Identifying Medically Unexplained Symptoms among Frequent
advertisement

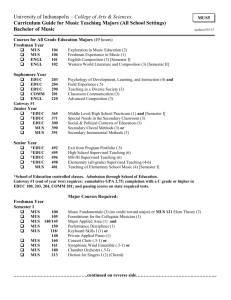
Identifying Medically Unexplained Symptoms among Frequent Attenders to the Emergency Department: Research to inform Service Design Dr Rebecca Jacob Consultant Psychiatrist and CLAHRC Fellow CPFT Dr Cecily Morrison, Research Associate, EDC, Engineering Dept, University of Cambridge Background MUS are defined as physical symptoms which are not or insufficiently explained by somatic disease. Symptoms include chest, abdominal, or back pain, tiredness, dizziness, headache, ankle swelling, shortness of breath, insomnia and numbness. Fink P, Toft T et al 2007, Nimnuan C, Hotopf M et al 2000 Functional Somatic Syndromes according to medical specialty Medical specialty Functional somatic syndromes Gastroenterology IBS Rheumatology Fibromyalgia, chronic back pain Cardiology Non cardiac chest pain Neurology Non-epileptic Seizures, tension headache ENT Globus syndrome Infectious Disease Chronic Fatigue Syndrome Psychiatry Somatoform, conversion disorders Henningsen P, Fink P et al 2011 Relationship between MUS and frequent attendance at ED Patients with MUS frequently attend primary and secondary care health services, including ED. Hotopf et al (2002) in cohort of 400 FA’s to the ED:17% had at least two medically unexplained consultation episodes, higher referrals to secondary care and > invasive tests. Older age patients also frequent attenders but research shows attendance often appropriate with Medically ‘Explained’ Symptoms. Aminzadeh F, Dalziel WB. 2002 ‘Frequent Attender’ Overt meaning numeric or statistical, and majority of studies suggest attendance at ED’s >4 times/year. More covert/pejorative meaning, refers to patients perceived by health professionals as taking up disproportionate amount of consultation time and/or burden on resources. Hodgson P, Smith P et al, 2005 CLAHRC Fellowship study of Frequent Attenders FA to the ED: proportionally on the increase. can be subdivided into Extreme FA (EFA) (>20) and Moderate FA (MFA) (<20/year). EFA’s had less urgent conditions, more mental health/alcohol problems, were less likely to be admitted (and are being targeted by ‘FACE’.) Wong M, Morrison C et al, 2011 Moderate Frequent Attenders Approximately 97% of FA population locally, had more cardiovascular problems, more often required admission. Abdominal complaints predominant presentation in those re-attending the ED within 7 days. Questions raised by this project Do MFA’s include those with MUS and are their service needs being met? Would designing a service improve the health outcomes and reduce health costs of this group? Will proposed RAID model encompass this patient group? Characterisation of FA’s and Service Evaluation Project Research Questions Amongst a sub-group of patients who frequently attend the ED (>4/year), how many suffer from MUS/mental disorders/both? What is their current service provision? What are low cost methods of identifying this patient group amongst FA’s to the emergency department? Study Design Setting: The emergency department at Addenbrooke’s hospital, CUHFT. Service design under the auspices of NIHR CLAHRC, (EDC) which has enabled a working relationship between CPFT and the University of Cambridge Methods: Stage 1 Characterisation of FA’s Case note review of 100 consecutive patients attending the ED >4 times in a period of 12 months. Demographics, No of ED attendances, clinical impression of MUS, invasive tests, OP visits, mental health diagnoses, service pathways and mental health input. Analysis considered proportion of FA’s with MUS/mental health, specialist mental health input, factors related to clinical impression of MUS, current service provision for MUS Method: Stage 2 Designing Service for MUS 1. 2. ED clinicians requested to give all FA’s attending the ED >4 times a year, two rating scales: Patient Health Questionnaire (PHQ15) Hospital Anxiety and Depression Scale (HADS) For each FA filling questionnaire case note review to be conducted. Stage 2: Planned Analysis The proportion of FA’s with mental health needs/MUS based on case note review Relationship between FA’s with clinical recognition of MUS and high PHQ scores Relationships between high HADS score and clinical recognition of depression and anxiety. Results will be used to inform service design Results: 100 FA’s attending ED Age range of sample 17-95 years 65% had mental health symptoms/disorders (mentioned in notes) 71% of this group (46/65) had both MUS and mental health problems. 15% of total sample had significant alcohol problems. Proportion of FA’s with MUS 45% had a clinical diagnosis of MUS Clinical dx by any specialist reporting Non-epileptic seizures, Chronic Fatigue, Fibromyalgia, IBS, MUS in medical notes Common symptoms related to ED presentation: abdominal pain, chest pain, SOB, back pain, dizziness. MUS and Age Mean Age of patients with MUS- 36.8/ Median 32 years. 87% (39/45) with MUS under 65 years MUS associated significantly younger age (p<0.001) but not with gender (>0.05) Older age more likely to have positive test results or medically ‘explained’ symptoms (p=0.004) MUS and Frequency of ED Attendance Number of ED attendances not significantly different for those with/out MUS (p>0.05) MUS were ‘MFAs’ as hypothesised, 36/45 were Moderate Frequent Attenders ( p<0.001) Service provision 41/45 patients with MUS (91%) had invasive tests/procedures requested by multiple specialities. All patients with MUS were seeing >1 OP speciality, average was 5 specialist clinics. 32/45 had MUS and MH symptoms (71%) 15/32 of those with both MUS/MH had specialist mental health input (47%). Only 4% (2/45) had specific psychiatric input for MUS Results: Service Design Only 4 forms returned ED busy environment, staff work shifts Administrative staff available; clinicians rarely, Staff ‘ drowning in paperwork’ Changes in ED’s physical structure during project ED one dept. however has multiple domains Staff spoke of frustration with FAs, keen to have service BUT research/service evaluation not a priority when clinical commitments are high. Case Vignette 1 35 year old man, married with 2 children, 9 ED attendances/year for back pain, SOB, chest pain No psychiatric history, ‘stress’ reported. Referred by ED /GP to Cardiology, Rheumatology, Medicine, Trauma Respiratory, Infectious Disease OPD’s Multiple tests: X-rays/ECHO/MRI unremarkable Dx: MUS suspected by Medicine, I D team report ‘post viral fatigue’, Cardiology ‘non-cardiac chest pain’. Case Vignette 2 91 yr. old widowed lady, 7 ED attendance /year for recurrent falls, UTI, often admitted. GP treating for anxiety with SSRI’s Referred by ED/GP to Geriatric Medicine, Gynecology, Dermatology, Rheumatology, General medicine Multiple tests: biopsy/MRI/ECHO/Chest X-ray Diagnoses: Squamous cell Carcinoma hand, polymyalgia, cerebrovascular disease, Giant cell arteritis, Ischemic Heart Disease, Hysterectomy (fibroids) Case Vignette 3 24 year old female, 13 ED attendances in the last year. ED and GP referred to Surgery, Ophthalmology, Hepatology, Gastroenterology Dx with Cholecystitis: cholecystectomy Invasive tests post surgery: US/OGD/Laparoscopy/Colonoscopy Postoperative ED visits with multiple medically unexplained symptoms, chest pain, abdominal pain, double vision, headache Gastroenterologist: Irritable Bowel Syndrome? Clinical Implications MUS is a common presentation amongst FA’s to the ED Multiple specialist clinic visits and multiple invasive tests in those with MUS, clinical and cost implications. Older age FA’s more often showed Medically Explained symptoms and appropriate use of ED, replicating other studies. Design Implications ED is a useful hub for identifying patients with MUS ED Clinicians alone are unlikely to be able to identify and signpost this patient group However involvement of primary/secondary care at the ED interface may be an ideal focus for service design. Designing service with an age focus may narrow down cohort Future studies Designing, delivering and evaluating the planned pathway of care for patients with MUS within the ED. Health economic study to estimate the cost savings of creating a service for patients with MUS, evaluating whether or not there is a tangible reduction in ED attendance. Challenges encountered Study plans had to be changed-and more than once! Whilst ED staff were enthusiastic about developing a service, they were not keen/able to be part of the service evaluation project i.e. distributing PHQ/HADS questionnaires to all FA’s Everything takes significantly more time than projected on the GANTT chart What I Learnt MUS: a heterogeneous group (with/out MH symptoms) posing a clinical and financial challenge for health services locally. The importance of robust data when planning service development Value of CLAHRC’s cross cutting themes (Psychiatry/EDC); provides different, objective perspectives. Acknowledgements Dr. Cecily Morrison, EDC, Dept of Engineering, University of Cambridge Dr. Peter Watson, Senior Statistician, MRC Cognition and Brain Sciences Unit, Cambridge Dr. Catherine Hayhurst, Consultant ED Physician, ED Dept, Addenbrooke’s Hospital Dr. Cathy Walsh, Consultant Psychiatrist, Dept of Liaison Psychiatry Professor Peter Jones, Dr.Belinda Lennox, Dr. Christine Hill: CLAHRC References 1. Fink P, Toft T et al .Symptoms and syndromes of bodily distress: An exploratory study of 978 internal medical, neurological, and primary care patients. Psychosomatic medicine 2007; 69:30-9 2. Nimnuan C, Hotopf M et al. Medically unexplained symptoms: how often and why are they missed? QJM Monthly Journal of the Associations of Physicians 2000;93 3. Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med. 2002;39:238-247. 6. Hodgson P, Smith P et al Stories from frequent attenders: Qualitative Study in Primary Care. Ann Fam Medicine 2005: 318-23 7. Wong W, Morrison C. A service design approach to frequent attendance in the ED. CLAHRC Fellowship Report, 2011.