Downloaded from UvA-DARE, the Institutional Repository of the University of Amsterdam (UvA)
http://dare.uva.nl/document/41972
File ID
Filename
41972
Karsdorp.pdf
SOURCE, OR PART OF THE FOLLOWING SOURCE:
Type
Dissertation
Title
Biased perception of heart symptons in patients with cogenital heart disease
Author
P.A. Karsdorp
Faculty
Faculty of Social and Behavioural Sciences
Year
2007
Pages
134
FULL BIBLIOGRAPHIC DETAILS:
http://dare.uva.nl/record/210182
Copyrights
It is not permitted to download or to forward/distribute the text or part of it without the consent of the copyright holder
(usually the author), other then for strictly personal, individual use.
UvA-DARE is a service provided by the Library of the University of Amsterdam (http://dare.uva.nl)
Biased perception of heart symptoms in patients
with congenital heart disease
ISBN-10: 90-9021440-2
ISBN-13: 978-90-9021440-5
Cover designed by Tamara M. Karsdorp, www.taam.nl
Printed by Print Partners Ipskamp, Amsterdam
Biased perception of heart symptoms in patients
with congenital heart disease
ACADEMISCH PROEFSCHRIFT
ter verkrijging van de graad van doctor
aan de Universiteit van Amsterdam
op gezag van de Rector Magnificus
prof. mr. P.F. van der Heijden
ten overstaan van een door het college voor promoties ingestelde
commissie, in het openbaar te verdedigen in de Aula der Universiteit
op donderdag 18 januari 2007, te 12:00 uur
door Petronella Anna Karsdorp
geboren te Amsterdam
Promotores:
prof. dr. M. Kindt
prof. dr. B.J.M. Mulder
Co-promotor: prof. dr. W.T.A.M. Everaerd
Faculteit der Maatschappij en Gedragswetenschappen
Financial support by the Netherlands Heart Foundation for the publication of this thesis is
gratefully acknowledged. The study described in this thesis was supported by a grant of
the Netherlands Heart Foundation (NHF-1999B38).
“If I only knew”, Hans Castorp went on, and laid his hands like a lover on his
heart, “if I only knew why I have palpitations the whole time…”
(Mann, 1927, the Magic Mountain, p. 103)
Contents
Chapter 1. General introduction
9
Chapter 2. Psychological and cognitive functioning in children and pre-adolescents
with congenital heart disease: a meta-analysis
25
Chapter 3. Heart symptoms induced by false heart rate feedback in high trait
anxious patients with congenital heart disease
49
Chapter 4. Stress-induced heart symptoms and perceptual biases in patients with
congenital heart disease
63
Chapter 5. Preattentive processing of heart cues and the perception of heart
symptoms in congenital heart disease.
77
Chapter 6. Interpretation bias for heart sensations in congenital heart disease and
its relation to quality of life
Chapter 7. General discussion
93
109
Nederlandse samenvatting (Summary in Dutch)
124
Dankwoord (Acknowledgements)
132
General introduction
10 Chapter 1
General introduction
Congenital heart disease (ConHD) is a term describing a wide spectrum of cardiac
abnormalities that are present at birth. Although in the Netherlands accurate statistics are
lacking, it is estimated that almost 1 % of newborns are born with some form of ConHD
(Warnes et al., 2001). With significant advances in the diagnosis and treatment of ConHD,
survival rates have improved remarkably. Nowadays more than 85% of the children with
complex ConHD survive beyond their first year of age as compared to 20% in the 40’s
(Warnes et al., 2001). As a result, a rather new patient group has emerged consisting of
adults with ConHD. With this new patient group, new questions have been raised
concerning their unique psychological needs. In the past fifteen years, several studies
investigated whether ConHD in adults is related to the development of psychopathology
and diminished quality of life.
A review of research in which mixed groups of patients with ConHD were
investigated suggests that adults with ConHD experience increased levels of overall
psychopathology, anxiety, and depression (Utens et al., 1998; Brandhagen, Feldt, &
Williams, 1991; Van Rijen et al., 2005b; Bromberg et al, 2003). Moreover, patients with
ConHD overall report increased levels of heart symptoms and a diminished quality of life
regarding general health and physical functioning (Lane, Lip, & Milane, 2002, Van Rijen
et al., 2005a; Hager & Hess, 2005; Moons et al., 2004; Rose et al., 2005; Jefferies,
Noonan, Keller, Wilson, & Griffith, 2004). Additionally, some studies show diminished
quality of life with respect to mental health, vitality, and daily functioning due to physical
health problems (Rose et al., 2005; Hager & Hess, 2005; Jefferies et al., 2004). The
findings with respect to perceived social functioning in ConHD are conflicting. Although
reduced social functioning has been reported (Hager & Hess, 2005), other studies revealed
no or even more favourable results among patients with ConHD (Rose et al., 2005;
Jefferies et al., 2004; Van Rijen et al., 2005a). Finally, no limitations have been observed
among patient with ConHD regarding bodily pain and daily functioning due to emotional
problems (Van Rijen et al., 2005a; Hager & Hess, 2005; Jefferies et al., 2004).
Overall these findings suggest that ConHD adversely affects patients’ psychological
functioning and quality of life, at least with respect to psychopathology and perceived
physical functioning and general health. However, little is known of the mechanisms by
which ConHD affects psychological adjustment and quality of life. The present thesis is
aimed at unravelling these mechanisms. This may be both of theoretical interest and
clinical interest in that it may contribute to the development of evidence-based
psychological treatment of patients with ConHD. Several hypotheses have been proposed
that may explain the relation between ConHD on the one hand and psychopathology or
Introduction
11
diminished quality of life on the other hand. The most prevailing hypotheses are indicated
as 1) the somatic hypothesis, 2) the symptom perception hypothesis and 3) the
vulnerability-stress hypothesis. These three hypotheses will be described in the following
paragraphs.
Somatic hypothesis
In traditional medicine it is postulated that there is a one-to-one relation between physical
disease and experienced physical symptoms (Cacioppo, Tassinary, & Bernston, 2000;
Cioffi, 1991; Pennebaker, 1982; Rose et al., 2005). According to this rather naïve
hypothesis, denoted the somatic hypothesis1, the concomitant reduced oxygenation of the
blood or irregular heart rate may directly increase the perception of symptoms such as
breathlessness or heart pounding. Consequently, this may reduce patients’ physical
functioning and general physical well being and in turn leads to a change in the patient’s
psychological and social functioning (Rose et al., 2005; Wilson & Cleary, 1995).
To test this direct linear relation between cardiac functioning and experienced
physical symptoms and quality of life, researchers have investigated whether the severity
of heart disease is related to physical symptoms, psychopathology, and quality of life.
However, conflicting results have been obtained depending on the methods used to assess
disease severity. Studies that classified disease severity based on the initial diagnosis (such
as transposition of the great arteries or ventricular septal defect) did not report a relation
between disease severity on the one hand and psychopathology (Utens et al., 1998; Van
Rijen et al., 2004; Van Rijen et al., 2005b) and quality of life on the other (Moons, Van
Deyk, De Geest, Gewillig, & Budts, 2005; Ternestedt et al., 2001; Van Rijen et al., 2005a).
When disease severity was determined by the presence of cyanosis or arrhythmias, disease
severity was related to quality of life. For example, it has been shown that patients with
cyanosis or arrhythmias report less physical functioning, daily activities due to physical
health problems, vitality, general health, mental health, social functioning, and
experienced pain than patients without these conditions (Lane et al., 2002; Jefferies et al.,
2004; Saliba et al., 2001; Moons et al., 2005; Irtel et al., 2005; Kamphuis et al., 2002).
Additionally, when disease severity was determined by peak oxygen uptake assessed
during a physical exercise task (Rose et al., 2005) or exercise capacity, disease severity was
related to overall behaviour problems, perceived physical symptoms, physical functioning,
and general health (Rose et al., 2005; Hager & Hess, 2005; Irtel et al., 2005; Van Rijen et
al., 2004). Finally, studies that classified disease severity based on the complexity of
cardiac surgery (e.g., curative, corrective, palliative, inoperable) showed a relation
1
The somatic hypothesis is also called the biomedical hypothesis.
12 Chapter 1
between disease severity on the one hand and depression (Bromberg et al., 2003),
perceived heart symptoms, worries about the future, and impact of cardiac surveillance,
such as ECG recordings and hospital admissions, on the other hand (Kamphuis et al.,
2004). However, these studies did not reveal a relation between disease severity and
quality of life (Lane, Lip, & Milane, 2002).
The findings with respect to the initial diagnosis suggest that the relation between
disease severity and psychological adjustment is absent. Conversely, the findings
regarding the presence of cyanosis or arrhythmias, peak oxygen uptake, and exercise
capacity suggest that disease severity is related to quality of life and psychopathology.
These later findings in combination with the observation that disease severity is
specifically related to the physical subscales of quality of life (e.g., Rose et al., 2005; Hager
& Hess, 2005) seem to support the somatic hypothesis stating that a direct linear relation
between heart disease and perceived physical symptoms may be present. However, there
are several reasons why these observed relations do not convincingly support the somatic
hypothesis. Firstly, the strength of the observed relations between disease severity and
quality of life may be overestimated. For example, peak oxygen consumption assessed
during an exercise task depends on a patient’s decision to interrupt the exercise task due
to experienced exhaustion and physical symptoms. Because perceived physical symptoms
are related to quality of life (Kamphuis et al., 2004; Rietveld et al., 2005) the observed
relation between peak oxygen consumption and quality of life might be explained by a
patient’s experience of physical symptoms rather then by the severity of heart disease
itself.
A second reason, why the observed relations between disease severity and
symptom perception or quality of life do not convincingly support the somatic hypothesis,
is that these relations may be indirect rather than direct. For example, severe heart disease
is associated with more potentially stressful experiences with the disease, such as openheart surgeries, medical check-ups, and hospitalizations (Kamphuis et al., 2004). It has
been shown that these disease-related experiences increase the risk of developing
psychopathology (Connoly, McClowry, Hayman, Mahony, & Artman, 2004; DeMaso et al.,
1991; Utens et al., 1998; Van Rijen et al., 2004). Alternatively, physicians may impose
more restrictions with regard to sports (sometimes unnecessarily; e.g., Fekkes et al., 2001)
to patients with severe ConHD. It has been shown that these restrictions are negatively
related to quality of life (Bar-Mor, Bar-Tal, Krulik, & Zeevi, 2000; Fekkes et al., 2001; Van
Rijen et al., 2004). These findings suggest that it is possible that the relation between
disease severity on the one hand and quality of life and psychopathology on the other is
mediated by exposure to potentially stressful disease-related experiences and physical
restrictions imposed by the physician. This may imply that the observed relation between
Introduction
13
heart function and perceived heart symptoms and quality of life does not represent a
direct relation, as stated by the somatic hypothesis, but instead an indirect relation. Note
that disease-related experiences may not be stressful to all patients. In the paragraph
entitled “vulnerability-stress hypothesis” we will elaborate on the role of trait anxiety in
enhancing the stressfulness of disease-related experiences.
A third reason why the findings do not convincingly support the somatic
hypothesis is that heart function and perceived physical symptoms were not assessed
within the same period in time. That is, researchers only assessed symptom perception
and quality of life retrospectively (e.g., Rose et al., 2005; Kamphuis et al., 2002).
Therefore, it cannot be inferred from these studies whether experienced heart symptoms
actually coincide with acute heart dysfunction, as stated by the somatic hypothesis. There
are reasons to suggest that patients with ConHD also perceive physical symptoms in the
absence of cardiac dysfunction. For example, it has repeatedly been demonstrated that the
relation between physiology and simultaneously perceived symptoms is generally weak
(e.g., Hoehn-Saric & McLeod, 2000; Richards & Bertram, 2000; Katkin, Morell,
Goldband, Bernstein, & Wise, 1982; Steptoe & Vögele, 1992; Pennebaker, 1982; Barsky et
al., 1994). Moreover, cardiologists are often confronted with patients complaining of heart
symptoms without clear cardiac origin (Ehlers, Mayou, Springings, & Birkhead, 2000; Van
Peski-Oosterbaan et al., 1998). Thus research, showing a relation between disease severity
and retrospectively assessed physical symptoms, may also reflect a relation between
disease severity and perceived symptoms that do not coincide with acute cardiac
dysfunction. This is in contrast to the somatic hypothesis.
Taken together, evidence for a direct and linear relation between heart function
and perceived physical symptoms and quality of life, as stated by the somatic hypothesis,
is weak. Moreover, even if there is a relation between disease severity and psychological
adjustment, disease severity does not fully explain quality of life and psychopathology in
ConHD (e.g., Rose et al., 2005; Wilson & Cleary, 1995). This implies that research should
focus on significant mediators and moderators that may affect the relationship between
heart disease and perceived heart symptoms. Indeed, the lack of evidence for the somatic
hypothesis inspired researchers to formulate alternative hypotheses, of which the
symptom perception hypothesis is one of the most prevailing ones.
Symptom perception hypothesis
Pennebaker (1982) postulated that people are unable to consciously perceive all the
physiological changes in their body, due to the overload of physiological changes occurring
at the same time. Moreover, he noted that physical sensations are often vague and
ambiguous and do not necessarily coincide with real physiological changes. As a result, in
14 Chapter 1
sharp contrast with the somatic hypothesis, it was hypothesized that the perception of
physical symptoms is coloured by the beliefs and expectations people hold about
symptoms and disease. According to this hypothesis, people selectively search for (or
attend to) physical sensations and interpret vague and ambiguous sensations in line with
their expectations and beliefs. There are many findings that support this hypothesis (e.g.,
Pennebaker & Skelton, 1981; Bishop, Briede, Cavazos, Grotzinger, & McMahon, 1987;
Pohl, Frohnau, Kerner, & Fehm-Wolfsdorf, 1997; Wager et al., 2004). For example, it has
been shown that healthy individuals who were given false feedback of elevated blood
pressure reported physical symptoms similar to those reported by patients with
hypertension (Bauman, Cameron, Zimmerman, & Leventhal, 1989).
Pennebaker (1982) and Nerenz and Leventhal (1983) assumed that the
expectations and beliefs people hold are formed by previous learning experiences with
symptoms and disease. Learning experiences are, for example, the perception of heart
pounding and breathlessness in a hospital setting, before an exam or during physical
exercise. These learning experiences are stored in cognitive memory structures or so called
illness schemes, consisting of associative relations between physical symptoms and
disease-related internal and external cues (Bower, 1981). Disease-related external cues
are, for example, an exam, sports or a hospital setting. Disease-related internal cues are,
for example, the subjective experience of stress, perceived physiological changes, and
thoughts about disease. The perception of a disease-related cue may activate an illness
scheme. In turn, patients may expect to experience disease-related symptoms, may
allocate their attention towards disease-related bodily changes, and may interpret these
changes as disease-related symptoms. As a result, in the presence of harmless diseaserelated cues, such as thoughts about disease, or a hospital setting, patients may perceive
symptoms that cannot be explained by acute physical disease. Conversely, in the absence
of these cues patients may fail to perceive acute physical disease.
On the basis of this hypothesis, it may be assumed that the development of illness
schemes moderates the relation between physical functioning and simultaneously
perceived symptoms in patients with chronic disease. Support for this conjecture has been
found among patients with asthma. In several experiments patients with asthma and
healthy controls were exposed to asthma-related cues such as stress-induced physiological
changes, false feedback of a reduced lung function, or false wheezing sounds (Rietveld,
Van Beest, & Everaerd, 1999; Rietveld, Kolk, & Prins, 1996; Rietveld & Houtveen, 2004;
Rietveld, Kolk, Prins, & Colland, 1997). Breathlessness and real lung function were
assessed before and after exposure to these asthma-related cues. In accordance with the
symptom perception hypothesis, patients with asthma showed an enhanced perception of
Introduction
15
breathlessness after exposure to these disease-related cues, whereas their simultaneous
lung function did not differ from healthy controls.
The role of illness schemes in ConHD is yet unknown. However, patients with
ConHD may be specifically vulnerable to develop such illness schemes, as ConHD is a
chronic condition that is present from birth. A variety of studies showed that specifically
adverse experiences during childhood predispose individuals to develop psychopathology
later in life (Heim et al., 2002; Heim & Nemeroff, 2001; Kendler, Kessler, Neale, Heath, &
Eaves, 1993). Therefore, it may be assumed that early exposure to heart disease
experiences facilitates the development of heart disease schemes in ConHD, predisposing
patients to develop a reduced quality of life. Moreover, because of the chronicity of
ConHD, accumulation of disease experiences may increase the number of associative
relations in the brain between symptoms and disease-related cues. Moreover, repeated
exposure may increase the sensitivity for certain disease-related stimuli (Ursin, 1997).
That is, repeated exposure to symptoms and disease may increase the synaptic strength in
the brain, decreasing the threshold for the perception of disease-related stimuli.
Although the symptom perception hypothesis may contribute to a better
understanding of symptom perception in patients with ConHD, the development of illness
schemes cannot fully explain the apparent variance of symptom perception and
psychological functioning in patients with ConHD. That is, if patients develop illness
schemes, all patients with ConHD should report reduced psychological functioning. In
contrast to this prediction, not all patients with ConHD show an increased perception of
heart symptoms or increased levels of psychopathology and reduced quality of life as
compared to the general population (e.g., Irtel et al., 2005; Rietveld et al., 2002; Fekkes et
al., 2001). This indicates that disease experiences are not inherently stressful to all
patients, but instead are only stressful to patients with certain characteristics. This
assumption is supported by research on the adverse impact of negative life events (e.g.,
Enns, Cox, & Clara, 2005; De Beurs et al., 2005; Zvolensky, Kotov, Antipova, & Schmidt,
2005; Sembi, Tarrier, O’Neill, Burns, & Faragher, 1998; Aben et al., 2002), and has
resulted in the formulation of the vulnerability-stress hypothesis.
Vulnerability-stress hypothesis
The vulnerability-stress hypothesis states that only individuals with certain psychological
vulnerabilities are at increased risk of developing psychopathology when exposed to
potentially stressful experiences, such as chronic disease. A psychological vulnerability
that is specifically relevant to disease and physical symptoms is neuroticism or its lowerorder dimension trait anxiety (Lilienfeld, 1996; Costa & McCrae, 1987; Watson &
Pennebaker, 1989). Trait anxiety has generally been defined as a pervasive disposition to
16 Chapter 1
react anxiously to ambiguous and potentially anxiety-provoking stimuli (Spielberger,
Gorsuch, & Lynche, 1970).
There are several reasons to expect that trait anxiety is a vulnerability factor for
developing biased symptom perception, psychopathology, and diminished quality of life in
chronic disease. First, trait anxiety seems to have significant genetic basis, as it is
associated with specific genetic variants (e.g., 5-HTTLPR; Sen, Burmeister, & Ghosh,
2004; Schinka, Busch, & Robichaux-Keene, 2004). Second, trait anxiety is a rather stable
trait (Watson & Walker, 1996), that is unaffected by the presence of chronic disease such
as ConHD (Van Rijen et al., 2003; Utens et al., 1994; Cox, Lewis, Stuart, & Murphy,
2002). Third, trait anxiety has been linked to processing biases for ambiguous physical
sensations that enhance the perception of physical symptoms (Watson & Pennebaker,
1989; Costa & McCrae, 1987). For example, processing biases that are characteristic of
high trait anxious individuals are a tendency to interpret ambiguous sensations as
threatening (Clark et al., 1997; Kamieniecki, Wade, & Tsourtos, 1997), to respond to
physical sensations with increased anxiety (Rapee, & Medoro, 1994; Forsyth, Lejuez, &
Finlay, 2000; Ehlers, Margraf, Roth, Taylor, & Birbaumer, 1988), to detect disease-related
cues early even without conscious awareness, and to show increased attention to diseaserelated information (Keogh, Dillon, Georgiou, & Hurt, 2001; Lundh Wikström,
Westerlund, & Öst,1999; Lim & Kim, 2005). Moreover, high trait anxious individuals show
an increased sensitivity and a decreased specificity for physiological changes (Table 1).
That is, they show a tendency to accurately perceive bodily changes (true positives; i.e.
Richards & Bertram, 2000; Ryan, Dulay, Suprasongsin, & Becker, 2002; Critchley, Wiens,
Rothstein, Öhman, & Dolan, 2004; Van der Does, Antony, Ehlers, & Barsky, 2000) and to
perceive symptoms in the absence of bodily changes (false positives; e.g., Steptoe &
Vögele, 1992; Hoehn-Saric, McLeod, Funderburk, & Kowalski, 2004; Sturges, Goetsch,
Ridley, & Whittal, 1998). A fourth reason why trait anxiety may be a vulnerability factor in
chronic disease is that it has been demonstrated that high trait anxiety in combination
with potentially adverse life events or physical disease, increases the perception of
symptoms (Zvolensky et al., 2005) and psychopathology (e.g., Aben et al., 2002; Sembie et
al., 1998; Kelly et al., 1998).
Table 1. Schematic representation of the concepts sensitivity and specificity
Physiological changes
No physiological changes
Symptom perception
True positives
False positives
No symptoms
False negatives
True negatives
Sensitivity = true positives /
Specificity = true negatives /
(true positives + false negatives)
(true negatives + false positives)
Introduction
Integration
of
the
symptom-perception
and
17
vulnerability-stress
hypothesis
In an attempt to incorporate the influence of trait anxiety on symptom perception in
chronic disease, we adjusted the classic symptom perception model of Pennebaker (1982).
We hypothesized that patients with chronic disease who are also high trait anxious are the
most likely to develop illness schemes related to their chronic disease. The reason for this
assumption was that high trait anxious patients with chronic disease probably have the
most stressful and anxious experiences with symptoms. That is, the presence of chronic
disease may increase the number of disease-related experiences and the presence of high
trait anxiety may result in a catastrophic interpretation of these disease-related
experiences. Moreover, high trait anxious patients with chronic disease may experience
probably the most disease-related experiences, as high anxious individuals are more
sensitive perceivers of real physical disease.
We hypothesized that, due to these stressful disease-related experiences, high trait
anxious patients with chronic disease may show processing biases that are characterised
by: (1) catastrophic interpretation of disease-related sensations, 2) selective attention to
disease-related sensations, and (3) increased perception of disease-related symptoms. In
addition, we hypothesized that (4) high trait anxious patients with chronic disease may
show these processing biases when exposed to subliminal or supraliminal disease-related
cues. Finally, we hypothesized that (5) these processing biases explain a diminished
quality of life in chronic disease.
Outline of the present thesis
The aim of the present thesis was to clarify whether the hypothesis concerning the role of
trait anxiety and symptom perception in chronic disease applies to adults with congenital
heart disease. The main research question of this thesis was whether a combination of
ConHD and high trait anxiety would result in perceptual biases for heart-related
symptoms and, in turn, a diminished quality of life.
The present thesis contains three sections. The first section (chapter 2) focuses on
possible adverse effects of ConHD on general psychological and cognitive functioning. We
conducted a meta-analysis of existing studies on children and adolescents. We tested
whether chronological age and disease severity influenced psychopathology and cognitive
functioning. Note that we did not review studies on adults with ConHD because at the
time the meta-analysis was conducted, research had mainly focused on children and
adolescents and research on adults was limited. In the second section (chapter 3 and 4),
we address biased perception of heart-related symptoms in ConHD. We tested the
hypothesis that false heart-rate feedback (a harmless heart-related cue) or acute stress
18 Chapter 1
triggers an increased perception of heart-related symptoms in high trait anxious patients
with ConHD that could not be explained by simultaneous cardiac dysfunction. In the third
section (chapter 5 and 6), we addressed whether both attentional and interpretational
biases explain biased perception of heart-related symptoms in ConHD. We tested the
hypothesis that ConHD in combination with high trait anxiety would result in an
increased difficulty shifting attention away from heart-related sensations (chapter 5) and
in a negative interpretative bias for heart-related symptoms (chapter 6). Moreover, in
chapter 5, we tested whether processing biases are elicited by disease-related cues that are
not consciously perceived. Additionally, in chapter 6, we tested whether a negative
interpretation bias mediated the relation between trait anxiety and quality of life. Finally,
chapter 7 provides an integration and further reflection on the results presented in the
separate studies.
References
Aben, I., Denelott, J., Lousberg, R., Verhey, F., Wojciechowski, F., & Honig, A. (2002). Personality
and vulnerability to depression in stroke patients. A 1-year prospective follow-up study.
Stroke, 33, 2391-2395.
Bar-Mor, G., Bar-Tal, Y., Krulik, T., & Zeevi, B. (2000). Self-efficacy and physical activity in
adolescents with trivial, mild, or moderate congenital cardiac malformations. Cardiology
in the Young, 10, 557-559.
Barsky, A.J., Clearly, P.D., Barnett, M.C., Christiansen, C.L., & Ruskin, J.N., (1994). The accuracy of
symptom reporting by patients complaining of palpitations. The American Journal of
Medicine, 97, 214-221.
Bauman, L.J., Cameron, L.D., Zimmerman, R.S., & Leventhal, H. (1989). Illness representations
and matching labels with symptoms. Health Psychology, 8, 449-469.
Bishop, G.D., Briede, C., Cavazos, L., Grotzinger, R., & McMahony, S. (1987). Processing illness
information: the role of disease prototypes. Basic and Applied Social Psychology, 8, 21-43.
Bower, G.H. (1981).Mood and memory. American Psychologist, 36, 128-148.
Brandhagen, D.J., Feldt, R.H., & Williams, D.E. (1991). Long-term psychologic implications of
congenital heart disease: a 25-years follow-up. Mayo Clinics Proceedings, 66, 474-479.
Bromberg, J.I., Beasley, P.J., D’Angelo, E.J., Landzberg, M., & DeMaso, D.R. (2003). Depression
and anxiety in adults with congenital heart disease: a pilot study. Heart and Lung, 32, 105110.
Caccioppo, J.T., Tassinary, L.G., & Berntson, G.G. (2000). Psychophysiological science. In J.T.
Caccioppo, L.G. Tassinary, & G.G. Berntson (Eds.), Handbook of psychophysiology (pp. 1115). Cambridge: University Press.
Cioffi, D. (1991). Beyond attentional strategies: a cognitive-perceptual model for somatic
interpretation. Psychological Bulletin, 109, 25-41.
Introduction
19
Clark, D.M., Salkovskis, P.M., Ost, L.G., Breitholz, E., Koehler, K.A., Westling, B.E., Jeavons, A., &
Gelder, M. (1997). Misinterpretation of body sensations in panic disorder. Journal of
Consulting and Clinical Psychology, 65, 203-213.
Connoly, D., McClowry, S., Hayman, L., Mahony, L., & Artman, M. (2004). Posttraumatic stress
disorder in children after cardiac surgery. Journal of Pediatrics, 144, 480-484.
Costa, P.T., & McCrae, R.R. (1987). Neuroticism, somatic complaints, and disease: is the bark worse
than the bite? Journal of Personality, 55, 299-316.
Cox, D., Lewis, G., Stuart, G., & Murphy, K. (2002). A cross-sectional study of the prevalence of
psychopathology in adults with congenital heart disease. Journal of Psychosomatic
Research, 52, 65-68.
Critchley, H.D., Wiens, S., Rothstein, P., Öhman, A., & Dolan, R.J. (2004). Neural systems
supporting interoceptive awareness. Nature Neuroscience, 7, 189-195.
Daliento, L., Mapelli, D., Russo, G., Scarso, P., Limongi, F., Lannizzi, P., Melendugno, A., Mazzotti,
E., & Volpe, B. (2005). Health related quality of life in adults with repaired tetralogy of
Fallot, psychological and cognitive outcomes. Heart, 91, 213-218.
De Beurs, E., Comijs, H., Twisk, J.W.R., Sonnenberg, C., Beekman, A.T.F., & Deeg, D. (2005).
Stability and change of emotional functioning in late life: modelling of vulnerability
profiles. Journal of Affective Disorders, 87, 53-62.
DeMaso, D.R., Campis, L.K., Wypij, D., Bertram, S., Lipshitz, M., & Freed, M. (1991). The impact of
maternal perceptions and medical severity on the adjustment of children with congenital
heart disease. Journal of Pediatric Psychology, 16, 137-149.
Ehlers, A., Margraf, J., Roth, W.T., Taylor, B., & Birbaumer, N. (1988). Anxiety induced by false
heart rate feedback in patients with panic disorder. Behaviour Research and Therapy, 26,
1-11.
Ehlers, A., Mayou, R.A., Sprigings, D.C., & Birkhead J. (2000). Psychological and perceptual factors
associated with arrhythmias and benign palpitations. Psychosomatic Medicine, 62, 693702.
Enns, M.W., Cox, B.J., & Clara, I.P. (2005). Perfectionism and neuroticism: a longitudinal study of
specific vulnerability and diathesis-stress models. Cognitive Therapy and Research, 29,
463-478.
Fekkes, M., Kamphuis, R.P., Ottenkamp, J., Verrips, E., Vogels, T., Kamphuis, M., & VerlooveVanhorick, S.P. (2001). Health-related quality of life in young adults with minor congenital
heart disease. Psychology and Health, 16, 239-250.
Forsyth, J.P., Lejuez, C.W., & Finlay, C. (2000). Anxiogenic effects of repeated administration of
20% CO2-enriched air: stability within sessions and habituation across time. Journal of
Behavior Therapy and Experimental Psychiatry, 31, 103-121.
Hager, A., & Hess, J. (2005). Comparison of health related quality of life with cardiopulmonary
exercise testing in adolescents and adults with congenital heart disease. Heart, 91, 517-520.
Heim, C., & Nemeroff, C.B. (2001). The role of childhood trauma in the neurobiology of mood and
anxiety disorders: preclinical and clinical studies. Biological Psychiatry, 49, 1023-1039.
20 Chapter 1
Heim, C., Newport, J., Wagner, D., Wilcox, M.M., Miller, A.H., & Nemeroff, C.B. (2002). The role of
early adverse experience and adulthood stress in the prediction of neuroendocrine stress
reactivity in women: a multiple regression analysis. Depression and Anxiety, 15, 117-125.
Hoehn-Saric, R., & McLeod, D.R. (2000). Anxiety and arousal: physiological changes and their
perception. Journal of Affective Disorders, 61, 217-224.
Hoehn-Saric, R., McLeod, D.R., Funderburk, F., & Kowalski, P. (2004). Somatic symptoms and
physiologic responses in generalized anxiety disorder and panic disorder: An ambulatory
monitor study. Archives of General Psychiatry, 61, 913-921.
Irtel, T.A., Vetter, C., Struber, T., Kuemin, A., Heimes, T., Pfammater, J., Tüller, D., Carrel, T.,
Delacrétaz, E. (2005). Impact of arrhythmias on health-related quality of life in adults with
congenital heart disease. Cardiology in the Young, 15, 627-631.
Jefferies, J.L., Noonan, J.A., Keller, B.B., Wilson, J.F., & Griffith, C. (2004). Quality of life and
social outcomes in adults with congenital heart disease living in rural areas of Kentucky.
American Journal of Cardiology, 94, 263-266.
Kamieniecki, G.W., Wade, T., & Tsourtos, G. (1997). Interpretive bias for benign sensations in panic
disorder with agoraphobia. Journal of Anxiety Disorders, 11, 141-156.
Kamphuis, M., Ottenkamp, J., Vliegen, H.W., Vogels, T., Zwinderman, K.H., Kamphuis, R.P., &
Verloove-Vanhorick, S.P. (2002). Health related quality of life and health status in adult
survivors with previously operated complex congenital heart disease. Heart, 87, 356-362.
Kamphuis, M., Zwinderman, K.H., Vogels, T., Vliegen, H.W., Kamphuis, R.P., Ottenkamp, S.P.,
Verloove-Vanhorick, & Bruil, J. (2004). A cardiac-specific health-related quality of life
module for young adults with congenital heart disease: Development and validation.
Quality of Life Research, 13, 735-745.
Katkin, E.S., Morell, M.A. Goldband, S., Bernstein, G.L., & Wise, J.A. (1982). Individual differences
in heartbeat discrimination. Psychophysiology, 19, 160-166.
Kelly, B., Raphael, B., Judd, F., Kernutt, G., Burnett, P., & Burrows, G. (1998). Posttraumatic stress
disorder in response to HIV infection. General Hospital Psychiatry, 20, 345-352.
Keogh, E., Dillon, C., Georgiou, G., & Hunt, C. (2001). Selective attentional biases for physical
threat in physical anxiety sensitivity. Anxiety Disorders, 15, 299-315.
Kendler, K.S., Kessler, R.C., Neale, M.C., Heath, A.C., & Eaves, L.J. (1993). The prediction of major
depression in women: toward an integrated model. American Journal of Psychiatry, 150,
1139-1148.
Lane, D.A., Lip, G.Y.H., & Millane, T.A. (2002). Quality of life in adults with congenital heart
disease. Heart, 71-75.
Lim, S.L., & Kim, J.H. (2005). Cognitive processing of emotional information in depression, panic,
and somatoform disorder. Journal of Abnormal Psychology, 114, 50-61.
Lilienfeld, S.O. (1996). Anxiety sensitivity is not distinct from trait anxiety. In R.M. Rapee (Ed.),
Current controversies in the anxiety disorders (pp. 288-244). New York: Guilford Press.
Lundh, L.G., Wikström, J., Westerlund, J., & Öst, L.G. (1999). Preattentive bias for emotional
information in panic disorder with agoraphobia. Journal of Abnormal Psychology, 108,
222-232.
Introduction
21
Moons, P., De Blesser, L., Budts, W., Sluysmans, T., De Wolf, D., Massin, M., Gewilig, M., Pasquet,
A., Suys, B., & Vliers, A. (2004). Health status, functional abilities, and quality of life after
the Mustard or Senning operation. The Annals of Thoracic Surgery, 77, 1359-1365.
Moons, P., Van Deyk, K., De Geest, S., Gewillig, M., & Budts, W. (2005). Is the severity of
congenital heart disease associated with the quality of life and perceived health of adult
patients. Heart, 91, 1193-1198.
Nerenz, D.R., & Leventhal, H. (1983). Self-regulation theory in chronic illness. In: T.G., Burish, &
L.A., Bradley, (Eds.), Coping with chronic disease research and applications (pp.13-37).
New York: Academic Press.
Pennebaker, J.W. (1982). The psychology of physical symptoms. New York: Springer-Verlag.
Pennebaker, J.W., & Skelton, J.A. (1981). Selective monitoring of physical sensations. Journal of
Personality and Social Psychology, 41, 213-223.
Pohl, J., Frohnau, G., Kerner, W., & Fehm-Wolfsdorf, G. (1997). Symptom awareness is affected by
the subjects’ expectations during insulin-induced hypoglycaemia. Diabetes Care, 20, 796802.
Rapee, R.M., & Medoro, L. (1994). Fear of physical sensations and trait anxiety as mediators of the
response to hyperventilation in nonclinical subjects. Journal of Abnormal Psychology,
103, 693-699.
Richards, J., & Bertram, S. (2000). Anxiety sensitivity, state and trait anxiety, and the perception of
change in sympathetic nervous system arousal. Journal of Anxiety Disorder, 14, 413-427.
Rietveld, S., Van Beest, I., & Everaerd, W. (1999). Stress-induced breathlessness in asthma.
Psychological Medicine, 29, 1359-1366.
Rietveld, S., & Houtveen, J.H. (2004). Acquired sensitivity to relevant physiological activity in
patients with chronic health problems. Behaviour Research and Therapy, 42, 137-153.
Rietveld, S., Karsdorp, P.A., & Mulder, B.J. (2004). Heartbeat sensitivity in adults with congenital
heart disease. International Journal of Behavioral Medicine, 11, 203-211.
Rietveld, S., Kolk, A.M., & Prins, P.J. (1996). The influence of lung function information on selfreports of dyspnea by children with asthma. Journal of Pediatric Psychology, 21, 367-377.
Rietveld, S., Kolk, A.M., Prins, P.J., & Colland, V.T. (1997). The influence of respiratory sounds on
breathlessness in children with asthma: a symptom-perception approach. Health
Psychology, 16, 547-553.
Rietveld, S., Mulder, B.J., Van Beest, I., Lubbers, W., Prins, P.J., Vioen, S., Bennebroek-Evererz, F.,
Vos, A., Casteelen, G., & Karsdorp, P. (2002). Negative thoughts in adults with congenital
heart disease. International Journal of Cardiology, 86, 19-26.
Rose, M., Köhler, K., Köhler, F., Sawitzky, B., Fliege, H., & Klap, B.F. (2005). Determinants of the
quality of life of patients with congenital heart disease. Quality of Life Research, 14, 35-43.
Ryan, C.M., Dulay, D., Suprasongsin, C., & Becker, D.J. (2002). Detection of symptoms by
adolescents and young adults with type 1 diabetes during experimental induction of mild
hypoglycaemia. Diabetes Care, 25, 852-858.
22 Chapter 1
Saliba, Z., Butera, G., Bonnet, D., Bonhoeffer, P., Villain, E., Kachaner, J., Sidi, D., & Iserin, L.
(2001). Quality of life and perceived health status in surviving adults with univentricular
heart. Heart, 86, 69-73.
Schinka, J.A., Busch, R.M., & Robichaux-Keene, N. (2004).A meta-analysis of the association
between the serotonin transporter gene polymorphism (5-HTTLPR) and trait anxiety.
Molecular Psychiatry, 9, 197-202.
Sembi, S., Tarrier, N., O’Neill, P., Burns, A., & Faragher, B. (1998). Does Post-traumatic stress
disorder occur after stroke: a preliminary study. International Journal of Geriatric
Psychiatry, 13, 315-322.
Sen, S., Burmeister, M., & Ghosh, D. (2004). Meta-analysis of the association between a serotonin
transporter promoter polymorphism (5-HTTLPR) and anxiety-related personality traits.
American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 127, 85-89.
Spielberger, C.D., Gorsuch, R., & Lusheve, R. (1970). STAI Manual for the State-Trait Anxiety
Inventory. Palo Alto, CA: Consulting Psychologists Press.
Steptoe, A., & Vögele, C. (1992). Individual differences in the perception of bodily sensations: the
role of trait anxiety and coping style. Behaviour Research Therapy, 30, 597-607.
Sturges, L.V., Goetsch, V.L., Ridley, J., & Whittal, M. (1998). Hyperventilation challenge:
Physiologic arousal, interoceptive acuity, and subjective distress. Journal of Anxiety
Disorders, 12, 103-115.
Ternestedt, B.M., Wall, K., Oddsson, H., Riesenfeld, T., Groth, I., & Scholin, J. (2001). Quality of
life 20 and 30 years after surgery in patients operated on for tetralogy of Fallot and for
atrial septal defect. Pediatric Cardiology, 22, 128-132.
Utens, E.M.W.J., Verhulst, F.C., Erdman, R.A.M., Meijboom, F.J., Duivenvoorden H.J., Bos, E.,
Roelandt, J.R., & Hess, J. (1994). Psychosocial functioning of young adults after surgical
correction for congenital heart disease in childhood; a follow-up study. Journal of
Psychosomatic Research, 38, 745-758.
Utens, E.M., Versluis-Den Bieman, H.J., Verhulst, F.C., Meijboom, F.J., Erdman, R.A., & Hess, J.
(1998). Psychopathology in young adults with congenital heart disease. European Heart
Journal, 647-651.
Ursin, H. (1997). Sensitization, somatization, and subjective health complaints. International
Journal of Behavioral Medicine, 4, 105-116.
Van der Does, A.J.W., Antony, M.M., Ehlers, A., & Barsky, A.J. (2000). Heartbeat perception in
panic disorder: a reanalysis. Behaviour Research and Therapy, 38, 47-62.
Van Peski-Oosterbaan, A.S., Spinhoven, P., Koch, G.C., Van der Does, A.J., Padmos, I., & Bruschke,
A.V. (1998). Unexplained non-cardiac chest pain: its prevalence and natural course.
Nederlands Tijdschrift voor Geneeskunde, 142, 2468-2472.
Van Rijen, E.H.M., Utens, E.M.W.J., Roos-Hesselink, J.W., Meijboom, F.J., Van Domburg, R.T.,
Roelandt, J.R.T.C., Bogers, A.J.J.C., & Verhulst, F.C. (2003). Psychosocial functioning of
the adult with congenital heart disease: a 20-33 year follow-up. European Heart Journal,
24, 673-683.
Introduction
23
Van Rijen, E.H.M., Utens, E.M.W.J., Roos-Hesselink, J.W., Meijboom, F.J., Van Domburg, R.T.,
Roelandt, J.R.T.C., Bogers, A.J.J.C., & Verhulst, F.C. (2004). Medical predictors for
psychopathology in adults with operated congenital heart disease. European Heart
Journal, 25, 1605-1613.
Van Rijen, E.H., Utens, E.M., Roos-Hesselink, J.W., Meijboom, F.J., Van Domburg, R.T., Roelandt,
J.R.T.C., Bogers, A.J.J.C., & Verhulst, F.C. (2005a). Current subjective state of health, and
longitudinal psychological well-being over a period of 10 years, in a cohort of adults with
congenital cardiac disease. Cardiology in the Young, 15, 168-175.
Van Rijen, E.H.M., Utens, E.M.W.J., Roos-Hesselink, J.W., Meijboom, F.J., Van Domburg, R.T.,
Roelandt, J.R.T.C., Bogers, A.J.J.C., & Verhulst, F.C. (2005b). Longitudinal development of
psychopathology in an adult congenital heart disease cohort. International Journal of
Cardiology, 99, 315-323.
Wager, R.D., Rilling, J.K., Smith, E.E., Sokolik, A., Casey K.L., Davidson R.J. Kosslyn S.M., Rose
R.M., & Cohen, J.D. (2004). Placebo-induced changes in fMRI in the anticipation and
experience of pain. Science, 303, 1162-1167.
Watson, D., & Walker, L.M. (1996). The long-term stability and predictive validity of trait measures
of affect. Journal of Personality and Social Psychology, 70, 567-577.
Watson, D., & Pennebaker, J.W. (1989) Health complaints, stress, and distress: exploring the
central role of negative affectivity. Psychological Review, 96, 234-54.
Warnes, C.A., Liberthson, R., Danielson, G., Dore, A., Harris L., Hoffman, J.I., Sommerville J.,
Williams, R.G., & Webb, G.D. (2001). Task force 1: The changing profile of congenital heart
disease in adult life. Journal of American College of Cardiology, 37, 1170-1175.
Wilson, I.B., & Cleary, P.D. (1995). Linking clinical variables with health-related quality of life.
Journal of the American Medical Association, 273, 59-65.
Zvolensky, M.J., Kotov, R., Antipova, A.V., & Schmidt, N.B. (2005). Diathesis stress model for
panic-related distress: a test in a Russian epidemiological sample. Behaviour Research and
Therapy, 43, 521-532.
Psychological
and
cognitive
functioning
in
children and pre-adolescents with congenital
heart disease: a meta-analysis
Karsdorp, P.A., Everaerd W., Kindt, M., & Mulder, B.J.M. (in press). Journal of Pediatric
Psychology.
26 Chapter 2
Abstract
The objective of the present study was to establish whether congenital heart disease
(ConHD) affects psychological and cognitive functioning in children and adolescents. We
conducted a meta-analysis to review studies on behaviour problems and cognitive
functioning in ConHD. A relationship was found between age and behaviour problems.
Specifically, pre-adolescents with ConHD displayed an increased risk for overall,
internalizing and to a lesser extent externalizing behaviour problems. In addition, patients
with severe ConHD exhibited lower cognitive functioning than patients with less severe
ConHD. Performance intelligence as compared with verbal intelligence seemed to be most
affected in ConHD. Moreover, decreased cognitive functioning remained relatively stable
across different age groups. These findings suggest that children with severe heart disease
may benefit from interventions specifically targeting perceptual organizational abilities,
such as visual spatial abilities. Moreover, pre-adolescents with ConHD may benefit from
psychological interventions reducing anxiety and depression.
Meta-analysis 27
Introduction
Congenital heart disease (ConHD) refers to a heterogeneous group of diseases
characterized by a structural heart defect at birth. It is estimated that about 1 % of
newborns are born with a form of ConHD that needs specialized cardiologic care (Warnes
et al., 2001). At least ninety percent of the patients are diagnosed in infancy and childhood
and most of these patients are expected to undergo an operation or interventional
catheterization in infancy to correct or palliate their defect (Warnes et al., 2001). After
cardiac intervention residual anatomical abnormalities may remain and patients may still
be at risk for premature death or co-morbidities, such as arrhythmias, hypertension, or
pulmonary, renal, myocardial, or coronary artery disease. Most patients with ConHD need
to be seen regularly by a cardiologist and almost 50 % of the patients who have undergone
surgery require additional surgery at an older age (Warnes et al., 2001). Advances in
diagnostic and surgical techniques have increased survival rates in ConHD remarkably.
Nowadays, more than 85% of the children with complex ConHD survive beyond the first
year of age as compared to 20% in the forties (Warnes et al., 2001). Due to increased
survival rates, greater attention has been directed towards understanding the impact of
ConHD on psychological and cognitive functioning. Nowadays, the goal of medical care is
not only to achieve long-term survival but also to achieve the best possible psychological
and cognitive development.
A considerable number of studies have been conducted to assess the impact of
ConHD on children’s and adolescents’ psychological and cognitive functioning. The
outcome measure that is used in the majority of these studies assessing psychological
functioning is the Child Behaviour Checklist parent form (CBCL; Achenbach & Edelbrock,
1983). This is a parent report measure that provides an estimate of overall emotional and
behavioural problems and of internalizing (e.g., anxiety, depression, social withdrawal)
and externalizing behaviour problems (e.g., hyperactivity, oppositional behaviour,
aggression). The outcome measure that is used in the majority of studies assessing overall
cognitive functioning, verbal (VIQ; e.g., verbal comprehensive abilities) and performance
intelligence quotients (PIQ; e.g., perceptual organizational abilities) is the Wechsler
Intelligence Tests for Children (WISC; Wechsler, 1991). Consensus among studies
assessing psychological and cognitive functioning in ConHD has not been reached.
Authors report higher rates of behaviour problems and reduced cognitive functioning
among children and adolescents with ConHD (e.g., Mahle et al., 2000; Hövels-Gürich et
al., 2002), whereas others report no significant differences between patients with ConHD
and a comparison group (Jedlicka-Köhler & Wimmer, 1987; Utens, Versluis-Den Bieman,
Wisenburg, Bogers, Verhulst, & Hess, 2001).
28
Chapter 2
An important distinction among studies is the severity of heart disease of the
patient sample. Studies provide estimates of behaviour problems and cognitive
functioning for separate patient groups with only simple or severe ConHD (e.g., Clarkson
et al., 1980), or for a heterogeneous group of patients with ConHD (Utens et al., 1993). It
has been suggested that patients with more severe heart disease are exposed to more
detrimental factors such as diminished cerebral perfusion (Gupta, Giuffre, Crawford, &
Waters, 1998; Newburger, Silbert, Buckley, & Fyler, 1984), difficult surgery (Clarkson et
al., 1980; Stavinoha, Fixler, & Mahony, 2003), and physical impairments (Paul & Wessel,
1999). Therefore, the different findings among studies could be explained by the fact that
patients with severe heart disease are at increased risk for psychological and cognitive
problems. In the literature, however, no consensus has been reached on the effect of
disease severity on psychological and cognitive functioning. That is, some authors report
worse psychological and cognitive functioning in more severe ConHD (e.g., Haneda, Itoh,
Togo, Ohmi, & Mohri, 1996; Hesz & Clark, 1988), whereas others do not (e.g., Utens et al.,
1993; Forbess, Visconti, Bellinger, Howe, & Jonas, 2002).
A second discrepancy among studies has been the age of the patients with ConHD.
Cognitive and psychological functioning is tested in patients varying in age from 4 months
to 18 years old. There are two reasons why different results may have been obtained due to
age differences. Firstly, the reliability and predictive validity of assessments of IQ and
behaviour problems is low in infancy and todllerhood (e.g., Gruneau, Whitfield, & Petrie,
2000; McGrath, Wypij, Rappaport, Newburger, & Bellinger, 2004), and is moderate to
high in children aged 4 years or above (Samerhoff, Seifer, Baldwin, & Baldwin, 1993;
Hofstra, Van der Ende, & Verhulst, 2000). Therefore, the different findings across studies
may reflect the low reliability and validity of the findings in infancy. Secondly, older
patients with ConHD may differ from younger patients in psychological and cognitive
functioning, because older patients are exposed to more risk factors during the course of
their life. Risk factors that have been suggested are for example: overprotection by
parents, rejection by peers, diminished cerebral perfusion, seizures, hospitalizations,
cardiac surgeries, hormonal changes, genetic vulnerabilities, and physical impairment.
Research comparing psychological and cognitive functioning of patients with different
ages is limited. Only some studies showed age effects on psychological and cognitive
functioning (e.g., Wray & Sensky, 1998; Jedlicka-Köhler, Sinko-Sanz, Schlemmer, &
Wimmer, 1995), whereas others did not (e.g., Kern, Hinton, Nereo, Hayes, & Gersony,
1998; DeMaso, Baerdslee, Silbert, & Fyler, 1990).
Some reviews have been written to integrate the literature on psychological and
cognitive functioning in ConHD. However, the conclusions of these reviews as to whether
patients with ConHD are at increased risk of diminished psychological and cognitive
Meta-analysis 29
functioning and whether disease severity is a risk factor have been inconsistent (Gardner
& Angelini, 1995; Griffin, Elkin, & Smith, 2003; Samango-Sprouse, & Suddaby, 1997;
Shillingford & Wernovsky, 2004; Foster et al., 2001). Moreover, these reviews have not
included all relevant literature, and the criteria for inclusion are not always presented.
Furthermore, these reviews rely on significance testing, increasing the likelihood of a type
II error, as the sample sizes of the patients with ConHD are often small.
The goal of the present study is to determine the impact of ConHD on
psychological and cognitive functioning in children and adolescents. We provide a
systematic review of the current empirical body of literature on psychopathology and
cognitive functioning in ConHD, using meta-analytic techniques. Meta-analytic
techniques provide a reliable overall estimate of effect sizes and statistical tests to
determine whether differences in methodological characteristics, (e.g., control group
used), and sample characteristics, such as age and severity of heart disease, influence the
findings. Note that in the present study we did not test the effect of variables such as
surgical techniques and patients’ level of neuroticism, because the number of studies was
insufficient.
Methods
Literature search
Because medical technology and medical treatment have changed dramatically over the
last 25 years (Griffin, Elkin, & Smith, 2003), the literature search was restricted to articles
published between 1980 and May 2005. We performed a search in Medline and Psychinfo
databases using the following keywords: “congenital heart defects or disease”, paired with
the descriptors “mental disorders”, “behaviour”, “psychology”, and “cognitive”. In
addition, we searched reference lists of studies included in this meta-analysis. To ascertain
the likelihood of a publication bias, a file drawer analysis was conducted. A file drawer
analysis is a method to estimate the number of additional studies averaging null findings
that would be necessary to bring small and medium effect sizes (ESs) for psychopathology
and cognitive functioning to negligible ESs (Hunter & Schmidt, 1990).
Inclusion criteria
Criteria for inclusion in the meta-analysis were as follows: (1) studies had to be published
in a peer-reviewed English- or German-language journal; (2) studies solely included
patients with ConHD; (3) studies included patients between 2 to 19 years old, and with a
mean age of 4 years or above; (4) studies included solely patients who had undergone
surgery or interventional catheterization; (5) studies included the Child Behaviour
30
Chapter 2
Checklist parent form to measure psychopathology; (6) and / or studies included a
measure of cognitive function (British Ability Scale, Bayley Scales of Infant Development,
Differential Ability Scale, Kaufman Assessment Battery for Children, Leiter International
Scale, McCarthy Scales of Children’s Abilities, Stanford Binet Scale, Wechsler Intelligence
Test for Children, Wechsler Preschool and Primary Scale of Intelligence); (7) studies
reported sufficient data necessary to compute effect sizes; (8) studies included a control
group (healthy controls, siblings, individuals with innocent heart murmur, or published
norms).
Studies were excluded that only tested patients with syndromes in which ConHD
was part of the total syndrome, like Williams, Marfan, or velo-cardio-facial syndrome.
Note that studies included in the meta-analysis are marked with an asterisk in the
reference list.
Variables coded from each study
To determine between-rater-agreement, two independent judges coded 19 randomly
selected studies of the sample. Information coded from each study included: meeting
inclusion criteria, year of publication, age of the patients, name of questionnaires,
construct measured, type of heart disease, type of control group, sample sizes, inferential
statistics, and mean and standard deviation of psychopathology and cognitive functioning.
Discrepancies in coding were measured with Kappa’s coefficient and Pearson’s correlation
for categorical and non-categorical data, respectively (e.g., Whittington, Podd, & Kan,
2000). Between-rater agreement showed that the coding for each variable was very
reliable (mean agreement for the variables coded: r = .93, SD = .13). Discrepancies in
coding were solved through discussion between judges. A cardiologist classified the heart
defects into complex (e.g., transposition of the great arteries), moderate (e.g., tetralogy of
Fallot) and simple ConHD (e.g., ventricular septal defect) based on risk of morbidity and
mortality, according to the classification system presented at the 32nd Bethesda
Conference (Warnes et al., 2001).
Meta-analytic procedures
The basic approach primarily focused on effect sizes and was modeled on the metaanalytic techniques of Hunter and Schmidt (1990). This method provides the opportunity
to determine how much of the variance in effect sizes across studies is due to sampling
error. Moreover, this method allows adjusting for the effect of sampling error, yielding an
estimate of the true population variability of study outcomes. Finally, it provides a method
to test whether effect sizes across studies are uniform (homogeneous). This method is less
Meta-analysis 31
vulnerable to type II error (i.e., concluding that the ES are uniform when in fact they are
not) than the often-used chi-square statistics (Hedges & Olkin, 1985).
Calculation effect sizes
The standardized mean difference, d (Cohen, 1988), was used as the estimate of ES. The d
statistics can be defined as the difference between the group means divided by the pooled
standard deviation. Where a study reported the percentages of patients with ConHD who
exceeded a cutoff score, the ES was determined by consulting a table using probit
transformation methods to convert differences in proportions to ES (Glass, McGaw, &
Smith, 1981). Effect sizes expressed in eta squared were transformed to Cohen’s d (Cohen,
1988). Where published norms or standard scores were provided the sample size of the
control group was equated with the sample size of the patient group. Where standard
deviation of the patient group was missing the standard deviation of the control group was
substituted. For psychopathology, a positive ES reflects more psychopathology in ConHD
relative to controls. For cognitive functioning a negative ES reflects decreased cognitive
functioning in ConHD relative to controls.
To correct for differences in sample size, the weighted mean ES and variance were
computed (Hunter & Schmidt, 1990). To correct for sampling error, the population
(residual) variance was then computed by subtracting the sampling error variance from
the observed variance (Hunter & Schmidt, 1990). Sampling error variance was computed
using the formula Se 2 = ([N - 1] / [N - 3]) ([4 / N] [1 + D2 / 8]), N being the average sample
size across all groups and D the weighted average of Cohen’s d. The estimate of the
population variance served as the multiplier in the formula for the 95% confidence
interval. Finally, an unbiased ES (d*) was calculated by removing a small sample bias. The
unbiased ES was computed by d* = d / a. where a = 1 + .75 / (N - 3) (Hunter & Schmidt,
1990).
To reliably interpret the estimated population ES, the ESs should be uniform
across studies, i.e. homogenous. To test to what extent the ESs are homogenous, we
determined the degree to which any residual variance of the ESs (i.e., variance after
removal of sampling error) could be explained by artifacts not corrected for. This was
calculated by the percentage of observed variance explained by sampling error variance.
The data set can be considered homogeneous if more than 75% of the observed variance is
explained by sampling error (Hunter & Schmidt, 1990). If less than 75% of the observed
variance is explained by sampling error, the data set can be considered heterogeneous.
This may indicate that there are moderating variables explaining the residual variance of
the ESs.
32
Chapter 2
To examine the effect of moderating variables, the data set was subdivided as a
function of the moderator. For continuous moderator variables, Pearson product-moment
correlation coefficients were calculated between the unbiased ESs and the moderator
variable. According to Cohen (1988) small, medium, and large effect sizes were d = 0.20,
0.50, and 0.80, respectively.
Results
Psychopathology
Eleven studies were selected for inclusion in the meta-analysis, providing 16 ESs for
overall behaviour problems and 14 ESs for internalizing (e.g., anxiety, depression) and
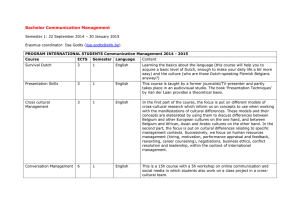
externalizing (e.g., hyperactivity, aggression) behaviour problems (Table 1). The analysis
showed that patients with ConHD exhibited more overall (medium ES), internalizing
(medium ES), and externalizing behaviour problems (small ES) than controls (Table 2).
However, only for externalizing behaviour problems a homogeneous data set was
obtained.
Correlations between age and ESs for behaviour problems showed that older
patients with ConHD have more overall, internalizing, and externalizing problems than
younger patients, respectively r (16) = .67, p = .005, r (14) = .77, p = .001, and r (14) = .73,
p = .003. Disease severity was not significantly related to overall, r (13) = .18, p = .54,
internalizing, r (12) = .11, p = .74, and externalizing problems, r (12) = -.05, p = .88.
Separate analysis of pre-adolescents (mean age > 10 years) showed homogeneous data
sets (Table 2). Pre-adolescents showed more internalizing (medium ES) and to a lesser
extent externalizing problems (small ES) than controls.
Table 2. Cumulated effect size (ES) estimates and residual variation as a function of behaviour
problems after accounting for sampling error
Behaviour problems
k
N
d*
Se2
Sres2
95 % CI
Overall
15
1277
0.47
0.05
0.03
0.42 – 0.52
66
Externalizing
14
1225
0.19
0.05
0.01
0.17 – 0.20
82
Internalizing
14
1225
0.47
0.05
0.03
0.42 – 0.53
62
Externalizing
7
846
0.25
0.03
0.00
0.25 – 0.25
100
Internalizing
7
846
0.56
0.04
0.00
0.56 – 0.56
100
% Var
Mean age > 10 years
Note. k = number of ESs; N = n of patients with ConHD and control group; d* = unbiased ES statistic;
Se2
= variance due to
sampling error; Sres2 = residual variance; 95 % CI = confidence interval for d*; % Var = percentage of variance attributable to
sampling error.
26
55
26
25
39
54
74
30
51
33
54
26
144
24
11
29
Casey et al. (1996)
Ellerbeck et al. (1998)
Goldberg et al. (2000), sample A
Goldberg et al. (2000), sample B
Gupta et al. (2002)
Hövels-Gürich et al. (2002)
Karl et al. (2004)
Oates et al. (1994), sample A
Oates et al. (1994), sample B
Oates et al. (1994), sample C
Oates et al. (1994), sample D
Spurkland et al. (1993)
Utens et al. (1993)
Utens et al. (2001), sample A
Utens et al. (2001), sample B
Wright & Nolan (1994)
69
27
58
59
62
77
38
61
81
Male
9.5
4–7
4-7
10 - 15
16.0
10.4
10.7
10.9
10.1
9.1
10.5
10.1
2.8 - 8
2.8 - 8
8.2
8.8
Age
ToF / TGA
Combined
Combined
Combined
ASD
ASD
VSD
ToF
m, c
s, m
s, m
s, m, c
s,m
s,m
s
m
c
c
TGA
TGA
c
s, m, c
c
c
c
c
Severity
TGA
Combined
SV
HLHS
d-TGA
SV
ConHD
Murmer
Norms
Norms
Norms
Norms
Healthy
Healthy
Healthy
Healthy
Friends
Norms
Norms
Norms
Norms
Siblings
Murmer
Control
0.31
0.05
-0.08
0.44
0.53
0.42
0.52
0.53
0.76
0.35
0.89
0.59
-0.12
-0.14
0.76
0.70
Overall
0.45
0.23
-0.11
0.43
0.47
0.55
0.53
0.74
0.76
0.75
-0.25
-0.14
0.76
0.64
Intern.
0.42
-0.32
-0.18
0.20
0.28
0.35
0.35
0.55
<0.01
0.21
-0.29
-0.22
0.44
-0.21
Extern.
Effect size (Cohen’s d)
problems; Intern. = internalizing problems; Extern. = externalizing problems.
ventricular septum defect. Severity = severity of heart disease; c = complex; m = moderate; s = simple; Control = control group; Murmer = innocent heart murmer; Overall = overall behaviour
defect; HLHS = hypoplastic left heart syndrome; PAD = patent arterial duct; (d-) TGA = (dextro-) transposition of the great arteries; ToF = tetralogy of Fallot; SV = single ventricle; VSD =
Note. N is the sample size of patients with ConHD. Male is the proportion of male patients with ConHD (%). Age is mean or median age of the patients with ConHD in years. ASD = atrium septum
N
Study
Table 1. Overview of studies included in the meta-analysis with respect to behaviour problems
Meta-analysis 33
34 Chapter 2
Overall cognitive functioning
Twenty-five studies were selected for inclusion in the meta-analysis, providing 50 effect
sizes for overall cognitive functioning (Table 3). There was considerable heterogeneity in
the data set (Table 4), which points to significant moderators. Because healthy controls,
patients with innocent heart murmurs, and siblings scored significantly higher on
cognitive functioning (medium ES) as compared to normative data (Table 4), we
substituted their means and SDs by means and SDs of the norm, in order to create a more
homogeneous data set. However, the data set remained heterogeneous.
Correlations between heart disease severity and ESs for cognitive functioning
revealed that patients with severe ConHD exhibited lower cognitive functioning than
patients with less severe ConHD, r (46) = -.45, p = .002. In addition, older patients
showed less adverse cognitive outcome than younger patients, r (50) = .31, p = .03. The
effect of disease severity on cognitive functioning remained after controlling for mean age,
r (43) = -.39, p = .009. The effect of age did not reach significance after controlling for
disease severity, r (43) = .23, p = .12.
Table 4 provides the ESs of overall cognitive functioning for the various congenital
heart defects including: hypoplastic left heart syndrome (HLHS), transposition of the
great arteries (TGA), tetralogy of Fallot (ToF), atrium septum defect (ASD), and
ventricular septum defect (VSD). The data sets are homogeneous, except for ToF. Mean
cognitive functioning was higher among patients with VSD as compared to normative data
(small ES). Cognitive functioning of patients with ASD was within the normative range.
Patients with HLHS and TGA had significantly lower cognitive functioning than normative
data, respectively a large and small ES. For patients with ToF, the analysis showed that
older patients tended to exhibit higher cognitive functioning than younger patients, but
this effect did not reach significance, r (7) = .77, p = .08. For the other patient groups
separately (HLHS, TGA, ASD and VSD), no relation was observed between mean age and
cognitive functioning, all ps > .21. For the patients with VSD, ASD, TGA and HLHS
together, a significant relation between chronological age and cognitive functioning was
found, r (25) = .40, p = .049. However, when patients with HLHS were excluded, the age
effect dissipated, r (21) = .16, p = .48.
To determine whether the relation between chronological age and cognitive
functioning could be explained by the fact that patients with HLHS were tested at a
younger age and to determine whether differences in cognitive functioning between
patient groups could be explained by differences in chronological age, we tested whether
mean age differed between the patient groups (VSD, M = 9.31, SD = 3.05; ASD, M = 10.63,
SD = 2.09; ToF, M = 7.96, SD = 3.08; TGA, M = 8.26, SD = 2.37; HLHS, M = 5.82, SD =
2.08). T tests showed that patients with HLHS were significantly younger than patients
Meta-analysis 35
with ASD, t (8) = 3.37, p = .01. This indicates that the observed age effects on cognitive
functioning for all patients with ConHD were explained by the fact that patients with
HLHS were tested at a younger age. Moreover, this indicates that differences in cognitive
functioning among patients with VSD, ASD, TGA, and ToF could not be explained by
differences in age, but instead by differences in type of heart defect.
Table 4. Cumulated effect size (ES) estimates and residual variation as a function of overall
cognitive functioning after accounting for sampling error
Moderator
k
N
d*
Se2
Sres2
Overall a
50
3654
-0.25
0.06
0.12
-0.47 – -0.02
33
Overall b
50
2668
-0.21
0.06
0.07
-0.35 – -0.07
46
7
514
0.47
0.06
0.01
0.45 – 0.49
85
VSD
5
216
0.18
0.10
0.00
0.18 – 0.18
100
ASD
6
282
0.12
0.09
0.02
0.08 – 0.16
81
ToF
6
452
-0.17
0.05
0.05
-0.27 – -0.06
51
TGA
11
1108
-0.14
0.04
0.01
-0.15 – -0.13
89
HLHS
4
160
-0.82
0.11
0.01
-0.85 – -0.79
88
Healthy controls, innocent
95 % CI
% Var
heart murmer, and siblings
Note. k = number of ESs; N = n of patients with ConHD and control group; d* = unbiased ES statistic; Se2 = variance due to
sampling error; Sres2 = residual variance; 95 % CI = confidence interval for d*; % Var = percentage of variance attributable to
sampling error; ASD = atrium septum defect; HLHS = hypoplastic left heart syndrome; TGA = transposition of the great
arteries; ToF = tetralogy of Fallot; VSD = ventricular septum defect. a Healthy controls, patients with innocent heart murmer
or siblings are included as a comparison group. b Only normative data are used as a comparison group.
N
14
13
7
20
63
77
155
55
34
209
25
23
14
49
7
7
5
5
12
10
8
77
13
Study
Clarkson et al. (1980), sample A
Clarkson et al. (1980), sample B
Clarkson et al. (1980), sample C
Clarkson et al. (1980), sample D
DeMaso et al. (1990), sample A
DeMaso et al. (1990), sample B
Dunbar-Masterson et al. (2001)
Ellerbeck et al. (2001)
Forbess et al. (2002), sample A
Forbess et al. (2002), sample B
Goldberg et al. (2000), sample A
Goldberg et al. (2000), sample B
Haneda et al. (1996), sample A
Haneda et al. (1996), sample B
Haneda et al. (1996), sample C
Haneda et al. (1996), sample D
Haneda et al. (1996), sample E
Haneda et al. (1996), sample F
Haneda et al. (1996), sample G
Hesz & Clark (1998), sample A
Hesz & Clark (1998), sample B
Hövels-Gürich et al. (1997)
Ikle et al. (2003)
71
61
76
57
71
Male
TGA
HLHS
4 – 6.6
VSD
TGA
Shunt
DORV
CAVC
ASD
TGA
ToF
VSD
SV
HLHS
BV
c
c
c
c
c
c
m, c
s, m
c
m
s
c
c
s, m, c
c
c
d-TGA
SV
c
m
c
c
s
m
s
Severity
d-TGA
ToF
d-TGA
TGA
PVD
ToF
VSD
ConHD
5.4
6.6 - 14
6.6 - 14
2 - 13
2 - 13
2 - 13
2 - 13
2 - 13
2 - 13
2 - 13
2.8 - 8
2.8 - 8
5
5
8.2
8.1
5.7
5.7
2.4 - 7
2.4 - 7
2.4 - 7
2.4 - 7
Age
WPPSI-R / WISC-III
K-ABC
WISC-R
WISC-R
SB
SB
SB
SB
SB
SB
SB
BSID / WPPSI-R / WISC-III
BSID / WPPSI-R / WISC-III
WPPSI-R
WPPSI-R
-0.82
-0.06
-0.07
-0.57
<0.01
-0.25
0.40
0.80
0.78
-0.26
0.25
0.43
-0.37
-0.12
-0.64
-0.52
ed.
SB
4th
-0.19
-0.44
WISC-III
WPPSI / LIS
WPPSI / LIS
-0.24
-0.39
ed.
SB
3rd
0.07
-0.57
-0.21
IQ
-0.69
-0.01
-0.56
0.64
-0.06
-0.08
-0.46
-0.02
VIQ
Effect size (d)
SB 3rd ed.
SB 3rd ed.
SB 3rd ed.
IQ measure
Table 3. Overview of studies included in the meta-analysis with respect to cognitive functioning
-0.79
-0.05
-0.59
0.12
-0.65
-0.14
-0.72
-0.34
PIQ
36 Chapter 2
N
13
28
74
14
28
30
51
33
54
31
18
9
13
17
39
23
32
7
35
15
32
26
19
Study
Jedlicka-Köhler et al. (1987)
Jedlicka-Köhler et al. (1995)
Karl et al. (1987)
Kern et al. (1995)
Mahle et al. (2000)
Oates et al. (1995), sample A
Oates et al. (1995), sample B
Oates et al. (1995), sample C
Oates et al. (1995), sample D
O’Dougherty et al. (1985)
Satvinoha et al. (2003)
Tindall et al. (1999), sample A
Tindall et al. (1999), sample B
Utens et al. (1993), sample A
Utens et al. (1993), sample B
Utens et al. (1993), sample C
Utens et al. (1993), sample D
Utens et al. (1993), sample E
Utens et al. (2001), sample A
Utens et al. (2001), sample B
Uzark et al. (1998)
Visconti et al. (1999), sample A
Visconti et al. (1999), sample B
8.8
82
53
62
55
44
58
46
67
57
12.3
10.6
6.3
2.5 - 7
2.5 - 7
13.2
12.7
12.5
12.5
12.9
5.4
5.3
8.5
9.1
10.4
10.7
10.9
10.1
9.0
64
80
4.4
57
9.1
6.4
Age
77
Male
c
HLHS
ASD II
ASD II
SV
Combined
Combined
PS
TGA
ToF
VSD
ASD II
Combined
Combined
ASD
TGA
ASD
VSD
ToF
TGA
s, m
s, m
c
s, m
s, m
s
c
m
s
s,, m
s, m, c
s, m, c
s, m
c
s, m
s
m
c
c
c
TGA
HLHS
c
m
Severity
TGA
ToF
ConHD
ed.
WISC-III
WISC-III
SB
4th
MSCA
MSCA
WISC-R
WISC-R
WISC-R
WISC-R
WISC-R
MSCA
MSCA
DAS
WISC-III
WISC-R
WISC-R
WISC-R
WISC-R
WISC-III
WPPSI-R
WPPSI-R/ WISC-III
HAWIK/ HAWIVA/ HAWIE
HAWIK / HAWIVA/ SB
IQ measure
Table 3. (continued) Overview of studies included in the meta-analysis with respect to cognitive functioning
0.59
0.27
-0.18
-0.23
0.13
-0.02
-0.13
0.56
0.39
-0.16
-0.36
-0.63
-0.44
-0.01
0.07
0.15
<0.01
<0.01
-1.02
-1.32
0.14
0.27
IQ
VIQ
0.48
0.41
0.07
0.14
-0.14
-0.06
-0.73
-0.89
-0.07
-0.47
Effect size (d)
0.57
0.12
<0.01
0.14
0.13
0.07
-1.10
-1.49
0.37
-0.16
PIQ
Meta-analysis 37
20
73
17
30
29
Wernovsky et al. (2000), sample A
Wernovsky et al. (2000), sample B
Wray et al (2001), sample A
Wray et al (2001), sample B
Wright & Nolan (1994)
66
Male
9.5
7.3
7.5
6 - 16
3.7 - 6
Age
ToF/ TGA
Combined
Combined
SV
SV
ConHD
m, c
s, m, c
m, c
c
c
Severity
WISC-R
BAS
BAS
WISC-III
WPPSI-R
IQ measure
-0.41
1.22
-0.24
-0.22
-0.48
IQ
-0.11
-0.05
-0.53
VIQ
-0.60
-0.39
-0.34
PIQ
Effect size (d)
Primary Scale of Intelligence. d = Cohen’s d using normative data; VIQ = verbal intelligence quotient; PIQ = performance intelligence quotient.
Leiter International Scale; MSCA = McCarthy Scales of Children’s Abilities; SB = Stanford Binet Scale; WISC = Wechsler Intelligence Test for Children; WPPSI = Wechsler Preschool and
HAWIK = Hamburger Wechsler Intelligence Test for Children; HAWIVA = Hamburger Wechsler for Children in Pre-school Age; K-ABC = Kaufman Assessment Battery for Children; LIS =
moderate; s = simple; BAS = British Ability Scale; BSID = Bayley Scales of Infant Development; DAS = Differential Ability Scale; HAWIE = Hamburger Wechsler Intelligence Test for Adults;
transposition of the great arteries; ToF = tetralogy of Fallot; Shunt = shunt cases; SV = single ventricle; VSD = ventricular septum defect; Severity = severity of heart disease; c = complex; m =
septum defect (secundum); BV = biventricle; DORV = double outlet right ventricle; HLHS = hypoplastic left heart syndrome; PVD = pulmonary vascular disease; (d-) TGA = (dextro-)
Note. N is the sample size of patients with ConHD. Male is the proportion of male patients with ConHD (%). Age is mean or median age of the patients with ConHD in years. ASD (II) = atrium
N
Study
Table 3. (continued) Overview of studies included in the meta-analysis with respect to cognitive functioning
38 Chapter 2
Meta-analysis 39
Table 5. Cumulated effect size (ES) estimates and residual variation as a function of verbal and
performance intelligence quotients after accounting for sampling error
Behaviour problems
k
N
d*
Se2
Sres2
95 % CI
% Var
Overall
Verbal IQ
16
1466
-0.05
0.04
0.02
-0.33 – 0.24
68
Performance IQ
16
1466
-0.20
0.04
0.07
-0.70 – 0.30
40
Verbal IQ
5
280
0.20
0.07
0.00
0.20 – 0.20
100
Performance IQ
5
280
0.13
0.07
0.00
0.13 – 0.13
100
Verbal IQ
3
390
-0.05
0.03
0.00
-0.05 – -0.05
100
Performance IQ
3
390
-0.29
0.03
0.00
-0.29 – -0.29
100
Verbal IQ
3
104
-0.43
0.13
0.01
-0.66 – -0.23
91
Performance IQ
3
104
-0.88
0.14
0.00
-0.88 – -0.88
100
ASD and VSD
TGA
HLHS
Note. k = number of ESs; N is n of patients with ConHD and control group; d* = unbiased ES statistic; Se2 = variance due to
sampling error; Sres2 = residual variance; 95 % CI = confidence interval for d*; % Var = percentage of variance attributable to
sampling error; ASD = atrium septum defect; HLHS = hypoplastic left heart syndrome; TGA = transposition of the great
arteries; VSD = ventricular septum defect.
Verbal and performance intelligence
Twelve studies (Table 3) were selected for inclusion in the meta-analysis, providing 21 ESs
for verbal IQ (VIQ; verbal comprehensive abilities) and performance intelligence (PIQ;
perceptual organizational abilities). The analysis demonstrated that the data sets of PIQ
and VIQ were characterized by considerable heterogeneity (Table 5). Follow-up analysis
demonstrated that patients with more severe ConHD exhibited lower PIQ and VIQ than
would be expected by normative data, r (20) = -.62, p = .003 and r (20) = -.59, p = .006,
respectively. Moreover, younger patients with ConHD exhibited lower PIQ but not lower
VIQ than normative data, r (21) = .53, p = .01 and r (21) = .38, p = .09, respectively. The
effect of age on PIQ dissipated after excluding patients with HLHS or after controlling for
disease severity, r (17) = .39, p = .13 and r (16) = .32, p = .19, respectively. The effect of
disease severity on PIQ and VIQ remained after controlling for mean age, r (17) = -.42, p =
.07 and r (17) = -.47, p = .04, respectively.
Table 5 provides the ESs of VIQ and PIQ for HLHS, TGA, VSD, and ASD; the data
sets are homogeneous. Patients with ASD and VSD had significantly higher VIQ and PIQ
than normative data, a small and negligible ES, respectively. Patients with HLHS had
lower VIQ and PIQ than norms, respectively a medium and large ES. Patients with TGA
had lower VIQ than normative data (a negligible ES). With respect to PIQ, no
40 Chapter 2
homogeneous data set was obtained for the patients with TGA. Exclusion of one study in
which full-flow cardiopulmonary bypass was used as a surgical technique (ES = 0.34; Karl
et al., 2004), resulted in a homogeneous data set with lower PIQ scores for patients with
TGA as compared to normative data (small ES).
File drawer analysis
We estimated the number of additional studies averaging null findings that would be
necessary to bring the small and medium ESs for psychopathology and cognitive
functioning below a negligible ES, d = |0.1| (Cohen, 1988). The results provide confidence
that the effects found would not be invalidated even if a publication bias existed, since an
increase of 50-850 % in existing numbers of studies would be necessary.
Discussion
Psychopathology
The variance in effect sizes across studies with respect to psychopathology could not solely
be attributed to sampling error. Chronological age appeared to be significantly related to
psychopathology, indicating that age was a significant moderator variable in ConHD.
Specifically, pre-adolescents with ConHD displayed an increased risk of overall,
internalizing (medium ES) and to a lesser extent externalizing problems (small ES). This
effect could not be explained solely by the presence of ConHD since disease severity was
unrelated to psychopathology. These findings suggest that exposure to potential risk
factors during the course of a patient’s life may increase the development of internalizing
behaviour problems in pre-adolescents with ConHD.
The finding that pre-adolescents with ConHD exhibited more internalizing than
externalizing problems is consistent with other reviews on pediatric chronic disease
(Lebovidge, Lavigne, Donenberg, & Miller, 2003; Lavigne & Faier-Routman, 1992). Future
research may focus on the mechanisms that explain increased levels of internalizing
problems among pre-adolescents with ConHD. An overprotective parenting style in
ConHD (Linde, 1982; Casey, Sykes, Craig, Power, & Mulholland, 1996) may be a possible
risk factor for internalizing problems (Gilliom & Shaw, 2004). Alternatively, hormonal
and brain changes during adolescence triggering the expression of genetic vulnerabilities
in combination with potentially stressful disease experiences may increase internalizing
behaviour problems (Walker, Sabuwalla, & Huot, 2004).
Meta-analysis 41
Cognitive functioning
The variance in effect sizes across studies with respect to cognitive functioning could not
solely be attributed to sampling error. Disease severity appeared to be a significant
moderator. That is, a relation between severity of ConHD and cognitive functioning was
observed. Patients with HLHS (large effect size) and patients with TGA (small to medium
effect size) demonstrated decreased cognitive functioning compared to normative data,
specifically in the area of perceptual organizational abilities. Patients with ASD and VSD
showed cognitive functioning within the normative range. An additional finding is that for
the patients with ConHD overall, chronological age was related to cognitive functioning.
However, for the patients with VSD, ASD, TGA, and HLHS separately, no effect of age was
observed. Only younger patients with ToF tended to show decreased cognitive functioning
as compared to older patients. However, this effect did not reach significance. Additional
analysis showed that the observed age effects could be explained by the fact that patients
with severe ConHD, specifically those with HLHS, were tested at an earlier age than
patients with less severe ConHD. Therefore, these findings do not provide evidence that
cognitive functioning in ConHD improved with increasing age.
The finding that severe ConHD resulted in more impaired cognitive functioning
relative to their counterparts with less severe ConHD may be explained by the fact that
severe ConHD is associated with risk factors that may have a cumulative adverse effect on
cognitive functioning. For example, patients with more severe disease are at increased risk
for congenital brain anomalies (Glauser, Rorke, Weinberg, & Clancy, 1990b) that may be
associated with prenatal physiological events (Kaltman, Tian, & Rychik, 2005) and with
chromosomal anomalies (Ternsedt, Chaoui, Korner, & Dietel, 1999). Moreover, patients
with severe heart disease are at increased risk for acquired cognitive impairment (Glauser,
Rorke, Weiberg, & Clancy, 1990a; Trittenwein et al., 2003) as a result of more difficult and
frequent surgery (Clarkson, MacArthur, Barrat-Boyes, Whitlock, & Neutze 1980;
Stavinoha, Fixler, & Mahony, 2003), pre- and postoperative poor cerebral perfusion,
seizures, and physical incapacity (Forbess, Visconti, Bellinger, Howe, & Jonas, 2002;
Newburger, Silbert, Buckley, & Fyler, 1984; Goldberg et al., 2000).
The present results suggest that specifically perceptual organizational abilities are
impaired in TGA and HLHS as compared to normative data. Although, some caution is
warranted, as the number of studies was small, the present findings are in accord with
other studies on children with early brain damage (Ewing-Cobbs, Barnes, & Fletcher,
2003; Muter, Taylor, & Vargha-Khadem, 1997). The basis for the detrimental effects on
perceptual organizational abilities is unclear. One possibility is that, left-hemisphere
injury may cause functional reorganisation of language functions from the left to the right
hemisphere to preserve language functions. This transfer may be achieved at the expense
42 Chapter 2
of visuospatial abilities (Muter et al., 1997). Alternatively, reduced motor abilities resulting
from ConHD and operative recovery time may impede the normal development of motor
and spatial relation skills (Muter et al., 1997; Goldberg et al., 2000).
The present meta-analysis does not support the assumption that cerebral plasticity
reorganises or restores cognitive functioning in ConHD. Instead cognitive functioning
remained relatively stable in patients with TGA, HLHS, ASD, and VSD. A possible
explanation for the observed stability of decreased cognitive functioning in ConHD is that
patients with ConHD suffer from neurological impairment at an early age. Brain damage
at an early age has been shown to be a risk factor for enduring decreased cognitive
functioning (Levin, 2003; Ewings-Cobbs, Barnes, & Fletcher, 2003; Mutter et al., 1997).
One possibility is that, young patients are more vulnerable to brain damage because they
have a less-well-established skill repertoire (Ewings-Cobbs et al., 2003) and because
myelination takes place during that period, which is important for connectivity and
organization of networks in the brain (Levin, 2003).
Limitations of the study
Several potential limitations of this review should be considered. The meta-analysis is
based on the assumption that IQ is normally distributed among patients with ConHD.
However, some studies have shown a non-normal distribution of IQ that is skewed to the
left (e.g., Mahle et al., 2000). This may indicate that the present meta-analysis
underestimates the extent to which patients with ConHD show diminished functioning.
Research has shown a rise in mean intelligence scores during the 20th century
(Rowe & Rodgers, 2001). This so-called Flynn effect may explain why patients with simple
ConHD (e.g., VSD) showed higher cognitive functioning than suggested by normative
data. If the Flynn effect influenced the present findings the adverse effect of ConHD on
cognitive outcome may be underestimated.
In the present study, cognitive functioning of patients with ConHD was compared
to normative data and not to cognitive functioning of a study-recruited control group.
However, a recruited control group provides the opportunity to careful match patients and
controls on demographic characteristics and to control for a possible Flynn effect. The
present study reveals that the study-recruited control groups evidence higher cognitive
functioning than normative data. This indicates that comparison of patients with ConHD
with a recruited control group would have resulted in larger effect sizes than comparison
of patients with normative data. This may suggest that the present findings underestimate
the degree of cognitive dysfunction in ConHD.
The present meta-analysis only included studies that employed tests of overall
cognitive functioning. It is possible, however that patients with ConHD exhibit a deficit in
Meta-analysis 43
a specific area of cognitive functioning. Because IQ scores may average scores on
unaffected and affected areas (Schatz, Finke, Kellett, & Kramer, 2002) the present study
may underestimate cognitive dysfunction in ConHD.
Some caution is warranted with respect to the observed effect of chronological age
on psychopathology. The meta-analysis is cross-sectional, and may therefore be subject to
potential confounds such as cohort effects across studies or sampling biases. Therefore,
the association between chronological age and psychopathology should be viewed only as
suggestive. Prospective studies of children with ConHD and a control group are needed to
verify the observed age effect.
The meta-analysis only relied on studies using the CBCL as a measure of child
psychopathology. However, concerns have been raised regarding the use of the CBCL in
research with children with chronic disease, because the internalizing problem scale
includes items that tap physical symptoms (Perrin, Stein, & Drotar, 1991). One study on
ConHD addressed this issue and demonstrated that the difference between patients and
the reference group remained after excluding items with a somatic content (Utens et al.,
1993). Moreover, the present study showed that severity of heart disease was unrelated to
internalizing problem scores. Therefore, it is unlikely that the specific medical diagnosis
explained an increased report of internalizing problems in pre-adolescents.
Another limitation of the meta-analysis is the potential impact of rater bias on
reported psychopathology in ConHD. Assessment of behaviour problems was exclusively
based on parents’ reports. However, studies comparing parent and child reports have
found that children tend to report more behaviour problems (specifically internalizing)
than their parents (Utens et al., 1993). Consequently, the ratings of caregivers in the
current study may have underestimated the level of internalizing problems in patients
with ConHD.
Conclusions
The present study suggests that the sole presence of ConHD may not affect the
development of internalizing problems. However, the interaction of ConHD and exposure
to potential risk factors during the course of patients’ development can have an adverse
effect on patients’ psychological functioning in pre-adolescence. Moreover, the present
study suggests that severe ConHD may adversely impact on cognitive functioning,
specifically in the area of perceptual organizational abilities. To promote psychological and
cognitive functioning, future research should attempt to unravel the role of possible risk
factors such as diminished cerebral perfusion, treatment characteristics, overprotective
parents, or hospitalizations. Many risk factors are highly interrelated. Therefore, future
studies are required in which cognitive and psychological functioning are assessed
44 Chapter 2
longitudinally and in which homogeneous patient groups are randomly assigned to
medical treatments. Once the impact of individual risk factors is clarified adverse
psychological and cognitive functioning in ConHD can be prevented. Another important
direction for future research is to move beyond the broad focus on internalizing and
externalizing problems and verbal and performance IQ towards the examination of
specific domains of psychopathology and cognitive functioning (e.g., anxiety, depression,
and visual-spatial skills). Overall, the current study suggests that young children with
severe heart disease (HLHS and TGA) may benefit from interventions specifically
targeting perceptual organizational abilities (e.g., visual spatial abilities). Moreover, preadolescents with ConHD may benefit from psychological interventions reducing anxiety
symptoms and depression.
References
Achenbach, T.M., & Edelbrock, C.S. (1983). Manual for the Child Behaviour Checklist and revised
profile. Burlington: University of Vermont, Department of Psychiatry.
* Casey, F.A., Sykes, D.H., Craig, B.G., Power, R., & Mulholland, H.C. (1996). Behavioral
adjustment of children with surgically palliated complex congenital heart disease. Journal
of Pediatric Psychology, 21, 335-352.
* Clarkson, P.M., MacArthur, B.A., Barrat-Boyes, B.G., Whitlock, R.M., & Neutze, J.M. (1980).
Developmental progress after cardiac surgery in infancy using hypothermia and circulatory
arrest. Circulation, 62, 855-861.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ:
Lawrence Erlbaum Associates.
* DeMaso, D.R., Baerdslee, W.R., Silbert, A.R., & Fyler, D.C. (1990). Psychological functioning in
children with cyanotic heart defects. Journal of Developmental and Behavioral Pedaitrics,
11, 289-294.
* Dunbar-Masterson, C., Wypij, D., Bellinger, D.C., Rappaport, L.A., Baker, A.L., Jonas, R.A., &
Newburger, J.W. (2001). General health status of children with D-transposition of the great
arteries after the arterial switch operation. Circulation, 104, I-138-I-142.
* Ellerbeck, K.A., Smith, M.L., Holden, E.W., McMenamin, S.C., Badawi, M.A., Brenner, J.I., Kan,
J.S., & Hyman, S.L. (1998). Neurodevelopmental outcomes in children surviving dtransposition of the great arteries. Journal of Developmental and Behavioral Pediatrics,
19, 335-341.
Ewing-Cobbs, L., Barnes, M.A., & Fletcher, J.M. (2003). Early brain injury in children:
development and reorganization of cognitive function. Developmental Neuropsychology,
24, 669-704.
Meta-analysis 45
* Forbess, J.M., Visconti, K.J., Bellinger, D.C., Howe, R.J., & Jonas, R.A. (2002).
Neurodevelopmental outcomes after biventricular repair of congenital heart defects.
Journal of Thoracic and Cardiovascular Surgery, 123, 631-639.
Foster, E., Graham, T.P., Driscoll, D.J., Reid, G.J., Reiss, J.G., Russell, I.A., Sermer, M., Siu, S.C.,
Uzark, K., Williams, R.G., & Webb, G.D. (2001). Task force 2: special health care needs of
adults with congenital heart disease. Journal of the American College of Cardiology, 37,
1176-1183.
Gardner, F.V., & Angelini, G.D. (1995). Psychological aspects of congenital heart disease.
Cardiology in the Young, 5, 302- 309.
Gilliom, M., & Shaw, D.S. (2004). Codevelopment of externalizing and internalizing problems in
early childhood. Developmental Psychopathology, 16, 313-333.
Glass, G.V., McGaw, B., & Smith, M.L. (1981). Meta-analysis in social research. Beverly Hills, CA:
Sage.
Glauser, T.A., Rorke, L.B., Weinberg, P.M., & Clancy, R.R. (1990a). Acquired neuropathologic
lesions associated with the hypoplastic left heart syndrome. Pediatrics, 85, 991-1000.
Glauser, T.A., Rorke, L.B., Weinberg, P.M., & Clancy, R.R. (1990b). Congenital brain anomalies
associated with the hypoplastic left heart syndrome. Pediatrics, 85, 984-990.
* Goldberg, C.S., Schwarz, E.M., Brunberg, J.A., Mosca, R.S., Bove, E.L., Schork, M.A., Stetz, S.P.,
Cheatham, J.P., & Kulik, T.J. (2000). Neurodevelopmental outcome of patients after the
fontan operation: A comparison between children with hypoplastic left heart syndrome and
other functional single ventricle lesions. Journal of Pediatrics, 137, 645-652.
Griffin, K.J., Elkin, T.D., & Smith, C.J. (2003). Academic outcomes in children with congenital
heart disease. Clinical Pediatrics, 42, 401-409.
* Gupta, S., Giuffre, R.M., Crawford, S., & Waters, J. (2001). Covert fears and anxiety in asthma and
congenital heart disease. Child: Care, Health, and Development, 27, 335-348.
Gruneau, R.E., Whitfield, M.F., & Petrie J. (2000). Predicting IQ of biologically "at risk" children
from age 3 to school entry: sensitivity and specificity of the Stanford-Binet Intelligence
Scale IV. Journal of Developmental Behavior in Pediatrics, 21, 401-407.
* Haneda, K., Itoh, T., Togo, T., Ohmi, M., & Mohri, H. (1996). Effects of cardiac surgery on
intellectual function in infants and children. Cardiovascular Surgery, 4, 303-307.
Hedges, L.V., & Olkin, I. (1985). Statistical methods for meta-analysis. Orlando, FL: Academic
Press.
* Hesz, N., & Clark, E.B. (1988). Cognitive development in transposition of the great vessels.
Archives of Disease in Childhood, 63, 198-200.
Hofstra, M.B., Van der Ende, J., & Verhulst, F.C. (2000). Continuity and change of
psychopathology from childhood into adulthood: a 14-year follow-up study. Child and
Adolescent Psychiatry, 37, 850-858.
* Hövels-Gurich, H.H., Seghaye, M., Däbritz S., Messmer, B.J., & von Bernuth, G. (1997). Cognitive
and motor development in preschool and school-age children after neonatal switch
operation. Journal of Thoracic Cardiovascular Surgery, 114, 578-585.
46 Chapter 2
* Hövels-Gurich, H.H., Konrad, K., Wiesner, M., Minkenberg, R., Herpertz-Dahlmann, B.,
Messmer, B.J., & von Bernuth, G. (2002). Long term behavioural outcome after neonatal
arterial switch operation for transposition of the great arteries. Archives of Disease in
Childhood, 87, 506-510.
Hunter, J.E., & Schmidt, F.L. (1990). Methods of meta-analysis: correcting error and bias in
research findings, (1st ed.). Newbury Park, CA: Sage Publications.
* Ikle, L., Hale, K., Fashaw, L., Boucek, M., & Rosenberg, A.A. (2003). Developmental outcome of
patients with hypoplastic left heart syndrome treated with heart transplantation. Journal
of Pediatrics, 142, 20-25.
*Jedlicka-Köhler, I., Sinko-Sanz, K., Schlemmer, M., & Wimmer, M. (1995). Kognitive Entwicklung
von Kindern und Jugendlichen nach Korrektur einer Transposition der großen Gefäße.
[Cognitive development of children and adolescents after correction of transposition of
great vessels]. Klinische Pädiatrie, 207, 68-72.
*Jedlick-Köhler, I., & Wimmer, M. (1987). Der Einfluß des Operationszeitpunktes auf die
intellektuelle und psychosziale Entwicklung bie Kindern mit Fallotischer Tetralogie. [Effect
of timing of surgery on the intellectual and psychosocial development of children with
tetralogy of Fallot]. Klinische Pädiatrie, 199, 86-89.
Kaltman, J.R., Tian, H.D.I.Z., & Rychik, J.R. (2005). Impact of congenital heart disease on
cerebrovascular blood flow dynamics in the fetus. Ultrasound in Obstetrics and
Gynaecology, 25, 32-36.
* Karl, T.R., Hall, S.M., Ford, G., Kelly, E.A., Brizard, C.P.R., Mee, R.B.B., Weintraub, R.G.,
Cochrane, A.D., & Glidden, D. (2004). Arterial switch with full-flow cardiopulmonary
bypass and limited circulatory arrest: neurodevelopmental outcome. Journal of Thoracic
and Cardiovascular Surgery, 127, 213-222.
* Kern, J.H., Hinton, V.J., Nereo, N.E., Hayes, C.J., & Gersony, W.M. (1998). Early developmental
outcome after the nordwood procedure for hypoplastic left heart syndrome. Pediatrics,
102, 1148-1152.
Lavigne, J.V., & Faier-Routman, J. (1992). Psychological adjustment to pediatric physical
disorders: a meta-analytic review. Journal of Pediatric Psychology, 17, 133-157.
Lebovidge, J.S., Lavigne, J.V., Donenberg, G.R., & Miller, M.L. (2003). Psychological adjustment of
children and adolescents with arthritis: a meta-analytic review. Journal of Pediatric
Psychology, 28, 29-39.
Levin, H.S. (2003). Neuroplasticity following non-penetrating traumatic brain injury. Brain Injury,
17, 665-674.
Linde, L.M. (1982). Psychiatric aspects of congenital heart disease. Psychiatric Clinics of North
America, 5, 399-406.
* Mahle, W.T., Clancy, R.R., Moss, E.M., Gerdes M., Jobes, D.R., & Wernovsky, G. (2000).
Neurodevelopmetal outcome and lifestyle assessment in school-aged and adolescent
children with hypoplastic left heart syndrome. Pediatrics, 105, 1082-1089.
Meta-analysis 47
McGrath, E., Wypij D., Rappaport, L.A., Newburger, J.W., & Bellinger, D.C., (2004). Prediction of
IQ and Achievement at age 8 years from neurodevelopmental status at age 1 year in
children with D-transposition of the great arteries. Pediatrics, 114, e572-e576.
Muter, V., Taylor, S., & Vargha-Khadem, F. (1997). A longitudinal study of early intellectual
development in hemiplegic children. Neuropsychologia, 35, 289-298.
Newburger, J.W., Silbert, A.R., Buckley, L.P., & Fyler, D.C. (1984). Cognitive function and age at
repair of transposition of the great arteries in children. New England Journal of Medicine,
310, 1495-1499.
* Oates, R.K., Simpson, J.M., Cartmill, T.B., & Turnbull, J.A.B. (1995). Intellectual function and age
of repair in cyanotic congenital heart disease. Archives of Disease in Childhood, 72, 298301.
* Oates, R.K., Turnbull, J.A.B., Simpson, J.M., & Cartmill, T.B. (1994). Parent and teacher
perceptions of child behaviour following cardiac surgery. Acta Paediatrica, 83, 1303-1307.
* O’Dougherty, M., Wright F.S., Loewenson, R.B., Torres, F. (1985). Cerebral dysfunction after
chronic hypoxia in children. Neurology, 35, 42- 46.
Paul, M.H., & Wessel, H.U. (1999). Exercise studies in patients with transposition of the great
arteries after atrial repair operations (Mustard / Senning): a review. Pediatric Cardiology,
20, 49 -55.
Perrin, E.C., Stein, R.E.K., & Drotar, D. (1991). Cautions in using the Child Behaviour Checklist:
Observations based on research about children with a chronic disease. Journal of Pediatric
Psychology, 16, 411-421.
Rowe, D.C., & Rodgers J.L. (2002). Expanding variance and the case of historical change in IQ
means: a critique of Dickens and Flynn (2001). Psychological Review, 109, 759-763.
Samango-Sprouse C., & Suddaby, E.C. (1997). Developmental concerns in children with congenital
heart disease. Current Opinion in Cardiology, 12, 91-98.
Samerhoff A.J., Seifer R., Baldwin, A., & Baldwin, C. (1993). Stability of intelligence from preschool
to adolescence: the influence of social and family risk factors. Child Development, 64, 8097.
Schatz, J., Flinke, R.L., Kellett, J.M., & Kramer, J.H. (2002). Cognitive functioning in children with
sickle cell disease: a meta-analysis. Journal of Pediatric Psychology, 27, 739-748.
Shillingford, A.J., & Wernovsky, G. (2004). Academic performance and behavioral difficulties after
neonatal and infant heart surgery. Pediatric Clinics of North America, 51, 1625-1639.
*Spurkland I, Bjornstad PG, Lindberg H, & Seem E. (1993). Mental health and psychosocial
functioning in adolescents with congenital heart disease. A comparison between
adolescents born with severe heart defect and atrial septal defect. Acta Paediatrica, 82, 7176.
* Stavinoha, P.L., Fixler, D.E., & Mahony, L. (2003). Cardiopulmonary bypass to repair an atrial
septal defect does not affect cognitive function in children. Circulation, 107, 2722-2725.
* Tindall, S., Rothermell, R.R., Delamater, A., Pinsky, W., & Klein, M.D. (1999). Neuropsychological
abilities of children with cardiac disease treated with extracorporeal membrane
oxygenation. Developmental Neuropsychology, 16, 101-115.
48 Chapter 2
Tennsedt, C., Chaoui, R., Korner, H., & Dietel, M. (1999). Spectrum of congenital heart defects and
extracardiac malformations associated with chromosomal abnormalities: results of a seven
year necropsy study. Heart, 82, 34-39.
Trittenwein, G., Nardi, A., Pansi, H., Golej, J., Burda, G., Hermon, M., Boigner, H., & Wollenek, G.
(2003). Early postoperative prediction of cerebral damage after pediatric cardiac surgery.
Annuals of Thoracic Surgery, 76, 576-580.
* Utens, E.M.W.J., Verhulst, F.C., Meijboom, F., Duivenvoorden, H.J., Erdman, R.A.M., Bos, E.,
Roelandt, J.R.T.C., & Hess, J. (1993). Behavioural and emotional problems in children and
adolescents with congenital heart disease. Psychological Medicine, 23, 415-424.
*Utens, E.M.W.J., Versluis-Den, Bieman, H.J., Witsenburg, M., Bogers, J.J.C., Verhulst, F.C., &
Hess, J. (2001). Cognitive, and behavioural and emotional functioning of young children
awaiting elective cardiac surgery or catheter intervention. Cardiology in the Young, 11, 153160.
* Uzark, K., Lincoln, A., Lamberti, J.L., Mainwaring, R.D., Spicer, R.L., & Moore, J.W. (1998).
Neurodevelopmental outcomes in children with fontan repair of functional single ventricle.
Pediatrics, 101, 630-603.
* Visconti, K.J., Bichell, D.P., Jonas, R.A., Newburger, J.W., & Bellinger, D.C. (1999).
Developmental outcome after surgical versus interventional closure of secundum atrial
septal defect in children. Circulation, 100, II-145-II-150.
Walker, E.F., Sabuwalla, Z., & Huot, R. (2004). Pubertal neuromaturation, stress sensitivity, and
psychopathology. Developmental Psychopathology, 16, 807-824.
Warnes, C.A., Liberthson, R., Danielson, G.K., Dore, A., Harris, L., Hoffman, J.I., Somerville, J.,
Williams, R.G., & Webb, G.D. (2001). Task force 1: the changing profile of congenital heart
disease in adult life. Journal of the American College of Cardiology, 37, 1170-1175.
Wechsler, D. (1991). Wechsler Intelligence Scales for Children, 3rd ed. San Antonio: Psychological
Corporation.
* Wernovsky, G., Stiles, K.M., Gauvreau, K., Gentles, T.L., duPlessis, A.J., Bellinger, D.C., Walsh,
A.Z., Burnett, J., Jonas, R.A., Mayer, J.E., & Newburger, J.W. (2000). Cognitive
development after the Fontan operation. Circulation, 102, 883-889.
Whittington, C.J., Podd, J., & Kan, M.M. (2000). Recognition memory impairment in Parkinson’s
disease: power and meta-analyses. Neuropsychology, 14, 233-246.
Wray, J., & Sensky, T. (1998). How does the intervention of cardiac surgery affect the selfperception of children with congenital heart disease? Child: Care Health and
Development, 24, 57-72.
* Wray, J., & Sensky, T. (2001). Congenital heart disease and cardiac surgery in childhood: effects
on cognitive function and academic ability. Heart, 85, 687-691.
* Wright, M., & Nolan, T. (1994). Impact of cyanotic heart disease on school performance. Archives
of Disease in Childhood, 71, 64-70.
Heart symptoms induced by false heart rate
feedback in high trait anxious patients with
congenital heart disease
Karsdorp, P.A., Kindt, M., Rietveld, S., Everaerd, W., & Mulder, B.J.M. (submitted for
publication).
50 Chapter 3
Abstract
The aim of the present study was to test whether harmless heart cues will result in an
increased perception of heart symptoms in patients with congenital heart disease
(ConHD) and high trait anxiety. Forty-six patients with ConHD and 56 healthy controls
performed two exercise tasks. During one of the exercise tasks participants were exposed
to a harmless heart cue consisting of false heart rate feedback (regular or irregular).
Perceived heart symptoms were assessed and heart rate, arterial partial pressure of CO2,
and respirator rate were monitored continuously. In line with the predictions, false heart
rate feedback resulted in an increased perception of heart symptoms in high trait anxious
patients with ConHD that could not be explained by acute heart dysfunction. However,
unexpectedly this effect was not observed immediately after the false heart rate feedback
task but after a second exercise task without false feedback. The results suggest that not
the sole presence of ConHD, but ConHD in combination with high trait anxiety results in a
vulnerability to overperceive heart symptoms.
False feedback 51
Introduction
Due to advances in medical and surgical treatment, most of the patients with congenital
heart disease (ConHD) will reach adulthood nowadays (Warnes et al., 2001). In spite of
this increased life expectancy some patients experience a reduced quality of life (Rietveld
et al., 2002; Kamphuis et al., 2002). To develop psychological treatment aimed at
improving the quality of life of adults with ConHD, researchers have become interested in
the mechanisms that may explain a diminished quality of life.
Several hypotheses have been proposed that may explain these mechanisms. For
instance, the influential somatic hypothesis postulates that the heart defect directly and
linearly increases perceived heart symptoms and in turn decreases patients’ quality of life
(e.g., Hager & Hess, 2005; Rose et al., 2005). However, in sharp contrast to this
hypothesis, the severity of heart disease turned out to be only weakly related to physical
symptoms and quality of life (e.g., Kamphuis et al., 2002; Rose et al., 2005). These
findings resulted in the development of the symptom perception hypothesis stating that
experienced heart symptoms are explained by perceptual biases, such as selective
attention and negative interpretation of physical sensations (e.g., Pennebaker, 1982).
According to the symptom perception hypothesis and the vulnerability-stress
hypothesis, high trait anxious patients with chronic disease are vulnerable to develop
perceptual biases (Beurs et al., 2005; Watson & Pennebaker, 1989; Zvolensky, Kotov,
Antipova, & Schmidt, 2005). That is, disease experiences in combination with long-lasting
vulnerabilities, such as high trait anxiety, may result in stressful experiences with disease.
These experiences are stored in cognitive memory structures or so-called illness schemes.
Perception of disease-related cues may activate such an illness scheme, eliciting
perceptual biases for disease-related symptoms (Pennebaker, 1982). As a result, patients
with chronic disease may not only perceive physical symptoms due to physiological
changes, they may also perceive symptoms based on cues that are unrelated to their actual
bodily state, such as disease-related environmental cues (e.g., a hospital setting) or false
expectations of becoming ill (e.g., Hoehn-Saric & McLeod, 2000; Koyama, McHaffie,
Laurienti, & Coghill, 2005).
The aim of the present study was to test whether false perception of heart rate
changes will result in a perceptual bias for heart symptoms in high trait anxious patient
with ConHD. We manipulated the false perception of heart rate changes by exposing
patients and healthy controls to false heart rate feedback (Vallins, 1966). We included a
healthy control group to test whether a combination of ConHD (disease experience) and
trait anxiety influenced the perception of symptoms rather than solely trait anxiety. Each
participant accomplished two standardized physical exercise tasks on a treadmill, one with
52 Chapter 3
false feedback of either a regular or an irregular heart rate and one without feedback. The
regular heart rate feedback was included to test whether awareness of ones heart rate in
general or whether specifically an irregular heart rate increased perceived heart
symptoms. The exercise tasks were meant to induce ambiguous physiological arousal that
may increase uncertainty about the functioning of the heart (Schachter & Singer, 1962).
An exercise task without feedback was included to exclude the possibility that perceived
heart symptoms could be explained solely by the exercise task, by differences in exertion
or baseline levels of perceived heart symptoms. To exclude the possibility that the
perception of symptoms could be explained by acute heart dysfunction in ConHD, cardiac
functioning was monitored continuously. We predicted that the false heart rate feedback,
specifically feedback of an irregular heart rate, would elicit an increased perception of
heart symptoms in high trait anxious patients with ConHD. Moreover, we predicted that
this increased perception could not be explained by acute heart dysfunction.
Method
Participants
Consecutive adult patients with ConHD were selected from the outpatient clinics of
cardiology in the Academic Medical Centre, in Amsterdam. Inclusion criteria were: age
between 18 and 55 years and no mental retardation. Forty-four percent of the contacted
patients participated in the experiment (n =46). A cardiologist classified the heart defects
into complex, moderate, and simple ConHD based on risk of morbidity and mortality,
according to the classification system presented at the 32nd Bethesda Conference (Warnes
et al., 2001). No differences were found between the patients that participated and those
that did not participate, according to age, gender, and disease severity (p >.05). A healthy
comparison group (n = 56) was recruited via advertisements.
Two patients with ConHD showed heart rhythm disturbances during the
experiment and therefore had to be excluded from further analysis. Trait anxiety scores of
two healthy controls were missing. Two patients with ConHD and 2 participants from the
control group noticed that the regular heart rate feedback was false. Six patients with
ConHD and 8 participants from the control condition noticed that the irregular-feedback
was false. These patients were excluded from further analysis, leaving the sample size to
36 patients with ConHD (11 with complex, 11 with moderate, and 14 with simple ConHD)
and 44 healthy participants. Twenty-nine of the patients with ConHD had undergone
cardiac surgery or intervention to repair or correct their cardiac defect, 17 patients used
heart medication, and 10 had experienced heart rhythm disturbances in the past. Age and
gender did not differ significantly (all ps > .05) between patients with ConHD (17 women
False feedback 53
and 19 men; mean age = 31.69 years, SD = 8.68, range 19-54 years) and healthy
participants (18 women and 27 men; mean age = 29.18 years, SD = 9.73, range 18-54
years).
Due to technical errors, the heart rate, arterial partial pressure of CO2, and
respiratory rate were not recorded for 1, 4, and 3 patients with ConHD, respectively, and
for 1 healthy control. The local ethical committee of the Amsterdam Medical Centre and
the University of Amsterdam approved the study.
Design
We used a 2 Feedback (feedback versus no feedback) x 2 Sound (regular versus irregular)
fractional factorial design, with feedback as within-subject variable and sound as betweensubject variable. The order of the two exercise tasks (feedback and no feedback) was
randomized across participants. Seventeen patients and 24 healthy controls received the
feedback condition first. Moreover, participants were randomly assigned to the regular or
the irregular heart rate feedback condition. Sixteen patients and 17 controls were assigned
to the regular feedback condition.
Materials
False heart rate feedback
The heart rate feedback was created by means of digitally recorded drum sounds, such
that it resembled the typical heart sounds that are perceived using a stethoscope. The
drum sounds were transformed into two heart sounds of 20 seconds: a regular and an
irregular heart sound. The regular sound consisted of a heart rate of 115 beats per minute
(b/m). The irregular heart sound consisted of a heart rate of 115 b/m followed by skipping
heartbeats and a sudden increase in heart rate until 210 b/m. Two hi-fi speakers placed at
the left side of the treadmill were connected to a computer and generated the heart rate
sounds.
Trait anxiety
We used a Dutch translation of the 20-item Spielberger trait version of the State-Trait
Anxiety Inventory (STAI) to measure trait anxiety (Van der Ploeg, Defares, & Spielberger,
1979; Spielberger, Gorsuch, & Lusheve, 1970). Response categories vary from 1 “almost
never” to 4 “almost always.” Total scores ranged from 20 to 80. Psychometric performance
(reliability and validity) of the trait version of the Dutch STAI is satisfactory (Spielberger
et al., 1970).
54 Chapter 3
Perception of heart symptoms versus non-heart symptoms
A 3-item symptom scale was constructed that assessed three experienced heart symptoms:
heart palpitations, rapid heart rate, and chest pain. Item selection was based on a pilot
study that showed that these symptoms are the most frequently experienced symptoms
among patients with ConHD (n = 131) as compared to healthy controls (n = 111), Fs (1,
240) ≥ 6.37, ps ≤ .01, η²s ≥ .03. All participants rated orally on a 5-point scale the degree
to which they experienced these 3 symptoms (1 “not at all” to 5 “very much”). The heart
symptoms were pooled and named “heart symptoms.”
Manipulation check
At the end of the experiment, we assed whether participants were aware of the false heart
rate manipulation. The participants rated on a 5-point scale how much they believed the
false feedback reflected their own heart rate. (1 = “not at all” to 5 “very much”).
Participants scoring 1 were excluded from the analysis.
Physiology
Heart rate, respiratory rate, and arterial partial pressure of CO2, were monitored
continuously to exclude the possibility that acute heart dysfunction could explain
perceived heart symptoms in ConHD. Heart rate was monitored from three Ag/AgCl
electrodes, attached via the modified lead-2 placement. Respiratory rate and arterial
partial pressure of CO2 were monitored with a Capnogard etco2 monitor (Novametrix,
Medical Systems, Walingsford, CT, USA). Arterial partial pressure of CO2 (mmHg) was
estimated by measuring the PetCO2 (CO2 pressure) in the exhaled air at the end of a
normal expiration. A tube was inserted in the nostrils of the participants.
Heart rate was also monitored with a polar vantage heart rate monitor, which was
strapped around the chest of the participant (Polar electro Oy, FIN-90440 Kempele,
Finland). This monitor signalled the research assistant when the participant’s heart rate
reached 120 b/m. At this moment, the false feedback was presented.
Procedure
The experiment consisted of two exercise tasks on a treadmill for each participant: a
feedback and a non-feedback task. Between the two tasks there was a ten-minute
relaxation period. The experiment was conducted under supervision of a cardiologist who
sat in an adjacent room and watched the ECG recording for safety reasons and to
determine whether patients showed heart rhythm disturbances or extrasystoles.
Participants were told that the experiment was concerned with the assessment of
their physical condition and their experience of physical sensations. After informed
False feedback 55
consent, the physiological recording equipment was attached to the participant. Moreover,
a small microphone was attached near the heart region of the participant. Research
assistant A explained that she would register the participants’ heart rate by the
microphone, the headphone, and the polar heart rate monitor. Both the microphone and
the headphone were dummy equipment, used to give the impression that heart sounds
were recorded.
The exercise task consisted of six stages in which the speed was raised gradually:
2.5, 4, 5, 6, 7, and 8 km/hour, respectively. Participants had to walk for 30 seconds in each
stage. It took 10 seconds for research assistant B to raise the speed. The exercise task
maximally lasted 5 minutes.
In the feedback task, research assistant A controlled the manipulation of the
feedback sounds. As soon as the polar heart rate monitor signalled a heart rate of 120 b/m,
research assistant A said “listen to this!” to assistant B, pressed a button to play one of the
false heart rate sounds, and signalled research assistant B to stop raising the speed of the
treadmill. In the non-feedback task, assistant A only signalled to stop raising the speed for
20 seconds (normally the duration of the heart rate feedback) and pressed a button to
mark the physiological signals, which was necessary for the analysis of the physiological
data. After the false feedback, or 20 seconds in the non-feedback task, the speed of the
treadmill was reset to 2.5 km/hour for one minute. During this period, research assistant
B assessed participants’ experienced symptoms. After the first exercise task, the
physiological recording equipment were disconnected, the participant relaxed for ten
minutes, and the second exercise task was performed. Participants were interviewed about
the heart rate manipulation. Next, all equipment was disconnected and participants were
instructed about a questionnaire booklet containing the STAI and biographical questions,
which they had to complete at home. Finally, the participants were paid and ensured that
the false feedback did not reflect their real heart rate.
Data reduction
To test the effect of false heart rate, the dependent variable was derived from change
scores, i.e. by subtracting mean perceived heart symptoms in the non-feedback condition
from mean perceived heart symptoms in the feedback condition (∆M heart = M
non-feedback).
feedback
–M
Positive scores of heart symptoms (∆M heart) indicate an increased perception of
heart symptoms during false feedback relative to non-feedback.
The physiological date were averaged over a one-minute period, 20 seconds after
the heart rate had reached 120 b/m. In this period perceived symptoms were assessed. For
these physiological variables, also change scores were calculated.
56 Chapter 3
Statistical analyses
To test the prediction that a combination of trait anxiety and ConHD would result in an
increased perception of heart symptoms specifically after the irregular heart rate feedback
a 2 ConHD (ConHD versus healthy) x 2 Sound (irregular versus regular) x 4 Trait Anxiety
(low, medium low, medium high, and high trait anxious) x 2 Exercise Order (first versus
second exercise task with feedback) ANOVA was conducted with heart symptoms as the
dependent variables and ConHD, trait anxiety, sound, and exercise order, as between
subjects-factors. The participants were divided in a low and high trait anxious group based
on quartiles (25th, 50th, and 75th percentiles were 33, 38, and 43, respectively). If the effect
of trait anxiety turned out to be significant, a post-hoc linear regression analysis was
conducted with trait anxiety as independent variable and heart symptoms as dependent
variable. For the effects without trait anxiety post-hoc ANOVA’s and t tests were
conducted. Note that we also performed the analysis with age, sex, exercise time,
physiology as covariates. The results of these analyses were not presented here because
they yielded very similar results.
To test whether acute heart dysfunction could explain differences in perceived
heart symptoms, a similar ANOVA and linear regression analysis was conducted as with
heart symptoms, but now with either change in physiology as dependent variables. We
conducted a Spearman rank correlation and t tests to determine whether either disease
severity (healthy controls excluded), use of medication, heart rhythm disturbances in the
past, and cardiac interventions (all dichotomous variables) were related to the perception
of heart symptoms. Finally, in order to test whether trait anxiety was influenced by the
sole presence of ConHD, a one-way ANOVA was performed with ConHD as betweensubjects factor, and a Spearman Rank correlation was performed between disease severity
and trait anxiety.
Results
Perception of heart symptoms
The ANOVA showed a significant main effect of trait anxiety on perceived heart
symptoms, and two significant three-way interactions between ConHD, sound, and
exercise order, and between sound, trait anxiety, and exercise order, all Fs > 2.77, ps < .05,
η²s > .12. However, post-hoc analyses for these effects did not reach significance (all ps >
.05).
Furthermore, the ANOVA revealed a significant three-way interaction between
ConHD, trait anxiety, and exercises order, F (1, 50) = 6.82, p =.01, η² = .12. Post-hoc
linear regression analysis showed that the interaction term Trait Anxiety x ConHD did not
False feedback 57
explain a significant amount of variance of perceived heart symptoms for the participants
receiving false feedback in the second exercise task, β = -.12, t (38) = -0.72, p = .48.
However, for the participants receiving false feedback in the first exercise task, post-hoc
linear regression analysis showed that the interaction term Trait Anxiety x ConHD
explained a significant amount of variance of perceived heart symptoms, β = -.36, t (40) =
-2.44, p = .02. As shown in Figure 1, in contrast to our predictions trait anxiety was related
to a decreased perception of heart symptoms after false heart rate feedback relative to
non-feedback as compared to healthy controls.
To determine whether this unpredicted finding could be explained by a decreased
perception of heart symptoms during false feedback or by an increased perception during
the non-feedback condition, we conducted two additional linear regression analyses, with
perceived heart symptoms during either the false feedback or the non-feedback task as
dependent variables. These analyses were only conducted for the participants receiving
the false-feedback during the first exercise task. The interaction term ConHD x Trait
Anxiety explained a significant amount of variance in perceived heart symptoms during
the non-feedback exercise task, β = .37, t (40) = 2.48, p = .02, and not during the false
feedback exercise task, β = .10, t (40) = 0.61, p = .55. Inspection of the scatter plots
revealed that high trait anxious patients with ConHD showed an increased perception of
heart symptoms during the exercises task without false feedback when they were exposed
to false heart rate feedback in a previous exercise task.
Figure 1. Regression slopes depicting the relationship between trait anxiety and change in
perceived heart symptoms after feedback in the false feedback first condition.
58 Chapter 3
Finally, the predicted interaction between either ConHD, trait anxiety, and sound
or ConHD, trait anxiety, sound, and exercise order did not reach significance, F (1, 50) =
2.27, p =.14, η² = .04 and F (3, 50) = 2.05, p =.12, η² = .11, respectively. This indicated that
the observed interaction between trait anxiety, ConHD, and exercise order was not
restricted to feedback of irregular heart rate but was also observed in the regular feedback
condition.
Group differences in heart function
The ANOVA only revealed that participants showed a larger increase in heart rate after
regular heart rate feedback than after irregular heart rate feedback, F (1, 48) = 5.32, p
=.03, η² = .10. Follow-up paired t tests showed that the heart rate (M = 114, SD = 15) after
regular feedback tended to be higher than after no feedback (M = 110, SD = 20), t (45) =
1.83, p = .07, whereas the heart rate after the irregular feedback did not differ from the
heart rate after no feedback.
For respiratory rate the ANOVA revealed a significant three-way interaction
between ConHD, sound, and trait anxiety, and for PetCO2 two significant two-way
interactions between sound and trait anxiety, sound and exercise order, and two
significant three-way interactions between ConHD, sound, and trait anxiety and between
ConHD, sound, and exercise order, all Fs > 3.04, all ps < .03, all η²s > .10. However, posthoc analysis did not reveal significant effects (all ps > .05).
Severity of heart disease was unrelated to change in reported heart symptoms, r
(36) = .05, p = .77. Moreover, the same pattern was observed for use of medication, heart
rhythm disturbances in the past, and cardiac interventions (all ps > .05).
Trait anxiety
A one-way ANOVA showed that patients with ConHD (M = 40.33, SD = 9.59) did not
significantly differ on trait anxiety from controls (M = 38.06, SD = 9.44), F (1, 78) = 1.13, p
= .29, η² = .01. Severity of heart disease was unrelated to trait anxiety, r (36) = -.10, p =
.55.
Discussion
The prediction that false heart rate feedback would increase the perception of heart
symptoms in individuals with ConHD who are also high trait anxious was only partially
confirmed. As predicted high trait anxious patients with ConHD showed an increased
perception of heart symptoms subsequently to the false heart rate feedback. However,
unpredictably this increased symptom perception was not yielded immediately after the
False feedback 59
false heart rate feedback, but only in the second exercise task subsequent to the task with
false heart rate feedback. Moreover, this effect was obtained not only after the irregular
false feedback, but also after the regular false feedback. The increased perception of heart
symptoms in high trait anxious patients with ConHD could not be explained by
simultaneous cardiac dysfunction. Patients with ConHD and healthy controls did not
differ in their physiological responses. Moreover, the patients with ConHD included in this
study did not show uncommon heart rhythm disturbances or extrasystoles during the
experiment. Finally, severity of heart disease was unrelated to the perception of heart
symptoms. In contrast to the somatic hypothesis, the present study suggests that the sole
presence of cardiac dysfunction does not necessarily result in the perception of heart
symptoms. Instead, exposure to harmless heart cues and perceptual biases, due to a
combination of trait anxiety and a history of ConHD, seem to moderate the relation
between heart function and perceived heart symptoms in ConHD.
The unexpected finding that the false heart rate feedback did not immediately
evoke biased perception in high trait anxious patients with ConHD may be explained by
the competition of cues hypothesis (Pennebaker 1982). According to this hypothesis
individuals attend less to internal sensory information in the presence of salient external
environmental information. Possibly, high anxious patients may have allocated their
attention to the false heart rate feedback (e.g., Parkinson, 1985; Rietveld, Karsdorp &
Mulder, 2004; Stern, Botto, & Herrick, 1972), rather than to heart rate changes in their
own body. This may have counteracted the tendency of high trait anxious patients with
ConHD to perceive increased heart-related symptoms immediately after the false heart
rate feedback.
The finding, that high trait anxious patients only showed an increased perception
of heart symptoms after exposure to false feedback in the second exercise task, indicates
that patients expected to experience cardiac dysfunction during the second task. Due to
these catastrophic expectations, high trait anxious patients may have directed their
attention to their own heart to search for possible signs of cardiac dysfunction and
misinterpreted harmless heart rate changes as signs of cardiac dysfunction (Pennebaker,
1982).
The finding that the regular heart rate feedback evoked similar responses as the
irregular heart rate feedback, suggests that the regular feedback also induced catastrophic
beliefs about heart functioning. This assumption is also supported by the finding that the
regular heart rate feedback induced increases in real heart rate in all participants. This
may be due to the fact that the regular heart rate feedback was false and incongruent to
the real heart rate, inducing uncertainty about the heart condition. In addition, high trait
anxious patients with ConHD may habitually interpret an increased heart rate as a sign of
60 Chapter 3
heart dysfunction, irrespective of whether it is regular or not. Finally, it is possible that
any cue that is somehow associated with the heart may elicit hypervigilance towards heart
symptoms in high trait anxious patients with ConHD.
An alternative explanation for the increased perception of heart symptoms in high
anxious patients with ConHD is that this feedback induced parallel changes in the viscera
and autonomic nervous system in these patients (e.g., Crucian et al., 1999; Ehlers,
Margraf, Roth, Taylor, & Birbaumer, 1988). The present study showed that the regular
heart rate feedback tended to induce heart rate increases immediately after exposure to
the false feedback. However, high anxious patients with ConHD did not show a different
physiological response during the assessment of heart symptoms. Therefore, physiological
responses induced by the false feedback could not explain the observed increase in
symptom perception in this group.
We assumed that the level of trait anxiety is independent of the presence of heart
disease. Alternatively, the heart defect may have increased the level of trait anxiety
(Connoly, McClowry, Hayman, Mahony, & Artman, 2004) or trait anxiety may have
increased the severity of heart disease (Sher, 2005). Little support for these assumptions
has been found in the present study, since trait anxiety was unrelated to the severity of
heart disease.
Some caution is warranted about the generalization of the findings, as the response
rate and sample sizes were relatively low. Because the order of the exercise tasks with and
without feedback unexpectedly affected the perception of heart symptoms, it is possible
that the power was too small to reveal significant effects of the regular or the irregular
heart rate feedback. Another limitation of the present study is that experiences with
disease in general rather than with heart disease are related to an increased perception of
heart symptoms, as we only included a healthy control group. Conversely, it has been
shown that patients with asthma display biased perceptions towards asthma-related
symptoms (breathlessness) and not towards heart-related symptoms such as heart
pounding (Rietveld & Houtveen, 2004). This may imply that an increased perception of
heart-related symptoms is specific to patients with ConHD.
The present findings suggest that ConHD in combination with high trait anxiety
explains overperception of heart symptoms. This finding is consistent with previous
studies on ConHD (Karsdorp, Kindt, Rietveld, Everaerd, & Mulder, in press). High
anxious patients with ConHD may interpret harmless heart-related cues, such as acute
stress, (Karsdorp et al., in press), perceived heart rate changes, and expectations and
thoughts about disease, as signs of cardiac dysfunction. This may encourage patients to
scan their body for possible signs of cardiac dysfunction, increasing their perception of
heart symptoms. In case of heart dysfunction, this may be an adaptive response because
False feedback 61
patients may act appropriately and in turn increase their survival chances. However, in the
absence of acute heart dysfunction, overperception of heart symptoms may unduly result
in avoidance of physical and social activities (Rietveld et al., 2004) and unnecessary
doctor visits (e.g., Ehlers, Mayou, Sprigings, & Birkhead, 2000). High anxious patients
with ConHD who are bothered by physical symptoms despite good medical care may
benefit from psychological interventions such as biofeedback training (O’Brien, Reid, &
Jones, 1998). This may be helpful, because it increases the accuracy of heart beat
perception and may reduce the negative effect of false believes and expectations about
heart function.
References
Connoly, D., McClowry, S., Hayman, L., Mahony, L., & Artman, M. (2004). Posttraumatic stress
disorder in children after cardiac surgery. Journal of Pediatrics, 144, 480-484.
Crucian, G.P., Hughes, J.D., Barrett, A.M., Williamson, D.J.G., Bauer, R.M., Bowers, D., & Heilam,
K.M. (2000). Emotional and physiological responses to false feedback. Cortex, 36, 623647.
De Beurs, E., Comijs, H., Twisk, J.W.R., Sonnenberg, C., Beekman, A.T.F., & Deeg, D. (2005).
Stability and change of emotional functioning in late life: modelling of vulnerability
profiles. Journal of Affective Disorders, 84, 53-62.
Ehlers, A., Margraf, J., Roth, W.T., Taylor, B., & Birbaumer, N. (1988). Anxiety induced by false
heart rate feedback in patients with panic disorder. Behaviour Research and Therapy, 26,
1-11.
Ehlers, A., Mayou, R.A., Sprigings, D.C., & Birkhead, J. (2000). Psychological and perceptual
factors associated with arrhythmias and benign palpitations. Psychosomatic Medicine, 62,
693-702.
Hager, A., & Hess, J. (2005). Comparison of health related quality of life with cardiopulmonary
exercise testing in adolescents and adults with congenital heart disease. Heart, 91, 517-520.
Hoehn-Saric, R., & McLeod, D.R. (2000). Anxiety and arousal: physiological changes and their
perception. Journal of Affective Disorders, 61, 217-224.
Karsdorp, P.A., Kindt, M., Rietveld S., Everaerd, W., & Mulder, B.J.M. (in press). Stress-induced
heart symptoms and perceptual biases in patients with congenital heart disease.
International Journal of Cardiology.
Kamphuis, M., Ottenkamp, J., Vliegen, H.W., Vogels, T., Zwinderman, K.H., Kamphuis R.P., &,
Verloove-Vanhorick, S.P. (2002). Health related quality of life and health status in adult
survivors with previously operated complex congenital heart disease. Heart, 87, 356-362.
Koyama, T., McHaffie, J.G., Laurienti, P.J., & Coghill, R.C. (2005). The subjective experience of
pain: Where expectations become reality. Proceedings of the National Academy of
Sciences, 102, 12950 -12955.
62 Chapter 3
O’Brien, W.H., Reid, G.J., & Jones, K.R. (1998). Differences in heartbeat awareness among males
with higher and lower levels of systolic blood pressure. International Journal of
Psychophysiology, 29, 53-63.
Parkinson, B. (1985). Emotional effects of false autonomic feedback. Psychological Bulletin, 98,
471-494.
Pennebaker, J.W. (1982). The psychology of physical symptoms. New York: Springer-Verlag.
Rietveld, S., & Houtveen, J.H. (2004). Acquired sensitivity to relevant physiological activity in
patients with chronic health problems. Behaviour Research and Therapy, 42, 137-153.
Rietveld, S., Karsdorp, P.A., & Mulder, B.J.M. (2004). Heartbeat sensitivity in adults with
congenital heart disease. International Journal of Behavioral Medicine, 11, 203-211
Rietveld, S., Mulder, B.J., Van Beest, I., Lubbers, W., Prins, P.J., Vioen, S., Bennebroek-Evererz, F.,
Vos, A., Casteelen, G., & Karsdorp, P (2002). Negative thoughts in adults with congenital
heart disease. International Journal of Cardiology, 86, 19-26.
Rose, M., Köhler, K., Köhler, F., Sawitzky, B., Fliege, H., & Klap, B.F. (2005). Determinants of the
quality of life of patients with congenital heart disease. Quality of Life Research, 14, 35-43.
Schachter, S., & Singer J. (1962). Cognitive, social, and physiological determinants of emotional
state. Psychological Review, 69, 121-128.
Sher, L. (2005). Type D personality: the heart, stress, and cortisol. Quarterly Journal of Medicine,
98, 232-239.
Spielberger, C.D., Gorsuch, R., & Lusheve, R. (1970). STAI Manual for the State-Trait Anxiety
Inventory. Palo Alto, CA: Consulting Psychologists Press.
Stern, R.M., Botto, R.W., & Herrick, C.D. (1972). Behavioral and physiological effects of false heart
rate feedback: a replication and extension. Psychophysiology, 9, 21-29.
Vallins S. (1966). Cognitive effects of false heart-rate feedback. Journal of Personality and Social
Psychology, 4, 400-408.
Van der Ploeg, H.M., Defares, H.B., & Spielberger, C.B. (1979). Handleiding bij de
zelfbeoordelingsvragenlijst. Een nederlandse bewerking van de Spielberger State-Trait
Anxiety Inventory. [Validity of the Zelf-Beoordelings-Vragenlijst. A Dutch version of the
Spielberger State-Trait Anxiety Inventory]. Lisse: Zwets and Zeitlinger.
Warnes, C.A., Liberthson, R., Danielson, G., Dore, A., Harris, L., Hoffman, J.I.E., Sommerville, J.,
Williams, R.G., & Webb, G.D. (2001). Task force 1: The changing profile of congenital heart
disease in adult life. Journal of American College of Cardiology, 37, 1170-1175.
Watson, D., & Pennebaker J.W. (1989). Health complaints, stress and distress: exploring the
central role of negative affectivity. Psychological Review, 96, 234-254.
Zvolensky, M.J., Kotov, R., Antipova, A.V., & Schmidt, N.B. (2005). Diathesis stress model for
panic-related distress: a test in a Russian epidemiogical sample. Behaviour Research and
Therapy, 43, 521-532.
Stress-induced heart symptoms and perceptual
biases in patients with congenital heart disease
Karsdorp, P.A., Kindt, M., Rietveld, S., Everaerd, W., & Mulder, B.J.M. (in press).
International Journal of Cardiology.
64 Chapter 4
Abstract
The aim of the present study is to clarify whether biased symptom perception towards
heart symptoms may explain a reduced quality of life in patients with congenital heart
disease (ConHD). The present study tested the hypothesis that the combination of ConHD
and high trait anxiety increases the perception of heart symptoms during acute stress.
Twenty-five patients and 24 healthy participants completed a stressful computer task. The
participant’s heart and non-heart symptoms were measured after stress and after
relaxation. Heart rate, blood pressure, respiratory rate, and arterial partial pressure of CO2
were monitored continuously. In line with the prediction, a combination of high trait
anxiety and ConHD resulted in an increased perception of specifically heart symptoms
during stress. Moreover, the increased perception of heart symptoms could not be
explained by acute heart dysfunction. Heart dysfunction is not the only cause of an
increased perception of heart symptoms. A history of disease experience in combination
with high trait anxiety may increase the perception of heart symptoms during stress and
may eventually result in an increased risk of developing a reduced quality of life.
Stress 65
Introduction
Research suggests that only some patients with congenital heart disease (ConHD) are
vulnerable to developing a reduced quality of life (Rietveld et al., 2002). Several
hypotheses have been proposed to explain which patients with ConHD are at risk. A
classic view designated the somatic hypothesis states that heart disease is directly related
to experienced heart symptoms and quality of life (Hager & Hess, 2005; Rose et al., 2005).
Accordingly, patients with severe heart disease may experience a reduced quality of life. In
contrast, however, there is compelling evidence that disease severity is only weakly related
to the perception of symptoms and quality of life (Rose et al., 2005; Kamphuis et al.,
2002).
Alternative views, denoted the symptom-perception and the vulnerability-stress
hypothesis, postulate that personality traits and learning experiences with disease,
moderate the relation between ConHD and perceived heart symptoms (Pennebaker, 1982;
De Beurs et al., 2005). High trait anxiety in combination with chronic disease may result
in negative and stressful experiences with disease and symptoms (De Beurs et al., 2005;
Dersh, 2001; Zvolensky, Kotov, Antipova, & Schmidt, 1981). These experiences may be
stored in cognitive memory structures or so-called illness schemes (Pennebaker, 1982).
Perception of cues that are associated with these schemes may elicit processing biases
towards disease-related sensations (Pennebaker, 1982; Bower, 1981). Examples of these
processing biases are a tendency to draw attention to disease-related sensations, and
interpreting these ambiguous sensations as disease–related symptoms (Pennebaker 1982;
Rietveld, Van Beest, & Everaerd, 1999). Acute stressors, such as an intelligence test, have
been shown to elicit such processing biases in anxiety prone individuals (Houtveen,
Rietveld, & De Geus, 2003; Steptoe & Vögele, 1992) and in patients with chronic disease
(Rietveld et al., 1999, Rietveld & Houtveen, 2004).
The aim of the present study was to clarify whether a combination of trait anxiety
and experiences with ConHD explains an increased perception of heart symptoms in
ConHD during acute stress. We predicted that the combination of high trait anxiety and
ConHD would result in an increased perception of specifically heart symptoms during
stress that could not be explained by acute heart dysfunction (heart rate, blood pressure,
respiratory rate, and arterial partial pressure of CO2).
66 Chapter 4
Method
Participants
Consecutive adult patients with ConHD were selected from the outpatient clinics of
cardiology in the Academic Medical Centre, in Amsterdam. Inclusion criteria were: age
between 18 and 65 years and no mental retardation. Twenty-five percent of the contacted
patients participated in the experiment (10 women and 15 men, mean age = 32.70 years,
SD = 11.37, range 21 to 64 years). A cardiologist classified the heart defects into complex,
moderate, and simple ConHD, based on risk of morbidity and mortality and according to
the classification system that was presented at the 32nd Bethesda Conference of the
American College of Cardiology (Warnes et al., 2001). Seven patients had complex (e.g.,
transposition of the great arteries), 10 moderate (e.g., tetralogy of Fallot), and 8 had
simple ConHD (e.g., VSD). Fifteen patients had undergone cardiac surgery or intervention
to repair or correct their cardiac defect, twelve patients used heart medication, and seven
had experienced heart rhythm disturbances in the past. Age and disease severity did not
differ between patients that participated and those that did not participate (p >.05).
However, a smaller proportion of women participated than the proportion of women that
did not participate (p =. 04).
To test whether a combination of ConHD (disease experience) and trait anxiety
influenced the perception of symptoms rather than solely trait anxiety, a comparison
group was recruited, consisting of 24 healthy adults (13 women and 12 men, mean age =
27.29 years, SD = 10.64, range 19 to 55 years). Age and gender did not differ significantly
between patients with ConHD and healthy participants (p > .05). The local ethical
committee of the Amsterdam Medical Centre and the University of Amsterdam approved
the study.
Materials
Mental stress task
Participants completed a mental stress task to elicit processing biases for heart-related
symptoms. This task was an intelligence test, consisting of questions presented on a
computer screen for 30 seconds (Rietveld & Houtveen, 2004). A reaction time task was
presented simultaneously, in which randomly falling red and green coins were to be seen
on the screen. When a green coin was falling on either the left or the right side,
participants had to press the left or right button, respectively. The computer
acknowledged each response with a brief auditory signal: a musical tone indicating a
correct response and a low frequency buzz indicating an error. Initially, participants could
win 100 euros, which were represented on the screen. After a wrong answer this amount
Stress 67
decreased rapidly. Due to the difficulty of the questions, none of the participants won any
money.
Perception of heart symptoms
A symptom scale was constructed that assessed perceived heart and non-heart symptoms.
The non-heart symptoms were included to assess perceptual biases for specifically heart
symptoms rather than for unspecific symptoms. Item selection was based on a pilot study,
in which patients with ConHD (N = 31) rated on a 7-point scale (1 “to a very small degree”
to 7 “to a very strong degree”) whether symptoms from the Pennebaker Inventory of
Limbic Languidness (PILL; Pennebaker, 1982) and a Dutch symptom index (Rietveld &
Houtveen, 2004) signaled heart disease. The mean scores for the selected heart and nonheart symptoms ranged from 3.27 to 4.84 and from 1.14 to 1.97, respectively. The five
heart symptoms were: heart palpitations, rapid heartbeat, shortness of breath, dizziness
and chest pain. The five non-heart symptoms were: running nose, ringing ears,
stomachache, itch, and watering eyes.
State anxiety
State anxiety was assessed to determine whether the stress task did indeed result in a
subjective stress response. To measure state anxiety, we used a 2-item, 7-point scale on
which the participants rated the degree of experienced anxiety and tenseness (1 “very
small degree” to 7 “very strong degree”; Rietveld & Houtveen, 2004). The two items were
pooled and named ‘state anxiety’.
Trait anxiety
We used a Dutch translation of the 20-item Spielberger trait version of the state-trait
anxiety inventory (STAI; Spielberger, Gorush, & Lusheve, 1970; Van der Ploeg, Defares, &
Spielberger, 1979). Total scores ranged from 20 to 80. Psychometric performance
(reliability and validity) of the Dutch trait version of the STAI is satisfactory (Van der
Ploeg et al., 1979).
Physiology
Heart rate, diastolic and systolic blood pressure, respiratory rate, and arterial partial
pressure of CO2 were monitored continuously; to exclude the possibility that acute heart
dysfunction could explain perceived heart symptoms. Heart rate was monitored from
three Ag/AgCl electrodes, attached via the modified lead-2 placement. A cardiologist
analyzed the ECG registration for abnormal heart rhythm disturbances and extrasystoles.
Diastolic and systolic blood pressures (mm Hg) were monitored from the middle finger of
68 Chapter 4
the left hand using a Finapress (Ohmeda 2300E). Arterial partial pressure of CO2 was
estimated by measuring the PetCO2 (CO2 pressure, mm Hg) in the exhaled air at the end of
a normal expiration. PetCO2 and respiratory rate were monitored from a tube inserted in
the nostrils using the Capnogard etco2 monitor (Novametrix, Medical Systems,
Walingsford, CT, USA).
Procedure
During the enrollment it was explained to potential participants that the experiment
consisted of a computer task. Participants completed the STAI-trait questionnaire at
home. After that, they attended the experiment consisting of three within-subject
conditions: (1) a baseline period (15 minutes), (2) a mental stress task (10 minutes), and
(3) a recovery period (15 minutes). After informed consent, the experimenter attached the
physiological recording equipment. Next, participants watched a relaxing movie and rated
their symptoms and emotions. Subsequently, participants completed the mental stress
task. Meanwhile, a research assistant, who was wearing a white doctor’s coat to symbolize
professionalism, made notes and gave standardized negative feedback every 2 minutes.
After the task, participants rated their symptoms and emotions. Finally, participants
resumed watching the relaxing movie and rated their symptoms and emotions. Finally,
participants were paid for participation (12 euros) and explained about the difficulty of the
questions and the negative feedback.
Data reduction
To test whether trait anxiety specifically affected heart symptoms in ConHD, the
dependent variable, i.e. perceived heart symptoms, was construed by subtracting mean
scores of perceived non-heart symptoms from mean scores of perceived heart symptom
(∆M heart = M heart symptoms – M non-heart symptoms). In addition, the effect of induced stress on the
reported symptoms was calculated by change scores, i.e. by subtracting scores during
recovery from scores during stress (∆M stress response = M stress - M recovery). The recovery scores
were used instead of the baseline scores in order to eliminate the effect of anticipation
anxiety during the baseline period. Positive change scores of relative heart symptoms (∆M
heart, stress response)
indicate an elevated perception of specifically heart symptoms (as
compared to non-heart symptoms) during stress relative to the recovery period. Negative
change scores indicate a decreased perception of specifically heart symptoms during stress
relative to the recovery period.
The physiological data were averaged over the last five minutes of baseline and
recovery and over the total stress task. Also, for these physiological variables, change
Stress 69
scores were calculated by subtracting mean scores during recovery from mean scores
during stress.
Statistical analysis
To determine whether stress indeed resulted in a subjective and physiological stress
response, a repeated measure MANOVA was conducted with state anxiety or the
physiological measures as dependent variables and stress level (baseline, stress, and
recovery) as within-subject factor.
To test the hypothesis that a combination of trait anxiety and ConHD would result
in an increased perception of heart symptoms during stress, a multiple regression analysis
was conducted with the relative change in heart symptoms (∆M
heart, stress response)
as the
dependent variable. At the first step, the main effects of trait anxiety, and ConHD were
entered. At the second step, the interaction between trait anxiety and ConHD was entered.
Trait anxiety was log10 transformed to obtain normal distributions.
To rule out the possibility that acute heart dysfunction could explain differences in
perceived heart symptoms, a similar multiple regression analysis was performed, but now
with change in the physiological measures as dependent variables. Moreover, we
conducted a Spearman rank correlation and ANOVA to test whether disease severity was
related to the perception of heart symptoms. Finally, we conducted a Spearman rank
correlation and ANOVA to analyze whether the sole presence of ConHD was related to
trait anxiety.
Results
Stress manipulation check
A repeated measure MANOVA showed that the stress manipulation had succeeded. That
is, a significant main effect of stress was obtained for the physiological measures, all Fs ≥
4.62, ps ≤ .02, η²s ≥ .18, with higher heart rate, respiratory rate, diastolic and systolic
blood pressure during stress than during baseline and recovery, all ts ≥ 3.06, p < .01. Also,
the stress task induced a subjective stress response, F (2, 47) = 45.69, p < .001, η² = .66,
with higher state anxiety scores during stress (M = 2.16, SD = 0.80) than during baseline
(M = 1.24, SD = 0.38) or recovery (M = 1.17, SD = 0.36), all ts ≥ 8.88, p < .001.
Perception of heart symptoms
Mean scores and standard deviations for perceived heart and non-heart symptoms are
presented in Table 1. Note that in the table, the ConHD and control group are split into a
low and high trait anxiety group for ease of interpretation. For the statistical analysis, trait
70 Chapter 4
anxiety remained a continuous variable. Two healthy controls were considered outliers, as
their change scores of relative heart symptoms (∆M
heart, stress response)
were extremely
negative (> 3 SD from the mean). However, the results were similar with these outliers
included.
Table 1. Means and standard deviations of heart and non-heart symptoms in patients with
ConHD and healthy controls
Congenital heart disease
Control
LT-anxiety a
HT-anxiety a
LT-anxiety a
HT- anxiety a
(n = 11)
(n = 14)
(n = 14)
(n = 8)
M (SD)
M (SD)
M (SD)
M (SD)
Baseline
1.07 (0.13)
1.16 (0.21)
1.06 (0.12)
1.05 (0.09)
Stress
1.04(0.08)
1.41 (0.42)
1.16 (0.26)
1.15 (0.23)
Recovery
1.02 (0.06)
1.10 (0.17)
1.06 (0.17)
1.12 (0.21)
Baseline
1.05 (0.09)
1.13 (0.31)
1.24 (0.45)
1.12 (0.21)
Stress
1.05 (0.13)
1.14 (0.23)
1.16 (0.24)
1.10 (0.21)
Recovery
1.02 (0.06)
1.20 (0.27)
1.13 (0.20)
1.10 (0.21)
Stress
-0.02 (0.17)
0.27 (0.51)
0.00 (0.34)
0.05 (0.26)
Recovery
0.00 (0.09)
-0.10 (0.30)
-0.07 (0.27)
0.03 (0.13)
-0.02 (0.14)
0.37 (0.40)
0.07 (0.13)
0.03 (0.17)
Heart symptoms
Non-heart symptoms
∆M heart
b
∆M heart, stress response c
Note. Based on the median split of the STAI-T (Me = 32) the sample was split into a low (LT) and high trait (HT) anxious
a
group.
b
Mean heart symptoms minus mean non-heart symptoms.
c
Mean relative heart symptoms during stress minus
recovery .
Table 2. Hierarchical multiple regression of trait anxiety, ConHD, and the interaction effect on
changes in perceived heart symptoms a
Step
Variable
β
1
ConHD
0.14
log10 Trait Anxiety
0.38*
2
ConHD
-4.90*
log10 Trait anxiety
-0.11
log10 Trait anxiety x ConHD
5.22*
R2
adjusted R2
0.19**
0.16
0.31**
0.26
Note. N = 47. Mean heart symptoms (relative to non-heart symptoms) during stress minus mean heart symptoms (relative
a
to non-heart symptoms) during recovery. * p < .05, two-tailed; ** p < .01, two-tailed.
Stress 71
Figure 1. Regression slopes depicting the relationship between trait anxiety and change in
perceived heart symptoms for patients with ConHD and healthy controls.
Change in mean heart
symptoms is mean heart symptoms (relative to non-heart symptoms) during stress minus mean heart symptoms (relative to
non-heart symptoms) during recovery. Positive scores indicate an increased perception of specifically heart symptoms
during stress.
In the regression analysis, the main effects of ConHD and trait anxiety explained a
significant amount of variance in changes in relative heart symptoms (∆M heart, stress response),
R2 = .19, F (4, 44) = 5.28, p < .01 (Table 2). Trait anxiety was the only significant
contributor to the variance explained, indicating that high trait anxious participants
perceived more heart symptoms than low trait anxious participants. At step 2, the two-way
interaction between trait anxiety and ConHD subsumed the main effect of trait anxiety
and significantly explained an additional amount of variances in changes in relative heart
symptoms, ∆R2 = .11, ∆F (1, 43) = 6.94, ∆p = .01. As shown in Figure 1, among patients
with ConHD, higher trait anxiety resulted in an increased perception of specifically heart
symptoms during stress than among the healthy controls.
Group differences in heart function
In the regression analysis, the main effects of ConHD and trait anxiety, did not explain a
significant amount of variance in heart rate, respiratory rate, PetCO2, diastolic and systolic
blood pressure, all R2s < .09, Fs < 2.30, ps > .11. At step 2, the two-way interaction
between trait anxiety and ConHD did not significantly explain an additional amount of
variance in heart rate, respiratory rate, PetCO2, diastolic and systolic blood pressure, all
∆R2s < .03, ∆Fs < 1.35, ∆ps > .25. Note, that two patients with ConHD and one healthy
72 Chapter 4
control were excluded (scores > 3 SD from the mean) for PetCO2 and diastolic / systolic
blood pressure, respectively, to obtain normal distributions.
None of the patients with ConHD showed extrasystoles or abnormal heart rhythm
disturbances during the experiment. Finally, severity of heart disease, use of medication,
heart rhythm problems in the past, operations, and time since last hospital admission
were unrelated to perceived heart symptoms (all ps >.05).
Trait anxiety
A two-way ANOVA showed that patients with ConHD (M = 35.80, SD = 10.85) did not
significantly differ on trait anxiety from controls (M = 30.92, SD = 6.45), F (1, 45) = 3.63,
p = .06, η² = .07. Severity of heart disease was unrelated to trait anxiety, r (25) = .02, p >
.05.
Discussion
The main prediction, that the combination of trait anxiety and ConHD would result in a
larger increase in specifically perceived heart symptoms during stress, was confirmed.
Moreover, the increased perception of heart symptoms in the high trait anxious patients
with ConHD could not be explained by the direct physiological effect of the heart defect
itself. That is, patients with ConHD did not show uncommon heart rhythm disturbances
or extrasystoles during the experiment. In addition, patients with ConHD and controls did
not differ in their physiological response (heart rate, diastolic and systolic blood pressure,
respiratory rate, and partial arterial pressure of CO2). Also, the finding that the severity of
heart disease was unrelated to the perception of heart symptoms was in line with the
assumption that sole the presence of heart disease only weakly influences the perception
of heart symptoms. This study demonstrates that psychological factors as opposed to
somatic factors determine the increased perception of heart symptoms in patients with
ConHD. A perceptual bias for heart sensations, due to a history of ConHD and high trait
anxiety, may serve as a good candidate to explain individual differences with respect to
perceived heart symptoms in patients with ConHD.
The finding that high trait anxious patients showed an increased perception of
heart symptoms supports the hypothesis that trait anxiety is a vulnerability factor in
ConHD (De Beurs et al., 2005; Zvolensky et al., 2005; Kendler, Kuhn, & Prescott, 2004).
High trait anxious patients with ConHD may show an increased perception of heart
symptoms in two ways. Firstly, high trait anxious patients with ConHD may have a
lowered threshold for the perception of changes in heart rate, resulting in a more accurate
perception of heart rate (Critchley, Wiens, Rothstein, Öhman, & Dolan, 2004; Van der
Stress 73
Does, Antony, & Ehlers, 2000; Williams, Watt, Macleod, & Mathews, 1997). Secondly,
anxious patients may show an increased tendency for false positives (Williams et al.,
1997), i.e. perceiving heart symptoms without actual heart rate changes. Although this
perceptual bias may have a survival value, because failure of responding to signals of heart
dysfunction (false negatives) is more costly for survival than responding when there is no
actual heart dysfunction (false positives), it may also be dysfunctional. Trait anxiety may
force patients with ConHD to perceive innocuous sensations as heart symptoms. This bias
may increase the stressfulness of experiences with heart disease and may diminish the
quality of life (Rietveld et al., 2002).
The present finding that acute stress triggered perceptual biases for heart-related
symptoms in patients with ConHD is in line with other studies. Acute stress triggered
perceptual biases for disease-related symptoms in patients with asthma and irritable
bowel syndrome (breathlessness and rectal sensitivity, respectively) and in anxiety prone
individuals (Rietveld et al., 1999; Steptoe & Vögele, 1992; Dickhaus et al., 2003).
A key assumption in this study was that trait anxiety moderates the relationship
between ConHD and perceptual biases for heart symptoms. However, an alternative
hypothesis may be that the presence of ConHD caused the development of trait anxiety
(Connoly, McClowry, Hayman, Mahony, & Artman, 2004) and thus mediates the
relationship between heart disease and symptom perception. The present study does not
support this view, since severity of heart disease was unrelated to trait anxiety. Moreover,
other studies observed that patients with ConHD did not show higher trait anxiety (Cox,
Lewis, Stuart, & Murphy, 2002; Utens et al., 1994). Therefore, the current available
evidence does not warrant readjustment of our assumption.
Some caution is warranted to the generalizability of the findings as the response
rate and sample sizes were relatively low. The smaller proportion of women participating
versus not participating indicates that the study has been subject to some selection bias.
Inspection of the trait anxiety scores suggests that high trait anxious individuals were
somewhat underrepresented. Due to this restriction of range, the observed relation
between trait anxiety and biased symptom perception may be underestimated.
Notwithstanding these limitations, the present study demonstrates that, in
ConHD, a history of disease experiences in combination with trait anxiety is related to an
increased perception of specifically heart symptoms during acute stress. This suggests that
high trait anxious patients with ConHD perceiving heart symptoms without acute heart
dysfunction may benefit from psychological interventions. These interventions should be
aimed at reducing a tendency to attend to heart-related sensation and interpret harmless
heart sensations as heart symptoms. Ideally, these interventions should be applied in
74 Chapter 4
childhood to reduce the stressfulness of disease related experiences, and in turn to prevent
the development of perceptual biases and diminished quality of life.
References
Bower, G.H. (1981). Mood and memory. American Psychologist, 36, 128-148.
Connoly, D., McClowry, S., Hayman, L., Mahony, L., & Artman, M. (2004). Posttraumatic stress
disorder in children after cardiac surgery. Journal of Pediatrics, 144, 480-484.
Cox, D., Lewis, G., Stuart, G., & Murphy, K. (2002). A cross-sectional study of the prevalence of
psychopathology in adults with congenital heart disease. Journal of Psychosomatic
Research, 52, 65-68.
Critchley, H.D., Wiens, S., Rothstein, P., Öhman, A., & Dolan, R.J. (2004). Neural systems
supporting interoceptive awareness. Nature Neuroscience, 7, 189-195.
De Beurs, E., Comijs, H., Twisk, J.W.R., Sonnenberg, C., Beekman, A.T.F., & Deeg, D (2005).
Stability and change of emotional functioning in late life: modelling of vulnerability
profiles. Journal of Affective Disorders, 84, 53-62.
Dersh, J. (2001). Chronic spinal disorder and psychopathology: research findings and theoretical
considerations. Spine Journal, 1, 88-94.
Dickhaus, B., Mayer, E.A., Firooz, N., Stains, J., Conde, F., Olivas, T.I., Fass, R., Change, L., Mayer,
M., & Naliboff, B.D. (2003). Irritable bowel syndrome patients show enhanced modulation
of visceral perception by auditory stress. American Journal of Gastroenterology, 98, 135143.
Hager, A., & Hess, J. (2005). Comparison of health related quality of life with cardiopulmonary
exercise testing in adolescents and adults with congenital heart disease. Heart, 91, 517-520.
Houtveen, J.H., Rietveld, S., & De Geus, E.J.C. (2003). Exaggerated perception of normal
physiological responses to stress and hypercapnia in young women with numerous
functional somatic symptoms. Journal of Psychosomatic Research, 55, 481-490.
Kamphuis, M., Ottenkamp, J., Vliegen, H.W., Vogels, T., Zwinderman, K.H., Kamphuis R.P., &
Verloove-Vanhorick, S.P. (2002). Health related quality of life and health status in adult
survivors with previously operated complex congenital heart disease. Heart, 87, 356-362.
Kendler, S.K., Kuhn, J., & Prescott, C.A. (2004). The interrelationship of neuroticism, sex, and
stressful life events in the prediction of episodes of major depression. American Journal of
Psychiatry, 161, 631-636.
Pennebaker, J.W. (1982). The psychology of physical symptoms. New York: Springer-Verlag.
Rietveld, S., Van Beest, I., & Everaerd, W. (1999). Stress-induced breathlessness in asthma.
Psychological Medicine, 29, 1359-1366.
Rietveld, S., & Houtveen, J.H. (2004). Acquired sensitivity to relevant physiological activity in
patients with chronic health problems. Behaviour Research and Therapy, 42, 137-153.
Stress 75
Rietveld, S., Mulder, B.J., Van Beest, I., Lubbers, W., Prins, P.J., Vioen, S., Bennebroek-Evererz, F.,
Vos, A., Casteelen, G., & Karsdorp, P. (2002). Negative thoughts in adults with congenital
heart disease. International Journal of Cardiology, 86, 19-26.
Rose, M., Köhler, K., Köhler, F., Sawitzky, B., Fliege, H., & Klap, B.F. (2005). Determinants of the
quality of life of patients with congenital heart disease. Quality of Life Research, 14, 35-43.
Spielberger, C.D., Gorsuch, R., & Lusheve, R. (1970). STAI Manual for the State-Trait Anxiety
Inventory. Palo Alto (CA): Consulting Psychologists Press.
Steptoe, A., & Vögele, C. (1992). Individual differences in the perception of bodily sensations: the
role of trait anxiety and coping style. Behaviour Research and Therapy, 30, 597-607.
Utens, E.M.W.J., Verhulst, F.C., Erdman, R.A.M., Meijboom, F.J., Duivenvoorden H.J., Bos, E.,
Roelandt, J.R., & Hess, J. (1994). Psychosocial functioning of young adults after surgical
correction for congenital heart disease in childhood; a follow-up study. Journal of
Psychosomatic Research, 38, 745-758.
Van der Does, A.J.W., Antony, M.M., Ehlers, A., & Barsky, A.J. (2000). Heartbeat perception in
panic disorder: a reanalysis. Behaviour Research and Therapy, 38, 47-62.
Van der Ploeg, H.M., Defares, H.B., & Spielberger, C.B. (1979). Handleiding bij de
zelfbeoordelingsvragenlijst. Een nederlandse bewerking van de Spielberger State-Trait
Anxiety Inventory. [Validity of the Zelf-Beoordelings-Vragenlijst. A Dutch version of the
Spielberger State-Trait Anxiety Inventory]. Lisse: Zwets and Zeitlinger.
Warnes, C.A., Liberthson, R., Danielson, G., Dore, A., Harris L., Hoffman, J.I., Sommerville J.,
Williams, R.G., & Webb, G.D. (2001). Task force 1: The changing profile of congenital heart
disease in adult life. Journal of American College of Cardiology, 37, 1170-1175.
Willams, J.M.G., Watt, F.N., Macleod, C.M., & Mathews, A. (1997). Attention to emotional stimuli.
In J.M.G., Willams, F.N., Watt, C.M., Macleod, and A., Mathews, (Eds.), Cognitive
psychology and emotional disorders (pp. 51-72). Chichester: John Wiley & Sons.
Zvolensky, M.J., Kotov, R., Antipova, A.V., & Schmidt, N.B. (2005). Diathesis stress model for
panic-related distress: a test in a Russian epidemiogical sample. Behaviour Research and
Therapy, 43, 521-532.
Preattentive processing of heart cues and the
perception of heart symptoms in congenital heart
disease.
Karsdorp, P.A., Kindt, M., Everaerd W., & Mulder B.J.M. (under revision).
78 Chapter 5
Abstract
The present study was aimed at clarifying whether preattentive processing of heart cues
results in biased perception of heart sensations in patients with congenital heart disease
(ConHD) who are also highly trait anxious. Twenty-six patients with ConHD and 22
healthy participants categorized heart-related (heart rate) or neutral sensations (constant
vibration) as either heart or neutral. Both sensations were evoked using a bass speaker
that was attached on the chest of the participant. Before each physical sensation, a
subliminal heart-related or neutral prime was presented. Biased perception of heartsensations would become evident by a delayed categorization of the heart-related
sensations. In line with the prediction, a combination of high trait anxiety and ConHD
resulted in slower responses after a heart-related sensation that was preceded by a
subliminal heart cue. Preattentive processing of harmless heart cues may easily elicit over
perception of heart symptoms in highly trait anxious patients with ConHD.
Preattentive processing 79
Introduction
Advances in surgical and medical care have improved the life expectancy of patients with
congenital heart disease (ConHD) enormously (Warnes et al., 2001). In order to improve
medical and psychological care, research has begun to study how ConHD affects patients’
quality of life (Kamphuis et al., 2002; Lane, Lip, & Millane, 2002; Moons, Van Deyk, De
Geest, Gewillig, & Budts, 2005). A current hypothesis designated the symptom-perception
hypothesis is that experience with chronic disease, like ConHD, results in acquired
perceptual biases for disease-related symptoms, such as selective attention (Pennebaker,
1982). These perceptual biases may increase the perception of symptoms and diminish
quality of life. However, recent studies show that this assertion seems to be unjustified.
That is, the sole presence of chronic disease seems not to be a sufficient condition to
increase symptom perception (e.g., Rietveld et al., 2002). Rather, psychological
vulnerabilities, such as trait anxiety, in combination with disease experiences are
supposed to influence quality of life (e.g., Aben et al., 2002; Kelly et al., 1998; Zvolensky,
Kotov, Antipova, & Schmidt, 2005). The present study is aimed to clarify whether trait
anxiety affects perceptual biases for heart-related symptoms in ConHD.
An integration of the symptom-perception (Pennebaker, 1982) and vulnerability
stress hypothesis (e.g., Zvolensky et al., 2005) explains how trait anxiety may influence the
development of perceptual biases in chronic disease. Chronic disease combined with trait
anxiety may increase the number of stressful experiences with symptoms. These
experiences may be stored in long-term memory as a network of associative relations
between symptoms and internal and external cues (i.e., physiological changes, a hospital
setting; Bower, 1981). Perception of these internal or external cues may needlessly activate
catastrophic expectations about patients’ physical health through spreading of activation.
In turn, patients may allocate their attention towards disease-related physical sensations
(Spence, Bentley, Philips, McGlone, & Jones, 2002) and may keep their attention focused
on these sensations for better identification and evaluation. As a result, patients may show
a difficulty shifting their attention away from the sensations, interrupting ongoing
behaviour (e.g., performance on a neutral cognitive task; e.g., Fox, Russo, Bowles, &
Dutton, 2001; Koster, Crombez, Verschure, & De Houwer, 2004). A difficulty shifting
attention may even increase the experience of physical symptoms. Accordingly, the
perception of disease-related cues may increase the perception of symptoms in highly trait
anxious patients with chronic disease. Irrelevant and harmless cues, such as thoughts
about disease or a hospital setting, may increase the perception of physical symptoms,
even in the absence of acute physical dysfunction (Rietveld, Kolk, & Prins, 1996; Rietveld,
Kolk, & Prins, 1997).
80 Chapter 5
Research on chronic disease has mainly focused on conscious processing of
disease-related cues (e.g., Rietveld, Kolk, & Prins, 1996; Rietveld, Kolk, & Prins, 1997).
However, it remains unclear to what extent preattentive processing of these cues (i.e.
processes which occur before conscious processing) may play a role in the perception of
symptoms. If disease-related cues are processed at a preattentive level, it may suggest that
overperception of symptoms is easily elicited in chronic disease, even without conscious
awareness of its precipitating internal or external cues. Emotion theories postulate that
the brain automatically and preattentively computes the affective valence of a stimulus,
i.e. whether a stimulus is threatening or not (LeDoux, 1994). Support for this theory has
been found in studies showing that highly anxious individuals display processing biases
towards threat, such as disease-related information, presented outside conscious
awareness (Mathews & MacLeod, 1994; Lundh, Wikström, Westelund, & Öst; Lim & Kim,
2005). It may be inferred from these observations that disease-related information is
processed at a preattentive level in highly anxious patients with chronic disease.
The present study was aimed at clarifying whether preattentive processing plays a
role in overperception of heart symptoms in ConHD. Based on the model presented above,
we hypothesized that highly anxious patients with ConHD process heart–related cues at a
preattentive level and in turn may show an increased difficulty shifting their attention
away from heart-related sensations. This hypothesis was tested with a priming paradigm
consisting of three phases: presentation of a prime, presentation of a target, and
categorization of the target. Priming involves a change in the response to a “target”
stimulus (for example a heart-related sensation) as a consequence of a prior presentation
of a related “prime” stimulus (a heart-related cue). Conscious elaboration of the prime
could be prevented through sandwich-masking techniques (Hermans, Spruyt, & De
Houwer, 2003) and a short presentation of the prime (10 ms). Sandwich masking
techniques entail that the prime is both preceded (forward masking) and followed by a
masking stimulus (backward masking). Preattentive processing of heart-related cues
(prime) and next a difficulty shifting attention away from heart-related sensations (target)
would become evident from delayed responses on the categorization of heart-related
sensations preceded by subliminally presented heart-related cues.
The primes in the present study consisted of a disease-related word (i.e. “heart”)
and a neutral word (i.e. “buzz”). The target stimuli consisted of two physical sensations: a
heart-related sensation (heart rate) and a neutral vibrating sensation (buzz). A bass
speaker that was attached on the chest of the participant generated a heart rate sound and
a vibrating sound that could be physically felt rather than heard. Note that these heartrelated sensations may be comparable to real heart sensations because heartbeat
perception is based on the mechanical vibrations in the thorax following each ejection of
Preattentive processing 81
blood volume during a heartbeat (Schandry, Bestler, & Montoya; Vaitl, 1996). Participants
were instructed to categorize the target sensation as heart or buzz. A healthy control group
was included to test the hypothesis that the combination of disease experience and trait
anxiety rather than trait anxiety alone resulted in a specific bias for heart-related
sensations. We predicted that highly trait anxious patients with ConHD would show larger
response latencies, when a heart rate sensation was preceded by a subliminally presented
heart cue than by a neutral cue.
Method
Participants
Consecutive adult patients with ConHD were selected from the outpatient clinics of
cardiology in the Academic Medical Centre in Amsterdam. Inclusion criteria were: age
between 18 and 60 years and no mental retardation. Thirty-seven percent of the contacted
patients participated in the experiment (14 women and 12 men, mean age = 28.19 years,
SD = 11.02, range 18 - 59 years). A cardiologist classified the heart defects into complex,
moderate, and simple ConHD, based on risk of mortality and morbidity and according to
the classification system that was presented at the 32nd Bethesda Conference of the
American College of Cardiology (Warnes et al., 2001). Ten patients had complex (e.g.,
transposition of the great arteries), 13 moderate (e.g., tetralogy of Fallot), and 3 had
simple ConHD (e.g., VSD). Twenty patients had undergone cardiac surgery or intervention
to repair or correct their cardiac defect, 9 patients used heart medication, and 3 had
experienced heart rhythm disturbances in the past. No differences were found between the
patients who participated and those who did not participate, according to age, gender, and
disease severity (p > .05). A comparison group was recruited using the inclusion criteria:
age between 18 and 60 years, no physical disease, no use of medication, and not a
psychology student. Twenty-two healthy adults (13 women and 9 men, mean age = 27.68
years, SD = 7.42, range 18 - 53 years) participated in the experiment. Age, gender, and
year income did not differ significantly between patients with ConHD and healthy
participants (p > .05). The local ethical committees of the Amsterdam Medical Centre and
the University of Amsterdam approved the study.
Design
We used a 2 ConHD (ConHD or healthy) x 2 Trait Anxiety (high or low) x 2 Prime (heartrelated or neutral) x 2 Target (heart-related or neutral sensation) factorial design, with
ConHD and trait anxiety as between subject variables and prime and target as withinsubject variables.
82 Chapter 5
Materials
Setting and apparatus
The experiment was conducted in a dimly lit room. Participants were seated at a table
facing a 17-inch computer screen with a viewing distance of 50 cm for presentation of the
primes. For the presentation of the targets, a speaker with a diameter of 20 cm (Monacor
BR-25) was attached on the left middle of the participants’ chest (the position of the
heart). This speaker generated a powerful bass sound, which could only be physically felt
rather than heard. For the registration of the responses, two button boxes were used to
measure decision times. One was labeled with the word heart, the other with the word
buzz. The position (left or right) of these buttons was randomized across participants.
Stimulus presentation and response registration was controlled by the Vsrrp98 software
package (Versatile Stimulus Response Registration Program, 1998) running on a
Windows2000 PC. This computer was connected to an amplifier (Monacor BR-25) and
the two button boxes.
Stimuli
The stimuli consisted of both a heart-related and a neutral prime and heart-related and
neutral target. The neutral stimuli were included to rule out the possibility that the
semantic relation rather than the affective relation explained response differences for
heart-related prime-target combinations. The primes, presented on the computer screen,
consisted of a disease word heart (in Dutch ‘hart’) or a neutral word buzz (in Dutch
‘zoem’). The target sensations consisted of two sounds: a heart rate sound and a neutral
sound (buzz). Both sounds were created by digitally recorded drum sounds. The heart rate
sound was created by transforming the drum sounds such that it resembled a heart rate of
130 beats / minute. We used this heart rate because a fast heart rate would assumingly
provoke more anxiety than a slow heart rate. For the neutral sound (buzz), a drum sound
was transformed into a constant vibrating sound. To prevent recognition of the prime, a
mask was presented before and after presentation of the prime. The masks consisted of a
string of 4 random letters.
Trait anxiety
To measure trait anxiety, we used a Dutch translation of the 20-item Spielberger trait
anxiety inventory (STAI; Van der Ploeg, Defares, & Spielberger, 1979; Spielberger,
Gorsuch, & Lusheve, 1970). Response categories vary from 1 “not at all” to 4 “very much
so.” Total trait scores range from 20 to 80. Psychometric (reliability and validity)
performance of the Dutch STAI is satisfactory (Van der Ploeg et al., 1979). The sample was
split into a low trait anxiety group (n ConHD = 13, M ConHD = 27.38, SD ConHD = 4.01; n healthy =
Preattentive processing 83
11, M healthy = 27.72, SD healthy = 3.66) and a high trait anxiety group (n ConHD = 13, M ConHD =
41.31, SD ConHD = 7.27; n healthy = 9, M healthy = 39.99, SD healthy = 4.56) based on median split
of the STAI-trait (Me = 32).
Procedure
After informed consent, it was explained that the aim of the experiment was to study the
causes of physical complaints. Next, participants completed the STAI-trait version and
some biographical questions. Participants were told that the speaker would generate
amplified feedback of their heart rate or a constant vibration. Next, the speaker was
attached on the participants’ chest. To distinguish the heart rate feedback and the constant
vibration accurately, participants were exposed five times to the heart rate and neutral
sounds for three seconds. Next, participants were told that a word would be presented on
the computer screen that they would probably not see. Participants were requested to
ignore this word and to categorize as quickly as possible the sensation felt on their chest by
pushing either a heart or a buzz button. To prevent that participants would ignore the
computer screen completely, we instructed participants to attend to the computer screen
to answer questions later on.
The experimental task consisted of 40 trials in which four prime-target
combinations were randomly presented for 10 times: heart-heart, heart-buzz, buzz-heart,
and buzz-buzz. The experimental trials proceeded as follows: first, a fixation dot appeared
for 1000 ms, followed by a mask for 500 ms, followed by the presentation of the prime for
10 ms. Immediately after the prime, both a (second) mask and a target sensation appeared
simultaneously for maximally 3000 ms. The target was terminated as soon as the
participant pressed one of the two buttons. The mask remained on the screen until the
3000 ms had elapsed. After that, the next trial started. The experimental task started with
eight practice trials.
To check whether participants were unable to consciously perceive the prime, a
forced-choice awareness task was presented after the experimental task. This task was
similar to the experimental task except that no target was displayed. In the forced-choice
awareness task, the experimenter explained that the word heart or buzz would be
presented for such a short time that conscious perception would probably be hampered.
Participants were instructed to guess whether they had seen the word heart or buzz by
pressing the heart or buzz button. The task consisted of 40 trials of 20 randomly presented
heart and buzz primes. The awareness task started with eight practice trials. Finally, they
were paid and ascertained that the heart rate feedback did not represent their own heart
rate.
84 Chapter 5
Data analysis
Mean latencies for the four prime target combinations (heart - heart; heart - buzz; buzz heart; buzz - buzz) were calculated for every participant and submitted to repeatedmeasures ANOVA with trait anxiety and disease as between subjects-factors. In addition,
we calculated a priming index, which was the dependent variable in a linear regression
analysis with the predicted interaction between trait anxiety scores and ConHD as the
independent variable. This linear regression analysis was conducted to rule out the
possibility that the median split had resulted in an arbitrary classification of participants
as low or high trait anxious. The priming index was calculated by subtracting incongruent
trials from congruent trials. This resulted in the following priming index (RT heart, heart - RT
heart, buzz)
– (RT
buzz, heart
- RT buzz, buzz). High scores on the priming index indicate increased
response latencies to heart sensations proceeded by a heart prime. Small, medium and
large effect sizes for ANOVA’s were η² = 0.01, 0.06, and 0.14, respectively, and for linear
regression analysis r = .10, .30, and .50, respectively (Cohen, 1988). The alpha level was
set at the .05 level for all statistical tests. SPSS for Windows version 11 (SPSS Inc, Chicago,
Illinois, USA) was used to perform statistical calculations.
Results
Data reduction
One healthy participant was excluded from the analyses because her response latencies
were extremely large (M = 2488 ms, SD = 805 ms) compared to a mean response latency
of 991 ms (SD = 301 ms) for the other participants. In addition, one healthy participant
was excluded because his priming index (M = -519 ms) deviated more than 3 SDs from the
mean (M = 11 ms, SD = 147 ms).
Reaction times on trials for which participants gave no or an incorrect response
were excluded (4.25 % of all data points). Note that overall the number of error rates were
too low to consider in the remainder of the analyses. Reaction times greater than 1500 ms
or smaller than 250 ms were excluded (Hermans et al., 2003). This resulted in a mean
outlier rate of 11.06%.
Response latencies
Means and standard deviations of response latencies are presented in Table 1. A repeated
measure ANOVA showed no significant main effects of prime, target, ConHD, and trait
anxiety, all Fs (1, 42) < .27. In addition, no significant two-way interactions emerged, all
Fs (1, 42) < 2.62. Only a trend emerged for the two-way interaction between Prime x Trait
Anxiety, F (1, 42) = 3.12, p = .09, η2 = .07. A significant three-way interaction was found
Preattentive processing 85
between Prime x Target x ConHD, F (1, 42) = 4.52, p = .04, η2 = .10. However, follow-up
test for the patients with ConHD and healthy controls separately, did not show a
significant interaction between Prime x Target within each group, all Fs < 2.94. No other
significant three-way interactions emerged, all Fs (1, 42) < .99.
In line with the prediction, that highly anxious patients with ConHD would show
larger response latencies to heart sensations preceded by a heart cue, the analysis showed
a significant four-way interaction between Prime x Target x Trait Anxiety x ConHD, F (1,
42) = 4.62, p = .04, η2 = .10. In order to explore this 4-way interaction, post-hoc analyses
were performed for patients with ConHD and healthy controls separately. For the healthy
participants, no significant interaction was found between Prime x Target x Trait Anxiety,
F (1, 18) = 0.36, p > .05, η2 = .05. However, as predicted, follow-up tests for patients with
ConHD showed a significant interaction between Prime x Target x Trait Anxiety, F (1, 24)
= 4.67, p = .04, η2 = .16. Separate analysis for the low anxious patients with ConHD
showed no significant interaction between prime by target, F (1, 12) = 0.76, p > .05, η2 <
.01. However in line with the predictions, the highly anxious patients with ConHD showed
a significant interaction of prime by target, F (1, 12) = 7.68, p = .02, η2 = .39, indicating
that highly trait anxious patients with ConHD exhibited larger response latencies when a
heart rate sensation was preceded by a heart cue (M = 969, SD = 216) than by a neutral
cue (M = 896 ms, SD = 183), t (12) = 2.64, p =. 02. This finding supports the hypothesis
that highly anxious patients with ConHD process heart related information at a
preattentive level resulting in an increased difficulty shifting attention away from heart
sensations.
Table 1. Means and standard deviations of response latencies in ms of patients with ConHD and
healthy controls
Congenital heart disease
Control
LT-anxiety a
HT-anxiety a
LT-anxiety a
HT -anxiety a
(n = 13)
(n = 13)
(n = 11)
(n = 9)
Prime
Target
M
SD
M
SD
M
SD
M
SD
Heart
Heart
821
236
969
216
917
203
785
195
Buzz
Heart
860
204
896
183
932
214
813
230
Heart
Buzz
822
237
921
189
879
237
838
168
Buzz
Buzz
848
239
956
205
883
201
799
159
Note. a Based on the median split of the STAI-T (Me = 32) the sample was split in a low (LT) and high trait (HT) anxious
group.
86 Chapter 5
A linear regression analysis with the priming index as dependent variable and the
interaction between trait anxiety (continuous variable) and ConHD as independent
variables confirmed the results obtained with the repeated-measure ANOVA (Figure 1).
The interaction of trait anxiety by ConHD explained a significant amount of variance of
the priming index, β = .30, t (45) = 2.05, p < .05.
Figure 1. Regression slopes depicting the relationship between trait anxiety and the priming
index for patients with ConHD and controls. An increased priming index indicates a relative delayed response to
the heart sensations preceded by a heart cue.
Awareness check
We determined the accuracy of the heart or buzz decisions obtained during the recognition
task by calculating hit rates. Neither the hit rates for heart (M = 47 %, SD = 15) nor the hit
rates for buzz (M = 50 %, SD = 15) differed significantly from chance (50%), t (45) = -1.30,
p =. 20 and t (45) = 0.14, p =. 89, respectively. This suggests that the participants were
unaware of the true nature of the presented primes.
Severity of heart disease
Spearman rank correlations showed no significant relation between severity of heart
disease (controls excluded) and the priming index, r (26) = -.15, p = .47. Finally, patients
who used medication or who had undergone cardiac interventions or surgery did not show
different response latencies (all ps > .05).
Preattentive processing 87
Trait anxiety
A one-way ANOVA showed that patients with ConHD did not significantly differ from
healthy controls on trait anxiety, F (1, 44) = 0.19, p = .66, η2 < .01. Spearman rank
correlations showed no relation between severity of heart disease and trait anxiety, r (26)
= -.29, p = .15.
Discussion
The present results are in line with the hypothesis that patients with ConHD who are also
high trait anxious process heart-related cues (prime) preattentively and in turn show a
difficulty shifting attention away from heart-related sensations. This was evidenced by
delayed responses on the categorization of heart-related sensations preceded by
subliminally presented heart-related cues. The finding that disease severity was unrelated
to trait anxiety indicates that the relation between ConHD and perceptual biases for heart
symptoms is moderated rather than mediated by trait anxiety. Moreover, the fact that
disease severity was unrelated to perceptual biases for heart-related sensations
strengthens our assumption that not the sole presence of ConHD but ConHD in
combination with high trait anxiety results in perceptual biases.
The present study is in accordance with studies showing that trait anxiety is a
vulnerability factor for biased perception of physical symptoms (Zvolensky et al., 2005;
Watson & Pennebaker, 1989). Moreover, the present study may indicate that the observed
perceptual bias is the result of a difficulty shifting attention away from heart-related
stimuli. This would be in line with studies showing that highly anxious individuals have
difficulty disengaging from fearful stimuli (Fox et al., 2001; Koster et al., 2004). It is
noteworthy that response latencies after heart rate sensation were only delayed after
presentation of a heart cue as compared to a neutral cue. The sole presentation of
subliminal heart cues or heart rate sensations did not result in a general delay of responses
in highly anxious patients with ConHD. Similar results were observed among highly
anxious individuals, whose responses to a threatening picture (target) were only delayed
after short presentation of another threatening picture (prime) (Berner & Maier, 2004;
Maier, Berner, & Pekrun, 2003). These findings are in accordance with theories stating
that perceptual biases are most reliably shown in the presence of bias-related cues that
activate the fear network (Bower, 1981; Beck, Rush, Shaw, & Emery, 1997). In this case,
bias-related cues may be for example a hospital setting, reading books about heart disease,
or physical sensations.
The finding that subliminal heart cues influenced processing of heart-related
sensations in highly trait anxious patients with ConHD suggests that the affective meaning
88 Chapter 5
of the cues must have been processed preattentively in these patients. This is in line with
studies showing that individuals who are preoccupied with physical symptoms show
preattentive processing of physical information (Lundh et al., 1999; Lim & Kim, 2005).
Note, however, that the priming task consisted of three phases: presentation of the prime,
the target, and the categorization of the target. Therefore, it remains unknown in what
phase of the present task the dysfunctional processing occurs. That is, either processing of
the subliminal heart-related prime, disengagement from the heart sensation, or both
processes are disturbed in the highly trait anxious patients with ConHD. Future research
may unravel which phase of processing is affected by disease-relevant information.
The present study circumvented some methodological weaknesses that were
present in other studies on processing biases for disease-related information (Rietveld,
Karsdorp, & Mulder, 2004; Lim & Kim, 2005). First, we presented the heart-related and
neutral sensation in exactly the same sensory modality and spatial location on the
participant’s chest. In this way we excluded the possibility that highly anxious patients
with ConHD showed difficulty shifting their attention from a specific sensory modality or
spatial location rather than from specifically heart-related sensations (Fox et al., 2001).
Moreover, we required participants to make the same categorization response to the
heart-related and neutral target sensations. Therefore, we excluded the possibility that a
difficulty switching from performing one task to another task could explain the results
(Fox et al., 2001). Additionally, we increased the external validity of the experiment by
eliciting real heart-related physical sensations rather than using disease-related words or
sounds that are mostly used in studies on processing biases (e.g., Rietveld et al., 2004;
Lim & Kim, 2005).
Some methodological issues of the present study may need clarification. Due to
technical limitations, the time interval between participants’ response and the next trial
was relatively long. That is, the next trial started after presentation of the backward mask
for 3000 ms, irrespective of response latencies. It has been shown that very short intervals
between a response and the next trial increase time pressure and magnify processing
biases (Sharma & McKenna, 2001). Therefore, the absence of time pressure in the present
study may have underestimated the observed processing biases among highly anxious
patients with ConHD. Moreover, the absence of time pressure may have resulted in
relatively slow overall response latencies. These slow response latencies in combination
with the elimination of outliers based on an absolute cut-off score of 1500 ms, may have
resulted in a relatively large omission of response latencies. Although this was within the
reasonable range of 10 –15% (Ratcliff, 1993), it could be argued that a cut-off score based
on individual subject standard deviations would have been more appropriate. An absolute
cut-off score was used in the present study to increase comparability with other priming
Preattentive processing 89
studies on trait anxiety that also used an absolute cut-off score (Hermans et al., 2003;
Berner & Maier, 2004; Maier et al., 2003). Moreover, studies using eye movement
monitoring have shown that hypervigilance in highly anxious individuals is followed by
avoidance strategies at 1500 to 2000 ms after the onset of a threat cue (Calvo, & Avero,
2005; Hermans, Vansteenwegen, & Eelen, 1999; Rohner, 2004). Since avoidance
strategies were not the processes under study, we used a cut-off score that eliminated
responses latencies that presumably were affected by avoidance strategies.
Some caution is warranted to the generalizability of the findings as the response
rate and sample sizes were relatively low. Nevertheless, the present findings suggest that
unconscious perception of internal and external cues may easily elicit attention to heartrelated sensations in highly anxious patients with ConHD. In case of acute heart
dysfunction, preattentive processing of heart-related sensations may be an adaptive
response strategy as it may increase survival chances in ConHD (Williams, Watt,
MacLeod, & Matews, 1997). For example, signals of acute heart dysfunction initially
inaccessible for conscious elaboration, may still elicit attention to heart sensations,
facilitating conscious perception of heart dysfunction and increasing the likelihood that
patients will take appropriate action. However, in the absence of acute heart dysfunction,
preattentive processing may be maladaptive as it may elicit overperception of heart
symptoms and reduce quality of life. For example, when patients unconsciously perceive a
hospital setting or harmless changes in heart rate, they may direct their attention to their
heart. This may intensify experienced physical sensations and eventually may result in
unnecessary avoidance of social and physical activities. Since there is some evidence that
preattentive processing biases are susceptible to psychological treatment (Mogg, Bradley,
Millar, & White, 1995), patients with ConHD who suffer from symptoms that cannot
directly be explained by the medical disease may profit from cognitive behaviour therapy.
In future research, it could be tested whether subliminal heart cues affect the experienced
intensity and interpretation of heart-related sensations in highly anxious patients with
ConHD.
References
Aben, I., Denollet, J., Lousberg, R., Verhey, F., Wojciechowski, F., & Honig, A. (2002). Personality
and vulnerability to depression in stroke patients: A 1-Year Prospective follow-up study.
Stroke, 33, 2391-2395.
Beck, A.T., Rush, A.J., Shaw, B.F., & Emery, G. (1997). Cognitive Therapy of Depression. New
York: Guilfors Press.
90 Chapter 5
Berner, M.P., & Maier, M.A. (2004). The direction of affective priming as a function of trait anxiety
when naming target words with regular and irregular pronunciation. Experimental
Psychology, 51, 180-190.
Bower, G. H. (1981). Mood and memory. American Psychologist, 36, 128-148. Calvo, M.G., &
Avero, P. (2005). Time course of attentional bias to emotional scenes in anxiety: gaze
direction and duration. Cognition and Emotion, 19, 433-451.
Cohen, J.B. (1998). Statistical power analysis for the behavioural sciences. Hillsdale: Lawrence
Erlbaum.
Fox, E., Russo, R., Bowles, R., & Dutton, K. (2001). Do threatening stimuli draw or hold visual
attention in subclinical anxiety? Journal of Experimental Psychology, 130, 681-700.
Hermans, D., Spruyt, A., De Houwer, J., & Eelen, P. (2003). Affective priming with subliminally
presented pictures. Canadian Journal of Experimental Psychology, 57, 97-114.
Hermans, D., Vansteenwegen, D., & Eelen, P. (1999). Eye movement registration as a continuous
index of attention deployment: data from a group of spider anxious students. Cognition
and Emotion, 13, 419-434.
Kamphuis, M., Ottenkamp, J., Vliegen, H.W., Vogels, T., Zwinderman, K.H., Kamphuis, R.P., &
Verloove-Vanhorick, S.P. (2002). Health related quality of life and health status in adult
survivors with previously operated complex congenital heart disease. Heart, 87, 356-362.
Kelly, B., Raphael, B., Judd, F., Kernutt, G., Burnett, P., & Burrows, G. (1998). Posttraumatic stress
disorder in response to HIV infection. General Hospital Psychiatry, 20, 345-352.
Koster, E.H.W., Crombez, G., Verschure, B., & De Houwer, J. (2004). Selective attention to threat
in the dot probe paradigm: differentiating vigilance and difficulty to disengage. Behaviour
Research and Therapy, 42, 1183-1192.
Lane, D.A., Lip, G.Y., & Millane, T.A. (2002). Quality of life in adults with congenital heart disease.
Heart, 87, 356-362.
LeDoux, J.E. (2000). Emotion circuits in the brain. Annual Review of Neuroscience, 23, 155-184.
Lim, S., & Kim, J. (2005). Cognitive processing of emotional information in depression, panic, and
somatoform disorder. Journal of Abnormal Psychology, 114, 50-61.
Lundh, L.G., Wikström, J., Westerlund, J., & Öst, L.G. (1999). Preattentive bias for emotional
information in panic disorder with agoraphobia. Journal of Abnormal Psychology, 108,
222-232.
Maier, M.A., Berner, M.P., & Pekrun, R. (2003). Directionality of affective priming: effects of trait
anxiety and activation level. Experimental Psychology, 50, 116-123.
Mathews, A., & MacLeod, C. (1994). Cognitive approaches to emotion and emotional disorders.
Annual Review of Psychology, 45, 25-50.
Mogg, K., Bradley, B.P., Millar, N., & White, J. (1995). A follow-up study of cognitive bias in
generalized anxiety disorder. Behaviour Research and Therapy, 33, 927-935.
Moons, P., Van Deyk, K., De Geest, S., Gewillig, M., & Budts, W. (2005). Is the severity of
congenital heart disease associated with the quality of life and perceived health in adult
patients? Heart, 91, 1193-1198.
Pennebaker, J.W. (1982). The psychology of physical symptoms. New York: Springer-Verlag
Preattentive processing 91
Ratcliff, R. (1993). Methods for dealing with reaction time outliers. Psychological Bulletin, 114, 510532.
Rietveld, S., Karsdorp, P.A., & Mulder, B.J. (2004). Heartbeat sensitivity in adults with congenital
heart disease. International Journal of Behavioral Medicine, 11, 203-211.
Rietveld, S., Kolk, M., & Prins, P.J. (1996). The influence of lung function information on selfreports of dyspnea by children with asthma. Journal of Pediatric Psychology, 21, 367-377.
Rietveld, S., Kolk, A.M., & Prins, P.J.M. (1997). The influence of respiratory sounds on
breathlessness in children with asthma: a symptom-perception approach. Health
Psychology, 16, 547-553.
Rietveld, S., Mulder, B.J., Van Beest, I., Lubbers, W., Prins, P.J., Vioen, S., Bennebroek-Evererz, F.,
Vos, A., Casteelen, G., & Karsdorp, P. (2002). Negative thoughts in adults with congenital
heart disease. International Journal of Cardiology, 86, 19-26.
Rohner, J.C. (2004). Memory-based attentional biases: anxiety is linked to threat avoidance.
Cognition and Emotion, 18, 1027-1054.
Schandry, R., & Bestler, M., Montoya, P. (1993). On the relation between cardiodynamics and
heartbeat perception. Psychophysiology, 30, 467-474.
Sharma, D., & McKenna, F.P. (2001). The role of time pressure on the emotional Stroop task.
British Journal of Psychology, 92, 471-481.
Spence, C., Bentley, D.E., Phillips, N., McGlone, F.P., & Jones, A.K.P. (2002). Selective attention to
pain: a psychophysiological investigation. Experimental Brain Research, 145, 395-402.
Spielberger, C.D., Gorsuch, R., & Lusheve, R. (1970). STAI Manual for the Sate-Trait Anxiety
Inventory. Palo Alto, CA: Consulting Psychologists Press.
Vaitl, D. (1996). Interoception. Biological Psychology, 42, 1-27.
Van der Ploeg, H.M., Defares, H.B., & Spielberger, C.B. (1979). Handleiding bij de
zelfbeoordelingsvragenlijst. Een nederlandse bewerking van de Spielberger State-Trait
Anxiety Inventory. [Validity of the Zelf-Beoordelings-Vragenlijst. A Dutch version of the
Spielberger State-Trait Anxiety Inventory]. Lisse: Zwets and Zeitlinger.
Warnes, C.A., Liberthson, R., Danielson, G.K., Dore, A., Harris, I., Hoffman, J.I., Sommerville J,
Williams RG, & Webb GD. (2001). Task force 1: the changing profile of congenital heart
disease in adult life. Journal of American College of Cardiology, 37, 1170-1175.
Watson, D., & Pennebaker, J.W. (1989). Health complaints, stress and distress: exploring the
central role of negative affectivity. Psychological Review, 96, 234-254.
Willams, J.M.G., Watt, F.N., Macleod, C.M., & Mathews, A. (1997). Attention to emotional stimuli.
In J.M.G., Willams, F.N., Watt, C.M., Macleod, & A., Mathews (Eds.), Cognitive psychology
and emotional disorders (pp. 51-72). Chichester: John Wiley & Sons.
Zvolensky, M.J., Kotov, R., Antipova, A.V., & Schmidt, N.B. (2005). Diathesis stress model for
panic-related distress: a test in a Russian epidemiological sample. Behaviour Research and
Therapy, 43, 521-532.
Interpretation bias for heart sensations in
congenital heart disease and its relation to quality
of life
Karsdorp, P.A., Kindt M., Rietveld S., Everaerd W., & Mulder, B.J.M. (under revision).
94 Chapter 6
Abstract
We hypothesized that the relation between trait anxiety and the physical aspects of quality
of life in patients with congenital heart disease (ConHD) is mediated by a negative
interpretation bias for heart-related sensations. Sixty-six patients with ConHD and 50
healthy participants read a vignette about a person experiencing ambiguous heart-related
sensations. Interpretation bias to these sensations was assessed with the Implicit Models
of Illness Questionnaire. In addition, participants completed Spielberger trait and state
anxiety questionnaires and the physical subscales of the TNO-AZL Adult Quality of Life
Questionnaire. Path-analysis showed that a negative interpretation bias mediated the
relation between trait anxiety and daily activities specifically in patients with ConHD. In
contrast, trait anxiety and interpretation bias were less influential with respect to gross
motor functioning. These results suggest that a combination of ConHD and high trait
anxiety diminishes daily functioning due to a negative interpretation bias for heart-related
sensations.
Interpretation bias 95
Introduction
Patients with congenital heart disease (ConHD) report a reduced health-related quality of
life specifically with respect to physical functioning (e.g., Fekkes et al., 2001; Kamphuis et
al., 2002). Several theories have been proposed to explain how ConHD affects quality of
life. A classic hypothesis, denoted the somatic hypothesis, is that the heart disease directly
results in a diminished quality of life (Hager & Hess, 2005). For example, reduced
oxygenation of the blood may cause a reduced exercise tolerance (Hager & Hess, 2005;
Rose et al., 2005). Although it is proposed that the severity of ConHD reduces the physical
activity level, the observed relation is weak (Kamphuis et al., 2002). Therefore, it may be
suggested that the presence of ConHD is not a sufficient condition to affect quality of life.
Other factors such as psychological vulnerabilities may also be required to explain the
relation between heart disease and quality of life (de Beurs et al., 2005; Zvolensky, Kotov,
Antipova, & Schmidt, 2005). It may be suggested that ConHD in combination with
psychological vulnerabilities such as negative affectivity or its related construct trait
anxiety (Watson & Pennebaker, 1989) may result in a reduced quality of life. In line with
this conjecture is the frequently observed relation between trait anxiety and quality of life
in patients with chronic disease (Rietveld et al., 2002; Paschalides et al., 2004; Page et al.,
2004).
Several hypotheses have been proposed that may explain how trait anxiety affects
quality of life in chronic disease. Current explanations are designated as the symptom
perception hypothesis (Watson & Pennebaker, 1989) and the vulnerability stress
hypothesis (e.g., De Beurs et al., 2005; Zvolensky et al., 2005). According to these
hypotheses, high trait anxiety (a long-lasting vulnerability factor) in combination with
chronic disease (a stressor; Roesch & Weiner, 2001) may facilitate the development of
negative cognitive schemes representing associations between sensations and disease
(Page et al., 2004; Paschalides et al., 2004). These are called illness schemes and are
supposed to result in information processing biases that, for instance, are characterized by
a negative interpretation of ambiguous illness-related sensations (Pennebaker, 1982).
Here, a negative interpretation is associated with the tendency to view ambiguous
sensations as relatively serious, uncontrollable, unchangeable, and requiring less personal
responsibility (Roesch & Weiner, 2001). It has been shown that these negative
interpretations in turn are related to a reduced quality of life (Roesch & Weiner, 2001;
Page et al., 2004; Paschalides et al., 2004). This may imply that a negative interpretation
bias for disease-related sensations mediates the frequently observed relation between trait
anxiety and quality of life specifically in chronic disease. The aim of the present study is to
test this hypothesis in ConHD.
96 Chapter 6
Emotional-congruency theories emphasize that illness schemes only elicit
processing biases when activated by schema-related moods or events (Bower, 1981).
Indeed, the relation between trait anxiety and processing biases are most reliably shown in
participants that displayed elevated levels of both trait and state anxiety (Mathews &
MacLeod, 1994; Rusting, 1998). It follows that highly trait anxious patients with ConHD,
who also display elevated levels of state anxiety are expected to show the most pronounced
negative interpretation biases for heart-related sensations.
In the present study, the following hypotheses were tested: 1) the relation between
trait anxiety and quality of life is mediated by a negative interpretation bias for heartrelated sensations specifically in ConHD; 2) the relation between trait anxiety and
interpretation bias is mediated by state anxiety. In order to assess negative interpretation
bias, we used a method developed by Schwarzman and McDermid (1993). Participants
read a written vignette about a person experiencing ambiguous heart-related sensations.
Interpretation bias to these sensations was assessed with the Implicit Models of Illness
Questionnaire (IMIQ; Turk, Rudy, & Salovey, 1986). The physical aspects of quality of life
were assessed with two subscales of the Netherlands Organisation for Applied Scientific
Research Academic Medical Centre (TNO-AZL) Adult Quality of Life Questionnaire
(TAAQOL; Bruil, Fekkes, Vogels, & Verrips, 2004). Disease severity was assessed to rule
out the possibility that the sole presence of ConHD affected trait-state anxiety,
interpretation bias, and quality of life, as stated by the somatic hypothesis. Note that we
measured only the physical aspects of quality of life, because these aspects are most
affected in patients with ConHD, and because subscales assessing negative affect, such as
depressive moods and vitality, may correlate with trait anxiety. A healthy control group
was included to assess whether trait-state anxiety in combination with ConHD resulted in
a negative interpretation bias for heart-related sensations rather than trait anxiety alone.
Method
Participants
Consecutive adult patients with ConHD were selected from the archives of the department
of cardiology of the Academic Medical Centre, in Amsterdam. Hundred-fifteen patients
were sent a booklet with the questionnaires. Two patients died during the study. Sixty-six
patients returned the booklet (36 women, mean age = 33.00 years, SD = 8.83, range 18 56 years). The response rate, corrected for deceased patients was 58.4 %. A cardiologist
rated the severity of heart disease to determine whether disease severity was related to
state, trait anxiety, interpretation bias, and quality of life. The classification of disease
severity was based on risk of morbidity and mortality according to the classification
Interpretation bias 97
system that was presented at the 32nd Bethesda Conference of the American College of
Cardiology (Warnes et al., 2001). Sixteen patients had complex ConHD (e.g., transposition
of the great arteries, single ventricle), 38 had moderate ConHD (e.g., ASDII, coarctation
aortae), and 12 had simple ConHD (e.g., isolated VSD, isolated mitral valve disease). No
differences were found between the patients with ConHD, who participated and those who
did not participate, with respect to age, gender, and disease severity (p >.05). To form a
control group we recruited healthy adults that matched in terms of age and education
level. Fifty healthy participants (response rate = 62.2%) returned the booklet (27 women,
mean age = 29.32 years, SD = 8.96, range 19 - 53 years). No differences were found
between the patients with ConHD and healthy controls according to age, gender, and
education level (all tests p > .05). The local ethical committee of the Amsterdam Medical
Centre and the University of Amsterdam approved the study.
Materials
Stimulus material
To measure interpretation bias with respect to heart-related sensations a vignette was
composed consisting of six sentences about a woman, who experienced five heart-related
sensations: irregular heartbeat, chest pain, shortness of breath, tingling in arms and legs,
and dizziness. No information was given in the vignette concerning the cause of the
sensations. Therefore, the sensations were ambiguous in the sense that they could be a
manifestation of heart disease, another disorder, emotional stress, or physical exertion.
Interpretation bias
Interpretation bias was measured with the IMIQ (Turk, Rudy, & Salovey, 1986), which was
translated to Dutch for the present study. Note that the Illness Perception QuestionnaireRevised (IPQ-R; Moss-Morris et al., 2002), which is presently more current, was not yet
available at the time our study was designed. The IMIQ comprised 24-items, which
formed four subscales: seriousness (9 items, range 9-81), personal responsibility (8 items,
range 8-2), controllability (5 items, range 5-45), and changeability (2 items, range 2-18).
The seriousness scale referred to views about whether the disease is contagious, difficult to
cure, and long lasting, and requires medical attention. The personal responsibility scale
referred to beliefs about how responsible the individual is for the cause and cure of the
disease. The controllability scale referred to whether anyone or anything can influence the
disease course. The changeability scale referred to whether the symptoms are invariant
over time. Ratings were made on a 9-point scale, ranging from 1 “strongly agree” to 9
“strongly disagree.” A high score on each subscale represented a stronger negative bias. In
the present study, the internal reliability (Cronbach’s α) for the subscales seriousness,
98 Chapter 6
personal responsibility, controllability, and changeability was .98, .97, .91, and .73,
respectively.
State and trait anxiety
We used a Dutch translation of the 40-item Spielberger state-trait anxiety inventory
(STAI; Spielberger, Gorsuch, & Lusthene, 1970; Van der Ploeg, 1980). Response categories
vary from 1 “not at all” to 4 “very much so.” Total trait and state scores range from 20-80.
Psychometrically, i.e., with respect to reliability and validity, the STAI is satisfactory (Van
der Ploeg, 1980). In the present study, the internal reliability (Cronbach’s α) of both state
and trait anxiety were .94.
Health-related quality of life
To measure the physical aspects of health-related quality of life we used two subscales of
the TNO-AZL Adult Quality of Life Questionnaire (TAAQOL) (Bruil, Fekkes, Vogels, &
Verrips, 2004): gross motor functioning (4 items), and daily activities (4 items). The
subscales measure problems or limitation concerning gross motor functioning, and
independent daily functioning, respectively. The subscales are highly correlated with the
physical subscales of the Short-Form Health Survey (SF-36; McHorney, Ware, & Raszek,
1993). These subscales are: physical functioning and role limitations due to physical
health, respectively (Bruil et al., 2004). The frequency of occurrence of a health status
problem, as expressed in each item, was assessed. If such a problem was reported, the
emotional reaction to this problem was determined. The reference period for a give
problem is formulated as “the last month.” Examples of a gross motor and daily activity
question are “did you have difficulty with walking up the stairs in the last month’ and ‘did
you have difficulty with work, study, or other day-to day activities.’ The response
categories were ‘no’, ‘a little’, ‘some’, or ‘a lot.’ When the response was ‘a little’, ‘some’ or ‘a
lot’, the question was followed by the statement ‘how much did that bother you’, with
response categories ‘not at all’, ‘a little’, ‘quite a lot’, or ‘very much’. Scores of each subscale
are normalized to a scale ranging from 0 to 100, with higher scores representing better
quality of life. Psychometric performance (i.e., reliability and validity) of the TAAQOL is
satisfactory (Bruil et al., 2004). In the present study, the internal reliability (Cronbach’s α)
for gross motor functioning and daily activities was .78 and .85, respectively.
Procedure
Given informed consent, and following the completion of the STAI and TAAQOL-scales,
each participant read the vignette and completed the IMIQ.
Interpretation bias 99
Statistics
A path analysis was used to investigate the hypothesized model. Path analysis is a method
for representing linear (arguably, “causal”) relations in multivariate data (McDonald &
Ho, 2002). LISREL 8.5 (Jöreskog & Sörbom, 2001) was applied to estimate model
parameters and to compute fit statistics. Path coefficients were considered significant if
their associated t-values exceeded 1.65 in absolute value. To assess the overall goodness of
fit of a given model, we considered of the following fit indices (Bollen & Long, 1993;
Bentler, 1990): chi-square, non-normed fit index (NNFI), comparative fit index (CFI), and
the root mean square error of approximation (RMSEA). The chi-square is a measure of
overall fit of the model to the data. Relative to the degrees of freedom of the model, small
chi-square values (p > .05) indicate good fit. A NNFI of about > 0.92 and a CFI > .90 is
viewed as indicative of a well-fitting model. Finally, the RMSEA is a measure of
discrepancy per degree of freedom. An RMSEA of 0.05 or less is indicative of a good
approximation (Browne & Cudeck, 2002).
First we tested the fit of the hypothesized model in ConHD and the healthy control
group (Figure 1). In the hypothesized model trait anxiety indirectly influenced gross motor
functioning and daily activities via state anxiety and interpretation bias (seriousness,
personal responsibility, controllability, and changeability). In addition, in the
hypothesized model, trait anxiety influenced interpretation bias indirectly via state
anxiety. The model also included a direct causal connection between state anxiety and
quality of life, because it is deemed unlikely that interpretation bias mediated the relation
between trait-state anxiety and quality of life completely. Moreover, highly trait anxious
individuals who are also highly state anxious are more likely to evaluate their quality of life
negatively and to remember negative aspects of their quality of life (e.g., Bower 1981). We
allowed for a co-variation between the four subscales assessing interpretation bias and
between the two subscales assessing gross motor functioning and daily activities.
To test whether the path coefficients from state anxiety to interpretation bias were
stronger among patients with ConHD than among healthy controls, we performed a multigroup analysis. First, the models were tested with the parameters not constrained to be
equal across models. This unconstrained multiple group model served as the baseline
against which to judge a model, in which the parameters from state anxiety to
interpretation bias were forced to be equal. We used a chi-square difference test between
the non- restrictive and restrictive model to test whether the parameters differed between
patients with ConHD and healthy controls. This entails calculating the differences in chisquare and the difference in degrees of freedom of the two models. If the deleted path
coefficients are zero, this difference itself follows a chi-square distribution, and thus may
be used to test the hypothesis of zero path coefficients (Tabachnick & Fidell, 2001).
100 Chapter 6
Results
General characteristics of the data
Missing data was limited to the state and trait scores of one patient with ConHD and one
healthy control. These missing data were imputed using the regression method (SPSS 11).
According to the Shapiro-Wilk Statistic, trait, state anxiety, seriousness,
changeability, daily activities, and gross motor functioning were non-normally distributed
(p < .05) among patients with ConHD. Similarly, state anxiety, controllability, daily
activities, and gross motor functioning were non-normally distributed among the healthy
controls (p < .05). Therefore, we used robust maximum likelihood estimation, which
adjusts the standard errors and provides the Satorra-Bentler scaled chi-square (Satorra &
Bentler, 1988). Means, SDs, and Pearson product-moment correlation coefficients among,
state-trait anxiety, quality of life, and interpretation bias (seriousness, personal
responsibility, controllability, and changeability) are presented in Table 1.
Severity of heart disease
Spearman rank correlation coefficients among severity of heart disease and state-trait
anxiety, interpretation bias (seriousness, personal responsibility, controllability, and
changeability), gross motor functioning, and daily functioning are shown in Table 1. No
significant correlations (p > .05) were obtained. Only the correlation between disease
severity and gross motor functioning reached significance, indicating that patients with
more severe heart disease reported more difficulties with gross motor functioning, r (66) =
-.24, p = .05.
Hypothesized model
The hypothesized model showed an adequate fit to the data of patients with ConHD and
healthy controls. All fit indices suggested that the model fits well among the patients with
ConHD, Sattora-Bentler scaled χ2 (df = 6, n = 66) = 5.12, p = .45, RMSEA (90%-CI) = .00
(.00 - .15), CFI = 1.00, NNFI = 1.00 and among the healthy controls, χ2 (6, n = 50) = 1.98,
p = .92, RMSEA (90%-CI) = .00 (.00 - .06), CFI = 1.00, NNFI = 1.26.
-
2. Trait anxiety
-
3. State anxiety
-
b Patients
-.07
-.02
-
.21
.18
-.08
4
with ConHD differ significantly from healthy controls, p < .05,;
p < .001 (two-tailed); * p < .05, **; p < .01, *** p < .001 (two-tailed).
Note. a Patients
9. Gross motor functioning
8. Daily activities
7. Changeability
6. Controllability
5. Personal responsibility
4. Seriousness
.77***
-
.77***
.01
3
2. Trait anxiety
Controls
9. Gross motor functioning
8. Daily activities
7. Changeability
6. Controllability
5. Personal responsibility
4. Seriousness
3. State anxiety
-.12
2
1. Severity heart disease
ConHD
-
-.10
.12
-.12
-.06
-
.10
.22
.26*
.27*
-.02
6
-
.12
.21
-.15
.20
.18
-
.41**
.22
.20
.19
.12
.11
7
-
-.16
-.04
-.06
-.04
-.63***
-.52***
-
-.38**
-.42**
-.27*
-.27*
-.49***
-.47***
-.07
8
with ConHD differ significantly from healthy controls,
-
-.22
-.07
-.12
-
.41**
.24
.25*
.06
5
Table 1. Correlations, means, and SDs for patients with ConHD and controls
-
.44**
-.17
-.17
-.10
-.13
-.38**
-.24
-
.55***
-.23
-.16
-.27*
-.10
-.14
-.08
-.24
9
94.38 ± 12.64
80.15 ± 24.43
8.40 ± 3.08
25.44 ± 5.16
37.56 ± 10.22
63.08 ± 8.34
32.05 ± 8.48
36.05 ± 8.72
86.27 a ± 20.22
75.76 ± 27.98
8.08 ± 3.25
25.21 ± 6.61
47.97 b ± 12.71
65.88 ± 8.11
34.19 ± 11.49
36.88 ± 11.53
M± SD
Interpretation bias 101
102 Chapter 6
Multigroup analysis
We performed a multigroup analysis to test whether trait-state anxiety was more strongly
related to interpretation bias in ConHD than in the healthy controls. When the parameters
were not constrained to be equal across models, the model yielded a Sattora-Bentler
scaled χ2 (df =12, n = 116) = 10.36, p = .59, RMSEA (90%-CI) = .00 (.00- .12), CFI = 1.0,
NNFI = 1.09. When the parameters depicting the relation between state anxiety and
interpretation bias were forced to be equal across models, the model yielded a SattoraBentler scaled χ2 (df =16, n = 116) = 23.57, p = .10, RMSEA (90%-CI) = .09 (.00 - .16), CFI
= 1.0, NNFI = .98. As predicted, the chi-square difference test (∆χ2) between the nonrestrictive and restrictive model indicated that the relation between state anxiety and
interpretation bias was stronger among patients with ConHD than among healthy
controls, Sattora-Bentler scaled ∆χ2 (df = 4, n = 116) = 13.21, p < .05.
Direct and indirect effects
The direct and indirect effects suggested that interpretation bias mediated the relation
between trait-state anxiety and daily activities in patients with ConHD (Figure 1). First,
trait anxiety directly influenced state anxiety (standardized coefficients [st.c.] = .77, p <.
05) and state anxiety directly influenced interpretation bias: seriousness (st.c. = .15, p <.
05), personal responsibility (st.c. = .27, p <. 05), controllability (st.c. = .15, p <. 01), and
changeability (st.c. = .05, p <. 05). In addition, controllability and changeability directly
influenced daily activities (st.c. = -.95, p <. 05 and st.c. = -1.66, p <. 05, respectively).
Moreover, trait anxiety indirectly influenced daily activities via state anxiety and
interpretation bias (st.c. = -.91, p < .05). Trait anxiety indirectly influenced interpretation
bias via state anxiety: seriousness (st.c. = .11, p < .05), personal responsibility (st.c. = .20,
p < .05), controllable (st.c. = .12, p < .05), and changeability (st.c. = .04, p < .05), and state
anxiety indirectly influenced daily activities via interpretation bias (st.c. = -.32, p < .05).
In contrast to the predictions, however, interpretation bias did not mediate the
relation between trait-state anxiety and gross motor functioning. That is, although
personal responsibility directly influenced gross motor functioning (st.c. = -.39, p <. 05),
neither trait nor state anxiety was indirectly related to gross motor functioning (st.c. = .18, p > .05 and st.c. = - .15, p > .05, respectively).
As predicted the results of the healthy participants showed that interpretation bias
did not significantly mediate the relation between trait-state anxiety on the one hand and
daily activities and gross motor functioning on the other (Figure 1). That is, although trait
anxiety directly influenced state anxiety (st.c. = .75, p <. 05), and state anxiety directly
influenced changeability (st.c. = .07, p <. 05), interpretation bias did not significantly
influence daily activities or gross motor functioning. Moreover, state anxiety was not
Interpretation bias 103
indirectly related to gross motor functioning and daily activities (st.c. = -.03, p > .05 and
st.c. = .04, p > .05, respectively).
Figure 1. Results for the hypothesized model for patients with ConHD and healthy
controls. Numbers at straight arrows are standardized regression weights. Percentages at variables represent percentage
of variance explained by the model. First numbers are for patients with ConHD and bracketed numbers are for healthy
controls.
Discussion
As predicted, the present findings suggest that interpretation bias for ambiguous heartrelated sensations mediated the relation between trait-state anxiety and experienced
limitations in daily activities more strongly in ConHD than in healthy individuals. Highly
trait anxious patients who were also highly state anxious displayed a tendency to interpret
the heart-related sensations as more serious, less controllable, and less changeable. In
addition, they tended to perceive the person who experienced the symptoms as less
responsible for the cause and cure of the symptoms. In turn, the tendency to perceive the
heart related sensations as less controllable and changeable seemed to have an adverse
effect on daily functioning. In contrast to the predictions, interpretation bias did not
mediate the relation between trait-state anxiety and gross motor functioning. Moreover,
gross motor functioning was marginally associated with the severity of heart disease.
These findings only partially support the symptom perception and vulnerability stress
104 Chapter 6
hypothesis. In accordance with these hypotheses not the sole presence of ConHD but
ConHD in combination with trait-state anxiety was related to a diminished daily
functioning. However, in contrast to these hypotheses, the sole presence of ConHD and
not ConHD in combination with trait anxiety seemed to affect gross motor functioning.
An explanation of the possible adverse effects of interpretation biases on daily
functioning may be found in the anxiety literature (Williams, Watt, Macleod, & Mathews,
1997). A tendency to interpret heart sensations negatively may be adaptive for survival in
that this interpretation may result in the patients acting appropriately when there is
something wrong with their heart. However, in the absence of acute heart dysfunction,
this interpretation bias may be maladaptive. Specifically, a vicious circle may develop: trait
anxiety combined with elevated levels of state anxiety may result in a negative
interpretation bias; this bias may in turn induce a sense of powerlessness (Roesch &
Weiner, 2001), may increase the stressfulness of perceived heart symptoms, and may
result in avoidance of physical activities. Finally this avoidance may result in experienced
limitations in work, study, and other daily activities (see for a similar model on anxiety
disorders, Mathews & Macleod, 1994).
The present finding that severity of heart disease and not trait anxiety was
associated with gross motor functioning is in agreement with other studies. For example,
it has been shown that disease severity was related to physical functioning (Kamphuis et
al., 2002; Hager & Hess, 2005). Note that the observed relation between disease severity
and physical functioning may not fully reflect a direct relation between heart function and
gross motor functioning, as stated by the somatic hypothesis. Disease severity is
associated with more potentially stressful experiences, such as medical checkups,
hospitalizations, and open-heart surgery. These, experiences may in turn affect quality of
life in ConHD (Connoly, McClowry, Hayman, Mahony, & Artman, 2004). Therefore as
opposed to the somatic hypothesis, the relation between disease severity and physical
functioning may be partially mediated by stressful disease experiences.
It should be noted that the observed mediating effect of interpretation bias in the
present study was weak. This can be explained in the light of several study characteristics.
Firstly, participants evaluated symptoms of someone else with an unknown medical
diagnosis instead of evaluating their own symptoms. This was done to control for
individual differences in perceived heart sensation. Nevertheless, the supposed
dysfunctional heart-related schemes in patients with ConHD may be more accessible when
patients experience the symptoms themselves. Therefore, in future research, stronger
effects may be expected when patients evaluate their own heart-related sensations induced
by manipulations such as stress or physical exercises (Rietveld, Van Beest, & Everaerd,
1999). Moreover, the relatively weak effects suggest that there are moderator variables
Interpretation bias 105
that influence the relationship between interpretation bias and quality of life. For
example, the detrimental effect of negative interpretation biases may depend on
situational factors in daily life. For example, an upcoming stressful exam may increase
experienced physical sensations and state anxiety (Rietveld et al., 1999), and in turn may
trigger negative interpretation biases. In the absence of such situational factors,
interpretation bias may not adversely affect daily functioning. Another explanation for the
relatively weak mediating effect of interpretation bias is that we measured interpretation
bias for only one situation. Assessing interpretation bias for several ambiguous situations
may increase reliability of the measures. Therefore, more research is necessary to test the
effect of interpretation biases on different dimensions of quality of life.
Caution is warranted to the generalizability of the present findings, as the sample
sizes were relatively small. The absence of a significant mediating effect of interpretation
bias in the healthy control group may be due to a lack of statistical power. However,
inspection of the magnitude of the present findings in the healthy control group revealed
that the amount of variance of interpretation bias explained by state anxiety (<1 - 4 %) was
negligible. Taken together, the present study suggests that the relation between trait
anxiety and daily functioning can be explained by a negative interpretation bias for heart
sensations specifically in ConHD. In addition, it was demonstrated that elevated levels of
both trait and state anxiety are required to reveal a relationship between interpretation
bias and daily functioning. As this study was correlational, we cannot draw strong
conclusions concerning the causal relationships among trait-state anxiety, interpretation
bias, and daily functioning. Studies addressing the causal relationship between these
concepts are required. Causal relationships could be investigated by testing whether
induction of negative interpretations leads to reduced physical exercise or social activities
or whether reduction of negative interpretations leads to an increased daily functioning.
Nonetheless, the present study suggests that trait anxiety in combination with ConHD
rather than ConHD per se has detrimental consequences for daily functioning. In contrast,
the objective heart disease may have detrimental consequences for gross motor
functioning. To improve daily functioning and gross motor functioning in patients with
ConHD different interventions may be needed. To improve gross motor functioning,
patients may benefit most from interventions focussing on somatic functioning. To
improve daily functioning, patients may benefit from additional psychological
interventions, aimed at reducing negative interpretations of heart sensations.
106 Chapter 6
References
Bentler, P.M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107,
238-246.
Bollen, K.A., & Long, J.S. (1993). Testing structural equation models. Newbury Park, CA: Sage.
Bower, G.H. (1981). Mood and memory. The American Psychologist 36: 129-148.
Browne, M.W., & Cudeck, R. (1993). Alternative ways of assessing model fit. In K.A. Bollen, & J.S.
Long. (Eds.), Testing structural equation models (pp. 136-162). Newbury Park, CA: Sage.
Bruil, J., Fekkes, M., Vogels, T., & Verrips, G.H.W. (2004). TAAQOL Manual Leiden Center for
Child Health and Pediatrics. Leiden: LUMC-TNO
Connoly, D., McClowry, S., Hayman, L., Mahony, L., & Artman, M. (2004). Posttraumatic stress
disorder in children after cardiac surgery. Journal of Pediatrics, 144, 480-484.
De Beurs, E., Comijs, H., Twisk, J.W.R, Sonnenberg, C., Beekman, A.T.F., & Deeg, D. (2005).
Stability and change of emotional functioning in late life: modelling of vulnerability
profiles. Journal of Affective Disorders, 84, 53-62.
Fekkes, M., Kamphuis, R.P., Ottenkamp, J., Verrips, E., Vogels, T., Kamphuis, M., & VerlooveVanhorick, S.P. (2001). Health-related quality of life in young adults with minor congenital
heart disease. Psychology and Health, 16, 239-250.
Hager, A., & Hess, J. (2005). Comparison of health related quality of life with cardiopulmonary
exercise testing in adolescents and adults with congenital heart disease. Heart, 91, 517-520.
Jöreskog, K.G., & Sörbom, D. (2001). LISREL 8: Structural Equation Modeling with the SIMPLIS
Command Language. Chicago: Scientific Software International.
Kamphuis, M., Ottenkamp, J., Vliegen, H.W., Vogels, T., Zwinderman, K.H., Kamphuis, R.P., &
Verloove-Vanhorick S.P. (2002). Health related quality of life and health status in adult
survivors with previously operated complex congenital heart disease. Heart, 87, 356-362.
Mathews, A., & MacLeod, C. (1994). Cognitive approaches to emotion and emotional disorders.
Annual Review of Psychology, 45, 25-50.
McDonald, R.P., & Ho, M.H. (2002). Principles and practise in reporting structural equation
analyses. Psychological Methods, 7, 64-82.
McHorney, C.A., Ware, J.E., & Raszek, A.E. (1993). The MOS 36-item short-form health survey
(SF-36) II: Psychometric and clinical tests of validity in measuring physical and mental
health constructs. Medical Care, 31, 247-263.
Moss-Morris, P., Weinman, J., Petrie, K.J., Horne, R., Cameron, L.D., & Buick, D. (2002). The
revised illness perception questionnaire (IPQ-R). Psychology and Health, 17, 1-16.
Page, L.A., Howard, L.M., Husain, K., Tong, J., Dowson, A.J., Weinman, J., & Wessely, S.C. (2004).
Psychiatric morbidity and cognitive representations of illness in chronic daily headache.
Journal of Psychosomatic Research, 57, 549-555.
Paschalides, C., Wearden, A.J., Dunkerley, C., Bundy, C., Davies, R., & Dickens, C.M. (2004). The
association of anxiety, depression and personal illness representations with glycaemic
control and health-related quality of life in patients with type 2 diabetes mellitus. Journal
of Psychosomatic Research, 57, 557-564.
Interpretation bias 107
Pennebaker, J.W. (1982). The psychology of physical symptoms. New York: Springer-Verlag.
Rietveld, S., Mulder, B.J.M., Van Beest, I., Lubbers, W., Prins, P.J.M., Vioen, S., BennebroekEvererz, F., Vos, A., Casteelen, G., & Karsdorp P. (2002). Negative thoughts in adults with
congenital heart disease. International Journal of Cardiology, 86, 19-26.
Rietveld, S., Van Beest, I., & Everaerd, W. (1999). Stress-induced breathlessness in asthma.
Psychological Medicine, 29, 1359-1366.
Roesch, S.C., & Weiner, B. (2001). A meta-analytic review of coping with illness; do causal
attributions matter? Journal of Psychosomatic Research, 50, 205-219.
Rose, M., Köhler, K., Köhler, F., Sawitzky, B., Fliege, H., & Klap, B.F. (2005). Determinants of the
quality of life of patients with congenital heart disease. Quality of Life Research, 14, 35-43.
Rusting, C.L. (1998). Personality, mood, and cognitive processing of emotional information: three
conceptual frameworks. Psychological Bulletin, 124,165-196.
Satorra, A., & Bentler, P.M. (1988). Scaling corrections for chi-square statistics in covariance
structure analysis. Proceedings of the American Statistical Association, 308-313.
Spielberger, C.D., Gorsuch, R.L., & Lusthene, R.E. (1970). Manual for the State-Trait Anxiety
Inventory. Palo Alto: Consulting Psychological Press.
Swartzman, L.C., & McDermid, A.J. (1993). The impact of contextual cues on the interpretation of
and response to physical symptoms. Journal of Behavioral Medicine, 16, 183-198.
Tabachnick, B.G., & Fidell, L.S. (2001). Using multivariate statistics (pp. 653-773). Boston: Allyn
and Bacon.
Turk, D.C., Rudy, T.E., & Salovey, P. (1986). Implicit models of illness. Journal of Behavioral
Medicine, 9, 453-474.
Van der Ploeg, H.M., Defares, H.B., & Spielberger, C.B. (1979). Handleiding bij de
zelfbeoordelingsvragenlijst. Een nederlandse bewerking van de Spielberger State-Trait
Anxiety Inventory. [Validity of the Zelf-Beoordelings-Vragenlijst. A Dutch version of the
Spielberger State-Trait Anxiety Inventory]. Lisse: Zwets and Zeitlinger.
Warnes, C.A., Liberthson, R., Danielson, G.K., Dore, A., Harris, L., Hoffman, J.I., Somerville, J.,
Williams, R.G., & Webb, G.D. (2001). Task force 1: the changing profile of congenital heart
disease in adult life. Journal of the American College of Cardiology, 37, 1170-1175.
Watson, D., & Pennebaker, J.W. (1989). Health-complaints, stress, and distress: exploring the
central role of negative affectivity. Psychological Review, 96, 234-254.
Willams, J.M.G., Watt, F.N., Macleod, C.M., & Mathews, A. (1997). Attention to emotional stimuli.
In J.M.G., Willams, F.N., Watt, C.M., Macleod, & A., Mathews (Eds.), Cognitive psychology
and emotional disorders (pp. 51-72). Chichester: John Wiley and Sons.
Zvolensky, M.J., Kotov, R., Antipova, A.V., & Schmidt, N.B. (2005). Diathesis stress model for
panic-related distress: a test in a Russian epidemiological sample. Behaviour Research and
Therapy, 43, 521-532.
General discussion
110 Chapter 7
General discussion
This thesis was designed to investigate whether (1) congenital heart disease (ConHD) has
detrimental effects on patients’ psychological and cognitive functioning, (2) whether the
combination of temperamental vulnerabilities (e.g., trait anxiety) and ConHD explains
perceptual biases for heart-related symptoms, and 3) whether these perceptual biases
mediate the relation between trait anxiety and quality of life in ConHD. For these
objectives, a meta-analysis was performed on the existing literature on psychological and
cognitive functioning in children and adolescents with ConHD. Moreover, four studies
were conducted on the role of trait anxiety and perceptual biases in ConHD. In these
studies it was examined whether high trait anxious patients with ConHD displayed
perceptual biases for heart-related sensations subsequent to acute stress or the
presentation of subliminal or supraliminal heart-related cues. In addition, it was tested
whether a negative interpretive bias with respect to heart-related sensations mediated the
relation between trait anxiety and quality of life.
In this section we summarize the main results of the studies. We evaluate the
findings in the light of other relevant findings reported in research and we present some
limitations of the studies. Possible implications for the assessment and treatment of
patients with ConHD will be given and ideas for future research will be presented
Psychological and cognitive functioning in ConHD
Findings of research into the effect of ConHD on psychological and cognitive functioning
of children and adolescents are inconsistent (e.g., Goldberg et al., 2000, Ellerbeck et al.,
1998; Forbess, Visconti, Bellinger, Howe, & Jonas, 2002; Visconti, Bichell, Jonas,
Newburger, & Bellinger, 1999). In order to systematically review the research, a metaanalysis was conducted on behaviour problems (as assessed by the CBLC) and cognitive
functioning (as assessed by intelligence tests) (Chapter 2). The findings of the metaanalysis revealed that the effect sizes in studies dealing with psychological and cognitive
functioning varied considerably. This indicated that the findings were influenced by
characteristics of the patient sample, such as chronological age or disease severity.
Chronological age appeared to be related to psychological functioning, whereas disease
severity was related to cognitive functioning. Specifically, pre-adolescents with ConHD
showed more internalizing (e.g., anxiety and depression) problems and to a lesser extent
externalizing problems (e.g., aggression) than a comparison group. Patients with more
severe ConHD, such as those with hypoplastic left heart syndrome and tetralogy of Fallot,
exhibited reduced cognitive functioning, specifically with respect to performance IQ as
compared to normative data.
Discussion 111
The first conclusion that can be drawn from these findings is that the sole presence
of cardiac dysfunction is related to cognitive functioning. Physiological damage either
caused by the heart defect, invasive medical procedures, or chromosomal anomalies may
decrease cognitive functioning. A second conclusion that can be drawn from these findings
is that the sole presence of cardiac dysfunction does not affect internalizing and
externalizing behaviour problems. This finding contrasts with the somatic hypothesis
stating that cardiac dysfunction directly and linearly increases the perception of heart
symptoms and in turn reduces the patient’s quality of life (e.g., Rose et al., 2005; Wilson &
Cleary, 1995). However, the findings may support the vulnerability-stress hypothesis
(e.g., De Beurs et al., 2005; Zvolensky et al., 2005), as exposure to certain risk factors
during the course of a patient’s development may increase behaviour problems in ConHD.
Due to the limited number of studies in the current meta-analysis, it was
impossible to determine the risk factors that may affect the development of internalizing
behaviour problems in adolescents with ConHD. However, there are some findings in
recent studies suggesting that the long-lasting vulnerability factor trait anxiety may be an
important risk factor in ConHD. For example, it has been suggested that hormonal
changes in the brain during adolescence may trigger the expression of genetic
vulnerabilities for dysfunctional behaviour (Walker, Sabuwalla, & Huot, 2004). Moreover,
it has been shown that the combination of trait anxiety and exposure to potential stressors
are related to anxiety disorders (e.g., Zvolensky, Kotov, Atipova, & Schmidt, 2005). To test
the hypothesis that trait anxiety is a risk factor in ConHD and to unravel the processes that
may explain the possible relation between trait anxiety and patients’ psychological
functioning, we conducted four studies. The findings of these studies will be described in
the next paragraph.
The role of trait anxiety and perceptual biases in ConHD
To gain more insight in the effect of trait anxiety in ConHD, we developed a model on the
basis of the vulnerability-stress hypothesis (e.g., De Beurs et al., 2005; Zvolensky et al.,
2005) and the symptom perception hypothesis (Pennebaker, 1982). It was hypothesized
that the possible relationship between trait anxiety and quality of life in ConHD was
explained by perceptual biases for heart-related symptoms. These biases are characterized
by a tendency to selectively attend to heart-related sensations and interpret ambiguous
sensations as heart symptoms (e.g., Mathews & MacLeod, 1994). In the subsequent
studies we tested this hypothesis (Chapter 3, 4, 5, and 6).
In two studies, it was examined whether patients with ConHD who are also high
trait anxious tend to show an increased perception of heart-related symptoms that cannot
be explained by acute cardiac dysfunction (Chapter 3 and 4). In both studies patients with
112 Chapter 7
ConHD and healthy controls were exposed to either a harmless heart-related cue (false
heart rate sounds) or acute psychological stress to trigger perceptual biases. Physiological
parameters such as heart rate, respiratory rate, arterial partial pressure of CO2, and blood
pressure were assessed continuously. As predicted, the findings revealed that high trait
anxious patients with ConHD showed an increased perception of heart symptoms after
exposure to heart-related cues while there were no signs of cardiac dysfunction. These
findings support the vulnerability-stress and symptom perception hypothesis and suggest
that harmless heart related cues and stress might trigger an increased perception of heart
symptoms in high trait anxious patients with ConHD even in the absence of acute heart
dysfunction.
In chapter 3 and 4 we demonstrated that heart-related cues prompt perceptual
biases in high trait anxious patients with ConHD. However, it remains unclear to what
extent heart-related cues that remain outside the patient’s awareness influence the
perception of heart symptoms. Findings suggest that emotional stimuli such as diseaserelated cues could be processed at a preattentive level (i.e. before conscious awareness)
(Lim & Kim, 2005; Lundh, Wikström, Westerlund, & Öst, 1999). In chapter 5, it was tested
whether preattentive processing of disease-related cues may explain biased perception of
heart symptoms in high trait anxious patients with ConHD. Participants categorized
heart-related (heart rate) or neutral sensations (constant vibration) as either heart or
neutral. Both sensations were evoked using a bass speaker that was attached on the chest
of the participants. Biased perception of heart-sensations would become evident by an
increased difficulty shifting attention away from heart-related sensations, in turn
decreasing the categorization of heart-related sensations. The findings revealed that high
trait anxious patients with ConHD showed an increased delay after heart sensations that
were preceded by subliminal heart cues. This suggested that biased perception in high
trait anxious patients with ConHD is easily elicited even when patients are unaware of the
eliciting stimuli.
In Chapter 6, it was determined whether perceptual biases for heart-related
symptoms mediate the relation between trait anxiety and quality of life. In this study it
was tested whether a negative interpretation of ambiguous heart-related sensations
described in a written vignette mediated the relationship between trait anxiety and the
physical subscale of quality of life, i.e. perceived gross motor functioning and daily
functioning. In support of the vulnerability-stress and symptom perception hypothesis,
negative interpretation of heart-related sensations mediated the relation between trait
anxiety and daily functioning in ConHD and not in healthy controls. However, in contrast
to the hypotheses, the sole presence of ConHD and not trait anxiety was marginally related
to perceived gross-motor functioning. At first sight, this latter finding seems to support
Discussion 113
the somatic hypothesis stating that cardiac dysfunction is directly related to perceived
physical symptoms and in turn to perceived gross motor functioning (e.g., Rose et al.,
2005; Wilson & Cleary, 1995). However, it is also possible that the relationship between
disease severity and perceived gross motor functioning is mediated by other variables than
the experience of heart symptoms. For example, it has been shown that a patient’s belief in
self-efficacy or the recommendations of the cardiologist regarding physical activity
mediated the relationship between disease severity and involvement in physical activity
(Bar-Mor, Bar-Tal, Krulik, & Zeevi, 2000). Moreover, a third factor, like chromosomal
anomalies may explain the observed relationship. For example, it is possible that motor
delay is not so much caused by the presence of ConHD but by chromosomal anomalies
that are associated with both ConHD and motor delay (e.g., Swillen et al., 2005).
Overall the present findings provide support for the assumption that trait anxiety
in combination with disease experience results in the development of perceptual biases for
heart-related symptoms and in turn a diminished quality of life with respect to daily
functioning.
Methodological issues
Some methodological issues of the present thesis may need clarification. An important
limitation is that the presented studies concerning the role of trait anxiety were quasiexperimental designs (Chapter 3, 4, 5, 6). Participants in the study could not be randomly
assigned to the ConHD group or the high anxiety group. Therefore, it cannot be excluded
that a fourth factor associated with ConHD, trait anxiety, and perceptual biases may
explain the present findings. For example, in the present thesis it was assumed that longlasting factors such as trait anxiety or a history of disease experiences explained biased
perception in ConHD. However, these long-lasting factors are also associated with more
temporary factors, such as state anxiety (Rusting, 1998) and acute cardiac dysfunction
making it difficult to determine the exact causes of the observed perceptual bias in high
trait anxious patients with ConHD. For example, it is possible that the observed perceptual
bias for heart symptoms in high trait anxious patients with ConHD in the current thesis is
explained by an increased sensitivity of high state anxious individuals to perceive acute
cardiac dysfunction.
There are some findings in the present thesis that suggest that it is unlikely that
only temporary factors, such as acute cardiac dysfunction and state anxiety, explained the
findings. Firstly, in two studies (Chapter 3 and 4) no evidence was found that acute cardiac
dysfunction actually explained the observed perceptual biases in ConHD. In these
experiments continuous assessment of cardiac functioning revealed that there were no
physiological differences between patients with ConHD and healthy individuals with
114 Chapter 7
respect to heart rate, respiratory rate, arterial partial pressure of CO2, and diastolic and
systolic blood pressure. Moreover, patients with ConHD did not show extrasystoles or
heart rhythm disturbances during the experiment. These findings suggest that disease
history rather than acute cardiac deviations explain the observed perceptual biases in
ConHD. However, some caution is warranted, as we did not assess other physiological
parameters, such as cardiac output. Therefore, we cannot exclude the possibility that the
increased perception of heart symptoms of high trait anxious patients with ConHD was
explained by differences in other physiological parameters. Secondly, concerning the
influence of state anxiety, in one study (chapter 4) no evidence was found that elevated
levels of state anxiety alone explained the observed perceptual bias in high trait anxious
patients with ConHD. In this study it was demonstrated that even though all participants
displayed a subjective and physiological anxiety response, only the high trait anxious
patients with ConHD exhibited perceptual biases during stress. This corroborates our
hypothesis that trait anxiety influences perceptual biases and that the observed
relationship between trait anxiety and perceptual biases could not be explained solely by
increased levels of state anxiety (Rusting 1998, 1999).
A related issue is that we did not test whether the effect of trait anxiety and ConHD
on biased perception of heart symptoms was simply mediated by learning experiences
with physical symptoms. However, several experiments have been conducted that address
the impact of learning experiences on symptom perception. These experiments revealed
that individuals acquire perceptual biases through operant and classical conditioning (Van
den Bergh 1998; Hölzl et al., 2005). Moreover, specifically the high trait anxious
individuals appeared to be vulnerable acquiring these biases after classical conditioning
(Devriese et al., 2000; Put et al., 2004; Fredrikson et al., 1993). These findings provide
evidence that high trait anxious patients with ConHD may acquire perceptual biases
subsequent to disease related experiences.
In the present study, it was assumed that trait anxiety moderated the relationship
between ConHD and biased symptom perception. However, alternative hypotheses such
as the psychosomatic hypothesis and disability hypothesis postulate that trait anxiety may
increase disease severity or that disease may increase trait anxiety (Watson & Pennebaker
1989; Costa & McCrae, 1987). Little support is found for these hypotheses in the present
thesis. That is, trait anxiety did not differ between patients and healthy controls.
Moreover, disease severity was unrelated to trait anxiety. These findings are in accord with
other studies on patients with ConHD, demonstrating that patients with ConHD did not
display higher levels of trait anxiety or neuroticism (Cox, Lewis, Stuart, & Murphy, 2002;
Utens et al., 1994). Therefore, there is no reason to modify our assumption that trait
anxiety is a moderator rather than a mediator.
Discussion 115
Another limitation of the present thesis is that we included a healthy comparison
group to test whether learning experiences with ConHD influenced perceptual biases for
heart symptoms. This healthy comparison group consisted of individuals without
temporary or chronic physical disease and who did not use medication. We included such
a group rather than a group of individuals only without heart disease, because symptoms,
such as heart pounding, dizziness, and shortness of breath, may also be associated with
other physical diseases. However, a disadvantage of this procedure is that patients with
ConHD did not only differ from healthy individuals by the presence of ConHD, but also by
the presence of a chronic physical disease in general. Therefore, experiences with disease
in general rather than specifically with heart disease may be related to an increased
perception of heart symptoms. However, conversely, it has been shown that patients with
asthma display biased perceptions towards specifically asthma-related symptoms
(breathlessness) and not towards heart-related symptoms such as heart pounding
(Rietveld & Houtveen, 2004). This may imply that an increased perception of heartrelated symptoms in ConHD is the result of the patient’s heart disease history.
Nevertheless, future research is necessary in which a hospitalized comparison group is
included with chronic congenital problems not associated with heart related symptoms
(e.g., oro-facial deformities or orthopaedic congenital limb deformities).
Recommendations for clinical practice
On the basis of the findings of the present thesis, we may conclude that in order to prevent
the development of psychopathology and reduced daily and cognitive functioning in
patients with ConHD, psychological assessment and treatment are necessary from an early
age. An ideal strategy would be to screen for reduced cognitive functioning from the age of
four, specifically with respect to performance IQ (e.g., visual spatial abilities) and to refer
children with reduced cognitive functioning to special educational interventions (Swanson
& Sachse-Lee, 2000).
Moreover, a recommended strategy would be to assess the patient’s psychological
functioning during pre-adolescence, focusing on behaviour problems, unexplained heart
symptoms, and diminished daily functioning. The trait version of the State-Trait Anxiety
Inventory (STAI; Spielberg, Gorsuch, & Lusheve, 1970) could be a helpful tool to
determine which patients are at increased risk for adverse psychological development.
Patients who report heart symptoms that cannot be explained by simultaneous cardiac
dysfunction or who report reduced daily functioning may benefit from psychological
treatment. It has been shown that reassurance by a cardiologist only is not an effective
intervention for patients who seek medical treatment for unexplained cardiac symptoms.
Most patients continue to experience heart symptoms, persist in worrying about heart
116 Chapter 7
disease, and restrict their activities (Mayou, Bryant, Forfar, & Clark, 1994; Mayou,
Sprigings, Gilbert, 1999; Swinson, Soulios, Cox, & Kuch, 1992; Salkovskis & Warwick,
1986). This suggests that patients with ConHD need psychological treatment rather than
reassurance.
Psychological treatment of patients with ConHD may preferably be aimed at
reducing anxiety levels and catastrophic interpretations of heart-related sensations and
cues. Cognitive-behaviour interventions have been shown to be useful techniques to
diminish catastrophic interpretations and anxiety (Mayou, Sprigings, Birkhead, & Price,
2002; Mayou et al., 1997). For example, these treatments could help to identify which
internal and external heart-related cues (such as a hospital setting) trigger anxiety and
heart symptoms. Subsequently, patients could test evidence for having acute heart
dysfunction and identify testable, alternative explanations in which anxiety, physical
exercise, or attentional factors account for the symptoms experienced (Salkovskis &
Warwick, 1986; Mayou et al., 1997). Alternatively, high trait anxious patients may also
benefit from muscle relaxation training, decreasing their anxiety levels (Eifert, 1992).
Apart from these interventions exposure to interoceptive cues through physical
exercise or hyperventilation-provocation tests could also be applied. Such exposure
techniques provide patients the opportunity to learn more appropriate interpretations of
body sensations and to inhibit conditioned fear responses (Swinson et al., 1992; Aikens et
al., 1999). When anxiety has decreased to an acceptable level, patients may gradually
increase their level of activity in daily life (Mayou et al., 1997). For example, they could
draw up a hierarchy of activities they are avoiding because of heart symptoms and
gradually expose themselves to these activities. Another option is to offer patients exercise
training (Fredriksen et al., 2000; Therrien et al., 2003; Rhodes et al., 2005). More
importantly, increasing the activity levels in patients with ConHD may not only be
beneficial for anxiety levels and maladaptive beliefs about heart symptoms, it may also
increase general fitness and reduces the risk of additional health problems such as
cardiovascular disease (Thalouw & Fredriksen, 2004).
An additional recommended therapeutic strategy would be to teach patients to
accurately monitor the sensations arising from everyday activity and emotions (Cioffi,
1991), because acute heart dysfunction is realistic in ConHD. Cognitive behaviour
interventions alone do not improve accurate heartbeat monitoring (Ehlers, Breuer, Dohn,
& Fiegenbaum, 1995). Therefore, in order to improve heartbeat perception additional
techniques are required, such as biofeedback training (O’Brien, Reid, & Jones, 1998;
Schandry & Weitkunat, 1990). In biofeedback training patients are asked to verify whether
feedback lights or sounds flash immediately after each heartbeat or after a brief delay.
Discussion 117
Future research
There are several areas of interest for future research. Firstly, perceptual biases in the
present study were only assessed in the absence of cardiac dysfunction. It would, however,
be interesting to determine whether high trait anxious patients with ConHD are also more
sensitive to real cardiac dysfunction such as arrhythmias. If so, biased perception of heart
symptoms may also be beneficial for a patient’s physical health. Findings in the literature
indicate that high trait anxious patients with disease are more sensitive to signs of their
disease (Ryan, Dulay, Suprasongsin, & Becker, 2002; Cameron, Leventhal, & Love, 1998).
For example, it has been shown that high anxious patients with diabetes were more
accurate perceivers of their blood glucose levels during experimentally induced
hypoglycaemia (Ryan et al., 2002). Moreover, it has been shown that high trait anxious
patients receiving medication as opposed to placebo medication reported more
medication-related symptoms (and not more medication-unrelated symptoms) then low
trait anxious patients (Cameron et al., 1998). In order to test the sensitivity hypothesis in
ConHD a diary study might be designed to test whether cardiac arrhythmias coincide with
perceived heart symptoms (see also Barsky, Cleary, Brener, & Ruskin, 1993; Barsky,
Cleary, Barnett, Christiansen, & Ruskin, 1994; Hoehn-Saric, McLeod, Funderburk, &
Kowalski, 2004). An alternative method is to manipulate the patient’s heart rate in an
experiment. For example, the perception of heart symptoms could be assessed in patients
with a pacemaker, while their heart rate is manipulated by varying the pacing rate of the
pacemaker (e.g., Windmann, Schonecke, Frohlig, & Maldener, 1999).
Another direction for future research pertains to the impact of biased perception
on quality of life. In the present thesis it was tested whether negative interpretations
influence perceived motor functioning and daily activities in ConHD (Chapter 6). The
findings only revealed a relatively weak relation between symptom interpretations and
perceived daily functioning, whereas perceived motor functioning was marginally related
to disease severity. Because these findings may be attributed to several methodological
limitations more research is required on this topic to unravel the processes that influence
quality of life. For example, quality of life, cardiac functioning, and catastrophic
interpretations were not assessed at the same moment. That is, gross motor and daily
functioning were assessed by retrospective self-report measures, whereas cardiac
functioning was determined by the initial diagnosis. Therefore, we are unable to verify
whether reduced physical exercise and avoidance of daily activities are actually
precipitated by cardiac dysfunction or by catastrophic interpretations of heart symptoms.
Moreover, although perceived daily activities and gross motor functioning provide
information about patients’ psychological adjustment, it is unclear how these perceptions
are related to objective physical functioning and daily activities. Objective measurement of
118 Chapter 7
activity levels provides information of patients’ physical fitness and may predict future
psychological and health problems such as low self-esteem and coronary heart disease
(Thaulow & Fredriksen, 2004). To gain more insight in the effect of catastrophic
interpretations on a patient’s objective physical functioning, an experiment could be
conducted in which an interpretive bias is induced before an exercise task. For example, a
suitable method for induction of interpretative bias is to present patients a task containing
negative or positive interpretations about ambiguous physical symptoms (Mathews &
Mackintosh, 2000). In this way, it could be tested whether a negative interpretative bias
affects a patient’s physical performance.
Another fruitful area of future research is to study the effect of biased perception
on medical consumption in ConHD. Increased hospital visits due to benign heart
symptoms may result in an inappropriate use of expensive diagnostic tests. Conversely,
increased hospital visits due to acute cardiac dysfunction may result in effective treatment
and increased survival chances in ConHD. Findings in research suggest that high trait
anxious patients with ConHD may tend to seek medical care more often for heart
symptoms of both cardiac and non-cardiac origin. For example, it has been shown that
anxiety is positively related to the number of doctor consultations for heart symptoms that
cannot be explained by cardiac dysfunction (Ehlers, Mayou, Sprigings, & Birkhead, 2000;
Yingling, Wulsin, Arnold, & Rouan, 1993). Moreover, it has been demonstrated that
exposure to heart-related disease experiences in the past is associated with increased
number of visits to the emergency department for unexplained heart symptoms (Aikens et
al., 1999; Fleet et al., 1996). In addition, it has been revealed that patients who are anxious
and interpret symptoms catastrophically seek medical treatment more rapidly for real
physical disease (Ristvedt & Trinkaus 2005; Walsh, Lynch, Murphy & Daly, 2004;
Rozniatowski et al., 2005). Finally, it has been demonstrated that the prevalence of panic
attacks in individuals seeking medical treatment for heart symptoms (chest pain and
palpitations) of cardiac origin is higher than the prevalence of panic attacks in the general
population (Ehlers et al., 2000; Yingling, Wulsin, Arnold, & Rouan, 1993). From these
findings it can be inferred that high trait anxious patients with ConHD seek medical care
faster and more often when cardiac dysfunction is either present (true positives) or absent
(false positives). It would be important to test this hypothesis in patients with ConHD in
order to improve the effectiveness of medical care.
The present study was based on the assumption that a history of disease
experiences is a risk factor in the development of perceptual biases. It would be appealing
to investigate whether specific events such as the occurrence of arrhythmias or open-heart
surgeries enhance the perception of heart symptoms in high trait anxious patients.
Moreover, it would be interesting to establish the developmental course of perceptual
Discussion 119
biases and the factors that maintain these biases after exposure to a potentially stressful
disease experience. Finally, another important area for future research is the development
of psychological interventions that may reduce biased perception of heart symptoms in
ConHD. For example, it has been shown that a brief psycho-educational intervention
based on cognitive-behavioural principles reduces disability in patients with benign
palpitations (Mayou et al., 2002). It is important to resolve whether such interventions are
effective for patients with ConHD.
Conclusion
Little is known about the mechanisms that explain how ConHD adversely affects patients’
quality of life. To gain more insight in these mechanisms a model was developed in the
present thesis based on the symptom–perception and the vulnerability-stress hypothesis.
It was hypothesized that trait anxiety constitutes a vulnerability factor in ConHD for
adverse psychological outcome. Moreover, it was hypothesized that the relationship
between trait anxiety and psychological functioning is mediated by perceptual biases for
heart-related symptoms. In line with these hypotheses, the present thesis showed that
high trait anxious patients with ConHD are at increased risk of developing quality of life
problems. High trait anxious patients with ConHD display perceptual biases for heartrelated symptoms and in turn develop a reduced quality of life. These findings are a
starting point for the development of evidence-based psychological treatment aimed at
reducing perceptual biases and may eventually contribute to an improved quality of life in
patients with ConHD.
References
Aikens, J.E., Michael, E., Levin T., Myers T.C., Lowry E., & McCracken, L.M. (1999). Cardiac
exposure history as a determinant of symptoms and emergency department utilization in
noncardiac chest pain patients. Journal of Behavioural Medicine, 22, 605-617.
Bar-Mor, G., Bar-Tal, Y., Krulik, T., & Zeevi, B. (2000). Self-efficacy and physical activity in
adolescents with trivial, mild, or moderate congenital cardiac malformations. Cardiology
in the Young, 10, 557-559.
Barsky, A.J., Cleary, P.D., Brener, J., & Ruskin, J.N. (1993). The perception of cardiac activity in
medical outpatients. Cardiology, 83, 304-315.
Barsky, A.J., Cleary, P.D., Barnett, M.C., Christiansen, C.L., & Ruskin, J.N. (1994). The accuracy of
symptom reporting by patients complaining of palpitations. The American Journal of
Medicine, 97, 214-221.
120 Chapter 7
Cameron, L.D., Leventhal, H., & Love, R.R. (1998).Trait anxiety, symptom perceptions, and illnessrelated responses among women with breast cancer in remission during a tamoxifen
clinical trial. Health Psychology, 17, 459-469.
Cioffi, D. (1991). Beyond attentional strategies: a cognitive-perceptual model for somatic
interpretation. Psychological Bulletin, 109, 25-41.
Costa, P.T., & McCrae, R.R. (1987). Neuroticism, somatic complaints, and disease: is the bark worse
than the bite? Journal of Personality, 55, 299-316.
Cox, D., Lewis, G., Stuart, G., & Murphy, K. (2002). A cross-sectional study of the prevalence of
psychopathology in adults with congenital heart disease. Journal of Psychosomatic
Research, 52, 65-68.
De Beurs, E., Comijs, H., Twisk, J.W.R., Sonnenberg, C., Beekman, A.T.F., & Deeg, D. (2005).
Stability and change of emotional functioning in late life: modelling of vulnerability
profiles. Journal of Affective Disorders, 87, 53-62.
Devriese S., Winters, W., Stegen, K., Van Diest, I., Veulemans, H., Nemery, B., Eelen, P., Van de
Woestijne, K., & Van den Bergh, O. (2000). Generalization of acquired somatic symptoms
in response to odors: a pavlovian perspective on multiple chemical sensitivity.
Psychosomatic Medicine, 62, 751-759.
Ehlers, A., Breuer, P., Dohn, D., & Fiegenbaum, W. (1995). Heartbeat perception and panic
disorder: possible explanations for discrepant findings. Behaviour Research and Therapy,
33, 69-76.
Ehlers, A., Mayou, R.A., Sprigings, D.C., & Birkhead, J. (2000). Psychological and perceptual
factors associated with arrhythmias and benign palpitations. Psychosomatic Medicine, 62,
693-702.
Eifert, G.H., (1992). Cardiophobia: a paradigmatic behavioural model of heart focused anxiety and
non-anginal chest pain. Behaviour Research and Therapy, 30, 329-345.
Ellerbeck, K.A., Smith, M.L., Holden, E.W., McMenamin, S.C., Badawi, M.A., Brenner, J.I., Kan,
J.S., & Hyman, S.L. (1998). Neurodevelopmental outcomes in children surviving dtransposition of the great arteries. Journal of Developmental and Behavioral Pediatrics,
19, 335-341.
Fleet, R.P., Dupuis, G., Marchand, A., Burelle, D., Arsenault, A., & Beitman, B.D. (1996). Panic
disorder in emergency department chest pain patients: prevalence, comorbidity, suicidal
ideation, and physician recognition. American Journal of Medicine, 101, 371-380.
Forbess,
J.M.,
Visconti,
K.J.,
Bellinger,
D.C.,
Howe,
R.J.,
&
Jonas,
R.A.
(2002).
Neurodevelopmental outcomes after biventricular repair of congenital heart defects.
Journal of Thoracic and Cardiovascular Surgery, 123, 631-639.
Fredriksen, P.M., Kahrs, N., Blaasvaer, S., Sigurdsen, E., Gundersen, O., Roeksund, O., Norgaand,
G., Vik, J.T., Soerbye, O., Ingjer, E., & Taulow, E. (2000). Effect of physical training in
children and adolescents with congenital heart disease. Cardiology in the Young, 10, 107114.
Discussion 121
Frederikson, M., Fürst, C.J., Lekander M., Rotstein, S., & Blomgren, H. (1993). Trait anxiety and
anticipatory immune reactions in women receiving adjuvant chemotherapy for breast
cancer. Brain, Behavior, and Immunity, 7, 79-90.
Goldberg, C.S., Schwarz, E.M., Brunberg, J.A., Mosca, R.S., Bove, E.L., Schork, M.A., Stetz, S.P.,
Cheatham, J.P., & Kulik, T.J. (2000). Neurodevelopmental outcome of patients after the
fontan operation: A comparison between children with hypoplastic left heart syndrome and
other functional single ventricle lesions. Journal of Pediatrics, 137, 645-652.
Hager, A., & Hess, J. (2005). Comparison of health related quality of life with cardiopulmonary
exercise testing in adolescents and adults with congenital heart disease. Heart, 91, 517-520.
Hoehn-Saric, R., McLeod, D.R., Funderburk, F., & Kowalski, P. (2004). Somatic symptoms and
physiologic responses in generalized anxiety disorder and panic disorder: an ambulatory
monitor study. Archives of General Psychiatry, 61, 913-921.
Hölz R., Kleinböhl, D., & Huse, E. (2005). Implicit operant learning of pain sensitization. Pain, 115,
12-20.
Lim, S.L., & Kim, J.H. (2005). Cognitive processing of emotional information in depression, panic,
and somatoform disorder. Journal of Abnormal Psychology, 114, 50-61.
Lundh, L.G., Wikström, J., Westerlund, J., & Öst, L.G. (1999). Preattentive bias for emotional
information in panic disorder with agoraphobia. Journal of Abnormal Psychology, 108,
222-232.
Mathews, A., & MacLeod, C. (1994). Cognitive approaches to emotion and emotional disorders.
Annual Review of Psychology, 45, 25-50.
Mathews, A., & Mackintosh, B. (2000). Induced emotional interpretation bias and anxiety. Journal
of Abnormal Psychology, 109, 602-615.
Mayou, R., Sprigings, D., & Gilbert T. (1999). Patients with palpitations referred for 24-hour ecg
recording. Journal of Psychosomatic Research, 46, 491-496
Mayou, R., Bryant, B., Forfar, C., & Clark, (1994). Non-cardiac chest pain and benign palpitations
in the cardiac clinic. British Heart journal, 72, 548-553.
Mayou, R.A., Bryant, B.M., Sanders, D., Bass, C., Klimes, I., & Forfar, C. (1997). A controlled trial of
cognitive behavioural therapy for non-cardiac chest pain. Psychological Medicine, 27,
1021-1031.
Mayou, R., Sprigings, D., Birkhead, J., & Price, J. (2002). A randomized controlled trial of a brief
educational and psychological intervention for patients presenting to a cardiac clinic with
palpitations. Psychological Medicine, 32, 699-706.
O’Brien, W.H., Reid, G.J., & Jones, K.R. (1998). Differences in heartbeat awareness among males
with higher and lower levels of systolic blood pressure. International Journal of
Psychophysiology, 29, 53-63.
Pennebaker, J.W. (1982). The psychology of physical symptoms. New York: Springer-Verlag.
Put, C., Van den Bergh, O., Van Ongeval, E., De Peuter S., Demedts, M., & Verleden, G., (2004).
Negative affectivity and the influence of suggestion on asthma symptoms. Journal of
Psychosomatic Research, 57, 249-255.
122 Chapter 7
Rietveld, S., & Houtveen, J.H. (2004). Acquired sensitivity to relevant physiological activity in
patients with chronic health problems. Behaviour Research and Therapy, 42, 137-153.
Rhodes, J., Curran, T.J., Camil, L., Rabideau, N., Fulton, D.R., Gauthier, N.S., Gauvreau, K., &
Jenkins, K.J. (2005). Impact of cardiac rehabilitation on the exercise function of children
with serious congenital heart disease. Pediatrics, 116, 1339-1345.
Ristvedt, S.L., & Trinkaus, K.M. (2005). Psychological factors related to delay in consultation for
cancer symptoms. Psychooncology, 14, 339-350.
Rozniatowski, O., Reich, M., Mallet, Y., Penel, N., Fournier, C., & Lefebvre, J.L. (2005).
Psychosocial factors involved in delayed consultation by patients with head and neck
cancer. Head and Neck, 27, 274-280.
Rusting, C.L. (1998). Personality, mood, and cognitive processing of emotional information: three
conceptual frameworks. Psychological Bulletin, 124, 165-196.
Rusting C.L. (1999). Interactive effects of personality and mood on emotion-congruent memory
and judgement. Journal of Personality and Social Psychology, 77, 1073-1986.
Ryan, C.M., Dulay, D., Suprasongsin, C., & Becker, D.J. (2002). Detection of symptoms by
adolescents and young adults with type 1 diabetes during experimental induction of mild
hypoglycaemia. Diabetes Care, 25, 852-858.
Salkovskis, P.M., & Warwick, H.M. (1986). Morbid preoccupations, health anxiety and reassurance:
a cognitive-behavioural approach to hypochondriasis. Behaviour Research and Therapy,
24, 597-602
Schandry, R., & Weitkunat, R. (1990). Enhancement of heartbeat-related brain potentials through
cardiac awareness training. International Journal of Neuroscience, 53, 243-253.
Spielberger, C.D., Gorsuch, R., & Lusheve, R. (1970). STAI Manual for the State-Trait Anxiety
Inventory. Palo Alto, CA: Consulting Psychologists Press.
Swanson, H.L., & Sachse-Lee, C. (2000). A Meta-Analysis of single-subject-design intervention
research for students with LD. Journal of Learning Disabilities, 33, 114-136.
Swillen, A., Feys, H., Adriaens, T., Nelissen, L., Mertens L., Gewillig, M., Devriendt, K., & Fryns,
J.P. (2005). Early motor development in young children with 22q.11 deletion syndrome
and a conotruncal heart defect. Development Medicine and Child Neurology, 47, 797-802.
Swinson, R.P., Soulios, C., Cox, B.J., & Kuch, K. (1992). Brief treatment of emergency room patients
with panic attacks. American Journal of Psychiatry, 149, 944-947.
Thaulow, E., & Fredriksen, P.M. (2004). Exercise and training in adults with congenital heart
disease. International Journal of Cardiology, 97, 35-38.Therrien, J., Fredriksen, P.,
Walker, M., Granton, J., Reid, G.J., & Webb, G. (2003). A pilot study of exercise training in
adult patients with repaired tetralogy of Fallot. Canadian Journal of Cardiology, 19, 685689.
Utens, E.M.W.J., Verhulst, F.C., Erdman, R.A.M., Meijboom, F.J., Duivenvoorden, H.J., Bos, E.,
Roelandt, J.R., & Hess, J. (1994). Psychosocial functioning of young adults after surgical
correction for congenital heart disease in childhood; a follow-up study. Journal of
Psychosomatic Research, 38, 745-758.
Discussion 123
Van den Bergh, O., Stegen, K., & Van de Woestijne, K.P. (1997). Psychosomatic Medicine, 59, 1323.
Visconti, K.J., Bichell, D.P., Jonas, R.A., Newburger, J.W., & Bellinger, D.C. (1999). Developmental
outcome after surgical versus interventional closure of secundum atrial septal defect in
children. Circulation, 100, II-145-II-150.
Walker, E.F., Sabuwalla, Z., & Huot, R. (2004). Pubertal neuromaturation, stress sensitivity, and
psychopathology. Developmental Psychopathology, 16, 807-824.
Walsh, J.C., Lynch, M., Murphy, A.W., & Daly, K. (2004). Factors influencing the decision to seek
treatment for symptoms of acute myocardial infarction: an evaluation of the SelfRegulatory Model of illness behaviour. Journal of Psychosomatic Research, 56, 67-73.
Watson, D., & Pennebaker J.W. (1989). Health complaints, stress and distress: exploring the
central role of negative affectivity. Psychological Review, 96, 234-254.
Windmann, S., Schonecke, O.W., Frohlig, G., & Maldener, G. (1999). Dissociating beliefs about
heart rates and actual heart rates in patients with cardiac pacemakers. Psychophysiology,
36, 339-342.
Yingling, K.W., Wulsin, L.R., Arnold, L.M., & Rouan, G.W. (1993). Estimated prevalences of panic
disorder and depression among consecutive patients seen in an emergency department
with acute chest pain. Journal of General International Medicine, 8, 231-235.
Zvolensky M.J., Kotov R., Antipova A.V., & Schmidt N.B. (2005). Diathesis stress model for panicrelated distress: a test in a Russian epidemiological sample. Behaviour Research and
Therapy, 43, 521-532.
124 Nederlandse samenvatting
Nederlandse samenvatting (Summary in Dutch)
Selectieve waarneming van hartsymptomen door patiënten
met een aangeboren hartafwijking
De term congenitale hartafwijking (ConHD) verwijst naar een breed spectrum van
hartafwijkingen die bij de geboorte aanwezig zijn. Geschat wordt dat 1% van de baby’s met
één of andere vorm van ConHD geboren wordt. Door vooruitgang in de behandeling van
ConHD, zijn de overlevingskansen van patiënten de laatste decennia enorm verbeterd.
Tegenwoordig bereikt meer dan 85% van de kinderen met een ernstige ConHD het eerste
levensjaar, dit in vergelijking tot 20% in de jaren '40. Als gevolg van deze ontwikkelingen
is een relatief nieuwe groep ontstaan van volwassenen met ConHD. Deze nieuwe groep
brengt ook nieuwe vragen met zich mee zoals: wat zijn de lange termijn effecten van
ConHD op het psychologisch en cognitief functioneren en waar dient eventuele
psychologische hulp zich op te richten bij volwassenen met ConHD?
De afgelopen 15 jaar hebben onderzoekers zich gericht op de vraag of ConHD
negatieve gevolgen heeft voor de kwaliteit van leven en psychologische ontwikkeling. De
bevindingen van deze onderzoeken tonen aan dat volwassenen met een aangeboren
hartafwijking meer psychopathologie en een verminderde kwaliteit van leven rapporteren
vooral met betrekking tot algemene gezondheid en fysiek functioneren. Onduidelijk is
echter welke mechanismen ten grondslag liggen aan het schadelijke effect van ConHD.
Verschillende hypothesen zijn geformuleerd met betrekking tot deze mechanismen,
namelijk (1) de somatische hypothese, (2) de symptoomperceptie hypothese en (3) de
kwetsbaarheid-stress hypothese.
Bij de somatische hypothese wordt ervan uitgegaan dat er een één-op-één relatie is
tussen een lichamelijke ziekte en waargenomen lichamelijke klachten. Zo wordt er
verondersteld dat hartritme stoornissen of verminderd zuurstof in het bloed direct leidt
tot de waarneming van lichamelijke klachten, zoals hartkloppingen en ademnood. Tevens
wordt aangenomen dat als gevolg van deze klachten lichamelijke activiteiten worden
vermeden, wat weer resulteert in een verminderde kwaliteit van leven en ontwikkeling van
psychopathologie. Om deze hypothese te toetsen hebben onderzoekers bekeken of de ernst
van de hartafwijking gerelateerd is aan gerapporteerde hartklachten, kwaliteit van leven
en psychopathologie. Deze onderzoeken geven echter onvoldoende bewijs voor de
somatische hypothese. Enerzijds omdat de relatie tussen ernst van de ziekte en kwaliteit
van leven vaak niet wordt gevonden. Anderzijds omdat onderzoeken die wel een relatie
rapporteren een aantal methodologische beperkingen hebben. Hierdoor kunnen
Nederlandse samenvatting 125
alternatieve verklaringen, die haaks staan op de somatische hypothese, niet worden
uitgesloten. Dit wijst erop dat er mogelijk modererende en medierende factoren zijn die de
relatie beïnvloeden tussen enerzijds de aanwezigheid van een ernstige aangeboren
hartafwijking en anderzijds het psychologisch functioneren. Dit heeft geleid tot de
formulering van de symptoomperceptie hypothese.
De symptoomperceptie hypothese gaat ervan uit dat mensen met chronische ziekte
worden blootgesteld aan verschillende leerervaringen met hun ziekte. Een dergelijke
leerervaring is bijvoorbeeld last krijgen van pijn op de borst tijdens fysieke inspanning. Als
gevolg van deze ervaringen ontwikkelen patiënten bepaalde ideeën en opvattingen over
hun ziekte. Deze opvattingen worden in het geheugen vastgelegd in de vorm van
associatieve netwerken ook wel ziekteschema’s genoemd. Een dergelijk schema bestaat uit
associaties tussen symptomen en ziektegerelateerde stimuli zoals sport, ziekenhuis, arts en
angst. De waarneming van ziektegerelateerde stimuli kan een ziekteschema activeren en
kan vervolgens leiden tot waarneming van lichamelijke klachten. Deze toename in
klachten kan worden verklaard door selectieve waarneming. Bij selectieve waarneming
richten patiënten selectief hun aandacht op sensaties die met de ziekte samenhangen.
Tevens interpreteren zij vage en ambigue lichamelijke sensaties als symptomen van hun
ziekte. Een patiënt die bijvoorbeeld in het verleden last heeft gehad van pijn op de borst
tijdens inspanning, zal bij een volgende inspanning opnieuw pijn op de borst ervaren
zonder dat hier direct een organische oorzaak voor hoeft te zijn. Hoewel deze hypothese
meer duidelijkheid verschaft over het ontstaan of aanhouden van onverklaarde
lichamelijke klachten, biedt de hypothese geen afdoende verklaring voor de verminderde
kwaliteit van leven bij patiënten met ConHD. Volgens de symptoomperceptie hypothese
zouden namelijk alle patiënten met ConHD een ziekteschema ontwikkelen, omdat elke
patiënt op enigerlei wijze wordt blootgesteld aan leerervaringen met zijn of haar ziekte. Dit
blijkt echter geenszins het geval te zijn. Uit onderzoek blijkt dat een aangeboren
hartafwijking niet bij alle patiënten negatieve gevolgen heeft voor het psychologisch
functioneren. Dit heeft geleid tot de formulering van de kwetsbaarheid-stress hypothese.
Volgens deze hypothese leidt een potentieel stressvolle gebeurtenis, zoals het hebben van
een ziekte, alleen tot een verminderde kwaliteit van leven en verhoogde psychopathologie,
als mensen een kwetsbare persoonlijkheid hebben, zoals een angstig temperament.
In een poging de symptoomperceptie hypothese en de kwetsbaarheid-stress
hypothese te integreren werd in het huidige onderzoek verondersteld dat alleen patiënten
met ConHD en een angstige aanleg selectieve waarneming van hartgerelateerde klachten
ontwikkelen en als gevolg daarvan een verminderde kwaliteit van leven. Onderzocht werd
(1) of ConHD een negatieve invloed heeft op het cognitief en psychologisch functioneren
van kinderen en adolescenten, (2) of patiënten met ConHD die tevens een angstige aanleg
126 Nederlandse samenvatting
hebben hartklachten selectief waarnemen, en (3) of selectieve waarneming van
hartklachten bij hoog angstige patiënten met ConHD is gerelateerd aan een verminderde
kwaliteit van leven. Om deze vraagstellingen te onderzoeken zijn een meta-analyse en vier
experimenten uitgevoerd.
In hoofdstuk 2 wordt een meta-analyse beschreven waarin is onderzocht of een
aangeboren hartafwijking negatieve gevolgen heeft voor het psychologisch en cognitief
functioneren van kinderen en adolescenten. Uit de analyse bleek dat de verschillende
studies een grote variatie vertonen in de mate waarin ConHD het psychologisch en
cognitief functioneren beïnvloedt. Dit wees op belangrijke modererende factoren die het
schadelijke effect van ConHD op het psychologisch en cognitief functioneren beïnvloeden.
Zo bleek er een relatie te zijn tussen de ernst van de hartafwijking en cognitief
functioneren. Alleen patiënten met een ernstige hartafwijking, zoals hypoplastisch linker
hart syndroom en transpositie van de grote vaten hadden een verminderd cognitief
functioneren vergeleken met de norm, vooral wat betreft visueel-ruimtelijke vaardigheden
(performale intelligentie). Tevens werd een relatie gevonden tussen de leeftijd van de
hartpatiënten en psychopathologie. Vooral de oudere kinderen (jonge adolescenten)
vertoonden meer internaliserende gedragsproblemen (bijvoorbeeld angst en depressie) in
vergelijking met een controle groep. Bovendien was de ernst van de hartafwijking niet
gerelateerd aan psychopathologie. Deze bevindingen suggereren dat een ernstige
hartziekte schadelijke gevolgen heeft voor het cognitief functioneren. Een hartziekte heeft
echter niet per definitie schadelijke gevolgen voor het psychologisch functioneren. Alleen
oudere kinderen vertonen namelijk gedragsproblemen en de ernst van de hartafwijking is
niet gerelateerd aan het psychologisch functioneren.
Omdat alleen adolescenten gedragsproblemen vertonen, lijkt het er veeleer op dat
de combinatie van een hartziekte met bepaalde risico factoren leidt tot internaliserende
gedragsproblemen. Een risico factor voor internaliserende problemen zou mogelijkerwijs
een angstige persoonlijkheid kunnen zijn. Het is bijvoorbeeld denkbaar dat genetische
kwetsbaarheden, zoals onder andere een angstige aanleg, tot uiting komen in de pubertijd
als gevolg van hormonale veranderingen. Deze genetische kwetsbaarheden kunnen
vervolgens
de
ontwikkeling
van
psychopathologie
beïnvloeden,
waardoor
gedragsproblemen ontstaan bij adolescenten met ConHD. Om de invloed van angst als
persoonlijkheidstrek op het psychologisch functioneren van hartpatiënten verder te
onderzoeken zijn een viertal experimenten uitgevoerd die zijn beschreven in de
hoofdstukken 3 tot en met 6. In deze experimenten wordt bekeken of angstige patiënten
met ConHD hartklachten selectief waarnemen en een verminderde kwaliteit van leven
ervaren.
Nederlandse samenvatting 127
In hoofdstuk 3 wordt een onderzoek beschreven waarin is getoetst of onschuldige
hartgerelateerde stimuli (valse hartslag feedback) een toename in de waarneming van
hartklachten veroorzaken bij patiënten met ConHD en een angstige persoonlijkheid.
Patiënten met ConHD en gezonde mensen kregen achtereenvolgens twee inspanningstests
op een lopende band. Tijdens een van deze tests kregen zij valse feedback van hun hartslag
te horen. Deze feedback representeerde ofwel een regelmatige hartslag ofwel een
onregelmatige hartslag, en was niet gebaseerd op de daadwerkelijke hartslag van de
proefpersoon. Tijdens beide inspanningstaken werden drie hartklachten gemeten, te
weten: hartkloppingen, versnelde hartslag en pijn op de borst. Gedurende het hele
experiment werd de hartslag, ademhalingsfrequentie en partiële CO2 druk aan het eind
van elke ademhaling geregistreerd, om uit te sluiten dat een eventuele toename van
hartklachten bij hartpatiënten verklaard kon worden door acuut disfunctioneren van het
hart. Volgens de verwachtingen bleken patiënten met ConHD, die tevens een angstige
aanleg hadden, meer hartklachten te rapporteren na de valse feedback. Deze toename in
hartklachten kon niet verklaard worden door fysiologische verschillen tussen patiënten
met ConHD en gezonde individuen. Echter, tegen de verwachtingen in lieten
hartpatiënten met een angstige aanleg de toename in hartklachten niet direct na de valse
feedback zien, maar in een daarop volgende inspanningstest zonder valse feedback.
Tevens bleek dat er geen onderscheid gemaakt kon worden tussen het effect van de
regelmatige en de onregelmatige hartslag feedback. Deze bevindingen suggereren dat
patiënten met ConHD die tevens angstig zijn, meer hartklachten rapporteren in de
aanwezigheid van onschuldige hartgerelateerde stimuli in de omgeving.
In hoofdstuk 4 wordt een onderzoek beschreven waarin is getoetst of patiënten
met ConHD en een angstige persoonlijkheid geneigd zijn meer hartklachten te
rapporteren ten tijde van acute stress. Tevens werd onderzocht of hartpatiënten specifiek
meer hartklachten rapporteren in plaats van meer klachten in het algemeen. Patiënten
met ConHD en gezonde mensen kregen een stressvolle intelligentietest op een computer.
Voor en na de intelligentietest, respectievelijk de baseline en herstel periode, kregen zij
een rustgevende film te zien. Tijdens baseline, herstel en tijdens stress werden vijf
symptomen gemeten die geassocieerd worden met hartziekte (hartkloppingen, versnelde
hartslag, kortademigheid, duizeligheid, pijn op de borst) en vijf symptomen die niet
geassocieerd worden met hartziekte (loopneus, buikpijn, suizende oren, jeuk en waterige
ogen). Tevens werd het functioneren van het hart gedurende het gehele experiment
gemeten door registratie van de hartslag, bloeddruk, ademhalingsfrequentie en partiële
CO2 druk aan het eind van elke uitademing. In overeenstemming met de verwachtingen,
bleken hartpatiënten met een angstige persoonlijkheid tijdens stress meer hartklachten te
rapporteren dan algemene klachten. Tevens bleek dat deze toename in hartklachten niet
128 Nederlandse samenvatting
verklaard kon worden door verschillen in hartfunctioneren op dat moment tussen
hartpatiënten en gezonde individuen. Deze resultaten bevestigen de hypothese dat
hartpatiënten met een angstige aanleg, door een combinatie van leerervaringen met de
ziekte en een angstig temperament, ten tijde van stress geneigd zijn hartklachten waar te
nemen die niet direct verklaard kunnen worden door acuut disfunctioneren van het hart.
In de hoofdstukken 3 en 4 zijn de ziektegerelateerde stimuli, stress en valse
hartslag feedback, zodanig aangeboden dat de patiënten de stimuli op een bewust niveau
konden verwerken. Onduidelijk blijft nog in hoeverre ziektegerelateerde stimuli die niet op
bewust niveau verwerkt kunnen worden selectieve waarnemingen teweeg brengen bij
hartpatiënten met een angstige persoonlijkheid. Als dat zo is, dan zou dat betekenen dat
selectieve waarneming van hartklachten gemakkelijk en snel uitgelokt kan worden zonder
dat de patiënt weet wat de uitlokkende stimuli zijn. In hoofdstuk 5 wordt een onderzoek
beschreven waarin deze hypothese is onderzocht. Verwacht werd dat subliminaal (buiten
het bewustzijn) aangeboden ziektegerelateerde stimuli selectieve waarneming van
hartsensaties teweeg zouden brengen bij hartpatiënten met een angstige aanleg. Patiënten
met ConHD en gezonde mensen kregen een luidspreker op de borst bevestigd die alleen
lage tonen voortbracht die voelbaar waren en niet hoorbaar. Via deze luispreker werden
twee soorten lichamelijke sensaties opgewekt: een hartslag en een neutrale sensatie,
bestaande uit een constante trilling. Voorafgaand aan deze sensaties werd heel kort (10
ms), buiten het bewustzijn van de proefpersoon, een woord gepresenteerd op een
computerscherm, bestaande uit ofwel het woord “hart” ofwel een neutraal woord “zoem.”
Proefpersonen werden gevraagd de sensaties op de borst zo snel mogelijk te categoriseren
als zijnde een hart of neutrale stimulus. Een vertraging in de categorisatie van de
hartsensaties betekende selectieve waarneming van hartsensaties. In overeenstemming
met de verwachtingen bleek dat hartpatiënten met een angstige aanleg hartsensaties, die
voorafgegaan werden door het woordje “hart,” trager categoriseerden. Deze resultaten
suggereren dat ook hartstimuli die niet bewust worden waargenomen een selectieve
waarneming kunnen oproepen bij hartpatiënten met een angstige persoonlijkheid.
In hoofdstuk 6 wordt een onderzoek beschreven waarin is getoetst of selectieve
waarneming van hartklachten in patiënten met ConHD en een angstige aanleg
geassocieerd is met een verminderde kwaliteit van leven. Verwacht werd dat patiënten met
ConHD en een angstige aanleg hartsensaties negatief interpreteren. Tevens werd verwacht
dat patiënten die hartsensaties negatief interpreteren vervolgens een verminderde
kwaliteit van leven ervaren op het gebied van dagelijkse activiteiten en fysiek
functioneren. Tevens werd verwacht dat patiënten met ConHD en een angstige aanleg
hartsensaties negatief interpreteren als zij ook hoog angstig zijn op dat moment
(toestandsangst). Proefpersonen kregen een vignet waarin een persoon beschreven stond
Nederlandse samenvatting 129
die verschillende ambigue sensaties waarnam die normaliter geassocieerd worden met
hartziekte. Proefpersonen werden gevraagd de ambigue sensaties te interpreteren. Een
negatieve interpretatie van de sensaties werd gekenmerkt door een tendens de sensaties
als ernstiger te beoordelen, de persoon minder verantwoordelijkheid toe te schrijven voor
het ontstaan en instandhouden van de sensaties en de sensaties als minder controleerbaar
en veranderbaar te beoordelen. Conform de verwachtingen bleek dat de relatie tussen een
angstige persoonlijkheid en dagelijks functioneren alleen bij patiënten met ConHD
gemedieerd werd door negatieve interpretaties van hartsensaties. Tevens bleek
toestandsangst de relatie tussen een angstige persoonlijkheid en negatieve interpretaties
van sensaties te medieren. Tegen de verwachtingen in bleek de relatie tussen een angstige
persoonlijkheid en fysiek functioneren niet gemedieerd te worden door negatieve
interpretaties van hartsensaties. Fysiek functioneren bleek, echter, wel marginaal
gerelateerd te zijn aan de ernst van de hartafwijking. Deze resultaten wijzen erop dat een
angstige aanleg bij patiënten met ConHD, hoge toestandsangst en negatieve interpretaties
van hartsensaties induceert en vervolgens een verminderd dagelijkse functioneren. Fysiek
functioneren, daarentegen, lijkt veeleer af te hangen van de ernst van de hartafwijking.
In de algemene discussie wordt ingegaan op de implicaties van de bevindingen
voor de klinische praktijk. Allereerst wordt het belang aangegeven van screening van
kinderen en adolescenten met ConHD op gedragsproblemen en problemen in de
cognitieve ontwikkeling. Tevens wordt aanbevolen om patiënten door te verwijzen voor
een psychologische behandeling als zij last hebben van hartklachten die niet verklaard
kunnen worden door acute hartproblemen. Een dergelijke behandeling zou gericht
kunnen zijn op de volgende doelen: 1) het herkennen van interne en externe stimuli die
selectieve waarneming van hartklachten uitlokken; 2) het corrigeren van negatieve
interpretaties van onschuldige hartsensaties; 3) het stimuleren van lichamelijke
activiteiten en 4) het signaleren van acute hartproblemen. Tevens worden voorstellen
gedaan voor toekomstig onderzoek. Om te bepalen of selectieve waarneming ook gunstige
effecten kan hebben, zoals het op tijd herkennen van acute hartproblemen, is onderzoek
nodig naar de accuratesse waarmee patiënten met ConHD en een angstige aanleg
hartproblemen waarnemen. Ook is het relevant de factoren te onderzoeken die van
invloed zijn op dagelijkse activiteiten en fysiek functioneren van patiënten met ConHD.
Hoewel in het huidige onderzoek al enigszins is ingegaan op deze vraag, is meer onderzoek
op dit gebied wenselijk. Zo zouden onderzoekers in een vervolgonderzoek negatieve
interpretaties van hartsensaties experimenteel kunnen manipuleren en fysieke prestaties
objectief kunnen meten. Om meer inzicht te verkrijgen in welke factoren bijdragen aan
een verminderde kwaliteit van leven bij patiënten met ConHD is ook onderzoek wenselijk
naar het schadelijke effect van specifieke gebeurtenissen, zoals een hartritmestoornis of
130 Nederlandse samenvatting
openhartoperatie. Ander onderzoek zou gericht kunnen worden op de vraag hoe vaak
patiënten met ConHD het ziekenhuis of de huisarts bezoeken. Idealiter wordt overmatig
gebruik van de medische zorg gereduceerd. Hiertoe is meer kennis nodig over de factoren
die bepalend zijn voor een patiënt om hulp te zoeken voor hartklachten die al of niet
verklaard kunnen worden door een onderliggend hartprobleem. Tot slot is onderzoek
geboden naar de effectiviteit van psychologische behandeling gericht op het verbeteren
van de kwaliteit van leven van patiënten met ConHD.
Samenvattend kan gesteld worden dat een ernstige aangeboren hartafwijking
negatieve gevolgen lijkt te hebben voor het cognitief functioneren van patiënten. Een
aangeboren hartafwijking in combinatie met blootstelling aan bepaalde risico factoren lijkt
tot een verhoogde kans op gedragsproblemen te leiden bij adolescenten, zoals angst en
depressie. Tot slot kan gesteld worden dat een angstige persoonlijkheid een
kwetsbaarheidfactor is voor patiënten met ConHD. De combinatie van een angstige aanleg
en leerervaringen met een chronische ziekte zoals ConHD blijkt te resulteren in selectieve
waarneming van hartklachten en uiteindelijk in een verminderde kwaliteit van leven. Deze
bevindingen vormen de basis voor de ontwikkeling van therapeutische interventies die
gericht zijn op verbetering van de kwaliteit van leven van patiënten met ConHD.
132 Dankwoord
Dankwoord (Acknowledgements)
Graag wil ik van de gelegenheid gebruik maken alle mensen te bedanken die ieder op hun
eigen wijze hebben bijgedragen aan de totstandkoming van dit proefschrift. Allereerst gaat
mijn dank uit naar mijn promotores Merel Kindt en Barbara Mulder en mijn co-promotor
Walter Everaerd. Merel, ik ben blij dat jij halverwege mijn promotieproject promotor
wilde zijn. Het moet voor jou niet gemakkelijk zijn geweest om een project binnen te
stappen waar de onderzoeken al grotendeels waren uitgevoerd. Jouw komst was voor mij
een zeer positieve ervaring. Onze constructieve discussies, je helderheid en je nieuwe
perspectief op het onderzoek zijn voor mij zeer leerzaam en motiverend geweest. Je
humoristische en positieve houding (nog bedankt voor de lekkere chocolaatjes), je
inlevingsvermogen en je sterke relativeringsvermogen (je krijgt een paar moeilijke vragen
tijdens je promotie maar meer is het ook niet) hebben voor mij stressreducerend gewerkt
en maakten dat ik met plezier mijn proefschrift heb kunnen afronden.
Barbara, jij bent een van de initiatiefneemsters geweest van het project en bent tot
het einde betrokken gebleven. Jarenlang heb ik met groepjes studenten op de cardiologie
afdeling rondgelopen om tijdens spreekuren patiënten te werven voor het onderzoek.
Bedankt voor al je hulp bij de werving. Ik hoop dat de rust inmiddels weer is wedergekeerd
op de afdeling cardiologie. Tevens wil ik je bedanken voor de constructieve feedback op de
manuscripten.
Walter Everaerd, jij hebt opgetreden als mijn begeleider op tijden dat andere
begeleiding schaars was. Ik waardeer je rust en betrouwbaarheid zeer. Je meer
neuropsychologische kijk op symptoomperceptie, iets waar ik tot dan toe niet erg in thuis
was, hebben me geholpen mijn kennis te verbreden. Ook dank voor de feedback op de
manuscripten. Ik vind het bewonderingwaardig hoe jij met weinig woorden toch de vinger
op de zere plek kan leggen.
Simon Rietveld, jij bent de bedenker geweest van het onderzoeksproject. Wat mij
bij zal blijven is je enthousiasme voor het doen van onderzoek. Ik heb veel geleerd van de
wijze waarop jij experimenten bedacht. Jij streefde ernaar om in het lab op subtiele wijze
een situatie in het dagelijkse leven na te bootsen. ‘Context’ was hierbij het toverwoord.
Soms leek je net een toneelspeler in een spannend toneelstuk.
Dit proefschrift had nooit geschreven kunnen worden zonder de bereidwilligheid
van mensen met een aangeboren hartafwijking om deel te nemen aan het onderzoek. Het
is niet mis wat jullie hebben moeten doorstaan tijdens de experimenten, zoals
verontrustende hartgeluiden of een onbegrijpelijk intelligentie test in de aanwezigheid van
een zeer kritische beoordelaar. Ik wil jullie bedanken dat jullie dit allemaal hebben willen
ondergaan. Ook wil ik studenten psychologie bedanken voor de hulp die ze mij geboden
Dankwoord 133
hebben bij het uitvoeren van de onderzoeken. In het bijzonder wil ik de studenten
bedanken die betrokken waren bij het valse feedback onderzoek, een van de lastigste
experimenten van dit proefschrift: Sachlan Apil (ook alweer een tijd promovendus in
Leiden), Sophie van Zeyl, Tim Ziermans, Beate Lauxterman, Greetje Carlier en Simone
van Geel. Ook Sanne Marcelis, Esther Winnubst en Tim Veassen wil ik bedanken voor het
zeer efficiënt en effectief uitvoeren van de onderzoeken naar respectievelijk de invloed van
stress en subliminale hartstimuli.
De mensen bij methodologie wil ik bedanken voor hun statistische adviezen. In het
bijzonder wil ik Conor Dolan bedanken. Dankzij jou heb ik een padanalyse kunnen
uitvoeren. Ik waardeer het enorm dat je zoveel tijd hebt vrij gemaakt om mijn vragen te
beantwoorden. Een bezoek aan jou was iedere keer weer een avontuur. Pieter Koele, dank
voor de snelle reacties op al mijn e-mails (overigens in Maastricht begint iedereen z’n mail
met “Hallo”). Harrie Vorst, wil ik bedanken voor het op weg helpen van de meta-analyse
en Ger Hanewald voor de statistische hulp in de begin jaren van mijn aio-tijd (en
natuurlijk ook voor de gezellige borrels tot diep in de nacht!)
Bert Molenkamp, de held van de systeemgroep, wil ik bedanken voor de snelle hulp
in het lab bij crashende computers, niet werkende knoppenkastjes en onverklaarbare ruis
op het ECG. Erg knap ook, Bert, dat je in elke situatie positief bleef en erop vertrouwde dat
er altijd wel een oplossing voor het probleem te vinden was (meestal een stekkertje dat
niet in het apparaat zat). Nico Notenbaart, onze geluidsexpert, wil ik bedanken voor de
hartgeluiden en de aanschaf van de basluidspreker. Dit heeft mij gestimuleerd om toch de
valse hartslag feedback via een luidspreker op de borst aan te bieden.
De artsen, Gijs Nollen en Thomas Oosterhof, wil ik bedanken voor de vele uren die
zij in het lab hebben doorgebracht om de ECG’s van de patiënten na te lopen en om hulp te
bieden bij acute hartprobleem. Kiki Hohnen en Eline Tuijn wil ik bedanken voor het
checken van het Engels van delen van mijn proefschrift.
Mijn Kamergenoten op 820, Saskia van Oord, Arnold van Emmerik (jaja?, zie
proefschrift Arnold), Hilde Geurts en later Wieke de Vente en Janet de Jager wil ik
bedanken voor het uitwisselen van onze promotieperikelen en de laatste nieuwtjes van de
afdeling. De promovendi Marieke Effting, Sam Ghane, Leentje Vervoort, en Merel Krijn,
wil ik bedanken voor de gezellige lunches. Marieke, extra bedankt voor het
afscheidsetentje en Sam, bij nader inzien had ik toch graag een kompas willen hebben,
want ik ben toch een keer verdwaald in de bergen van Mongolië. Mark Spiering bedankt
voor je stimulans om onderzoeker te worden, voor de fijne werkstukbegeleiding tijdens
m’n studententijd en voor de gezellige gesprekken. Stephanie Both en Anda van Stegeren
bedankt voor de intellectuele stimulans tijdens de onderzoeksbijeenkomsten. De
feestcommissie van Klinische Psychologie, Herman Vinkers, Sandra Diets, Louise
134 Dankwoord
Beekman en Kitty Rolf, wil ik bedanken voor de gezelligheid rondom het organiseren van
borrels en het jaarlijkse dagje uit. Herman ook dank voor de mooie reisverhalen.
Guido Valk, Sharon Klinkers, Jean Louis van Gelder, Jessica van Sluijs, Sumit
Mehra, Odile Swagemakers en Kim de Jong wil ik bedanken voor de enorm fijne tijd die ik
heb gehad tijdens het onderzoekspracticum. Ik zal de gezellige uurtjes in Kriterion en de
weekendjes zeilen missen. Jan Doorn wil ik bedanken voor de mogelijkheid om
therapeutische ervaring op te doen in zijn praktijk. Met name de patiënten met een
hartziekte en paniekaanvallen waren voor mij heel leerzaam.
Anja van Greeven, mijn Haagse vriendin, bedankt voor al je gezelligheid en
meligheid bij ons onderzoeksclubje samen met Sonja en Marieke. Ik verheug me op meer
toekomstige etentjes, Maastrichtse bezoekjes en Thaise massages. Welmoet Merk, ook
Hagenees tegenwoordig, bedankt voor je fijne relativerende gesprekken over onderzoek en
het leven. Ik hoop je snel in je nieuwe woonplaats te bezoeken.
Ook wil ik de mensen van de woensdagavond, 3voor12, bedanken: Floris Müller,
Martijn Mertens, Najiba Brakee, Jennie van Beek en Naomi (inmiddels Castelein-)
Nettinga. Jullie zorgden voor mijn wekelijkse ontspanning, relativering en slaaptekort.
3voor12 gaf mij een ‘boost’ om het een en ander af te ronden. Een groot deel van de
discussies in dit proefschrift zijn dan ook geschreven op de donderdagen na 3voor12.
Mijn twee paranimfen Marieke Brauer en Sonja van Well wil ik bedanken voor de
hechte band die we de afgelopen jaren samen hebben gehad. Marieke sinds het
onderzoekspracticum van onze studie psychologie zijn onze wegen onafscheidelijk
gebleven (in januari 2007 alweer ons 10 jarig jubileum!). Samen hebben we ons
afstudeeronderzoek gedaan en samen zijn we aan een promotietraject begonnen gericht
op lichamelijke symptomen (jij dan wel in Leiden). Bedankt voor al je lieve steun en ik
hoop nog veel leuke dingen samen met jou te ondernemen. Sonja jou heb ik leren kennen
tijdens m’n aio-tijd op de UvA. In mijn herinnering was je vanaf dag 1 m’n beste maatje. Er
is niemand met wie ik zo fijn over onderzoek kan praten. Ik zal onze wandelingetjes en
wekelijkse aerobic les enorm missen! (ik mis het nu al)
Verder wil ik mijn lieve ouders en zussen bedanken voor de onvoorwaardelijke
steun en belangstelling die zij mij hebben gegeven. Ik vind het knap hoe jullie ondanks alle
stress van de afgelopen jaren toch ruimte konden vinden om mij te supporten. Tamara,
ook bedankt voor de fantastische kaft die je hebt gemaakt en Nienke wat geweldig dat je
als fotomodel hebt willen optreden! Als laatste wil ik mijn allerliefste vriend Gertjan
bedanken voor al het begrip en geduld dat hij heeft opgebracht om mij aan dit proefschrift
te laten werken. Gertjan samen met jou kan ik alles wel aan, zelfs een promotie!