso rd ers a n d are at
risk for unnecessary, poten tially h arm fu l d iagnostic p ro ce d u re s a n d trea tm e n ts.2,3,8M oreover,
p a rt of the b u rd e n to G Ps are the difficulties in ex p lain in g th e sy m p to m s, fin d in g a sh ared
u n d e rsta n d in g necessary to reach reassu ran ce a n d accep tatio n of th e sy m p to m s a n d th e lack of
tre a tm e n t o p tio n s.9,10 O ften, G Ps label these p atien ts as 'h eartsin k p atien ts' or 'helpoholic
p atien ts'.11 For patien ts, as w ell as G Ps a n d th e h ea lth care sy stem it is im p o rta n t to p rev e n t
persisten t MUS. T herefore, G Ps sh o u ld be able to recognize p atien ts w ith a h ig h risk of
persisten t MUS. H ow ever, G Ps experience difficulties in d istin g u ish in g self lim itin g MUS from
persisten t MUS.12 K now ledge of p rog n o stic factors m ay im p ro v e o u r m a n ag e m en t of p atien ts
w ith MUS, as p atien ts w ith a good p ro g n o sis can be rea ssu re d ab o u t th e fav o u rab le sp o n tan eo u s
recovery rates, w h ereas a m ore inten siv e ap p ro a ch in c lu d in g som e fo rm of re a ttrib u tio n or
cognitive b eh a v io u ral th e ra p y m ig h t be in d ic ated fro m th e b eg in n in g in th e h ig h -risk groups.
The aim of o u r stu d y is to gain in sig h t in th e course of MUS a n d in factors in flu en cin g its co u rse .
Method
Data sources and search strategy
W e system atically rev iew ed prosp ectiv e co h o rt stu d ies in p rim ary , seco n d ary or te rtiary care on
p atien ts w ith MUS, som atoform d iso rd ers a n d h y p o ch o n d riasis. W e s tu d ie d so m atisatio n
diso rd er, MUS a n d h y p o ch o n d riasis to g eth er because th ey a p p e a r to h av e m u c h in com m on:
m edically u n ex p lain e d sym ptom s, ty p ical illness a n d sick role b eh av io u r, d isp ro p o rtio n a te
disability a n d p reo c cu p atio n w ith h ea lth a n d illn ess.7
46 I Chapter 3
A lth o u g h th e re are m an y other general term s to describe physical sy m p to m s w ith o u t an organic
explanation, w e use the te rm 'm edically u n ex p lain e d sy m p to m s' as n o n e of these term s are ideal
an d this is the m o st n e u tra l description .13'14
W e d id n o t include clinical trails in th is review as th e p atien ts rec ru ited into trails are often n o t
rep rese n tativ e of th e p o p u la tio n w ith th e d iso rd er.15'16 M oreover, p articip a tin g in a trial can
influence th e n a tu ra l course of th e sy m p to m s as p a rticip a tin g in a trial can be co n sid ered as an
in te rv en tio n in itself.
W e searched in th e M EDLINE d atab ase for p u b licatio n s p u b lish ed b etw e en 1965 a n d 1 June
2006, in PsycIN FO b etw e en 1967 an d 1 June 2006, in CIN A H L b etw e en 1982 a n d 1 June 2006 and
in EMBASE b etw e en 1965 a n d 1 June 2006. W e o b tain ed a d d itio n a l references fro m th e reference
lists of review articles an d retriev ed o rig in al p ap ers. W e u se d th e fo llo w in g keyw ords:
s o m a to fo rm
d is o rd e r,
h y p o c h o n d r ia s is ,
n e u ra s th e n ia ,
c o n v e rs io n
d is o rd e r,
psychophysiological d iso rd er, functio n al som atic sym pt* a n d m edically unexplained*.
W e com bined this search u sin g the B oolean o p era to r A N D w ith th e sen sitiv e M EDLINE search
for clinical stu d ies o n p rognosis.17 The search strateg y is sh o w n in A p p en d ix A. T here w ere no
lim itations reg a rd in g the lan g u ag e of pub licatio n . W e tested th e search strateg y o n 30
publicatio n s a b o u t m edically u n ex p lain e d sy m p to m s in o u r o w n d atab ase an d fo u n d th e search
strateg y to be sensitive as all k n o w n articles w ere found.
Study selection
T oH an d MB in d e p e n d e n tly screened th e titles a n d ab stracts of all id e n tified citations to identify
eligible articles. W h en w e co u ld n o t decide on inclusion, w e co n su lted th e full publication.
If after stu d y in g the com plete m a n u scrip t d isag reem en t p ersisted , w e co n su lted a th ird
review er (FvdL). W e u se d C ohen's k ap p a statistic
(k )
to assess ag reem en t b etw e en th e tw o
review ers.18 Inclusion criteria w ere: p ro sp ectiv e cohort design, focus o n p ro g n o sis of p atien ts
w ith m edically u n ex p lain e d sy m p to m s a n d a fo llo w -u p of 3 m o n th s or m ore.
W e excluded stu d ies th a t focu sed p rim a rily o n p atien ts w ith m edical or psychiatric disease
(except som atoform d iso rd ers an d h y p o ch o n d riasis). W e also ex clu d ed stu d ies th a t focused on
p a tie n ts su ffe rin g fro m
sin g le -sy m p to m
u n e x p la in e d
d is o rd e r (te n sio n h ea d ac h es,
d ysm enorrhoea) or p atien ts suffering fro m d istinctive fu n ctio n al som atic sy n d ro m es (irritable
bow el sy n d ro m e, chronic fatig u e sy n d ro m e) becau se w e w ere in te reste d in th e course and
p ro g n o s is of u n d if fe r e n tia te d
m e d ic a lly u n e x p la in e d sy m p to m s. W e fo c u s e d on
un d iffe ren tia te d MUS as w e assu m e th a t th ese are m ore difficult to h an d le for th e p h y sician th an
Course and prognosis, a systematic review | 47
single sy m p to m u n ex p lain e d d iso rd ers an d d istinctive fu n ctio n al sy n d ro m es. A fter all, the
latter give m ore o p p o rtu n ity to ex p lain th e sy m p to m s to p atien ts. Finally, th e re is evidence th at
th e n am e of a co n d itio n influences p rognosis.19 S tu d ies o n ch ild ren a n d ad o lescen ts (age < 18
years) a n d stu d ies o n specific g ro u p s of p atien ts su c h as refugees, street p ro stitu tes etc, w ere
excluded. C ase-control stu d ies, cross-sectional stu d ies an d case stu d ies w ere also excluded.
Data extraction
Tw o review ers (ToH an d MB) in d e p en d e n tly scored th e m eth o d o lo g ical q u ality of th e in clu d ed
studies. W e u se d a sta n d a rd iz e d checklist of p red e fin e d criteria (see A p p en d ix B), w h ich has
b een u se d in p rev io u s p rognostic review s.20'21 The list is b ased o n th eo retical co n sid eratio n s an d
m eth odological aspects described by H u d a k et al.22a n d A ltm an.23W e m o d ified th ese checklists
according to n ew insights.24W e tested th e q u ality assessm en t checklist in a p ilo t assessm ent. A
d etailed ex p lan atio n of each criterion is giv en in A p p en d ix C. E ach criterio n w as scored positive
(+), neg ativ e (-) or u nclear (?). The total q u ality score is th e su m of all th e criteria th a t are scored
positive. The m axim um qu ality score is 21. W e calculated th e q u ality of a s tu d y as th e percentage
of th e m ax im u m score.
W e d iscu ssed disagreem ents in the sco rin g of q u ality item s in a co n sen su s m eeting. In a case of
persistin g d isag reem en t b etw e en the tw o rev iew ers a th ird rev iew er (FvdL) m ad e th e final
decision.
W e categorized qu ality criteria into fo u r m ajor fo rm s of bias: selection bias, com p leten ess of
follow -up, info rm atio n bias a n d confo u n d in g . F u rth erm o re, w e d efin ed stu d ies w ith a quality
score of 60% or h ig h er as stu d ies w ith h ig h q u ality .25
The tw o review ers (ToH a n d MB) in d e p en d e n tly extracted th e in fo rm atio n fro m th e selected
p ap e rs by u sin g sta n d a rd iz e d a n d p re-tested d ata-ex tractio n form s. The extracted in fo rm atio n
in v o lv ed d ata o n s tu d y p o p u la tio n , d iagnostic criteria, inclu sio n an d exclusion criteria, setting,
ty p e of prognostic factors, d u ra tio n of fo llo w -u p , outco m es a n d d ata o n associations. In a case of
d isagreem ent, w e reach ed consensus after d iscu ssio n w ith a th ird rev iew er (FvdL).
Data synthesis
W e d id n o t p la n statistical p o o lin g as w e an ticip ated con sid erab le hetero g en eity . T herefore, a
qualitative analysis (best evidence synthesis) w as p erfo rm ed to su m m arize the v alu e of the
prognostic indicators. F urth erm o re, w e co n sid ered the stre n g th of evidence reg a rd in g a
prognostic factor as strong, m oderate, w ea k or inconclusive d e p e n d in g o n consistency of the
fin d in g s a n d o n qu ality of th e stu d y :26'27
48 I Chapter 3
- strong: co nsistent fin d in g s (> 75% of th e stu d ies rep o rtin g o n a factor sh o w ed th e sam e
directio n of th e association) in at least tw o h ig h q u ality stu d ies
- m oderate: co nsistent fin d in g s (> 75 % of th e stu d ies rep o rtin g o n a factor sh o w ed th e sam e
directio n of th e association) in on e h ig h q u ality co h o rt an d at least one low q u ality stu d y
- w eak: fin d in g s of one h ig h q u ality co h o rt or co n sisten t fin d in g s (> 75% of th e stu d ies
rep o rtin g o n a factor sh o w ed th e sam e d irectio n of th e association) in at least th ree or m ore
low quality stu d ies
-
inconclusive: inconsistent fin d in g s irresp ectiv e of stu d y q u ality , or less th a n th ree low
qu ality stu d ies available
W e only p rese n t prognostic factors w h ich in at least one s tu d y sh o w ed a statistically significant
association. Preferably, w e d eriv ed th e associations fro m th e m u ltiv ariate results. If only
u n iv a riate resu lts w ere p rese n ted in th e o rig in al stu d y , w e u sed th ese u n iv a riate associations to
d eterm in e th e stre n g th of evidence.
W e p rese n t resu lts of th e stu d ies o n MUS, so m atisatio n d iso rd er a n d h y p o ch o n d riasis
separately.
Figure 1. Selection of studies
Excluded (n=50)
after reading the full
publication
Excluded (n=5)
after discussion for
consensus
Course and prognosis, a systematic review | 49
Results
W e retrie v ed a to tal of 4867 p u blicatio n s fro m searches of th e v ario u s electronic b ib lio g rap h ies
(1673 P ub m ed , 933 Psychinfo, 1222 CIN A H L a n d 1039 EMBASE) (see F igure 1). A fter screening
th e titles a n d abstracts, 68 abstracts seem ed to fulfil th e in clu sio n criteria. A fter assessin g th e full
publication, 13 articles fulfilled all inclu sio n criteria a n d w ere in c lu d ed in o u r rev iew .28-40M ajor
reasons for excluding p ap e rs w ere: focus n o t o n p atien ts w ith m edically u n ex p lain e d sy m p to m s
(n=30) a n d no stu d y of prognostic factors (n=14). The reference lists of th e retriev ed p ap e rs d id
n o t reveal any relev an t publication. Six stu d ies re p o rte d on MUS,28-31'36'37 six stu d ies on
h y p o ch o n d ria sis32-35,38,39 a n d one s tu d y o n ab rid g e d so m atizatio n .40 The a b rid g e d d efin itio n of
so m atisatio n re q u ire d the presence of fo u r sy m p to m s in m ales a n d six sy m p to m s in fem ales.41
W e d id n o t fin d an y prosp ectiv e cohort stu d ies o n D S M -IV so m ato fo rm disorders.
The intero b serv er ag reem en t for in clu sio n b etw e en th e tw o rev iew ers (ToH, MB) w as
k
= 0,73
(95 %-CI: 0.59 - 0.87). W e co n sid ered th e stre n g th of ag reem en t to be 'good' .42
Study characteristics
W e fo u n d 6 stu d ies on MUS. Table 1 gives th e d ata of th e q u ality assessm en t of th e in clu d ed
studies. The qu ality score of MUS pub licatio n s ran g e d fro m 62% to 86%. As n o n e of th e in clu d ed
stu d ies described a trea tm e n t su b se q u en t to inclu sio n in th e stu d y co h o rt (item L), w e can n o t
decide o n w h eth e r th e n a tu ra l course w as stu d ie d or course d u rin g tre a tm e n t (as u su a l). Loss to
follow -up ran g e d fro m 0 to 27%.
W e fo u n d one prosp ectiv e cohort s tu d y o n a b rid g e d som atisation. The q u ality of this
p u b licatio n scored 67%.
W e in c lu d e d 6 stu d ie s o n h y p o c h o n d ria sis. T he m e th o d o lo g ic a l q u a lity sco re of
h y p o ch o n d riasis p u blications ran g e d fro m 57% to 76%. (see Table 1) A s in th e MUS stu d ies, in
these six hyp o ch o n d riasis stu d ies ap p licatio n of treatm en ts w as n o t described. So w h e th e r the
n a tu ra l course or course d u rin g tre a tm e n t w as s tu d ie d can n o t be co ncluded. Selection bias and
c o n fo u n d in g w as p rese n t in all stu d ies a n d in fo u r of th e six stu d ies in fo rm atio n bias w as
p rese n ted .32'33'38'39(see T able 1) Loss to fo llo w -u p ran g e d fro m 4% to 36,6%.
A su m m ary of th e stu d y characteristics is p rese n ted in Table 2, in c lu d in g p o p u la tio n , setting,
diagnostic criteria, follow -up a n d baseline ch aracteristics.
F our of th e six stu d ies on MUS are p erfo rm ed in The N eth erlan d s. S tudies re p o rtin g on MUS
d efined MUS as sy m p to m s th a t could n o t be a ttrib u te d to a clear organic cause acco rd in g to the
p h ysician's ju d g m e n t after a th o ro u g h ph y sical ex am in atio n in c lu d in g lab o rato ry tests. So,
p h ysician's ju d g m e n t w as often the m o st im p o rta n t d iagnostic in stru m en t.
50 I Chapter 3
Table 1. Results of the m ethodological quality of prognostic cohort studies on MUS, abridged som atisation
and hypochondriasis
A
B
C
D
F
G
I
c i
US election bias
Q u a lity criteria
J
C o m p le te n ess
-.
of fo llo w -u p
N
O
P
L
Q
R
E
H
K
In fo rm atio n
, .
C o n fo u n d in g
b ias
°
M
S
T
U
.
D escriptive item s
r
Q u a lity
^
a
scorea
Score
,
(%)
MUS
+
+
+
+
-
+
+
+
+
+
+
-
+
+
-
+
+
+
+
+
+
18
86.0
+
+
+
+
+
+
+
+
+
-
+
-
-
+
+
-
+
+
+
-
+
16
76.2
+
+
+
+
+
+
+
+
+
-
+
+
-
+
+
+
+
+
-
16
76.2
C arso n et al.,
200331
+
+
+
+
+
+
+
+
+
+
+
+
14
66.6
Speckens et al.,
+
+
+
+
-
+
-
+
+
+
+
-
13
61.9
+
+
+
+
+
+
+
+
+
+
+
+
13
61.9
+
+
14
66.6
+
-
+
+
+
K ooim an et al.,
200430
De G u c h t et al.,
200429
Speckens et al.,
199636
+
-
-
+
+
-
+
-
-
+
+
199637
H e n n in g se n et al.,
+
200528
A bridged som atisation
+
-
+
+
N oyes et al.,
199435
+
+
+
+
B arsky et al.,
199833
+
+
+
+
-
+
+
-
B arsky et al.,
2000
+
+
+
+
+
+
+
B arsky et al.,
1993
+
-
+
?
+
F e rn a n d e z et al.,
200538
+
+
+
+
-
-
S im on et al.,
200139
+
-
+
+
-
+
G ureje a n d Sim on,
1999
+
+
+
+
+
+
+
+
+
-
+
+
-
+
+
+
+
+
+
16
76.2
+
-
+
+
-
+
+
+
+
+
-
14
66.7
-
+
-
-
+
-
+
+
+
+
-
-
13
61.9
+
+
+
+
+
+
+
+
12
57.1
Hypochondriasis
-
-
+
-
+
+
+
-
+
+
-
+
-
-
-
+
+
+
+
-
12
57.1
+
-
-
-
-
+
+
+
+
+
-
12
57.1
a T otal '+ '.
In these six MUS stu d ies w e fo u n d h ig h levels of h etero g en eity reg a rd in g clinical settin g
(prim ary care, seco n d ary care an d te rtiary care), n u m b e rs en ro lled in th e co h o rt (80 to 377
patients), d u ra tio n of follow -up (6 to 15 m onths) a n d loss to fo llo w -u p (0 to 27%). O nly tw o
stu d ies re p o rte d o n the d u ra tio n of sy m p to m s at b aseline.28'36Speckens et al.36 (1996) re p o rte d a
m e d ian d u ra tio n of sym p to m s of 7,8 m o n th s (range 0-168), w h ereas H en n in g sen et al.28 (2005)
re p o rte d a m e an d u ra tio n of 70 ± 94 m o n th s (m ed ian 26).
The stu d y o n ab rid g e d som atisatio n w as p erfo rm ed in p rim a ry care fro m 15 sites in 14 countries
an d e n ro lled 1596 p atien ts into the cohort. A b rid g ed so m atisatio n w as d iag n o sed a cco rd in g to
th e Som atic S ym ptom s Index (SSI). D u ra tio n of sy m p to m s at in clu sio n w as n o t rep o rted .
Course and prognosis, a systematic review | 51
All stu d ies o n h y p o ch o n d riasis u se d a fo rm al d iagnostic in terv iew to d iagnose p atien ts w ith
h y p o ch o n d riasis as sta te d in th e D S M -III-R . (see Table 2) F ern an d ez et al.38 (2005) in clu d ed
p atien ts w ith h ea lth anxiety. T hese p atien ts sh are m an y characteristics w ith p atien ts suffering
fro m h y p o ch o n d riasis.38D espite the u se of fo rm al d iagnostic in terv iew s, th e re w as considerable
h eterogeneity in th e six in c lu d ed stu d ies. D u ra tio n of fo llo w -u p (one to five years), n u m b ers
en ro lled in the cohort (50 to 129 patien ts) a n d loss to fo llo w -u p (4 to 37%) v ary considerable
b etw een the in c lu d ed studies. O nly tw o stu d ies re p o rte d on d u ra tio n of sy m p to m s a t baseline.
N oyes et al.35 (1994) in c lu d ed p atien ts w ith a m e d ian d u ra tio n of sy m p to m s of 19 (range 2-144)
m o n th s. F ern an d ez et al .38 (2005) re p o rte d th a t w o rries o n h ea lth sta rte d m o re th a n 5 y ears ago in
36% of th e patien ts, w h ereas in 12% of th e p atien ts these w o rries sta rted in th e last 6 m onths.
Course of MUS, somatisation disorder and hypochondriasis
Five o u t of 6 articles o n MUS re p o rte d o n th e course of th e sy m p to m s (see Table 2). Based on
prevalence, th e typical MUS p a tie n t in o u r review is fem ale, b etw e en 35 a n d 45 y ears o ld an d
co n su lted a p rim a ry care practice or seco n d ary care o u tp a tie n t clinic. Irrespective of th e clinical
setting, the m ajority of th e p atien ts w ith MUS (50 to 75%) im p ro v e d u rin g follow -up. H ow ever,
ab o u t 10% to 30% of th e p atien ts d e te rio ra te .
Five o u t of six stu d ies o n h y p o ch o n d riasis re p o rte d o n th e course of h y p o ch o n d riasis. Based on
prevalence, th e typical h y p o ch o n d ria sis p a tie n t is ag ain fem ale a n d b etw e en 35 a n d 45 y ears old.
Fifty to 70% of the p atien ts w ith h y p o ch o n d riasis d id n o t recover. O nly S im on et al.39 fo u n d a
recovery rate in h y p o ch o n d riasis p atien ts of 85%.
The only stu d y o n so m atisatio n d iso rd er stu d ie d a m o d ified concept.40 R ecovery rates w ere
com parable w ith the d ata fo u n d in stu d ies o n MUS p a tie n ts.
Prognostic factors of MUS, somatisation disorder and hypochondriasis
In T able 3 a su m m ary of outcom es m easures, p ro g n o stic factors a n d (stren g th of) significant
associations is given. A p art fro m th e h ig h h etero g en eity in s tu d y characteristics, w e also fo u n d
considerable h eterogeneity in progn o stic factors a n d o utcom e m easu res in th e 13 stu d ies
in c lu d ed in this review .
Four of th e six publicatio n s o n MUS stu d ie d p o te n tia l p ro g n o stic facto rs o n th e outcom e
29,30,36,37
'sy m p to m c h a n g e'.
T here is som e evidence th a t the n u m b e r of sy m p to m s at b aseline p red ic t th e course of MUS. (see
Table 4)
M oreover, it seem s th a t th e m ore serio u s th e co n d itio n at baseline, th e m ore
u n fav o u rab le the prognosis. This is rep rese n ted b y th e factors G en eral H ea lth P ercep tio n
52 I Chapter 3
=
g
s
CT
ar
a
<N
<U
H
3
/
of m ain study characteristics and course of MUS, abridged som atisation, and hypochondrias
Study
quality
(%)
Settingcountry
Number
enrolled
in
cohort
K ooim an
et al.,
2004s”
81
G e n era l in tern a l
m edicine o u tp atien t
clin ic/T h e
N e th e rlan d s
127
De G u c h t
et al.,
200429
76
P rim a ry care
p ra c tic e s /
The N e th e rlan d s
S peckens
et al.,
1996*
76
C arson
et al.,
200331
S peckens
et al.,
199637
Gender
(M/F) and
age
(years±S.D.)
at baseline
Duration of
follow-up
[months
(range)]
Loss to
follow-up
[n ,(%)]
Ju d g em en t
in v estig ato rs on base
of in te rn is t's final
conclusion
14.1 (12.2-17.8)
0
43:84
40.2±12.7
62% im p ro v ed ;
38% n o t
im p ro v e d
377
J u d g m e n t FP
6
59 (16.0)
103:274
43.5±12.2
53.1% decrease
of sym ptom s;
33.6% increase of
sym ptom s;
9.7% sam e
G e n era l m edical
o u tp a tie n t c lin ic /
The N e th e rlan d s
81
Ju d g em en t
in v estig ato rs on
base of m edical
re co rd s
15.2±4.0
0
28:53
39.4±10.7
30%
46%
13%
11%
67
G e n era l neu ro lo g y
o u tp a tie n ts /U K
90
Ju d g m en t
n e u ro lo g ist
8
24 (27.0)
24:42b
42b
46% im p ro v ed ;
41% sam e;
14% w o rse
62
G e n era l m edical
o u tp a tie n t c lin ic /
The N e th e rlan d s
87
J u d g m e n t p h y sician
11.6±0.8
5 (6.0)
N o t giv en
N o t giv en
20%
51%
18%
11%
T ertia ry care clin ic s /
G e rm an y
186
Judgm ent of 2
phy sician s
6
43 (23.0)
84:102b
42.1±13.5b
N o t given
P rim ary
ca re /E u ro p e ,
S o u th A m erica, US
1596
D iagnostic
in terv iew
12
525 (32.9)
N o t giv en
N o t giv en
51.3% re m itted ;
48.7%
u n re m itte d
76
M edicine clin ic/U S
50
D iagnostic
in terv iew
13.8 (12.6-20.3)
2 (4.0)
10:38b
39.6±0.9b
33% re m itted ;
67% u n re m itte d
Barsky
et al.,
1998s3
67
P rim a ry care
clin ic/U S
Q :60
C 2:60
D iagnostic
in terv iew
Q:64.7±6.8
C2:50.2±5.0
Q :13
(15.0)
C :22
(123.3)
22:63b
53.5b
36.5% re m itted ;
63.5%
u n re m itte d
Barsky
et al.,
2000s2
62
P rim a ry care
clin ic/U S
60
D iagnostic
in terv iew
50.2±5.0
22 (36.6)
11:27b
48.0±15.2b
34.2% re m itted ;
65.8%
u n re m itte d
Barsky
et al.,
199334
57
P rim a ry care
clin ic/U S
28
D iagnostic
in terv iew
22.2 (12-35)
6 (21.4)
N o t giv en
N o t giv en
N o t given
F ern a n d ez
et al.,
200538
57
P rim a ry care h ea lth
c e n tre /S p a in
25
S em i-stru ctu re d
in te rv ie w a n d
qu estio n n aire s
11.3
4 (16.0)
6:19
40.1
52% re m itted ;
48% u n re m itte d e
Sim on
et al.,
200139
57
P rim ary
ca re /E u ro p e ,
S o u th A m erica, US
129
D iagnostic
in terv iew
12
N ot
f
given
N o t giv en
N o t giv en
84.5% rem ited ;
15.5%
u n re m itte d
First
author
Criteria for
diagnosis
Course
MUS
H e n n in g se n 62
et al.,
200528
recovered;
im p ro v ed ;
sam e;
w o rse
recovered;
im p ro v ed ;
sam e;
w o rse
A bridged som atisation
G ureje an d
Sim on,
19994”
67
Hypochondriasis
N oyes
et al., 199435
Q : co h o rt 1.
Q : co h o rt 2.
a N u m b e r o f M US; 3.6 % m issing.
b B aseline characteristics on ly ca lculated fo r p a tie n ts w h o co m p lete d the fo llo w -u p perio d .
c A c co rd in g to th e clinical global im p ro v e m e n t scale.
d T ra n sie n t hy p o ch o n d ria sis.
e H e alth anxiety.
f Loss to fo llo w -u p only ca lculated fo r th e w h o le co h o rt of th e W o rld H e a lth O rg an izatio n 's P sychological P roblem in G e n era l H e a lth C are (PPGHC)
, 67
study.
Course and prognosis, a systematic review | 53
Table 3. Prognostic factors
F irst a u th o r
O u tc o m e m e a su re s
P ro g n o stic fa cto rs
D ire c tio n o f s ig n ific a n t a sso c ia tio n s
(1) S y m p to m change
(2) C h an g e in g eneral
h e a lth p e rcep tio n
(3) M edical
c o n su m p tio n
(4) P sychiatric
p ath o lo g y
(a) A lexithym ia
(b) S ociodem ograpic
characteristics
(c) M edical h isto ry
(d) M ental p ro b lem s
(e) Illness b e h a v io u r
(f) S y m p to m ch aracteristics
(g) A ttrib u tio n
S y m p to m change
- L o n g er d u ra tio n o f th e sym p to m : absence of
im p ro v em en t
- H ig h e r n u m b e r of p h y sical sym ptom s:
absence of im p ro v em en t
C h an g e in g en e ral h e a lth p erc e p tio n (GHP)
- L o w e r initial G H P a t baseline: p o o r G H P at
fo llo w -u p
- H ig h e r n u m b e r of p h y sical sym ptom s: p o o r
G H P at fo llo w -u p
- Less pain: p o o r G H P at fo llo w -u p
S tre n g th o f
as s o c ia tio n 3
MUS
K ooim an
et al.,
200430
De G u c h t
et al.,
200429
S peckens
et al.,
1996*
(1) C h an g es in n u m b e r
o f M US
(2) S y m p to m persistence
o rre c u rre n c e
(1) C h an g e in sy m p to m s
(2) C h an g e in fu n c tio n a l
im p a irm e n t
(a) N e u ro tic ism
(b) A lexithym ia
(c) N egative o r p o sitiv e
affective state
(d) S ociodem ographics
(a) G e n d er
(b) A ge
(c) N u m b e r an d d u ra tio n
of sy m p to m s
(d) P sychiatric d iso rd ers
N u m b e r o f M US
- N eg ativ e affect increase fro m T1 to T2:
increase
-P o s itiv e affect decrease fro m T1 to T2:
increase
P resence o f a consistently h ig h n u m b e r of
MUS
- Fem ale: increase
- C on sisten tly h ig h neg a tiv e affect: increase
- D ifficulty in id en tify in g fe elin g s (dim ension
of alexithym ia): increase
C h an g e in sy m p to m s
- F em ale gender: absence o f im p ro v em en t
- H ig h e r n u m b e r of sym p to m s: absence of
im p ro v em en t
C h an g e in fu n c tio n a l im p a irm e n t (FI):
(b, 95% CI)
- H ig h e r FI at baseline: h ig h e r FI a t fo llo w -u p
- H ig h e r age: h ig h e r FI a t fo llo w -u p
C arson
et al.,
200331
(1) C h an g e in global
clinical im p ro v em en t
(a) A ge
(b) G e n d er
(c) H e a lth statu s
(d) M ental state
C h an g e in global clinical i m p ro v e m e n t
- Less p h y sical fun ctio n : absence im p ro v em en t
S peckens
et al.,
199637
(1) R ecovery of
sy m p to m s
(2) C h an g e in m edical
care u tiliz atio n
(a) H y p o c h o n d riasis
(questionnaire; WI)
(b) H y p o c h o n d riasis
(interview )
(c) Illness attitu d e
(d) S o m atosensory
am plification
R ecovery o f sy m p to m sb
- H ig h e r scores on hy p o ch o n d ria sis
q u estio n n aire (WI): less recovery
C h an g e in m ed ica l care u tiliz atio n (n u m b er of
m edical visits)
- H ig h e r scores on illness b eh a v io u r subscale
o f th e illness a ttitu d e scale: increase of
n u m b e r o f m ed ica l visits
(a) A ttrib u tio n
A ffective a n d cognitive sy m p to m s
- O rganic causal a ttrib u tio n : m o re dep ressiv e
sy m p to m s
Q u a lity of life
- O rganic causal a ttrib u tio n : less q u ality of life
H e n n in g se n
et al.,
200528
(1) A ffective and
cognitive sy m p to m s
(2) S om atoform
sy m p to m s
(3) H y p o c h o n d riasis
(4) Q u a lity o f life
£=0.01 (0.005), P<.05
£=0.05 (0.02), P<.05
£=-0.04 (0.01), P<.01
£=0.07 (0.03), P<.05
£=-0.03 (0.01), P<.05
OR =1.78 (1.33 to 2.39)
OR=0,71 (0.54 to 0.94)
OR =2.29 (1.14 to 4.62)
OR =2.77 (1.46 to 5.27)
OR= 1.08 (1.02 to 1.14)
OR=2.7 (1.01 to 7.4)
£=1.0 (0.1 to 1.9)
£ =0.30 (0.17 to 0.43)
£ =0.03 (0.01 to 0.05)
P<.02
£ =-0.89 (-1.58 to -0.20)
£ =0.31 (0.09 to 0.52)
P<.03
P <.01
A bridged som atisation
G ureje an d
Sim on,
199940
(1) P ersistence of
ab rid g e d
so m atisatio n
(a) G e n d er
(b) S elf-rated p o o r h ea lth
(c) O c cu p atio n al disability
(d) P h y sic ia n -ra ted p o o r
p h y sical h ea lth
(e) D epression
(f) G e n era liz ed anxiety
d is o rd e r
(g) A ge
(h) N u m b e r of cu rren t
sy m p to m s a t baseline
P ersistence o f a b rid g e d som atisation
- S elf-rated p o o r o verall hea lth : p ersisten c e
- M o d e ra te /s e v e re o cc u p atio n al disability:
p ersistence
OR =1.82 (1.32 to 2.52)
OR =1.55 (1.17 to 2.06)
54 I Chapter 3
Table 3. Prognostic factors (continued)
First
author
Outcome
m easures
_
.. . .
Prognostic factors
0
D irection of significant
. ..
0
associations
Strength of
. . a
association
(a) D em o g rap h ics
(b) H e alth care u tiliz atio n
(c) Social ad ju stm en t
(d) O verall fu n c tio n in g
(e) D u ra tio n a n d scores of
hy p o ch o n d ria ca l
sy m p to m s
(f) H e alth p erc e p tio n
(g) S ensitivity to bodily
sen sa tio n s and
en v iro n m e n ta l stim uli
(h) P ersonality,
neu ro tic ism ,
extro v ersio n
(i) C o m o rb id d e p re s s io n o r
anxiety
R em ission of h y p o ch o n d ria sisb
- L o w e r scores of h y p o ch o n d ria ca l sy m p to m s
o n WI: rem ission
- L o w e r scores of h y p o c h o n d ria c a l sy m p to m s
o n SSI: rem issio n
- L o w e r m e a n ra tin g of hy p o chondriasis:
rem issio n
- S h o rter m e a n d u ra tio n o f illness: re m issio n
- H ig h e r level of overall functioning: rem ission
Level o f h y p o ch o n d ria ca l sy m p to m s
- M ore un re alistic fe a r of illness: h ig h e r
- H ig h e r scores on SSI: h ig h e r
- H ig h e r so m ato sen so ry am plification: h ig h e r
- H ig h e r scores on s o m atisatio n (SCL-90):
h ig h e r
-H ig h e r level of neu ro ticism : h ig h e r
- O ld e r age: h ig h e r
- M ore social ad ju stm en t: h ig h e r
Hypochondriasis
N oyes
et al., 199435
(1) R em ission of
h y p o ch o n d ria sis
(2) Levels of
h y p o c h o n d ria ca l
sy m p to m s
Barsky
et al.,
1998”
(1) R em ission of
h y p o ch o n d ria sis
(a) H y p o c h o n d riaca l
sy m p to m s (WI a n d SSI)
(b) H y p o c h o n d riaca l
som atic co m p lain ts (26item s SSI)
(c) S y m p to m s
am plification
(d) F un ctio n al statu s
(e) P sychiatric com orbidity
(f) M edical com orbidity
R em ission of h y p o c h o n d ria s is
- D ecreases in h y p o c h o n d ria c a l som atic
com plaints: re m issio n
Barsky
et al.,
200032
(1) R em ission of
h y p o ch o n d ria sis
(a) H y p o c h o n d riaca l
som atic co m p lain ts (26item s SSI)
(b) S om atosensory
am plification
(c) N o rm a tiv e beliefs ab o u t
h e a lth a n d sickness
R em ission of h y p o c h o n d ria s is
- The 3 -w ay in tera ctio n o f h e a lth n o rm s x
h y p o ch o n d ria ca l som atic co m p lain ts x
am plification significantly in cre ase d the
likelihood of a diag n o sis of hy p o ch o n d ria sis
af follow -up
Barsky
et alA,
199334
(1) H y p o c h o n d riaca l
sy m p to m s
(2) S om atisation
(3) D isability
(a) A ge
(b) G e n d er
(c) P erso n a lity d is o rd e r
(d) H e a lth statu s
(e) S om atosensory
am plification
(f) H y p o c h o n d riaca l
sy m p to m s (WI)
(g) H y p o c h o n d riaca l
som atic co m p lain ts (SSI)
(h) In term ed iate activities
of d aily living
N u m b e r of h y p o c h o n d ria c a l sy m p to m s
- H ig h e r so m ato sen so ry am plifications: m ore
h y p o ch o n d ria ca l sy m p to m s
F ern a n d eze
et alA,
200538
(1) P ersisten t hea lth
anxiety
(a) D e p ressio n / anxiety
(b) N eg ativ e affectivity
(c) S om atic disco m fo rt
(d) P ersonal a n d fam ily
experiences re la ted to
illness th ro u g h o u t
child h o o d
(e) C u rre n t stress a n d
illness
(f) S ociodem ographics
(g) S atisfaction w ith
m edical atten tio n
(h) E v alu a tio n o f state of
h e a lth
(i) D egree of h e a lth anxiety
P ersistent h e a lth anxietyb
- Less p o s itiv e m edical self- ev a lu atio n of
h e a lth p ro b lem s: persisten c e
- G re a te r deg ree of self-judged h e a lth anxiety:
persisten c e
(a) A nxiety
(b) D epressive d is o rd e r
N o significant association fo u n d
S im on et al.,
200139
(1) P ersistence of
h y p o ch o n d ria sis
P<.05
P<.05
P<.05
P<.05
P<.05
r=0.4; P = 0 1
r=0.4; P = 0 1
r=0.39; P = 0 1
r=0.38; P = 0 2
r=0.36; P=.02
r=0.34; P = 0 2
r=0.34; P=.02
P<.05
OR=0.98
P n o t given
P=.031
P=.049
WI: W hitely Index; SSI: S om atic S y m p to m In ventory; SCL-90: S y m p to m Checklist-90.
A d ju sted estim ates a n d 95% CI.
b O nly u n iv a ria te re su lts available (crude estim ates a n d 95% CI, significant differences of associations).
,
c The m ea su re o f h y p o ch o n d ria ca l s y m p to m s at fo llo w -u p w a s th e s u m of the W hitely Index x 5.6 + th e S om atic S ym ptom
Course and prognosis, a systematic review | 55
(GHP), degree of pain, physical fu n ctio n in g a n d illness b eh av io u r. It is u n clear w h e th e r fem ale
g en d er p red icts an u n fav o u rab le course of MUS as tw o stu d ies fo u n d th a t g en d er w as of
prognostic significance, w h ereas one s tu d y fo u n d th a t g en d er w as n o t of p ro g n o stic
significance.31 S tudies o n com orbid m en tal h ea lth p ro b lem s su ch as affective state an d
alexithym ia sh o w ed conflicting results.29'30'36
W e fo u n d w ea k evidence th a t p o o r self-ev alu atio n of overall h ea lth a n d for o ccupational
disability a t baseline p red icts persisten ce of ab rid g e d so m atisatio n .40
P otential prognostic factors o n recovery of h y p o ch o n d riasis w ere stu d ie d in fo u r p u b licatio n s
(see Table 3 ).32'33'35'39 W e fo u n d som e evidence for th e n u m b e r of som atic co m p lain ts o n the
Som atic S ym ptom In ventory (SSI) a t baseline p red ic tin g recovery of h y p o ch o n d riasis. A higher
score p red ic ts persistence of h y p o ch o n d riasis (Table 4).33'35 F u rth erm o re w e fo u n d w ea k
evidence for the p rognostic v alu e on th e course of h y p o ch o n d ria sis of sy m p to m s scores o n the
W hitley Index, rate of severity of hypo ch o n d riasis, d u ratio n , level of fu n ctio n in g a n d degree of
un realistic fears of illness. A gain, it looks like th a t th e m o re serio u s th e co n d itio n a t baseline, the
m ore u n fav o u rab le th e outcom e (i.e. p ersisten ce of h y p o ch o n d riasis). P sychiatric com orbidity
seem s n o t to influence the course of h y p o ch o n d riasis,33'35'38'39 w h ereas so m ato sen so ry
am plification seem ed to influence the o u tco m e of h y p o ch o n d riasis in tw o stu d ies M'æ
Discussion
Main results
A lth o u g h a lot of research is done o n the ep id em io lo g y of, a n d in te rv en tio n s fo r m edically
un ex p lain e d sym ptom s, w e are n o t aw a re of a system atic review of th e literatu re th a t focuses on
th e course an d th e p rognosis of m edically u n ex p lain e d sy m p to m s. C reed a n d B arsky7
p erfo rm e d a system atic rev iew
of th e e p id em io lo g y of s o m a tisa tio n d iso rd e r an d
h y p o ch o n d riasis to exam ine the characteristics a n d asso ciated fea tu re s of these diso rd ers.
H ow ever, th ey d id n o t system atically search a n d stu d y p ro g n o stic factors.7 So, th is is th e first
system atic review w h ich system atically search ed for stu d ies o n p ro g n o stic factors in th is area.
G enerally, th e in c lu d ed stu d ies w ere of good quality. H o w ev er, th e h etero g en eity b etw een
those in c lu d ed stu d ies reg a rd in g clinical setting, n u m b e rs en ro lled in the cohort, d u ra tio n of
follow -up, loss to follow -up, prognostic facto rs a n d outcom e m easu res u se d is considerable.
This lim its direct com parability of th e stu d ies an d m akes it difficult to d raw reliable conclusions.
The stu d ies o n MUS an d a b rid g e d som atisatio n sh o w ed im p ro v e m en t rates of 50 % or m ore. This
is b etter th a n w e expected. H ow ever, 10 to 30% of p atien ts w ith MUS d eterio rate. G iv en th e large
56 I Chapter 3
Table 4. Strength of evidence of prognostic factors w ith a significant influence on outcome in m ultivariate analysis
Prognostic factor
Outcome
QS>60%
S y m p to m change
S y m p to m change
S y m p to m change
S y m p to m change
S y m p to m change
S y m p to m change
C h an g e in g eneral h e a lth p e rcep tio n
C h an g e in g eneral h e a lth p e rcep tio n
C h an g e in g eneral h e a lth p e rcep tio n
C h an g e in global clinical im p ro v em en t
D ifference in fu n c tio n a l im p airm en t
C h an g e in m edical care u tiliz atio n
Q u a lity of life
y2 (50%)
2 / 3 (66%)
1 / 2 (50%)
1 / 2 (50%)
2 / 2 (l00%)
1 / 3 (33%)a
1 /1 (100%)
1 / 1 (100%)
1 / 1 (100%)
1 / 1 (100%)
1 / 1 (100%)
1 / 1 (100%)
Persistence of ab rid g e d so m atisatio n
P ersistence of ab rid g e d so m atisatio n
1 / 1 (100%)
1 / 1 (100%)
R em ission o f h y p o ch o n d ria sis
R em ission o f h y p o ch o n d ria sis
R em ission o f h y p o ch o n d ria sis
R em ission o f h y p o ch o n d ria sis
R em ission o f h y p o ch o n d ria sis
R em ission o f h y p o ch o n d ria sis
H y p o c h o n d riaca l s y m p to m level
H y p o c h o n d riaca l s y m p to m level
H y p o c h o n d riaca l s y m p to m level
H y p o c h o n d riaca l s y m p to m level
H y p o c h o n d riaca l s y m p to m level
H y p o c h o n d riaca l s y m p to m level
H y p o c h o n d riaca l s y m p to m level
N u m b e r hy p o ch o n d ria ca l sy m p to m s
C h an g e in h e a lth anxiety
C h an g e in h e a lth anxiety
1 /1
2 /2
1 /1
1 /1
1 /1
1 /1
1 /1
1 /1
1 /1
1 /1
1 /1
1 /1
1 /1
QS<60%
Strength ° f
evidence
MUS
A ffective s ta te /d e p re s s iv ity
F em ale g en d e r
A lexithym ia
S y m p to m d u ra tio n
N u m b e r of sy m p to m s
H y p o c h o n d riasis q u estio n n aire (WI)
Initial G H P
N u m b e r of p h y sical sy m p to m s
P ain
P hysical fu n c tio n
Age
Illness b e h a v io u r subscale o f IAS
A ttrib u tio n
1 / 1 (100%)
Inconclusive
Inconclusive
Inconclusive
Inconclusive
S trong
Inconclusive
W e ak
W eak
W eak
W eak
W eak
W eak
Inconclusive
Abridged somatisation
S elf-rated o verall he a lth
O c cu p atio n al disability
-
W e ak
W e ak
Hypochondriasis
H e alth n o rm s x s o m atisatio n x am plification0
H y p o c h o n d riaca l som atic c o m p lain ts (SSI)
H y p o c h o n d riaca l sy m p to m s (WI)
R ating of h y p o ch o n d ria sis
D u ra tio n of illness
Level of overall fu n c tio n in g
U n realistic fe a r of illness
H y p o c h o n d riaca l sy m p to m s (SSI)
S o m atosensory am plification
S om a tisa tio n (SCL-90)
N eu ro tic ism
Age
Social a d ju stm en t
S o m atosensory am plification
S elf-evaluation of h e a lth p ro b lem s
D egree o f self-judged h e a lth anxiety
(100%)
(100%)d
(100%)
(100%)
(100%)
(100%)
(100%)
(100%)
(100%)
(100%)
(100%)
(100%)
(100%)
1 / 1 (100%)
1 / 1 (100%)
1 / 1 (100%)
W eak
S trong
W eak
W eak
W eak
W eak
W eak
W e ak
W e ak
W eak
W eak
W eak
W eak
Inconclusive
Inconclusive
Inconclusive
O nly fa cto rs are p re s e n te d w h ich scored significant associations in a t least one stu d y .
QS: Q u a lity score; IAS: Illness A ttitu d e Scale.
a Significant association on ly in one s tu d y w ith u n iv a ria te analysis.
b O nly u n iv a ria te analysis available
c O nly th e th ree -w a y in tera ctio n significantly im p ro v e d th e m odel a n d in cre ase d th e likelihood o f a diag n o sis o f h y p o ch o n d ria sis at follow -up.
d S ignificant association in one s tu d y w ith m u ltiv a riate analysis a n d in one s tu d y w ith u n iv a ria te analysis.
n u m b e rs of p atien ts p rese n tin g w ith MUS in p rim a ry a n d seco n d ary care, d eterio ratio n of one
th ird of these p atien ts still m eans th a t large n u m b e rs of p atien ts w ith MUS are g oing to get
w orse. The stu d ies o n h y p o ch o n d riasis sh o w ed a less optim istic picture: th e m ajority of these
p atien ts (50 to t 70%) do n o t recover d u rin g follow u p. This m ig h t be d u e to th e d efin itio n of
h y p o ch o n d riasis w h ich req u ires p atien ts to h av e sy m p to m s for six m o n th s or m o re .
W e d id n o t fin d an y prosp ectiv e s tu d y o n course or p ro g n o stic factors in p atien ts w ith D S M -IV
som atoform disorders. A s th e evidence for th e n u m b e r of sy m p to m s at baseline in MUS as a
prognostic factor o riginate fro m only tw o of th e in c lu d ed MUS stu d y , w e conclude th at, th ere is
som e evidence th a t th e n u m b e r of sy m p to m s at b aselin e p red icts th e course of MUS. In the
stu d ies on h y p o ch o n d riasis w e fo u n d som e ev idence th a t th e som atic sy m p to m score o n th e SSI
Course and prognosis, a systematic review | 57
at baseline p red icts the course of h y po ch o n d riasis. F u rth erm o re, th e co n d itio n of p atien ts w ith
MUS at baseline, rep rese n ted by h ea lth p erc ep tio n an d physical fu n ctio n in g , a n d th e co n d itio n
of p atien ts w ith h y p o ch o n d riasis at baseline, rep rese n ted by ra tin g of severity, physical
fu n ctio n in g a n d d u ra tio n o f illness, sh o w ed a w ea k asso ciatio n w ith th e o utcom e of MUS an d
h y pochondriasis. So, w e conclude th a t th e re is som e evidence th a t th e serio u sn ess of the
conditions of p atien ts w ith MUS or h y p o ch o n d riasis a t baseline m ig h t be of p rognostic
significance.
W e fo u n d only w ea k evidence for m an y o th er p ro g n o stic factors. E vidence o n g en d er to b e of
prognostic significance w as inconclusive. R em arkably, w e fo u n d no evidence to s u p p o rt the
influence of psychiatric com orbidity an d p erso n ality traits o n th e course of MUS, ab rid g e d
so m atisatio n an d hypochondriasis.
Comparison with the literature
A lth o u g h only a m in o rity of th e MUS p rese n ted d u rin g co n su ltatio n re su lt in a chronic
condition, p atien ts w ith MUS are prob lem atic in h ea lth care.4P hysicians p erceive th ese p atien ts
as difficult a n d d em an d in g .43,44 T hey also believe th a t p atien ts w ith MUS increase h ea lth care
costs d u e to sickness absence a n d service use, th a t th ey are at risk for u n n ecessary diagnostic
procedures. P hysicians express the n ee d to p re v e n t som atic fix atio n in these p atien ts.45-47
H ow ever, w e fo u n d th a t th e p rogn o sis of MUS in p rim a ry a n d seco n d ary care is m ore
fav o u rab le th e n expected, as th e m ajority of th e p atien ts w ith MUS im prove. A possible
ex p lan atio n for th is fin d in g is th a t im p ro v e m en t of sy m p to m s is p artly cau sed by reg ressio n to
th e m ean because sym p to m s are o n th eir w o rst w h e n selecting p atien ts d u rin g p rim a ry or
seco n d ary care clinic visits.
H ow ever, o u r fin d in g th a t th e m ajority of th e p atien ts w ith h y p o ch o n d riasis do n o t recover is
su p p o rte d by the literatu re in w h ich h y p o ch o n d riasis is co n sid ered to be a chronic
condition.3'48,49 A lthough, according to th e literatu re, sp o n ta n eo u s recovery of h y p o ch o n d riasis
is rare, w e fo u n d recovery rates of 35% to 50%. A possible e x p lan atio n for th is fin d in g m ig h t be
th e p ro ce d u re as req u ired for inclusio n in th e s tu d y cohorts. This p ro ce d u re is an extensive
clinical assessm ent consisting of diagnostic in terv iew s a n d ad d itio n a l te stin g an d m ig h t in itself
be of th erap eu tic im portance.50'51
G iving th e m an y factors h y p o th e siz ed to be p ro g n o stic for a chronic course of MUS,
som atisatio n d iso rd er a n d hypoch o n d riasis, th ere is n o t m uch evidence o n th ese factors.
A lth o u g h p erso n ality traits, in c lu d in g n eu ro ticism a n d alexithym ia,52'53 a n d psychiatric
com orbidity, in c lu d in g anxiety a n d d ep ressio n 54-56 h av e b een d em o n strate d to be associated
w ith MUS a n d hypoch o n d riasis, only a lim ited n u m b e r of stu d ies h av e ex am in ed th eir
58 I Chapter 3
prognostic value. In th is review w e d id n o t fin d evidence for th eir p ro g n o stic v alue.29'30'33'35"39
H ow ever, in w ell d efined m edically u n ex p lain e d sy n d ro m es su ch as chronic fatig u e sy n d ro m e
an d irritable bow el sy n d ro m e the evidence o n p ro g n o stic factors is m u c h stro n g er.57-61 C airns et
al. fo u n d th a t less fatigue severity at baseline, a sense of control o ver sy m p to m s an d n o t
a ttrib u tin g illness to a physical cause w ere asso ciated w ith a good outcom e.57 T heir fin d in g s of
th e p rognostic significance of th e fatig u e sev erity at baseline is in line w ith o u r fin d in g s.
Strengths and limitations
In this system atic review , w e u se d an extensive search strateg y to id en tify relev an t studies. We
a d d e d rigor to o u r s tu d y by p re-testin g th e search strateg y o n p u b licatio n s ab o u t MUS in our
o w n d atab ase a n d by searching all rele v an t d atab ases w ith o u t lan g u ag e restriction. M oreover,
w e h a d good intero b serv er ag reem en t for in- a n d exclusion. Finally, w e in d e p en d e n tly
extracted d ata a n d assessed the qu ality of in c lu d ed stu d ies w ith a v alid ated checklist.
Because th e q u ality of the in d iv id u a l stu d y influences outcom es, w e p rese n ted o u r results
to g eth er w ith a q u ality score of each stu d y . So, w e v isu alize th e su scep tib ility of each stu d y for
bias. C urrently, n o sta n d a rd iz e d m e th o d is available to assess th e q u ality of p ro g n o stic studies.
T herefore, w e u se d a checklist of p red e fin e d criteria w h ich has b een u se d in p rev io u s prognostic
20'21
review s.
The m e d ian n u m b e r of p articip a n ts en ro lled in th e co h o rts of th e in c lu d ed stu d ies in th is review
is 87. O nly one stu d y o n MUS, one s tu d y o n a b rid g e d so m atisatio n a n d n o n e of th e stu d ies on
h y p o ch o n d riasis en ro lled m ore th a n 200 p atien ts into th e cohort.29,40 These low n u m b e rs of
p articip a n ts in the cohorts lim its th e stre n g th of th e evidence concern in g o u tco m e an d
p rognostic factors.
O nly a m inority of the in c lu d ed stu d ies p rese n ted sufficient d ata o n th e d u ra tio n of sy m p to m s at
baseline. T herefore, it is n o t clear w h eth e r th e s tu d y p atien ts w ere all in c lu d ed at a sim ilar p o in t
in th e course of th eir disease. S tudies rep o rtin g d u ra tio n of sy m p to m s at b aselin e sh o w ed a
considerable ran g e of d u ra tio n of sym p to m s. This also lim its th e in te rp re ta tio n of o u r results.
A n o th er lim itation of th is review is th e absence of a d etailed d escrip tio n of trea tm e n ts d u rin g
follow -up. The resu lts of o u r stu d y ap p ly to th e course of MUS, h y p o ch o n d riasis an d
som atisatio n d iso rd er in th e m edical system . W e assu m e th a t d u rin g th e stu d ies in all p atien ts
som e k in d of trea tm e n t has b een ap p lied , a lth o u g h no s tu d y re p o rte d o n th is .
As statistical p o o lin g w as n o t p ossible becau se of th e h ig h h etero g en eity of stu d y p o p u latio n s,
p rognostic factors a n d outcom e m e asu res am o n g in c lu d ed stu d ies, w e p erfo rm ed a best
Course and prognosis, a systematic review | 59
evidence synthesis. A lth o u g h such a q u alitativ e analysis is n o t as objective as a m eta-analysis,
w e w ere able to su m m arize the v alu e of p ro g n o stic in d icato rs w h ich tak es th e m ethodological
qu ality into account.62
Implications for further research and clinical practice
The pessim istic v iew s of G Ps a n d th e ir w o rries ab o u t th e d ev elo p m en t of som atic fix atio n in
p atien ts w ith MUS a n d ab rid g e d so m atisatio n m ig h t n o t alw ay s b e ju stified as th e m ajority of
these p atien ts generally h av e a fav o u rab le p rognosis. H o w ev er, th e m ajority of th e p atien ts w ith
h y p o ch o n d riasis do n o t recover su g g estin g th a t h y p o ch o n d riasis is a m ore severe condition.
E stablishing th e n u m b e r of som atic sy m p to m s a n d serio u sn ess of th e co n d itio n in p atien ts w ith
MUS or h y p o ch o n d riasis d u rin g th e first co n su ltatio n s m ig h t help G Ps to v alu e th e risk of
p ersistence a n d m ay gu id e G Ps w h e th e r to offer o nly reassu ran ce ab o u t th e fav o u rab le
p ro g n o sis or, for th e h igh-risk patien ts, a m o re in ten siv e ap p ro a ch su ch as reattrib u tio n .
H ow ever, d u e to its heterogeneity, th e d ata collated in this system atic review o n p rognostic
factors are in a d eq u a te to iden tify p red icto rs of th e course of MUS, so m atisatio n d iso rd er an d
hypo ch o n d riasis. T herefore, it is difficult to ad v ise clinicians h o w to d istin g u ish b etw een
patien ts w ith low a n d h ig h risks of p ersisten c e.
A lth o u g h it is w id ely accepted th a t p erso n ality traits a n d co m orbid d ep ressio n a n d anxiety are
associated w ith MUS, so m atisatio n d iso rd er a n d h y p o ch o n d riasis, stu d ies ex am in in g th eir
prognostic v alu e show conflicting results. A s a consequence of th e p au c ity of c u rre n t research,
th e re is n ee d for m ore w ell co n d u cted p ro sp ectiv e cohort stu d ies w ith a reaso n ab le n u m b e r of
patien ts (>200 patients), in w h ich assessm en t of trea tm e n ts d u rin g fo llo w -u p a n d in clu sio n of
patien ts at a sim ilar p o in t in th e course of th e ir disease are im p o rta n t topics.
A lth o u g h w e kn o w for long th a t th e d o cto r-p atien t relatio n sh ip effects th e o utcom e of
consultations a n d can be therap eu tic, n o n e of th e in c lu d ed stu d ies to o k th e d o cto r-p atien t
relatio n sh ip into account.63-65The m ore non-specific aspects of co n su ltatio n su ch as described in
th e p atien t-c en tred clinical m e th o d n eed s atten tio n in fu tu re research .66
60 I Chapter 3
Appendix A. Search strategy
(som atoform d iso rd er [mesh] OR so m atizatio n [tw] OR so m atisatio n [tw] OR h y p o ch o n d riasis
[mesh] OR n e u ra sth e n ia [mesh] OR co n v ersio n d iso rd er [mesh] OR so m ato fo rm disorder* [tw]
OR h y p o c h o n d ria sis [tw] OR n e u ra sth e n * [tw] OR c o n v e rsio n d iso rd er* [tw] OR
p s y c h o p h y s io lo g ic a l d is o r d e r
[M esh ]
O R p s y c h o s o m a tic
m e d ic in e
[M esh ]
OR
psychophysiological disorder* [tw] OR psychosom at* [tw] OR p sy chosom atic m ed icin e [tw]
OR functional som atic sym pt* [tw] OR fu n ctio n al som atic syndrom * [tw] OR fu nctional
syndrom * [tw] OR u n ex p lain e d sym pt* [tw] OR m edically u n ex p lain e d [tw] OR u n ex p lain ed
m edical sym pt* [tw] OR psychogen* [tw] OR non-organ* [tw] O R non-specific com plain* [tw]
OR non-specific sym pt* [tw]) A N D (incidence[M eSH :noexp] OR m ortality[M eS H Term s] OR
follow u p studies[M eSH :noexp] OR prognos*[Text W ord] OR predict*[Text W ord] OR
course*[Text W ord]) A N D (((Prospective stu d ies [mesh] OR cohort stu d ies [mesh] OR follow u p stu d ies [mesh] OR o b servational stud* [tw] OR p ro sp ectiv e stud* [tw] OR co h o rt stud* [tw]
OR follow -up stud* [tw])) OR ((rando m ized co n tro lled trial [pt] OR co n tro lled clinical trial [pt]
OR ran d o m ized controlled trials [mh] OR ra n d o m allocation [mh] OR d o u b le-b lin d m eth o d
[mh] OR single-blind m e th o d [mh] OR clinical trial [pt] OR clinical trials [mh] OR "clinical trial"
[tw] OR ((singl* [tw] OR doubl* [tw] OR trebl* [tw] OR tripl* [tw]) A N D (mask* [tw] OR blind*
[tw])) OR "latin square" [tw] OR placebos [mh] OR placebo* [tw] OR random * [tw] OR research
d esig n [m h:noexp] OR co m p arativ e stu d y [mh] OR ev a lu a tio n stu d ies [mh] OR follow -up
stu d ies [mh] OR prosp ectiv e stu d ies [mh] OR cross-over stu d ies [mh] OR control* [tw] OR
prospectiv* [tw] OR volunteer* [tw]) N O T (anim al [mh] N O T h u m a n [mh])))
Appendix B. Criteria list for assessing the methodological quality of
prognostic cohort studies on chronic medically unexplained
symptoms
Criteria
Score
Study population
A. Description of inception cohort
B. Description of study population
C. Description of relevant inclusion and exclusion criteria
D. Definition of chronic functional somatic symptoms
E. Num ber of subject in study population ä 200
+/
+/
+/
+/
+/
-/
-/
-/
-/
-/
?
?
?
?
?
Response
F. Response rate ä 75%
G. Information about non-responders versus responders
+/ -/ ?
+/ -/ ?
Follow-up (extend and length)
H. Follow-up of at least 12 months
I. Loss-to-follow-up < 20%
J. Information about completers versus those loss-to-follow-up
K. Prospective data collection
+/
+/
+/
+/
-/
-/
-/
-/
?
?
?
?
Course and prognosis, a systematic review | 61
Treatment
L. Description of possible treatm ent in cohort
+/ -/
Outcome
M. Clinically relevant outcome measures
N. Standardized assessment of symptom outcome
O.
Standardized assessment of functional outcome
+/ -/
+/ -/
+/ -/
Prognostic factors
P. Standardized assessment of potential prognostic factors
+/ -/
Analysis
Q. Appropriate univariate crude estimates
R. Appropriate multivariate analysis techniques
+/ -/
+/ -/
Data presentation
S. Frequencies of most im portant outcome measures presented
T. Frequencies of most im portant prognostic factors presented
U. Influence of prognostic factors presented
+/ -/
+/ -/
+/ -/
+, positive (design or conduct adequate);
-, negative (design or conduct inadequate);
?, unclear (insufficient information)
Appendix C. Explanation of the criteria of the checklist for
methodological quality
A.
D escription of inception cohort
Positive if it is described in w hat setting the subjects were recruited (i.e. general population, patients attending the
general practitioner, inpatient or outpatient setting).
B. D escription of study population
Positive if it is described which subjects from the inception cohort are recruited and if age and sex are described.
C. D escription of relevant inclusion and exclusion criteria
Positive if it is described how subjects were identified w ith chronic functional somatic symptoms (CFSS) or
somatization.
+ = CFSS or somatization diagnosed by the general practitioner or standardized diagnostic interview
- = CFSS or somatization diagnosed by a (standardized) self-administered sym ptom checklist
? = not clear
D. D efinition of chronic functional somatic sym ptom s
Positive if the definition is described of CFSS or somatization.
E. N um ber of subjects in study population ä 200
Positive if the num ber of subjects w ith CFSS or somatization in the study population was at least 200 at baseline.
F. Response rate ä 75%
Positive if response rate is at least 75%. Response rate: the num ber of patients in the study population, divided by the
num ber of subjects in the inception cohort.
G. Inform ation about non-responders versus responders
Positive if demographic or clinical information (such as age and sex) was presented for responders and
nonresponders, or if there was no selective response, or no nonresponse.
H. Follow-up of at least 12 m onths
Positive if the follow-up period was at least 12 months.
I. Loss-to-follow-up < 20%
Positive if total num ber of patients w ith CFSS or somatization was at least 80% at the end of follow-up compared to
the num ber of participants with CFSS or somatization at baseline. Loss to follow-up: the num ber of patients in the
study population at baseline minus the num ber of patients at the main health status measurement for the main
outcome measure at the end of follow-up, divided by the num ber of patients in the study population at baseline.
J. Inform ation about com pleters versus those loss-to-follow-up / dropouts
Positive if demographic or clinical information (such as age and sex, disease characteristics and other potential
prognostic predictors) was presented for completers w ith CFSS or somatization and those lost to follow-up at the
m ain moment of outcome m easurement, or if there was or no selective loss-to-follow-up, or no loss-to-follow-up.
K. Prospective data collection
Postive if m ain outcome measures on potential prognostic predictors was collected prospectively.
L. D escription of possible treatm ent in cohort
Positive if treatm ent subsequent to inclusion in cohort is fully described or standardized. Also positive if no treatment
is given.
62 I Chapter 3
M.
N.
O.
P.
Q.
R.
S.
T.
U.
+ = treatm ent/m ultivariate correction for treatm ent in analysis, or no treatm ent given
= different treatment regimens, not clear how outcome is influenced by it
? = not clear if any treatm ent is given
Clinically relevant outcome measures
Positive if at least one of the following outcome measures is presented: CFSS / somatization diagnosis, symptoms,
remission or recurrence, functional status, social functioning, lost days of work, quality of life, impairment, mortality.
Standardized assessm ent of sym ptom outcome
Positive if standardized questionnaires or objective outcome measurements of at least one of the following three
outcome measures were used for each follow-up measurement:
a. CFSS / somatization diagnosis
b. Symptoms
c. Remission or recurrence
Standardized assessm ent of functional outcome
Positive if standardized questionnaires or objective outcome measurements of at least one of the following six
outcome measures were used for each follow-up measurement:
a. functional status
b. social functioning
c. lost days of w ork
d. quality of life
e. impairm ent
f.
mortality
Standardized assessm ent of potential prognostic factors
Positive if standardized questionnaires or objective measurements were used at baseline of at least 4 of the following
18 potential prognostic factors:
a. sex
b. age
c. marital status
d. family history of CFSS/somatization
e. race
f.
social economic status (SES)
g. education level
h. num ber of episodes of CFSS/somatization
i.
sick leave
j.
functional impairment
k. comorbidity (i.e. anxiety disorder or chronic disease)
l.
duration of symptoms
m. social support
n. stressful life events
o. difficult doctor-patient relationship
p. coping strategy
q. perception of symptoms (i.e. illness attitude, somatosensory amplification)
r.
personality traits
A ppropriate univariate crude estim ates
Positive if separate univariate (repeated measures) analysis of variance were calculated for each dependent measure.
A ppropriate m ultivariate analysis techniques
Positive if multivariate (repeated measures) analysis of variance were calcultated for changes among the dependent
measures occuring during the follow-up interval.
Frequencies of m ost im portant outcome m easures presented
Positive if frequency, percentage or mean, m edian (interquartile range) and standard deviation/confidence intervals
are reported of the most im portant outcome measures.
Frequencies of m ost im portant prognostic factors presented
Positive if:
a. frequency of percentage is reported, or
b. mean and standard deviation or standard error are reported, or
c. m edian and interquartile range are reported, or
d. if the influence of each separate factor is reported
Influence of prognostic factors presented
Positive if the influence of each separate prognostic factor on the natural course of CFSS or somatization is presented.
Course and prognosis, a systematic review | 63
Reference List
1
K roenke K, M angelsdorff AD. C om m on sy m p to m s in am b u lato ry care: incidence,
ev aluation, th erap y , a n d outcom e. A m J M ed 1989; 86(3):262-266.
2
B arsky AJ, Borus JF. S om atizatio n an d m ed icalizatio n in th e era of m a n ag e d care. JAMA
1995; 274(24):1931-1934.
3
K ellner R. S om atization an d H y po ch o n d riasis. N ew York: P raeger; 1986.
4
V erhaak PF, M eijer SA, V isser AP, W olters G. P ersisten t p rese n tatio n of m edically
u n ex p lain e d sy m p to m s in general practice. Fam P ract 2006; 23 (4) :414-420.
5
A m erican P sychiatric A ssociation. D iagnostic an d statistical m a n u al of m en tal d iso rd ers. 4
ed. W a sh in g to n (DC) : A m erican P sychiatric A ssociation; 1994.
6
W orld H ea lth O rganisation. The ICD-10 classification of m en tal a n d b eh av io u ral disorders:
7
C reed F, Barsky A. A system atic review of th e ep id em io lo g y of so m atisatio n d iso rd er an d
8
S m ith GR, Jr., M onson RA, Ray DC. P sychiatric co n su ltatio n in so m atizatio n d iso rd er. A
diagnostic criteria for research. G eneva: W o rld H ea lth O rganisation; 1993.
hypoch o n d riasis. J Psychosom Res 2004; 56(4):391-408.
ran d o m ized co ntrolled stu d y . N Engl J M ed 1986; 314(22):1407-1413.
9
D eyo RA, D iehl AK. P atien t satisfaction w ith m edical care for low -back pain. S pine 1986;
11(1):28-30.
10 olde H a rtm a n TC, franke L, L ucassen PLBJ, v an S p aen d o n ck K.P.M., v a n W eel C.
E xplaining th e unexplainable: fam ily physicians' m a n ag em en t of p atien ts w h o freq u en tly
p rese n t m edically u n ex p lain e d sy m p to m s. A focus g ro u p stu d y . A n n F am M ed 2008;
subm itted.
11 E pstein RM, Q uill TE, M cW hinney IR. S o m atizatio n reco n sid ered : in c o rp o ratin g the
p atien t's experience of illness. A rch In tern M ed 1999; 159(3):215-222.
12 R osendal M, Bro F, Sokolow ski I, Fink P, Toft T, O lesen F. A ran d o m ised co n tro lled trial of
brief train in g in assessm ent a n d trea tm e n t of som atisation: effects o n GPs' attitu d es. Fam
P ract 2005; 22(4):419-427.
13 M ayou R, F arm er A. ABC of psychological m edicine: F unctional som atic sy m p to m s an d
sy n d ro m e s. BMJ 2002; 325(7358):265-268.
14 R ief W , S h a rp e M. S o m a to fo rm
d is o r d e r s - n e w
a p p r o a c h e s to
c la s s ific a tio n ,
conceptualization, an d treatm ent. J P sychosom Res 2004; 56(4):387-390.
15 B ennett JC. Inclusion of w o m en in clinical trials--policies for p o p u la tio n su b g ro u p s. N Engl J
M ed 1993; 329(4):288-292.
16 L aupacis A, W ells G, R ichardson WS, T ugw ell P. U sers' g u id es to th e m edical literatu re. V.
H ow to use a n article ab o u t prognosis. E vidence-B ased M edicine W orking G ro u p . JAMA
1994; 272(3):234-237.
17 W ilczynski NL, H aynes RB. O p tim al search strateg ies for id en tify in g m en tal h ea lth co n ten t
in MEDLINE: a n analytic survey. A n n G en P sy ch iatry 2006; 5:4.
64 I Chapter 3
18
C ohen J. A coefficient of agreem en t for n o m in al scales. E d u catio n al a n d psychological
m e asu rem en t 1960; 20:37-46.
19 H am ilto n W T, G allagher AM, T hom as JM, W hite PD. The p ro g n o sis of different fatig u e
diagnostic labels: a lo n g itu d in al survey. F am P ract 2005; 22(4):383-388.
20 H erm en s ML, v a n H o u t H P, T erlu in B, v a n d er W in d t DA, B eekm an AT, v a n DR et al.
The p ro g n o sis of m inor d ep ressio n in th e g eneral p o p u latio n : a system atic review . G en
H osp P sychiatry 2004; 26(6):453-462.
21 Scholten-Peeters GG, V erhagen AP, B ekkering GE, v a n d er W in d t DA, Barnsley L,
O o ste n d o rp RA et al. P rognostic factors of w h ip lash -asso ciated d iso rd ers: a system atic
review of prosp ectiv e cohort stu d ies. P ain 2003; 104(1-2):303-322.
22 H u d a k PL, Cole DC, F rank JW. P erspectives on p ro g n o sis of soft tissu e m usculoskeletal
disorders. Int J Rehabil Res 1998; 21(1):29-40.
23 A ltm an DG. System atic review s of ev alu atio n s of p ro g n o stic variables. BMJ 2001;
323(7306):224-228.
24 H a y d e n JA, C ote P, B om bardier C. E v alu atio n of th e q u ality of p ro g n o sis stu d ies in
system atic review s. A n n In tern M ed 2006; 144(6):427-437.
25 K uijpers T, v a n d er W in d t DA, v a n d er H eijd en GJ, B outer LM. System atic review of
prognostic cohort stu d ies o n sh o u ld e r diso rd ers. P ain 2004; 109(3):420-431.
26 Sackett DL, S traus SE, R ichardso n WS. H o w to practice an d teach EBM. G uidelines.
E dinburgh: C hurchill L ivingstone; 2000.
27 A riens GA, v a n MW , B ongers PM, B outer LM, v a n d er WG. P hysical risk factors for
neck pain. Scand J W ork E nviron H ea lth 2000; 26(1):7-19.
28 H en n in g sen P, Jakobsen T, S chiltenw olf M, W eiss MG. S o m atizatio n revisited: d iagnosis
an d perceived causes of com m on m en tal d iso rd ers. J N erv M ent D is 2005; 193(2):85-92.
29 De G ucht V, Fischler B, H eiser W. P erso n ality a n d affect as d eterm in a n ts of m edically
u n ex p lain e d sy m p to m s in p rim a ry care; A fo llo w -u p stu d y . J P sychosom Res 2004;
56(3):279-285.
30 K ooim an CG, Bolk JH, R ooijm ans HG, T rijsburg RW. A lexithym ia does n o t p red ic t the
persistence of m edically u n ex p lain e d phy sical sy m p to m s. Psychosom M ed 2004;
66(2):224-232.
31
C arson AJ, Best S, P ostm a K, Stone J, W arlow C, S h arp e M. The o utcom e of n eu ro lo g y
o u tp a tie n ts w ith m edically u n ex p lain e d sym ptom s: a p ro sp ectiv e co h o rt stu d y . J N eu ro l
N eu ro su rg P sychiatry 2003; 74(7):897-900.
32 Barsky AJ, Bailey ED, Fam a JM, A h ern DK. P red icto rs of rem issio n in DSM
h y pochondriasis. C om pr P sychiatry 2000; 41(3):179-183.
33 B arsky AJ, F am a JM, Bailey ED, A h ern DK. A p ro sp ectiv e 4- to 5-year s tu d y of DSM-IIIR h y pochondriasis. A rch G en P sychiatry 1998; 55(8):737-744.
34 B arsky AJ, C leary PD, Sarnie MK, K lerm an GL. The course of tran sien t h y p o ch o n d riasis.
A m J P sychiatry 1993; 150(3):484-488.
Course and prognosis, a systematic review | 65
35
N oyes R, Jr., K athol RG, F isher M M, P hillips BM, S uelzer MT, W o o d m an CL. O ne-year
follow -up of m edical o u tp a tie n ts w ith h y p o ch o n d riasis. Psychosom atics 1994; 35(6):533545.
36 Speckens AE, v a n H em ert AM, Bolk JH, Rooijm ans H G , H en g ev eld MW. U n ex p lain ed
physical sym ptom s: outcom e, u tiliza tio n of m edical care a n d asso ciated factors. Psychol
M ed 1996; 26(4):745-752.
37 Speckens AE, v a n H em ert AM, S p in h o v en P, Bolk JH. The d iagnostic a n d p rognostic
significance of th e W hitely Index, th e Illness A ttitu d e Scales a n d th e Som atosensory
A m plification Scale. P sychol M ed 1996; 26(5):1085-1090.
38 F ern an d ez C., F ern an d ez R., Isaac A m igo D. C haracteristics a n d one-y ear fo llo w -u p of
p rim a ry care p atien ts w ith h ea lth anxiety. P rim ary Care a n d C o m m u n ity P sychiatry
2005; 10(3):81-93.
39 S im on GE, G ureje O, F u llerto n C. C ourse of h y p o ch o n d riasis in an in te rn atio n a l p rim ary
care stu d y . G en H osp P sychiatry 2001; 23(2):51-55.
40 G ureje O, S im on GE. The n a tu ra l h isto ry of so m atizatio n in p rim a ry care. P sychol M ed
1999; 29(3):669-676.
41 E scobar JI, W aitzkin H , Silver RC, G ara M, H o lm a n A. A b rid g ed som atization: a stu d y
in p rim a ry care. Psychosom M ed 1998; 60(4):466-472.
42
C h m u ra KH, P eriyakoil VS, N o d a A. K appa coefficients in m edical research. Stat M ed
2002; 21(14):2109-2129.
43 Lin EH, K aton W , V on K orff M, B ush T, Lipscom b P, R usso J et al. F ru stra tin g patients:
physician a n d p a tie n t persp ectiv es a m o n g d istre ssed h ig h u sers of m edical services. J
G en In tern M ed 1991; 6(3):241-246.
44 Ring A, D ow rick C, H u m p h ris G, S alm on P. Do p atien ts w ith u n ex p lain e d physical
sym p to m s p ressu rise general p ractitio n ers for som atic treatm en t? A q u alitativ e study.
BMJ 2004; 328(7447):1057.
45 S m ith GR, Jr., M onson RA, Ray DC. P atien ts w ith m u ltip le u n ex p lain e d sym ptom s.
Their characteristics, functional health , an d h ea lth care u tilization. A rch In tern M ed
1986; 146(1):69-72.
46 Barsky AJ, E ttner SL, H orsk y J, Bates DW. R esource u tiliza tio n of p atien ts w ith
hypoch o n d riacal h ealth anxiety a n d som atization. M ed C are 2001; 39(7):705-715.
47 G rol R. To heal or to harm . The p rev e n tio n of som atic fix atio n in G en eral Practice. 1981.
48 K ellner R. P rognosis of tre a te d h y p o ch o n d riasis. A clinical stu d y . A cta P sy ch iatr S cand
1983; 67(2):69-79.
49 K ellner R. D iagnosis a n d trea tm e n ts of h y p o ch o n d riacal sy n d ro m es. P sychosom atics
1992; 33(3):278-289.
50 G u th rie B. W hy do general p ractitio n ers take blood? A cross-sectional s tu d y of use of
b lo o d tests in UK general practice. E ur J G en P ract 2001; 7:138-142.
66 I Chapter 3
51
Little P, C antrell T, R oberts L, C h ap m an J, L an g rid g e J, P ickering R. W hy do GPs
perfo rm investigations?: The m edical a n d social ag e n d as in arran g in g back X-rays. Fam
P ract 1998; 15(3):264-265.
52 V assend O. N eg ativ e affectivity, subjective som atic co m plaints, a n d objective h ealth
indicators. M ind a n d b o d y still sep arated ? In: M aes S, L eventhal H , Jo h n sto n M, editors.
In tern atio n al review of h ea lth psychology, vol. 3. C hichester: W iley; 1994. 97-118.
53 D e G u ch t V, H eiser W. A lexithym ia a n d som atisation: q u an tita tiv e review of the
literature. J P sychosom Res 2003; 54(5):425-434.
54 F ink P. P sychiatric illness in p atien ts w ith p ersisten t som atisation. Br J P sychiatry 1995;
166(1):93-99.
55 B arsky AJ, W yshak G, K lerm an GL. P sychiatric co m o rb id ity in DSM-III-R
hypoch o n d riasis. A rch G en P sych iatry 1992; 49(2):101-108.
56 N oyes R, Jr., K athol RG, F isher M M, P hillips BM, S uelzer MT, W o o d m an CL. Psychiatric
com orbidity am o n g p atien ts w ith h y p o ch o n d riasis. G en H o sp P sychiatry 1994; 16(2):7887.
57 C airns R, H o to p f M. A system atic review d escrib in g th e p ro g n o sis of chronic fatig u e
syndrom e. O ccup M ed (Lond) 2005; 55(1):20-31.
58 T habane M, K ottachchi DT, M arshall JK. System atic rev iew a n d m eta-analysis: The
incidence an d p ro g n o sis of post-infectious irritab le b ow el sy n d ro m e. A lim ent
P harm acol T her 2007; 26(4):535-544.
59 Joyce J, H o to p f M, W essely S. The p ro g n o sis of chronic fatig u e a n d chronic fatig u e
syndrom e: a system atic review . QJM 1997; 90(3):223-233.
60 C hitkara DK, v a n T ilburg M A, B lois-M artin N , W h iteh ead WE. Early life risk factors th a t
co n trib u te to irritable b ow el sy n d ro m e in ad u lts: a system atic review . A m J
G astroenterol 2008; 103(3):765-774.
61 El-Serag HB, P ilgrim P, Schoenfeld P. System ic review : N a tu ra l h isto ry of irritab le bow el
syndrom e. A lim ent P harm acol T her 2004; 19(8):861-870.
62 L icht-S trunk E, v a n d er W in d t DA, v a n M arw ijk H W , de H M , B eekm an AT. The
p rognosis of d ep re ssio n in older p atien ts in g eneral practice a n d th e co m m unity. A
system atic review . F am P ract 2007; 24(2):168-180.
63 S tew art MA, M cW hinney IR, Buck CW. The d o c to r/p a tie n t relatio n sh ip a n d its effect
u p o n outcom e. J R Coll G en P ract 1979; 29(199):77-81.
64 Balint M. The doctor, his p a tie n t a n d th e illness. E d inburgh: C hurchill L ivingstone; 2000.
65 M cW hinney IR. A textbook of Fam ily M edicine. N ew York; O xford: O xford U niversity
Press; 1989.
66 S tew art M. Reflections o n th e d o cto r-p atien t relationship: fro m ev idence a n d experience.
Br J G en P ract 2005; 55(519):793-801.
Course and prognosis, a systematic review | 67
70 I Chapter 4
Summary
Purpose.
The interactio n b etw e en FPs a n d p atien ts w ith p ersisten t m edically u n ex p lain ed
sym p to m s (p ersistent MUS) is describ ed as com plicated. A lth o u g h p ersp ectiv es of p atien ts
w ith an initial p rese n tatio n of MUS are stu d ied , research o n p ersp ectiv es of p atien ts w ith
p ersisten t MUS are lacking. K now ledge of o p in io n s of p atien ts w ith a lo n g h isto ry of p resen tin g
MUS m ig h t gu id e in terv en tio n s to im p ro v e th e care for th ese p atients.
Methods.
A q u alitativ e ap p ro ach , in te rv iew in g 17 p atien ts w ith p ersisten t MUS. D ata w ere
an aly zed u sin g a n iterativ e process acco rd in g to th e p rin cip les of co n stan t com parative
analysis.
Results.
P atients w ith p ersisten t MUS stressed th e im p o rtan ce of a p erso n al co n tin u in g
d o cto r-p atien t relationship. Such a relatio n sh ip is b u ilt o n p h y sician attitu d e , m edical
com petence, availability an d sh a re d au th o rity . P atien ts w a n t to be ta k en serio u s in a n o n ju d g m e n ta l o p en com m unication style. They ap p reciate a th o ro u g h ex p lo ratio n a n d a
com prehensible ex p lan atio n of th e sy m p to m s. F u rth erm o re, th ey w a n t a co m p eten t FP w h o is
easy accessible an d w h o engage th e m as p a rtn e rs in th e co n su ltatio n an d th e decision m ak in g
process.
Conclusions.
P atients w ith p ersisten t MUS v alu e a h ealin g F P -p atien t relatio n sh ip . They
ap p re cia te a p atien t-cen tered com m u n icatio n a n d o rien tatio n to care in w h ich p erso n al
co n tin u ity an d continuity of th e relatio n sh ip are im p o rta n t elem ents.
O pinions of patients w ith persistent MUS, an interview study | 71
Introduction
P hysical sym p to m s such as h eadach e, back p ain , dizzin ess a n d fatig u e are com m o n in the
general p o p u la tio n a n d m o st peo p le do n o t contact pro fessio n al m edical care for these
sy m p to m s.1-3In those w h o do p rese n t th ese sy m p to m s, ph y sician s o ften do n o t fin d a n organic
cause (i.e. m edically u n ex p lain e d sym p to m s).4;5F o rtu n ately , m edically u n ex p lain e d sy m p to m s
(MUS) have a beneficial course w h e th e r or n o t as a re su lt of physicians' m a n ag em en t.6 O nly a
m inority of p atien ts w ill develop persistent MUS. Exactly th ese p atien ts rep rese n t a serious
p ro b lem in h ea lth care as they suffer fro m th eir sy m p to m s, are fu n ctio n ally im p a ired , an d are at
risk for p o ten tially h arm fu l a d d itio n a l te stin g an d trea tm e n t.5;7
The interactio n b etw e en FPs a n d p atien ts w ith persistent MUS is d escrib ed as com plicated.
E ncounters b etw e en FPs an d these p atien ts o ften leave b o th w ith fru stra tio n a n d confusion.8-10
W hile the FP persp ectiv e on persistent MUS has b een stu d ie d ,11;12research o n p atien ts' v iew s an d
experiences reg a rd in g the care they receive is still lim ited. K n ow ledge in th is area is n ecessary in
o rd er to im prove the care for these patients.
E xisting know ledge reg a rd in g p a tie n t p ersp ectiv es o n MUS o rig in ates fro m p atien ts w ith an
initial p rese n tatio n of u n ex p lain e d sy m p to m s.11;13-15This research p o in te d o u t th a t p atien ts often
feel stig m atized a n d n o t ta k en serious,16th a t th ey o ften w ish to h av e a convincing, leg itim atin g
an d em p o w e rin g ex p lan atio n for their sy m p to m s,17-20 a n d th a t th ey w a n t em otional s u p p o rt
fro m th eir FP.21 F u rtherm ore, analysis of v id e o ta p e d co n su ltatio n s in p rim a ry care rev ealed a
m ism atch b etw e en w h a t p atien ts w ith initial MUS w a n t a n d w h a t th ey actu ally receive fro m
th eir FP.13;14This m ism atch m ig h t exp lain w h y p atien ts fre q u en tly exp ress th eir dissatisfaction
w ith the m edical care received d u rin g th eir illness. H o w ev er, it is u n clear to w h a t ex ten t these
resu lts can be generalized to p atien ts w ith persistent MUS in p rim a ry care. S tu d ies in p atien ts
w ith the distinctive fun ctio n al sy n d ro m es chronic fatig u e sy n d ro m e (CFS) an d irritab le bow el
sy n d ro m e (IBS) co ncluded th a t p atien ts feel dissatisfied because of th e delay of or confusion
o ver the diagnosis, the a ttitu d e of the d o ctor a n d the in a d eq u a te a n d o ften conflicting
info rm atio n given by their d octors.22123
In o rd er to im prove the m a n ag e m en t of p atien ts w ith persistent MUS in fam ily m edicine, w e
p erfo rm ed an interview s tu d y focusin g on th e o p in io n s of p atien ts w ith a long h isto ry of
p rese n tin g MUS to th eir FP.
72 I Chapter 4
Method
Study sample
W e co n d u cted 17 sem i-stru ctu red in terv iew s w ith p atien ts w ith p ersisten t MUS w h o recently
atte n d e d the FP. W e selected 12 p atien ts fro m th e C o n tin u o u s M o rb id ity R eg istratio n (CMR)
project an d 5 p atien ts fro m th ree practices of th e authors.
CMR project
W e selected p atien ts w h o w ere d iag n o sed w ith persistent MUS for th e first tim e b etw e en 2006
an d 2008 fro m the CMR database. W e in v ited p atien ts ag ed > 18 years, w h o w ere longer th an
one y ear o n th e practice list, w ith o u t lan g u ag e barriers, p sychiatric diseases (anxiety d isorder,
d epressive d iso rd er, PTSS, d ru g or alcohol abuse) or cognitive disabilities acco rd in g to th eir FP
(n = 59). T hese p atien ts w ere sen t a letter a n d if n ecessary a rem in d er in w h ich w e ask ed th em to
p articip a te in an interview s tu d y re g a rd in g th e q u ality of care th ey receive fro m th eir FP. A total
of 31 p atien ts re sp o n d e d to this letter a n d 12 p atien ts v o lu n te ered to participate.
In th e CMR project of th e D ep a rtm en t of P rim ary a n d C o m m u n ity care at th e R ad b o u d
U niv ersity N ijm egen M edical C entre ev ery ep iso d e of illness seen by, or re p o rte d to, th e FP is
reg istered as soon as it is established u sin g a n a d a p te d v ersio n of th e E-list.24-27As far as w e are
aw are, th e CMR project is the only m o rb id ity reg istra tio n sy stem w ith a stru ctu ra l p o ssibility to
classify p atien ts w ith persisten t MUS .28;29
Table 1. Patient characteristics
Characteristic
Age in years (mean (range))
50.4 (27-76)
Sex
- Women
- Men
15
2
Level of education3
- Low
- Middle
- ffigh
5
6
6
Situation of living
- W ith partner
- W ith partner and children
- Single
9
4
4
Time on practice list
- < 1 year
- 1-3 years
- 3-5 years
- > 5 years
0
2
2
13
a Education level was classified as low (primary and lower secondary education), m iddle (upper secondary education, until age 17-18), and
high (pre-university, higher vocational training, and university)
O pinions of patients w ith persistent MUS, an interview study | 73
Authors practices
The 5 p atien ts selected fro m th e au th o rs' practices w ere u se d to test th e in terv iew g u id e an d to
train the interview technique. T hey w ere selected as th ey p ersisten tly co n su lted w ith sym p to m s
th a t could n o t be attrib u te d to a clear organic cause (as d escrib ed in th e CMR project). We
in c lu d ed these p atien ts in th e analysis as th e in terv iew s p ro v id e d rich data.
S ociodem ographic details (age, sex, m a rital statu s, level of ed u catio n , an d tim e o n th e practice
list) w ere o b tain ed fro m th e particip an ts. A su m m ary of p atien ts ch aracteristics of the 17
in terv iew ed p atien ts is sh o w n in T able 1.
Semi-structured interviews
O ne of the au th o rs (JN) co n d u cted th e se m i-stru ctu red in terv iew s at th e p atien t's hom e. These
in terv iew s w ere recorded, tran scrib ed verb atim , a n d en tered into A tlas.ti, a so ftw are p ro g ram
for the analysis of q u alitativ e data. The in terv iew er w as g u id e d by a list of topics, b ased on
im p o rta n t topics h ig h lig h ted in the literatu re re g a rd in g p atien ts' v iew s o n MUS. (see Table 2)
O p en qu estio n s w ere u se d to encou rag e p atien ts to com m u n icate th e ir v iew s o n im p o rta n t
aspects of the care th ey receive for th eir p ersisten t MUS.
A s th e collection of d ata an d th e analysis in q u alitativ e research is an iterativ e process, tw o
researchers (ToH, PL) a d d e d relev an t topics to th e in terv iew topic list after a p relim in ary
analysis of th e first five interview s. Ideas a n d th o u g h ts th a t em erg ed in p rim a ry stages of the
analysis w ere b ro u g h t back to su b se q u en t in terv iew s as th e s tu d y proceeded.
Analysis
The interv iew s w ere an aly sed in d e p en d e n tly by tw o research ers (ToH, HvR) after re a d in g the
tran sc rip ts several tim es to fam iliarize th em selv es w ith th e d ata. The tw o research ers co d ed the
tran sc rip ts an d co m p ared a n d d iscussed these codes w ith each other. C odes in each in terv iew
w ere co m p ared w ith those in oth er interview s. A d d itio n al codes, w h ich em erge from
discussions w ere also a p p lied to th e tran scrip ts. C oncepts a n d categories em erg ed th ro u g h this
iterativ e process of coding, analysis a n d d iscu ssio n (constant co m p arativ e q u alitativ e
analysis).30;31 The resu lts of the analysis w ere d iscu ssed w ith a th ird research er (PL). D ata
collection co n tin u ed u n til sa tu ra tio n w as reach ed a n d no n ew th em es em erg ed .32
74 I Chapter 4
Table 2. Interview guidebook
Jnderstanding, recognition and support
- Do you think your FP understands your symptoms and problems?
- Are you satisfied w ith the help and support you get from your FP?
- Does your FP take your symptoms serious?
;Ps' consulting behaviour
- Did you discuss your own thoughts a n d /o r concerns regarding your symptoms w ith your FP?
- Did you get enough space to communicate your own feelings and emotions during the consultations?
- Did your FP do additional diagnostic tests, and w hat do you think of that?
- Did your FP give you the advice to come back for a new, possibly longer consultation?
ime and attention
- Do you think you get enough space and time to discuss your symptoms and problems?
- Do you think your FP has enough attention during the consultation?
- Did you feel hurried during the consultation?
knowledge and interest in the patient's context
- Does your FP know about your personal circumstances?
- Did your FP discuss the influence of y our sym ptom s/problem s on your daily life?
- Did you discuss w ays of coping w ith your sym ptom s/problem s during consultation?
xplanation and reassurance
- H ow did your FP explain the symptoms to you?
- Did your FP give you a diagnosis for your symptoms?
- W hat did you think of the explanation of your symptoms, did it satisfy you?
- Did your FP give you advice on how to handele your symptoms?
hared decision making
- W hat did you expect your FP w as going to do (referral, additional diagnosic tests, etc.) w ith your symptoms?
- Did your FP explain/discuss the treatm ent plan to /w ith you?
- Did you and your FP make a shared decision on the treatm ent plan?
rust
- H ow do you characterize/perceive the doctor-patient relationship?
- Did the doctor-patient relationship change over time?
uality of care
- Are you satisfied w ith the quality of care you received from your FP for your sym ptom s/problem s?
- Which elements in the quality of received care are important and which are less im portant for you?
Results
FP-patient relationship
P atients indicate th a t they w a n t a w arm , p erso n al co n tin u in g F P -p atien t relatio n sh ip . S uch a
relatio n sh ip m akes it easier for p atien ts to discuss sy m p to m s an d p ro b lem s w ith th e ir FP.
P atients m en tio n th a t th e re has to be a m atch b etw e en th e FP an d th e p atien t. F u rth erm o re, they
state th a t the F P -patient relatio n sh ip is b u ilt o ver tim e .
'it used to be that the distance between the doctor and the patient was really big. Now, the distance is
much smaller. You're basically on the samefooting now [...] I fin d that much nicer'
(P1 : fem ale, age 59)
'I have the sense that it clicks. I feel good and safe there. I don ' t feel like that there are certain things I
would be reluctant to say' (P13: fem ale, age 28)
'I've had the same FP since I was 19 so you really do know each other, also because, before all the vague
complaints started, I would go to m y FP for this or that, a sore throat and what not. And,actually, m y
history of vague health complaints is already so long that we 've come to know what to expectfrom each
other and how to play into each other. ' ( P3: fem ale, age 33)
O pinions of patients w ith persistent MUS, an interview study | 75
W e could d istin g u ish fo u r key-them es o n w hich, acco rd in g to th e in te rv iew ed p atien ts, a
satisfy in g F P -p atien t rela tio n sh ip is b u ild : p h y sician s attitu d e , m ed ical com petence,
availability an d sh a re d au th o rity . These co m p o n en ts are describ ed in F igure 1.
Physician attitude
Shared authority
Non judgemental
Attentive listening
Paying attention to fears
Partnering
Respecting patient values
Discussing referral
p
th
it
tnts
ie
at
p
to
diin
r
cco
Figure 1.. D octor-patient relationship m odel a
ersistent MUS
A vailability
M edical competence
Easily accessible
Taking time
Follow-up
Active involvement
Knowledge
Taking symptoms seriously
Clear explanation
Referral w hen neccessary
1. Physician attitude
Patients state th a t they w an t an FP w ith an o p en m in d u sin g a n o n-judgm ental com m unication
style. Such a com m unication m akes patients feel at ease an d free to tell their story. F urtherm ore, it
m akes patients feel free to visit their FP. P atients expect an FP to be an attentive listener show ing a
lot of understanding.
'and then he says, have a seat. A n d then I start to talk, o f course (...) and he listens. (...) he let's me first
tell m y story (...) I can say whatever I want to say. So, that's nice.' (P4: fem ale, age 29)
'she has an active way of listening. She knows me (...) then responds and her voice is so understanding.
It's like, Okay, I understand that is very frustrating for you.' (P3: fem ale, age 33)
'You ju st notice that she really listens. She is not thinking, what am I going to eat this evening?' (P13:
fem ale, age 28)
Patients appreciate FPs w ho take the sym ptom s as w ell as the p erso n seriously. W hen patients
notice th a t the FP does n o t take them seriously, they hesitate or even po stp o n e to go to the FP.
F urtherm ore, they feel pow erless, according to the in terview ed patients. K now ing th a t the FP
takes him or her seriously is reassuring. Some p atients fear th a t frequently visiting the FP w ill have
a negative influence o n the FP's attitude. P atients state th a t it can take quite som e tim e before they
have the feeling of being taken seriously.
76 I Chapter 4
'I'm always reluctant to go to m y FP because I don't feel like I am taken seriously. (...) It's really
humiliating and it makes you really feel sad because you have pain and you can't explain it. You can't
ju st say, I do have pain! I need more tests.' (P5: fem ale, age 76)
'I: Do you have any idea how long it took before you got the impression that he does take you seriously,
that he believes you? P: Well, I think that it took about a year.' (P9: m ale, age 75)*
*I = interviewer; P =patient
Patients appreciate it if the FP p ays atten tio n to em otions. W hen the FP is n o t p ay in g atten tio n to
the patient's fears, this can resu lt in a feeling of n o t being tak en seriously. P atients state th a t talking
about the fear is n o t alw ays enough, som etim es a referral for reassurance is necessary.
'so that more attention is paid to your feelings? Yeah, I'd definitely appreciate that. Yes.'
(P1: fem ale, age 59)
'I: A n d were you able to then discuss thatfear with your FP? P: Yes, I did do that. I said, I am scared. A nd
he dealt with that well. He said, W hat are you scared of? I am scared that I have some kind o f cancer in m y
bowels. Then he examined m y belly and he started to talk about stress (...) I really appreciated the fact
that he did that but, in the back of m y mind, I thought (...) I think that he kind o f felt that and so he said,
Well, I'll refer you to your specialist.' (P6: fem ale, age 60)
2. Medical competence
Patients w a n t a skillful a n d com petent FP. Som eone w ho, from the first presentation, takes a close
look at the sym ptom s to find o u t w h at is w ro n g a n d w h o gives good advice. They w a n t a doctor
w ho reacts quickly, sharply an d adequately to the sym ptom s p resen ted d u rin g the consultation.
F urtherm ore, the FP's attitu d e has to be positive an d supporting.
'I'll take care of thatfor you. I know we'll make it through this.' (P1: fem ale, age 59)
'that it's properly examined to determine if something is wrong or if it is serious or if it ju st requires some
rest, that someone ju st takes a look to fin d out what's going on and ju st gives you good advice.' (P13:
fem ale, age 28)
W hen the FP an d the p atient together get stuck w ith the sym ptom s, som e p atien ts stress th at
referral to specialty care is necessary.
'sometimes, I think, send someone to the specialist earlier. All too often, it's we'll try this medication
first. I f it doesn't work, we'll try another kind o f medication. Then you can keep coming back and only
after a really long time do you get a referral.' (P5: fem ale, age 76)
O pinions of patients w ith persistent MUS, an interview study | 77
Some patients stress the im portance of getting a diagnosis for their sym ptom s. Patients state that
such a diagnosis is im portant b o th for them selves an d for their FP. H ow ever, p atients realize an d
accept the difficulty FPs face w h en searching for a diagnosis for their v ag u e com plaints.
'on the one hand, it changes absolutely nothing. On the other, it allows me to label it and then I can look
for a solution more effectively. A n d I think that it is also important for m y FP. Then he can also be more
focused and effective in lookingfor a solution together with me.' (P3: fem ale, age 33)
All patients stressed the n eed for an explanation for their sym ptom s in com prehensible language.
D ifferent explanations from different doctors confuse patients. P atients expect explanations about
w h a t is going o n in their body. They w a n t to know w h ere their sym ptom s com e from an d how
their body functions.
'Then she explains it to me in a really simple fashion. She says, this and that...and that's w hy your body
reacts differently and that's w hy you have those complaints. (...) Now she is the first that has given me
that kind of concrete information' (P8: fem ale, age 27)
Patients also m ention exam ples of explanations w hich contain a link betw een physical an d
psychological processes.
'He explained that the mind and the body are connected, and that maybe, yeah, if (...) the psychological
pressure were off (...) then maybe things would improve. So, I totally understood the explanation.'
(P8: fem ale, age 27)
If th e FP does n o t know the origin of the sym ptom s, patien ts appreciate the doctor m entioning
this.
Experiences of the p ast are taken into account w h en patien ts ju d g e the FP's m edical com petence.
Patients regard a good past perform ance of th e FP in d iagnosing an d treatin g sym ptom s as very
im portant: it strengthens the FP's m edical com petence an d patients' tru st in the doctor.
'earache, ear drops - you walk around with this for a week and only then do they send you to the hospital.
You end up with a double ear infection that has to be lanced...yeah, then I'm angry!'
(P5: fem ale, age 76)
'usually he [the FP] tries to figure it out himself. He suspected that there was something in m y knee
because of strain or overuse. A n d what did it turn out to be? Indeed, it was strain. He was right!'
(P4: fem ale, age 29)
78 I Chapter 4
Som etim es patients question the m edical com petence as a resu lt of stories of other patien ts in
w h o m som ething w en t w rong.
3. Availability
Patients have experienced quite som e fru stratio n s concerning the access to their FP. They m ention
th a t their 'own' FP is n o t available d u rin g evenings, n ig h ts an d w eekends. M oreover, n o t all FPs
w o rk fulltim e. Some patients fin d it difficult th at they have to w ait several days before they can see
their FP. Furtherm ore, patients dislike discussions w ith the practice n u rse before they are allow ed
to have an app o in tm en t w ith their FP.
'He only works 2 or 3 days a week. So, usually, when you call to make an appointment, he's already
booked. The first available appointment is normally about 2 weeks away. I think that's really
unfortunate.' (P11:fem ale, age 52)
'Whenever you call for something or about something, the assistant always screens the calls and w on't
put you through. I want to speak to the doctor himself about something. Then you need to do a lot to be
put through, (...) I say, I want to speak to him directly, and then the assistant says, But what is it about?
And, it's n o tp o ssib le.a n d it's constant blocking' (P11: fem ale, age 52)
P atients state that they need an FP w h o takes tim e for them . The lim ited consultation tim e
som etim es has a negative influence on the contact w ith th e FP, m any patien ts consider the
sta n d ard of 10 m inutes consultation tim e too short. Some m entioned the long tim e they sp e n d in
the w aiting room a n d the feeling of h u rry w hich this causes d u rin g the consultation.
'It's not like, you're in, you're out. He really does take the timefor you. He lets you finish talking.'
(P4: fem ale, age 29)
'Yeah, you always have to wait. You're never seen on time (...) I feel the time pressure and I see it clearly
in him [the FP]. (...) Obviously, that's not good.' (P11: fem ale, age 52)
Patients appreciate follow -up appointm ents, especially w h en initiated by the FP, an d the
possibility of longer consultation tim e. A ctive involvem ent from the FP, for exam ple visiting a
p atient spontaneously after a m ajor event, is highly app reciated by the patients.
'I had to come back on regular intervals - every three or four weeks or so. N ot that they send you out on
your own tofigure it out. No, it's nice that they keep tabs on you.' (P4: fem ale, age 29)
'I think that they are really concerned and involved and empathic. We have experienced this over the past
couple of months [as m y father was being caredfor prior to his passing] in many different ways. (...) The
FP was wonderful. We got phone calls asking how he was. I am really happy with the guidance and help
we receivedfrom the FP.' (P1: fem ale, age 59)
O pinions of patients w ith persistent MUS, an interview study | 79
4. Shared authority
Patients state th a t they w a n t to be engaged as p artn ers in th e consultation, to look an d search
together for possibilities an d solutions. P atient appreciate the FP for initiating the search for
solutions an d for explaining w h y a certain solution is preferable. H ow ever, som e patien ts w an t to
m ake their o w n choice based o n the p ro v id ed inform ation. They expect the FP to respect their
decision.
'we think about things together. It's not one-way like that I have to think about things on m y own.
Together, we come up with the best approach and determine what's possible.' [...] Together, we try to
fin d the best solution, and then I trust that she [the FP] is the one who takes the lead. That's best.'
(P10: fem ale, age 52)
'she [the FP] helps me make decisions by providing the information needed to make the decision'
(P3: fem ale, age 33)
W hen patients them selves provide solutions, for exam ple in com plem entary or alternative
m edicine, they expect su p p o rt a n d a positive reaction from their FP. Some patien ts stress the
im portance of clarifying their o w n ideas, thoughts, w ishes a n d n eed s to the FP.
'the FP w asn't open to that. In any event, he didn't suggest it. A n d when I then said, maybe this is
something for a homeopath?, he said, Yeah, that's up to you. I don't really have a lot o f faith in that. So,
obviously, I'm not really encouraged to explore those options. I don't think that's very good.'
(P11: fem ale, age 52)
'Well, then, at a certain point in time, I ju st decided to go see a craniosacral therapist. He thought that
was odd. It's crazy that she [the FP] didn't tell me that that also exists.' (P1: fem ale, age 59)
Patients stress their problem s w ith FPs resistance for referral. But w h en an FP im m ediately agrees
w ith the requested referral or additio n al test, p atients m en tio n ed to be surprised. A positive
response to a request for referral is n o t alw ays necessary as long as the FP has a proposal for further
inquiry.
'then you have to practically beg: Can you please refer me to the neurologist?' (P7: fem ale, age 49)
,I said, at home, to m y husband, I am going to demand a bowel examination. I was incredibly surprised
that he [the FP] was okay with that. I expected that he would say that that wouldn't be necessary.'
(P6: fem ale, age 60)
'He [the FP] always tries to fin d a way to help you himself. I really appreciate that. It's better than being
referred to all sorts of other practitioners and agencies.' (P4: fem ale, age 29)
80 I Chapter 4
Discussion
Summary of main findings
Patients w ith persistent MUS stressed the im portance of a p ersonal continuing FP-patient
relationship. A ccording to these patients, such a relationship is bu ilt o n four com ponents:
physician attitude, m edical com petence, availability an d sh ared authority. Patients w a n t to be
taken serious by an FP w ith an op en m in d w h o uses a n o n-judgm ental com m unication style.
F urtherm ore they w an t a skillful an d com petent FP w h o is su p p o rtin g a n d offers a
com prehensible explanation for their sym ptom s. Patients w ith persisten t MUS also w an t easy
access to their 'own' FP w ho takes tim e to explore an d discuss the patients' sym ptom s a n d /o r
problem s. Finally, patients w an t to be engaged as p artn ers in the consultation in a w ay they can
m ake their o w n choices based o n the p ro v id ed inform ation.
Comparison with existing literature
S tudies on opinions of persistent MUS p atients in p rim ary care reg ard in g the doctor-patient
relationship are scarce. S tudies o n expectations of patien ts d u rin g the initial p resen tatio n of MUS
suggest that physician attitu d e an d m edical com petence are im p o rta n t at the beginning of an
episode of unexplained sym ptom s. H ow ever, o u r patients w ith persistent MUS considered also the
availability of the doctor a n d shared au th o rity of m ajor im portance. This is probably d u e to the
fact that d u rin g the course of persistent MUS personal continuity (i.e. the im portance of seeing a
personal doctor) an d continuity of the relationship w ith the FP becom es m ore a n d m ore
im portant.
Shared au thority reflects the patients' expectations concerning their FP to listen to their treatm ent
proposals a n d to go th ro u g h a process of sh ared decision m aking. Churchill in terview ed fifty
practitioners, w ho w ere identified as "healers" by their peers. S haring au th o rity ap p eared to be
one of the eight healing skills. This skill is described as sh arin g the responsibility for healing at the
v ery beginning of the consultation, recognizing the p atien t as a 'fellow expert', w ith a particular
level of expertise, an d h aving a n d show ing confidence in the relationship w ith the patient.33Scott
conducted in -d ep th interview s about healing relationships w ith FPs an d their patients. A key
process w hich em erged from these interview s w as 'appreciating pow er'. E ngaging p atients as
partn ers in decisions ab o u t diagnosis an d treatm en t w as seen as quintessential. These FPs
reported th a t m ost often they w o rk to increase patients' pow er.34
Patients opinions o n the doctor-patient relationship in o u r stu d y (Figure 1) show great overlap
w ith 'the healing relationship m odel' of Scott et al. a n d 'the eight h ealing skills' of Churchill et al.33;34
H ow ever, the patients interview ed by Scott et al. w ere n o t selected on basis of their illnesses, b ut
they suffered fro m different chronic illnesses. A lthough w e selected p atien ts b ased o n the
O pinions of patients w ith persistent MUS, an interview study | 81
presence of persistent MUS, their perspective u p o n the relationship w ith the doctor does n o t seem
to differ from the other patients w ith chronic conditions. F urtherm ore patients' opinions
reg ard in g the doctor-patient relationship in o u r stu d y seem to be in line w ith the opinions of a
specific group of practitioners reg ard in g healing skills. Churchill described the im portance of
taking tim e for the patients an d d em on stratin g th a t there is space for their story. This fits perfectly
w ith the w ish of the patients w ith persisten t MUS: they w an t their FP to be m indfully present,
listening to their story an d giving them room to tell their story.
Strengths and limitations
This is the first stu d y o n opinions of patients w ith persistent MUS ab o u t the doctor-patient
relationship. M ost of the patients interview ed in o u r stu d y know their FP for m ore th a n 5 years.
F urtherm ore they are included in the stu d y because they visit their FP frequently w ith MUS and
because they are all currently receiving care for persistent u ndifferentiated MUS from their FP.
Therefore, our results reflect the opinions of p atients w h o have h ad recent an d relatively m any
contacts w ith the health care system a n d their FP. These patients have bu ilt their opinions about
the doctor-patient relationship on a b ro ad experience w ith m edical services. As the attitu d e of FPs
tow ards p atients w ith MUS is often negative,“ one could expect th a t the interview ed p atients are
m ore likely to have experienced their consultations as unsatisfactory a n d stressful an d therefore
they m ight be m ore critical ab o u t the doctor-patient relationship th a n others. O n the other hand,
m ost patients included in this stu d y know their FP already for m ore th a n 5 years, w hich possibly
im plicates satisfaction w ith their FP.
The qualitative m eth o d has been recom m ended as th e best m eth o d to explore an d clarify patients'
opinions.35 By u sing a cyclical an d interactive w ay of collecting a n d analyzing data, 'progressive
focusing' an d exploration of patients' opinions in d ep th w as possible.36 T ranscribing the
interview s verbatim , entering the full texts into Atlas.ti, an d coding an d re-organizing d ata by tw o
in d e p en d e n t researchers, stren g th en s o u r findings. A lth o u g h sm all, th e n u m b e r an d
characteristics of participants in clu d ed in o u r stu d y are considered ad eq u ate for cap tu rin g an
optim al v ariety of opinions.37 The findings p resen ted here, how ever, reflect the perceptions of a
sm all g roup of patients an d m ay n o t rep resen t the view s of p atients in general. The valid ity of our
analysis is enhanced by the diversity of train in g an d experience of the analysis team (experienced
FP an d a psychiatrist) an d reflexivity (reflecting on o u r o w n experiences).38
A w eakness of the stu d y is that patients w ere recruited by sen d in g th em a letter an d a rem in d er to
ask for participation in a stu d y reg ard in g the quality of care they receive from their FP. O nly 12 of
the 31 patients (39%) agreed to participate. This m ig h t have caused response bias as p atients w ho
are satisfied w ith their FP are possibly m ore inclined to participate in such a study. Therefore,
certain specific view points could have been left o u t of sight in this study.
82 I Chapter 4
Interview ed patients d id n o t m entio n any expectation ab o u t receiving inform ation ab o u t the
prognosis of the sym ptom s. N one of the patien ts m ad e rem arks ab o u t discussing the d u ratio n of
sym ptom s. This m ight be due to the fact th a t alm ost all in terview ed patien ts h a d chronic
com plaints an d assum e th at the doctor w ill n o t be able to predict the d u ratio n of the sym ptom s.
The doctor-patient relationship is bu ilt over tim e a n d over m any consultations. Interview ing
patients reg ard in g their opinions on the doctor-patient relationship gives only a sn ap sh o t in time.
Patients m ay change their perspective over tim e as a response to th e sym ptom s, diseases, life
events, a n d /o r other circum stances.
Implications for further research and clinical practice
Like patients p resenting initial MUS to their FP, p atients w ith persistent MUS w a n t an m edical
com petent FP w ith an op en non-judgem ental attitude. H ow ever, p atien ts w ith persistent MUS also
w a n t personal continuity a n d a therapeutic doctor-patient relationship.39A n easily accessible FP
w ho is w illing to see the p atient as a p artn er in the decision m aking process contributes to a
patient-centered orientation to care w hich is highly v alu ed by these patients.
The doctor-patient relationship largely d ep en d s o n the com m unication style of the FP. F urther
research sho u ld focus on stu d y in g an d m axim izing the therapeutic effects of FPs' com m unication
to achieve b etter health outcom es in p atients w ith persisten t MUS. A s patien ts appreciate a nonjudgm ental an d attentive listening style, educational pro g ram s in h ealth com m unication
interventions as m indful com m unication m ight be of h e lp M;41 F urtherm ore, stu d y in g the effects of
the (im provem ent of the) quality of the FP-patient relationship o n sym ptom s, im p airm en t and
satisfaction of patients w ill gain significant insights into the how FP-patient relationships
contribute to healing an d w ell-being of patients w ith persistent MUS.
Acknowledgements
W e th an k the FPs from the CMR practices for b eing able to select p atien ts from their practice lists.
W e are grateful to the patients w ho w ere w illing to p articipate in this interview study.
O pinions of patients w ith persistent MUS, an interview study | 83
Reference List
1
K roenke K, A rrin g to n ME, M angelsdorff AD. The p rev alen ce of sy m p to m s in m edical
o u tp a tie n ts a n d th e ad eq u acy of th erap y . A rch In tern M ed 1990; 150(8):1685-1689.
2
G reen LA, Fryer GE, Jr., Y aw n BP, Lanier D, D ovey SM. The ecology of m edical care
revisited. N Engl J M ed 2001; 344(26):2021-2025.
3
v a n de L isdonk EH. E rvaren en aa n g eb o d e n m o rb id iteit in de h u isartsp rak tijk . Thesis.
N ij m egen: K atholieke U niversiteit N ijm egen, 1985.
4
P eveler R, K ilkenny L, K inm o n th AL. M edically u n ex p lain e d physical sy m p to m s in
p rim a ry care: a co m p ariso n of self-rep o rt screening q u estio n n aires a n d clinical opinion. J
P sychosom Res 1997; 42(3):245-252.
5
B arsky AJ, Borus JF. S om atizatio n a n d m ed icalizatio n in th e era of m a n ag e d care. JAMA
6
V erhaak PF, M eijer SA, V isser AP, W olters G. P ersisten t p rese n tatio n of m edically
7
S m ith GR, Jr., M onson RA, Ray DC. P atien ts w ith m u ltip le u n ex p lain e d sy m p to m s. Their
1995; 274(24):1931-1934.
u n ex p lain e d sym p to m s in general practice. F am P ract 2006; 23(4):414-420.
characteristics, functional health , an d h ea lth care u tilizatio n . A rch In tern M ed 1986;
146(1):69-72.
8
W alker EA, U n u tze r J, K aton WJ. U n d ersta n d in g a n d carin g for th e d istre ssed p a tie n t w ith
m u ltip le m edically u n ex p lain e d sy m p to m s. J A m B oard Fam P ract 1998; 11 (5) :347-356.
9
Lin EH, K aton W , V on K orff M, B ush T, Lipscom b P, R usso J et al. F ru stra tin g patients:
physician a n d p a tie n t p erspectives am o n g d istre ssed h ig h u sers of m edical services. J G en
In tern M ed 1991; 6(3):241-246.
10 W alker EA, K aton WJ, K eegan D, G ard n er G, S u llivan M. P red icto rs of p h y sician fru stra tio n
in the care of p atien ts w ith rh eu m ato lo g ical com plaints. G en H o sp P sychiatry 1997;
19(5):315-323.
11 H a rtz AJ, N oyes R, Bentler SE, D am iano PC, W illard JC, M om any ET. U n ex p lain ed
sym p to m s in p rim a ry care: persp ectiv es of doctors a n d patien ts. G en H o sp P sy ch iatry 2000;
22(3):144-152.
12 olde H a rtm a n TC, H assink-F ran k e LJ, L ucassen PL, v a n S p aen d o n ck KP, v a n W eel C.
E xplanation a n d relations. H ow do g eneral p ractitio n ers deal w ith p atien ts w ith p ersisten t
m edically u n ex p lain e d sym ptom s: a focus g ro u p stu d y . BMC Fam P ract 2009; 10:68.
13 S alm on P, R ing A, D ow rick CF, H u m p h ris GM. W h at do g eneral p ractice p atien ts w a n t
w h e n they p rese n t m edically u n ex p lain e d sy m p to m s, an d w h y do th eir doctors feel
p ressu rized ? J P sychosom Res 2005; 59(4):255-260.
14 R ing A, D ow rick CF, H u m p h ris GM , D avies J, Salm on P. The so m atisin g effect of clinical
consultation: W h at p atien ts a n d doctors say an d do n o t say w h e n p atien ts p rese n t m edically
u n ex p lain e d physical sym ptom s. Soc Sci M ed 2005; 61 (7) :1505-1515.
84 I Chapter 4
15 Salm on P, P eters S, S tanley I. P atients' p ercep tio n s of m edical ex p lan atio n s for so m atisatio n
disorders: q u alitativ e analysis. BMJ 1999; 318(7180):372-376.
16 Jo hansson EE, H am b erg K, L in d g ren G, W estm an G. "I've b een crying m y w ay "--qualitative
analysis of a gro u p of fem ale patien ts' co n su ltatio n experiences. Fam P ract 1996; 13(6):498503.
17 R ing A, D ow rick C, H u m p h ris G, Salm on P. Do p atien ts w ith u n ex p lain e d physical
sy m p to m s p ressu rise g eneral practitio n ers for som atic treatm en t? A q u alitativ e stu d y . BMJ
2004; 328(7447):1057.
18 E pstein RM, S hields CG, M e ld ru m SC, Fiscella K, C arroll J, C arney PA et al. Physicians'
responses to patien ts' m edically u n ex p lain e d sy m p to m s. P sychosom M ed 2006; 68(2):269276.
19 D ow rick CF, Ring A, H u m p h ris G M , S alm on P. N o rm alisatio n of u n ex p lain e d sy m p to m s
by general practitioners: a fun ctio n al typology. Br J G en P ract 2004; 54(500):165-170.
20 Coia P, M orley S. M edical reassu ran ce a n d p atien ts' responses. J P sychosom Res 1998;
45(5):377-386.
21 P eters S, S tanley I, Rose M, S alm on P. P atien ts w ith m edically u n ex p lain e d sym ptom s:
sources of patien ts' a u th o rity a n d im p licatio n s for d em an d s o n m edical care. Soc Sci M ed
1998; 46(4-5):559-565.
22 D eale A, W essely S. P atients' p ercep tio n s of m edical care in chronic fatig u e sy n d ro m e. Soc
Sci M ed 2001; 52(12):1859-1864.
23 B ertram S, K u rlan d M, L ydick E, Locke GR, III, Y aw n BP. The p atien t's p ersp ectiv e of
irritable bow el syndrom e. J Fam P ract 2001; 50(6) :521-525.
24 olde H a rtm a n TC, L ucassen PLBJ, v a n de L isd o n k EH, Bor JHJ, v a n W eel C. C hronic
fun ctio n al som atic sym ptom s: a single sy n d ro m e? Br J G en P ract 2004;54(509):922-7.
25 v a n W eel C, S m ith H, Beasley JW. Fam ily practice research n etw o rk s. E xperiences fro m 3
countries. J F am P ract 2000; 49(10):938-943.
26 v a n W eel C, de G ra u w WJ. Fam ily practices reg istra tio n n etw o rk s c o n trib u ted to p rim ary
care research. J C lin E pidem iol 2006; 59(8):779-783.
27 de G ra u w WJ, v a n G erw en W H , v a n d e L isd o n k EH, v an d en H o o g en HJ, v a n d en Bosch WJ,
v a n W eel C. O utcom es of au d it-en h an c ed m o n ito rin g of p atien ts w ith ty p e 2 diabetes. J Fam
P ract 2002; 51(5):459-464.
28 H u y g en FJ. Fam ily M edicine. The m edical life h isto ry of fam ilies. N ijm egen: D ekker & V an
de V egt; 1978.
29 G rol R. To heal o r to harm . The p rev e n tio n of som atic fixation in G en eral Practice. London:
Royal C ollege of G eneral P ractitioners; 1981.
30 G laser BG, S trauss AL. The discovery of g ro u n d e d theory. C higago: A ldine; 1967.
31 S trauss A. Q ualitativ e analysis for social scientists. L ondon: C am b rid g e U n iv ersity Press;
1987.
O pinions of patients w ith persistent MUS, an interview study | 85
32 K uper A, Reeves S, L evinson W. A n in tro d u c tio n to re a d in g a n d a p p ra isin g q u alitativ e
research. BMJ 2008; 337:a288. doi: 10.1136/bmj.a288.:a288.
33 C hurchill LR, Schenck D. H ealin g skills for m edical practice. A n n In tern M ed 2008;
149(10):720-724.
34 Scott JG, C ohen D, cicco-Bloom B, M iller WL, Stange KC, C rabtree BF. U n d ersta n d in g
healin g relatio n sh ip s in p rim a ry care. A n n F am M ed 2008; 6(4) :315-322.
35 B ritten N. Q ualitativ e in terv iew s in m edical research. BMJ 1995; 311 (6999) :251-253.
36 B ritten N, Jones R, M u rp h y E, Stacy R. Q u alitativ e research m e th o d s in g eneral practice an d
p rim a ry care. Fam P ract 1995; 12(1):104-114.
37 K itzinger J. Q ualitativ e research. In tro d u c in g focus gro u p s. BMJ 1995; 311(7000):299-302.
38 M a lteru d K. The a rt an d science of clinical know ledge: ev idence b e y o n d m e asu res an d
num b ers. L ancet 2001; 358(9279):397-400.
39 S tew art M, B row n JB, W eston W W , M cW hinney IR, M cW illiam C, F reem an T. P atientcen tered m edicine. second ed itio n ed. O xford: Radcliffe m edical press; 2003.
40 K rasner MS, E pstein RM, Beckm an H, S u ch m an AL, C h ap m an B, M ooney CJ et al.
A ssociation of an educatio n al p ro g ra m in m in d fu l co m m u n icatio n w ith b u rn o u t, em pathy,
a n d a ttitu d e s am o n g p rim a ry care physicians. JAMA 2009; 302(12):1284-1293.
41 G rep m air L, M itterlehner F, Loew T, Bachler E, R other W, N ickel M. P ro m o tin g m in d fu ln ess
in p sy c h o th erap ists in tra in in g influences th e tre a tm e n t resu lts of th eir p atients: a
ran d o m ized , d ouble-blind, contro lled stu d y . P sy ch o th er P sychosom 2007; 76(6):332-338.
88 I Chapter 5
Abstract
Background.
P ersisten t p rese n tatio n of m edically u n ex p lain e d sy m p to m s (MUS) is
trou b leso m e for general p ractitio n ers (GPs) an d causes p ressu re o n th e d o cto r-p atien t
relationship. As a consequence, G Ps face th e p ro b lem of estab lish in g an o n going, preferably
effective relatio n sh ip w ith these patien ts. This s tu d y aim s at ex p lo rin g G Ps' p ercep tio n s ab o u t
explaining MUS to p atien ts an d ab o u t ho w relatio n sh ip s w ith th ese p atien ts evolve o ver tim e in
daily practice.
Methods.
A q u alitativ e ap p ro ach , in te rv iew in g a p u rp o siv e sam p le of tw en ty -tw o D utch
G Ps w ith in five focus groups. D ata w ere an aly zed acco rd in g to th e p rin cip les of co n stan t
co m p arativ e analysis.
Results.
G Ps recognise th e im po rtan ce of an ad e q u ate ex p lan atio n of th e diag n o sis of MUS
b u t often feel incapable of bein g able to ex p lain it clearly to th eir p atien ts. G Ps th erefo re indicate
th a t they try to reassu re p atien ts in non-specific w ay s, for ex am ple by telling p atien ts th a t th ere
is n o disease, by u sin g m etap h o rs a n d by n o rm alizin g th e sy m p to m s. W h en p atien ts keep
re tu rn in g w ith MUS, G Ps rep o rt th e im p o rtan ce of m ain ta in in g th e d o cto r-p atien t relationship.
G Ps describe th ree d ifferent m odels to do this; m u tu a l alliance ch aracterized by ritu al care (e.g.
reg u la r physical exam ination, reg u la r d octor visits) w ith a p p ro v a l of th e p a tie n t an d th e doctor,
am biv alen t alliance characterized by ritu a l care w ith o u t a p p ro v a l of th e d octor a n d non-alliance
characterized by cu ttin g off all reaso n s for en c o u n ter in w h ich sy m p to m s are n o t of som atic
origin.
Conclusion.
G Ps feel difficulties in ex p lain in g th e sy m p to m s. G Ps re p o rt th at, w h e n
p atien ts keep p rese n tin g w ith MUS, th ey focus o n m ain ta in in g th e d o cto r-p atien t relatio n sh ip
by u sin g ritu a l care. In th is care th ey m eticu lo u sly b alance b etw e en m ain ta in in g a g o o d doctorp atien t relatio n sh ip a n d th e p rev e n tio n of u n in te n d e d consequences of unnecessary
interventions.
H ow do GPs deal w ith patients w ith persistent MUS, a focus group study | 89
Background
In 25 to 50 p erc en t of th e contacts p atien ts p rese n t m edically u n ex p lain e d sy m p to m s (MUS) to
th e g eneral p rac titio n e r (GP).1'2A lth o u g h it is only a m in o rity (2.5 percent) of th ese contacts th a t
w ill resu lt in a chronic co n d itio n associated w ith rec u rren t co n su ltatio n s, extensive
investigations a n d referrals, th is m in o rity of chronic p atien ts rep rese n ts a serio u s p ro b lem in
p rim a ry care.3 P ersistent p rese n tatio n of MUS is tro u b leso m e for th e G P because m an y G Ps
experience difficulties in th e com m un icatio n a n d th e rela tio n w ith th ese p atien ts .4-11
T here is evidence th a t th e difficulties in co m m u n icatio n m ay resu lt fro m m isp ercep tio n s of
p atien ts' n ee d s an d w o rries by G Ps.12 G Ps feel p re ssu riz e d by p atien ts to ap p ly b iom edical
in te rv en tio n s b u t they do n o t have m u ch to offer in a strictly b iom edical w ay .13'14 A t th e sam e
tim e, m o st p atien ts w ith MUS do n o t ov ertly insist o n a d d itio n a l som atic in terv en tio n s. They
p rim a rily w a n t to be u n d e rsto o d a n d seek em otional su p p o rt, w h ich d o cto rs do n o t p ro v id e.15-18
M oreover, th e lack of a biom edical ex p lan atio n h in d e rs G Ps in ad e q u ately telling p atien ts w h at
is w ro n g .19As a consequence patien ts' n ee d s are u n m et, reassu ran ce w ill be h a m p e re d a n d relief
of sy m p to m s w ill be com plicated.20'21
Recent research has sh o w n th a t the cu rren t m a n ag e m en t of p atien ts w ith MUS sh o u ld consist of:
com m u n icatin g to the p atien ts th a t th e sy m p to m s are real, m ak in g p atien ts feel u n d ersto o d ,
en g ag em en t of th e G P to establish com m o n g ro u n d w ith th e p atien t, offering a d etailed
ex p lan atio n ab o u t the n a tu re of the com plaints, a n d if n ecessary sy m p to m atic relief.22-25
By definition, p atien ts w ith p ersisten t MUS w ill keep atte n d in g th e co n su ltin g h o u rs of their
G Ps w ith MUS. H ow ever, they w ill also face o th e r h ea lth care p roblem s, for ex am ple serious
som atic disease.26 G iven the im p o rtan ce of a good relatio n w ith th e p a tie n t in th e lig h t of
co n tin u ity of care, G Ps have to fin d strateg ies to specifically deal w ith th ese p atien ts.10 To o u r
kn o w led g e it is n o t k n o w n how G Ps do th is a n d how , acco rd in g to G Ps, th is relatio n sh ip evolves
over tim e.27 F u rtherm ore, w e n ee d to k n o w GPs' o p in io n s ab o u t ex p lain in g th e n a tu re of
un ex p lain e d sym p to m s to p atien ts w ith p ersisten t MUS d u rin g con su ltatio n s, in o rd er to
develop m ore effective in terv en tio n s for th ese p atients.
In this q u alita tiv e explo rato ry stu d y w e focus o n GPs' p ercep tio n s of giv in g ex p lan atio n s to
p atien ts w ith p ersisten t MUS a n d o n G Ps' p ercep tio n s a b o u t th e d o cto r-p atien t relatio n sh ip an d
how th e relatio n sh ip evolves over tim e.
90 I Chapter 5
Methods
W e co n d u cted five focus g ro u p s w ith 22 D u tch G Ps to s tu d y th eir v iew s o n MUS. Each focus
g ro u p consisted of 4 to 5 GPs. W e u sed a p u rp o siv e sa m p lin g strateg y to increase th e external
v alid ity of o u r resu lts w ith resp ect to th e v ariety of ex istin g v iew s am o n g GPs. F rom the
literature, w e co n sid ered th e follow in g characteristics as rele v an t for th is variety: age, gender,
w o rk in g experience, n u m b e r of listed p atien ts, 'academ ic w o rk in g career', geographical
location of practice (city v ersu s rural) a n d site of ed u catio n .28"31
Each focus gro u p w as hom o g en o u s for th e characteristics 'academ ic w o rk in g career' an d
'geographical location' (Table 1); p articip a n ts o th erw ise rep rese n ted a v arie ty of th e listed
characteristics (T able 2).
W e chose focus g ro u p s ra th e r th a n in d iv id u al in terv iew s to u se g ro u p in teractio n w h ich
stim u lates p articip a n ts to explore a n d clarify th eir v iew s in to m ore d ep th .32 D iscussions w ere
facilitated b y a skilled m o d erato r, an d lasted for ap p ro x im ately one an d a h alf hour.
F ollow ing th e g u idelines for co n d u ctin g focus g ro u p s, th e m o d e ra to r u sed a d iscu ssio n g u id e to
direct th e d iscussion a n d to fulfil th e research aim s (Table 3). The d iscu ssio n g u id e w as m ainly
b ased o n im p o rta n t topics h ig h lig h ted in th e lite ra tu re .
The discussions w ere tap e-reco rd ed w ith th e p articip an ts' co nsent a n d com pletely v erb atim
transcribed. D ata collection an d analysis p ro ce ed ed as an iterativ e process. Tw o researchers
(ToH, LH) a d d e d relev an t a n d n ew topics to th e d iscu ssio n g u id e after a p relim in ary analysis of
each session. In this w ay, id eas a n d th o u g h ts th a t em erg ed in p rim a ry stages of th e analysis w ere
b ro u g h t fo rw ard in su b se q u en t focus g ro u p s as th e s tu d y proceeded.
Finally, the first a u th o r verified th e tran sc rip tio n an d e n tered all d a ta in to A tlas.ti, a softw are
p ro g ra m u se d to s u p p o rt the analysis of q u alitativ e data.
Table 1. Focus group charcteristics
characteristic
Focus group 1
GPs w ith an academic working career in Radboud University Nijmegen Medical Center
Focus group 2
GPs without an academic working career working in a rural area
Focus group 3
GPs without an academic working career working in a rural area
Focus group 4
GPs w ith an academic working career in VUmc Am sterdam or AMC University Amsterdam
Focus group 5
GPs without an academic working career working in a city
H ow do GPs deal w ith patients w ith persistent MUS, a focus group study | 91
Table 2. Key characteristics of purposive sam ple of general practitioners
N um ber of general practitioners
Gender
Male
Female
14
8
Working hours
Full time*
Part time
Not practicing at the moment
10
11
1
Type of practice
Solo
Duo
Group
Variable
Not practicing at the moment
1
2
17
1
1
Urbanization
Rural
Suburban
Urban
Variable
Not practicing at hthe moment
3
6
11
1
1
Age in years (range)
47 (31-58)
Experience as a GP in years (range)
15 (0-30)
* f u l l tim e : 80% to 100% fu l l tim e
Table 3. Focus group interview guidebook
What are the characteristics of patients with
persistent MUS?
- Regarding patient characteristics?
- Regarding sym ptom characteristics?
- Do you have problems to recognize these patients?
How do you call patients w ith persistent MUS?
- Which terms do you use to characterize these patients?
- Which terms do you tell to your patients?
W hat's the aetiology of persistent MUS?
- W hat is the nature of these symptoms?
- W hen do patients experience these symptoms?
- Why do these symptoms persist for such a long time?
Do you explain the diagnosis persistent MUS to
your patients?
- Do you think explanation is im portant in consultations with
these patients?
- How do you explain the diagnosis persistent MUS to the
patient?
- Which specific w ords do you use during explanation of the
symptoms?
How do you manage patients w ith persistent
MUS?
- How do you deliver health care to them?
- W hat do you do w ith requests for additional research?
- Which problems do you face in the management of these
patients?
- How do you manage diagnostic uncertainty?
- Do you feel capable to manage these patients?
How do you describe the doctor-patient
relationship w ith those patients?
- Is the doctor-patient relationship important, and why?
- Do you experience problems in the doctor-patient relationship?
How do you experience the MUS consultations?
- Which problems do you face during the MUS consultation?
92 I Chapter 5
Analysis
A nalysis follow ed th e principles of co n stan t co m p arativ e analysis in w h ich tran sc rip ts are
su b seq u en tly them atically coded.33 The m ain aim of th is analysis is to org an ize resp o n ses by
them e a n d explore sim ilarities an d differences in a n d b etw e en g ro u p s.
Tw o researchers (ToH, LH) rea d all in terv iew s several tim es to fam iliarize them selv es w ith the
data. They in d e p en d e n tly m ad e a first categ o rizatio n by co d in g m ean in g fu l sentences. Initial
codes w ere discussed, seeking ag reem en t o n th eir content. In th e ev en t of d isag reem en t, the
o p in io n of a th ird researcher (PL) w as sought. W e g ro u p ed th e codes in to th em es to id en tify key
featu res of G Ps' v iew s o n MUS. R ecurren t an d im p o rta n t th em es w ere freq u en tly d iscu ssed an d
refin ed as p a rt of an ongo in g iterativ e process.34 D u rin g th e en tire analysis w e con stan tly
m a tch ed th e d ev elo p in g th em es w ith th e tran sc rip ts a n d w ith available scientific literatu re on
th is subject. Therefore, these re p e a te d th em es are g ro u n d e d in th e d ata a n d n o t im p o sed o nto the
d a ta by th e researcher. W e also checked o u r d ev elo p in g th em es for inconsistencies w ith the
transcripts.
D ata collection co n tin u ed u n til s a tu ra tio n w as reach ed w ith no n ew m ajor th em es a risin g from
analysis of the fifth focus group.
The v alid ity of o u r fin d in g s w ere ex p lo red by checking o u r resu lts in a n in d e p e n d e n t g ro u p of
G Ps w h o h a d no specific in terest in MUS. They ju d g e d the resu lts to be co n sisten t w ith th eir
p ercep tio n s a n d experiences.35
Results
The G Ps in this s tu d y co n sid ered th e ex p lan atio n of th e n a tu re of th e sy m p to m s as w ell as
m ain ta in in g th e d o cto r-p atien t relatio n sh ip as a difficult b u t im p o rta n t task in h elp in g p atien ts
w ith p ersisten t MUS.
G Ps w ith an academ ic w o rk in g career d iscu ssed m ore a b o u t the classification a n d cu rren t
theories a b o u t p atien ts w ith p ersisten t MUS. G Ps w ith o u t an academ ic w o rk in g career h ad a
m ore clear focus o n th e difficulties th ey experience in d aily p ractice w o rk in g w ith th ese p a tie n ts .
W e co u ld n o t fin d fu rth e r m ajor differences b etw e en the p ersp ectiv es of academ ic a n d n o n ­
academ ic GPs. F u rtherm ore, w e co u ld n o t fin d differences in p ersp ectiv e b etw e en ru ra l an d
u rb a n w o rk in g GPs.
H ow do GPs deal w ith patients w ith persistent MUS, a focus group study | 93
GPs' perceptions of giving explanations
Im portance of explan atio n s a n d difficulties in ex p lain in g w ere rec u rren t th em es in th e focus
g ro u p discussions. The first focus gro u p d iscu ssio n (GPs w ith an academ ic w o rk in g career in
N ijm egen) rev ealed th a t difficulties in a g o o d ex p lan atio n w as an im p o rta n t topic in
con su ltatio n s w ith MUS patients. D u rin g th e focus g ro u p s w ith G Ps w ith o u t a n academ ic
w o rk in g career (focus gro u p 2, 3 an d 5) w e d iscu ssed in d e p th th e w ay s of ex p lain in g MUS to the
p atient. B oth G Ps w ith an academ ic w o rk in g career (focus g ro u p 4) as G Ps w ith o u t an academ ic
w o rk in g career stressed the im portan ce of a clear exp lan atio n . In focus g ro u p 5, no n ew them es
o n the im portance of ex p lan atio n cam e u p .
G Ps stressed the im po rtan ce of a clear e x p lan atio n of th e sy m p to m s. A n a d e q u ate ex p lan atio n
w as re g a rd e d as im p o rta n t in b o th rea ssu rin g p atien ts th a t th e re is no serio u s disease, a n d in
h elp in g p atien ts to accept th a t th e re is n o t alw ay s a m edical ex p lan atio n for physical sym ptom s.
"GP13 (male, 5 years GP working experience): B ut you need to explain damned well. GP12 (male, 29
years GP working experience): The doctor has the monopoly o f truth, so you need to be very clear about
the cause of the symptoms. D on't be vague because otherwise a patient will return home muddled
which make things worse" [FG 3]
G Ps sta te d th a t ad e q u ate fo rm u late d ex p lan atio n s m ay help p atien ts u n d e rsta n d th e connection
b etw e en th eir psychosocial life a n d th e sy m p to m s. A ccording to th e GPs, p atien ts' fam ily
m em bers a n d p atien ts' colleagues also w ish an ex p lan atio n of th e sy m p to m s too, especially
w h e n p atien ts have benefits of bein g ill.
A lth o u g h G Ps firm ly agreed o n th e im p o rtan ce of a clear ex p lan atio n of th e sy m p to m s they
experience difficulties in d o in g this. G Ps h av e difficulties in d icatin g fro m w h ich co n d itio n s the
sym p to m s originate. W e see th is fro m th e v ag u e an d av o id in g an sw ers of th e G Ps to the
q uestions of the m o d e ra to r a n d th e long silence after a q u estio n of th e m o d e ra to r on th is topic.
"GP4 (male, 26 years GP working experience): I explain to patients which symptoms are bothering
them and I leave the diagnosis in the middle. I accept the symptoms as such and ask about the
consequences o f the symptoms. GP3 (female, 8 years GP working experience): Yes, I avoid diagnostic
terms too and I confine m yself to the particular symptom and I explain that it could be anything.
Moderator: B ut which terms do you use? (moments o f silence) GP2 (male, 17 years GP working
experience): I discuss with them a different way o f coping w ith their symptoms which may relieve
them." [FG 1]
94 I Chapter 5
"GP5 (male, 7 years GP working experience): In these patients there is often no connection between
symptoms and problems in daily life. A t least I can't see one. GP7 (male, 25 years GP working
experience): I often tell them that we are not yet knowledgeable. Particularly about patients who really
have difficulties with their symptoms, yes, you have to respond differently. GP5: But, when you ask me
'where exactly do the symptoms comefrom, that chronicfatigue', then I d on't have an answer" [FG 2]
O u r analysis rev ealed three appro ach es, acco rd in g to GPs, to ex p lain th e u n ex p lain ed
sym ptom s. First, G Ps indicate th a t th ey tell patients there is no disease. H o w ev er, G Ps h ig h lig h ted
th e dilem m a of how to com m unicate th e fin d in g of a p a tie n t su fferin g fro m sy m p to m s w ith o u t
evidence of any physical anom aly. They describe th a t th ey try to rea ssu re p atien ts w ith
statem en ts th a t 'n o th in g is w ro n g '.
"GP9 (female, 19 years GP working experience): Yes, I always say: I d on't know it either. It is not your
heart, not your lungs, we did not fin d any abnormality. GP6 (female, 1 year GP working experience):
Yes, I recognize what [GP9] is saying: at least we can conclude that it's nothing serious. We have
examined a lot, but the question as to what you are actually suffering from is difficult to answer. GP5
(male, 7 years GP working experience): Yes, these symptoms are not caused by a disease" [FG 2]
S econdly, G Ps indicate th a t they use metaphors to give p atien ts som e in sig h t in th e h y p o th esized
interactions b etw e en sy m p to m s an d psychosocial life. G Ps re p o rte d th a t th ey use m e tap h o rs often a tangible physical m echanism in d icatin g som e k in d of im balance b etw e en lo ad an d
capacity - th a t reflect th eir tacit beliefs a n d id eas ab o u t th e n a tu re of MUS. A ccording to th e GPs,
som etim es th e m e tap h o r facilitates a d iscu ssio n of psychological or social problem s.
"GP5 (male, 7 years GP working experience): Every human being has a weak spot and i f there's
something wrong you feel it there. GP9 (female, 19 years GP working experience): I always tell them to
compare it with
a heavily overloaded elevator. GP7 (male, 25 years GP working experience): I
recognize your story, I always tell patients that everyone has a backpack and this backpack can be too
heavy. " [FG 2]
T hirdly, G Ps indicate th a t they normalize the symptoms of th e p atien ts, tellin g p atien ts th a t h av in g
sym p to m s is a p a rt of n o rm al life. G Ps rep o rted th a t th ey ex p lain to th e p a tie n t th a t the
sym p to m s are w ith in a com m on, acceptable range, th a t th ey are n o t d an g e ro u s an d th a t
d iagnostic p ro ced u res or tre a tm e n t are n o t n ec essary .
"GP10 (female, 1 year GP working experience): I normalize. I mean, I explain to patients that it is
normal, that it's not strange. I try to normalize as much as possible. GP12 (male, 29 years GP working
experience): Yes. GP10 : saying that it is part o f normal life. GP12: Yes" [FG 3]
H ow do GPs deal w ith patients w ith persistent MUS, a focus group study | 95
GPs' perceptions of the evolving doctor-patient relationship
In all focus g ro u p s G Ps d iscussed th e im p o rtan ce of th e d o cto r-p atien t relatio n sh ip . The
difficulties arisin g in the relatio n sh ip w as a rec u rren t them e. Focus g ro u p s w ith G Ps w ith o u t an
academ ic w o rk in g career (focus gro u p 2, 3 a n d 5) d iscu ssed th e w ay of d ealin g w ith th e doctorp a tie n t relatio n sh ip in p atien ts w ith p ersisten t MUS. F u rth erm o re, focus g ro u p 4 a n d 5 GPs
discu ssed th e difficulties th ey face in th e relatio n sh ip w ith th ese p a tie n ts.
G Ps in te n d to clarify the link (as su p p o se d by them ) b etw een som atic experiences and
psychosocial circum stances of th e patien t. In o th er w o rd s, th ey in d icate to try to change the
agenda. W hen talk in g ab o u t psychosocial circum stances is n o t successful, G Ps re p o rte d th a t they
su g g est an d discuss a ran g e of activities: d o in g som e sp o rts, g iving m o re fre q u en t co nsultations
for th e sym ptom s, u sin g a sy m p to m diary , ta k in g m ed icatio n or referrin g to a social w orker.
W h en ch an g in g th e ag e n d a d o esn 't w o rk o u t w ell, G Ps re p o rte d th a t th ey focus o n dealing with
the doctor-patient relationship. W ithin th is strateg y w e co uld d istin g u ish th ree d ifferen t doctorp a tie n t relatio n sh ip m odels.
A first d o cto r-p atien t relatio n sh ip m o d el can be ch aracterized as mutual alliance. This alliance is
realized by som e sort of ritu a l care. G Ps sta te d th a t th ey use ritu a ls w ith seem in g ly m u tu a l
ap p ro v a l a n d th a t these ritu a ls em erge g rad u a lly after m an y consultations.
"GP9 (female, 19 years GP working experience): A t a certain moment in your approach o f the patient,
when a patient has had all diagnostic procedures and many referrals, then comes the moment when one
realizes: this is the only way this patient can live. Consequently I let him consult me sporadically, even
without complaints [...] A n d when he feels such a ritual is sufficient, examining his heart, lungs and
blood pressure, reassurance is reached to keep him happy for some time. [...] GP7 (male, 25 years GP
working experience): Finally, you have created some kind o f relationship, some kind o f game in which
patients are quite satisfied w ith little. Someone listening [...] a pat on the back. " [FG2]
E xam ples of those ritu a ls are reg u la r phy sical ex am ination, referral to a p h y sio th erap ist,
prescribing m ed icatio n or p erfo rm in g a d d itio n a l in v estig atio n s, all w ith p rese rv in g a good
relatio n sh ip w ith th e p a tie n t a n d k eep in g in m in d th e u n in te n d e d consequences of unnecessary
interventions.
"GP16 (male, 23 years GP working experience): Sometimes I ju st wait and see, and take care not to
cause any damage in these patients" [FG4]
96 I Chapter 5
G Ps said th a t these ritu a ls are connected w ith req u ests or w ish es of th e p atien ts a n d th a t they
p rim arily aim a t reach in g agreem en t. G Ps re p o rte d th a t th ey p ro v id e th is k in d of care w ith
w a rm th an d em p ath y a n d th a t th ey assu m e th a t p atien ts are satisfied w ith it.
The second d o cto r-p atien t relatio n sh ip m o d el is ambivalent alliance. As sta te d by th e GPs, this
m odel is characterized b y th e sam e ritu a ls as in th e first m odel, b u t in fact th e G Ps do n o t agree
w ith the ritu a ls a n d are u n h a p p y w ith th e situation. T here is often a n eg ativ e co lo u rin g in GPs'
u tteran ces a b o u t this m ethod.
"GP14 (male, 15 years GP working experience): Nowadays I ask patients to undress and I practice all
sorts of complicated physical examinations I can think of, and when I have done all the physical
examinations; then I say: everything is all right, you are healthy and then they go home satisfied [...] A
patient visits me six times for a referral note, yes, when he or she comes for the third time, then I agree
with a referral, inevitable, otherwise you have an argument and in m y working experience that does
not work at all [...]"[FG4]
G Ps re p o rte d th a t th e am b iv alen t alliance indicates a d isag reem en t w ith su p p o se d req u ests for
m edical in te rv en tio n s as m edical necessity of th ese in te rv en tio n s is d o u b tfu l. They re p o rte d th at
in these situ atio n s th e p a tie n t is in contro l of th e situation.
The th ird relatio n sh ip m odel a p p e a rin g fro m th e discu ssio n s is non-alliance. G Ps rep o rted th at
th is m o d el rarely occurs in daily practice. T hey sta te d th a t th is m o d el is ch aracterized by cu ttin g
off all reaso n s for enco u n ter in w h ich sy m p to m s are n o t of som atic o rig in by ta k in g a cool,
objectifying m edical gaze.
"GP12 (male, 29 years GP working experience): sometimes it is easier to be very short, in a way o f 'you
have to fin d out for yourself1. Go to a social worker and do not bother me with that problem again. Just
be practical. Then it does not bother me at all. The patient is the one with the problem, it is not m y
problem, it is your problem, and you have to solve that w ith the social worker." [FG3]
In this non-alliance m odel, G Ps re p o rte d th a t in case of an absence of a som atic ex p lan atio n for
th e sym ptom s, they com m unicate th is n eg ativ e fin d in g directly to th e p a tie n t an d at th e sam e
tim e give th e m essage th a t th e p a tie n t sh o u ld n o t co n su lt w ith th ese k in d s of p ro b le m s.
A nalysis in a n d b etw e en th e focus g ro u p d iscu ssio n s rev ealed th a t each G P h as a p referre d w ay
of h a n d lin g th e relatio n sh ip problem . G Ps w h o stressed th e im p o rtan ce of th e relatio n sh ip
preferre d the m u tu a l alliance m odel, w h ereas G Ps w h o stressed th e im p o rtan ce of ch an g in g the
ag e n d a seem ed to rely o n th e am biv alen t alliance m odel. N on-alliance w as n o t freq u en tly
m entioned. O ne G P sta te d th a t he cop ed w ith p atien ts w ith p ersisten t MUS in su c h a w ay d u rin g
his G P residency. O ne G P to ld th a t he u se d th is n on-alliance m o d el to cope w ith th ese p atien ts
d u rin g out-of-our-services.
H ow do GPs deal w ith patients w ith persistent MUS, a focus group study | 97
Discussion
G Ps are aw a re of th e im p o rtan ce of ex p lain in g th e diag n o sis of MUS ad eq u ately to p atien ts w ith
p ersisten t u n ex p lain e d sym ptom s. H o w ev er, th ey face difficulties in ex p lain in g th e n a tu re of
th e sy m p to m s d u rin g th e en c o u n ter w ith these patien ts. G Ps state th a t th ey use th ree different
ap p ro ach es to ex p lain the sym p to m s to th e p atien ts; n o rm aliza tio n of sy m p to m s, telling
p atien ts th a t th e re is no disease, a n d u sin g m etap h o rs. A ccording to th e literature,
n o rm aliza tio n of sy m p to m s a n d tellin g p atien ts th a t th ey d o n 't h av e a disease is n o t effective
an d m ay ev en resu lt in m ore health-care seeking.19,36This m ig h t co n trib u te to th e fact th a t a sm all
b u t relev an t p ro p o rtio n of MUS p atien ts becom e p ersisten tly im p a ired an d k eep a tten d in g the
G P.37 M etaphors, o n th e other h an d , can be u sefu l in reach in g sh a re d u n d e rsta n d in g b etw een
p a tie n t a n d doctor because th ey are tan g ib le a n d n o n -b lam in g , alth o u g h th e re is lim ited
evidence for th eir effectiveness.36,38 Seem ingly, th ere is a p ara d o x in a rg u in g th a t physicians
sh o u ld p ro v id e explan atio n s for a p ro b lem th a t th ey them selv es describe as un ex p lain ed .
H ow ever, m o st com plaints p rese n ted in p rim a ry care rem a in at th e level of a sy m p to m
diagnosis a n d n ev e r re su lt in the diag n o sis of a disease.39 The co n n o tatio n 'u n ex p lain ed ' in
m edically u n ex p lain e d sy m p to m s in d icates th a t th e sy m p to m s are n o t explainable fro m the
red u c tio n ist disease fram ew o rk .40H ow ev er, these sy m p to m s are fre q u en tly explainable in other
term s given b y m odels as th e som ato sen so ry a m p lificatio n m o d el or th e co g n itiv e-p ercep tu al
m odel.41 A p p aren tly , G Ps lack the com petence to u se th ese available m o d els ad e q u ately in
p atien ts p rese n tin g w ith p ersisten t MUS. H o w ev er, search in g for a sy m p to m ex p lan atio n
to g eth er w ith the p a tie n t is an im p o rta n t task of G Ps in d aily practice as it gives th em the
o p p o rtu n ity to establish com m on g ro u n d on w h ich th ey can jo in tly u n d e rsta n d an d m an ag e the
p atien ts' n ee d s.42
G Ps realize the u sefulness a n d im p o rtan ce of a good relatio n in en co u n ters w ith th ese patien ts,
a lth o u g h they face difficulties in p u ttin g th is into p ractice w h e n ex p lain in g an d rem o v al of
sym p to m s is n o t feasible. W h en p atien ts keep p rese n tin g MUS, G Ps re p o rt th a t th e doctorp a tie n t relatio n sh ip evolves into th ree d ifferen t m o d els ch aracterized by th e presen ce or
absence of m u tu a l u n d e rsta n d in g a n d a careful b alance b etw e en m a in ta in in g th e d o cto r-p atien t
relatio n sh ip a n d p re v e n tin g u n in te n d e d consequences of th e interventions.
A lth o u g h G Ps recognize th e lim itatio n s an d difficulties of estab lish in g an on g o in g an d
p referably effective relatio n sh ip w ith th ese p ersisten t MUS p atien ts in daily practice, th ey
seem s to take responsibility to b u ild a n d m a in ta in su ch a relatio n sh ip . T aking th is responsibility
fits into the p h ilo so p h y of p rim a ry care in w h ich a lo n g -term a n d co n tin u o u s relatio n sh ip in
g eneral practice is em p h asized .20,43These relatio n sh ip s evolve o ver tim e an d are b u ilt o n reg u lar
con su ltatio n s as w ell as other sh a re d ex periences.20,26It is k n o w n fro m th e literatu re th a t b u ild in g
98 I Chapter 5
o n a n d establishing an effective a n d satisfactory d o cto r-p atien t relatio n sh ip has a n appreciable
im pact o n h ea lth outcom es for patien ts.44
G Ps sta te d th a t d ifferent relatio n sh ip m o d els w ith p atien ts w ith p ersisten t MUS dev elo p over
tim e: m u tu a l alliance, am biv alen t alliance an d non-alliance. These relatio n sh ip m o d els are, as
far as w e know , n o t d escribed elsew here. The mutual alliance m odel, a n d to a lesser deg ree the
ambivalent alliance m odel, can be co n cep tu alized as co m p risin g a po sitiv e relatio n sh ip an d
collaboration w ith m u tu a l a p p ro v a l b etw een p a tie n t an d doctor.45The goal of th is co llaboration
is to m a in ta in the d o cto r-p atien t relatio n sh ip by p ro v id in g em o tio n al s u p p o rt th ro u g h som e
k in d of ritu a l care. In this strateg y G Ps keep in balance th e d o cto r-p atien t relatio n sh ip a n d the
u n in te n d e d consequences of in terv en tio n s. R eaching m u tu a l alliance co rresp o n d s w ith
fin d in g s th a t p atien ts w ith MUS seek a h ig h level of em otional s u p p o rt rath er th a n som atic
in terv en tio n s.17'46
C h ew -G raham p o in te d o u t th a t G Ps w h o experience difficulties in th e relatio n sh ip s w ith som e
g ro u p s of p atien ts felt th a t con cen tratin g o n m ain ta in in g the d o cto r-p atien t relatio n sh ip m ake
th e m to collude w ith p atien ts a n d th eir sy m p to m s.47 It is possible th a t G Ps in th e 'ambivalent
alliance ' m o d el are h in d e re d by this collusion a n d feel u n h a p p y w ith th e ritu a l care.
O ne could arg u e th a t th e p rese n ted m odels for th e d o cto r-p atien t relatio n sh ip are doctorcentred. This m ay be th e resu lt of th e aim of o u r s tu d y to exam ine GPs' percep tio n s. W e ask ed the
G Ps in th e focus g ro u p s how they m an ag e p atien ts w ith p ersisten t MUS. In o th er w o rd s, w e
asked for their o w n G P perspective. In resp o n se th ey describ ed ho w th ey stru g g le to p reserve
their relatio n w ith the patient. In this resp ect the G Ps are w o rk in g p atien t-cen tred . M oreover,
the m u tu a l alliance strateg y as w ell as the am b iv alen t alliance strateg y in co rp o rate certain
elem ents of p atien t-cen tred n ess such as fin d in g com m on g ro u n d reg a rd in g m a n ag em en t an d
enh an cin g the d o cto r-p atien t relatio n sh ip .48 H o w ev er, a m ore p atien t-c en tred ap p ro a ch in
w h ich a n exp lo ratio n of the patien ts' n ee d s a n d ex pectations in o rd er to s u p p o rt p atien ts' self
m a n ag em en t a n d coping w ith the sym p to m s, d id n o t com e u p in the focus g roups. G Ps d id n o t
in tro d u c e several other aspects of p atien t-c en tred n e ss su ch as disclosing p atien ts' concerns an d
suffering, a n d focussing o n patien ts' self m a n ag em en t a n d coping.49W e assu m e th a t th is can be
ex plained by th e fact th a t d u rin g o u r focus g ro u p in terv iew s w e focussed o n situ atio n s in daily
practice in w h ich G Ps felt th a t they get stu c k w ith th ese p atien t. Possibly, strateg ies as disclosing
concerns, relief of suffering, a n d focu ssin g o n self m a n ag em en t a n d co p in g h a d failed in an
earlier stage of th e d o cto r-p atien t contact.
H ow do GPs deal w ith patients w ith persistent MUS, a focus group study | 99
Strengths and limitations of this study
The q u alitativ e m e th o d is a p p ro p ria te to explore a n d clarify w h a t G Ps th in k a b o u t th ese p atien ts
an d w h a t they experience in th e consu ltatio n s w ith th ese p atien ts.32H o w ev er th is m eth o d does
n o t p ro v id e in sig h t in th e G Ps actual b eh av io u r. By u sin g a cyclical a n d in teractiv e w ay of
collecting a n d an aly zin g data, 'prog ressiv e focusing' an d ex p lo ratio n of GPs' p ercep tio n s in
d e p th w ere realized .50 In focus g ro u p discu ssio n s th e p articip a n ts influence each o th er by
listening a n d discussing. Such g ro u p dyn am ics m ay silence in d iv id u a l co n trastin g o p in io n s an d
resu lt in the articu latio n of gro u p n o rm s or early consensus before all view s w ere fully
expressed.32H ow ever, the goal is n o t to reach consensus. In stead , o u r goal w as to stu d y h o w G Ps
as p rofessionals th in k ab o u t p atien ts w ith p ersisten t MUS. It w o u ld n ev erth eless b e in terestin g
to analyze how in d iv id u a l p articip a n ts in flu en ced each o th e r d u rin g th e discussion, b u t this w as
n o t the aim of o u r stu d y . To reach an o p tim al v ariety of o pinions, w e u sed a p u rp o siv e sam p lin g
strategy. A lth o u g h sm all, th e n u m b e r of p articip a n ts is co n sid ered a d e q u ate for th is p u rp o se.32
By u sin g a p u rp o siv e sa m p lin g strateg y w e h av e ca p tu red th e v ariety of o p in io n s p rese n t in the
p o p u la tio n of G P s.
A s MUS are n o t equally d istrib u ted am o n g m en an d w o m en a n d m en a n d w o m en h av e different
expectations a n d experiences of clinical en co u n ters,6 a g en d er p ersp ectiv e m ay enhance
u n d ersta n d in g . H ow ever, w e d id n o t stu d y th e differences in th in k in g a b o u t p atien ts w ith
persisten t MUS b etw e en fem ale v ersu s m ale G Ps, as in this s tu d y w e focussed o n eliciting GPs'
p ercep tio n s of giving ex planations a n d th eir p ercep tio n s ab o u t th e d o cto r-p atien t relationship.
A lth o u g h w e kn o w fro m recent research th a t th ere are cu ltu ral differences in th e d istrib u tio n of
MUS a n d th e m e an in g a n d significance of a sy m p to m d ep e n d s o n th e p erceiv ed relatio n sh ip
w ith diseases in a cu ltu re,51-53G Ps d id n o t sp o n tan eo u sly in tro d u c e th eir o p in io n s o n cu ltu ral
aspects of p ersisten t MUS d u rin g the focus g ro u p discussions.
This q u alitativ e s tu d y exam ines G Ps' p ercep tio n s a n d n o t actu al b eh av io u r. W e deliberately
chose to stu d y th e percep tio n s because actual b eh a v io u r m ay re su lt fro m p ercep tio n s to a certain
degree. M oreover, this stu d y is p a rt of a larg er project in w h ich w e exam ine actu al b eh av io u r
an d com m unication strategies of G Ps in a v id eo reg istratio n s tu d y an d th e p a tie n t p ersp ectiv e in
a q u alitativ e interview study.
W e describe o u r resu lts by u sin g th e p h rase 'relatio n sh ip m odels'. A lth o u g h w e are aw a re of the
overlap w ith com m unication strategies, w e th in k th a t 'relatio n sh ip m odels' is a m ore
a p p ro p ria te te rm in th e context of o u r fin d in g s as it reflects th e o p in io n s of th e G Ps th a t
m ain ta in in g th e relatio n sh ip w ith tho se p atien ts is of m ajor im portance. G Ps in d icate th a t th ey
m a in ta in th e relatio n sh ip n o t only by th e w ay th ey com m u n icate b u t also b y th e w ay th ey take
care for these patients.
100 I Chapter 5
T ape-recording th e discussion, m u ltip le co d in g d u rin g analysis a n d o u r tria n g u latio n strateg y
of ask in g in d e p e n d e n t G Ps to ju d g e o u r resu lts to be consistent w ith th eir o w n p ercep tio n s an d
experience, a d d e d to th e rigor of the study.
F u rth e r stu d ies u sin g a m ixed m e th o d m eth o d o lo g y m ay reveal effective m e th o d s of explaining
sym p to m s to p atien ts w ith MUS. M oreover, it w o u ld be u sefu l to s tu d y th e effects of th e three
relatio n sh ip m odels re p o rte d by th e G Ps o n outcom es an d satisfaction in patien ts. In research, as
w ell as e d u c atio n w e sh o u ld face th e challenge of ex p lain in g th e u n ex p lain ed sy m p to m s an d
b u ild in g a tru ly effective d o cto r-p atien t relatio n sh ip w ith th ese fascin atin g p atien ts. W ith the
resu lts of fu rth e r research w e w o u ld like to a d d re ss th e challenge of ex p lain in g u n ex p lain ed
sy m p to m s ad e q u ately an d b u ild in g effective d o cto r-p atien t relatio n sh ip s w ith th ese p atients,
preferab ly by ed u c atin g doctors w ith tools ho w to do so.
Conclusion
G Ps are aw are of th e im p o rtan ce of ex p lain in g MUS ad eq u ately to th eir p atien ts, h o w ev er they
h av e difficulties in d o in g so. G Ps re p o rt th at, w h e n p atien ts keep p rese n tin g w ith MUS, they
focus o n m ain ta in in g th e d o cto r-p atien t relatio n sh ip by u sin g ritu a l care. These relatio n sh ip s
evolves into th ree d ifferent m odels ch aracterized by th e presen ce or absence of m u tu a l
u n d e rsta n d in g a n d a careful balance b etw e en m ain ta in in g th e d o cto r-p atien t relatio n sh ip and
p re v e n tin g u n in te n d e d consequences of th e in te rv e n tio n s.
Acknowledgements
W e th a n k the G Ps w h o atte n d e d the focus g ro u p discussions so th a t w e co uld realize this
research project. W e also th a n k Prof. F. W ester for his s u p p o rt o n th e q u alitativ e research
m eth o d o lo g y a n d J. Reeve a n d S. Schellekens for rev iew in g th e E nglish lan g u ag e of the
m anuscript.
How do GPs deal w ith patients w ith persistent MUS, a focus group study | 101
Reference List
1
Bass C e: S om atisation: Physical S ym ptom s a n d Psychological d iso rd er. O xford:
Blackwell; 1990.
2
B arsky AJ, Borus JF: S om atizatio n a n d m ed icalizatio n in th e era of m a n ag e d care. JAMA
1995, 274:1931-1934.
3
V erhaak PF, M eijer SA, V isser AP, W olters G: P ersisten t p rese n tatio n of m edically
u n ex p lain e d sym p to m s in general practice. Fam P ract 2006, 23:414-420.
4
A sbring P, N a rv a n e n AL: Ideal v ersu s reality: p h y sician s p ersp ectiv es on p atien ts w ith
5
W alker EA, U n u tze r J, K aton WJ: U n d e rsta n d in g an d carin g for th e d istre ssed p atien t
chronic fatig u e sy n d ro m e (CFS) an d fibrom yalgia. Soc Sci M ed 2003, 57:711-720.
w ith m u ltip le m edically u n ex p lain e d sy m p to m s. J A m B oard F am P ract 1998, 11:347-356.
6
M a lteru d K: S ym ptom s as a source of m edical know ledge: u n d e rsta n d in g m edically
u n ex p lain e d d iso rd ers in w om en. F am M ed 2000, 32:603-611.
7
Lin EH, K aton W , V on K orff M, B ush T, Lipscom b P, R usso J, W ag n er E: F ru stra tin g
patients: physician an d p a tie n t p ersp ectiv es am o n g d istre ssed h ig h u sers of m edical
services. J G en In tern M ed 1991, 6:241-246.
8
W alker EA, K aton WJ, K eegan D, G a rd n e r G, S u llivan M: P red icto rs of p h y sician
fru stra tio n in th e care of p atien ts w ith rh eu m ato lo g ical com plaints. G en H osp
P sychiatry 1997, 19:315-323.
9
L u n d h C, S egesten K, B jorkelund C: To be a h elpless helpoholic--G Ps' experiences of
w o m en p atien ts w ith non-specific m u scu lar pain. Scand J P rim H ea lth C are 2004, 22:244­
247.
10 S m ith S: D ealing w ith th e difficult p atien t. P o stg rad M ed J 1995, 71:653-657.
11 H a h n SR, T ho m p so n KS, W ills TA, S tern V, B u d n er NS: The difficult d o cto r-p atien t
relationship: so m atization, p erso n ality a n d psy ch o p ath o lo g y . J C lin E pidem iol 1994,
47:647-657.
12 E pstein RM, S hields CG, M e ld ru m SC, Fiscella K, C arroll J, C arney PA, D u b erstein PR:
Physicians' responses to patien ts' m edically u n ex p lain e d sy m p to m s. P sychosom M ed
2006, 68:269-276.
13 G o ld b erg DP, B ridges K: Som atic p rese n tatio n s of p sychiatric illness in p rim a ry care
setting. J P sychosom Res 1988, 32:137-144.
14 R eid S, W hooley D, C rayford T, H o to p f M: M edically u n ex p lain e d sym ptom s--G P s'
attitu d e s to w ard s their cause a n d m an ag em en t. Fam P ract 2001, 18:519-523.
15 Ring A, D ow rick C, H u m p h ris G, Salm on P: Do p atien ts w ith u n ex p lain e d physical
sy m p to m s p ressu rise general p ractitio n ers for som atic treatm en t? A q u alita tiv e study.
BMJ 2004, 328:1057.
102 I Chapter 5
16 S alm on P, D ow rick CF, R ing A, H u m p h ris GM: V oiced b u t u n h e a rd agendas: q u alitativ e
analysis of the psychosocial cues th a t p atien ts w ith u n ex p lain e d sy m p to m s p rese n t to
general p ractitioners. Br J G en P ract 2004, 54:171-176.
17 S alm on P, Ring A, D ow rick CF, H u m p h ris GM: W h at do g eneral p ractice p atien ts w a n t
w h e n they p rese n t m edically u n ex p lain e d sy m p to m s, a n d w h y do th eir d o cto rs feel
p ressu rized ? J P sychosom Res 2005, 59:255-260.
18 D ow nes-G rainger E, M orriss R, G ask L, F arag h er B: Clinical factors asso ciated w ith
sh o rt-term changes in outcom e of p atien ts w ith so m atized m en tal d iso rd er in p rim a ry
care. P sychol M ed 1998, 28:703-711.
19 S alm on P, P eters S, S tanley I: P atients' p ercep tio n s of m edical ex p lan atio n s for
so m atisatio n disorders: qu alitativ e analysis. BMJ 1999, 318:372-376.
20 S tew art M: Reflections o n the d o cto r-p atien t relationship: fro m ev idence a n d experience.
Br J G en P ract 2005, 55:793-801.
21 D ow rick C: R ethinking the d o cto r-p atien t relatio n sh ip in g eneral practice. H ea lth &
Social Care in th e C o m m unity 1997, 5:11-14.
22 M ayou R, F arm er A: ABC of psychological m edicine: F unctional som atic sy m p to m s an d
syndrom es. BMJ 2002, 325:265-268.
23 R osendal M, O lesen F, F ink P: M an ag em en t of m edically u n ex p lain e d sy m p to m s. BMJ
2005, 330:4-5.
24 B lankenstein A H , v a n d er H o rst HE, Schilte AF, de V ries D, Z aat JO, A n d re KJ, v a n Eijk
JT, de HM : D evelopm ent an d feasibility of a m o d ified re a ttrib u tio n m o d el for
som atising patien ts, a p p lied by th eir o w n g eneral practitioners. P atien t E duc C ouns
2002, 47:229-235.
25 H en n in g sen P, Z ipfel S, H erzo g W: M an ag em en t of fu n ctio n al som atic syndrom es.
L ancet 2007, 369:946-955.
26 M cW hinney IR: A textbook of Fam ily M edicine. N ew York; O xford: O xford U niversity
Press; 1989.
27 M ainous AG, III, G o o d w in M A, Stange KC: P atien t-p h y sician sh a re d experiences a n d
v alu e p atien ts place o n co n tin u ity of care. A n n F am M ed 2004, 2:452-454.
28 G e rra rd TJ, R iddell JD: D ifficult p atients: black holes an d secrets. BMJ 1988, %2027;297:530-532.
29 G rol R: To heal or to harm . The p rev e n tio n of som atic fixation in G eneral Practice. 1981.
30 L am berts H.: In h et huis v an de h u isarts: v ersla g v a n h et T ransitieproject. L elystad:
M editekst; 1991.
31 M athers N , Jones N , H an n a y D: H ea rtsin k p atients: a stu d y of th eir general
p ractitioners. Br J G en P ract 1995, 45:293-296.
32 K itzinger J: Q ualitativ e research. In tro d u c in g focus gro u p s. BMJ 1995, 311:299-302.
33 G laser BG, S trauss AL: The discovery of g ro u n d e d theory. C higago: A ldine; 1967.
How do GPs deal w ith patients w ith persistent MUS, a focus group study | 103
34 B ritten N: Q ualitativ e interv iew s in m edical research. BMJ 1995, 311:251-253.
35 M ays N, P ope C: R igour a n d q u alitativ e research. BMJ 1995, 311:109-112.
36 D ow rick CF, Ring A, H u m p h ris GM , Salm on P: N o rm alisatio n of u n ex p lain ed
sy m p to m s by general practitioners: a fu n ctio n al typology. Br J G en P ract 2004, 54:165­
170.
37 olde H a rtm a n TC, B orghuis MS, L ucassen PL, v a n d e L aar FA, Speckens AE, v a n W eel
C: M edically u n ex p lain e d sym pto m s, so m a tisa tio n d iso rd er a n d hypoch o n d riasis:
course a n d prognosis. A system atic review . J P sychosom Res 2009, 66:363-377.
38 M abeck CE, O lesen F: M etaphorically tran sm itte d diseases. H o w do p atien ts em b o d y
m edical explanations? F am P ract 1997, 14:271-278.
39 O kkes IM, O skam SK, v a n Boven K, L am berts H.: M ost sy m p to m s - som atic or
psychological - p rese n ted to th e p rim a ry care p hysician, are no sig n of an d do n o t evolve
into organic diseases or m ental d iso rd ers. In E pisodes of care in Fam ily Practice.
E pidem iological d ata b ased o n th e ro u tin e use of th e In tern atio n al C lassification of
P rim ary Care (ICPC) in th e T ran sitio n Project of th e A cadem ic M edical
C e n te r/U n iv e rsity of A m ste rd a m (1985-2003). A m sterdam : U n iv ersity of A m sterdam ;
2005.
40 S tu rm b erg JP: The fo u n d atio n s of p rim a ry care. D arin g to be different. O xford - Seattle:
Radcliffe P ublish in g Ltd; 2007.
41 Rief W , B roadbent E: E xplaining m edically u n ex p lain e d sy m p to m s-m o d els a n d
m echanism s. C lin Psychol Rev 2007, 27:821-841.
42 S alm on P: Conflict, collusion or co llaboration in co n su ltatio n s a b o u t m edically
u n ex p lain e d sym ptom s: th e n ee d for a cu rricu lu m of m edical ex planation. P atien t Educ
C ouns 2007, 67:246-254.
43 B alint M: The doctor, his p a tie n t a n d th e illness. E d inburgh: C hurchill L ivingstone; 2000.
44 S tew art M A, M cW hinney IR, Buck CW: The d o c to r/p a tie n t relatio n sh ip a n d its effect
u p o n outcom e. J R Coll G en P ract 1979, 29:77-81.
45 C ape J: P atie n t-ra te d th erap eu tic relatio n sh ip a n d o u tco m e in general p ractitio n er
tre a tm e n t of psychological problem s. Br J C lin P sychol 2000, 39 ( P t 4):383-395.
46 P eters S, S tanley I, Rose M, Salm on P: P atien ts w ith m edically u n ex p lain e d sym ptom s:
sources of p atien ts' a u th o rity a n d im p licatio n s for d em an d s o n m edical care. Soc Sci
M ed 1998, 46:559-565.
47 C h ew -G raham CA, M ay CR, R oland MO: The h arm fu l consequences of elev atin g the
d o cto r-p atien t relatio n sh ip to be a p rim a ry goal of th e g eneral p ractice consultation. Fam
P ract 2004, 21:229-231.
48 Little P, E veritt H , W illiam son I, W arn er G, M oore M, G o u ld C, F errier K, P ayne S:
P references of patien ts for p a tie n t cen tred ap p ro a ch to co n su ltatio n in p rim a ry care:
o bservational stu d y . BMJ 2001, 322:468-472.
104 I Chapter 5
49 L evenstein JH, M cC racken EC, M cW hinney IR, S tew art M A, B row n JB: The p a tie n t­
cen tred clinical m ethod. 1. A m o d el for th e d o cto r-p atien t in teractio n in fam ily
m edicine. Fam P ract 1986, 3:24-30.
50 B ritten N , Jones R, M u rp h y E, Stacy R: Q u alitativ e research m e th o d s in general practice
a n d p rim a ry care. Fam P ract 1995, 12:104-114.
51 E scobar JI, G ureje O: Influence of cu ltu ral a n d social facto rs o n th e ep id em io lo g y of
idio p ath ic som atic com plaints an d sy n d ro m es. P sychosom M ed 2007, 69:841-845.
52 K arasz A, D em psey K, Fallek R: C u ltu ral differences in th e experience of ev ery d ay
sym ptom s: a co m parative stu d y of S o u th A sian an d E u ro p ean A m erican w om en. C ult
M ed P sychiatry 2007, 31:473-497.
53 olde H a rtm a n TC, H assink-F rank e L, D ow rick C, Fortes S, L am C, v a n d er H o rst H,
L ucassen P, v a n W eel-B aum garten E: M edically u n ex p lain e d sy m p to m s in fam ily
m edicine: d efining a research ag en d a. P ro ceed in g s fro m W O N C A 2007. F am P ract 2008,
25:266-271.
How do GPs deal w ith patients w ith persistent MUS, a focus group study | 105
108 I Chapter 6
Abstract
Introduction.
D u rin g co nsultatio n s, th e p ersp ectiv e of th e p a tie n t an d th e fam ily p h y sician
com e together. In o rd er to reach a sh a re d v iew ab o u t th e sy m p to m s it is im p o rta n t to k now the
ag e n d a of th e patient. C ues (i.e. non-explicit rem ark s th a t can enclose a special m eaning) can
serve as a tool to clarify th e agenda.
Case Report.
In th is article, w e describe a p a tie n t w ith u n ex p lain e d p alp ita tio n s d u rin g
v acuum ing. D u rin g one of the follow in g co n su ltatio n s she p ro v id e d an im p o rta n t psychosocial
cue w h ich ch an g ed m y p erspective o n h er p alp ita tio n s, resu ltin g in a d ee p er u n d e rsta n d in g of
her sym ptom s.
Discussion.
R ecognition a n d ex p lo ratio n of cues is im p o rta n t for reach in g m u tu a l
u n d e rsta n d in g of doctors an d p atien ts ab o u t th e sym ptom s. M oreover, it enhan ces the
th e ra p eu tic relatio n sh ip a n d im p ro v es illness outcom es an d p a tie n t satisfaction.
Conclusion.
N o ticing cues in the m edical co n su ltatio n h elp s to u n d e rsta n d th e p atien t's real
w orries. It gives us, as doctors, a b etter u n d e rsta n d in g of th e p atien t's perspective.
Case report | 109
Introduction
A n im p o rta n t ta sk for fam ily physician (FPs) is listen in g to p atien ts.1,2 The p atien t's sy m p to m s
are d iscussed b y th e p a tie n t a n d th e d octor to g eth er d u rin g co n su ltatio n . P atien ts h av e their
o w n ideas, w o rries a n d expectations ab o u t th eir sy m p to m s a n d so has th e FP, p artly becau se of
w h a t he w as ta u g h t in m edical edu catio n , b u t m ain ly becau se of his experience.3,4 D u rin g
co n su ltatio n th e p erspectives of th e p a tie n t a n d th e FP com e together.
O ne of the m o st im p o rta n t tasks of the FP is to com e to a m u tu a l u n d e rs ta n d in g w ith th e patient:
a sh a re d view a b o u t th e sy m p to m s.5 To reach th is ag reem en t, th e d octor n eed s to k n o w the
ag e n d a of th e patient. This can be ach iev ed by ex p lo rin g th e p atien t's expectations, cognitions
a n d em otions.5-7 T h ro u g h this w o rk in g style, th e d o ctor enhan ces th e p atien t's satisfaction,
ad h eren ce a n d h ealth .8,9
In daily practice it ap p e ars to be difficult to get to k n o w th e ag e n d a of th e p atien t.10 In
ap p ro x im ately half of all consultation s th e doctor does n o t reveal th e reaso n for en co u n ter an d
th e w o rries of th e p atien t.9 In a b o u t 20% of all co n su ltatio n s th e p a tie n t has a n u n v o iced
biom edical or psychosocial a g e n d a.11
D u rin g a co n su ltatio n p atien ts often give cues. C ues are n o n-explicit rem ark s th a t can enclose a
special m eaning. They can p o in t to w a rd s ideas, w o rries or ex pectations th e p a tie n t h as n o t
sh a re d before.3 N o ticing an d explo rin g th e p atien t's 'cues' is help fu l, it can serv e as a 'tool' to
clarify th e a g e n d a of th e p atien t.3,5H ow ev er, d octors ap p e ars to h av e g reat difficulty in detectin g
an d resp o n d in g to m ore in d ire ct form s of co m m u n icatio n su ch as cues.12 The fo llo w in g case
ch an g ed m y (ToH) com m unication skills a n d illu strates th e im p o rtan ce of n o ticin g an d
explo rin g a cue.
Case
The first consultation
A 79 y ear old w o m a n visits m e (ToH) w ith sy m p to m s of fatig u e an d p a lp ita tio n s. The sym p to m s
sta rte d w h ile v acu u m in g ; she freq u en tly h a d to sto p d o in g it ju st to recover for a w hile. She is
very active, b u t th e y ea rs seem to sta rt counting. She asks m e w h y she su d d e n ly develo p ed
palpitations. She is w o rrie d because she n ever h a d th e m before. F u rth er h isto ry ta k in g does n o t
give any indicatio n for an u n d e rly in g cause of th e p alp itatio n s. Because she has p alp itatio n s
d u rin g exertion, I w a n t to exclude a cardiac problem . W ith th e p atien t's ap p ro v a l I decide to
m ake an electrocardiogram a n d test her b lo o d to exclude cardiac an d oth er causes for the
palpitations.
110 I Chapter 6
The f ollow ing consultations
The electrocardiogram is no rm al, th e b lo o d test reveals a h y p o th y ro id ism . This co uld explain
her fatigue, b u t n o t her p alpitations. I rea ssu re her, a n d after d iscu ssin g th is w e d ecide to g eth er
th a t I w ill prescribe h er thyrax. W e settle a co u p le of ap p o in tm e n ts for follow u p consultations.
D u rin g these con su ltatio n s I ad ju st th e th y rax d osage a n d also h av e a ch at w ith her. G ra d u ally I
get to k n o w h er a little better. She tells m e m ore a b o u t h er h isto ry a n d b ack g ro u n d . I enjoy these
consultations. W ith the thyrax th e th y ro id fu n ctio n n o rm alises a n d th e fatig u e d isa p p ea rs
alm ost com pletely.
A special consultation
Six w eeks after th e first consultation, she com es for a fo llo w -u p v isit again. H er b lo o d h as been
te ste d an d h er th y ro id function is stable. She is h a p p y a n d satisfied w ith th is n ew s. T hen she
b rin g s u p h er p alp ita tio n s again. She w a n ts to k n o w w h eth e r it is possible th a t th ey are cau sed
b y h er th y ro id problem . I ask her if th ey h av e in creased since th e sta rt of th e th y rax , w h ich she
denies. I explain to h er th a t the p alp ita tio n s are p ro b ab ly u n re la te d to h er h y p o th y ro id ism an d
p ro b ab ly benign. She seem s to accept th is a n d says : 'W ell doctor, it is all ab o u t ho w life is lived'.
'W hat a rem ark ab le sentence' I think. I sh o w m y w o n d e r an d ask: 'W ell th en , h o w is life lived?'
A n d in fro n t of m e, th e re a n d th e n a sto ry u n fo ld s th a t h a d b een u n k n o w n to me. A t th e age of 16
she w e n t into a convent. Initially she h a d a good tim e th ere, b u t th is ch an g ed w h e n a n ew m o th er
su p e rio r w as a p p o in te d w ith w h o m she co u ld n o t get on. M o th er su p e rio r allo tted h er all the
n asty tasks an d she d e g ra d e d h er to b ein g a cleaner. For a lo n g tim e she d id n o t do a n y th in g b u t
scru b b in g floors. She w as te ase d a n d co ld -sh o u ld ered by h er fellow sisters. Y ears of b u lly in g
follow ed. A couple of tim es she trie d to b rin g u p th is subject, b u t th ey d id n o t seem to h ear her.
D u rin g th is p erio d she often h ad physical sy m p to m s, as a re su lt of w h ich she co u ld n o t p erfo rm
h er cleaning tasks. A fter living in the co n v en t for 15 y ea rs she h a d to leave - cast o u t fro m the
convent.
W ith asto n ish m e n t I listen to h er sto ry a n d she says: 'Gosh, doctor, I h av e n ev e r to ld th is to
any b o d y ' a n d 'm aybe th a t is w h y I get th ese p alp ita tio n s d u rin g v acu u m in g . I w ill th in k ab o u t it
at hom e'. W e ta lk som e m ore a n d she leaves m y co n su ltatio n ro o m noticeably relieved, w ith the
w o rd s 'thanks for listening d o c to r'.
Half a year later
D u rin g the follow -up v isit for h er th y ro id p ro b lem th e w o m an is cheerful. I realize th a t it has
been half a y ear since the d ay th a t she to ld m e th a t special story. I ask h er ab o u t h er p alp itatio n s.
She tells m e th a t she has h ad th e m a couple of tim es since th e last co n su ltatio n , b u t she is h ard ly
b o th e re d by th em anym ore. V acuum in g has becom e easier n o w a n d she feels b etter too. She says
ev ery th in g is fine n o w .
Case report | 111
Reflection on the case
D u rin g th e first co n su ltatio n I (ToH) collected d ata by ask in g o p en en d e d questions,
su m m arisin g a n d asking directive questions. F u rth erm o re, I aim ed at search in g for a biom edical
diagnosis of h er palpitations. I looked a t h er p alp ita tio n s fro m a bio m ed ical p o in t of v iew an d
w a n te d to exclude a cardiac cause. W h en I fo u n d a h y p o th y ro id fu n ctio n w ith th e b lo o d test I
m ainly focused on th e m edical policy an d m a n ag em en t p lan , w ith o u t reco n sid erin g the
p alp ita tio n s a n d w ith o u t leg itim ising p atien t's feelings.
L ooking back o n th is case I realised th a t initially I h a d n 't d w elled o n th e fact th a t th e p alp itatio n s
cam e u p especially d u rin g v ac u u m cleaning. W hy of all tim es d id she get th e m d u rin g v acu u m
cleaning? A t this stage I sh o u ld have sh o w n m y curiosity. D id she get p alp ita tio n s because of the
exercise or co u ld it be lin k ed to v ac u u m cleaning in p articu lar? A b etter ex p lo ratio n of her
cognitions an d w o rries ab o u t th e p alp ita tio n s w o u ld h av e b een helpful. H o w ev er, th e follow ing
con su ltatio n s gave m e th e o p p o rtu n ity to ask q u estio n s reg a rd in g p atien t's social situ atio n an d
h isto ry a n d b u ild th e d o cto r-p atien t relatio n sh ip . T hanks to th e rem ark: 'W ell doctor, it's all
a b o u t how life is lived', I w as capable of leav in g m y bio m ed ical p o in t of view . T ogether w ith the
p a tie n t I fo u n d a d ee p er m e an in g in h er sym ptom s.
D id m y co n su ltatio n skills change since th is case? Yes, th ey certain ly have. T h ro u g h th is case I
becam e keener o n p icking u p cues p atien ts give d u rin g th e consultation. C ues are a n easy tool in
d o cto r-p atien t com m unication a n d v ery u sefu l in daily practice. O f course, I do n o t k n o w for
su re if there is a causal relatio n sh ip b etw e en tellin g th e sto ry an d h er im p ro v em en t. B ut the
p a tie n t seem ed to benefit fro m discu ssin g th e p ossible relatio n sh ip , especially co n sid erin g her
relief at th e en d of the consultation.
Cues in the consultation
In p rim a ry care th ere is a tra d itio n of p ay in g atten tio n to cues a n d th eir m eaning. R ecognition of
cues a n d exp lo ratio n of th eir m e an in g is im p o rta n t for th e m u tu a l u n d e rs ta n d in g of th e doctor
a n d th e patient. W ith th e p atien t-cen tered n ess m o v em en t at th e en d of th e 1980s, p ay in g
a tten tio n to th e significance of cues becam e in v o g u e ag ain .5
R e sp onding to patien ts' cues is one of th e m o st im p o rta n t tools for a successful co n su ltatio n .13
C ues are described in d ifferent w ay s by d ifferen t au th o rs. G ask a n d U sh erw o o d refer to verbal
a n d n o n v erb al expressions of th e p a tie n t th a t h in t at psychosocial or social p ro b lem s.13L ivinson
et al describe 'cues' as direct or in d ire ct expressions w ith in fo rm atio n a b o u t p atien ts' life an d
feelings.14 B alint uses th e w o rd 'offers' for expressions b y th e p a tie n t ab o u t th e significance of
their sym p to m s an d for expressions ab o u t th e reaso n for en co u n ter w ith th e FP.15 B ranch an d
M alik describe cues as 'w in d o w s of o p p o rtu n ity ' for th e d octor to sh o w em p ath y .16 It is
112 I Chapter 6
im p o rta n t to detect a n d resp o n d to cues a t th e tim e th ey are offered by th e p atien ts.13 N o t
ad d re ssin g cues d u rin g clinical enco u n ters m ay in h ib it p atien ts fro m fu rth e r disclosures.
Berkatis et al re p o rte d a significant relatio n sh ip b etw e en th e d o cto r's resp o n se to em otional cues
an d th e p atien t's disclosure.17 M oreover, cues enable b etter u n d e rsta n d in g of p atien ts' life,
cognitions a n d em otions.18'19 R ecognition a n d ex p lo ratio n of th em h as an o th er ad v an tag e. It
show s th a t th e FP is listening carefully, w a n ts to u n d e rsta n d th e m ean in g of th e sy m p to m s an d is
in terested in th e patient.3 By pickin g u p cues a n d ex p lo rin g them , th e FP enhan ces the
th erap eu tic relatio n sh ip an d , as a consequence, im p ro v es illness outcom es a n d p atien t
satisfaction.17'20
W e k n o w th a t doctors have difficulties reco g n isin g cues. L ivinson et al ex am in ed h o w p atien ts
p rese n ted cues a n d how FPs reacted to them .21 In m o re th a n h alf of th e co n su ltatio n s, cues w ere
p rese n t (average of 2.6 cues p er consultation). P atien ts in itiated 71% of th e cues them selv es an d
29% w ere in itiated by th e FP ask in g o p en q uestions. In a m ajority of th e co n su ltatio n s (79%), FPs
m issed th e o p p o rtu n ity to react to th e cues given in th e co n su ltatio n . M oreover, these
con su ltatio n s w ere of significantly lo n g er d u ratio n . B utow et al fo u n d th e sam e resu lts in th eir
s tu d y of verb al cues in cancer p atients: oncologists d id n o t consistently d etect an d ad d re ss cues
for em otional su p p o rt. C o nsultations in w h ich oncologists re sp o n d e d to h ig h er p ro p o rtio n s of
p atien ts' cues d id n o t last longer th a n o th er co n su ltatio n s.22 C egala an aly sed v id e o tap e d
p rim a ry care consultations of 16 doctors w ith 32 p atien ts, a n d fo u n d th a t d o cto rs rarely p ro v id e
in fo rm atio n in th e absence of a direct p a tie n t q u estio n .12 M oreover, p atien ts' in d ire ct cues of
inform ational an d em otional n ee d s are far m ore com m on th a n direct p a tie n t q uestions. T hus, a
focus o n cues of n ee d s in th e clinical en co u n ter is im p o rtan t.
S alm on et al stu d ie d con su ltatio n s a b o u t m edically u n ex p lain e d sy m p to m s a n d sh o w ed th at
m o st p atien ts gave explicit cues ab o u t em otional o r social p ro b lem s.23M ost FPs reacted to these
cues b y either blocking or facilitating a d iscu ssio n ab o u t psychosocial issues. The FPs w h o
blocked a discu ssio n d id n o t p ay atte n tio n to th e cues, th ey refocused o n th e sy m p to m s an d
n o rm alised th e w o rries of th e p a tie n t or stressed p atien ts' o w n responsibility. The FPs w h o
facilitated a d iscussion a b o u t psychosocial issues d id so by ask in g q u estio n s ab o u t the
experiences of th e p a tie n t an d by explo rin g th e p ro b lem s of th e p atien t. H o w ev er, w h e n th e FPs
gave a n ex p lan atio n of the sym ptom s, th e FPs rarely to o k th e psychosocial p ro b lem s into
account. C onsequently, patien ts' concerns w ere n o t a d d re sse d a n d reassu ran ce failed.
Case report | 113
Conclusion
M ost peo p le in te rp re t th eir sy m p to m s in th e context of th eir p erso n al, fam ily a n d life
experiences. A ctive listening an d noticin g cues, as d escrib ed in th is case rep o rt, can h elp FPs to
get to kn o w their p atien ts.1
D iscovering th e patien ts' real w o rries a n d g ettin g to k n o w th eir stories gives us, as doctors, a
b etter u n d e rsta n d in g of th e ir o w n w o rld .24 In ad d itio n , m u tu a l u n d e rsta n d in g lead s to a h ig h er
satisfaction w ith care for b o th p a tie n t an d d octor a n d it stren g th en s th e d o cto r-p atien t
relatio n sh ip .3,25,26 R em arkable w o rd s, stran g e clauses, sentences th a t y o u do n o t directly
u n d e rsta n d - ask for their m eaning. It b rin g s th e p atien t's a n d th e d o cto r's w o rld closer together.
Acknowledgements
W e w o u ld like to th a n k E velyn v an W eel-B aum garten a n d P eter L ucassen for rev iew in g the
m a n u scrip t a n d their com m ents.
6
114 I Chapter 6
Reference List
1
S tu rm b erg JP. The fo u n d atio n s of p rim a ry care. D arin g to b e different. O xford - Seattle:
Radcliffe P u b lish in g Ltd; 2007.
2
3
M isselbrook D. T hinking a b o u t patien ts. N ew bury: Petroc press; 2001.
L ang F, Floyd MR, Beine KL. C lues to p atien ts' ex p lan atio n s a n d concerns ab o u t their
illnesses. A call for active listening. A rch F am M ed 2000; 9(3):222-227.
4
F oucault M. The b irth of th e clinic. A n A rchaeology of m edical p ercep tio n . London:
T avistock P ublications; 1973.
5
L evenstein JH, M cC racken EC, M cW hinney IR, S tew art M A, B row n JB. The p a tie n t­
cen tred clinical m ethod. 1. A m o d el for th e d o cto r-p atien t in teractio n in fam ily
m edicine. Fam P ract 1986; 3(1):24-30.
6
v a n D u lm en AM, F ennis JF, M okkink H G , V an der V elden H G , Bleijenberg G. D octord e p e n d e n t changes in com plain t-related cognitions an d anxiety d u rin g m edical
consultations in fun ctio n al ab d o m in al com plaints. P sychol M ed 1995; 25(5):1011-1018.
7
v a n D u lm en AM, F ennis JF, M okkink H G , V an der V eld en HG, Bleijenberg G. P ersistin g
im p ro v e m en t in com p lain t-related cognitions in itiated d u rin g m edical co n su ltatio n s in
fun ctio n al ab d o m in al com plaints. P sychol M ed 1997; 27(3):725-729.
8
Starfield B, W ray C, H ess K, G ross R, Birk PS, D 'L ugoff BC. The influence of p atien tp ractitio n er ag reem en t o n outcom e of care. A m J Public H ea lth 1981; 71(2):127-131.
9
S tew art MA, M cW hinney IR, Buck CW. The d o c to r/p a tie n t relatio n sh ip a n d its effect
u p o n outcom e. J R Coll G en P ract 1979; 29(199):77-81.
10 M aguire P, F aulkner A, B ooth K, Elliott C, H illier V. H elp in g cancer p atien ts disclose
their concerns. E ur J C ancer 1996; 32A(1):78-81.
11 P elte n b u rg M, Fischer JE, Bahrs O, v a n D u lm en S, v a n d en B rink-M uinen A. The
unex p ected in p rim a ry care: a m u lticen ter s tu d y o n th e em ergence of u n v o iced p atien t
agenda. A n n F am M ed 2004; 2(6):534-540.
12 C egala DJ. A stu d y of doctors' a n d p atien ts' co m m u n icatio n d u rin g a p rim a ry care
consultation: im plications for com m u n icatio n train in g . J H ea lth C o m m u n 1997; 2(3):169194.
13 G ask L, U sh erw o o d T. ABC of psychological m edicine. The consultation. BMJ 2002;
324(7353):1567-1569.
14 L evinson W , R oter DL, M ullooly JP, D ull VT, Frankel RM. P h y sician -p atien t
com m unication. The relatio n sh ip w ith m alpractice claim s am o n g p rim a ry care
ph ysicians an d surgeons. JAM A 1997; %19;277(7):553-559.
15 B alint M. The doctor, his p a tie n t a n d th e illness. E d in b u rg h : C hurchill L ivingstone; 2000.
16 B ranch W T, M alik TK. U sing 'w in d o w s of o p p o rtu n ities' in b rief in terv iew s to
u n d e rsta n d patien ts' concerns. JAM A 1993; 269(13):1667-1668.
Case report | 115
17 B ertakis KD, R oter D, P u tn am SM. The relatio n sh ip of p h y sician m edical in terv iew style
to p a tie n t satisfaction. J F am P ract 1991; 32(2):175-181.
18 Spiro H. W hat is em p ath y an d can it be ta u g h t? A n n In tern M ed 1992; 116(10):843-846.
19 Bryne PS, L ong BE. D octors ta lk in g to p atien ts. L ondon: H er m ajesty's statio n ery office;
1976.
20 S uchm an AL, M atthew s DA. W h at m akes th e p atien t-d o cto r relatio n sh ip th erap eu tic?
E xploring th e connexional dim en sio n of m edical care. A n n In tern M ed 1988; 108(1):125130.
21 L evinson W , G oraw ara-B hat R, L am b J. A stu d y of p a tie n t clues an d p h y sician resp o n ses
in p rim a ry care a n d surgical settings. JAM A 2000; 284(8):1021-1027.
22 B utow PN , B row n RF, C ogar S, T attersall M H , D u n n SM. O ncologists' reactions to
cancer patien ts' verbal cues. P sychooncology 2002; 11(1):47-58.
23 S alm on P, D ow rick CF, Ring A, H u m p h ris GM. V oiced b u t u n h e a rd agendas: q u alitativ e
analysis of the psychosocial cues th a t p atien ts w ith u n ex p lain e d sy m p to m s p rese n t to
general p ractitioners. Br J G en P ract 2004; 54(500):171-176.
24 Cole-Kelly K. Illness stories a n d p a tie n t care in th e fam ily p ractice context. F am M ed
1992; 24(1):45-48.
25 S tew art M, B row n JB, W eston W W , M cW hinney IR, M cW illiam C, F reem an T. P atientcentered m edicine. second ed itio n ed. O xford: Radcliffe m edical press; 2003.
26 W anzer MB, B ooth-B utterfield M, G ru b er K. P ercep tio n s of h ealth care p ro v id ers'
com m unication: relatio n sh ip s b etw e en p atien t-cen tered co m m u n icatio n a n d satisfaction.
H ea lth C o m m un 2004; 16(3):363-383.
118 I Chapter 7
Summary
Objectives.
To study doctor-patient interaction styles in consultations with patients
presenting persistent medically unexplained symptoms (MUS) and to study on which stages of
the consultation patients and doctors focus within the available time.
Methods.
Exploratory, qualitative analysis of transcripts of 20 videotaped consultations
between family physicians (FP) and persistent MUS patients.
Results.
Patients presented many symptoms in a rather unstructured way. However, FPs
hardly used structuring techniques such as agenda setting and summarizing. Patients with
persistent MUS got much opportunity to tell their story, but the reasons for encounter, their
beliefs and concerns were not discussed in a structured manner. Although consultations were
focused on these issues, mostly patients themselves initiated discussion of their ideas, concerns
and expectations. FPs' extensive explanations of the origin of the symptoms often did not take
patients' beliefs and concerns into account.
Conclusions.
Due to patients' multiple symptom presentation and the absence of FPs'
structuring techniques, consultations of persistent MUS patients proceed rather unfocused.
However, patients got ample opportunity to tell their story.
Practice implications.
Persistent MUS patients might benefit from structured
consultations focused on the exploration of the reason for encounter.
How patients and FPs com municate about persistent MUS | 119
Introduction
Patients complaining of physical symptoms in the absence of physical disease are common in
primary care. These symptoms are often described as medically unexplained symptoms
(MUS) .u In patients with MUS, symptoms or impairment improve when consultations meet the
patients' expectations or when patients feel understood.3 Recently, two studies showed that
physicians' communication during the initial presentation of MUS is hampered.4'5Epstein et al.
concluded that physicians face lack of time and do not explore and validate the MUS patient's
reason for visit, their ideas, expectations and concerns.4 Kappen and Van Dulmen concluded
that family physicians (FPs) explore patients' concerns mainly medically.5 Despite these
physicians' communication barriers during the initial presentation of MUS,6only a minority (2.5
percent) of the patients will evolve into a chronic disabling condition of persistent MUS.7From
this moment communication is often the only tool FPs have in handling these patients.4'8
However, doctor-patient interaction styles in consultations with patients with persistent MUS
have not been well studied, and may bring important insights to improve the quality of care of
these patients.
Consultations between doctors and persistent MUS patients are not straightforward but can be
considered as complex consultations.9 As symptoms are medically unexplained, the link
between cause and symptom is unclear, and FPs are uncertain about the way forward.10
Persistent MUS patients are aware of the complex nature of their problems.11-13 They have to
present complex and multifaceted reasons for consulting, discuss concerns about the symptoms
and problems, and choose whether or not to present emotional aspects of their problems, in a 10­
15 minutes consultation.13-15 It is understandable that both patients and FPs report insufficient
time to deal effectively with persistent MUS during consultations.16'17However, it is still not clear
how patients and FPs reach their goals during the consultations and on which stages in the
consultation they focus.
Therefore, the aim of this study is to analyze (1) how patients present and how FPs explore the
patients' symptoms and problems during consultations and (2) on which stages of the
consultation they focus within the available time.
Methods
Data source: Dutch National Survey of General Practice
Data for the present study were drawn from the Second Dutch National Survey in General
Practice (DNSGP-2).18This survey is a large-scale research project carried out in the Netherlands
between May 2000 and April 2002 and studied a representative sample of 104 family practices
120 I Chapter 7
with 195 FPs and 399,068 listed patients. The survey comprised an epidemiologic study about
the work of FPs and a video observation study of consultations in which each participating FP
consented to video tape approximately 20 clinical encounters on two arbitrary days. A total of
142 FPs (72.8% ) agreed to participate in the video observation study.19Prior to the consultation, a
research assistant informed the patients and asked informed consent about the video
observation. A total of 2784 patients participated in the video-observation study, 377 patients
(11.9%) refused. Before and after the videotaped encounter patients completed a questionnaire
about sociodemographic characteristics, presented symptoms and general health status.
Immediately after the consultation, FPs completed a questionnaire with items on characteristics
of the FP, questions about how familiar the FP was with the patient and how the FP valued the
psychosocial and work related aspects of the presented symptoms. Furthermore, FPs rated on a
5-point Likert-type scale (extremes labeled as 'not at all' and 'very much') whether they believed
psychosocial factors played a role in the problem presented during the consultation. FPs coded
patients' symptoms and diagnoses according to the International Classification in Primary Care
(ICPC) system.20'21
Selection of patients with m edically unexplained symptoms
We selected from the video-observation study all videotaped consultations in which medically
unexplained symptoms were the main subject of the encounter. Inclusion criteria were: (1)
patients consulting their own FP, (2) consultations for physical symptoms for which the patient
had consulted the FP before and in which, according to the FP, the symptoms were related to
psychosocial factors ('much'/'very much' on 5-point Likert-type scale), (3) age of the patient > 18
years and (4) no psychiatric diagnosis an d /o r social diagnosis according to the ICPC during this
consultation. Exclusion criteria were: bad sound-quality and consultations by one of the
authors. When more than one video consultation of a FP appeared in our selection, only the first
consultation was included. Two independent researchers (ToH and SvD or EvR) looked at the
video recordings and established whether medically unexplained symptoms were the main
topic. Encounters were included in the final sample when both researchers agreed. In case of
disagreement, we excluded the consultation. We used Cohen's kappa statistic
(k )
to assess
agreement between the two researchers.22
Data analysis
Data analysis started by using qualitative methods to develop a coding scheme of FPs'
exploration of the patients' symptoms and problems.23The theoretical framework guiding the
analysis was the broad concept of the biopsychosocial model.24This model proposes illness to be
viewed as a result of interacting mechanisms at the biomedical, interpersonal and
environmental levels. The model is widely used in primary care consultations. Using this model
in consultations implies that patients' symptoms, illness beliefs, anxiety, concerns, illness
behavior and social environment are addressed.25
How patients and FPs com municate about persistent MUS | 121
The included videotaped consultations were completely and anonymously verbatim
transcribed and entered into Atlas.ti. The qualitative analyses were executed with this software
program, a package for detailed coding in qualitative data analysis.
We analyzed the transcripts using the principles of constant comparative analysis.26During this
analysis transcripts are subsequently thematically coded. The main aim of this analysis is to
organize utterances by theme and to explore similarities and differences between consultations.
Two researchers (ToH, EvR) read all transcripts several times to familiarize themselves with the
data. They independently made a first categorization by applying codes to meaningful words
and sentences in the transcripts. These codes were discussed and refined during consensus
meetings. When additional codes emerged these were discussed and applied to the transcripts.
Concepts and categories emerged through this iterative process of coding, analysis and
discussion. Codes appearing from the utterances of the participants in the consultations are
presented in Table 1. During the iterative process of qualitative analysis we noticed the complex
structure of the consultations. To gain a better understanding of this complex structure we
decided to code the stages of the consultation, apart from the utterances of the participants
during the consultation. These stages were derived from the Dutch FPs' communication skills
training program15,27,28(Table 2). After 8 videotaped consultations, the first results of the analysis
were discussed with a senior researcher (PL). Data collection continued until no significant new
themes emerged (saturation).29This was achieved after 15 consultations. To quantify on which
stages of the consultation patients and FPs focus within the available time of the consultation,
we calculated, as a proxy, the percentage of text in the transcript (the number of text lines of a
particular stage of the consultation divided by the total number of text lines of the consultation)
spent on each of the different stages.
Ethical approval
The study was carried out according to Dutch privacy legislation rules. The privacy regulation
was approved by the Dutch Data Protection Authority.
Results
Sample characteristics
The total number of video consultations in the Second Dutch National Survey of General
Practice (DNSGP2) was 2784. Fifty nine of these video consultations met our inclusion criteria
and were screened by one of the authors (ToH). In 14 cases more than one video consultation of a
FP appeared in the selection, 4 video consultations had a bad sound quality and in 1 video
122
I C hapter 7
consultation one of the authors (PL) was the FP. These 19 video consultations were excluded.
Therefore, a total of 40 video consultations could be included for screening by two independent
researchers (ToH and SvD or EvR). Because MUS was not the main topic of the consultation in 20
of these video consultations, a total of 20 video consultations could be included for further
analysis (Figure 1). The interobserver agreement for inclusion was k = 0.79 (95%-CI: 0.59 - 0.99).
We considered this level of agreement to be 'good'.
Eight (40%) of the patients involved in the final video consultation sample were men, aged
between 25 and 80 (mean = 47) years. The 20 FPs consisted of 15 (75%) men, aged from 34 to 61
(mean = 45) years with an average of 15.7 (range 3 - 30) years of FP working experience. Mean
(and median) duration of consultation was 13.5 (12.1) minutes; ranging from 8.1 to 37.0 minutes.
Within the available time of the consultation, patients and doctors focus most on the story of the
patient, discussion and exploration of patients' beliefs and concerns, and on explaining the
symptoms (respectively 21.8, 18.7 and 16.8% of the total amount of text is spent on these stages)
(Table 3). Agenda setting, summarizing and evaluation of the consultation was limited.
Figure 1. Selection of p ersistent MUS video consultations
Excluded (n = 2725)
according to criteria
Excluded (n = 14)
because more than one
video consultation of a
FP in the selection
Excluded (n = 20)
because MUS was not
the main topic of the
video consultation
Excluded because of
bad sound quality (n = 4)
and because one of the
authors (PL) was the FP
in the video consultation
(n = 1)
How patients and FPs com municate about persistent MUS | 123
Table 1. Codes appearing from utterances of the participants of the persistent MUS consultations
Codes
Story of the patient (narrative)
Symptoms
Patients' beliefs and expectations
Patients' fears and concerns
Consequences on patients' daily activities and illness behavior
Consequences on patients' social environment
Explanation
Table 2. Stages of the consultation
Story of the patient (narrative)
The retelling, in patients' ow n words, of a series of unfolding events regarding the symptoms, representing the
patient individual viewpoint
A genda setting
Agreement (between patient and FP) of the issues which should be discussed during the consultation
Discussion / exploration of the symptom s
Discussion and exploration of the characteristics of the symptoms (nature, location, intensity, frequency and
duration)
Discussion / exploring of the reason for encounter (RFE)
Discussion and exploration of the reason for encounter, including the patients' expectations regarding the
actions of the doctor
Discussion / exploring of patients' beliefs and concerns"
Discussion and exploration of patients' ideas regarding the symptoms, such as patients' own explanations,
sym ptom attribution, patients' ow n influences on the sym ptoms (self-efficacy), concerns and (negative)
emotions regarding the symptoms
Discussion / exploration of the consequences on patients' daily activities, social environm ent and illness
behaviorb
Discussion and exploration of patients' behaviour in response to the symptoms, the w ay patients cope with
their symptoms, the consequences of the symptoms on patients' daily activities, the influences of the symptoms
on patients' social life, and reactions and opinions of the people in patients' surroundings.
Sum m arizing
FPs' sum m ary of the symptoms, reason for encounter, beliefs, concerns and consequences of the symptoms
presented during the consultation
Physical exam ination
The process by w hich the FP performs a physical examiniation
Explanation
FPs' explanation of the origin of the symptoms presented during the consultation
Evaluation of the consultation (including m aking a follow -up appointm ent)
Evaluation of the consultation, including the question w hether the consultation has been helpful, explanation
a n d /o r advices, whether the reason for encounter has been answered, and whether follow-up appointments
have been made.
a Matches w ith the codes "patients' beliefs and expectations" and "patients' fears and concerns" that appeared from the utterances of participants of
persistent MUS consultations.
b Matches w ith the codes "consequences on patients' daily activities and illness behavior" and "consequences on patients' social environment" that
appeared from the utterances of participants of the persistent MUS consultations.
124 I Chapter 7
Table 3. The percentage of text in the transcripts spent n each of the different stages of the consultation
Persistent MUS patient
M ean
Story of the patient (narrative)
21.8
A genda setting
limited
Symptom exploration
7.9
Reason for encounter (RFE)
Initiated by the FP
Initiated by the patient
0.6
2.1
Patients' beliefs and concerns
Initiated by the FP
Initiated by the patient
4.8
13.9
Consequences on patients' daily activities, social
en v iro n m en tan d illn e ss behavior
Initiated by the FP
Initiated by the patient
1.1
2.7
Sum m arizing
limited
Physical examination"
-
Explanations
16.8
Evaluation of the consultation
limited
Other”
28.3
aQuantifying physical examination is not possible by using the proxy percentage of text spent.
” Talk/discussion regarding medically explained symptoms (for example: presentation of a pneumonia, discussion on therapies for asthma,
discussion and management of hypertension, etc.).
Patients' symptom presentation
Most (95%) persistent MUS patients presented more than one symptom. Three quarters of the
patients presented medically unexplained symptoms as well as medically explained symptoms.
The average number of symptoms presented was 3.6 (range 1 - 5). The average number of MUS
presented was 2.4 (range 1 - 5). The most common symptoms were musculoskeletal (n = 15),
gastrointestinal (n = 8) and general and unspecified symptoms (n = 11), such as feeling ill,
weakness/tiredness, sweating or swelling.
Persistent MUS patients presented multiple symptoms and seemed to switch from one
symptom to another during all stages of the consultation.
They often started to discuss new symptoms and concerns after the FP finished history taking,
physical examination and explanation. (Quotation 1)
Quotation 1 (P11 116-12;023-111)
[Patient's story, symptom 1]*
P: It's either painful gas or it's a lot o f pain in m y belly. A n d m y bowel movements happen or don ' t
How patients and FPs com municate about persistent MUS | 125
happen but they look kind o f weird. B ut it will go away. It's always gone away eventually.
D : Okay, so you have had these comp laints for years.
[Medical exploration]
D: Abnormal bowel movements. No blood or mucus ?
P: No. No.
D: Firm and pulpy, no diarrhea?
P: No, I don't have that.
[No physical examination]
[Explanation]
D: Okay, it seems to me that you have irritable bowel syndrome - sensitive intestines - and that can
cause cramps. A bout 20% of the population has this kind o f bowel problem to some extent. It's not
malignant and there is no infection. It's ju s t that the intestines d on't function optimally. A n d so
it's important that you get enough fiber and that you take the powders (movicolon).
[Patient's story, symptom 2]
P: A n d the itch. It won ' t go away and it's awful.
D: So, we have to deal w ith the itch.
P: Yes, it's ridiculous but it's sometimes really bad on m y face and on m y back, it's the worst - it's
always the same place. I've had it for a really long time.
*the words between brackets represent the codes given by the researchers and used in the
constant comparative analysis
Patients' attempts to address their needs
In most encounters, the patients' reason for seeking help remained unclear. Although clarifying
the reason for encounter (RFE) is an important task for the FP in order to reach a more focused
communication, in 13 consultations (65%) there was no exploration of the reason for encounter
at all. The absence of FPs' exploration of the reason for encounter might be the reason why
patients themselves try to initiate such a discussion. It appeared from the data that during
consultations in which the reason for encounter was discussed (n = 7), most of the time the
patients themselves initiated talking about this subject (n = 5). (Quotation 2) Only in two
consultations the doctor initiated the discussion on the reason for encounter.
Discussions on the reason for encounter took 2.7% (range 0 - 15.7) of the text in the transcripts.
(Table 3)
Quotation 2 (P8 C10208;24-31)
P: A n d when I go to bed, I feel very restless. I have these heart palpitations.
D: Yes,
P: So I was wondering - 1 read about something called beta-blockers. I don ' t know i f that applies to
m y situation but -
126 I Chapter 7
D: Hmm
P: Someone told me about propanolol. I was wondering i f that was something for me.
D: Yeah, okay.
In all but two video consultations patients started talking about their beliefs and concerns.
However, in the two encounters in which no discussion on beliefs and concerns took place, the
patient tried to initiate such a discussion but the FP refrained from responding (Quotation 3). In
the encounters in which beliefs and concerns were discussed, patients mostly initiated such a
discussion: in 16 consultations (89%) patients made attempts to initiate discussion, whereas in 9
consultations (50%) FPs did. This is also reflected in the amount of text spent in the transcripts of
the consultations on this topic. The total amount of text spent in the transcripts regarding
discussing patients' beliefs and concerns initiated by the patient or by the FP is 13.9% (range 0 40.1), respectively 4.8% (range 0 - 17.8). (Table 3)
It is noteworthy that in the majority of the consultations (10 out of 18) in which patients' beliefs
and concerns were discussed, discussion of these beliefs and concerns only took place for a
limited number of symptoms presented during the consultation.
Quotation 3 (P1 C2601;132-140)
P: It's not good at all. I feel m yself going so unbelievably downhill.
D: This is something you need to discuss w ith a neurologist. You can make an appointment with
one. I'll write a referral letter and you can pick that up at m y assistant's desk. But your legs: that's
also an issue for you ?
P: Yes, I know I have a lot of weight to carry but, oh my, that's not easy. It's like something is
broken in m y brain. I think every time, 'I have to lose weight, I have to lose weight, ' and, at the very
same moment, I stuffm yself. It ju st doesn't work that way up here (P points to head).
D: You need to lose weight but you eat too.
The consequences of the symptoms on patients' daily activities, social environment and illness
behavior was less well discussed. In 9 consultations (45%) there was no discussion of these
themes at all. Again, most of the time discussion of these consequences of the symptoms was
initiated by the patients namely in 7 consultations; in one consultation this discussion was
initiated by the FP as well as the patient and in three consultations the FP initiated the
discussion. (Quotation 4) Almost 3% (2.7; range 0 - 12.3) of the total amount of text in the
transcripts of the consultations spent on talking about the consequences of the symptoms on
daily activities, social environment and illness behavior was initiated by the patient against 1.1%
(range 0 - 7.4) initiated by the FP. (see Table 3)
How patients and FPs com municate about persistent MUS | 127
Quotation 4 (P2 C070-13;34-45)
D: How are you sleeping?
P: A t night, I sleep okay now, but during the day, I try not to spend time in bed. It's nice to know
that I can go to bed but then I restrain myselfwith, 'No, I can't stay in bed all day. ' A n d then I try to
do some s tu ff around the house - the dishes, vacuuming, dusting.
D: So you do that?
P: A n d then I try to sleep at night. A n d when I wake up in the morning, I have those puffy eyes.
A n d those chewable pills, I don't take them one after another anymore. Or should I keep taking
them ? Because sometimes I still have - especially when I have to bend over, I still see stars.
D: B ut you eat well ?
P: Yes, if I know that I need some kind o f feeling or is that not necessary?
In nearly all consultations there was much opportunity for explanation of the symptoms. The
total amount of text in the transcripts about explanations is 16.8% (range 0 - 52.9). (Table 3)
Although almost one fifth of the text in the transcripts was spent on explaining the symptoms,
patients responded on FP explanations with new remarks about their symptoms, beliefs and
concerns.
Furthermore, most of the time, explanations given by the FPs did not incorporate beliefs and
concerns that patients presented during the consultation. Moreover, FPs attempts to reassure
patients were often not focused on the patients' concerns. (Quotation 5)
Quotation 5 (P4 C077-04:4-9;21-26; 80-85; 109-11)
[Patient concerns]
P: I'm having problems w ith m y throat, esophagus again. I feel it when I am doing exercise. It
doesn 't have anything to do w ith m y heart, does it? I have it every time I roll over at night.
D: Yes
P: I don't know but I think that it's lower. It's like something is stuck there.
[Reason for encounter and patient concerns]
P: I've also had chest pains so I wanted to ask i f you would be willing to take a look. I'm a little
concerned. I'd ju st like to know for sure that there ' s nothing going on.
D : I f we know that it's your throat and not your heart, then that ' s good.
P: Yes.
[Explanation]
P: I was also really busy earlier this week. I've been feeling kind o f hurried the last little while so I
took a seresta pill and the pain in m y throat w ent away.
D: Yes, that could mean that the tension that you feel inside is coming out through your throat, like
your throat is literally being choked.
P: Yes, I do have that kind of feeling.
128 I Chapter 7
[Patient response]
P: B ut m y heart has nothing to do w ith it?
D: No, your heart has nothing to do w ith it.
FPs' structuring behavior
In the video consultations, FPs gave patients with persistent MUS much opportunity to tell their
story (21.8% (range 5.1 - 80.7) of the text in the transcripts). However, FPs did not do an in-depth
inquiry of the symptoms (7.9% (range 0 - 39.4) of the text in the transcripts). In 50% of the
consultations (n = 10) there was no in-depth inquiry of the presented symptoms at all. In half of
the consultations in which an in-depth inquiry of the symptoms was performed, the FP did not
explore all medically unexplained symptoms presented during that consultation. Furthermore,
it appeared from the video consultations that FPs hardly use structuring techniques, such as
agenda setting, announcing and performing physical examination and summarizing the
information obtained during the consultation. Agenda setting was explicitly performed in one
consultation . Physical examination was performed in eight consultations and a summary was
given in only one consultation.
Discussion and conclusion
Discussion
Our findings of the difficulties of discussing the reason for encounter and patients' beliefs and
concerns regarding the symptoms during the persistent MUS consultations are in line with the
findings of Epstein et al.4 Furthermore, it is known from direct observation of patients'
presentations of MUS that almost all patients provide opportunities for FPs to address
psychosocial issues, psychosocial concerns.5,3“ Our study adds rigor to these findings as we
studied doctor-patient communication in persistent MUS consultations. Our results indicate
that doctor-patient communication can be improved by focusing on the exploration of patients'
beliefs and concerns and incorporating these into FPs' explanatory and reassuring strategies.
These findings are important as discussion of patient's ideas and concerns, shared
understanding and clarifying the reason for encounter contribute to a more satisfactory
consultation according to patients.31
The observations of our study confirm that the chaotic structure of most MUS consultations
reflect the chaotic narrative of the people who live with MUS.32Nettleton highlighted that the
narratives of MUS patients shared many features of chaos narratives.33 These narratives are
characterized by confusion and uncertainty in the absence of a diagnosis and prognosis.32
Moreover, these narratives are difficult to 'listen' to and difficult to 'hear', because it reminds us
How patients and FPs com municate about persistent MUS | 129
of our own vulnerability and limitations.34 This might explain why FPs have difficulties in
structuring the persistent MUS consultations and why patients present multiple symptoms in a
rather unstructured way. Although giving patients time for their story is an important element
of working patient-centered, persistent MUS patients might benefit from more focused patientcentered interaction style in which FPs structure the consultation and explore needs, concerns
and beliefs. The ample opportunity patients get to tell their story and present their symptoms
possibly reflect FPs' commitment with these patients which is in line with research on FPs
perceptions about patients with persistent MUS.10However, this commitment is worth to yield
more effect.
This is the first study in patients with heterogeneous undifferentiated persistent MUS using
consultations between doctor and MUS patients in which neither the doctor, nor the patient was
aware of the subject of study. Doctor-patient communication studied in this way represents
daily practice reality. Furthermore, FPs and patients in these consultations already built a
doctor-patient relationship as they knew each other for a long time and had discussed the
symptoms before. However, in most cases, a single consultation is not the beginning or the end
of the story. Each new consultation carries over memories of previous ones, which might have
influenced the videotaped consultations.35 This might explain why we found limited medical
exploration of the presented symptoms and no physical examination in most consultations.
However, we did not find utterances referring to the content of previous consultations on the
symptoms presented.
Video-recording has been recommended as the best method for researching doctor-patient
communication during consultations.36 According to Coleman, there is little evidence that
video-recording influences the behavior of either the FPs or patients (i.e. Hawthorne effect), but
it may cause bias in the characteristics of doctors and patients who agree to participate.37
However, with a response rate of 89% in the DNSFP-2 and the attendance of a representative
sample of family practices in The Netherlands, participation bias in our study will be limited.
Furthermore, we found 2.1% (59 out of 2784) of the total number of video consultations in the
DNSGP-2 concerned consultations with patients with persistent MUS. This is in line with the
findings of Verhaak et al. that 2.5% of the patients in primary care present with persistent MUS.7
By quantifying on which stages of the consultation patients and FPs focus within the available
time of the consultation, we studied the doctor-patient communication in persistent MUS
consultations on different levels which improved our understanding of the role of the doctorpatient communication.23'38We chose to quantify as measure of focus the number of text lines. We
decided to this approach as it had in our view, face validity, but it is important to formally
validate it in further study. Besides, we do realize that the FP's and patient's speaking rate, the
130 I Chapter 7
duration of silences within the consultation and other non-verbal characteristics can make the
number of text lines as a proxy of speech focus less reliable. As our goal was not to study doctorpatient interaction on micro level, we choose not to use conversation analysis techniques.39
The small sample size and the cross sectional nature of the qualitative analysis preclude
definitive conclusions. Our findings should be confirmed in a larger, prospective qualitative
study that could track doctor-patient communication regarding the unexplained symptoms
over time.
Conclusion
Patients' showed a rather unfocused and fragmented presentation of multiple symptoms
during all stages of the persistent MUS consultation. However, ways of giving structure to the
consultation such as agenda setting and summarizing were hardly ever used by the FPs. Patients
had ample opportunity to tell their story, but the reason for encounter, patients' beliefs and
concerns were not discussed in a structured manner. Mostly, patients themselves initiated
discussion on the reason for encounter, their beliefs and concerns and the consequences on daily
activities, social environment and illness behavior. Furthermore, the extensive explanation of
the origin of the symptoms they received from their FP was often not focused on their beliefs and
concerns.
Although consultations with persistent MUS patients seemed quite patient-centered as patients
have much opportunity for telling their story, patients might benefit more from a structured
consultation focused on the exploration of their ideas, concerns and expectations.
Practice implication
Exploration and validation of patients' experiences of illness, patients' distress and patients'
concerns and incorporating these items into explanations and reassurance may improve the care
of patients with persistent MUS.
Educational interventions in graduate and advanced professional training, aiming at enhancing
a systematic symptom exploration and reason for encounter, improving FPs symptom
explanation and reassurance during the persistent MUS consultation should be developed and
might result in a more focused patient-centered approach which can enhance the wellbeing of
patients with MUS.
How patients and FPs com municate about persistent MUS | 131
Acknowledgments
The Second Dutch National Survey of General Practice was funded by the Ministry of Health,
Welfare and Sports. The authors are grateful for the efforts of the family practices, the patients
and the research staff of the DNSGP-2.
This study was supported by grant 920-03-339 from ZonMw (Netherlands Organization for
Health Research and Development).
132 I Chapter 7
Reference List
1
Kroenke K, Mangelsdorff AD. Common symptoms in ambulatory care: incidence,
evaluation, therapy, and outcome. Am J Med 1989; 86(3):262-266.
2
Bridges KW, Goldberg DP. Somatic presentation of DSM III psychiatric disorders in
primary care. J Psychosom Res 1985; 29(6):563-569.
3
Downes-Grainger E, Morriss R, Gask L, Faragher B. Clinical factors associated with
short-term changes in outcome of patients with somatized mental disorder in primary
care. Psychol Med 1998; 28(3):703-711.
4
Epstein RM, Shields CG, Meldrum SC, Fiscella K, Carroll J, Carney PA et al. Physicians'
responses to patients' medically unexplained symptoms. Psychosom Med 2006;
68(2):269-276.
5
Kappen T, van Dulmen S. General practitioners' responses to the initial presentation of
medically unexplained symptoms: a quantitative analysis. Biopsychosoc Med 2008;
2(1):22.
6
olde Hartman TC, Borghuis MS, Lucassen PL, van de Laar FA, Speckens AE, van Weel
C. Medically unexplained symptoms, somatisation disorder and hypochondriasis:
course and prognosis. A systematic review. J Psychosom Res 2009; 66(5):363-377.
7
Verhaak PF, Meijer SA, Visser AP, Wolters G. Persistent presentation of medically
unexplained symptoms in general practice. Fam Pract 2006; 23(4):414-420.
8
Ring A, Dowrick CF, Humphris GM, Davies J, Salmon P. The somatising effect of clinical
consultation: What patients and doctors say and do not say when patients present
medically unexplained physical symptoms. Soc Sci Med 2005; 61(7):1505-1515.
9
Innes AD, Campion PD, Griffiths FE. Complex consultations and the 'edge of chaos'. Br J
Gen Pract 2005; 55(510):47-52.
10 olde Hartman TC, Hassink-Franke LJ, Lucassen PL, van Spaendonck KP, van Weel C.
Explanation and relations. How do general practitioners deal with patients with
persistent medically unexplained symptoms: a focus group study. BMC Fam Pract 2009;
10:68.:68.
11 olde Hartman TC, Lucassen PLBJ, van de Lisdonk EH, Bor JHJ, van Weel C. Chronic
functional somatic symptoms: a single syndrome? Br J Gen Pract 2005.
12 Escobar JI, Waitzkin H, Silver RC, Gara M, Holman A. Abridged somatization: a study
in primary care. Psychosom Med 1998; 60(4):466-472.
13 Peters S, Rogers A, Salmon P, Gask L, Dowrick C, Towey M et al. What do patients
choose to tell their doctors? Qualitative analysis of potential barriers to reattributing
medically unexplained symptoms. J Gen Intern Med 2009; 24(4):443-449.
14 Stuarts M, Lieberman J. The fifteen minute hour: therapeutic talk in primary care.
Abingdon: Radcliffe Publishing Ltd; 2008.
How patients and FPs com municate about persistent MUS | 133
15 van Dalen J, Prince CJ, Scherpbier AJ, van der Vleuten CP. Evaluating Communication
Skills. Adv Health Sci Educ Theory Pract 1998; 3(3):187-195.
16 Dowrick C, Gask L, Hughes JG, Charles-Jones H, Hogg JA, Peters S et al. General
practitioners' views on reattribution for patients with medically unexplained symptoms:
a questionnaire and qualitative study. BMC Fam Pract 2008; %19;9:46.:46.
17 Peters S, Stanley I, Rose M, Salmon P. Patients with medically unexplained symptoms:
sources of patients' authority and implications for demands on medical care. Soc Sci
Med 1998; 46(4-5):559-565.
18 Westert G, Jabaaij L, Schellevis F. Morbidity, performance and quality in primary care.
Dutch general practice on stage. Oxford: Radcliff publishing; 2006.
19 van den Brink-Muinen A, van Dulmen S, de Haes HC, Visser AP, Schellevis FG, Bensing
JM. Has patients' involvement in the decision-making process changed over time?
Health Expect 2006; 9(4):333-342.
20 Lamberts H, Hofmans-Okkes I. Episode of care: a core concept in family practice. J Fam
Pract 1996; 42(2):161-169.
21 WONCA International Classification Committee. ICPC-2: International Classification of
Primary care. second ed. Oxford: Oxford University Press; 1998.
22 Cohen J. A coefficient of agreement for nominal scales. Educational and psychological
measurement 1960; 20:37-46.
23 Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative
data. BMJ 2000; 320(7227):114-116.
24 Engel GL. The need for a new medical model: a challenge for biomedicine. Science 1977;
196(4286):129-136.
25 Metz JCM, Verbeek-Weel AMM, Huisjes HJ. Raamplan 2001 artsenopleiding; bijgestelde
eindtermen van de artsopleiding. Nijmegen: Mediagroep Nijmegen; 2001.
26 Glaser BG, Strauss AL. The discovery of grounded theory. Chigago: Aldine; 1967.
27 Ram P, Grol R, Rethans JJ, Schouten B, Van der Vleuten C, Kester A. Assessment of
general practitioners by video observation of communicative and medical performance
in daily practice: issues of validity, reliability and feasibility. Med Educ 1999; 33(6):447454.
28 Wigersma L, van Berkestijn LG, Giesen P. Eindtermen huisartsopleiding 2000. 2000.
Universitair Medisch Centrum Utrecht. Ref Type: Report
29 Lincoln YS, Guba EG. Naturalistic Inquiry. Beverly Hills, CA: Sage; 1985.
30 Salmon P, Dowrick CF, Ring A, Humphris GM. Voiced but unheard agendas: qualitative
analysis of the psychosocial cues that patients with unexplained symptoms present to
general practitioners. Br J Gen Pract 2004; 54(500):171-176.
31 Arborelius E, Bremberg S. What can doctors do to achieve a successful consultation?
Videotaped interviews analysed by the 'consultation map' method. Fam Pract 1992;
134 I Chapter 7
9(1):61-66.
32 Nettleton S, Watt I, O'Malley L, Duffey P. Understanding the narratives of people who
live with medically unexplained illness. Patient Educ Couns 2005; 56(2):205-210.
33 Frank AW. The wounded storyteller; body, illness, and ethics. Chicago and London: The
University of Chicago Press; 1995.
34 Nettleton S. Enigmatic Illness: Narratives of Patients who Live with Medically
Unexplained Symptoms. Social-Theory-and-Health 2004; 2(1):47-66.
35 McWhinney IR. A textbook of Family Medicine. New York; Oxford: Oxford University
Press; 1989.
36 Inui TS, Carter WB. Problems and prospects for health services research on provider­
patient communication. Med Care 1985; 23(5):521-538.
37 Coleman T. Using video-recorded consultations for research in primary care: advantages
and limitations. Fam Pract 2000; 17(5):422-427.
38 Borkan J.M. Mixed methods studies: a foundation for primary care research. Ann Fam
Med 2004; 2(1):4-6.
39 Frankel RM. From sentence to sequence: understanding the medical encounter through
micro-interactional analysis. Discourse Process 1984; 7:135-170.
How patients and FPs com municate about persistent MUS | 135
138
I C hapter 8
Summary
Background.
The feasibility as w ell as th e su itab ility of several th e ra p ies for m edically
u n ex p lain e d sy m p to m s (MUS) in p rim a ry care ap p lied by th e fam ily p h y sician (FP) a p p e a re d to
be low . FPs n ee d effective an d acceptable strateg ies to m an ag e th ese fu n ctio n ally im p aired
patients.
Objective.
To review im p o rta n t a n d effective elem ents in th e trea tm e n t of p atien ts w ith
MUS in p rim a ry care according to ex p erts in MUS research.
Methods.
W e p erfo rm ed a system atic search of n arrativ e rev iew s a n d scientific ed ito rials in
M edline an d PsycIN FO a n d tria n g u la te d o u r fin d in g s by co n d u ctin g a focus g ro u p w ith MUS
experts.
Results.
W e in c lu d ed 7 scientific ed ito rials a n d 23 n arrativ e review s. A ccording to MUS
experts th e m o st im p o rta n t elem ents in th e trea tm e n t of MUS are creatin g a safe th erap eu tic
e n v iro n m en t, generic in terv en tio n s (such as m o tiv atio n al in terv iew in g , giv in g tangible
explanations, reassu ran ce a n d reg u larly sc h ed u led ap p o in tm en ts) a n d specific in terv en tio n s
(such as cognitive ap p ro a ch es a n d p h arm aco th erap y ). F u rth erm o re, M US ex p erts in d icate th at
a m u lti-co m p o n en t ap p ro a ch in w h ich th ese th ree im p o rta n t elem ents are co m b in ed are m ost
h elp fu l for p atien ts w ith MUS. In co n trast to m o st specific in terv en tio n s, o p in io n s of MUS
experts re g a rd in g generic in terv en tio n s an d creatin g a safe th e ra p eu tic relatio n sh ip seem to be
m ore b ased o n theory an d experience th a n o n q u an tita tiv e research.
Conclusions.
MUS experts h ig h lig h t th e im p o rtan ce of generic in te rv en tio n s a n d doctor-
p a tie n t com m unication a n d relationsh ip . H o w ev er, stu d ies sh o w in g th e effectiveness of these
elem ents in th e m a n ag e m en t of MUS in p rim a ry care is still scarce. R esearch as w ell as m edical
p ractice sh o u ld focus m ore o n these non-specific aspects of th e m edical consultation.
Experts' opinions on the m anagem ent of MUS in prim ary care | 139
Introduction
M edically u n ex p lain e d sym p to m s (MUS) are som atic sy m p to m s th a t can n o t be attrib u te d to a
clear organic cause after a p p ro p ria te m edical assessm en t.1 MUS are a com m o n an d im p o rta n t
p ro b lem in p rim a ry care. In 19% - 50% of all sy m p to m s seen in p rim a ry h ea lth care, n o evidence
can be fo u n d for any physical disease (i.e. MUS).2-4M ost of th e tim e MUS are tran sien t a n d self
lim iting a n d do n o t n ee d fu rth e r m edical a tte n tio n after one or tw o consultation(s). A recent
D utch stu d y fo u n d th a t only 2.5% of th e atten d ees in g eneral practice p rese n tin g w ith MUS m eet
criteria for chronicity.5;6H ow ever, this m in o rity of p atien ts rep rese n t a m ajor p ro b lem in h ealth
care. These p atien ts suffer fro m their sy m p to m s, are fu n ctio n ally im p a ired an d are at risk of
unnecessary a n d p ossibly h arm fu l tests, referrals a n d trea tm e n t.4;7M oreover, scarce health care
resources are w a ste d w ith o u t clinical b enefit.2 This lead s to fru stra tio n for b o th d o cto r an d
patient.
T here is an often com plex o verlap b etw e en MUS a n d com m o n m en tal h ea lth p roblem s, b o th
lo n g itu d in ally an d cross-sectionally.8 For exam ple, som atic sy m p to m s are com m o n in m any
psychiatric conditions, su ch as anxiety or d ep ressiv e d iso rd ers, a n d of p rim a ry care p atien ts
w ith a diagnosable psychiatric d iso rd er, 50% - 70% initially p rese n t w ith som atic sy m p to m s.9;1°
Several trea tm e n ts for p atien ts w ith MUS h av e b een d escribed, w ith con sid erab le recent
research focused in p rim a ry care. Som e stu d ies show th a t a n tid ep ressan ts an d cognitive
b eh a v io u ral th e ra p y (CBT) are effective in th e tre a tm e n t of p ersistin g MUS, im p ro v in g
sy m p to m s a n d functional sta tu s a n d red u c in g psychological d istress.11;12R eattrib u tio n th erap y ,
a stru c tu re d in te rv en tio n to p ro v id e an ex p lan atio n of th e m ech an ism of p atien ts' sym p to m s
th ro u g h n eg o tiatio n a n d p atien t-c en tred co m m u n icatio n ,13is p ro b ab ly n o t effective as th ree of
fo u r trials do n o t show any benefit.14 M oreover, in one RCT re a ttrib u tio n train in g by FPs w as
associated w ith d ecreased qu ality of life.15 W hile fam ily ph y sician s (FPs) face a considerable
w o rk lo ad fro m p atien ts w ith MUS, th e ap p licab ility of CBT is lim ited becau se m an y p atien ts do
n o t accept CBT as th ey do n o t consider th eir co m p lain ts to be 'psychological'. T hereby a coherent
an d in teg rativ e m odel of disease m echanism s com bining p red isp o sin g , p recip itatin g an d
p e rp e tu a tin g factors is lacking.16
M oreover, the ap p licatio n of m ed icatio n is g enerally seen as less su itab le as it is a p assiv e fo rm of
trea tm e n t.17 In conclusion, th e evidence in th is field is th a t specific in te rv en tio n s for p atien ts
w ith MUS are at best of lim ited help for F Ps.
T herefore, to im p ro v e the care for p atien ts w ith MUS, it seem s v alu ab le to co n sid er ex p ert
opin io n s o n effective m a n ag e m en t strateg ies for p atien ts w ith MUS. Scientific ed ito rials an d
n arrativ e review s are a n im p o rta n t resource to le arn a b o u t th e o p in io n s of lead ers in th e field .18
140 I Chapter 8
W e d ecid ed to stu d y the elem ents ex p erts co n sid er im p o rta n t a n d effective in th e m an ag em en t
of MUS in p rim a ry ca re.
Methods
W e p erfo rm ed a system atic review w ith q u alitativ e analysis of ed ito rials an d n arrativ e review s.
Both types of p ap e rs are u su ally w ritte n by ex p erts in th e field. Scientific ed ito rials allow leaders
of research a n d clinical com m unities to com m u n icate w ith each o th er a n d are a fo ru m for the
expression of w id ely sh a re d ex p ert beliefs a n d opinions.18 N arra tiv e rev iew s tell u s w h a t is
k n o w n ab o u t th erap ies for p atien ts w ith MUS acco rd in g to ex p erts in th e field. The in fo rm atio n
o b tain ed fro m th e analysis of th e system atic rev iew w as tria n g u la te d by a focus g ro u p w ith
D utch experts in the field.
Data sources and search strategy
In O ctober 2009 w e p erfo rm ed a system atic search in M edline a n d PsycIN FO for n arrativ e
review s a n d scientific edito rials ab o u t MUS. W e u se d tw o search strin g s a n d com bined these
w ith th e Boolean o p era to r A N D . The first strin g consisted of term s in d icatin g so m atizatio n (for
exam ple: som atization, som atoform d iso rd ers, fu n ctio n al som atic sy n d ro m e, sym ptom ,
m edically unexplained). The second search strin g in c lu d ed term s for tre a tm e n t (for exam ple
th e ra p y , intervention). The search strateg y for M edline (see A p p en d ix 1) w as a d a p te d for
PsycIN FO . W e p re te ste d th e search strateg y o n five im p o rta n t articles th a t sh o u ld be in c lu d ed in
o u r stu d y . F urth erm o re, w e o b tain ed ad d itio n a l references fro m th e reference list of retriev ed
articles by system atically checking th e se .
A fter re a d in g several articles w e fo u n d th a t id eas a n d sta te m en ts p u b lish ed in articles in the
y ears before 2004 w ere rev iew ed a n d d iscu ssed in m o re recen t articles. T herefore, w e lim ited
o u r search strateg y to articles p u b lish ed in th e last 5 years.
Selection of studies
Tw o review ers (MH, physician w ith an in te rest in MUS; TCoH , FP w ith an in te rest in MUS)
in d e p en d e n tly rea d all titles an d abstracts for inclusion. The fu ll texts of th e in c lu d ed abstracts
w ere rea d by one review er (MH) w h o once ag ain checked for inclu sio n a n d exclusion criteria
before definitive inclusion. W h en in d o u b t she c o n su lted th e o th e r rev iew er (TCoH). Inclusion
criteria w ere n arrativ e review s or scientific ed ito rials fo cussing o n th e m a n ag em en t of p atien ts
w ith MUS. W e ex cluded p ap e rs th a t fo cu sed p rim arily o n diag n o sis or classification. A s w e
w ere in te reste d in im p o rta n t elem ents in th e m an ag em en t of u n d iffe ren tia te d MUS an d n o t in
th e m a n ag em en t of specific sy m p to m s or sy n d ro m es (for in stan ce m e lato n in for fib ro m y alg ia or
p robiotics for IBS), w e excluded articles a b o u t specific sy n d ro m es or single u n ex p lain ed
Experts' opinions on the m anagem ent of MUS in prim ary care | 141
sym ptom s. W e focused o n u n d iffe ren tia te d MUS as w e assu m e th a t these are m o re difficult to
h an d le for the physician th a n single sy m p to m u n ex p lain e d d iso rd ers a n d fu nctional
syndrom es: the latter give m ore o p p o rtu n ity for g u id elin e-b ased m a n ag em en t or a specific
referral to a m edical specialist w ith specific in te rest reg a rd in g fu n ctio n al sy n d ro m es. P ap ers on
ch ild ren a n d adolescents (age <18 years) an d p ap e rs o n specific g ro u p s of p atien ts (for exam ple
refugees, com m ercial sex w orkers) w ere ex clu d ed as w ell. W e calculated th e in ter-rev iew er
ag reem en t in article selection b ased o n title an d ab stracts w ith k a p p a statistics.19D isagreem ents
w ere resolved d u rin g a consensus m eeting.
Analysis
W e qualitativ ely an aly sed th e in c lu d ed scientific ed ito rials a n d n arrativ e rev iew s to explore
ex p ert o pinions a b o u t im p o rta n t elem ents in th e m a n ag em en t of MUS. A nalysis follow ed the
prin cip les of co n stan t co m parative analysis, in w h ich in c lu d ed stu d ies are su b seq u en tly
th em atically coded.20
T w o review ers (MH a n d TCoH) in d e p en d e n tly rea d tw o articles (one ed ito rial an d one
n arrativ e review ) to develop a coding schem e. Initial codes w ere discu ssed , seeking ag reem en t
o n th eir content. A fter th e tw o review ers ag re ed o n th e co d in g schem e, one rev iew er (MH)
cod ed one ed ito rial a n d one n arrativ e review . This initial co d in g w as checked by th e second
review er (TCoH). Since no significant d iscrepancies w ere d iscovered, th e first rev iew er (MH)
p ro ce ed ed to code the entire d ata set. In th e ev en t of d o u b t or am b ig u ity th e first rev iew er (MH)
so u g h t the o p in io n of th e second review er (TCoH). D u rin g su ch a consensus m eetin g th e coding
schem e w as rev iew ed a n d if necessary m odified. S u b seq u en tly th e tran sc rip ts w ere recoded
w ith th e m odified coding schem e. W e u se d A tlas.ti q u alitativ e d a ta analysis so ftw are for coding
a n d reco d in g th e transcripts. W e g ro u p ed th e codes into th em es to id en tify key featu res of
experts opinion. R ecurrent a n d im p o rta n t them es, id en tified by th e research ers, w ere
fre q u en tly discu ssed a n d refin ed as p a rt of an o n g o in g iterativ e process.21 D u rin g th e entire
analysis w e constantly m atch ed the d ev elo p in g th em es w ith th e tran scrip ts. T herefore, these
rep e ate d them es are g ro u n d e d in th e d a ta an n o t im p o sed o nto th e d a ta by th e rese arch e rs.
To tria n g u late th e resu lts of o u r q u alitativ e analysis w e co n d u cted a focus g ro u p m eeting. We
in v ited FPs w h o are p a rticip a tin g in th e g u id elin e com m ittee o n MUS in p rim a ry care of the
D utch College of G eneral P ractitioners. The p articip a n ts' characteristics are listed in Table 1. All
five have a specific in te rest in m a n ag in g p atien ts w ith MUS in p rim a ry care. M oreover, th ree
p articip a n ts d id their PhD in this field.22-24F ollow ing th e g u id elin es for co n d u c tin g focus g roups,
w e u se d an interview gu id e to direct th e d iscu ssio n an d to fulfill th e research aim s. This
interview gu id e w as b ased o n th e key th em es w e id en tified d u rin g th e analyses of th e articles
(Table 2). The d iscussion w as facilitated by a m o d e ra to r (MH) a n d lasted for ~1 h our. We
142
I C hapter 8
au d io ta p e d th e discussions in the focus g ro u p , tran scrib ed th e text an d en tered it into Atlas.ti.
N ext, w e an a ly se d w ith tw o review ers (M H a n d TCoH) th e text acco rd in g to th e p rin cip le of
co n stan t co m parative analysis a n d co m p ared th e resu lts w ith th e fin d in g s fro m th e system atic
review .
T a b le 1. C h aracteristics o f p a rtic ip a tin g FPs in th e fo cu s g ro u p d iscu ssio n
C h aracteristics
N u m b e r of fa m ily p h y sician s
G ender
- M ale
- Fem ale
4
W o rk in g h o u rs
- Full tim e
- P art tim e
5
1
0
T y p e o f p ractice
- Solo
- D uo
- G ro u p
3
A ge in y e ars (range)
51,4 (48-56)
Experience as a FP in y ears (range)
18,6 (10-25)
0
2
T a b le 2. Focus g ro u p in te rv ie w g u id e
O p e n in g
- W h at are im p o rtan t elem ents in the m an ag em en t of p atients w ith MUS?
- H o w d o y o u im p lem en t this in a consultation?
C re atin g a safe th e ra p e u tic
e n v iro n m e n t
- W h at are im p o rtan t elem ents in the m an ag em en t of p atients w ith M US th a t
create a safe environm ent?
- H o w d o y o u im p lem en t this in a consultation?
G en eric in te rv e n tio n s
- W h at are im p o rtan t elem ents in the m an ag em en t of p atients w ith M US th a t
b e lo n g to this them e?
- H o w d o y o u im p lem en t this in a consultation?
Specific in te rv e n tio n s
- W h at are im p o rtan t specific treatm ents for p atients w ith MUS?
- H o w d o y o u im p lem en t this in a consultation?
M u lti-c o m p o n e n t ap p ro ach
- W h at are im p o rtan t steps in the m an ag em en t of p atien ts w ith MUS?
- H o w d o y o u im p lem en t this in a consultation?
- W h en d o y o u take w h ic h step?
E nd
- W o u ld anyone like to a d d elem ents in the m an ag em en t of p atients w ith
M US w h ic h are n o t d iscussed today?
Experts' opinions on the m anagem ent of MUS in prim ary care | 143
Results
W e retrie v ed 960 articles fro m th e electronic d atab ases (572 M edline a n d 388 PsycIN FO ). A total
of 74 articles fo u n d w ith PsycIN FO h ad alread y b een fo u n d in th e M edline search (Fig. 1). A fter
screening the titles a n d abstracts, 53 p ap e rs fulfilled th e inclu sio n criteria. The in ter-rev iew er
a g reem en t w as
k
= 0.89 (95% confidence interval: 0.83-0.96). The fu ll text of 7 of th e 53 articles
w as n o t available in the N ijm egen lib rary a n d th e a u th o rs (living o u tsid e The N eth erlan d s) h ad
to be asked for a copy. As after 9 m o n th s no resp o n se cam e, th ese p a p e rs co u ld n o t be in c lu d ed in
th is stu d y . A fter re a d in g the full pub licatio n , w e in c lu d ed 30 of th e 46 articles in o u r analysis.
T hese articles concerned 23 n arrativ e rev iew s a n d 7 scientific ed ito rials.25-54
D u rin g th e analysis of th e in c lu d ed articles w e d istin g u ish e d fo u r key th em es d escribing the
im p o rta n t elem ents in the m a n ag e m en t of MUS in p rim a ry care acco rd in g to o p in io n lead ers in
th e field: (i) creating a safe th erap eu tic en v iro n m en t, (ii) generic in terv en tio n s, (iii) specific
in te rv en tio n s a n d (iv) m u lti-co m p o n en t ap p ro ach . These th em es w ill be d iscu ssed below .
Creating a safe therapeutic environment
A ccording to experts in th e field, a doctor has to actively create a safe th erap eu tic en v iro n m en t
before h e /s h e sta rts a therap y . In such a safe th e ra p eu tic e n v iro n m en t, th e p a tie n t sh o u ld have
th e o p p o rtu n ity to talk freely a b o u t th e sy m p to m s a n d p ro b lem s th a t b o th er h im /h e r. E xperts
state th a t a good d o cto r-p atien t relatio n sh ip a n d good co m m u n icatio n are n ecessary to create
such an environm ent.
D octor-patient relationship
In 17 of th e 30 in c lu d ed p ap e rs, th e im p o rtan ce of th e d o cto r-p atien t relatio n sh ip is stressed.
H ow ever, only one ex p ert referred to q u an tita tiv e ev idence fro m a ran d o m ized clinical trial
w h ich stu d ie d th e effectiveness of a p atien t-c en tred m e th o d to estab lish a good p atien t-p ro v id e r
relatio n sh ip .35
E xperts su g g est th a t a good d o cto r-p atien t relatio n sh ip is n ecessary for a tre a tm e n t to be
effective. A d octor can achieve this by b ein g em p ath ic, by sh o w in g th e p a tie n t th a t h e /s h e takes
th e p roblem s a n d sym p to m s seriously a n d th a t h e / she is w illin g to help th e patient.
Conversations in the primary care setting usually take place in the context o f long-standing,
trusting doctor-patient relationships. Such relationships have been shown to be an important
factor in the healing process.44
The doctor legitimized the patient's suffering, removed blame, and created a therapeutic alliance.
The symptom and emotion were thereby linked.43
144 I Chapter 8
Figure 1. Selection of studies
A good d o cto r-p atien t relatio n sh ip is n o t o nly im p o rta n t at th e sta rt of th e th erap y , acco rd in g to
experts, b u t also d u rin g the course of th e treatm en t. D octors s h o u ld fin d a w ay to deal w ith the
d o cto r-p atien t relatio n sh ip p roblem s w h ich th ey face in th e contact w ith th ese p a tie n ts.
D uring the course of treatment, a relationship o f mutual trust with the patient should be
maintained, but i f some problem occurs, it should be addressed directly w ith the patient in a
descriptive, yet non-judgmental manner.54
Experts' opinions on the m anagem ent of MUS in prim ary care | 145
D octor-patient communication
In 18 of th e 30 in c lu d ed n arrativ e rev iew s a n d ed ito rials ex p erts d iscu ssed th e d o cto r-p atien t
com m unication. H ow ever, no n e of th e MUS ex p erts describ ed q u an tita tiv e ev idence for the
effectiveness of the d o cto r-p atien t com m unication.
A ccording to experts, clear a n d focused co m m u n icatio n is an im p o rta n t elem en t in creatin g a
safe th e ra p eu tic environm ent. This m eans th a t a d octor sh o u ld listen carefully to his p a tie n t and
q u estio n the p atien t extensively ab o u t th e sy m p to m s, th e consequences of th e sy m p to m s for
daily life an d w h a t the sym p to m s m ean to th e p atien t. It is also im p o rta n t to ask th e p a tie n t ab o u t
h is /h e r cognitions, em otions, fears a n d concerns reg a rd in g th e sy m p to m s. The d o ctor has to try
to u n d e rsta n d th e p atien t's beliefs, sources of in fo rm atio n a n d k n o w led g e gaps.
Better communication has been associated with higher satisfaction in a number o f studies, as well
as greater adherence and lower rates o f litigation, but few studies have found a relationship
between communication and disease or symptom outcomes.35
Successful management o f patients with M U S has to address the subjective illness perceptions,
possibly underlying illness fears and information-processing biases. However, this requires not
only knowledge about the patient, but also behavioural skills in the doctor.32
MUS experts stressed th a t a clear a n d fo cu sed co m m u n icatio n b etw e en d o ctor an d p atien t can
enhance th e docto r-p atien t relatio n sh ip an d resu lts in a m ore p atien t-c en tred ex p lan atio n a n d
m a n ag em en t of th e sym ptom s. F u rth erm o re, w h e n th e influence of psychosocial facto rs has
b een elicited in an early stage of th e co n su ltatio n th e relevance of psychological facto rs becom es
m ore acceptable for th e patient.
To provide the patient w ith a qualifying explanation, it is necessary to thoroughly explore the
patient's illness beliefs and symptom worries. Identification o f the patient's dysfunctional beliefs
and behaviours lends the possibility o f helping the patient to modify them.27
Moreover, early recognition and communication o f the fact that symptoms may not result from
organic disease, and early appreciation o f the role o f psychosocial factors, may improve outcomes.34
In tw o p ap ers, experts m entioned, w ith o u t p ro v id in g q u an tita tiv e evidence, th a t giv in g a
su m m ary d u rin g MUS con su ltatio n s m ay be im p o rta n t.32;34 This su m m ary sh o u ld in clu d e
relev an t physical, psychological, social facto rs a n d possible links b etw e en them . A ccording to
th e MUS experts, giving a su m m ary is a w ay of sh o w in g th a t th e d o ctor is an a tten tiv e listener
a n d is in te reste d in th e p atien t's sym p to m s a n d problem s. F u rth erm o re, it h elp s th e d o ctor to
u ncover th e p atien t's o p in io n s an d ex pectations a n d w h e th e r or n o t th e p a tie n t agrees w ith the
trea tm e n t plan.
146 I Chapter 8
G eneric in te rve n tio n s
M otivationa l interviewing
In 13 of the 30 in c lu d ed p ap ers, MUS ex p erts m e n tio n m o tiv atio n al in te rv iew in g to stim u late
p atien ts' m o tiv atio n an d to enhance th e efficacy of specific in terv en tio n s. H o w ev er, th e experts
do n o t refer to q u an tita tiv e evidence for m o tiv atio n al in terv iew in g . A ccording to th e MUS
ex p e rts, d o cto rs sh o u ld , fo r ex am p le, e n c o u ra g e a p p ro p ria te ac tiv a tin g b e h a v io u r.
F urth erm o re, they h av e to give p atien ts p ractical a n d p o sitiv e ad vice for lifestyle changes,
w h ich they can ap p ly stra ig h t aw ay. E xam ples are reco m m en d atio n s for (graded) exercise,
dietary advice, sleep rou tin e, stress re d u c tio n a n d relaxation.
The essence of these recommendations is: to convey to the patient that his symptoms are real, to
offer positive advice and treatment and to engage the patient in an active role in alleviating the
often chronic symptoms.[...] The evidence o f non-pharmacological passive treatments, be they
invasive or non-invasive, seems to be weaker than the evidence o f non-pharmacological treatments
that involve active patients ' cooperation.33
Encourage patients to bring about change in lifestyle and diet, such as exercising, maintaining
regular hours and stopping use of alcohol, caffeine, nicotine and soforth.51
F urth erm o re, MUS experts stressed th e im p o rtan ce of in v o lv in g p atien t's allies (fam ily, friends,
etc.) in the m a n ag em en t of MUS in p rim a ry care. In th is w ay, p atien ts w o u ld be m o re m o tiv ated
to m ake im p o rta n t lifestyle changes.
Explanation
The im portance of ex p lan atio n of th e sy m p to m s in th e m a n ag e m en t of MUS is m e n tio n ed in 22
of th e 30 in c lu d ed p apers. In no n e of th e p ap e rs, MUS ex p erts referred to p ublications
q u an tita tiv e ly stu d y in g th e effectiveness of ex planations. A ccording to th e experts, a doctor
sh o u ld be able to give th e p a tie n t a tan g ib le ex p lan atio n for h is /h e r sy m p to m s, w h ich links the
physical com plaints w ith contextual factors a n d psychosocial influences. G iving th e p a tie n t a
positively fo rm u late d ex p lan atio n w ith p ractical advice for m a n ag em en t w o u ld enhance
trea tm e n t outcom e. T hey state th a t ex p lan atio n s sh o u ld be p erso n cen tred a n d a d ju ste d to the
p atien t's cognitions an d illness beliefs. H o w ev er, MUS experts do n o t give clear exam ples of
explaining th e sym p to m s to patients.
Explanations should integrate psychological and biological factors and provide patients and
doctors w ith a model for managing the condition.26
Experts' opinions on the m anagem ent of MUS in prim ary care | 147
Reassurance
In sixteen of th e 30 in c lu d ed p ap ers, th e im p o rtan ce of reassu ran ce is h ig h lig h ted . N o n e of the
MUS experts d escribed th e effect of reassu ran ce q u an titativ ely . In one n arrativ e review , an
ex p ert d escribed th a t the effect of diagnostic te stin g d ep e n d s o n w h a t p atien ts th in k a n o rm al
re su lt m eans.26
MUS ex perts su g g est th a t doctors sh o u ld explain, ed u cate, give advice a n d co m m unicate in
positive term s, in o rd er to reassu re the p atien t. S om etim es ad d itio n a l tests or referrals w ill be
necessary to rea ssu re the p atient. They su g g est th a t p rio r to th e d iagnostic tests, th e d octor h as to
explain w h a t a n o rm al test re su lt w ill m ean. M oreover, th e d octor sh o u ld ex p lain w h a t th e next
step w ill be if th e resu lts are n o rm al a n d th e sy m p to m s p ersist. F u rth erm o re, w h ile m ak in g the
choice for fu rth e r tests or referral, a doctor sh o u ld co nsider th e risk of iatrogenic h a rm cau sed by
th e ad d itio n a l in v estig atio n or referral, acco rd in g to th e MUS experts.
Discuss the planned examinations and their consequences with the patient as early as possible.
Anticipate when you will stop with medical investigations. Avoid unnecessary medical
investigations and petty diagnoses.34
Som e MUS ex perts m e n tio n th a t n o rm alizin g sy m p to m s an d test resu lts are likely to be m ore
beneficial.27;34
Regularly scheduled appointments
In 9 of the 30 in c lu d ed n arrativ e review s an d ed ito rials, MUS experts in d ic ated th a t reg u larly
sc h ed u led ap p o in tm e n ts sh o u ld have a place in the m a n ag em en t of p atien ts w ith MUS in
p rim a ry care. O ne ex p ert sta te d th a t evidence fro m ran d o m ized co n tro lled trials su g g ests th at
reg u larly sc h ed u led ap p o in tm en ts; p erfo rm in g a b rief ph y sical ex am in atio n at each visit, to
look for signs of disease ra th e r th a n rely in g o n sy m p to m s a n d av o id in g in v estig atio n s an d
h ospital adm issions, u nless clearly in d icated , decrease h ea lth service use a n d increase physical
functio n in g .26 H ow ever, the effect of co u n sellin g is n o t describ ed q u an titativ ely . A ccording to
MUS experts, these reg u larly sc h ed u led a p p o in tm e n ts en hance th e d o cto r-p atien t relationship.
A schedule o f regular, brieffollow-up office visits with the physician is an important aspect of
treatment. This maintains the therapeutic alliance with the physician, provides a climate of
openness and willingness to help, allows the patient an outlet for worry about illness and the
opportunity to be reassured repeatedly that the symptoms are not signs o f a physical disorder, and
allows the physician to confront problems or issues proactively. Scheduled visits may also prevent
frequent and unnecessary between-visit contacts and reduce excessive health care use.29
148 I Chapter 8
Specific interventions
In th e in c lu d ed publications, MUS ex p erts co m m en ted ab o u t th e specific treatm en ts: (i)
cognitive approaches, (ii) p h arm a co th e rap y , (iii) activ atin g th e ra p y a n d (iv) co m p lem en tary
an d altern ativ e m edicine.
Cognitive approaches
A lm ost all experts (in 28 of 30 in c lu d ed p ap ers) stress th e im p o rtan ce of cognitive ap p ro a ch es in
th e m a n ag em en t of MUS. O f these cognitive ap p ro ach es, th ey m o st o ften m e n tio n CBT.
A lth o u g h th ey h a d d ifferent o p in io n s a b o u t th e m a g n itu d e of th e effect of CBT, m an y experts
d escribed the evidence quantitativ ely . For exam ple, one ex p ert sta te d th a t th e resu lts of 31 CBT
con tro lled trials for trea tm e n t of so m ato fo rm d iso rd ers sh o w ed th a t w ith CBT, p atien ts
im p ro v e d m ore th a n controls in 71% of th e stu d ies.54A n o th er ex p ert sta te d th a t 82% of p atien ts
w ith MUS receiving CBT a n d 64% of co n tro l subjects h ad im p ro v e d or reco v ered at 6-m onth
follow -up a n d th a t this difference w as m a in ta in ed a t 12-m onth fo llo w -u p .43 H o w ev er, a th ird
ex p ert p o in te d o u t th a t the resu lts of th e effectiveness of CBT w ere no longer significant after
controlling for covariates.44 F u rtherm o re, H en n in g sen describ ed m o d e ra te evidence for the
effectiveness of CBT in p atien ts w ith MUS or so m ato fo rm d iso rd e r.33 In te rp re ta tio n of the
effectiveness of CBT seem s com plicated as m o st of th e tim e d ifferen t v aria n ts of CBT are stu d ied .
M oreover, it is n o t clear w h ich specific elem ents m ake th e CBT effective.
In CBT, the therapist structures the patient's social and physical environment to promote
appropriate behaviour (in this case, healthy social and personal adjustment without somatisation)
and discourage inappropriate behaviour (that is, illness behaviour and preoccupation with
physical symptoms).43
O ther cognitive th e ra p ies stu d ie d in th e literatu re are relax atio n train in g , rea ttrib u tio n ,
biofeedback, b o d y m e n talizatio n th e ra p y an d o th e r form s of p sy ch o th erap y . M ost ex p erts state
th a t their contents a n d resu lts are very h etero g en eo u s, w h ich h am p ers d ra w in g conclusions
reg a rd in g th eir effectiveness.
Pharmacotherapy
In 23 of the 30 in c lu d ed p ap ers, MUS ex p erts d iscu ssed th e im p o rtan ce of p h arm a co th e rap y in
th e m a n ag e m en t of MUS. They su g g e sted th a t an tid ep ressan ts can be h elp fu l an d p ro v id ed
qu an tita tiv e evidence for its effectiveness. For exam ple, one ex p ert sta te d th a t a system atic
review of 94 RCTs w ith a total of 6595 p atien ts w ith MUS fo u n d th a t an tid ep ressan ts
significantly im p ro v e d sy m p to m s (nu m b er n e e d e d to tre a t fo u r).26H o w ev er, one ex p ert stated
th a t a literatu re search d id n o t reveal any p u b lish ed co n tro lled stu d ies ev a lu a tin g th e efficacy of
ph arm a co th e rap y for MUS (either th e fu ll or a b rid g e d so m atizatio n d iso rd er d iag n o sis).45
Experts' opinions on the m anagem ent of MUS in prim ary care | 149
A ccording to MUS experts, an tid ep ressan ts can red u ce sy m p to m s of o ften co-m orbid
d ep ressio n of anxiety d iso rd e rs. F u rth erm o re, th ey m ig h t also be h elp fu l in reliev in g sym ptom s,
like pain, in the absence of a co-m orbid p sychiatric disease. H o w ev er, th e d o cto r-p atien t
relatio n sh ip an d com m unication m ay also play a role in th e effectiveness of an tid ep ressan ts,
according to the experts.
A literature review including a qualitative comparison o f information on understanding and
treatment of medically unexplained somatic symptoms was carried out by Burton (2003). He
found that CBT and anti-depressant drug are both effective treatments, but their effects may be
greatest when the patient feels empowered by the doctor to tackle his or her problem.55
W e fo u n d som e com m ents on other p h arm a co th e rap eu tic ag en ts b ein g stu d ie d in th e literatu re,
in c lu d in g anxiolytics. H ow ever, acco rd in g to MUS experts, th e re is n o t m u c h ev idence for their
effectiveness in the m a n ag em en t of MUS.
A ctivatin g therapy
A lth o u g h in 11 in c lu d ed p ap e rs MUS ex p erts d escrib ed th e p ossibility of activ atin g th erap y ,
n o n e of th em describe q u an tita tiv e evidence for th e effectiveness of th is th erap y . A lot of
differen t activ atin g th e ra p ies like g rad e d exercise, p h y sio th erap y an d rev a lid atio n are
m e n tio n e d by the experts. The ex perts su g g est th a t these th e ra p ies can be beneficial in som e
fun ctio n al som atic sy n d ro m es w h e n co m b in ed w ith o th er th erap ies. A ccording to MUS experts,
patien ts sh o u ld agree w ith th e activity. F u rth erm o re, th e activ ity sh o u ld be p erso n cen tred a n d
rele v an t to th e in d iv id u a l situ atio n a n d be stru c tu re d so th a t it g rad u a lly increases. D octors also
n ee d to tell the p a tie n t th a t h e /s h e m ig h t feel te m p o rarily w o rse b u t th a t th e re w ill be benefits in
th e long term .
E xpressive th e ra p ies like creative th e ra p y or w ritin g disclosure are also m e n tio n ed b y MUS
experts. H ow ever, th ey state th a t these th erap ies, like exercise th erap ies, seem m ostly beneficial
in com bination w ith o th e r therapies.
Cognitive techniques, psycho-education and attention training are suggested to alter cognitiveperceptual factors, and should be combined w ith the modification o f illness behaviour and graded
activity.47
Complementary and alternative medicine
In fo u r p ap ers, MUS experts d iscu ssed th e ap p licatio n of co m p lem en tary or altern ativ e
m edicine in th e m a n ag e m en t of MUS. Q u an titativ e ev idence w as n o t m en tio n ed . O ne expert
arg u e d th a t St John's W ort sh o w ed excellent efficacy o n s ta n d a rd iz e d assessm en t in stru m en ts
150 I Chapter 8
an d o utcom e m easures.42Som e experts m e n tio n ed h y p n o th e ra p y for th e m a n ag e m en t of MUS.
H ow ever, the experts sta te d th a t it is n o t clear w h ich specific elem en t of th ese th e ra p ies is
effective.
A couple of interesting placebo controlled trials have recently been published reporting on the
efficacy of St John's wort in the treatment o f somatization disorder, undifferentiated somatoform
disorder and somatoform autonomic dysfunction ( Volz, Murck, Kasper & Moller, 2002; Muller,
Mannel, M urck & Rahlfs, 2004). A Set o f standardized assessment instrum ents and outcome
measures were used in both studies and the data showed excellent efficacy, tolerability and safety
of S t John ' s wort, independent of any existing depressive symptomatology.42
Multi-component approach
In m o st scientific edito rials a n d review s experts in d icate th a t m a n ag em en t of MUS sh o u ld
consist of a m u lti-co m p o n en t ap p ro a ch w h ereb y creatin g a safe th erap eu tic en v iro n m en t, an d
general an d specific in te rv en tio n s are com bined. MUS experts o ften m e n tio n e d th e s te p p e d care
m odel. In this m odel, severity a n d chronicity of th e sy m p to m s g u id e th e m anagem ent.
Suchfindings lead to recommendations for stepped care as a basis for routine care:28
Step 1: Reassurance, advice, and explanation in the medical clinic;
Step 2: Reassessment, more extended CBT-based discussion and encouragement o f self-help;
Step 3: Reassessment, sessions of CB Tor other specialist care.
Results of focus group of experts in the field
The ex perts in th e focus g ro u p d iscu ssio n w ere inclined to discuss th e im p o rtan ce of a safe
th erap eu tic en v iro n m en t (clear an d fo cu sed d o cto r-p atien t com m unication) an d generic
in terv en tio n s (reassurance an d explanations).
... most important is that people feel they have been taken seriously. Therefore attention and
providing the opportunity to discuss all questions and concerns. (FP5, female, 25 years FP
working experience)
F urth erm o re, p articip a n ts su g g e sted th e im p o rtan ce of a th o ro u g h ex p lo ratio n of p atients'
som atic sym ptom s, beliefs a n d concerns, a n d consequences of th ese sy m p to m s o n p atients'
daily activities, social en v iro n m en t a n d illness b eh a v io u r in o rd er to reach a b etter
u n d e rsta n d in g of th e patien ts' sym p to m s an d problem s.
A ll symptoms have certain dimensions and the physical dimension is ju st one o f them. However
each symptom results in emotions, cognitions and illness behavior. I think that all these
Experts' opinions on the m anagem ent of MUS in prim ary care | 151
dimensions are important to explore. To look at all these dimensions together with the patient.
Sometimes, most of the time, you will fin d a starting-point for an intervention in one o f these
dimensions. (FP4, female, 24 years FP working experience)
Som e p articip a n ts u sed a sy m p to m d iary d u rin g th e MUS co n su ltatio n s as a tool to explore the
cognitions a n d em otions of th e p atien t. In this sy m p to m d iary th e p a tie n t sh o u ld w rite the
m o m en t of occurrence of th e sym p to m s an d h is /h e r th o u g h ts, fears a n d actions at th a t m om ent.
I ask patients to write down their own thinking, especially the thoughts not directly related to
disease. (FP3, female, 10 years FP working experience)
The p articip a n ts also in d icated the im p o rtan ce of g iving th e p atien t a po sitiv e tangible
e x p lan atio n a n d practical advices. H o w ev er, th ey d id n o t give exam ples of su ch explanations
a n d advices. F u rth erm o re they stressed th e v alu e of d iscu ssin g psychosocial factors influencing
th e sym p to m s at an early stage in the m a n ag em en t of th ese patients.
You have to explain patients at an early stage that you will use a somatic as well as a psychosocial
pathway during the management o f their unexplained symptoms. (FP1, 15 years FP working
experience.)
The p articip a n ts m e n tio n e d CBT, re a ttrib u tio n a n d referrals to p sy ch iatrist, p sy ch o lo g ist or
p h y sio th erap ist as specific in terventio n s. T hey also stressed th e im p o rtan ce of a good w o rk in g
relatio n sh ip w ith these caregivers.
I try to teach the patient cognitive techniques, relaxation exercises, or I refer them to a
physiotherapist. (FP 2,18 years FP working experience)
The p articip a n ts ag re ed th a t the m a n ag e m en t of MUS sh o u ld consist of a m u lti-co m p o n en t and
step-w ise approach. The severity of th e sy m p to m s a n d p ro b lem s m akes th e FP d ecide w h a t the
n ext step in the m a n ag e m en t w ill be.
It is nonsense to think that there should be one managementfor M U S. It really depends on the type
of symptoms, the type of patients and all dimensions that influence these symptoms. (FP4, female,
24 years FP working experience)
W h en w e com pare the resu lts fro m o u r literatu re review w ith th e resu lts of th e focus gro u p
discussion, w e conclude th a t no a d d itio n a l th erap eu tic elem ents w ere fo u n d . H o w ev er, the
p articip a n ts of th e focus g ro u p discu ssio n explicitly em p h asized th e im p o rtan ce of a safe
152 I Chapter 8
th erap eu tic en v iro n m en t a n d generic in terv en tio n s. F u rth erm o re, p articip a n ts of th e focus
gro u p d iscussion in d icated th a t th e m a n ag em en t of p atien ts w ith MUS sh o u ld consist of a m u lti­
com p o n en t ap p ro a ch in w h ich creatin g a safe th erap eu tic en v iro n m en t, generic a n d specific
in terv en tio n s are com bined.
Discussion
Summary of main findings
A ccording to MUS ex perts in th e field, th e m o st im p o rta n t elem ents in th e m a n ag e m en t of MUS
in p rim a ry care are: (i) creating a safe th erap eu tic en v iro n m en t th ro u g h a g o o d d o cto r-p atien t
com m unication an d an effective d o cto r-p atien t relatio n sh ip , (ii) generic in terv en tio n s su c h as
m otivational interview ing, giving tangible ex p lan atio n s a n d reassu ran ce a n d (iii) specific
in terv en tio n s such as cognitive ap p ro ach es a n d p h arm aco th erap y . H o w ev er, in co n trast to m ost
specific interv en tio n s, experts rarely describe th e effects of generic in terv en tio n s, d o cto r-p atien t
com m u n icatio n a n d relatio n sh ip q u an tita tiv e ly in th eir scientific ed ito rials a n d n arrativ e
review s. MUS experts indicate th a t a m u lti-co m p o n en t ap p ro a ch in w h ich th ese th ree im p o rta n t
elem ents are com bined are m ost help fu l for p atien ts w ith MUS.
Comparison with the literature
MUS experts stress the im po rtan ce of generic in terv en tio n s, clear a n d fo cu sed co m m unication,
prese rv in g th e d o cto r-p atien t relatio n sh ip a n d o th er non-specific aspects of th e co n su ltatio n
su ch as d escribed in th e p atien t-cen tred clinical m e th o d in o rd er to affect th e o utcom e of
consultations a n d to reach a th erap eu tic co n su ltatio n .56;57 H o w ev er, th ey do n o t describe the
effects of these in terv en tio n s quantitativ ely . A lth o u g h th e m a n ag e m en t of M US (especially in
seco n d ary care) as w ell as research in this area focus o n p la n n e d ap p ro ach es a n d specific
treatm en ts, w e assu m e th a t these non-specific aspects of th e co n su ltatio n elem ents, a lth o u g h
im p o rta n t for all m edical problem s, are specifically rele v an t for th e m a n ag e m en t of MUS
because of the pau city of effective interventions.
In recent years, several trea tm e n ts of p ersisten t u n ex p lain e d sy m p to m s h av e b een in tro d u c e d in
p rim a ry care such as CBT, re a ttrib u tio n th e ra p y , disclosure, g ro u p p sy c h o th erap y , psychiatric
consultation, etc.23;5S"61 H ow ever, th e ir effectiveness is q u estio n ab le a n d som etim e these
in terv en tio n s m ay be co u n terp ro d u c tiv e .62 E xperts' o p in io n s ab o u t th e im p o rtan ce of the
th erap eu tic enviro n m en t, th e d o cto r-p atien t relatio n sh ip a n d co m m u n icatio n an d the
im po rtan ce of generic interv en tio n s in d icate an im p o rta n t focus for p racticin g physicians to
m anage p atien ts w ith MUS. These factors fit w ell into th e d o m a in a n d th e p rin cip les of p rim ary
care.63 These elem ents sh o u ld be a p p lie d in ro u tin e daily practice, reg ard less of th e o rig in of the
Experts' opinions on the m anagem ent of MUS in prim ary care | 153
sym ptom s. The doctor as m edicine, as B alint sta te d y ears ago, m ig h t still b e th e m o st im p o rta n t
an d effective in te rv en tio n for p atien ts w ith MUS.64
Recent stu d ies su g g est th a t doctors a n d p atien ts h av e v ery d ifferen t p ersp ectiv es on MUS a n d
doctors' com m unication skills.65 T hey su g g est a m ism atch b etw e en w h a t p atien ts w ith MUS
w a n t an d w h a t they actually receive fro m th eir FP. S alm on et al.66 sh o w ed th a t p atien ts w ith
u n ex p lain e d sym p to m s often p rese n t o p p o rtu n ities for FPs to ad d re ss psychological need s. FPs'
en gagem ent w ith these cues, how ev er, seem s lim ited. F u rth erm o re, som e FPs p ro v id e
reassurance w ith o u t a clear ex p lan atio n of th e sy m p to m , w h ile p atien ts w ish to h av e a
convincing, leg itim atin g an d em p o w e rin g ex p lan atio n .67-70 Finally, FPs g enerally sh o w ed less
em pathic responses to w ard s p atien ts w ith M U S .71;72 These fin d in g s
m ig h t ex p lain w h y an
effective a n d clear com m unication w ith p atien ts w ith MUS m ig h t n o t be as straig h t fo rw ard as it
seem s a n d w h y im p lem e n ta tio n of the resu lts of th is stu d y in d aily practice m ay be co m p lex .
A lth o u g h o u r stu d y revealed im p o rta n t elem ents in th e m a n ag em en t of MUS in p rim a ry care,
w e did n o t stu d y th e effectiveness of th ese elem ents. The effectiveness of th ese sep arate
elem ents is still n o t w ell know n. R esearch in th e fu tu re sh o u ld a d d re ss these issu es in o rd er to
im p ro v e th e care for all p atien ts in p rim a ry care, especially those w ith MUS.
Strengths and limitations of this study
This s tu d y gives a b ro a d o verview of im p o rta n t elem ents in th e trea tm e n t of MUS acco rd in g to
o p in io n leaders. O u r find in g s reg a rd in g th e specific in te rv en tio n s like cognitive ap p ro ach es
a n d p h arm a co th e rap y w ere expected o n b efo reh an d . H o w ev er, as th ese specific in terv en tio n s
do n o t help the FP m u ch in daily practice, o u r fin d in g s re g a rd in g th e m o re generic in terv en tio n s
are ev en m ore im p o rtan t. The fact th a t w e fo u n d lim ited references a n d q u an titativ e
descriptions of th e effect of creating a save th e ra p eu tic en v iro n m en t an d generic in terv en tio n s
reflects th e necessity to s tu d y th e effects of th ese non-specific aspects of th e m edical
consultation. A lth o u g h such stu d ies m ig h t face m eth o d o lo g ical p ro b lem s of m easu rin g the
effect of these elem ents o n patien ts' outcom e, th e re are a v iew good exam ples of th ese k in d of
stu d ies in p rim a ry care. T hom as73, for exam ple, sh o w ed th e im p o rtan ce of b ein g p o sitiv e d u rin g
consultations w ith p atien ts w ith MUS in p rim a ry care, w h erea s v a n O s et al.74 ex am in ed the
effect of d ep ressio n treatm en t, em p ath y a n d su p p o rt, a n d th eir in teractio n o n p a tie n t outcom es
for d ep ressio n in p rim a ry care.
By p erfo rm in g o u r search in only tw o d atab ases (PubM ed an d PsycIN FO ), w e m ig h t have
m issed som e im p o rta n t edito rials re g a rd in g th e m a n ag em en t of MUS. H o w ev er, m ost
im p o rta n t a n d h ig h qu ality p eer rev iew ed jo u rn als w ill b e p rese n ted in o u r search.
F u rtherm ore, w e p re te ste d o u r search strateg y o n im p o rta n t p u b licatio n s ab o u t MUS in o u r ow n
154 I Chapter 8
database a n d w e co u ld retrieve all of th em by search in g in P ubM ed an d PsycIN FO . O u r good
inter-observer ag reem en t for inclusio n a n d exclusion en h an ced th e q u ality of o u r literatu re
search. F urth erm o re, b y d ev elo p in g a co d in g schem e by tw o in d e p e n d e n t rev iew ers an d
checking th e coding process of tw o p ap ers, w e co n clu d ed th a t one rev iew er (MH) w as able to
code th e entire d a ta set. Finally, b y co n d u ctin g a focus g ro u p d iscu ssio n in a d d itio n to the
q u alitativ e analysis of the literatu re stu d y , w e w ere able to tria n g u late o u r fin d in g s w ith
opin io n s of ex perts in th e field.
O ne could arg u e th a t th e re is som e ov erlap b etw e en th e key th em es th a t w e co u ld d istin g u ish in
this stu d y . For exam ple, creating a safe th erap eu tic en v iro n m en t is in terco n n ected to m ost
generic in terventions. F urth erm o re, som e generic in terv en tio n s, su ch as m o tiv atio n al
interv iew in g , co u ld also be co n sid ered as a specific in terv en tio n . H o w ev er, after an in -d e p th
discu ssio n d u rin g th e iterativ e process of analysis w e d ecide to categorize th e d ifferen t elem ent
into one of th e key them es: creatin g a safe th e ra p eu tic en v iro n m en t, generic in terv en tio n s or
specific interventions.
A s w e o nly in c lu d ed scientific edito rials a n d n arrativ e review s, w e co u ld n o t check w h e th e r or
n o t the o pinions an d statem en ts m e n tio n ed in th e p ap e rs w ere in co ncordance w ith th e fin d in g s
of th e o riginal studies. For exam ple, som e experts sta te d th a t n o rm alizin g sy m p to m s is likely to
be beneficial w h ile recent literatu re su g g e sted th a t th is is co n tro v ersial.69 F u rth erm o re, MUS
experts d id n o t give clear exam ples of ho w to ex p lain th e sy m p to m s to p atien ts w h ile exam ples
of ex planations in p rim a ry care research do exist.69 H o w ev er, by co n d u c tin g a focus gro u p
d iscussion in ad d itio n to th e literatu re stu d y , w e w ere able to check if experts in th e field of MUS
ag re ed w ith the o p in io n s fo u n d in th e n arrativ e rev iew s a n d scientific editorials. O ne could
arg u e th a t b y only in c lu d in g n arrativ e rev iew s a n d scientific ed ito rials p u b lish e d in th e last 5
y ears an d n o t in c lu d in g o riginal research, im p o rta n t elem ents in th e m a n ag e m en t of MUS (such
as th e n arrativ e m edical approach) h av e b een m issed. H o w ev er, th e v alid ity of o u r fin d in g s w as
explored by checking o u r resu lts d u rin g a focus g ro u p d iscu ssio n w ith ex p erts in th e field. N o
n ew elem ents in the m a n ag e m en t of MUS a p p e a re d fro m th is discussion. F u rth erm o re, they
ju d g e d th e resu lts to be consistent w ith th eir p ercep tio n s an d experiences.73
Conclusions
The experts' opin io n s o n m a n ag em en t of MUS seem to b e m o re b ased o n th eo ry a n d experience,
th a n o n h ig h qu ality research. A lth o u g h o p in io n lead ers do n o t describe th e ev idence reg a rd in g
its effectiveness q u an titativ ely , they em p h asize th e im p o rtan ce of creatin g a safe th erap eu tic
en v iro n m en t a n d other generic in terv en tio n s. F u rth erm o re, in accordance w ith th e evidence
re g a rd in g th e effectiv en ess of specific in te rv e n tio n s
(i.e co g n itiv e ap p ro a c h e s an d
p h arm aco th erap y ), ex perts indicate specific in terv en tio n s as im p o rta n t elem en ts in the
Experts' opinions on the m anagem ent of MUS in prim ary care | 155
m a n ag em en t of p atien ts w ith MUS. C reatin g a safe th erap eu tic en v iro n m en t an d generic
in terv en tio n s su ch as m otivational in terv iew in g , ex p lan atio n , reassu ran ce a n d reg u larly
sc h ed u led ap p o in tm e n ts m ig h t be key to im p ro v in g th e m a n ag em en t of p atien ts w ith MUS in
p rim a ry care.
Acknowledgments
I w o u ld like to th a n k the FPs w h o p articip a ted in th e focus g ro u p d iscu ssio n for their
co n trib u tio n in this s tu d y .
156 I Chapter 8
Appendix 1. Search strategy
( s o m a to f o r m
d is o r d e r s [ m e s h ]
h y p o c h o n d ria sis[m e sh ]
O R s o m a tiz a ti o n [ t w ]
O R s o m a tis a tio n [ tw ]
OR
O R n e u ra sth e n ia [m e s h ] O R c o n v e rsio n d iso rd e r[m e s h ] OR
som atoform disorder*[tw ] OR h yp o ch o n d riasis[tw ] OR neurasthen*[tw ] OR conversion
disorder*[tw ] OR psychophysiologic disorders[M esh] OR p sychosom atic m edicine[M esh] OR
psychophysiological disorder*[tw ] OR psychosom at*[tw ] OR p sychosom atic m edicine[tw ] OR
fu n c tio n a l som atic sym pt*[tw ] O R fu n c tio n a l so m atic syn d ro m * [tw ] O R fu n ctio n al
syndrom *[tw ] OR u n ex p lain e d sym pt*[tw ] OR m edically u n ex p lain ed [tw ] OR u n ex p lain ed
m edical sym pt*[tw ] OR psychogen*[tw ] OR non-organ*[tw ] OR non-specific com plain*[tw ] OR
non-specific sym pt*[tw ]) A N D (("therapy"[Subheading] OR "therapy"[tw ] OR "treatm ent"[tw ]
OR "therapeutics"[M eS H Term s] O R "th erap eu tics"[tw ]) O R ("th erap eu tics"[tw ]) OR
("m anagem ent"[tw ]) OR "intervention"[tw ] OR in terv en tio n s[tw ] OR ("therapies"[tw ]) OR
("therapeutic"[tw ]) OR ("treatm ents"[tw ]))
E x p erts' o p in io n s o n th e m a n a g e m e n t o f M U S in p rim a ry care | 157
Reference List
1
v a n d er W eijden T, v a n V elsen M, D in an t GJ, v a n H asselt CM, G rol R. U n explained
com plaints in general practice: p revalence, p atien ts' expectations, a n d professionals'
te st-o rd e rin g behavior. M ed Decis M aking 2003; 23(3):226-231.
2
P eveler R, K ilkenny L, K inm onth AL. M edically u n ex p lain e d ph y sical sy m p to m s in
p rim a ry care: a co m parison of self-rep o rt screen in g q u estio n n aires an d clinical op in io n . J
P sychosom Res 1997; 42(3):245-252.
3
K aton WJ, W alker EA. M edically u n ex p lain e d sy m p to m s in p rim a ry care. J Clin
P sychiatry 1998; 59 S u p p l 20:15-21.
4
Barsky AJ, Borus JF. S om atizatio n a n d m ed icalizatio n in th e era of m a n ag e d care. JAMA
1995; 274(24):1931-1934.
5
olde H a rtm a n TC, H assink-F rank e L, D ow rick C, Fortes S, L am C, v a n d er H o rst H et al.
M edically u n ex p lain e d sy m p to m s in fam ily m edicine: d efin in g a research agenda.
P roceedings fro m W O N C A 2007. F am P ract 2008; 25(4):266-271.
6
V erhaak PF, M eijer SA, V isser AP, W olters G. P ersisten t p rese n tatio n of m edically
u n ex p lain e d sy m p to m s in general practice. Fam P ract 2006; 23(4):414-420.
7
Sm ith GR, Jr., M onson RA, Ray DC. P atien ts w ith m u ltip le u n ex p lain e d sym ptom s.
Their characteristics, functional health , a n d h ea lth care u tilization. A rch In tern M ed
1986; 146(1):69-72.
8
de W aal MW , A rn o ld IA, E ekhof JA, v a n H em ert AM. S o m atoform d iso rd ers in general
practice: prevalence, functional im p a irm en t a n d co m o rb id ity w ith anxiety an d
depressive d isorders. Br J P sychiatry 2004; 184:470-6.:470-476.
9
G o ld b erg D. D etection a n d assessm en t of em otional d iso rd ers in a p rim a ry care setting.
Int J M ent H lth 1979; 8:30-48.
10 K irm ayer LJ, R obbins JM. T hree fo rm s of so m atizatio n in p rim a ry care: p revalence, co­
occurrence, a n d sociodem ograph ic characteristics. J N erv M ent Dis 1991; 179(11):647655.
11 K roenke K. Efficacy of trea tm e n t for so m ato fo rm diso rd ers: a review of ran d o m ized
controlled trials. P sychosom M ed 2007; 69(9):881-888.
12 S u m ath ip ala A. W hat is th e evidence for th e efficacy of trea tm e n ts for som atoform
d isorders? A critical review of p rev io u s in te rv en tio n studies. P sychosom M ed 2007;
69(9):889-900.
13 Little P, E veritt H , W illiam son I, W arn er G, M oore M, G o u ld C et al. O b servational
stu d y of effect of p a tie n t cen tred n ess a n d po sitiv e ap p ro a ch o n outco m es of general
practice consultations. BMJ 2001; 323(7318):908-911.
14 M orriss R, G ask L, D ow rick C, D u n n G, P eters S, Ring A et al. R an d o m ized trial of
re a ttrib u tio n o n psychosocial talk b etw e en d o cto rs an d p atien ts w ith m edically
H
'• jl
’
•
158 I Chapter 8
u n ex p lain e d sym ptom s. P sychol M ed 2010; 40(2):325-333.
15 M orriss R, D ow rick C, S alm on P, P eters S, D u n n G, R ogers A et al. C luster ran d o m ised
co ntrolled trial of train in g practices in re a ttrib u tio n for m edically u n ex p lain ed
sym ptom s. Br J P sychiatry 2007; 191:536-42.:536-542.
16 v a n R avenzw aaij J, olde H a rtm a n TC, v a n R avesteijn HJ, E veleigh R, v a n Rijswijk E,
L ucassen PLBJ. E xplanatory m od els of m edically u n ex p lain e d sym ptom s: a q u alitativ e
analysis of the literature. M ental H ea lth F am M ed. In p ress 2011.
17 T rim bos In s titu u t/N e th e rla n d s In stitu te of M ental H ea lth a n d A ddiction.
[M ultidisciplinary g uideline m edically u n ex p lain e d sy m p to m s a n d som atoform
disorders]. H outen: L adenius C om m u n icatie BV; 2010.
18 M iller FA, A h ern C, S m ith CA, H arv ey EA. U n d ersta n d in g th e n ew h u m a n genetics: a
review of scientific editorials. Soc Sci M ed 2006; 62(10):2373-2385.
19 C ohen J. A coefficient of ag reem en t for n o m in al scales. E du catio n al a n d psychological
m e asu rem en t 1960; 20:37-46.
20 G laser BG, S trauss AL. The discovery of g ro u n d e d theory. Chigago: A ldine; 1967.
21 B ritten N. Q ualitative interv iew s in m edical research. BMJ 1995; 311(6999):251-253.
22 A rnold IA, Speckens AE, v a n H em e rt AM. M edically u n ex p lain e d ph y sical sy m p to m s
The feasibility of g ro u p co g n itiv e-b eh av io u ral th e ra p y in p rim a ry care. J P sychosom Res
2004; 57(6):517-520.
23 B lankenstein A H , v a n d er H o rst HE, Schilte AF, de V ries D, Z aat JO, A n d re KJ et al.
D evelopm ent an d feasibility of a m o d ified re a ttrib u tio n m o d el for so m atisin g p atients,
a p p lied b y their o w n general practitioners. P atien t E duc C ouns 2002; 47(3):229-235.
24 v a n d er H o rst HE. Irritable bow el sy n d ro m e in g eneral practice. H ow effective is p atien t
ed u c atio n a n d counselling? [ A m sterd am : Vrije U n iv ersiteit A m sterd am ; 1997.
25 S paans JA, V eselka L, L uyten P, B u h rin g ME. [Bodily aspects of m en talizatio n : a
th erap eu tic focus in the tre a tm e n t of p atien ts w ith severe m edically u n ex p lain ed
sym ptom s]. Tijdschr P sychiatr 2009; 51(4):239-248.
26 H atch er S, A rroll B. A ssessm ent a n d m a n ag em en t of m edically u n ex p lain e d sym ptom s.
BMJ 2008; 336(7653):1124-1128.
27 F ink P, R osendal M. R ecent dev elo p m en ts in th e u n d e rsta n d in g a n d m a n ag em en t of
fun ctio n al som atic sym p to m s in p rim a ry care. C u rr O p in P sy ch iatry 2008; 21(2):182-188.
28 M ayou R. A re trea tm e n ts for com m o n m en tal d iso rd ers also effective for fu n ctio n al
sy m p to m s an d d isorder? P sychosom M ed 2007; 69(9):876-880.
29 O yam a O, P altoo C, G reengold J. S om atoform d iso rd ers. A m F am P hysician 2007;
76(9):1333-1338.
30 D eary V, C halder T, S harpe M. The cognitive b eh a v io u ral m o d el of m edically
u n ex p lain ed sym ptom s: a th eoretical an d em pirical review . Clin Psychol Rev 2007;
27(7):781-797.
Experts' opinions on the m anagem ent of MUS in prim ary care | 159
31 B row n RJ. In tro d u c tio n to th e special issue o n m edically u n ex p lain e d sym ptom s:
b ac k g ro u n d a n d fu tu re directions. C lin P sychol Rev 2007; 27(7):769-780.
32 Rief W. A nalyzing th e p roblem s in m a n ag in g p atien ts w ith m edically u n ex p lain ed
sym ptom s. J G en In tern M ed 2007; 22(5):704-706.
33 H en n in g sen P, Z ipfel S, H erzo g W. M an ag em en t of fu n ctio n al som atic syndrom es.
L ancet 2007; 369(9565):946-955.
34 S tep h en so n DT, Price JR. M edically u n ex p lain e d ph y sical sy m p to m s in em ergency
m edicine. E m erg M ed J 2006; 23(8):595-600.
35 Jackson JL, K roenke K. M anagin g som atization: m edically u n ex p lain e d sh o u ld n o t m ean
m edically ignored. J G en In tern M ed 2006; 21(7):797-799.
36 Jackson JL, O 'M alley PG, K roenke K. A n tid e p re ssa n ts a n d cognitiv e-b eh av io ral th e ra p y
for sy m p to m syndrom es. CNS Spectr 2006; 11(3):212-222.
37 Stone J, C arson A, S harpe M. F unctional sy m p to m s in n eu rology: m an ag em en t. J N eu ro l
N e u ro su rg P sychiatry 2005; 76 S u p p l 1:i13-21.
38 R euber M, M itchell AJ, H o w lett SJ, C rim lisk HL, G ru n e w ald RA. F u nctional sy m p to m s
in n eurology: q u estio n s an d answ ers. J N eu ro l N e u ro su rg P sy ch iatry 2005; 76(3):307-314.
39 R osendal M, O lesen F, F ink P. M an ag em en t of m edically u n ex p lain e d sy m p to m s. BMJ
2005; 330(7481):4-5.
40 Beutel ME, M ichal M, S ubic-W rana C. P sych o an aly tically -o rien ted in p a tie n t
p sy c h o th erap y of som atoform diso rd ers. J A m A cad P sychoanal D y n P sy ch iatry 2008;
36(1):125-142.
41 H en n in g sen P, H erzo g W. Irritable b ow el sy n d ro m e an d so m ato fo rm d iso rd ers. J
P sychosom Res 2008; 64(6):625-629.
42 Janca A. R ethinking som atoform d iso rd ers. C u rr O p in P sychiatry 2005; 18(1):65-71.
43 M ai F. S om atization disorder: a p ractical review . C an J P sy ch iatry 2004; 49(10):652-662.
44 F ritzsche K, Larisch A, C ierpka M, W irsching M. Im p ro v in g th e biopsychosocial
com petence of G erm a n p rim a ry care p h y sician s in d ia g n o sin g an d trea tin g so m ato fo rm
disorders. Fam Syst H ea lth 2004; 22(3):352-364.
45 Fallon BA. P h arm ac o th era p y of so m ato fo rm d iso rd ers. J P sychosom Res 2004; 56(4):455460.
46 H o to p f M. P rev en tin g som atization. P sychol M ed 2004; 34(2):195-198.
47 N an k e A, Rief W. B iofeedback in so m ato fo rm d iso rd ers an d rela ted sy n d ro m es. C u rren t
O p in io n in P sychiatry 2004; 17(2):133-138.
48 Rief W, S harpe M. S om atoform d iso rd ers-n ew ap p ro ach es to classification,
co nceptualization, a n d treatm ent. J P sychosom Res 2004; 56(4):387-390.
49 Janca A, Isaac M, V en to u ras J. T o w ard s b etter u n d e rs ta n d in g a n d m a n ag e m en t of
som atoform disorders. Int Rev P sy ch iatry 2006; 18(1):5-12.
50 K roenke K, R osm alen JG. S ym ptom s, sy n d ro m es, a n d th e v alu e of psychiatric
160 I Chapter 8
diagnostics in p atien ts w h o have fu n ctio n al som atic d iso rd ers. M ed C lin N o rth A m
2006; 90(4):603-626.
51 C h a tu rv ed i SK, D esai G, S haligram D. S om atoform d iso rd ers, so m atizatio n an d
ab n o rm al illness b ehaviour. Int Rev P sy ch iatry 2006; 18(1):75-80.
52 Jorsh MS. S om atoform disorders: th e role of co n su ltatio n liaison psy ch iatry . In t Rev
P sychiatry 2006; 18(1):61-65.
53 W aller E, S cheidt CE. S om atoform d iso rd ers as d iso rd ers of affect regulation: a
dev e lo p m e n t perspective. Int Rev P sy ch iatry 2006; 18(1):13-24.
54 Tazaki M, L andlaw K. B ehavioural m ech an ism s a n d co g n itiv e-b eh av io u ral in terv en tio n s
of som atoform disorders. In t Rev P sychiatry 2006; 18(1):67-73.
55 Janca A, Isaac M. ICD-10 an d DSM-IV sy m p to m s of so m ato fo rm d iso rd ers in different
cultures. Keio J M ed 1997; 46(3):128-131.
56 S tew art MA, M cW hinney IR, Buck CW. The d o c to r/p a tie n t relatio n sh ip a n d its effect
u p o n outcom e. J R Coll G en P ract 1979; 29(199):77-81.
57 S tew art M. Reflections o n the d o cto r-p atien t relationship: fro m ev idence a n d experience.
Br J G en P ract 2005; 55(519):793-801.
58 Schilte AF, P ortegijs PJ, B lankenstein A H , v a n d er H o rst HE, L ato u r MB, v a n Eijk JT et
al. R andom ised con tro lled trial of d isclo su re of em o tio n ally im p o rta n t ev en ts in
som atisatio n in p rim a ry care. BMJ 2001; 323(7304):86.
59 R ynearson EK, M elson SJ. S h ort-term g ro u p p sy ch o th erap y . A successful ap p ro a ch to
fun ctio n al com plaints. P o stg rad M ed 1984; 76(7):141-150.
60 S m ith GR, Jr., R ost K, K ashner TM. A trial of th e effect of a sta n d a rd iz e d psychiatric
co n su ltatio n o n h ea lth outcom es an d costs in so m atizin g patien ts. A rch G en P sychiatry
1995; 52(3):238-243.
61 K roenke K, S w indle R. C ognitive-behavioral th e ra p y for so m atizatio n a n d sy m p to m
syndrom es: a critical review of co n tro lled clinical trials. P sy ch o th er Psychosom 2000;
69(4):205-215.
62 M orriss RK, G ask L, R onalds C, D ow n es-G rain g er E, T h o m p so n H, G o ld b erg D. Clinical
an d p a tie n t satisfaction outcom es of a n ew tre a tm e n t for so m atized m en tal d iso rd er
ta u g h t to general p ractitioners. Br J G en P ract 1999; 49(441):263-267.
63 M cW hinney IR. A textbook of Fam ily M edicine. N ew York; O xford: O xford U niversity
Press; 1989.
64 B alint M. The doctor, his p a tie n t a n d th e illness. E d in b u rg h : C hurchill L ivingstone; 2000.
65 K enny DA, V eldhuijzen W , W eijden TV, Leblanc A, L ockyer J, L egare F et al.
In terp erso n a l p erc ep tio n in th e context of d o cto r-p atien t relatio n sh ip s: A dy ad ic analysis
of d o cto r-p atien t com m unication. Soc Sci M ed 2010; 70(5):763-768.
66 S alm on P, D ow rick CF, Ring A, H u m p h ris GM. V oiced b u t u n h e a rd agendas: q u alitativ e
analysis of th e psychosocial cues th a t p atien ts w ith u n ex p lain e d sy m p to m s p rese n t to
Experts' opinions on the m anagem ent of MUS in prim ary care | 161
general p ractitioners. Br J G en P ract 2004; 54(500):171-176.
67 Ring A, D ow rick C, H u m p h ris G, S alm on P. Do p atien ts w ith u n ex p lain e d physical
sy m p to m s p ressu rise general practitio n ers for som atic treatm en t? A q u alita tiv e study.
BMJ 2004; 328(7447):1057.
68 E pstein RM, S hields CG, M e ld ru m SC, Fiscella K, C arroll J, C arney PA et al. Physicians'
responses to patien ts' m edically u n ex p lain e d sy m p to m s. Psychosom M ed 2006;
68(2):269-276.
69 D ow rick CF, Ring A, H u m p h ris GM , Salm on P. N o rm alisatio n of u n ex p lain ed
sy m p to m s by general practitioners: a fu n ctio n al typology. Br J G en P ract 2004;
54(500):165-170.
70 Coia P, M orley S. M edical reassu ran ce a n d p atien ts' responses. J P sychosom Res 1998;
45(5):377-386.
71 P eters S, S tanley I, Rose M, S alm on P. P atien ts w ith m edically u n ex p lain e d sym ptom s:
sources of patien ts' a u th o rity a n d im plications for d em an d s o n m edical care. Soc Sci
M ed 1998; 46(4-5):559-565.
72 S alm on P, Ring A, D ow rick CF, H u m p h ris GM. W h at do g eneral p ractice p atien ts w a n t
w h e n th ey p rese n t m edically u n ex p lain e d sy m p to m s, a n d w h y do th eir doctors feel
p ressu rized ? J P sychosom Res 2005; 59(4):255-260.
73 M ays N , P ope C. R igour a n d q u alitativ e research. BMJ 1995; 311(6997):109-112.
164 I Chapter 9
Abstract
Background.
Medically unexplained symptoms (MUS) are common in primary health care.
Both patients and doctors are burdened with the symptoms that negatively affect patients'
quality of life. General practitioners (GPs) often face difficulties when giving patients legitimate
and convincing explanations for their symptoms. This explanation is important for reassuring
patients and for maintaining a good doctor-patient communication and relationship.
Objective.
To provide an overview of explanatory models for MUS.
Study design.
We performed a systematic search of reviews in PsycINFO and PubMed
about explanatory models of MUS. We performed a qualitative analysis of the data according to
the principles of constant comparative analysis to identify specific explanatory models.
Results.
We distinguished nine specific explanatory models of MUS in the literature:
somatosensory amplification, sensitisation, sensitivity, immune system sensitisation,
endocrine dysregulation, signal filter model, illness behaviour model, autonomous nervous
system dysfunction and abnormal proprioception. The nine different explanatory models focus
on different domains, including somatic causes, perception, illness behaviour and
predisposition. We also found one meta-model, which incorporates these four domains: the
cognitive behavioural therapy model.
Conclusion.
Although GPs often face difficulties when providing explanations to patients
with MUS, there are multiple explanatory models in the scientific literature that may be of use in
daily medical practice.
Explanatory m odels of MUS: a qualitative analysis of the literature | 165
Introduction
Medically unexplained symptoms (MUS) have a high prevalence in health care. Physical
symptoms such as headache, backache, pain in muscles and joints and fatigue are common. In
the general population two-thirds of men and four-fifths of women report at least one of these
complaints in the previous two weeks.1In about 25-50% of symptoms seen in primary health
care, no evidence can be found for any physical disease .2'3In specialist care these percentages are
even higher, ranging from 30 to 70 %.4'5
MUS can become chronic. Patients with persistent MUS are at risk for extensive investigations
and referrals, therefore becoming a great burden on health care.6'7Doctors and patients are both
burdened by the phenomenon of symptoms without disease. Bodily symptoms with unknown
physical pathology have a great impact on patient functioning. Such patients suffer greatly from
the symptoms and their quality of life is negatively affected.8'9
Unexplained physical symptoms are often confusing for both doctor and patient.10'11 Many
general practitioners (GPs) feel powerless and irritated when patients repeatedly visit their
practice with these symptoms.12Patients often feel disbelieved and not taken seriously by their
doctor.13Although it is often suggested that GPs are pressured by patients with MUS to deliver
somatic interventions, Ring et al pointed out that patients with MUS request somatic
interventions less often than physicians offer them.14Moreover, patients seek emotional support
and a legitimate and convincing explanation for their symptoms.15-17
GPs recognise the importance of explaining the diagnosis of MUS adequately to patients with
persistent MUS. However, they often face difficulties in explaining the nature of the symptoms
during the clinical encounter with these patients.18 Therefore, we searched and analysed the
literature for explanatory models for MUS. Providing an overview of such models can improve
the knowledge and communication of GPs, thus enhancing the quality of care for patients with
MUS.
Methods
Data sources and search strategy
We performed a qualitative analysis of systematic and narrative reviews on the topic of
medically unexplained symptoms using the databases PubMed and PsycINFO. We decided to
search for reviews, as in this type of article views of MUS and explanatory models are frequently
discussed. Our search strategy consisted of two search strings which we combined with the
166 I Chapter 9
Boolean operator AND. The first string contained keywords regarding MUS, combined with the
Boolean operator OR. The second string of our search strategy contained terms for explanatory
models, combined with OR (see Figure 1). This search string was limited to reviews, the English
and Dutch languages, articles published in the last five years, and age over18 years. We limited
our search strategy to articles published in the last five years as most articles about explanatory
models of MUS published before 2005 have been reviewed in more recent reviews.
We tested the accuracy of our search strategy by checking whether or not five key papers on
explanatory models in MUS were included in the results.
Figure 1. Search strategy
("2005/01/01"[Publication Date] : "3000"[Publication Date]) AND (((((Model [tw] OR
models [tw] OR conceptual*[tw] OR concept [tw] OR concepts OR pathophysiolog*[tw]
OR physiopatholog*[tw] OR mechanism* [tw] OR causal* [tw] OR cause [tw] OR
explanat* [tw] OR etiology [tw] OR aetiology [tw] OR aitiology [tw] ) AND (somatoform
disorder[mesh] OR somatization[tw] OR somatisation[tw] OR hypochondriasis[mesh]
OR neurasthenia[mesh] OR conversion disorder[mesh] OR somatoform disorder*[tw]
OR hypochondriasis[tw] OR neurasthen*[tw] OR conversion disorder*[tw] OR
psychophysiological disorder[Mesh] OR psychosomatic medicine[Mesh] OR
psychophysiological disorder*[tw] OR psychosomat*[tw] OR psychosomatic
medicine[tw] OR functional somatic sympt*[tw] OR functional somatic syndrom*[tw]
OR functional syndrom*[tw] OR unexplained sympt*[tw] OR medically
unexplained[tw] OR unexplained medical sympt*[tw] OR psychogen*[tw] OR nonorgan*[tw] OR non-specific complain*[tw] OR non-specific sympt*[tw])))))
Study selection
Two researchers (JvR, ToH) independently performed inclusion and exclusion of articles,
studying title and abstract. In case of doubt they consulted the full paper. Disagreements on
inclusion were discussed in a consensus meeting. All disagreements were easily resolved. We
calculated inter-rater agreement for inclusion with kappa statistics.19
We excluded studies that focused primarily on patients suffering from single-symptom
unexplained disorder (tension headaches, dysmenorrhoea) and distinctive functional somatic
syndromes (irritable bowel syndrome, chronic fatigue syndrome) because we were interested in
explanatory models of undifferentiated MUS in the literature. We focused on undifferentiated
MUS as we assume that these are more difficult to explain than single symptom unexplained
disorders and distinctive functional syndromes.20 We also excluded studies that focused
primarily on patients with medical or psychiatric disease (except somatoform disorders).
Studies on children and adolescents (age less than 18 years) and studies on specific groups of
patients such as refugees, street prostitutes etc. were also excluded.
Explanatory m odels of MUS: a qualitative analysis of the literature | 167
Data-analysis
We analysed the included reviews for explanatory models describing the cause of MUS. The
publications were fully entered into a computer database (Atlas.ti) suitable for qualitative
processing. The collection and analysis of data from the included reviews was performed both
parallel and cyclic, thus mutually influencing each other. First, two researchers (JvR and ToH)
independently read the articles in which many different models were assembled, to develop a
coding scheme of explanatory models. Initial coding was discussed to seek agreement on
content. The coding was improved, adjusted, explicated and specified by applying the constant
comparative method.21 One researcher (JvR) thematically coded the included articles in Atlas.ti
according to the final coding scheme.
Results
We retrieved 710 articles from the search in the electronic databases (480 PubMed and 230
PsycINFO). Sixty-five papers were duplicates. After two independent researchers screened title
and abstract, 24 papers fulfilled the inclusion criteria (Figure 2). The inter-rater agreement
(kappa) was 0.65 (95% CI: 0.51- 0.79), which was considered 'good'. Two articles were not
available in the Netherlands and were therefore excluded. After reading the full text, 19 out of 22
articles were included in our study.13,22-39 The three articles that were excluded reported on
therapy / diagnosis or somatic disease and one turned out to be a review of a book.
We could distinguish nine different explanatory models (somatosensory amplification,
sensitisation, sensitivity, immune system sensitisation, endocrine dysregulation, signal filter
model, illness behaviour model, autonomous nervous system dysfunction and abnormal
proprioception) and one meta-model (the cognitive behavioural therapy model) that contains
components of these nine different explanatory models. Each model is described, including
citations and comments from the reviews.
Explanatory models
A. Somatosensory amplification theory
The process described as somatosensory amplification suggests that a physical sensation arises
and that as a consequence, patients focus their attention on this sensation. They develop certain
cognitions and attributions which further amplify the perception of these physical signals. This
amplification results in a vicious circle in a way that symptoms are reinforced by patients'
thoughts and concerns. As a result patients with MUS experience a range of feelings as more
severe, more damaging, and more alarming.
168 I Chapter 9
' The strength of this model is its simple formulation, and it can even be used to explain the disorder
to patients. The basic mechanisms used in this model, such as attention, perception, and
attribution processes have some empirical validation, although the model neglects many other
well-validated factors, or offers only indirect explanations for them.' (p. 837)22
'Petrie and Weinman (2003) have called for more attention to be given to symptom appraisal and
we would widen this by calling for more attention to attention in general. The theoretical
literature and some of the empirical literature supports this mechanism as being an important part
of the cycle maintaining M U S.' (p. 791)23
'Amplification has, in general, been found to be related to reporting o f somatic symptoms.
However, there are conflicting reports on whether this is an independent effect or whether this is
mediated by such factors as anxiety, depression and negative affect/neuroticism. Findings
suggest that somatosensory amplification can only partially account for somatization, and that
other mechanisms may also be important in this process. ' (p. 28)26
Figure 2. S electio n o f stu d ies
Com puterised searches:
PubMed: 480
PsycINFO: 230
Duplicates (already found w ith
MEDLINE; n = 65)
Screening title and abstract (n = 645)
by tw o independent reviewers
Excluded after reading title and
abtract (n = 621)
Retrieving the full publication
(n = 24)
Paper only available abroad (n = 2)
Full text and article by one researcher
(n = 22)
Excluded after reading the full
w ith a second researcher; n = 3)
Final inclusion and analysis (n = 19)
Explanatory m odels of MUS: a qualitative analysis of the literature | 169
B. Sensitisation theory
Sensitisation means having an enhanced somatic response to sensations as a result of former
experiences of these sensations. In patients with MUS, repeated experiences of pain and
symptoms can lead to memory traces at a neuronal level which increase sensitivity for future
stimulation. This could result in normal benign stimuli being perceived as pain. A patient's body
reacts stronger to stimuli when it has become more sensitive by earlier and repetitive
encounters. The process of sensitisation has, besides a neural and sensory part, also a
psychological component. In MUS in general, a larger memory complex may play a role.
Experiencing a single symptom would not only sensitise this sensation, but would also activate
a wider memory trace. This in turn, can result in the experience of other physical symptoms.
Therefore, sensitization may cause a wide range of symptoms. Furthermore, expectations also
play a role in further sensitisation.
'The development o f symptom memories can be associated w ith cerebral restructuring. This has
been shown for single pain symptoms, where already 24 hours o f pain perception can cause
neuronal reorganization (neural plasticity) that will facilitate and intensify further symptom
perceptions (Arnstein, 1997). For the phenomenon o f multiple physical complaints, a general
symptom memory matrix can be postulated. ' (p. 830)22
' The repeated perception of physical signals in combination w ith uncertainty about the origin of
the sensations can hinder the habituation that would ordinarily be expected. ' (p. 1000)27
C. Sensitivity theory
This theory suggests that some individuals are more vulnerable to develop MUS. This
vulnerability can be based on personality traits, such as negative affect and neuroticism.
Furthermore, patients with MUS seem to have difficulty in experiencing the relationship
between bodily signals and emotions and thoughts. Catastrophic thinking may also play a part
in the vulnerability of pain in these patients. There is little evidence for genetic influences, but
many researchers suggest that early childhood experiences, such as abuse, insecure attachment
and parental influence, play an important role in the development of MUS.
' Viewing the M U S from the perspective o f underlying developmental influences that affect the
function of a variety of organs based on familial (genetic and environmental) predispositions
rather than from traditional viewpoint o f isolated organ-originated diseases has at least two
important implications. First, it provides a more parsimonious explanation for many findings
that have been quite difficult to account for. (...) Second, and more importantly, it invites
investigation of new areas of therapy that may otherwise escape consideration. ' (p. 142)28
170 I Chapter 9
'Studies w ithin the framework o f attachment theory have provided clear evidence that insecure
attachment patterns, and in particular an insecure dismissing attachment pattern, are associated
with an avoidant style of affect regulation. ' (p. 21)29
D. Immune system sensitization theory
The brain has a cytokine system that reacts to the immune system. It monitors danger in parts of
our body and coordinates the responses to these threats. The brain cytokine system is activated
by the immune system and mediates the subjective, behavioral and physiological components
of sickness, in a reversible way. It can be sensitised in response to activation during early stages
of development, repetitive stimulation or prior exposure to immunological stimuli. The brain
cytokine system, when sensitised, reacts very fast and is less likely to shut down after
eliminating the initial stimulus. Furthermore the brain cytokine system can be triggered by nonimmunological stimuli. In patients with MUS, a chronic immune activation with production of
cytokines can act as a motivation for the brain to change priorities in face of the presented threat
(such as stress or trauma) resulting in a feeling of being sick.
' The brain cytokine system also plays a key role in the experience o f pain that is associated with
danger, to the point that it has been proposed that pain is actually the main determinant o f sickness
behaviour rather than ju st a component o f it (Watkins and Mayer, 2000). ' (p. 951)30
'The main medical implication o f this view is that many somatization symptoms including
depressed mood, fatigue, and pain may represent the expression o f a previously sensitized brain
cytokine system that is reactivated by infectious or noninfectious trauma. ' (p. 853)31
'A growing body of evidence suggests that pathophysiological processes explain some o f the
aspects o f illness behaviour that are typically viewed as psychological in origin. The experience of
general malaise or feeling sick has a physiological basis, mediated by centrally acting
proinflammatory cytokines such as interleukin and tum our necrosis factor. ' (p. 56)32
E. Endocrine dysregulation theory
In the hypothalamus pituitary adrenal (HPA) axis, feedback loops exist to regulate the body's
response to acute and chronic stress. Dysregulation of this axis has been found in patients with
MUS. One interpretation is that prolonged activation has led to a 'burnout' response and a down
regulation of HPA activity in MUS. Another suggestion is that hypocortisolism may in fact be a
protective response of the body. Hypercortisolism has been found in patients with MUS. Early
traumata during pregnancy or childhood can have long lasting effects on the stress sensitivity of
the HPA axis which may be associated with increased prevalence of MUS.
Explanatory m odels of MUS: a qualitative analysis of the literature | 171
'The link so far found between central nervous system processes, such as the H PA axis, and
immunological processes are intriguing but far from conclusive; the causal relationships are
unclear, as are the nature o f the change in these systems in different conditions at different stages.
There is however already sufficient data to propose hypotheses about some o f the important links,
for example, between life events, H PA axis and immune functioning, that could be tested in
prospective studies.' (p. 791)23
'W e can conclude that the relevance o f the HPA-axis for the somatization syndrome is still
unclear. H PA-activity definitely plays a role; however, this role m ight be unspecific, course
depending, and multi-directional. ' (p. 998)27
F. Signalfilter theory
There is a permanent sensory stimulation from the body sending information to the brain. In
healthy individuals, however, this 'sensory noise' is filtered, in order to ensure that the brain is
not over-stimulated by information from physiological processes. In patients with MUS 'faulty
filtering' leads to the inability of these patients to differentiate between information from
physiological process (produced by the body) and information from pathophysiological
processes (produced externally). Patients with MUS experience both types of information.
Therefore, the number of physical sensations experienced by these patients is increased.
' The perception-filtering-model is in line with the findings on the relevance o f memory processes
and expectation, two empirically well-founded mechanisms not directly included in the other
models. Further strength of this model is the close relationship to the neuronal process o f
perception. Therefore they offer a link between psychological and psychobiological findings on
M U S.' (p. 837)22
' The effect of distraction on pain perception was demonstrated by Bantick et al., who found that
distraction leads to reduced activity in pain-associated centers (Bantick et al., 2002), again
supporting a signal-filter-model as presented. ' (p. 999)27
G. Illness behaviour theory
This theory hypothesises that patients' believes influence their behaviour. This behaviour can in
turn affect physiology and symptoms, resulting in a vicious circle and maintaining symptoms.
Avoidance of physical, social or mental activity can result in more symptoms. For example,
when a patient with chronic fatigue believes she will get more tired by doing sports, she will stop
all physical activity. This may result in an increase of bodily attention and physical
deconditioning, ending in more awareness and susceptibility of physical symptoms. Therefore
symptoms can be sustained because of patients' behaviour.
172 I Chapter 9
' There is actually relatively little literature concerning illness responses, despite a clinically
prevalent belief that 'all or nothing coping' and avoidance behaviours are important in the onset
and perpetuation of syndromes such as CFS. More longitudinal work o f this nature is needed to
clarify the role ofbehaviour in the development o f M U S.' (p. 787)23
'Behavioral aspects are also important in operant conditioning o f illness behavior, confirmation o f
health attitudes, and the development o f physical deconditioning. While these aspects could be of
major importancefor this patient group, their role has been insufficiently investigated in scientific
trials.' (p. 836)22
'Cognitive, emotional and behavioural factors have the capacity to relieve symptoms and even
change the brain. ' (p. 994)33
H. Autonomic nervous system dysfunction theory
Autonomic nervous system (ANS) dysfunction is a potential mechanism connecting
psychosocial stress to MUS. In healthy controls, the change from attention tasks to rest periods is
associated with a substantial decrease in heart rate activity ('recovery response'). This reduction
of physiological activity after mentally distressing tasks is not present in patients with MUS. It is
hypothesised that this is a result of a parasympathetic nerve system dysfunction, resulting in a
long lasting increased heart rate and stress burden in these patients.
'To summarize the results on autonomic physiological activity, we can conclude that only few
studies have addressed this question sofar. O nly small differences have been found, although there
is some consistency indicating the involvement o f the cardiovascular system. ' (p. 998)27
'W e conclude that current available evidence is not adequate to firm ly reject or accept a role of
A N S dysfunction in functional somatic disorders and it would therefore be misleading to provide
a definitive summary estimate.' (p. 108)34
I. Abnormal proprioception theory
Increased or abnormal proprioception can be a cause of physical symptoms in patients with
MUS. It is suggested that patients with MUS demonstrate more exact and sensitive perception of
their body than healthy individuals. In patients with MUS, minimal changes in muscle tension
would lead to an enhanced feeling of abnormality. Therefore, benign physiological sensations
(small changes in their body) can be interpreted as signs of a physical disease.
'I f patients with M U S perceive physical sensations more precisely, this could lead to increased
likelihoods of perceiving even minor physical symptoms, although these differences could also be
due to higher distraction by external stim uli in healthy controls. ' (p. 828)22
Explanatory m odels of MUS: a qualitative analysis of the literature | 173
J. Cognitive behavioural therapy model
This meta-model proposes that the cause of MUS is a self-perpetuating multi-factorial cycle,
with interaction of different factors in several domains. This model provides a framework to
incorporate patients' own personal perpetuating factors as well as predisposing and
precipitating factors. Each factor can result in physical symptoms an d /o r distress. Doctor and
patient together have to search for the patient's personal circumstances that might contribute to
the distress. Furthermore, this meta-model incorporates processes from at least five different
theories described above: sensitivity, sensitisation, somatosensory amplification, endocrine
dysregulation and illness behaviour model.
'This is the explicit purpose of the CBT assessment: to form a coherent multi-factorial case
conceptualization thatform s the rationale for treatment. ' (p. 789)23
' The biopsychosocial perspective becomes increasingly sophisticated, thus allowing the formation
of a tight chain of findings from psychology to specific disease processes playing a role in the
etiology and maintenance of illness conditions.' (p. 182)39
'As such the autopoietic explanation o f M U S as proposed by the CBT model both fits the current
data and could form a theoretically coherent basis for further research. More generally, the
research bears out the over-arching CBT hypothesis that the autopoietic interaction o f distinct but
linked systems could serve to produce physical symptoms in the absence o f physical pathology. '
(p. 789)23
Discussion
Summary of main findings
This review illustrates a considerable number of explanatory models of MUS, grounded in the
scientific literature. We could distinguish nine different explanatory models of MUS in the
literature: som atosensory am plification, sensitisation, sensitivity, im mune system
sensitisation, endocrine dysregulation, signal filter model, illness behaviour model,
autonomous nervous system dysfunction and abnormal proprioception. Furthermore, we
found one meta-model, the cognitive behavioural therapy model.
Some of the models aim at a physical explanation, such as the immune system sensitisation
theory, the endocrine dysregulation theory, the autonomic nervous system dysfunction theory
and the abnormal proprioception theory. Other models aim at a psychological explanation, such
as the somatosensory amplification theory and the sensitivity theory. And some models
174 I Chapter 9
combine a physical and psychological explanation, such as the sensitisation theory, the signal
filter theory and the illness behavior model.
The nine different explanatory models seek an explanation in different domains, including
somatic causes, perception, illness behaviour and predisposition. The meta-model integrates
these four domains.
Medical explanations in clinical practice
Current medical training focuses on acting (diagnosing and treating patients) instead of
listening, explaining and reflecting. Several studies pointed out that patients seek legitimacy for
their symptoms.16'40-42 They want to feel that the doctor accepts that the symptoms are real and
warrant the doctor's attention.25 Therefore, good and relevant doctor consultation skills,
including explaining symptoms, are needed. Plenty doctors think in terms of action and
reaction, while the explanation of symptoms in itself might be the most important intervention
for patients with MUS.43 Such explanations might prevent patients from extending or
elaborating symptoms and doctors from providing investigations or somatic treatment.3
Explanation as a consultation skill in its own right is rarely addressed in the literature and
teaching programs. As education on explaining and explanatory models is limited in today's
clinical education programs, medical students and GPs have little knowledge of theories and
models which they can use during consultation. This might explain part of the difficulties GPs
experience in giving an adequate and tangible explanation to patients with MUS. However, GPs
indicate that they build their own explanatory models of medically unexplained symptoms
based on their experience in daily practice.44Furthermore, building acceptable and effective (i.e.
reassuring) explanations together with the patient needs a mutual understanding of patients'
beliefs, concerns and expectations regarding their symptoms.45,46 Knowledge of explanatory
models of MUS, together with this mutual understanding and daily practice experiences can
facilitate the doctor-patient communication and strengthen the doctor-patient relationship with
these patients. Furthermore, mutual understanding between GP and individual patients on the
aetiology of MUS might result in greater reassurance, patient satisfaction and commitment to
the proposed interventions.25
Strengths and limitations of this study
In this qualitative analysis of the literature, we used an extensive and systematic search strategy
to identify relevant reviews. Including the full text papers and having them coded by two
independent researchers added rigour to our study. Moreover, we had good inter-rater
agreement for inclusion and exclusion.
Explanatory m odels of MUS: a qualitative analysis of the literature | 175
By using a cyclical way of analysing data, we were able to focus and explore explanatory models
in depth.47Entering the full text of included studies into Atlas.ti and using constant comparative
method to code and reorganise data strengthened our findings.
We limited our literature search to the past five years. It seems, however, that we have captured
most explanatory models in the literature as the reviews included in our study also discussed
and summarised explanatory models described in earlier literature. Although across cultures
many systems of medicine provide sociosomatic explanations linking problems in family and
community with bodily distress, we did not find culturally based explanatory models in our
literature search.48
A qualitative analysis of the literature is not as objective as a meta-analysis. However, we were
able to summarise the range of explanatory models grounded in the current scientific literature.
As studying the scientific evidence of the different models was not the goal of our study, we are
not able to draw conclusions on the degree of evidence of the explanatory models found in the
literature.
Implications for future practice and research
This review illustrates quite a number of different explanatory models of MUS described in
literature. Most theories are based on symptom perception, somatic causes, illness behaviour
and predisposition. On the other hand, more progress has to be made towards a fuller
understanding of the complex aetiology of MUS.
Further studies using in-depth interviews with GPs may reveal new explanatory models based
on experiences in daily medical practice. This qualitative analysis of the literature examines
explanatory models of MUS and not the usefulness of these models in clinical practice.
Therefore, new research has to clarify the usefulness of the different explanatory models in daily
practice. In addition, studies using a mixed method methodology have to point out patient
preferences and the effectiveness of the explanatory models individually in family practice.
As persistent MUS are present in all medical specialties, these explanatory models should be
integrated in the educational programs of all medical doctors in order to improve the quality of
care for patients with persistent MUS.
176 I Chapter 9
Reference List
1
Houtveen JH. De dokter kan niets vinden. Amsterdam: Uitgeverij Bert Bakker; 2009.
2
Peveler R, Kilkenny L, Kinmonth AL. Medically unexplained physical symptoms in
primary care: a comparison of self-report screening questionnaires and clinical opinion. J
Psychosom Res 1997; 42(3):245-252.
3
Ring A, Dowrick CF, Humphris GM, Davies J, Salmon P. The somatising effect of clinical
consultation: What patients and doctors say and do not say when patients present
medically unexplained physical symptoms. Soc Sci Med 2005; 61(7):1505-1515.
4
Nimnuan C, Hotopf M, Wessely S. Medically unexplained symptoms: an
epidemiological study in seven specialities. J Psychosom Res 2001; 51(1):361-367.
5
Reid S, Wessely S, Crayford T, Hotopf M. Medically unexplained symptoms in frequent
attenders of secondary health care: retrospective cohort study. BMJ 2001; 322(7289):767.
6
Kroenke K, Mangelsdorff AD. Common symptoms in ambulatory care: incidence,
7
Barsky AJ, Borus JF. Somatization and medicalization in the era of managed care. JAMA
evaluation, therapy, and outcome. Am J Med 1989; 86(3):262-266.
1995; 274(24):1931-1934.
8
Smith GR, Jr., Monson RA, Ray DC. Patients with multiple unexplained symptoms.
Their characteristics, functional health, and health care utilization. Arch Intern Med
1986; 146(1):69-72.
9
de Waal MW, Arnold IA, Eekhof JA, van Hemert AM. Somatoform disorders in general
practice: prevalence, functional impairment and comorbidity with anxiety and
depressive disorders. Br J Psychiatry 2004; 184:470-6.:470-476.
10 Banks J, Prior L. Doing things with illness. The micro politics of the CFS clinic. Soc Sci
Med 2001; 52(1):11-23.
11 Verhaak PF, Meijer SA, Visser AP, Wolters G. Persistent presentation of medically
unexplained symptoms in general practice. Fam Pract 2006; 23(4):414-420.
12 Mathers N, Jones N, Hannay D. Heartsink patients: a study of their general
practitioners. Br J Gen Pract 1995; 45(395):293-296.
13 Hatcher S, Arroll B. Assessment and management of medically unexplained symptoms.
BMJ 2008; 336(7653):1124-1128.
14 Barsky AJ, Ettner SL, Horsky J, Bates DW. Resource utilization of patients with
hypochondriacal health anxiety and somatization. Med Care 2001; 39(7):705-715.
15 Ring A, Dowrick C, Humphris G, Salmon P. Do patients with unexplained physical
symptoms pressurise general practitioners for somatic treatment? A qualitative study.
BMJ 2004; 328(7447):1057.
16 Peters S, Stanley I, Rose M, Salmon P. Patients with medically unexplained symptoms:
sources of patients' authority and implications for demands on medical care. Soc Sci
Med 1998; 46(4-5):559-565.
Explanatory m odels of MUS: a qualitative analysis of the literature | 177
17 Salmon P, Ring A , Dowrick CF, Humphris GM. What do general practice patients want
when they present medically unexplained symptoms, and why do their doctors feel
pressurized? J Psychosom Res 2005; 59(4):255-260.
18 olde Hartman TC, Hassink-Franke LJ, Lucassen PL, van Spaendonck KP, van Weel C.
Explanation and relations. How do general practitioners deal with patients with
persistent medically unexplained symptoms: a focus group study. BMC Fam Pract 2009;
10:68.
19 Cohen J. A coefficient of agreement for nominal scales. Educational and psychological
measurement 1960; 20:37-46.
20 olde Hartman TC, Borghuis MS, Lucassen PL, van de Laar FA, Speckens AE, van Weel
C. Medically unexplained symptoms, somatisation disorder and hypochondriasis:
course and prognosis. A systematic review. J Psychosom Res 2009; 66(5):363-377.
21 Glaser BG, Strauss AL. The discovery of grounded theory. Chigago: Aldine; 1967.
22 Rief W, Broadbent E. Explaining medically unexplained symptoms-models and
mechanisms. Clin Psychol Rev 2007; 27(7):821-841.
23 Deary V, Chalder T, Sharpe M. The cognitive behavioural model of medically
unexplained symptoms: a theoretical and empirical review. Clin Psychol Rev 2007;
27(7):781-797.
24 Henningsen P, Zipfel S, Herzog W. Management of functional somatic syndromes.
Lancet 2007; 369(9565):946-955.
25 Salmon P. Conflict, collusion or collaboration in consultations about medically
unexplained symptoms: the need for a curriculum of medical explanation. Patient Educ
Couns 2007; 67(3):246-254.
26 Duddu V, Isaac MK, Chaturvedi SK. Somatization, somatosensory amplification,
attribution styles and illness behaviour: a review. Int Rev Psychiatry 2006; 18(1):25-33.
27 Rief W, Barsky AJ. Psychobiological perspectives on somatoform disorders.
Psychoneuroendocrinology 2005; 30(10):996-1002.
28 Buffington CA. Developmental influences on medically unexplained symptoms.
Psychother Psychosom 2009; 78(3):139-144.
29 Waller E, Scheidt CE. Somatoform disorders as disorders of affect regulation: a
development perspective. Int Rev Psychiatry 2006; 18(1):13-24.
30 Dantzer R. Somatization: a psychoneuroimmune perspective.
Psychoneuroendocrinology 2005; 30(10):947-952.
31 Dimsdale JE, Dantzer R. A biological substrate for somatoform disorders: importance of
pathophysiology. Psychosom Med 2007; 69(9):850-854.
32 Kirmayer LJ, Looper KJ. Abnormal illness behaviour: physiological, psychological and
social dimensions of coping with distress. Curr Opin Psychiatry 2006; 19(1):54-60.
33 Wilhelmsen I. Biological sensitisation and psychological amplification: gateways to
178 I Chapter 9
subjective health complaints and somatoform disorders. Psychoneuroendocrinology
2005; 30(10):990-995.
34 Tak LM, Riese H, de Bock GH, Manoharan A, Kok IC, Rosmalen JG. As good as it gets?
A meta-analysis and systematic review of methodological quality of heart rate
variability studies in functional somatic disorders. Biol Psychol 2009; 82(2):101-110.
35 Spaans JA, Veselka L, Luyten P, Buhring ME. [Bodily aspects of mentalization: a
therapeutic focus in the treatment of patients with severe medically unexplained
symptoms]. Tijdschr Psychiatr 2009; 51(4):239-248.
36 Garcia-Campayo J, Fayed N, Serrano-Blanco A, Roca M. Brain dysfunction behind
functional symptoms: neuroimaging and somatoform, conversive, and dissociative
disorders. Curr Opin Psychiatry 2009; 22(2):224-231.
37 Maes M. Inflammatory and oxidative and nitrosative stress pathways underpinning
chronic fatigue, somatization and psychosomatic symptoms. Curr Opin Psychiatry 2009;
22(1):75-83.
38 Roelofs K, Spinhoven P. Trauma and medically unexplained symptoms towards an
integration of cognitive and neuro-biological accounts. Clin Psychol Rev 2007; 27(7):798820.
39 Nater UM, Gaab J, Rief W, Ehlert U. Recent trends in behavioral medicine. Curr Opin
Psychiatry 2006; 19(2):180-183.
40 Werner A, Malterud K. It is hard work behaving as a credible patient: encounters
between women with chronic pain and their doctors. Soc Sci Med 2003; 57(8):1409-1419.
41 Chew CA, May CR. The benefits of back pain. Fam Pract 1997; 14(6):461-465.
42 Nettleton S. 'I just want permission to be ill': towards a sociology of medically
unexplained symptoms. Social Science and Medicine 2005;62:1167-78.
43 Heijmans M. How to manage medically unexplained symptoms in primary care? A
qualitative analysis of reviews and scientific editorials. 2010.
Ref Type: Unpublished Work
44 van Ravenzwaaij J. Explaining medically unexplained symptoms. A qualitative
literature study supported by interviews with general practitioners. 2010.
Ref Type: Unpublished Work
45 Balint M. The doctor, his patient and the illness. Edinburgh: Churchill Livingstone; 2000.
46 Dowrick CF, Ring A, Humphris GM, Salmon P. Normalisation of unexplained
symptoms by general practitioners: a functional typology. Br J Gen Pract 2004;
54(500):165-170.
47 Britten N, Jones R, Murphy E, Stacy R. Qualitative research methods in general practice
and primary care. Fam Pract 1995; 12(1):104-114.
48 Kirmayer LJ, Groleau D, Looper KJ, Dao MD. Explaining medically unexplained
symptoms. Can J Psychiatry 2004; 49(10):663-672.
Explanatory m odels of MUS: a qualitative analysis of the literature | 179
182 I Chapter 10
Abstract
Background.
M edically u n ex p lain e d sy m p to m s (MUS) are freq u en tly p rese n ted in p rim a ry
care. U nfortunately, k n o w ledge of these p atien ts a n d / o r sy m p to m s in p rim a ry care is still
lim ited. A vailable research com es m ain ly fro m E u ro p e a n d N o rth A m erica, w h ile the
p erspectives of cu ltu res su c h as A frica, A sia a n d S o u th A m erica are relativ ely u n k n o w n . To
b rin g cultural p erspectives together, a sy m p o siu m a n d w o rk sh o p on MUS in p rim a ry care w as
h eld at the W O N C A W orld C onference 2007 in Singapore.
Objective.
M ain goals of this sy m p o siu m a n d w o rk sh o p - a p a rt fro m p rese n tin g o n g o in g
research a n d b rin g in g to g eth er experts in MUS - w ere to detect k n o w led g e g ap s in MUS a n d to
estab lish p rio rities in MUS research. This p u b licatio n focuses o n th e p ro p o sed research agenda.
Methods.
U sing a n o m in al g ro u p tech n iq u e w e g en erated research topics an d set priorities.
R esearch topics w ere g ro u p e d into research them es.
Results.
P articipants' (66 research ers an d G Ps fro m 29 n ationalities) m o st im p o rta n t
research topics w ere 'fo rm u latin g a b ro ad ly accepted d efin itio n of M US', 'fin d in g a strateg y to
recognize MUS b etter an d at a n earlier stage', 'stu d y in g th e v alu e of self-m an ag em en t and
e m p o w e rm en t in p atien ts w ith MUS' a n d 'fin d in g p red ic to rs to d ecide w h ich strateg y w ill best
help the in d iv id u a l p a tie n t w ith MUS'. P rio rities in research th em es of MUS are: (i) th erap eu tic
o p tio n s for p atien ts w ith MUS an d (ii) p ro b lem s in co n su ltatio n s w ith these patients.
Conclusions.
M ore research o n MUS in p rim a ry care is n e e d e d to im p ro v e th e co n su ltatio n s
w ith a n d m a n ag em en t of these p atien ts. In tern atio n ally p rim a ry care conferences are excellent
for exchanging ideas a n d fo rm u latin g cen tral issues of research.
MUS in fam ily medicine: defining a research agenda | 183
Introduction
A cute m edically u n ex p lain e d sy m p to m s (MUS) are com m on in fam ily m edicine. T w enty to fifty
p er cent of all contacts b etw een p a tie n t a n d G Ps concern u n ex p lain e d ph y sical sy m p to m s.1'2
M ostly, these sym p to m s resolve or do n o t n ee d fu rth e r m edical atten tio n after one consultation.
H ow ever, there is a gro u p of p atien ts w h o fre q u en tly co n su lt th e G P w ith u n ex p lain ed
sym ptom s. In a D utch su rv ey of G P -p atien t contacts, th e p rev alen ce of p atien ts w ith at least four
contacts p e r y ear for MUS w as 2,5 % .3F req u en t atten d e rs w ith MUS h av e a h ig h risk of extensive
investigations a n d referrals.4 O nly ab o u t a q u a rte r of p atien ts fre q u en tly p rese n tin g M US m et
th e criteria of one of the DSM-IV som ato fo rm categories (i.e. so m atisatio n or u n d ifferen tiated
som atoform disorder).5 This m eans th a t th e m ajority of p atien ts w ith MUS in p rim a ry care are
differen t fro m p atien ts m eetin g DSM-IV criteria for so m ato fo rm d iso rd er. C onsequently, this
rele v an t g ro u p of p atien ts in p rim a ry care d eserv e to b e s tu d ie d se p erate ly .6 H o w ev er, stu d y
an d hence k n o w led g e of m an y aspects of th is g ro u p of MUS p atien ts is scarce. For instance, w e
are still d eb atin g th e exact definition a n d classification of MUS w h ich is stro n g ly related to
cu ltu ral differences.7 Then, w e kn o w little ab o u t th e p ro g n o sis of th e sy m p to m s, a n d w e have
lim ited kn o w led g e a b o u t factors p red ic tin g th e p ro g n o sis or its course of MUS o ver tim e.
F urth erm o re, there is d o u b t ab o u t th e b est ap p ro a ch to a n d tre a tm e n t of th ese p a tie n ts.
In th e trad itio n al ap p ro a ch of p atien ts w h o rep e ate d ly p rese n t MUS, G Ps try to rea ssu re th em by
giving som e - b u t often in a d eq u a te - ex p lan atio n a b o u t th e sy m p to m s. F u rth erm o re, concerns
of p atien ts w ith MUS are less likely to be ex p lo red a n d facilitatio n of p atien ts' talk ab o u t
psychosocial p roblem s is lim ited.8-10 A s m an y p atien ts (and doctors) are n o t satisfied by this
trad itio n al ap p ro ach , in recent y ears som e research h as b een d one o n cognitive b eh av io u ral
th e ra p y (CBT)-based in terventions. These stu d ies sh o w conflicting results. M ost stu d ies show
no effect of CBT in terv en tio n s o n w ell-being, sick leave a n d lim itatio n s d u e to th e sy m p to m s.11-14
Several ex planations m ay be offered for these d isa p p o in tin g results: th e train in g of th e GPs
m ig h t have b een insufficient or im p o rta n t issu es su ch as th e an xiety of th e p atien ts m ig h t n o t
have b een ad eq u ately ad d re ssed . F urth erm o re, an a d e q u ate ex p lan atio n of th e sy m p to m s an d
non-specific effects caused by m u tu a l tru st, em p ath y a n d sh ared u n d e rs ta n d in g h av e n o t been
stu d ie d .15A lternatively, one m ig h t ask w h e th e r th e outcom es, su ch as n u m b e r a n d d u ra tio n of
sym ptom s, w ell-being, sick leave a n d lim itatio n s th a t d octors or research ers u su a lly stu d y , are
th e outcom es th a t p atien ts w o u ld also prefer. W e m u st conclude th a t th ere are still m any
un certain ties a b o u t this g ro u p of patients.
A lth o u g h MUS is a univ ersally com m o n p h en o m en o n , m o st research o n MUS com es from
E urope a n d N o rth A m erica. The persp ectiv es of o th e r cu ltu res su c h as A frica, th e A sia Pacific
a n d S o u th A m erica are relatively un k n o w n . It is k n o w n fro m recent research th a t th e re are
cu ltu ral differences in th e d istrib u tio n of MUS a n d th e m e an in g an d significance of a sy m p to m
n
184 I Chapter 10
d ep e n d s o n th e p erceived relatio n sh ip w ith diseases in a cu ltu re.7,16 M oreover, cu ltu ral an d
social n o rm s determ in e w h eth e r a p erso n w ith a p articu la r MUS can a d o p t th e sick role: cu ltu res
such as th e C hinese reject psychological sy m p to m s an d th erefo re cause p sy ch o so m atizatio n .17
B ringing these in te rn atio n a l p erspectiv es to g eth er m ig h t help to fill th e g ap s in k n o w led g e
ab o u t MUS.
W e therefore o rg an iz ed a sy m p o siu m a n d a w o rk sh o p ab o u t M US in p rim a ry care d u rin g the
W O N C A W orld C onference 2007 (Singapore, July 26). O u r aim w as to g ath er topics for research
o n MUS fro m discussions w ith research ers an d G Ps fro m all o ver th e w o rld a n d to prio ritize
these topics in o rd er to establish a global research agenda.
Methods
D u rin g th e sy m p o siu m 'MUS in fam ily m edicine: th e state of th e art', G P research ers p resen ted
o n g o in g research in MUS in different co u n tries all o ver th e w o rld . The tw o m ain th em es w ere
th e classification an d cu ltu ral v aria tio n of MUS a n d th e process of co n su ltatio n w ith MUS
p atien ts.18-20The sy m p o siu m w as also m e an t as an in tro d u c tio n to th e su b se q u en t w o rk sh o p . The
aim of th is w o rk sh o p 'MUS in fam ily m edicine: w h ere sh o u ld w e go?' w as to b rin g to g eth er GPs
w ith a b ro a d cu ltu ral variety in te reste d in MUS to discuss id eas ab o u t research to p ics in th e field
of MUS a n d to m ake choices o n w h ich id eas n ee d ed priority.
Participants in the workshop
In o rd er to discuss th e v ario u s p ersp ectiv es of MUS research a n d b rin g to g eth er G Ps from
d ifferent cu ltu ral b ack g ro u n d s to look at th e b ro ad e r p ic tu re of MUS, w e in v ited research ers and
in te reste d G Ps fro m d ifferent n ationalities. The n atio n ality of each p a rtic ip a n t in th e w o rk sh o p
w as reg istered by one of the org an izers (TC oH ).
Nom inal group technique
In th e w o rk sh o p , w e u se d the n o m in al g ro u p tech n iq u e to g en erate a research ag en d a. In the
n o m in al g ro u p technique, p articip a n ts are b ro u g h t to g eth er for discussion. The p ro ced u re
usu ally com prises fo u r stages: g en eratin g ideas, rec o rd in g of those ideas, clarification an d
prio rity votin g .21 This m e th o d enco u rag es co n trib u tio n s fro m ev ery o n e b y allo w in g equal
particip a tio n am o n g p articip an ts. M oreover, it is a stru c tu re d , tra n sp a re n t a n d replicable w ay of
sy n th esizin g a n d g en e ratin g ideas .22
D u rin g th e w o rk sh o p , w e g en erated id eas by stim u la tin g discussion: w e allo w ed 10 m in u tes of
b rain sto rm in g in sm all g ro u p s to discuss w h a t th ey th o u g h t to be th e m ost relev an t MUS
research topics. Each sm all g ro u p m ad e a sh o rtlist of th eir m ost im p o rta n t research topics. We
MUS in fam ily medicine: defining a research agenda | 185
co n tin u ed w ith an in v en to ry of all relev an t topics a risin g fro m th ese discussions. W e w ro te the
topics onto flip charts. If necessary, th e d iscu ssio n lead ers (LJAH-F, EMvW-B) ask ed for
clarification. A fter th is in ventory, each p a rtic ip a n t w as ask ed to choose five topics w ith the
h ig h est p rio rity fro m this list a n d ra n k them . Finally, w e ask ed all the p articip a n ts to vote,
allocating th e h ig h est score (5) to the m o st im p o rta n t research topic, th e n 4 to th e n ex t m ost
im p o rta n t sta te m en t a n d so on, by stick in g co lo u red card s o n th e flip charts. The o rg an izers of
th e w o rk sh o p an d p rec ed in g sy m p o siu m circu lated th e ro o m d u rin g th is task, g iv in g assistance
w here needed.
The research topics w ith the h ig h est votes w ere p rese n ted to the au d ien ce a n d d iscu ssed briefly
to clarify possible research m ethodolo g ies su itab le to an sw er th e research question.
Data analysis
O ne of the researchers (TCoH) su m m ed th e votes for each research topic th a t w as b ro u g h t up.
A ccording to th e v o tin g scores, topics w ere ran k ed , p ro d u cin g a list of th e p articip a n ts' 'priority
research topics'. Identical scores w ere g iven th e sam e ran k in g n u m b er; research topics w ith
h ig h er n u m b e r of in d iv id u al v otes w ere listed h ig h er.23 Finally, research to p ics w ere g ro u p ed
into research them es.
Results
Baseline characteristics of workshop attendees
A to tal of 66 researchers a n d G Ps fro m 29 n atio n alities fro m 6 d ifferen t co n tin en ts a tte n d e d our
w o rk sh o p . (Table 1) F ourteen p articip a n ts (21%) o nly atte n d e d th e in tro d u c tio n of the
w o rkshop.
Most important topics in MUS research
The n o m in al g ro u p technique resu lted in a total of 29 research topics. In Table 2, the ra n k in g of
these research topics is show n.
A lm ost h alf (48%) of th e aud ien ce agreed th a t th e m ost im p o rta n t p ro b lem is th a t MUS are n ot
clearly defined. T here is n e e d for a n u n am b ig u o u s d efin itio n of MUS th a t can be ap p lied
globally. W ith o u t a clear definition, research outcom es an d th eir m e an in g rem a in m u d d le d and
un certain. A s research a b o u t a definitio n is n o t possible, d iscu ssio n a n d reach in g consensus is
th e best w ay to solve this. A com m on consensus b u ild in g m eth o d is th e D elphi tech n iq u e.24The
p u rp o se of this tech n iq u e is to obtain co n sen su s o n th e o p in io n s of 'experts' th ro u g h q u estio n
ro u n d s u sin g stru c tu re d q uestionnaires. The au d ien ce em p h asized th eir preference of w o rk in g
as soon as possible o n a d efinition of MUS.
186
I C hapter 10
W orkshop p articip a n ts chose as second m o st im p o rta n t research q u estio n 'w h a t is th e best
strateg y to recognize MUS in p rim a ry care?' P atien ts w ith MUS are fu n ctio n ally im p a ired a n d at
risk for u nnecessary diagnostic p ro ce d u re s a n d treatm en ts. R ecognition of p atien ts w ith a h igh
risk of p ersisten t MUS is therefore of p a ra m o u n t im p o rtan ce. H o w ev er, in th e absence of a clear
definition, stu d y in g this research q u estio n is difficult.
T hirdly, research a b o u t effective in te rv en tio n s in p atien ts w ith MUS, especially self­
m a n ag em en t a n d p a tie n t em p o w erm en t, sh o u ld h av e p rio rity acco rd in g to 40% of the
w o rk sh o p audience. W e sh o u ld take th e cu ltu ral b ac k g ro u n d a n d p atien t p ersp ectiv es into
Table 1. N ation ality o f participants in the w orksh op on M US
Asia
- Korea
- S ingapore
- India
- M alaysia
- C hina
- H o n g K ong
- Philippines
- M ongolia
- T aiw an
- T h ailan d
21
1
3
1
5
3
3
2
1
1
1
M iddle East
- D ubai
- Q atar
- Israel
- B ahrain
- S au d i A rabia
6
1
2
1
1
1
Australia
3
Africa
- S o u th A frica
- N igeria
7
2
5
Europe
- UK
- The N e th erlan d s
- Slovenia
- T urkye
- Italy
- Spain
- Ireland
- P o rtu g al
22
4
10
1
2
2
1
1
1
N orth America
- US
- C an ad a
4
2
2
South America
- Brazil
1
1
Total num ber o f attendees
66
Total num ber o f participants
52a
a F o u rteen p a rtic ip a n ts on ly a tte n d e d the in tro d u c to ry p re s e n ta tio n of the w o rk sh o p .
MUS in fam ily medicine: defining a research agenda | 187
Table 2. R anking o f research topics in the fie ld o f M US
Rank
Research topic
Total
score
Total of
in d ivid u al
votes
1
W h at is th e d e fin itio n of MUS?
25
91
2
W h at is th e b est strateg y / tool to recognize M US in p rim ary care a n d w h e n d o I 18
h av e to sto p search in g for a ra re disease?
69
3
W h at is th e effect of self-m anagem ent a n d /o r p a tie n t e m p o w erm en t in p atients
w ith MUS?
21
58
4
H o w does the p a tie n t explain his sy m ptom s a n d w h a t d o patien ts d o w ith the
d iagnosis MUS?
14
44
5
W h at d o d octors in p rim ary care do w ro n g a n d rig h t in the consultations w ith
p atien ts w ith MUS?
13
44
6
W h at is th e aetiology of MUS?
11
40
7
W hich in terv en tio n s in p rim ary care are effective in p atien ts w ith MUS?
11
35
8
W h at is th e n a tu ra l course of M US in p rim ary care?
13
34
9
A re th ere cu ltu ral differences in d iag n o sin g MUS?
9
34
10
A t w h a t p o in t sh o u ld w e in terv en e to p re v e n t patients becom ing chronic
p resen ters of MUS?
13
32
11
W h at is th e effect of (the teaching of) com m unication skills of the doctor in
consultations w ith p atien ts w ith M US?
12
30
12
W h at is th e effect of a co m p reh en sive assessm ent of global aspects (spiritual,
psychosocial, contextual, fam ily view ) of p atien ts w ith MUS?
9
27
13
W h at a lte rn a tiv e /c o m p le m e n ta ry m edicine a p p ro a c h e s/in te rv e n tio n s are
effective in p atien ts w ith MUS?
9
23
14
W h at is th e v alue of the use of m etap h o rs b y p atients an d doctors in
consultations o n MUS
6
20
15
W h at m e th o d can w e use to m easu re m uscle ten sio n in rest?
9
16
16
W h at is th e influence of M US o n the Q OL of the p a tie n t an d the doctor?
5
14
17
Is th ere a re la tio n b e tw ee n M US p re v a le n c e /p re se n ta tio n a n d different h e alth
care system s (p ay m en t of care b y in surance or b y p atien ts them selves)?
6
13
18
W h at is th e efficacy of a step p ed -care m odel in the th e ra p y of p atients w ith
MUS?
4
12
19
W h at is th e influence of the role of the G P (gatekeeper - n on-gatekeeper) o n the
outcom e of MUS?
3
12
20
Is th ere a n e ed fo r a b e tte r categorisation of p atients w ith MUS?
5
10
21
W h at is th e effect of a co m m u n ity a n d /o r fam ily a p p ro a ch in therapies o n the
outcom e of MUS?
4
10
22
W h at a n d to w h a t e xtent sh o u ld G Ps explain to p atients ab o u t MUS?
4
9
23
W h at is th e re la tio n b e tw ee n M US a n d 'heartsink' patients?
4
8
24
W h at is th e difference b etw een M US an d hysteria?
2
8
25
H o w do p atien ts d ev elo p chronic MUS?
2
7
26
W h at is th e influence of the d im en sions of the b iopsychosocial m odel o n the
d e v elo p m en t of chronic MUS?
1
4
27
W h at is th e difference b etw een M US an d hyp o ch o n d ria?
1
3
28
W h at are the view s of p a tien ts on MUS?
1
2
29
A re p atien ts w ith M US satisfied w ith the consultation?
0
0
188
I C hapter 10
Table 3. Them es of research topics in the field of MUS
Research topic
Therapeutic options
- W h at is th e effect of s elf-m anagem ent a n d /o r p a tie n t e m p o w erm e n t in p atients w ith MUS?
- W hich in terv en tio n s in p rim ary care are effective in p atients w ith MUS?
- W h at is th e effect of (the teach in g of) co m m unication skills of the doctor in consultations
w ith p atien ts w ith MUS?
- W h at is th e effect of a co m p reh en siv e assessm ent of global aspects (spiritual, psychosocial,
contextual, fam ily view ) of p atien ts w ith MUS?
- W h at a lte rn a tiv e /c o m p le m e n ta ry m edicine a p p ro a c h e s/in te rv e n tio n s are effective in
p a tien ts w ith MUS?
- W h at is th e efficacy of a step p ed -care m o d el in the th e ra p y of p atients w ith MUS?
- W h at is th e effect of a co m m u n ity a n d /o r fam ily a p p ro a ch in therapies o n the outcom e of
MUS?
Problem s in consultations: The doctors' perspective
- W h at is th e b est strateg y / tool to recognize M US in p rim ary care a n d w h e n d o I h av e to
sto p search in g fo r a ra re disease?
- W h at d o d octors in p rim ary care d o w ro n g a n d rig h t in the consultations w ith p atien ts w ith
MUS?
- A t w h a t p o in t sh o u ld w e intervene to p re v e n t p atients becom ing chronic presenters of
MUS?
- W h at is th e v alu e of th e use of m etap h o rs b y p atien ts a n d doctors in consultations o n MUS?
- W h at a n d to w h a t extent s h o u ld G Ps e x plain to p atients ab o u t MUS?
D efin itio n
- W h at is th e d efin itio n of MUS?
- Is th ere a n e ed fo r a b e tte r categorisation of p atients w ith MUS?
- W h at is th e relatio n b e tw ee n M US an d 'heartsink' patients?
- W h at is th e difference b e tw ee n M US a n d hysteria?
- W h at is th e difference b e tw ee n M US a n d h y pochondria?
A etio lo g y and course
- W h at is th e etiology of M US?
- W h at is th e n a tu ra l course of M US in p rim ary care?
- W h at m e th o d can w e use to m easu re m uscle tension in rest?
- W h at is th e influence of M US o n th e Q OL of the p a tie n t an d the doctor?
- H o w d o p atien ts d evelop chronic MUS?
- W h at is th e influence of th e d im en sio n s of the b iopsychosocial m odel o n the d e v elo p m en t of
chronic MUS?
Cultural in flu en ces
- A re th ere c u ltu ra l differences in d iag n o sin g MUS?
- Is th ere a re la tio n b e tw ee n M US p re v a le n c e /p re se n ta tio n a n d different h e a lth care system s
(p ay m en t of care b y in su ran ce o r b y p atients them selves)?
- W h at is th e influence of th e role of th e G P (gatekeeper - non-gatekeeper) on the outcom e of
MUS?
Patient perspective
- H o w does the p a tie n t e xplain his sy m p tom s an d w h a t d o p a tients d o w ith the diagnosis
MUS?
- W h at are th e view s of p atien ts o n M US?
- A re p a tien ts w ith M US satisfied w ith the consultation?
Rank
Total
scorea
195
3
7
11
12
13
18
21
174
2
5
10
14
22
120
1
20
23
24
27
115
6
8
15
16
25
26
59
9
17
19
46
4
28
29
a S u m o f th e scores of each them e.
account. P robably, m ore th a n one in te rv en tio n is n e e d e d to help p atien ts w ith MUS. M ixed
m e th o d q u alitativ e research w ith doctors a n d p atien ts m ay b e th e key to dev elo p an effective
in te rv en tio n for these patients.
MUS in fam ily medicine: defining a research agenda | 189
Finally, w e discu ssed w h a t doctors in p rim a ry care m ig h t do w ro n g , a n d w h a t th ey do w ell, in
consultations w ith p atien ts w ith MUS. For instance, m edical in v estig atio n s can reassu re som e
p atien ts b u t can w o rsen sy m p to m s in o th er patien ts. It w o u ld be h elp fu l to s tu d y p red icto rs, in
o rd er to decide w h ich strateg y w ill help th e in d iv id u al p a tie n t w ith MUS m ost.
Themes in MUS research
In Table 3, w e g ro u p ed the research topic into six them es: (i) d efin itio n of MUS, (ii) aetiology and
p rognosis of MUS, (iii) p roblem s in the co n su ltatio n w ith p atien ts w ith MUS, (iv) th erap eu tic
op tio n s for p atien ts w ith MUS, (v) p a tie n t p ersp ectiv es a n d (vi) cu ltu ral differences. A s ap p ears
fro m this table, th e m o st im p o rta n t research th em es w o rth s tu d y in g w ere 'th erap eu tic o p tio n s
for p atien ts w ith MUS' a n d 'problem s in th e co n su ltatio n w ith p atien ts w ith MUS' (total score
195 a n d 174, respectively). R esearch ab o u t th e d efin itio n of MUS got a total score of 120 an d
research a b o u t aetiology a n d course 115. The research th em es 'cu ltu ral differences' a n d 'the
p a tie n t perspective' w ere re g a rd e d as less im p o rta n t (total score of 59 a n d 46, resp ectiv ely ).
Discussion
B ringing to g eth er experts of MUS research a n d d iscu ssin g th e state of th e a rt in MUS research
in te rn atio n ally w as of g reat value: w e co u ld sh are the global p ersp ectiv e on MUS a n d discuss
id eas a b o u t fu tu re dev elo p m en ts on MUS research. A lth o u g h cu ltu ral differences w ill play a
role in the classification of p atien ts w ith MUS, a n d doctors' p ersp ectiv es a n d m a n ag em en t of
p atien ts w ith MUS, w e d id n o t fin d m an y p ro m in e n t cu ltu ral differences d u rin g o u r
sy m p o siu m an d w o rk sh o p . D octors fro m all o ver th e w o rld face m o re or less th e sam e problem s
in consu ltatio n s w ith p atien ts w ith MUS. The h ig h atten d an ce rate an d the n u m b e r of
natio n alities in o u r sy m p o siu m a n d w o rk sh o p reflect th a t MUS are p rese n t all o ver the w o rld
a n d attract g reat atte n tio n of G Ps an d researchers.
The p ro b lem in MUS th a t w as recogn ized m o st w as th e in d istin ct a n d a m b ig u o u s d efin itio n of
MUS. T here is n ee d for an u n am b ig u o u s d efin itio n of MUS because w ith o u t a clear definition,
research outcom es a n d th eir m ean in g rem ain m u d d le d an d unclear. T his n ee d is ev en m ore
u rg e n t because in the n ext v ersions of ICD-11 a n d DSM-V th e en d of th e so m ato fo rm d iso rd er
category is bein g consid ered .25'26D ifficulties arisin g in d efin in g MUS are th e co nnection b etw een
MUS a n d p rev a len t m ental h ea lth d iso rd ers su ch as d ep ressio n a n d anxiety an d fu n ctio n al
som atic sy n d ro m es su ch as fibrom y alg ia a n d Irritable Bow el S y n d ro m e.27'28 Therefore,
in te g rate d research in p rim a ry care a n d specialized services is n eeded.
190 I Chapter 10
Important research themes worth studying appeared to be 'therapeutic options in patients with
MUS' and 'problems within the consultation with patients with MUS'. Recent research already
focus on these themes.20,29,30 There is need for more patient-oriented research, e.g. qualitative
research and mixed method research, to learn more about the needs of patients with MUS.31
Together with studying the course of MUS, this will provide GPs with instructions and advices
for the best therapeutic approaches towards these patients.12,13At best, the results of these studies
should be combined with the development and investigation of suitable and effective
interventions in these patients.
As far as we know, this is the first time that a research agenda in MUS has been defined by GPs
from all over the world. The participation of 29 nationalities from 6 different continents extends
the validity of the findings to cultures other than the Western culture. The strength of the
nominal group technique as a method for defining the research agenda is its structured, detailed
discussion. However, it may also lead to unrepresentative, unreliable judgements and
contextual differences, such as differences in national health care systems. Furthermore, the lack
of anonymity can make participants feel reserved to articulate their opinion.
We observed an interesting discrepancy: results of research as presented in the symposium
focussed on miscommunication between doctors and patients as reason for persisting MUS,
whereas in the workshop participants discussed MUS as if it were a real disease with its own
aetiology and course. Patients often want to discuss psychosocial problems but doctors do not
do so and choose a somatic pathway. This difference between patient's and doctor's perspective
is regarded as a cause of persistence of symptoms. Consequently, these symptoms have a
'course' and the workshop participants were particularly interested in that course. Only some
MUS patients turn out to have a "real" somatic or psychological disease during follow-up.
T urning all persistent unexplained symptoms into a disease is medicalising and not very helpful
for patients, because they actually want to be heard and discuss their psychosocial problems. If
doctors would facilitate this, more MUS might resolve.
Another interesting finding of our workshop was the fact that research on patient views was not
considered as priority. Knowledge of patients' expectations is necessary to answer patients
needs in consultations of MUS and enhances patients' satisfaction, adherence and health.32The
discussion on MUS as a real disease and the fact that only doctors participated in defining the
research agenda might explain the lack of priority of patient views. Moreover, it shows that
patient participation in defining a research agenda is needed in the future.
M US in fam ily m edicine: defining a research agenda | 191
It is clear from the literature, that more research on MUS in primary care is needed in order to
provide an improvement of the management of these patients and a better understanding of the
problems we face during consultations with patients with MUS. Moreover, it is important to
exchange ideas and coordinate research efforts on MUS in primary care at an international level,
in order to prevent redundancy. Future WONCA conferences, as well as other primary care
oriented conferences, offer excellent opportunities for this purpose.
192 I Chapter 10
Reference List
1
Peveler R, Kilkenny L, Kinmonth AL. Medically unexplained physical symptoms in
primary care: a comparison of self-report screening questionnaires and clinical opinion. J
Psychosom Res 1997; 42(3):245-252.
2
Burton C. Beyond somatisation: a review of the understanding and treatment of
3
Verhaak PF, Meijer SA, Visser AP, Wolters G. Persistent presentation of medically
medically unexplained physical symptoms (MUPS). Br J Gen Pract 2003; 53(488) :231-239.
unexplained symptoms in general practice. Fam Pract 2006; 23(4):414-420.
4
Smith GR, Jr., Monson RA, Ray DC. Patients with multiple unexplained symptoms.
Their characteristics, functional health, and health care utilization. Arch Intern Med
1986; 146(1):69-72.
5
Smith RC, Gardiner JC, Lyles JS, Sirbu C, Dwamena FC, Hodges A et al. Exploration of
DSM-IV criteria in primary care patients with medically unexplained symptoms.
Psychosom Med 2005; 67(1):123-129.
6
de Waal MW, Arnold IA, Eekhof JA, van Hemert AM. Somatoform disorders in general
practice: prevalence, functional impairment and comorbidity with anxiety and
depressive disorders. Br J Psychiatry 2004; 184:470-6.:470-476.
7
Escobar JI, Gureje O. Influence of cultural and social factors on the epidemiology of
idiopathic somatic complaints and syndromes. Psychosom Med 2007; 69(9):841-845.
8
Salmon P, Peters S, Stanley I. Patients' perceptions of medical explanations for
somatisation disorders: qualitative analysis. BMJ 1999; 318(7180):372-376.
9
Epstein RM, Shields CG, Meldrum SC, Fiscella K, Carroll J, Carney PA et al. Physicians'
responses to patients' medically unexplained symptoms. Psychosom Med 2006;
68(2):269-276.
10 Salmon P, Humphris GM, Ring A, Davies JC, Dowrick CF. Why do primary care
physicians propose medical care to patients with medically unexplained symptoms? A
new method of sequence analysis to test theories of patient pressure. Psychosom Med
2006; 68(4):570-577.
11 Arnold IA, Speckens AE, van Hemert AM. Medically unexplained physical symptoms
The feasibility of group cognitive-behavioural therapy in primary care. J Psychosom Res
2004; 57(6):517-520.
12 Morriss R, Dowrick C, Salmon P, Peters S, Dunn G, Rogers A et al. Cluster randomised
controlled trial of training practices in reattribution for medically unexplained
symptoms. Br J Psychiatry 2007; 191:536-42.
13 Rosendal M, Bro F, Sokolowski I, Fink P, Toft T, Olesen F. A randomised controlled trial
of brief training in assessment and treatment of somatisation: effects on GPs' attitudes.
Fam Pract 2005; 22(4):419-427.
M US in fam ily medicine: defining a research agenda | 193
14 Blankenstein AH, van der Horst HE, Schilte AF, de Vries D, Zaat JO, Andre KJ et al.
Development and feasibility of a modified reattribution model for somatising patients,
applied by their own general practitioners. Patient Educ Couns 2002; 47(3):229-235.
15 van Ravesteijn HJ, Lucassen PL, Hartman TC. Reattribution for medically unexplained
symptoms. Br J Psychiatry 2008; 192:314-5.
16 Karasz A, Dempsey K, Fallek R. Cultural differences in the experience of everyday
symptoms: a comparative study of South Asian and European American women. Cult
Med Psychiatry 2007; 31(4):473-497.
17 Kirmayer LJ, Sartorius N. Cultural models and somatic syndromes. Psychosom Med
2007; 69(9):832-840.
18 MUS of Chinese Patients Presenting to Primary Care. 18th WONCA World Conference
Singapore: 2007.
19 Ring A, Dowrick C, Humphris G, Salmon P. Do patients with unexplained physical
symptoms pressurise general practitioners for somatic treatment? A qualitative study.
BMJ 2004; 328(7447):1057.
20 Ring A, Dowrick CF, Humphris GM, Davies J, Salmon P. The somatising effect of clinical
consultation: What patients and doctors say and do not say when patients present
medically unexplained physical symptoms. Soc Sci Med 2005; 61(7):1505-1515.
21 Van de Ven AH, Delbecq AL. The nominal group as a research instrument for
exploratory health studies. Am J Public Health 1972; 62(3):337-342.
22 Raine R, Sanderson C, Hutchings A, Carter S, Larkin K, Black N. An experimental study
of determinants of group judgments in clinical guideline development. Lancet 2004;
364(9432) :429-437.
23 Tuffrey-Wijne I, Bernal J, Butler G, Hollins S, Curfs L. Using Nominal Group Technique
to investigate the views of people with intellectual disabilities on end-of-life care
provision. J Adv Nurs 2007; 58(1):80-89.
24 Green J, Britten N. Qualitative research and evidence based medicine. BMJ 1998;
316(7139):1230-1232.
25 Rief W, Rojas G. Stability of somatoform symptoms--implications for classification.
Psychosom Med 2007; 69(9):864-869.
26 Mayou R, Kirmayer LJ, Simon G, Kroenke K, Sharpe M. Somatoform disorders: time for
a new approach in DSM-V. Am J Psychiatry 2005; 162(5):847-855.
27 Lieb R, Meinlschmidt G, Araya R. Epidemiology of the association between somatoform
disorders and anxiety and depressive disorders: an update. Psychosom Med 2007;
69(9):860-863.
28 Wessely S, Nimnuan C, Sharpe M. Functional somatic syndromes: one or many? Lancet
1999; 354(9182):936-939.
n
194 I Chapter 10
29 Salmon P, Dowrick CF, Ring A, Humphris GM. Voiced but unheard agendas: qualitative
analysis of the psychosocial cues that patients with unexplained symptoms present to
general practitioners. Br J Gen Pract 2004; 54(500):171-176.
30 Salmon P, Ring A, Dowrick CF, Humphris GM. What do general practice patients want
when they present medically unexplained symptoms, and why do their doctors feel
pressurized? J Psychosom Res 2005; 59(4):255-260.
31 Borkan J.M. Mixed methods studies: a foundation for primary care research. Ann Fam
Med 2004; 2(1):4-6.
32 Stewart MA, McWhinney IR, Buck CW. The doctor/patient relationship and its effect
upon outcome. J R Coll Gen Pract 1979; 29(199) :77-81.
M US in fam ily m edicine: defining a research agenda | 195
I
198 I Chapter 11
The aim of this thesis was to explore the care GPs deliver and the care patients expect when
visiting the GP with persistent medically unexplained symptoms (MUS) in order to guide new
feasible and effective intervention strategies for these patients in primary care. In this final
chapter, the results of the previous chapters will be brought together for discussion and will be
related to existing literature. Subsequently, methodological considerations will be discussed.
Finally, implications and recommendations for intervention strategies, future research and
primary care development will be considered.
Summary of main findings
Analyzing the results of the studies of this thesis, we could distinguish three main themes:
course and prognosis of MUS, the mismatch in the doctor-patient communication, and the
importance of the doctor-patient relationship. Before we will outline and summarize these
themes, we have to notice that doctor-patient communication and doctor-patient relationship
are strongly interconnected as they highly influence each other. However, we assume that the
distinction between those two is worthwhile as doctor-patient communication focuses more on
interaction styles within a single consultation whereas doctor-patient relationship covers a
more longitudinal concept which is shaped throughout multiple consultations. For example,
the doctor-patient relationship is build over multiple consultations whereas the doctor-patient
communication is shaped in each single consultation.
Course and prognosis of MUS
In the first two studies (chapter 2 and 3) we examined the course and prognosis of MUS.
Simultaneously we searched for patient characteristics which can help GPs in daily practice to
identify patients who are at risk for persistent MUS.
By using the CMR registration project, we were able to determine patient characteristics during
the ten years before the diagnosis of chronic functional somatic symptoms (CFSS). The CMR
registration project has two unique features: (1) longitudinal registration which makes it
possible to follow the development towards persistent MUS and (2) a defined code for MUS and
persistent MUS (CMR classifies persistent MUS as chronic functional somatic symptoms
(CFSS)). Patients with CFSS appeared to consult their GP twice as much, to use much more
somatic and psychotropic medication, to have more psychiatric morbidity and to be more often
referred to mental health workers then patients without CFSS. Furthermore, they are more
likely to present symptoms in two or more body systems and to present a higher number and
greater diversity of symptoms to the GP then patients without CFSS.
To identify relevant prognostic factors in patients presenting persistent MUS we also performed
a systematic literature review on prognostic factors. The review showed that patients with MUS
General discussion | 199
and abridged somatisation (the abridged definition of somatisation which requires the presence
of four symptoms in males and six symptoms in females) had improvement rates of 50% or
more. However, 10-30% of patients with MUS symptoms deteriorated during the 6 to 15 months
follow-up period. Furthermore, the majority of patients with hypochondriasis did not recover
during follow-up. We found that the seriousness of the condition at baseline (i.e. number of
symptoms and severity of symptoms) might be of prognostic significance. We found no
evidence to support the influence of psychiatric comorbidity and personality traits on the course
of hypochondriasis.
Conclusion
The number, diversity and severity of symptoms are important characteristics in the course and
prognosis of MUS. Establishing the number of presented symptoms and the seriousness of the
condition in patients with MUS might help GPs to be aware of an increased risk of persistence of
MUS.
The mismatch in the doctor-patient communication
Analysis of video consultation of patients with persistent MUS (chapter 7) indicated that
patients present many symptoms in a rather unstructured way and GPs hardly used structuring
techniques such as agenda setting and summarizing. Furthermore patients with persistent MUS
got much opportunity to tell their story, but the reasons for encounter, their beliefs and concerns
were not discussed in a structured manner. The extensive explanation of the origin of the
symptoms given by the GP often did not take patients' beliefs and concerns into account. In the
interview study, patients indicate (chapter 4) that they appreciate a non-judgmental and
attentive listening style, a thorough exploration and a comprehensive explanation of this
symptoms. So, based on our qualitative analysis of the doctor-patient communication, we
conclude that there seems to be a mismatch between what patients with persistent MUS want
and what GPs deliver to them. This mismatch emerges most obvious in the domains:
'exploration' and 'explanation'.
Exploration
MUS experts (chapter 8) state that GPs should listen carefully to the patient and question them
extensively about the symptoms, the consequences of the symptoms for daily life and the
meaning of the symptoms for the patient. Furthermore they state that it is important to ask the
patient about his cognitions, emotions, fears, and concerns regarding the symptoms. So, this
concurs with what patients want as assessed in our interview study (chapter 4 ). Contrary to
these recommendations, GPs seldom explore patients' ideas, concerns and expectations in a
structured manner given their actual behaviour during the encounters with patients with
persistent MUS (chapter 7). We showed in a case report that recognizing and exploring cues
(non-explicit remarks) (chapter 6) can be a helpful tool for this exploration.
200 I Chapter 11
Explanation
GPs are aware of the importance of explaining the symptoms to the patient (chapter 5). This is in
line with the opinions of MUS experts (chapter 8), who stress the importance of providing
patients with a tangible explanation for h is/h er symptoms. However, GPs indicate that they
face difficulties to explain the nature of the presented unexplained symptoms (chapter 5). They
state that they use three different approaches to explain the symptoms to the patients;
normalization of symptoms, telling patients that there is no disease, and using metaphors. The
findings of chapter 9 offered a number of templates around which GPs could further develop
and specify their explanations. Some of these models aimed at a physical level of explanation,
such as the endocrine dysregulation theory. Other models aimed at a more psychological level
of explanation, such as the somatosensory amplification theory. And some models combined a
physical and psychological levels of explanation, such as the sensitization theory. Finally, one
model combined predisposing, precipitating and perpetuating factors such as somatic causes,
perception, and illness behaviour.
The relevance of more focused explanation came from chapter 7 in which we found that GPs'
extensive explanations of the origin of the symptoms often did not take patients' beliefs and
concerns into accounts. This might be a result of the limited exploration of these issues.
However, experts indicated the importance of linking the physical complaints with patients'
cognitions and illness beliefs. Therefore, understanding of patients' ideas, concerns and
expectations together with knowledge of the different explanatory models might help GPs to
improve their communication with patients with persistent M US.
The importance of the doctor-patient relationship
According to patients with persistent MUS (chapter 4), a good and effective doctor-patient
relationship depends on: (1) a GP with an open mind who uses a non-judgmental
communication style; (2) a skillful and competent GP who is supportive and who offers a
comprehensible explanation for the symptoms; (3) easy access to their 'own' GP who takes time
to explore and to discuss the patients' symptoms an d /or problems; (4) being taken seriously;
and (5) engagement as partners in the consultation in a way they can make their own choices
based on the provided information. This means that patients value a personal continuing GPpatient relationship built on physician attitude, medical competence, availability and shared
authority. These findings are in line with the opinions of GPs (chapter 5), who indicate the
usefulness and importance of a good doctor-patient relationship in encounters with patients
with persistent MUS. They are also in line with the opinions of MUS experts (chapter 8), who
state that the doctor-patient relationship is an important tool in order to create a safe therapeutic
environment for these patients. However, although patients, GPs and MUS experts recognize
the importance of the doctor-patient relationship, GPs indicate (chapter 5) that they face
difficulties in preserving the doctor-patient relationship during these encounters.
General discussion | 201
Although GPs realize the usefulness and importance of a good doctor-patient relation in
encounters with patients with persistent MUS, they face difficulties in putting this into practice.
This is in particular the case when explaining what is wrong or relieving of symptoms is
problematic. GPs try to overcome this by securing the relationship with some sort of ritual care
(e.g. regular physical examination, regular doctor visits). Some GPs do this wholeheartedly,
while others feel rather ambivalent with this ritual (chapter 5). Hereby, GPs carefully balance
between the maintenance of the doctor-patient relationship, their inability in explaining MUS,
and avoiding damage from drug therapy and interventions.
Comparison with the existing literature
Course and prognosis
The 'ecology of medical care' model explains that most people do not contact professional
medical care for most of their complaints.1Only a small minority of people contact a health care
professional when they feel ill.1'2 Twenty to thirty percent of the encounters of this small
minority concern symptoms that can not be explained by any physical disease.3-5However, most
of these episodes of illness remain restricted to one doctor-patient contact.6 Therefore we can
conclude that most of the symptoms are transient and disappear spontaneously in the course of
time or patients find a way to cope with their symptoms.7 This is in line with our findings. We
have found that the prognosis of MUS in primary and secondary care is more favourable than
expected, as the majority of the patients with MUS improve.
Creed and Barsky performed a systematic review of the epidemiology of somatisation disorder
and hypochondriasis to examine the characteristics and associated features of these disorders.8
Although they did not systematically search and study prognostic factors, they concluded that
the number of longitudinal studies providing data concerning natural history and predictors of
outcome is inadequate. Furthermore, they raised the hypothesis that abridged somatisation,
somatisation disorder and hypochondriasis are closely connected to anxiety and depressive
disorders.8 However, we could not confirm their hypothesis as in our review comorbid anxiety
and depression did not have prognostic value. Personality traits, including neuroticism and
alexithymia, have been demonstrated to be associated with MUS and hypochondriasis.9'10
However, our review did not find evidence for their prognostic value.
Our studies pointed out that the number, diversity and severity of symptoms are important
characteristics associated with the course of MUS. Patients with persistent MUS are more likely
to report higher number of symptoms, greater diversity of symptoms or more severe symptoms.
This is in line with the finding that patients with distinct functional somatic syndromes often
have symptoms overlapping with other functional somatic syndromes indicating a high
202 I Chapter 11
number and great diversity of symptoms in these patients.11Furthermore, patients with distinct
functional somatic syndromes often present symptoms in many body systems.12 Due to the
substantial overlap between the individual functional somatic syndromes the existence of
distinct specific somatic syndromes should be questioned. Taking the fundamental unity of
those syndromes into account, the GP, is the most appropriate practitioner to diagnose and treat
these patients as (1) they use a broad-based and generic approach; and (2) they try to prevent
iatrogenic harm of unnecessary interventions by using this approach.
In contrast to the limited numbers and considerable heterogeneity of studies focusing on the
prognosis of patients with undifferentiated MUS, distinct functional somatic syndromes are
studied more meticulously. Cairns and Hotopf for example, found 28 papers describing the
clinical follow-up of patients after the diagnosis chronic fatigue syndrome (CFS).13 The full
recovery rate in these patients was only 5% and only 40% of the patients improved. Lower
fatigue severity at baseline, a sense of control over symptoms, and not attributing illness to a
physical cause were associated with a good outcome. Their findings of the prognostic
significance of the fatigue severity at baseline are in line with our findings.
The mismatch in the doctor-patient communication
An important task for GPs is listening to patients,14,15 as patients seek understanding for their
symptoms16-19 and want to feel that the GP accepts the symptoms as real.20 To achieve this,
consultations skills, including exploration and explanation, are needed. However, we found
that exploration was only practiced to a limited extend by GPs when encountering patients with
persistent MUS. This is in line with the findings of others. According to Stewart et al. GPs do not
explore the reason for encounter and the worries of the patients in approximately half of the
consultations.21 Furthermore, in about 20% of all consultations the patient has an biomedical or
psychosocial agenda which is not addressed in the consultation.22An important tool to explore
patients' expectations and concerns is responding to patients' cues.23,24 Cues are non-explicit
remarks that can enclose a special meaning and point towards ideas, worries or expectations.
Discussing these cues enable better understanding of the reason for encounter, cognitions and
emotions.25,26 However, Salmon et al found that during the initial presentation of MUS, GPs'
engagement with explicit cues about emotional or social problems was limited.27This is in line
with our findings, as we found that GPs' exploration of patients' reason for encounter, beliefs
and concerns is also limited in persistent MUS consultations. Not exploring patients' beliefs and
expectations has several disadvantages. Firstly, patients might think that the GP is not listening
carefully, does not want to understand the meaning of the symptoms or is not interested in the
patient.28 Secondly, contrary to what is expected, these consultations will last significantly
longer. For example, Levinson found that in a majority of the consultations (79%), GPs missed
the opportunity to react to the cues given in the consultation resulting in a significant longer
General discussion | 203
duration of these consultations.29 Thirdly, not building a shared understanding regarding the
symptoms hampers effective explanation.20'30-32This might explain why GPs provide reassurance
without a clear explanation of the symptoms27; they simply lack information. For example,
normalization of symptoms and telling patients that they don't have a disease without
providing tangible mechanisms grounded in patients' concerns is not effective and results in
more demand for health-care.32 Finally, patient's satisfaction, adherence and health are
reduced.21,33'34 However, what we also have found in the video consultation study was that GPs
gave patients with persistent MUS ample opportunity to tell their story and this is exactly what
these patients want. In the interview study we found that patients want their GP to be mindfully
present, to listen to their story and to give them room to tell their story. Churchill described the
importance of taking time for the patients and demonstrating that there is space for their story.35
Furthermore, giving patients time for their story is one of the important elements of working in a
patient-centred way.36 However, we think that GPs' patient-centred working skills can further
be improved by a more focused communication, including enhancing GPs' exploratory
behaviour.
Prior research has indicated that doctor-patient communication is associated with patient
health outcomes.37-39Studies in cancer care revealed that words can be therapeutic because when
patients feel understood and reassured resulting in positive psychosocial health outcomes.40,41
Thomas showed the importance of being positive during consultations with patients with
MUS.42He studied patients receiving a positive consultation (firm diagnosis and confidence of a
good prognosis) or a non-positive consultation (no firm assurance and unsure about the
prognosis). Two weeks after the consultation, patients who received the positive consultation
were significantly more satisfied. Furthermore, 64% of those patients got better, compared with
39% of those who received a negative consultation. The role of patient- provider communication
was also studied in patients with osteoarthritis of the knee receiving traditional Chinese
acupuncture and sham acupuncture.43 Patient receiving a 'high expectations' communication
style (acupuncturist conveyed positive expectations of improvement about h is/h er treatment)
experienced statistically significant improvement in pain (effect size 0.25) and satisfaction
(effect size 0.22) compared with patients receiving a 'neutral expectations' communication style
(acupuncturist conveyed neutral expectations of improvement about h is/h er treatment). Cals
et al. evaluated the effect of doctor-patient communication on antibiotic prescribing for lower
respiratory tract infection and on patient recovery.44 They found that GPs who received a
training in enhanced communication skills prescribed significantly fewer antibiotics than those
not trained in these communication skills (27% vs 54%, P<0.01).
The three studies described above show that positive doctor-patient communication is essential
for the effectiveness of treatments in health problems in primary care. One of the proposed
204 I Chapter 11
pathways through which doctor-patient communication can contribute to improved health is a
shared understanding of illness.45 Although reaching a shared understanding in patients with
persistent MUS is often difficult15 and treatment for these patients are not easily available, a
positive doctor-patient communication is an important tool in the management of these
patients.
The importance of the doctor-patient relationship
GPs in our study recognized the importance of establishing an ongoing and effective doctorpatient relationship with patients with persistent MUS. Furthermore, they took responsibility to
build and maintain such a relationship. T aking this responsibility fits well in the values of family
medicine and general practice.30'46 Important indicators of the quality of the doctor-patient
relationship include mutual trust among GPs and patients, personal continuity, empathy,
compassion and the patient's perception of feeling respected and being cared for.45'47
It is known from the literature that the quality of the doctor-patient relationship affects health
outcomes by promoting patient's emotional well-being, enhancing continuity of care, patient
satisfaction, and patient commitment to treatment plans.48-50 Furthermore, in psychotherapy
outcome research therapist-client relationship factors have been estimated to contribute 30% of
patient outcomes.51Di Blasi et al. reviewed the empirical evidence of the therapeutic effect of the
doctor-patient relationship in medicine.52 They identified 25 trials studying the effects of the
patient-practitioner relationship on patients' health status. GPs who attempted to form a warm
and friendly relationship with their patients were found to be more effective than practitioners
who kept their consultations impersonal and formal.
Some studies have established the association between doctor-patient relationship and patient
health outcomes in mental health. Van Os et al. examined the effect of depression treatment,
empathy and support, and their interaction on patient outcomes for depression in primary.53
They found that only the combination of depression treatment according to the guidelines and
empathy and support resulted in an effective treatment of depression in primary care. Kaptchuk
et al. evaluated the effect of the doctor-patient relationship in patients with irritable bowel
syndrome (IBS).54 They found that augmented interaction (a warm, empathetic, and confident
patient-practitioner relationship) was more effective than limited interaction (patients
reporting adequate symptom relieve: respectively, 61% vs 53%). Smith et al. studied the effect of
explicitly establishing a good patient-provider relationship in high-utilizing patients with MUS
in primary care.55'56They found an absolute 14% improvement (48% improved vs 34% improved)
on the mental composite score of the SF-36 among those receiving the intervention, compared
with those who did not. Furthermore, depression and disability scores, as well as satisfaction
improved.
General discussion | 205
The three studies described above as well as the review of Di Blasi et al.52 show that the doctorpatient relationship is an important and potent therapeutic component which should not be
ignored. Furthermore, the role of the doctor-patient relationship should be explicitly addressed
in the treatment of (persistent) MUS in primary care. However, the doctor-patient relationship
should not be a primary goal of the consultation as, according to Chew-Graham, this may result
in GPs feelings of powerlessness to resolve the symptoms and problems presented and collusion
with patients' illness behaviour that maintain chronic incapacity.57Therefore, the doctor-patient
relationship should always be a means in stead of an arm to provide effective care.
Methodological considerations
The quantitative methods
To identify patient characteristics, course and prognosis of patients with persistent MUS we
performed (1) an observational study with a comparison control group using CMR longitudinal
data (chapter 2) and (2) a systematic review of the literature regarding prognostic factors in
patients presenting persistent MUS (chapter 3). Here we will describe the strengths and
limitations of the research methods we used in these two chapters.
Strengths
The CMR registration project is, as far as we are aware, the only morbidity registration system
with a structural possibility to classify patients with chronic functional somatic symptoms (i.e.
persistent MUS). The validity of morbidity registration is enhanced by monthly meetings of all
GPs involved to discuss classification problems, to monitor the application of diagnostic criteria
and to discuss coding problems of hypothetical case histories.58 Longitudinal research in the
field of MUS is mostly done by using questionnaires.59,60 However, questionnaires have been
shown to produce unreliable results due to recall bias. For example, the Psychological Problems
in General Health Care (PPGHC) study examined the stability of somatisation disorder and
somatisation symptoms and concluded that somatisation disorder showed considerable
instability during 12 months.61 In our review and our CMR registration study, MUS and
persistent MUS was diagnosed by the GPs or investigators themselves in patients experiencing a
certain threshold of relevance of symptoms as they seek medical care for them meaning that the
diagnosis of (persistent) MUS was not related to the recall of 'lifetime' symptoms.62
Our systematic review is the first which systematically searched for studies on prognostic
factors in patients with persistent MUS. We used an extensive search strategy to identify
relevant studies and we independently assessed the quality of included studies with a validated
checklist. Furthermore, we searched all relevant databases, in- and excluded studies with two
researchers independently and did not use language restrictions. Although the heterogeneity of
206 I Chapter 11
included studies was high, we were able to perform a best-evidence synthesis to summarize the
value of the different prognostic indicators taking methodological quality into account.
Limitations
In the CMR registration there might be an interdoctor variation in the diagnosis chronic
functional somatic symptoms as diagnosing these patients will always remain an interpretation
of the symptoms in which GPs will use their knowledge of the context of the specific
patients.21'58'63 One might argue that the higher frequency of GP visits, referrals and diagnostic
test was to be expected in advance, as the diagnosis chronic functional somatic symptoms can
only be made after repeated consultations for physical symptoms that remain medically
unexplained after adequate examination.
There were some limitations regarding the quality of included studies of the review. Firstly, the
numbers of participants enrolled in the cohorts is limited. Secondly, only a minority of the
included studies presented sufficient data on the duration of symptoms at baseline. Thirdly, a
detailed description of treatments during follow-up was absent although we assume that all
patients received some kind of treatment during the follow-up.
The qualitative methods
Most chapters of this thesis used qualitative research methods to explore the care GPs deliver to
patients with persistent MUS and to explore the care patients with persistent MUS expect. The
qualitative research methods used in this thesis are: qualitative interviews (chapter 4), focus
group discussions (chapter 5), consultation analysis (chapter 7), qualitative analysis of the
literature (chapter 8 and 9) and nominal group technique (chapter 10). Here we will discuss the
strengths and limitations of the research methods used in these different chapters.
Strengths
The qualitative methods used in the interview study, the focus group study, the two literature
studies and nominal group technique has been recommended as the best method to explore and
clarify opinions.64 For researching the doctor-patient communication during consultations,
video-recording has been recommended as the best method.31In all qualitative studies we used a
cyclical and interactive way of collecting and analyzing data in order to progressively refine the
focus and explore the data in depth.65 Furthermore, we transcribed the data verbatim, entered
the full texts into Altas.ti, and coded and re-organized data by two researchers independently
using the principles of constant comparative analysis.66 The constant comparative method
constitute the core of qualitative analysis in qualitative research.67
General discussion | 207
Our patient interview study is the first study on opinions and expectations of patients with
documented, persistent MUS and reflects opinions of patients who have had recent and
relatively frequent encounters with the healthcare system and their GP. Therefore, their
opinions are built on a broad and recent experience with medical services. By using a purposive
sampling strategy and a triangulation strategy of asking independent GPs to judge our results
we were able to capture and verify the variety of opinions present in the population of GPs. As
the focus group study examined GPs' perceptions and not actual behaviour, we performed a
video consultation study. As neither the GP nor the patient was aware of the subject of study and
as there is little evidence that video-recording influences the behaviour of either the GPs or
patients, the Hawthorne effect (the effect that participants improve or modify their behaviour in
response of the fact that they are being studied) in our video consultation study was limited. The
qualitative analysis of the literature regarding explanatory models of MUS and expert opinions
on the management of MUS gave a broad overview of this field. We used an extensive and
systematic search strategy to identify relevant papers and we included and coded the full text
papers by two independent researchers to minimize biases.
In this thesis we integrated more qualitative research techniques for data collection and
analysis, also referred to as mixed method research. Therefore, we were able to benefit from
combining the strengths of the different research methods resulting in a more holistic, valid and
robust exploration and description of the difficulties arising when GPs encounter patients with
persistent MUS.68"70 Furthermore, this helped us to gain more insight into the complex
phenomenon of persistent MUS in primary care.
Limitations
Qualitative research methods are not suited to quantify a certain phenomenon or variable, or to
generalize results from a small sample to a larger population. Therefore the results of our
interview study, focus group study, video consultation study, two literature studies and
nominal group technique should not be interpreted with a quantitative view. The methods
allow the in-depth exploration of the lived experience or actual behaviour of individuals or a
small group of people and put these into the context of the day-to-day reality. Generalization
towards GPs or towards patients with persistent MUS in general is only possible after
quantitative research in random samples of patients an d /or GPs, based on
hypotheses
resulting from qualitative analyses.
Patient interviews about opinions on the doctor-patient relationship give only a snapshot in
time, whereas this relationship is built over time and over many consultations. Patients'
perspectives might have changed over time as a response to their experiences with the GP
an d /or the health care system. The same counts for the video consultation study, as each new
208 I Chapter 11
consultation carries over memories of previous ones which might have influenced the
videotaped consultation. These longitudinal influences on the doctor-patient communication
and relationship were not captured in these studies. Furthermore, although participation bias in
our video consultations study was limited (response rate 89%), in our interview study this kind
of bias might have influenced our findings (response rate 39%) as patients who are satisfied with
their GP are possibly more inclined to participate in the interview study. In contrast to one-toone interviews, during focus group discussions group dynamics might result in the articulation
of group norms or consensus in stead of provoking individual contrasting opinions. By using a
purposive sampling strategy and a skilled moderator during the focus group discussions, we
tried to provoke and capture the full variety of GPs' opinions. In our two literature studies we
did a qualitative analysis of the literature. Although such an analysis is not as objective as a
meta-analysis, we were able to summarize the range of explanatory models and important
elements in the interventions described in the scientific literature nowadays. This summary and
overview might help to guide future intervention strategies for patients with persistent MUS.
However, we are not able to draw conclusions on the degree of evidence and the effectiveness of
the explanatory models and important elements in the interventions for patients with persistent
MUS as we did not study the evidence regarding these models and elements.
Recommendations for clinical practice
The worries of GPs regarding the development of persistent MUS are mostly not justified as the
majority of these patients generally have a favourable prognosis. Establishing the number of
somatic symptoms and the seriousness of the condition during the first consultations might help
GPs to value the risk of persistence and may guide GPs whether to offer only reassurance about
the favourable prognosis or a more intensive approach. Furthermore, it seems important to
communicate this favourable and positive prognosis with the patient during the MUS
consultation.
To improve the outcomes for patients with persistent MUS, GPs have to focus on the
consultation itself, the presented symptoms, and the words they use during these consultations.
GPs have to improve their communication towards a more clear and focused communication
style by (1) the exploration of patients' needs, beliefs, concerns and expectations, (2) the
exploration of the reason for encounter, (3) active listening and noticing cues, (4) agenda setting
and summarizing the information obtained during the consultation, (5) providing tangible,
positively formulated explanations incorporating patients' beliefs and concerns. Furthermore, a
positive and continuous doctor-patient relationship is necessary for a consultation to be
effective. Therefore, GPs have to focus on (a) taking patients seriously, (b) showing empathy, (c)
General discussion | 209
understanding the context of an individual patient with his or her illness and (d) mutual trust.
Regularly scheduled appointments can serve as a tool for this.
Creating a safe therapeutic environment shaped by a clear and focused communication and a
therapeutic doctor-patient relationship might be key to improve the health care delivered to
patients with persistent MUS.
Recommendation for future research
Although this thesis makes an important contribution to a more patient-oriented way of
studying the possibilities for improving the health care delivered to patients with persistent
MUS, more research is needed to provide GPs with instructions and advices for the best
individualized therapeutic approaches towards these patients. As our research agenda in MUS,
defined by GPs from all over the world, indicated, more research is needed on (1) aetiology and
course, (2) problems in the consultation, and (3) therapeutic options.
Regarding aetiology and course, there is need for more well-conducted prospective cohort
studies with a reasonable number of patients (>200 patients), in which assessment of treatments
during follow-up and inclusion of patients at a similar point in the course of there disease are
important topics. These studies should incorporate the quality of the communication and the
doctor-patient relationship, in order to reveal which nonspecific aspects of the clinical
encounter affects help-seeking behaviour in these patients, and the outcome of the consultations
with these patients.
Regarding the problems in the consultation, there is need for further examination of the efficacy
of improving the exploration of patients' ideas, concerns and expectation and the structure of the
persistent MUS consultation. Furthermore, our findings should be confirmed in a larger,
prospective qualitative study that could track doctor-patient communication regarding MUS
over time. Such studies should reveal whether patients wish and accept a more in-depth
exploration and structure of the consultation.
Regarding therapeutic options for patients with persistent MUS, mixed method methodology
may reveal effective methods of explaining the symptoms. Furthermore, this research should
study the effects of the (improvement of the) quality of the GP-patient relationship on
symptoms, impairment, disability and satisfaction in these patients.
210 I Chapter 11
Recommendations for medical education
Medical students and GP residents have to realize that they have powerful tools to effectively
manage and treat patients with persistent MUS. These students and residents have to be
convinced of this powerful tools, for example by presenting them the available evidence, about
the importance of a positive consultation and communication style and the therapeutic effects of
the doctor-patient relationship. Furthermore, we have to teach them about patients' preferences
and experts opinions regarding the management of persistent MUS in primary care.
Given that ideas in doctors' minds play such an important role, it is imperative that something
should be done about the way doctors are trained. In particular, we need to pay special attention
to the side-effects of the monolithic position of the biomedical approach. We need to teach our
students that the biomedical model is only one of many perspectives. We also need to focus on
the fact that doctors usually view symptoms as expressions of disease and on the fact that
doctors consider symptoms with a clear underlying pathology to be more real than symptoms
that cannot be objectively measured.
Renewed attention for the consultation behaviour is desirable. This extra attention means
paying attention to symptoms, expectations, ideas and feelings regarding presented symptoms
in order to attain a good understanding of the symptoms, finding common ground and building
mutual trust. Generic elements such as attentive listening, explaining symptoms to patients and
ways to reassure patients needs further attention
Conclusion
The majority of patients with MUS have a favourable prognosis. Only a minority ends up in a
chronic condition. Establishing the number, diversity and severity of the symptoms during the
first consultations might help GPs to value the risk of persistence of the symptoms.
There seems to be a mismatch between what patients with persistent MUS want and what GPs
deliver to them. Patients want a tangible and positive formulated explanation for their
symptoms, whereas GPs face difficulties in doing so. Furthermore, patients with persistent
MUS want GPs to pay attention to their ideas, concerns and expectations, whereas GPs actual
behaviour during the encounters with these patients show the opposite (i.e. limited exploratory
behaviour).
General discussion | 211
Patients with persistent MUS and GPs agree on the importance of a good doctor-patient
relationship. They both value a personal continuing GP-patient relationship built upon
physician attitude, medical competence, availability and shared authority. However, at the
same time GPs indicate that they often face difficulties in preserving the doctor-patient
relationship during encounters with these patients. They try to balance between the
maintenance of the relationship and the prevention of unintended consequences of their
interventions.
Based on these findings we conclude that there seems to be room for improving the care and
outcomes for patients with persistent MUS. For example by establishing a more clear and
focused communication style in which patients' ideas, concerns and expectations are explored
and taken into account. Active listening, noticing cues, agenda setting, summarizing the
information obtained during the consultation, exploring the reason for encounter, and giving
tangible and positively formulated explanations can help with that. Furthermore, a positive
doctor-patient relationship in which patients are taken seriously, GPs show empathy and try to
understanding the context of an individual patient, and both patients and GPs work on mutual
trust, might contribute to improve the care and outcomes for these patients.
212 I Chapter 11
Reference List
1
Green LA, Fryer GE, Jr., Yawn BP, Lanier D, Dovey SM. The ecology of medical care
revisited. N Engl J Med 2001; 344(26):2021-2025.
2
van de Lisdonk EH. Perceived and presented morbidity in general practice. A study
with diaries in four general practices in The Netherlands. Scand J Prim Health Care
1989; 7(2):73-78.
3
Bass C e. Somatisation: Physical Symptoms and Psychological disorder. Oxford:
Blackwell; 1990.
4
Trimble MR. Functional diseases. Br Med J (Clin Res Ed) 1982; 285(6357):1768-1770.
5
Katon WJ, Walker EA. Medically unexplained symptoms in primary care. J Clin
Psychiatry 1998; 59 Suppl 20:15-21.
6
van der Linden M, Westert G, de Bakker D, Schellevis F. Tweede Nationale Studie naar
ziekten en verrichtingen in de huisartspraktijk: klachten en aandoeningen in de
bevolking en in de huisartspraktijk (Second National Survey of morbidity and
interventions in general practice: symptoms and diseases in the population). 2004.
Ref Type: Report
7
Verhaak PF, Meijer SA, Visser AP, Wolters G. Persistent presentation of medically
unexplained symptoms in general practice. Fam Pract 2006; 23(4):414-420.
8
Creed F, Barsky A. A systematic review of the epidemiology of somatisation disorder
9
Vassend O. Negative affectivity, subjective somatic complaints, and objective health
and hypochondriasis. J Psychosom Res 2004; 56(4):391-408.
indicators. Mind and body still separated? In: Maes S, Leventhal H, Johnston M, editors.
International review of health psychology, vol. 3. Chichester: Wiley; 1994. 97-118.
10 De Gucht V, Heiser W. Alexithymia and somatisation: quantitative review of the
literature. J Psychosom Res 2003; 54(5):425-434.
11 Wessely S, Nimnuan C, Sharpe M. Functional somatic syndromes: one or many? Lancet
1999; 354(9182):936-939.
12 Nimnuan C, Rabe-Hesketh S, Wessely S, Hotopf M. How many functional somatic
syndromes? J Psychosom Res 2001; 51(4):549-557.
13 Cairns R, Hotopf M. A systematic review describing the prognosis of chronic fatigue
syndrome. Occup Med (Lond) 2005; 55(1):20-31.
14 Sturmberg JP. The foundations of primary care. Daring to be different. Oxford - Seattle:
Radcliffe Publishing Ltd; 2007.
15 Misselbrook D. Thinking about patients. Newbury: Petroc press; 2001.
16 Peters S, Stanley I, Rose M, Salmon P. Patients with medically unexplained symptoms:
sources of patients' authority and implications for demands on medical care. Soc Sci
Med 1998; 46(4-5):559-565.
General discussion | 213
17 Werner A, Malterud K. It is hard work behaving as a credible patient: encounters
between women with chronic pain and their doctors. Soc Sci Med 2003; 57(8):1409-1419.
18
Chew CA, May CR. The benefits of back pain. Fam Pract 1997; 14(6):461-465.
19 Nettleton S. 'I just want permission to be ill': Towards a sociology of medically
unexplained symptoms. Soc Sci Med 2006;62(5):1167-78.
20 Salmon P. Conflict, collusion or collaboration in consultations about medically
unexplained symptoms: the need for a curriculum of medical explanation. Patient Educ
Couns 2007; 67(3):246-254.
21 Stewart MA, McWhinney IR, Buck CW. The doctor/patient relationship and its effect
upon outcome. J R Coll Gen Pract 1979; 29(199) :77-81.
22 Peltenburg M, Fischer JE, Bahrs O, van Dulmen S, van den Brink-Muinen A. The
unexpected in primary care: a multicenter study on the emergence of unvoiced patient
agenda. Ann Fam Med 2004; 2(6):534-540.
23
Cegala DJ. A study of doctors' and patients' communication during a primary care
consultation: implications for communication training. J Health Commun 1997; 2(3):169194.
24 Kappen T, van Dulmen SM. General practitioners' responses to the initial presentation of
medically unexplained symptoms: a quantitative analysis. Biopsychosoc Med 2008;
2(1):22.
25 Spiro H. What is empathy and can it be taught? Ann Intern Med 1992; 116(10):843-846.
26 Bryne PS, Long BE. Doctors talking to patients. London: Her majesty's stationery office;
1976.
27 Salmon P, Dowrick CF, Ring A, Humphris GM. Voiced but unheard agendas: qualitative
analysis of the psychosocial cues that patients with unexplained symptoms present to
general practitioners. Br J Gen Pract 2004; 54(500):171-176.
28 Lang F, Floyd MR, Beine KL. Clues to patients' explanations and concerns about their
illnesses. A call for active listening. Arch Fam Med 2000; 9(3):222-227.
29 Levinson W, Gorawara-Bhat R, Lamb J. A study of patient clues and physician responses
in primary care and surgical settings. JAMA 2000; 284(8):1021-1027.
30 Balint M. The doctor, his patient and the illness. Edinburgh: Churchill Livingstone; 2000.
31 Inui TS, Carter WB. Problems and prospects for health services research on provider­
patient communication. Med Care 1985; 23(5):521-538.
32 Dowrick CF, Ring A, Humphris GM, Salmon P. Normalisation of unexplained
symptoms by general practitioners: a functional typology. Br J Gen Pract 2004;
54(500):165-170.
33 Arborelius E, Bremberg S. What can doctors do to achieve a successful consultation?
Videotaped interviews analysed by the 'consultation map' method. Fam Pract 1992;
9(1):61-66.
214 I Chapter 11
34 Starfield B, Wray C, Hess K, Gross R, Birk PS, D'Lugoff BC. The influence of patientpractitioner agreement on outcome of care. Am J Public Health 1981; 71(2):127-131.
35
Churchill LR, Schenck D. Healing skills for medical practice. Ann Intern Med 2008;
149(10):720-724.
36 Little P, Everitt H, Williamson I, Warner G, Moore M, Gould C et al. Preferences of
patients for patient centred approach to consultation in primary care: observational
study. BMJ 2001; 322(7284):468-472.
37 Stewart MA. Effective physician-patient communication and health outcomes: a review.
CMAJ 1995; 152(9):1423-1433.
38 Stewart M, Brown JB, Donner A, McWhinney IR, Oates J, Weston WW et al. The impact
of patient-centered care on outcomes. J Fam Pract 2000; 49(9):796-804.
39 Jackson JL. Communication about symptoms in primary care: impact on patient
outcomes. J Altern Complement Med 2005; 11 Suppl 1:S51-6.:S51-S56.
40 Thorne SE, Kuo M, Armstrong EA, McPherson G, Harris SR, Hislop TG. 'Being known':
patients' perspectives of the dynamics of human connection in cancer care.
Psychooncology 2005; 14(10):887-898.
41 Hack TF, Degner LF, Parker PA. The communication goals and needs of cancer patients:
a review. Psychooncology 2005; 14(10):831-845.
42 Thomas KB. General practice consultations: is there any point in being positive? Br Med
J (Clin Res Ed) 1987; 294(6581):1200-1202.
43 Suarez-Almazor ME, Looney C, Liu Y, Cox V, Pietz K, Marcus DM et al. A randomized
controlled trial of acupuncture for osteoarthritis of the knee: effects of patient-provider
communication. Arthritis Care Res (Hoboken ) 2010; 62(9):1229-1236.
44 Cals JW, Butler CC, Hopstaken RM, Hood K, Dinant GJ. Effect of point of care testing for
C reactive protein and training in communication skills on antibiotic use in lower
respiratory tract infections: cluster randomised trial. BMJ 2009; 338:b1374. doi:
10.1136/bmj.b1374.:b1374.
45 Street RL, Jr., Makoul G, Arora NK, Epstein RM. How does communication heal?
Pathways linking clinician-patient communication to health outcomes. Patient Educ
Couns 2009; 74(3):295-301.
46 Stewart M. Reflections on the doctor-patient relationship: from evidence and experience.
Br J Gen Pract 2005; 55(519):793-801.
47 McWhinney IR. A textbook of Family Medicine. New York; Oxford: Oxford University
Press; 1989.
48 Cabana MD, Jee SH. Does continuity of care improve patient outcomes? J Fam Pract
2004; 53(12):974-980.
49 Kim SC, Kim S, Boren D. The quality of therapeutic alliance between patient and
provider predicts general satisfaction. Mil Med 2008; 173(1):85-90.
General discussion | 215
50 Nutting PA, Goodwin MA, Flocke SA, Zyzanski SJ, Stange KC. Continuity of primary
care: to whom does it matter and when? Ann Fam Med 2003; 1(3):149-155.
51 Lambert MJ, Barley DE. Research summary on the therapeutic relationship and
psychotherapy outcome. In: Norcross JC, editor. Psychotherapy relationship that work:
therapist contributions and responsiveness to patients. Oxford University Press; 2002.
52 DiBlasi Z., Harkness E, Ernst E, Georgiou A, Kleijnen J. Influence of context effects on
health outcomes: a systematic review. Lancet 2001; 357(9258):757-762.
53 van Os TW, van den Brink RH, Tiemens BG, Jenner JA, van der Meer K, Ormel J.
Communicative skills of general practitioners augment the effectiveness of guidelinebased depression treatment. J Affect Disord 2005; 84(1):43-51.
54 Kaptchuk TJ, Kelley JM, Conboy LA, Davis RB, Kerr CE, Jacobson EE et al. Components
of placebo effect: randomised controlled trial in patients with irritable bowel syndrome.
BMJ 2008; 336(7651):999-1003.
55 Smith RC, Lyles JS, Gardiner JC, Sirbu C, Hodges A, Collins C et al. Primary care
clinicians treat patients with medically unexplained symptoms: a randomized controlled
trial. J Gen Intern Med 2006; 21(7):671-677.
56 Jackson JL, Kroenke K. Managing somatization: medically unexplained should not mean
medically ignored. J Gen Intern Med 2006; 21(7):797-799.
57 Chew-Graham CA, May CR, Roland MO. The harmful consequences of elevating the
doctor-patient relationship to be a primary goal of the general practice consultation. Fam
Pract 2004; 21(3):229-231.
58 Weel-Baumgarten EM, van den Bosch WJ, van den Hoogen HJ, Zitman FG. The validity
of the diagnosis of depression in general practice: is using criteria for diagnosis as a
routine the answer? Br J Gen Pract 2000; 50(453):284-287.
59 deGruy F, Columbia L, Dickinson P. Somatization disorder in a family practice. J Fam
Pract 1987; 25(1):45-51.
60 Feder A, Olfson M, Gameroff M, Fuentes M, Shea S, Lantigua RA et al. Medically
unexplained symptoms in an urban general medicine practice. Psychosomatics 2001;
42(3):261-268.
61 Simon GE, Gureje O. Stability of somatization disorder and somatization symptoms
among primary care patients. Arch Gen Psychiatry 1999; 56(1):90-95.
62 van Weel C. The Continuous Morbidity Registration Nijmegen: background and history
of a Dutch general practice database. Eur J Gen Pract 2008; 14 Suppl 1:5-12.
63 Reid S, Crayford T, Richards S, Nimnuan C, Hotopf M. Recognition of medically
unexplained symptoms--do doctors agree? J Psychosom Res 1999; 47(5):483-485.
64 Britten N. Qualitative interviews in medical research. BMJ 1995; 311(6999):251-253.
65 Britten N, Jones R, Murphy E, Stacy R. Qualitative research methods in general practice
and primary care. Fam Pract 1995; 12(1):104-114.
216 I Chapter 11
66 Glaser BG, Strauss AL. The discovery of grounded theory. Chigago: Aldine; 1967.
67 Boeije H. A Purposeful Approach to the Constant Comparative Method in the Analysis
of Qualitative Interviews. Quality and Quantity 2010; 36(4):391-409.
68 Lucassen PL, olde Hartman TC. Kwalitatief onderzoek. Praktische methoden voor de
medische praktijk. Houten: Bohn Stafleu van Loghum; 2007.
69 O'Byrne P. The advantages and disadvantages of mixing methods: an analysis of
combining traditional and autoethnographic approaches. Qual Health Res 2007;
17(10):1381-1391.
70 Creswell J.W., Fetters M.D., Ivankova N.V. Designing a mixed methods study in
primary care. Ann Fam Med 2004; 2(1):7-12.
General discussion | 217
Summary
This thesis explored (1) the care patients with persistent MUS expect when visiting the GP, (2)
the care GPs deliver to patients with persistent MUS and (3) the way GPs experience the care
they deliver to their patients with persistent MUS. Furthermore, we present starting points for
intervention strategies for patients with persistent MUS in primary care in order to improve the
care for these, often functionally impaired, patients.
Chapter 1. General introduction.
In this chapter the rationale, aims and outline of this thesis are described.
Medically unexplained symptoms (MUS) are common and most of these symptoms are
transient. However, a minority of the patients will keep visiting the doctor because of MUS (i.e.
persistent MUS). This minority represent a major problem in health care as they are responsible
for high, often unnecessary, health care costs. Furthermore, these patients suffer from their
symptoms and are functionally impaired.
We explored the knowledge regarding the problems arising when GPs meet patients with
persistent MUS in daily practice. Furthermore, we indicated knowledge gaps regarding the care
GPs deliver and the care patients expect when encountering with persistent MUS.
Patients with persistent MUS often feel the skepticism of their doctors and have the feeling that
the GPs don't take them serious. They are often dissatisfied with the medical care they receive.
Doctors experience patients with persistent MUS as difficult to manage. They tend to believe
that (1) these patients fail to see the connection between physical symptoms and psychological
distress, and that (2) there is incongruence between the presentation of MUS and the actual
burden. Furthermore, they feel pressurized to offer somatic interventions. Consultations
between GPs and patients with MUS seems to be less patient-centred. In these consultations
patients with MUS did not pressurize for somatic interventions, but desired more emotional
support.
Most research regarding the problematic interaction between GPs and patients with MUS did
not specifically focus on patients with persistent MUS. During the chronic condition in which
patients persistently present MUS to their GP, GPs have to find a way to manage these patients in
order to improve patients' health.
Summary | 221
The patient
Chapter 2. Chronic functional somatic symptoms: a single syndrome?
In this chapter we aimed to identify distinctive features in patients with persistent MUS by
studying the Continuous Morbidity Registration database. This is the only morbidity
registration system in the world with a structural possibility to classify patients with persistent
MUS (CMR classifies persistent MUS as chronic functional somatic symptoms (CFSS)). We
included 182 patients with persistent MUS and 182 matched controls from this registration
system and collected data on comorbidity, referrals, diagnostic tests, hospital admissions,
medication use and number of visits to the GP over a period of 10 years prior to the diagnosis. We
found that during the 10 years prior to the diagnosis persistent MUS patients presented MUS in
at least two body systems and used more somatic and psychotropic drugs compared to controls.
Furthermore, they visited the GP twice as much and had more psychiatric morbidity, and were
referred more often to mental health workers and somatic specialists. The number of patients
undergoing diagnostic test was also higher. Hospital admission rates were equal. We concluded
that patients with persistent MUS have a great diversity of unexplained symptoms, use more
somatic and psychotropic drugs in the years before diagnosis and show high rates of referrals
and psychiatric morbidity compared with controls.
Chapter 3. Medically unexplained symptoms, somatisation disorder and
hypochondriasis: course and prognosis. A systematic review.
In chapter 3 we studied the course of MUS, somatisation disorder and hypochondriasis and
related prognostic factors. We searched the relevant databases of the medical literature to select
studies focusing on patients with MUS, somatisation and hypochondriasis and to assess
prognostic factors. We performed a best-evidence synthesis for the interpretation of the results.
We could include six studies on MUS, six studies on hypochondriasis and one study on abridged
somatisation and found that approximately 50 to 75% of the patients with MUS improved,
whereas 10-30% of patients with MUS deteriorate. In patients with hypochondriasis recovery
rates varied between one third to 50%. In studies on MUS and hypochondriasis we found some
evidence that the number of somatic symptoms and the seriousness of the condition at baseline
influenced course and prognosis. Comorbid anxiety and depression did not seem to predict the
course of MUS, abridged somatisation or hypochondriasis. We concluded that due to the limited
number of studies and their high heterogeneity, there is a lack of empirical evidence to identify
relevant prognostic factors in patients with persistent MUS. However, it seems that a more
serious condition at baseline is associated with a worse outcome.
S
222
Chapter 4. The doctor-patient relationship from the perspective of patients with
persistent medically unexplained symptoms. An interview study.
In Chapter 4 we studied the perspectives of patients with persistent MUS regarding their
expectations of GPs' health care. By conducting qualitative semi-structured interviews with 17
patients with persistent MUS we were able to reveal opinions of patients with a documented
long history of presenting MUS. All patients stressed the importance of a personal continuing
doctor-patient relationship. They indicate that such a relationship is built on physician attitude,
medical competence, availability and shared authority. Patients want to be taken serious in a
non-judgmental open communication style. They appreciate a thorough exploration and a
comprehensible explanation of the symptoms. Furthermore, they want a competent. GP who is
easily accessible and who engages them as partners in the consultation and decision making
process. We conclude that patients with persistent MUS appreciate a patient-centred
communication and orientation to a form of care in which personal continuity and continuity of
the relationship are important elements.
The doctor
Chapter 5. Explanation and relations. How do general practitioners deal with
patients with persistent medically unexplained symptoms: a focus group study.
This chapter explored GPs' perceptions about explaining MUS to patients with persistent MUS
and about how relationships with these patient evolve over time in daily practice. We used a
qualitative focus group approach in which twenty-two GPs within five focus groups were
interviewed. GPs indicated that they recognise the importance of an adequate explanation of the
diagnosis of MUS but often feel incapable of being able to explain it clearly to their patients.
Therefore, they try to reassure patients in non-specific ways, for example by telling patients that
there is no disease, by using metaphors and by normalizing the symptoms. When patients keep
returning to the GP with MUS, GPs stress the importance of maintaining the doctor-patient
relationship. GPs describe three different models to do this: mutual alliance characterized by
ritual care (e.g. regular physical examination, regular doctor visits) with approval of the patient
and the doctor, ambivalent alliance characterized by ritual care without approval of the doctor
and non-alliance characterized by cutting of all reasons for encounter in which symptoms are
not of somatic origin. We conclude that GPs experience difficulties in explaining the symptoms
and that they meticulously balance between maintaining a good doctor-patient relationship and
the prevention of unintended consequences of unnecessary interventions.
Summary | 223
The consultation
Chapter 6. 'Well doctor, it is all about how life is lived': cues as a tool in the medical
consultation.
In this chapter we described a patient with unexplained palpitations during vacuuming. During
one of the consultations she provided an important psychosocial cue which changed my
perspective on her palpitations, resulting in a deeper understanding of her symptoms. We
experienced that this non-explicit remark that enclosed a special meaning served as a tool to
clarify the patient's agenda. This resulted in a mutual understanding about the symptoms,
enhanced the therapeutic relationship and improved the illness outcome. We concluded that
noticing cues in the medical consultation helps the doctor to understand the patient's real
worries and gives a better understanding of the patient's perspective.
Chapter 7. How patients and family physicians communicate about persistent
medically unexplained symptoms. A qualitative study of video-recorded
consultations.
This chapter describes an exploratory, qualitative analysis of 20 videotaped consultations
between GPs and patients with persistent MUS in order to study doctor-patient interaction
styles and to study on which stages of the consultation patients and doctors focus within the
available time. We found that patients presented many symptoms in a rather unstructured way.
However, GPs hardly use structuring techniques such as agenda setting and summarizing.
Patients with persistent MUS got much opportunity to tell their story, but the reasons for
encounter, their beliefs and concerns were not discussed in a structured manner. Most of the
time patients themselves had to initiated discussion of their ideas, concerns and expectations.
However, GPs' extensive explanations of the origin of the symptoms often did not take patients'
beliefs and concerns into account. We concluded that due to patients' multiple symptom
presentation and the absence of GPs' structuring techniques, consultations of patients with
persistent MUS in this study proceed rather unfocused. However, patients got ample
opportunity to tell their story. Furthermore, patients with persistent MUS might benefit from
structured consultations focused on the exploration of the reason for encounter.
Starting points fo r improving management
Chapter 8. Experts' opinions on the management of medically unexplained
symptoms in primary care. A qualitative analysis of narrative reviews and scientific
editorials.
This chapter reviewed important and effective elements in the treatment of patients with MUS
S
224
in primary care according to experts in MUS research in order to explore effective and acceptable
strategies to manage these functionally impaired patients. We performed a systematic search of
narrative reviews and scientific editorials in the most important databases of the medical
literature and triangulated our findings by conducting a focus group interview with MUS
experts. We included 7 scientific editorials and 23 narrative reviews. According to MUS experts
the most important elements in the treatment of MUS are: creating a safe therapeutic
environment; generic interventions (such as motivational interviewing, giving tangible
explanations, reassurance and regularly scheduled appointments); and specific interventions
(such as cognitive approaches and pharmacotherapy). However, in contrast to most specific
interventions, experts rarely describe the effects of generic interventions, doctor-patient
communication and relationship quantitatively in their scientific editorials and narrative
reviews. MUS experts indicate that a multi-component approach in which these three important
elements are combined are most helpful for patients with MUS. We concluded that, in contrast to
most specific interventions, opinions of MUS experts regarding generic interventions and
creating a safe therapeutic relationship seem to be more based on theory and experience, than on
quantitative research. Studies showing the effectiveness of these elements in the management of
MUS in primary care are still scarce. Research as well as medical practice should focus more on
these non-specific aspects of the medical consultation.
Chapter 9. Explanatory models of medically unexplained symptoms: a qualitative
analysis of the literature.
This chapter provides an overview of explanatory models for MUS in order to provide GPs with
explanatory models known from the scientific literature that may be useful in daily medical
practice. Therefore we performed a systematic search of reviews in the relevant databases of the
scientific literature and analyzed the data qualitatively according to the principles of constant
comparative analysis to identify specific explanatory models. We distinguished nine specific
explanatory models of MUS in the literature: somatosensory amplification, sensitization,
sensitivity, immune system sensitization, endocrine dysregulation, signal filter model, illness
behaviour model, autonomous nervous system dysfunction and abnormal proprioception. The
nine different explanatory models focus on different domains, including: somatic causes,
perception, illness behaviour and predisposition. We also found one meta-model, which
incorporates these four domains: the cognitive behavioural therapy model. We concluded that
although GPs often face difficulties when providing explanations to patients with MUS, there
are multiple explanatory models in the scientific literature that may be of use in daily medical
practice.
Summary | 225
Chapter 10. Medically unexplained symptoms in family medicine: defining a
research agenda. Proceedings from WONCA 2007.
In this chapter we detected knowledge gaps in MUS and established priorities in MUS research
by bringing together experts of MUS research and discussing the state of the art in MUS research
internationally. By using a nominal group technique, we generated research topics and themes,
set priorities in MUS research and proposed a research agenda. Participants' (66 researchers and
GPs from 29 nationalities) most important research topics were 'formulating a broadly accepted
definition of MUS', 'finding a strategy to recognize MUS better and at an earlier stage', 'studying
the value of self-management and empowerment in patients with MUS' and 'finding predictors
to decide which strategy will best help the individual patient with MUS'. Priorities in research
themes of MUS were: (i) therapeutic options for patients with MUS and (ii) problems in
consultations with these patients. We concluded that more research on MUS in primary care is
needed to improve the consultations with and management of these patients. Furthermore,
internationally primary care conferences seemed to be excellent for exchanging ideas and
formulating central issues of research.
Chapter 11. General discussion.
This final chapter considers the results described in this thesis together with some
methodological issues, and ends with implications and recommendations for intervention
strategies and suggestions for further research and general practice.
We conclude that (1) the majority of the patients with MUS have a favourable prognosis and that
establishing the number, diversity and severity of the symptoms during the first consultation
might help GPs to value the risk of persistence of the symptoms, (2) there seems to be a mismatch
between what patients with persistent MUS want and what they receive from their GP, and (3)
patients and GPs agree on the importance of a good doctor-patient relationship. Therefore,
exploring and taking into account patients' ideas, concerns and expectations, together with
building a positive doctor-patient relationship, might contribute to improve the care and
outcomes for patients with persistent MUS.
The most important recommendations for clinical practice are that we have to focus on the
consultation itself, the presented symptoms, and the words we use during these consultations.
Furthermore, we have to focus on creating a safe therapeutic environment shaped by a clear and
focused communication and a therapeutic doctor-patient relationship.
The most important recommendations for future research are that future MUS research has to
take the doctor-patient communication and relationship into account in order to reveal which
nonspecific aspects of the clinical encounter affects the outcome of these consultations.
226
Furthermore, effective methods of explaining symptoms to patients with persistent MUS have
to be tested.
Medical students and GP residents have to be taught that a positive consultations and
communication style and a good doctor-patient relationship are therapeutic in itself and
therefore a powerful and important tool in order to effectively manage and treat patients with
persistent MUS.
Sam envatting | 227
Samenvatting
Dit proefschrift beschrijft (1) de zorg die patiënten met persisterende somatisch onvoldoende
verklaarde lichamelijke klachten (SOLK) verwachten van hun huisarts, (2) de zorg die
huisartsen leveren aan patiënten met persisterende SOLK en (3) de ervaringen van huisartsen
met de zorg voor patiënten met persisterende SOLK. Vervolgens presenteren we
uitgangspunten voor de behandeling en begeleid ing van deze patiënten in de
huisartsenpraktijk met als doel de zorg te verbeteren voor deze patiënten die vaak erg beperkt
zijn in hun functioneren.
Hoofdstuk 1. Algemene inleiding.
In dit hoofdstuk beschrijven we de achtergronden, doelen en opbouw van dit proefschrift.
SOLK komen veel voor en meestal zijn deze klachten van voorbijgaande aard. Echter, een
minderheid van de patiënten blijft de huisarts bezoeken met SOLK omdat de klachten
aanhouden (i.e. persisterende SOLK). Deze minderheid vormt een groot probleem voor de
g e z o n d h e id sz o rg
o m d at ze v e r a n tw o o r d e lijk
is v o o r h o g e , v a a k o n n o d ig e ,
gezondheidszorgkosten. Bovendien hebben deze patiënten vaak veel last van hun klachten en
ondervinden ze beperkingen in hun dagelijks leven ten gevolge van de klachten. Consulten met
deze patiënten in de huisartspraktijk verlopen vaak niet zonder problemen.
We beschrijven de reeds bestaande kennis over de problemen die ontstaan wanneer huisartsen
en patiënten met persisterende SOLK elkaar ontmoeten in de dagelijkse praktijk. Daarnaast
geven we aan waar meer kennis nodig is over de zorg die huisartsen leveren en de zorg die
patiënten verwachten op het moment dat ze het spreekuur bezoeken met persisterende SOLK.
Patiënten met persisterende SOLK voelen vaak de scepsis van de verschillende dokters en
hebben vaak het gevoel dat de huisarts de klachten niet serieus neemt. Ze zijn vaak ontevreden
over de medische zorg die ze krijgen. Dokters vinden patiënten met persisterende SOLK vaak
moeilijk te behandelen. Ze hebben de neiging te denken dat (1) deze patiënten de link tussen
lichamelijke klachten en psychosociale problemen niet zien, en dat (2) de klachtpresentatie en de
daadwerkelijke ziektelast niet met elkaar in overeenstemming zijn. Daarnaast voelen
huisartsen zich vaak onder druk gezet om somatische interventies aan te bieden. Consulten
tussen huisartsen en patiënten met SOLK lijken weinig patiëntgericht. Bovendien blijkt dat
patiënten met SOLK helemaal geen druk uitoefenen voor het krijgen van somatische
interventies, maar dat ze vooral emotionele ondersteuning van hun huisarts willen.
Het meeste onderzoek naar de moeizame interactie tussen huisartsen en patiënten met SOLK is
niet specifiek gericht op patiënten met persisterende SOLK. Wanneer de klachten chronisch
228
worden en patiënten het spreekuur van de huisarts blijven bezoeken met SOLK, moet de
huisarts een manier vinden om deze patiënten te behandelen en te begeleiden om zo de
gezondheid van deze patiënten te verbeteren.
De patiënt
Hoofdstuk 2. Chronisch functionele klachten: één syndroom?
Het doel van dit hoofdstuk is om, vanuit de Continue Morbiditeit Registratie (CMR),
onderscheidende kenmerken van patiënten met persisterende SOLK te identificeren. De CMR
database is het enige registratie systeem in de wereld dat structureel patiënten met
persisterende SOLK in de huisartspraktijk registreert. De CMR classificeert persisterende SOLK
als chronisch nerveus-functionele klachten. We includeerden 182 patiënten met persisterende
SOLK en 182 controlepatiënten vanuit de CMR database en we verzamelden data over een
periode van 10 jaar voorafgaand aan de diagnose betreffende comorbiditeit, verwijzingen,
diagnostische testen, ziekenhuisopnames, medicatiegebruik en het aantal bezoeken aan de
huisarts. We vonden dat gedurende de 10 jaar voor de diagnose persisterende SOLK patiënten
onverklaarde klachten presenteerden in minstens twee delen van het lichaam en dat deze
patiënten meer somatische medicatie en meer psychofarmaca gebruikten dan de patiënten
zonder persisterende SOLK. Bovendien bezochten patiënten met persisterende SOLK hun
huisarts twee keer zo vaak, hadden ze meer psychiatrische comorbiditeit en werden ze vaker
verwezen naar de geestelijke gezondheidszorg en somatisch medisch specialisten. Het aantal
patiënten dat een diagnostische test onderging was ook hoger. Ziekenhuisopnames waren
gelijk. We concluderen dat patiënten met persisterende SOLK een grote diversiteit aan
onverklaarde klachten presenteren, meer somatische medicatie en psychofarmaca gebruiken in
de jaren voor de diagnose, dat ze vaker verwezen worden en meer psychiatrische aandoeningen
hebben in vergelijking met controlepatiënten.
Hoofdstuk 3. Somatische onvoldoende verklaarde lichamelijke klachten,
somatisatiestoornis en hypochondrie: beloop en prognose. Een systematische
review.
In hoofdstuk 3 beschrijven we het beloop van SOLK, somatisatiestoornis en hypochondrie en
hun prognostische factoren. We doorzochten de medische literatuur en selecteerden
onderzoeken gericht op SOLK, somatisatie en hypochondrie en hun prognostische factoren. We
voerden een best-evidence synthese uit om de resultaten te interpreteren. We konden zes
onderzoeken naar SOLK, zes onderzoeken naar hypochondrie en één onderzoek naar de
verkorte vorm van somatisatiestoornis (i.e. abridged somatisation) includeren en vonden dat
ongeveer 50 tot 70 % van de patiënten met SOLK verbeterden en 10 tot 30 % van de patiënten met
Sam envatting | 229
SOLK verslechterden. Bij patiënten met hypochondrie vonden we herstelpercentages van 30 tot
50%. In de onderzoeken naar SOLK en hypochondrie vonden we enig bewijs dat het aantal
klachten en de ernst van de klachten op baseline het beloop en de prognose beïnvloeden.
Comorbiditeit van angst of depressie lijkt het beloop van hypochondrie niet te beïnvloeden.
Onderzoeken naar de invloed van angst of depressie op het beloop van SOLK laten
tegenstrijdige resultaten zien. We concluderen dat door het beperkt aantal onderzoeken en de
grote heterogeniteit van die onderzoeken het onvoldoende mogelijk is om relevante
prognostische factoren bij patiënten met persisterende SOLK te identificeren. Wel lijkt de ernst
van de klachten op baseline geassocieerd met een slechter beloop.
Hoofdstuk 4. De arts-patiënt relatie volgens patiënten met persisterende SOLK. Een
interview studie.
In hoofdstuk 4 onderzoeken we de verwachtingen die patiënten met persisterende SOLK
hebben van de huisartsenzorg. We namen bij 17 patiënten met persisterende SOLK een semigestructureerd interview af om de meningen en opvattingen van deze patiënten boven tafel te
krijgen. Alle patiënten benadrukten het belang van een persoonlijke langdurige arts-patiënt
relatie. Patiënten gaven aan dat een dergelijke relatie gebaseerd is op de attitude, de medische
competentie, de beschikbaarheid van de dokter en het hebben van een gedeelde
verantwoordelijkheid. Patiënten willen serieus genomen worden door een huisarts die een nietveroordelende open manier van communiceren gebruikt. Ze waarderen een nauwgezette
uitdieping van hun klachten en een begrijpelijke uitleg. Bovendien willen ze een competente
huisarts die gemakkelijk toegankelijk is en die hen betrekt als partners in het consult en het
besluitvormingsproces. We concluderen dat patiënten met persisterende SOLK een
patiëntgerichte communicatie waarderen waarbij ze een persoonlijke langdurige arts-patiënt
relatie erg belangrijk vinden.
De dokter
Hoofdstuk 5. Uitleg en relatie. Hoe gaan huisartsen om met patiënten met
persisterende SOLK: een focusgroep onderzoek.
Dit hoofdstuk belicht de meningen en opvattingen van huisartsen over de uitleg van de klachten
aan patiënten met persisterende SOLK en hoe de relatie met deze patiënten zich ontwikkeld in
de loop van de tijd. We gebruikten een kwalitatieve focusgroep benadering waarin we 22
huisartsen verdeeld over 5 focusgroepen interviewden. Huisartsen geven aan dat ze het belang
van een goede uitleg van de persisterende SOLK onderkennen, maar dat ze vaak grote moeite
hebben met het geven van een dergelijke uitleg. Daarom proberen ze patiënten gerust te stellen
op een niet-specifieke manier, bijvoorbeeld door te zeggen dat er geen ziekte is, door metaforen
S
te gebruiken en door de klachten te normaliseren. Wanneer patiënten terug blijven komen bij de
huisarts met persisterende SOLK, is het volgens huisartsen belang om de arts-patiënt relatie
goed in stand te houden. Ze beschrijven drie verschillende modellen om dit te doen: (1)
onderlinge alliantie gekenmerkt door zorgrituelen (zoals regelmatig lichamelijk onderzoek,
regelmatig contact met de huisarts) met goedkeuring van zowel de patiënt als de dokter; (2)
ambivalente alliantie gekenmerkt door zorgrituelen zonder dat de dokter deze eigenlijk
goedkeurt; (3) non-alliantie gekenmerkt door het afkappen van alle consulten waarin klachten
worden gepresenteerd zonder duidelijk lichamelijke oorzaak. We concluderen dat huisartsen
moeilijkheden ervaren bij het uitleggen van de klachten en dat ze nauwgezet balanceren tussen
het in stand houden van de arts-patiënt relatie en het voorkomen van de negatieve
consequenties van onnodige interventies.
Het consult
Hoofdstuk 6. 'Ach dokter, het leven wordt nu eenmaal zo geleefd': het gebruik van
hints in het consult.
In dit hoofdstuk beschrijven we een patiënt met onverklaarde hartkloppingen tijdens het
stofzuigen. Tijdens een van de consulten gaf ze een belangrijke psychosociale hint die mijn
perspectief op haar hartkloppingen veranderde en resulteerde in een beter begrip van haar
klachten. Ik ondervond dat deze niet expliciete maar toch bijzondere opmerking behulpzaam
was voor het verder uitdiepen van het verhaal van de patiënt. Dit resulteerde in een gezamenlijk
begrip van de klachten, versterkte de therapeutische relatie en bevorderde het ziektebeloop. We
concluderen dat het oppikken van hints in het consult de dokter kan helpen om de mening,
opvattingen, verwachtingen en angst en zo het perspectief van de patiënt beter te begrijpen.
Hoofdstuk 7. Hoe praten patiënten en huisartsen over persisterende SOLK? Een
kwalitatief onderzoek van video consulten.
Dit hoofdstuk beschrijft een explorerende, kwalitatieve analyse van 20 consulten opgenomen
op videotape tussen huisartsen en patiënten met persisterende SOLK. Hierin belichten we de
arts-patiënt communicatie en onderzoeken we op welke onderdelen in het consult patiënten en
dokters zich richten. Patiënten blijken meerdere klachten te presenteren kris-kras door het
consult heen. Huisartsen gebruiken echter nauwelijks gesprekstechnieken, zoals het bepalen
van de agenda en samenvatten, om deze consulten te structureren. Patiënten met persisterende
SOLK krijgen ruim de mogelijkheid om hun verhaal te vertellen. De reden van komst, hun
ideeën en angsten worden echter niet structureel besproken. Meestal initiëren patiënten zelf een
discussie over hun eigen ideeën, angsten en verwachtingen. De uitgebreide uitleg die huisartsen
geven over de persisterende SOLK houdt vaak geen rekening met deze ideeën en angsten. We
Sam envatting | 231
concluderen dat doordat patiënten meerdere klachten presenteren en huisartsen deze consulten
niet actief structureren, consulten met patiënten met persisterende SOLK weinig gericht zijn op
het structureel uitdiepen van de klachten, ideeën, opvattingen en verwachtingen van patiënten.
Wel krijgen patiënten ruim de mogelijkheid om hun verhaal te vertellen. Patiënten met
persisterende SOLK hebben waarschijnlijk baat bij gestructureerde consulten gericht op het
uitdiepen van de reden van komst.
Uitgangspunten voor het verbeteren van de behandeling en begeleiding
Hoofdstuk 8. Meningen van experts over de behandeling en begeleiding van
patiënten met SOLK in de huisartspraktijk. Een kwalitatieve analyse van reviews
en editorials.
In dit hoofdstuk gaan we op zoek naar belangrijke en effectieve elementen in de behandeling en
begeleiding van patiënten met SOLK in de huisartspraktijk. Daarvoor inventariseerden we de
meningen van wetenschappelijke experts op het gebied van SOLK. We voerden een
sy ste m a tisc h e
z o e k a ctie
u it n a a r re v ie w s
(o v e rz ic h tsa rtik e le n )
en e d ito ria ls
(hoofdredactionelen) in de medische literatuur. We controleerden onze bevindingen aan de
hand van een focus groep interview met wetenschappelijke experts in Nederland. We
includeerden 7 editorials en 23 reviews. Volgens de wetenschappelijke experts zijn de meest
belangrijke elementen in de behandeling en begeleiding van patiënten met SOLK: het creëren
van een veilige therapeutische omgeving; generieke interventies (zoals motiverend
interview en, het geven van een duidelijke uitleg, geru ststelling en regelm atige
vervolgconsulten); en specifieke interventies (zoals cognitieve behandelingen en
farmacotherapie). In tegenstelling tot de meeste specifieke interventies beschrijven
wetenschappelijke experts bijna nooit de kwantitatieve effecten van de generieke interventies,
de arts-patiënt communicatie en de arts-patiënt relatie. Wetenschappelijke experts geven aan
dat een meervoudige benadering w aarin deze drie belangrijke elementen worden
gecombineerd het beste helpt bij patiënten met SOLK. We concluderen dat, in tegenstelling tot
de meeste specifieke interventies, de meningen en opvattingen van wetenschappelijke experts
over generieke interventies en het creëren van een veilige therapeutische omgeving meer
gebaseerd lijken te zijn op theorie en persoonlijke ervaring, dan op kwantitatief onderzoek.
Onderzoeken die de effectiviteit van deze elementen in de behandeling en begeleiding van
SOLK onderzoeken zijn schaars. Onderzoek en de dagelijkse praktijk moet zich meer richten op
deze non-specifieke aspecten van het consult.
S
Hoofdstuk 9. Verklaringsmodellen van SOLK: een kwalitatieve analyse van de
literatuur.
Dit hoofdstuk geeft een overzicht van de verklaringsmodellen voor SOLK beschreven in de
medisch wetenschappelijke literatuur. Kennis van deze verklaringsmodellen kan behulpzaam
zijn voor de dagelijkse praktijk van huisartsen. We verrichtten een systematische zoekactie in de
medische literatuur en analyseerden de data kwalitatief volgens de principes van de constant
vergelijkende analyse. We konden negen specifieke verklaringsmodellen voor SOLK
identificeren in de literatuur: somatosensorische amplificatie, sensitisatie, overgevoeligheid,
gevoeligheid van het immuunsysteem, endocriene dysregulatie, signaal-filter theorie,
ziektegedrag model, dysfunctie van het autonoom zenuwstelsel en abnormale proprioceptie.
De negen verschillende verklaringsmodellen zijn gericht op verschillende domeinen, te weten:
lichamelijke oorzaken, perceptie, ziektegedrag en aanleg. We vonden ook een overkoepelend
model die de vier domeinen incorporeert: het cognitieve gedragsmodel. We concluderen dat er
meerdere verklaringsmodellen in de medische literatuur te vinden zijn die eventueel gebruikt
kunnen worden in de dagelijkse praktijk.
Hoofdstuk 10. SOLK in de huisartsgeneeskunde: het definiëren van een
onderzoeksagenda. Uitkomsten van WONCA 2007.
In dit hoofdstuk gaan we op zoek naar ontbrekende kennis op het gebied van SOLK om
vervolgens prioriteiten in het SOLK onderzoek aan te geven. Dit deden we door
wetenschappelijk experts op het gebied van SOLK uit meerdere landen bijeen te brengen en de
stand van zaken van het wetenschappelijk onderzoek naar SOLK te bespreken. We gebruikten
een nominale groepstechniek om onderzoeksonderwerpen en thema's te genereren en
prioriteiten voor het SOLK onderzoek aan te brengen. Hieruit werd een onderzoeksagenda
opgebouwd. De deelnemers bestonden uit 66 wetenschappelijk onderzoekers en huisartsen uit
29 verschillende landen. Zij gaven aan dat 'het formuleren van een breed gedragen en
geaccepteerde definitie van SOLK', 'het vinden van een manier om SOLK in een eerder stadium
te herkennen', 'het bestuderen van de waarde van zelf-management en empowerment bij
patiënten met SOLK' en 'het vinden van voorspellers om te bepalen welke behandeling het
meest effectief is bij de individuele patiënt met SOLK' de belangrijkste onderzoeksonderwerpen
zijn. Ze gaven de hoogste prioriteit aan de volgende onderzoeksthema's: (i) therapeutische
opties voor patiënten met SOLK en (ii) problemen in het consult met deze patiënten. We
concluderen dat er meer onderzoek naar SOLK in de huisartsgeneeskunde nodig is om de
consulten met en de behandeling en begeleiding van deze patiënten te verbeteren. Bovendien
zijn internationale huisartsgeneeskundige congressen een uitstekende mogelijkheid om ideeën
uit te wisselen en onderzoeksthema's te bespreken.
Sam envatting | 233
Hoofdstuk 11. Algemene discussie.
Dit laatste hoofdstuk plaatst de resultaten van dit proefschrift in z'n perspectief, bespreekt
enkele methodologische kwesties, geeft implicaties en aanbevelingen voor de behandeling en
begeleiding van patiënten met persisterende SOLK en geeft suggesties voor verder onderzoek
en de dagelijkse praktijk.
We concluderen dat (1) de meerderheid van de patiënten met SOLK een goede prognose heeft en
dat het vaststellen van het aantal, de diversiteit en de ernst van de klachten tijden het eerste
consult huisartsen kan helpen om het risico van persisteren van klachten in te schatten, (2) er een
mismatch is tussen wat patiënten met persisterende SOLK willen en wat ze daadwerkelijk
krijgen van hun huisarts, en (3) patiënten en huisartsen het eens zijn over het belang van een
goede arts-patiënt relatie. Het uitdiepen van de ideeën, angsten en verwachtingen van de
patiënt tezamen met het opbouwen van een positieve arts-patiënt relatie dragen bij aan het
verbeteren van de zorg en haar uitkomsten voor patiënten met persisterende SOLK.
De belangrijkste aanbevelingen voor de dagelijkse praktijk zijn dat we ons moeten richten op de
consultvoering, de klachten die de patiënt presenteert en de woorden die we gebruiken in deze
consulten. Daarnaast moeten we ons richten op het creëren van een veilige therapeutische
omgeving voortkomend uit een heldere en gerichte communicatie en een therapeutische artspatiënt relatie.
De belangrijkste aanbevelingen voor toekomstig onderzoek is dat onderzoek naar SOLK zich
moet richten op de communicatie en relatie tussen arts en patiënt, om zodoende te achterhalen
welke non-specifieke aspecten van het consult de uitkomsten van deze consulten beïnvloeden.
Daarnaast is er behoefte aan onderzoek naar welke manieren effectief zijn om klachten uit te
leggen aan patiënten met persisterende SOLK.
We moeten medisch studenten en huisartsen in opleiding leren dat een positief consult,
positieve communicatie en een goede arts-patiënt relatie therapeutisch in zichzelf zijn en
daarmee een erg krachtig en belangrijk instrument om patiënten met persisterende SOLK te
behandelen en te begeleiden.
S
D ank !
In 2002 begon ik met dit project. In 2011 dan uiteindelijk de afronding. Sommigen van u zullen
wel denken, had dat niet wat sneller gekund? Ach ja, vast wel, zou mijn antwoord zijn, maar er
zijn ook zoveel andere leuke dingen: de huisartsopleiding, redactielidmaatschap bij Huisarts en
Wetenschap, internationale congressen en samenwerkingsverbanden, meeschrijven aan
nationale (multidisciplinaire) richtlijnen, een eigen praktijk starten en opbouwen en natuurlijk
de persoonlijke patiëntenzorg. En veel belangrijker nog: trouwen met mijn jeugdliefde, een huis
kopen, twee prachtige zoons krijgen en een leuk sociaal leven met familie en vrienden. Werk en
privé in een continu samenspel, en dat maakt de afronding van dit proefschrift ook zo mooi en
bijzonder.
Voor een succesvol samenspel is natuurlijk de inzet van meerdere personen nodig. Zij krijgen
dan ook een welverdiende plek in mijn dankwoord. Zo'n dankwoord is altijd gevaarlijk omdat
ik natuurlijk mensen zal vergeten te noemen. Daarom wil ik bij deze alle mensen bedanken die
hun steentje hebben bijgedragen aan al het leuks dat ik in de afgelopen 10 jaar heb mogen doen.
Peter Lucassen. Peter, jij bent de geestelijk vader van dit project, maar bovenal een goede vriend.
Je hebt het project bedacht en uitgeschreven. Onze eerste kennismaking was in 2002 toen ik me
meldde bij de toenmalige afdeling Huisartsgeneeskunde (HAG) van het UMC St. Radboud. Ik
wilde mijn huisartsopleiding graag combineren met een onderzoek, het liefst een klinische trial,
over een duidelijk somatische aandoening. En jij kwam met een kwalitatief onderzoek naar
onverklaarde lichamelijke klachten! Hoe vaag en pseudowetenschappelijk wil je het hebben,
dacht ik toen nog. Toch besloot ik, hoewel jij dat niet verwacht had, toe te happen. Achteraf de
beste keus die ik had kunnen maken. Samen hebben we de ontdekkingreis door kwalitatief
onderzoek en onverklaarde klachten ondernomen. Het was prachtig! Mede door de frequente
koffiediscussies werd mij steeds helderder waar het echt om gaat bij patiënten met onverklaarde
klachten en daarmee in de huisartsgeneeskunde. De persoonlijke zorg die jij aan je patiënten
geeft, geef je ook aan je promovendi. Je bent een groot voorbeeld voor mij.
Chris van W eel. Beste Chris, ik ben enorm trots dat je mijn promotor bent. Hoewel je veel in het
buitenland was, heb je mijn vorderingen in onderzoeksland van dichtbij gadegeslagen. Je vaak
subtiele commentaren op mijn stukken waren heerlijk om te verwerken. De stukken werden er
zienderogen beter van. Altijd had je oog voor de kern van het huisartsenvak die door moest
klinken in wat ik schreef. Ik heb er graag gebruik van gemaakt. Net als van je formidabele
internationale netwerk. Daar kreeg ik pas echt goed zicht op tijdens de WONCA World en de
NAPCRG annual meeting in 2004 in Orlando, Florida. De manier waarop je mij gevraagd en
ongevraagd voorstelde aan en in contact bracht met al die internationaal bekende
Dankwoord | 237
huisartsonderzoekers heb ik als een groot voorrecht ervaren. Ik raad alle jonge
huisartsonderzoekers op de afdeling aan nu het nog kan, gretig gebruik te maken van je
naamsbekendheid en enorme internationale netwerk.
Eric van Rijsw ijk. Eric, ik ben erg blij dat je mijn tweede copromotor bent. In de tijd dat ik begon
op de afdeling was jij bezig met de afronding van je eigen proefschrift. Ondertussen heb je een
geheel eigen onderzoekslijn palliatieve zorg opgebouwd. De enorme snelheid waarmee je dat
doet vind ik bewonderenswaardig. Het samen stukken schrijven, medisch studenten
begeleiden en natuurlijk de gezellige congresbezoeken maakten mijn promotietraject tot een
feest.
Lieke H assink-Franke. Onderzoeksmaatje! We begonnen ongeveer gelijktijdig met ons traject
en zaten jaren op dezelfde kamer. In Orlando sliepen we zelfs op dezelfde kamer (schuld van
Twanny!). Wat is het heerlijk om met iemand met zoveel positieve energie en enthousiasme te
mogen samenwerken. We hebben onze ganggenoten vaak gestoord met ons harde gelach. En
dat zal de komende tijd nog wel zo blijven, want we zullen de komende jaren samen de NMP-kar
gaan trekken. Lieke, ik ben ontzettend blij dat je mijn paranimf wilt zijn.
Evelyn van W eel - B aum garten. Beste Evelyn, samen met Peter, Eric en Lieke hebben we op
menig internationaal congres ons GGZ gedachtegoed gepresenteerd en verder uitgewerkt.
Presentaties, workshops, forums en posters, niets was je te gek. Veelal zat jij deze bijeenkomsten
op een interactieve en levendige manier voor. Je onderwijsachtergrond kwam daar geweldig bij
van pas. Door jouw Mental Health netwerk ontstonden er internationale samenwerkings­
verbanden en hebben we de GGZ onderzoekslijn internationaal op de kaart kunnen zetten. De
aanwezigheid van Chris Dowrick in mijn manuscriptcommissie heb ik daarmee vooral aan jou
te danken.
M ark van der W el. Mark, ik weet niet of je verwacht had dat ik je zo prominent in mijn
dankwoord zou noemen. Toch doe ik het. De laatste jaren zijn we, tot mijn grote plezier, steeds
intensiever gaan samenwerken. Je scherpzinnigheid, doorvragen en immer kritische blik
dwingen me vaak tot nadenken. Onze trip naar Japan (we konden niet eens languit liggen in de
business class), de hot tub op Vancouver Island (gelukkig hadden we bier en rendiersnacks) en
de dance events tijdens de NAPCRG (wij sprongen het hoogst) waren hoogtepunten naast het
harde werken wat we daar deden. Ik hoop, en ga er van uit, dat we nog veel meer zullen gaan
samenwerken in de toekomst.
Huub M eijerink. Amice, vriend van het eerste uur, paranimf. We ontmoetten elkaar in de
collegezaal in Rotterdam, september 1995, en zijn daarna samen opgetrokken in het medische
wereldje. Van studie naar co-schap, van basisarts tot specialist, van Rotterdam naar Nijmegen,
van doctorandus naar doctor. Hoe moet dat nou nu jij naar Heerenveen vertrekt om daar als
orthopeed te gaan werken? Graag een huis met aanlegsteiger en een boot, dan komen wij wel
logeren!
De huisartsgeneeskunde leer je niet vanuit boeken, leer je niet vanuit onderzoek, maar leer je
eigenlijk alleen maar door het dagelijks in praktijk te brengen:
H uisartsopleiding N ijm egen (VOHA). Ben Bottema bedankt voor het faciliteren van mijn
gecombineerde onderzoeks- en opleidingstraject. Rudy en Marijke Kleerekooper-Corsten,
bedankt dat ik mijn eerste huisartsopleidingsjaar bij jullie in Elst heb mogen doen. De gezellige
diensten zonder huisartsenpost (!) en met macaroni (van Leonard) in m'n haar zal ik niet snel
vergeten. Jaap Schreuder, mijn derdejaars opleider in Malden, bedankt dat je mij een kijkje in de
keuken van het lokale, regionale en landelijke bestuur van de huisartsgeneeskunde hebt
gegeven. Destijds in de huisartsopleiding een ondergeschoven kindje, maar voor mij, dankzij
j ou, een enorme aanvulling op mijn opleiding.
H uisartspraktijk M esker-N iesten. Jeanne en Pierre, bij jullie kwam ik als net afgestudeerde
huisarts om als waarnemer ervaring op te doen. Eigenlijk heb ik bij jullie een vervolgopleiding in
de kernwaarden van de huisartsgeneeskunde gekregen. Elke woensdag aan het eind van de
middag een patiëntenbespreking met veel discussies over onverklaarde klachten,
contextgeneeskunde en persoonlijke patiëntenzorg. Door de vier jaar die ik bij en met jullie heb
gewerkt ben ik een andere en ik denk veel betere huisarts geworden. Ik vind jullie een groot
voorbeeld voor de nieuwe generatie huisartsen.
H u isa rtsp ra k tijk
O o ste rh o u t.
Collega huisartsen Charles en Erna, Han en Inge,
doktersassistentes Marije, Karin, Audry, Hanneke en Laura, praktijkondersteuners Dyan, Ada
en Miep en financieel medewerker Lydia, wat een geweldig team hebben wij toch in Oosterhout.
Een heerlijke werksfeer waar iedereen zichzelf kan zijn en waar veel wordt gelachen. Het is voor
mij een groot voorrecht om deel uit te maken van dat team. Wat ben ik blij dat ik in Oosterhout
terecht ben gekomen. Annemarie Uijen, jij bent de enige vrouw (naast Marjolein) met wie ik een
contract heb. Ik ben ontzettend blij dat we samen onze praktijk en patiëntenzorg vorm kunnen
geven. Je energie en spontaniteit werken erg aanstekelijk. Wat ben ik blij dat jij in Oosterhout
terecht bent gekomen.
Patiënten en huisartsen. Op deze plek wil ik alle patiënten en huisartsen hartelijk bedanken die
hebben meegewerkt aan dit onderzoek door deel te nemen aan de focus groep discussies, diepte
interviews en video consulten. Zonder hen was er geen onderzoek en dus geen proefschrift.
Dankwoord | 239
Mijn speciale dank gaat uit naar de CMR artsen die hun praktijken openstelden voor mijn
onderzoek naar patiënten met 1359-3.
Hoewel je de huisartsgeneeskunde niet leert vanuit onderzoek, denk ik wel dat ik een betere
huisarts ben geworden door mijn onderzoek:
C oauteurs. Eloy van de Lisdonk, Hans Bor, Machteld Borghuis, Floris van de Laar, Anne
Speckens, Juke Nijenhuis, Karel van Spaendonck, Sandra van Dulmen, Mieke Heijmans, Janine
van Ravenzwaaij en Rhona Eveleigh bedankt voor de meer dan prettige samenwerking bij het
opzetten, analyseren en schrijven van onze artikelen.
Chris D ow rick. Dear Chris, we met for the first time in the reggae pub in Universal Studios in
Orlando, Florida. I was familiar with your name from your research papers on MUS. Together
with T ony Kendrick, Saskia Zandstra, Lieke Hassink-Franke and Peter Lucassen we danced the
whole night and drunk lots of beer. After that event we met on almost all WON CA and N APCRG
meetings. Our collaboration in the workshops, forums and papers was great. Your view on MUS
and mental health was of great importance for my thesis. Thank you for participating in the
assessment of my thesis. I hope we can work with you and your department even more closely in
the near future.
Oud redactieleden H& W . Als jonge huisartsonderzoeker trad ik toe tot de redactie van Huisarts
en Wetenschap, de leukste commissie in huisartsenland die er bestaat. Ik heb ontzettend veel
van jullie geleerd: van het schrijven van stukken tot het netjes opstellen van herschrijfbrieven,
van kritisch lezen tot het eten van kledderige broodjes. Joost Zaat, bedankt voor je kundige en
kritische begeleiding tijdens deze periode. Jij hebt me leren schrijven. Ik vind het een grote eer
dat je vandaag plaats neemt in mijn corona.
M arjolein B erger. Bij jou deed ik mijn eerste onderzoekservaring op tijdens mijn
afstudeeronderzoek op de afdeling huisartsgeneeskunde in Rotterdam. Jij liet me zien hoe leuk
en intrigerend, maar ook hoe ingewikkeld het doen van onderzoek is. Toen Peter met z'n idee
over kwalitatief onderzoek bij onverklaarde klachten kwam, adviseerde jij mij om die uitdaging
aan te gaan. Met Peter als begeleider zou het immers altijd goed komen, zo verzekerde jij mij.
Marjolein, dat was het beste advies dat je me kon geven. Ik ben daarom ook ontzettend trots dat
je als kersverse hoogleraar huisartsgeneeskunde zitting hebt in mijn corona.
R ichtlijncom m issies. Henriette van der Horst, Ingrid Arnold en Nettie Blankenstein, ik heb
zelden drie zo daadkrachtige dames gezien die het huisartsgeneeskundige gedachtegoed tot op
het bot verdedigen en uitdragen. Ik heb genoten van de scherpe discussies tijdens de
240
multidisciplinaire richtlijn vergaderingen en de NHG standaarden werkgroep over SOLK.
Maar bovenal zijn jullie gewoon drie heel plezierige mensen om mee samen te werken.
Secretariaat ELG. Twanny Jeijsman, Caroline Roos en Tilly Pouwels, jullie zijn de ruggengraat
van de onderzoeksafdeling ELG. Het secretariaat is altijd een heerlijke plek om even bij te
kletsen, uit te blazen of praktische zaken te regelen. Ik ben altijd weer verbaasd over jullie
enthousiasme en snelheid. Ontzettend bedankt voor alles.
K am ergenoten. Vorig jaar moest er plots verhuisd worden. Maakten Lieke en ik dan zoveel
lawaai? Met twee psychiaters in opleiding, Hiske van Ravesteijn en Inge van Dijk, kreeg de
kamer een extra dimensie. En de gezelligheid was gewaarborgd. Lea Peters, onze
onderzoeksassistente, jij bent echt van alle markten thuis. In je vakantie bedacht je dat mijn
proefschrift een QR-code moest hebben. Briljant idee! Daarnaast ben jij de continuïteit van zorg
(hoe huisartsgeneeskundig is dat!) op onze kamer. Je attente houding en aandacht voor iedereen
op de kamer en de gang is de smeerolie voor onze fijne samenwerking.
Persoonlijke patiëntenzorg als huisarts en drukke academische bezigheden als huisartsonderzoeker zijn eigenlijk alleen maar mogelijk vanuit een stevig fundament van vrienden,
buren, familie en thuisfront:
V rienden. Het zijn er teveel om allemaal persoonlijk bij naam te noemen. Met een
k am erad en g roep
u it T u bberg en
(nog v an u it m ijn m id d elb are sch o o ltijd ), een
vriendinnengroep uit Enter (vanuit de middelbare schooltijd van Marjolein) en een
vriendenkring uit Nijmegen (opgebouwd sinds we in Nijmegen zijn komen wonen) voel ik met
schatrijk. Door alle kinderen die er de afgelopen jaren zijn geboren is ons aantal bijna
verdubbeld. Ons huis wordt zo langzamerhand te klein voor het vieren van de verjaardagen.
Bedankt voor alle gezelligheid!
In heb bijzonder wil ik op deze plaats Joost Perik bedanken. Gekscherend heb ik al eens
geroepen dat ik je net zo goed in dienst kon nemen. Joost, jij hebt de hele lay-out en ontwerp van
mijn proefschrift vorm gegeven. Deze fantastische vormgeving komt volledig op jouw conto.
Onwijs bedankt!
Buren. Buren van de Vossenlaan, we zeggen zo vaak, beter een goede buur dan een verre vriend !
En zo is het ook echt. Wat is het toch heerlijk om in zo'n fijn buurtje te wonen. Even een praatje,
even een kop koffie, even een voetbalwedstrijd (fijn te merken dat FC Twente ook in jullie hart
een warm plekje heeft gekregen) en ondertussen de nodige biertjes en wijntjes. Ik geniet elke dag
van jullie fijne betrokkenheid bij ons gezin.
Dankwoord | 241
Fam ilie. Coen mijn tweelingbroer (en natuurlijk Anne Marije), Frank mijn kleine broertje (en
natuurlijk Martine), niemand van ons is in Tubbergen gebleven. We zijn alle drie een andere
richting op gegaan. Amstelveen, Utrecht en Nijmegen. Chartaal geld, pensioenen en
geneeskunde. En eigenlijk maakt dat onze band alleen maar sterker. Dank, dat jullie er altijd
gewoon zijn.
Schoonzus Annemarie, ik ken je al vanaf je 10de jaar. Zo oud was je toen ik voor het eerst bij jullie
over de vloer kwam. Inmiddels zijn er vele jaren verstreken, maar je bent nog steeds m'n kleine
schoonzusje. Je altij d goede humeur en gezelligheid maken je frequente bezoekjes aan Nijmegen
altijd erg speciaal.
Ben en Hermien Hofsté, jullie gastvrijheid in Almelo heb ik altijd als iets heel bijzonders ervaren.
In mijn studententijd stond er vrijdagavond altijd een bord eten en gezelligheid op me te
wachten. De ritjes naar Tubbergen en naar de trein waren jullie nooit teveel. Jullie oprechte
interesse in wat ik daar toch allemaal op de universiteit aan het doen was, heeft me altijd veel
goed gedaan.
Pa en ma, veel van wat ik heb bereikt heb ik aan jullie te danken. Jullie lieten me studeren,
stimuleerden me om buiten Twente te kijken (achter Almelo wordt immers ook brood
gebakken) en lieten me vrij in de keuzes die ik maakte. Resultaat is wel dat jullie nu een eind
moeten rijden om de kleinkinderen te zien opgroeien. Mede door jullie steun en vertrouwen sta
ik vanmiddag hier mijn proefschrift te verdedigen en heb ik me kunnen ontwikkelen tot degene
die ik nu ben. Bedankt dat jullie steeds voor ons klaar staan!
H et thuisfront. Lieve Marjolein, wat begon met brommers kiek'n aan de Benninksweg in
Reutum (bie Bais) duurt nog altijd voort. Ik ben blij dat ik bij alle belangrijke stappen en keuzes in
ons leven kan terugvallen op jou. Door je evenwichtigheid, mensenkennis en altijd goede
humeur kunnen we samen de hele wereld aan. Bedankt voor je ongelofelijke grote steun,
vertrouwen en liefde. Op naar een geweldige toekomst sam en........
Lieve Jop en Guus, in jullie kleine leventjes zijn jullie vooral bezig met eten, spelen en slapen.
Later als jullie groot zijn zal ik jullie alles vertellen over deze mooie dag. Jullie vrolijke lach en
gebrabbel maakt mijn leven compleet.
Marjolein, Jop en Guus, ik kijk nu al uit naar alle mooie momenten die nog gaan komen!
244
List of publications
Medically unexplained symptoms
Chronic functional somatic symptoms: a single syndrome?
olde Hartman T C , Lucassen PLBJ, van de Lisdonk EH, Bor HHJ, van W eel C.
Br JG en Pract. 2004;54:922-927
[Chronic functional complaints: A syndrome?]. Chronisch functionele klachten: één enkel syndroom?
olde Hartman TC, Lucassen PLBJ, van de Lisdonk EH, Bor HHJ, van Weel C.
Huisarts Wet. 2005;48(9):443-8
[Unexplained physical symptoms: a widespread problem but still low-profile in training programs and guidelines].
Onverklaarde lichamelijke klachten: een omvangrijk probleem, maar nog weinig zichtbaar in opleiding en richtlijnen.
olde Hartman TC, Poels PJP, van W eel-Baumgarten E, Lucassen PLBJ.
Ned Tijdschr Geneeskd. 2006;150(23):1318
Comment on 'Pain patients in a randomized trial did not show a significant effect of a positive consultation' by Knipschild
and Arntz.
Lucassen P, van Rijswijk E, olde Hartman TC, Borghuis M.
J Clin Epidemiol. 2006;59(8):868; author reply 868-9
Comment on 'Effectiveness of a time-limited cognitive behavior therapy-type intervention among primary care patients
with medically unexplained symptoms' by Escobar et al.
olde Hartman TC, Franke L, Lucassen P, van W eel-Baumgarten E.
Ann Fam Med. 2007; author reply
[Somatic fixation. New life for an old concept]. Somatische fixatie. Een nieuw leven voor een oud begrip.
Lucassen P, olde Hartman T, Borghuis M.
Huisarts Wet. 2007;50:11-15
[Somatic fixation. Reply]. Somatische fixatie. Reactie op ingezonden brief.
Lucassen P, olde Hartman T, Borghuis M.
Huisarts Wet. 2007;50:124
Reattribution for medically unexplained symptoms.
Van Ravesteijn HJ, Lucassen PLBJ, olde Hartman T C .
Br J Psychiatry. 2008;192:314-5
Comment on 'management of depression in adults' by Timonen M and Liukkonen T.
Van Ravesteijn H, Franke L, olde Hartman TC, Lucassen P.
BMJ. 2008; electronic letter
Medically unexplained symptoms in family medicine: defining a research agenda. Proceedings from WONCA 2007.
olde Hartman TC, Franke LJA, Dowrick C, Fortes S, Lam C, van der Horst H, Lucassen PLBJ, van Weel-Baumgarten E.
Fam Pract. 2008 Aug;25(4):266-71
Mental health problems and the presentation of minor illnesses: data from a 30-year follow-up in general practice.
olde Hartman TC, van Rijswijk E, van Ravesteijn H, Franke LJA, Bor H, van Weel-Baumgarten EM, Lucassen PLBJ.
Eur J Gen Pract. 2008;14 suppl 1:38-43
List o f publications | 245
Prognostic factors of medically unexplained symptoms, somatoform disorders and hypochondriasis: a systematic review
of prospective studies.
olde Hartman T C , Borghuis MS, van de Laar F, Lucassen PLBJ, Speckens A, van Weel C. J
Psychosom Res. 2009;66(5):363-77
"W ell doctor, it is all about how life is lived" : cues as a tool in the medical consultation.
olde Hartman T C , van Ravesteijn H.
Mental Health in Family Medicine 2008;5(3):183-7
Explanation and relations. How do general practitioners deal with patients with persistent medically unexplained
symptoms: a focus group study.
olde Hartman T C , Franke L, Lucassen PLBJ,van Spaendonck K, van Weel C.
BMC fam ily practice 2009;10:68
Problem-solving treatment in general practice residency: a focus group study of registrars' views.
Hassink-Franke L, olde Hartman T C , Beek M, van Weel C, Lucassen P, van Weel-Baumgarten E.
Patient Educ Couns. 2010 Sep 8. [E-pub ahead o f print]
Explanatory models of medically unexplained symptoms: a qualitative analysis of the literature.
Van Ravenzwaay J, olde Hartman T C , van Ravesteijn H, van Rijswijk E, Lucassen P.
M ental Health in Family Medicine 2010;7:223-31
The reassuring value of diagnostic tests: a systematic review.
van Ravesteijn H, van Dijk I, Darmon D, van de Laar F, Lucassen P, Olde Hartman T , van Weel C, Speckens A.
Patient Educ Couns. 2011, M ar 5. [E-pub ahead o f print]
Experts' opinions on the management of medically unexplained symptoms in primary care. A qualitative analysis of
narrative reviews and scientific editorials.
Heijmans M, olde Hartman T C , van W eel-Baumgarten E, Dowrick C, Lucassen P, van Weel C.
Fam Pract. 2011;28(4) :444-455
How patients and fam ily physicians communicate about persistent medically unexplained symptoms. A qualitative study
of video-recorded consultations.
Olde Hartman T C , van Rijswijk E, van Dulmen S, van Weel-Baumgarten E, Lucassen P, van Weel C.
Patient Educ Couns. 2011, A pr 7. [E-pub ahead o f print]
Do unexplained symptoms predict anxiety or depression? Ten-year follow-up data of from a practice-based research
network
Van Boven C, Lucassen P, van Ravesteijn H, olde Hartman T C , Bor H, van Weel-Baumgarten E, van Weel C.
Br J Gen Pract. 2011;61(587):316-25
Patients' reason for visit matter and should be a basis to value and analyse outcome of care.
olde Hartman T C , van Ravesteijn H, Lucassen P, van Boven K, van Weel-Baumgarten E, van W eel C.
Br J Gen Pract. 2011, in press
The doctor-patient relationship from the perspective of patients with persistent medically unexplained symptoms.
olde Hartman TC, van Ravesteijn H, Nijenhuis J, Lucassen P, van Weel C.
Submitted
246
W hat we talk about when we talk about depression: doctor-patient conversations and treatment decision outcome.
Karasz A, Dowrick C, Byng R, Buszewicz M, Ferri L, olde Hartman T , van Dulmen S, Van Weel-Baumgarten E, Reeve J.
Submitted
GPs' challenges in the management of patients w ith medically unexplained symptoms in Poland: A focus group-based
study.
Czachowski S, Piszczek E, Sowiñska A, olde Hartman T C .
Fam Pract. 2011, in press
Combining residency and research
[GP trainees and science - A difficult combination]. Haio's en de wetenschap, een moeilijke combinatie.
olde Hartman TC.
Huisarts Wet. 2004;47(8):362-363
Becoming a research-oriented family physician.
olde Hartman TC, Franke LJA, Borghuis MS, Lucassen PLBJ.
Fam Med. 2005;37(10):686-7
Family physicians' training program are useful for surgeons.
Poels PJP, olde Hartman T C , van W eel C.
Arch Surg. 2006;141(5):515
Toward a research-oriented culture in primary care. Rapid response to 'primary care research networks in the United
Kingdom' by F.Sullivan, C.Butler, M.Cupples, A.Kinmonth.
Franke LJA, olde Hartman T .C .
BMJ. 2007; rapid response
Combining vocational and research training.
olde Hartman TC, Poels PJP, Licht-Strunk E, van Weel C.
A ust Fam Physician. 2008;37(6):486-8.
Asthma/COPD
GP's attitudes to discussing prognosis in severe COPD: an Auckland (NZ) to london (UK) comparison.
Poels PJP, olde Hartman T C , Schermer TR, van Weel C.
Fam Pract. 2005 (31 October), e-letter
Influence of Spirometry on Patient Management in diagnostic studies unknown.
Poels PJP, olde Hartman T C , Schermer TR, Alberts M, van Weel C.
Chest. 2006;129(6):1733-4; author reply 1734
Qualitative studies to explore barriers to spirometry use: a breath of fresh air?
Poels PJP, olde Hartman T C , Schermer TR, van Weel C.
Respir Care. 2006;51(7):768
List o f publications | 247
Dermatology
Fungal nail infection.
olde Hartman T C , van Rijswijk E.
BMJ. 2008;337:a429
[The practice guideline 'Bacterial skin infections' (first revision) from the Dutch College of General Practitioners; a response
from the perspective of general practice]. De standaard 'Bacteriële huidinfecties' (eerste herziening) van het Nederlands
Huisartsen Genootschap; reactie vanuit de huisartsgeneeskunde.
olde Hartman TC, Uijen AA.
Ned.Tijdsch.Geneeskd. 2008;152:1602-3
Schim m elnagels.
E. van Rijswijk, T. olde Hartm an.
Huisarts Wet. 2009;52(3): 151
Onychomycosis.
Olde Hartman TC, van Rijswijk E.
Praxis (Bern 1994) 2009;98(4):213-4
Schimmelnagels.
E. van Rijswijk, T. olde Hartm an.
Tijdschr. Praktijkonderst. 2010;3:82-83
Gallbladder stones
Abdominal symptoms, do they disappear after cholecystectomy? A systematic literature review and a controlled
prospective study.
Berger MY, olde Hartman TC, van der Velden JJIM.
In dissertatie Berger MY: The clinical value ofabdom inal symptoms and sonography in gallstone disease; 38-51
Food intolerance not related to gallstones.
Berger MY, olde Hartman T C .
J Clin Gastroenterol. 1999;30(1):101-102
Abdominal symptoms do they disappear after cholecystectomy?
Berger MY, olde Hartman TC, Bohnen AM.
Surg Endosc. 2003;17(11):1723-8
Is 'biliary pain' exclusively related to gallbladder stones? A controlled prospective study.
Berger MY, olde H artman TC, van der Velden JJIM, Bohnen AM.
Br J Gen Pract. 2004;54(505):574-9
Other
W ishfull pharmaceutical thinking.
olde Hartman TC, van Rijswijk E, Lucassen PLBJ.
Br J Gen Pract. 2003;53(497):970
248
[New job responsibilities for general practitioners]. T atatata, een nieuw takenpakket.
olde Hartman T C , Zaat J.
Huisarts Wet. 2004;47(1):6-8
[A role for calcium glubionate injections in the treatment of solar urticaria? A case report: Be careful w ith the interpretation].
Een case-report: pas op met de interpretatie.
olde Hartman T C .
Huisarts Wet. 2005;48(8):419
[Topical NSAIDs in the treatment of arthrosis: A clinical lesson]. 'Dokter, ik heb het niet zo op pillen'. Topische NSAID's bij
artrose, een klinische les.
Dost MM, olde Hartman T C .
Huisarts Wet. 2005;48(5):236-9
[The importance of sexual problems during the use of antidepressants has been confirmed; reply]. Belang seksuele
problemen bij het gebruik van antidepressiva bevestigd.
olde Hartman T C .
Huisarts Wet. 2005; 48(12): 638-639
The paradox of specialization. Track discussion to Stange KC, Ferrer RL. The paradox of primary care. Ann Fam Med.
2009;7:293-99
van Weel C, olde Hartman T C .
Ann Fam Med. 2009 (28 July).
Course and prognosis of M yastenia Gravis. A systematic review.
Zhi-feng Mao, Xue-an Mo, Chao Qin, Yong-rong Lai, olde Hartman T C .
Eur J Neurol. 2010;17(7):913-21
Book(chapter)
[Qualitative research in medical practice]. Kwalitatief onderzoek in de medische praktijk.
Lucassen PLBJ, olde Hartman TC (eds).
ISBN 9789031349982.
Verschenen op 14 juni 2007.
Type: boek (160 pagina's).
Bohn Stafleu en Van Loghum, Utrecht 2007
'Dokter, ik heb het niet zo op pillen'. Topische NSAID's bij artrose, een klinische les.
Dost MM, olde Hartman T C .
In: Een bedrieglijke bijbal en 22 andere klinische lessen uit Huisarts en Wetenschap.
Editor G.A. van Essen.
Bohn Stafleu en Van Loghum, Utrecht 2007
List o f publications | 249
Abstracts
Medically unexplained symptoms
Chronic functional somatic symptoms: a single syndrome?
olde Hartman T C , Lucassen PLBJ, van de Lisdonk EH, Bor HJH, van Weel C.
Poster presentation.
European Organization o f National Colleges, Academies and Academic Associations o f General Practitioners/Family Physicians
(Wonca Europe2004), Amsterdam (NL)
Focus group studies in primary care.
Borkan J, Franke L, olde Hartman TC, van de Lisdonk E, Lucassen P, van Rijswijk E, van Weel-Baumgarten E.
Workshop.
World Organization o f National Colleges, Academies and Academic Associations o f General Practitioners/Family Physicians (Wonca
W orld2004), Orlando (USA)
Chronic functional somatic symptoms. W hy are they a burden to fam ily practitioners?
Olde Hartman TC, Franke L, Lucassen P, van Spaendonck K, van de Lisdonk E, van Weel C.
Poster presentation.
North American Primary Research Group (NAPCRG) 2005, Quebec City (Canada)
Chronic functional somatic symptoms: an international GP perspective.
Olde Hartman TC, Lucassen P, van Rijswijk E.
Workshop.
European Organization o f National Colleges, Academies and Academic Associations o f General Practitioners/Family Physicians
(Wonca Europe2006), Florence (Italy).
Medically Unexplained Symptoms in primary care: the state of the art.
Olde Hartman TC, Lucassen PLBJ, van W eel-Baumgarten E, Franke LJA.
Symposium.
European Organization o f National Colleges, Academies and Academic Associations o f General Practitioners/Family Physicians
(Wonca W orld2007), Singapore
Medically Unexplained Symptoms in primary care: where should we go.
Olde Hartman TC, Lucassen PLBJ, van W eel-Baumgarten E, Franke LJA.
Workshop.
European Organization o f National Colleges, Academies and Academic Associations o f General Practitioners/Family Physicians
(Wonca W orld 2007), Singapore
Medically unexplained symptoms, somatization and hypochondriasis: course and prognosis. A systematic review.
Olde Hartman TC, Borghuis M, van de Laar F, Lucassen PLBJ, Speckens AE, van Weel C. Poster presentation.
North American Primary Care Research Group (NAPCRG), annual meeting 2007, Vancouver (Canada)
[Mental health problems and the presentation of minor illnesses]. Kleine kwalen bij patiënten met een depressie of
chronisch onverklaarde lichamelijke klachten.
Olde Hartman TC, van Rijswijk E, Franke LJA, Bor H, van Weel-Baumgarten EM, Lucassen PLBJ.
Oral presentation
Jubileumsymposium CMR NMP 'omzien en vooruitkijken', UMC St. Radboud 2007, Nijmegen (The Netherlands)
250
Problematic communication with patients with medically unexplained symptoms.
O lde Hartman T C , van Rijswijk E, van Dulmen S, Lucassen P, Schellevis F, van Weel C. Poster presentation.
North American Primary Care Research Group (NAPCRG), annual meeting 2008, Puerto Rico (USA)
Medically unexplained symptoms (MUS) in fam ily medicine: towards consensus on the management of MUS.
Olde Hartman T C , Dowrick C, van W eel-Baumgarten E, Lucassen P, van Ravesteijn H, Rask M, Rosendal M, Olesen F,
Fortes S.
Workshop.
World Organization o f National Colleges, Academies and Academic Associations o f General Practitioners/Family Physicians (Wonca
W orld2010), Cancun (Mexico)
Medically unexplained symptoms (MUS) in fam ily medicine: the state of the art.
Olde Hartman T C , Dowrick C, van W eel-Baumgarten E, Lucassen P, van Ravesteijn H, Rask M, Rosendal M, Olesen F,
Fortes S.
Symposium.
European Organization o f National Colleges, Academies and Academic Associations o f General Practitioners/Family Physicians
(Wonca World 2010), Cancun (Mexico)
Combining residency and research
[Scientific publishing for GP registrars]. W etenschappelijk publiceren voor huisartsen-in-opleiding
Olde Hartman T C , Zaat JOM.
Cursus (in cooperation with language institute Vrije Universiteit Amsterdam).
Nederlands Huisarts Genootschap 2005, Utrecht (The Netherlands)
AIOTHO's: bedreigde diersoort of succesverhaal.
olde Hartman T C , Licht-Strunk E, Schellinghout J.
Workshop.
NHG w etenschapsdag2008, Rotterdam (TheNetherlands)
Combining FP residency and PhD programs, the start of future international initiatives.
olde Hartman T C , Miedema B, Kendrick T, Bell Brown J, Falloon K, Goodyear-Smith F, Gunn J, Dowrick C, Aroll B, Licht­
Strunk E, van W eel C.
Breakfast meeting.
North American Primary Care Research Group (NAPCRG), annual meeting 2008, Puerto Rico (USA)
Combining vocational and research training.
olde Hartman T C .
Oral presentation.
LOVAH congres 2009, Utrecht (The Netherlands)
Combining vocational and research training in primary care.
van der W el M, olde H artman T C , Rosser W, van W eel C. W orksho p.
Workshop.
European Organization o f National Colleges, Academies and Academic Associations o f General Practitioners/Family Physicians
(Wonca Europe 2009), Basel (Switzerland)
Combining vocational and research training: Building research capacity and leadership in primary care.
olde H artman T C , van der W el M, Falloon K, van Weel C, Kendrick T, Belle Brown J, Aroll B, Dowrick C, Miedema B, G unn J .
Forum.
North American Primary Care Research Group (NAPCRG), annual meeting 2009, Montreal (Canada)
List o f publications | 251
Research - what is research and how do I get started?
Harris N, olde Hartman T C .
Workshop.
World Organization o f National Colleges, Academies and Academic Associations o f General Practitioners/Family Physicians (Wonca
W orld2010), Cancun (Mexico)
254
Curriculum Vitae | 255
Curriculum V itae
Tim Christian olde Harman was born on March 13th 1977 in Almelo (The Netherlands) as son of Gerrit olde
Hartman and Annie olde Hartman-Droste. He grew up with his twin brother Coen and brother Frank in
Tubbergen. He completed his high school (VWO) in 1995 at the Pius X College in Almelo and was allowed to
enter medical school at the Erasmus University Rotterdam in the same year. In 1999 he conducted a research
elective at the department of general practice at the Erasmus Medical Centre Rotterdam, supervised by Dr.
Marjolein Berger. During this period his enthusiasm for scientific research and general practice increased.
He graduated as a medical doctor (cum laude) in 2001 and started to work at the department of Emergency
Medicine in hospital Zevenaar. In 2002 he started his PhD project on persistent medically unexplained
symptoms in primary care at the department of primary and community care at the Radboud University
Nijmegen Medical Centre. The results of this project are described in this thesis. At the same time he started
general practice (GP) residency training at the Radboud University Nijmegen Medical Centre in order to
combine research with vocational training (the combined residency and research training programme 'AIOTHO-programme'). He worked as GP resident in the practices of Rudy and Marijke KleerekooperCorsten (Elst, Gelderland) and Jaap Schreuder (Malden). During this period he was member of the editorial
board of the Journal of the Dutch college of General Practitioners (Huisarts en Wetenschap) and member of
the PhD Student Training Committee (PTC) of the Netherlands School of Primary Care Research (CaRe). In
2005 he finished GP training and started to work as GP in the practice of Jeanne and Pierre Mesker-Niesten.
He became member of the editorial board of the international peer-reviewed journal Mental Health in
Family Medicine and participated in the national multidisciplinary guideline committee on medically
unexplained symptoms and somatoform disorders. In 2007 he started his own private practice in
Oosterhout (Nijmegen) in the academic health care centre Oosterhout supported by the other practicing GPs
in Oosterhout (Charles Verhoeff, Erna van Ewijk-van der Wielen, Han Beekwilder and Inge NobachtWagenvoort). In 2010 he continued his academic practice in close collaboration with Annemarie Uijen.
In recent years he, together with Greg Irving (UK), Karen Falloon (New Zealand) and Mark van der W el (The
Netherlands), founded the MINERVA (Montreal INitiative de Education et Recherche Vocationale
Academique) initiative, which aims at promoting combined residency and research training programs in
family medicine globally. Last year he became chair of the Nijmegen Monitoring Project (NMP) a practicebased research network recording the process and outcome of care of chronic diseases in general practice.
Furthermore he participates in the national GP guideline committee on medically unexplained symptoms of
the Dutch college of General Practitioners. After his PhD defence he will continue his research activities as a
post-doctoral researcher at the department of primary and community care at the Radboud University
Nijmegen Medical Centre.
Tim is happily married to Marjolein olde Hartman-Hofsté, who works as an oncology nurse at the
department of surgery of the Radboud University Nijmegen Medical Centre. They are the proud parents of
two sons, Jop (2009) and Guus (2010).