WHY DO THEY
KEEP COMING
BACK?
PERSISTENT FREQUENT ATTENDERS
IN PRIMARY CARE
COLOFON
This study was part of the perfactio group. This research on
frequent attenders was funded by grants from the Academic
Medical Center, University of Amsterdam, the Netherlands;
Stichting steunfonds medische en sociale dienstverlening,
Reigersbos (Foundation to support medical and social
services Reigersbos); and a grant from the Netherlands
Organization for Health Research and Development (ZonMw),
programma Alledaagse ziekten (common diseases;
nr 42011002).
Copyright 2014 Frans Smits. All rights reserved. No part of this
thesis may be reproduced or transmitted, in any form or by any
means, without the prior permission of the author.
ISBN:
Cover image:
Graphic design:
Printed by:
978-90-6464-808-3
Unknown photographer, waiting room
Laura Smits
GVO drukkers & vormgevers B.V,
www.proefschriften.nl
WHY DO THEY KEEP COMING BACK?
PERSISTENT FREQUENT ATTENDERS
IN PRIMARY CARE
ACADEMISCH PROEFSCHRIFT
ter verkrijging van de graad van doctor
aan de Universiteit van Amsterdam
op gezag van de Rector Magnificus
prof. dr. D.C. van den Boom
ten overstaan van een door het college voor promoties ingestelde
commissie, in het openbaar te verdedigen in de Agnietenkapel
op donderdag 18 september 2014, te 14.00 uur
door Franciscus Thomas Maria Smits
geboren te Breukelen
PROMOTIE COMMISSIE
Promotores:
Prof. Dr. H. C. van Weert
Prof. Dr. A.H. Schene
Co-promotores:
Dr. G. ter Riet
Dr. J. Bosmans
Overige leden:
Prof. Dr. J.C.J.M. de Haes
Prof. Dr. H.E. van der Horst
Prof. Dr. A.L.M. Lagro-Janssen
Prof. Dr M. Maas
Dr. H.G. Ruhé
Prof. dr. K. Stronks
Faculteit der Geneeskunde
“Wherever the art of Medicine is loved,
there is also a love of Humanity”
HIPPOCRATES
contents
Chapter 1: General introduction
008
PART I: MAPPING FREQUENT ATTENDERS IN PRIMARY CARE
020
Chapter 2: Defining frequent attendance in general practice
020
Chapter 3: Epidemiology of (persistent) frequent attenders A 3-y historic cohort study comparing attendance, morbidity
and prescriptions of one-year and persistent frequent attenders-
030
Chapter 4: Is persistent frequent attendance predictable?
A historic 3-year cohort study
044
Chapter 5: Predictability of persistent frequent attendance in
primary care: A temporal and geographical validation study
058
Chapter 6: Morbidity and doctor characteristics only partly
explain the substantial healthcare expenditures of frequent
attenders - A record linkage study between patient data and
reimbursements data -
076
PART II: REVIEW OF THE LITERATURE ABOUT
INTERVENTIONS ON FREQUENT ATTENDERS IN PRIMARY
CARE
Chapter 7: Interventions on frequent attenders in primary care.
A systematic literature review
6
092
092
PART III: A PROSPECTIVE STUDY OF FREQUENT ATTENDERS
106
Chapter 8: Why do they keep coming back? -Aetiology of
persistence of frequent attendance in primary care;
a prospective cohort study-
106
Chapter 9: Is treatment of psychiatric morbidity in frequent
attenders cost-effective in comparison with usual general
practitioner care? Results of a modelling study
130
Chapter 10: General discussion
152
Chapter 11: Appendices
164
Summary
178
Samenvatting
184
Dankwoord
190
Curriculum vitae
194
PhD portfolio
196
List of publications
198
7
general
introduction
Background and motivation for this study
Every General Practitioner (GP) will recognize the slight confusion when the
name of a patient that recently visited the practice several times, is again on the
daily schedule: “A new appointment again? Didn’t we reach a conclusion last time?
Did the complaints aggravate? Was the diagnosis and intervention (perceived as)
insufficient?” Sometimes you feel you have fallen a bit short, annoyed or unable
to think of a good explanation. And you may wonder whether there might be
something in this patient that you did not recognize and, consequently, did not
treat adequately, resulting in this repeated attendance. Patients who visit their GP
much more often than other patients in the practice are called Frequent Attenders
(FAs). In this thesis we describe (persistent) FAs and investigate factors leading to
(persistence of) frequent attendance, relations with the wellbeing of these patients,
treatment options for FAs and cost consequences.
Most patients only attend their GP frequently for a short period of time1-4 and only
20–30% of FAs continues to attend frequently in the following year.1-3 FAs not only
frequently attend their GP, but they are also more often referred to specialist care
than non-frequent attenders (non-FAs).5 The burden on primary and secondary care
of FAs is high. In the United Kingdom approximately 80% of a GP’s clinical work
is spent on 20% of his/her patients, and this often leads to care that is not effective
in helping the patient.6 Most short-term frequent attendance can adequately be
explained, for example by a temporary medical problem. However, when frequent
attendance spans more (consecutive) years both chronic physical and long-lasting
psychosocial problems are often present in this group of patients.7-11 Psychological
distress, low physical quality of life (QoL), and a low educational level are associated
8
WHY DO THEY KEEP COMING BACK?
with persistent frequent attending.9;12 Persistent frequent attendance may be
considered an easily detectable type of behavior, indicating underlying psychosocial
or psychiatric problems and low QoL, sometimes undetected and untreated.
Therefore, we concentrate this research on persistent frequent attendance. Because
somatic problems are already adequately addressed in everyday GP-care and
(chronic) care models, we more specifically focus on the role of psychological and
social factors in the aetiology of (persistence of) frequent attendance. We think this
approach might also contribute to the thoughtful design of preventive strategies for
persistence of frequent attendance.
Definition of (persistent) frequent attenders and how to select FAs in a normal
GP’s practice?
Several methods for selecting frequent attenders have been used until now.13;14 The
older the patient, the more frequently he or she will visit healthcare professionals
in primary and secondary care, just because of physical aging.15 Women of all
age groups make more use of healthcare than men.11;16 Consultation frequencies
differ between countries and, within countries, by GP.14 Just selecting the most
attending persons thus will lead to the selection of predominantly older females
and patients of a limited number of GP’s. Hence, it is more appropriate to select
the exceptional users within every age and sex group of a GP (practice).14 Such a
proportional threshold definition selects the exceptional users compared to their
peers and allows for meaningful comparison between individual practices, periods,
and countries.
Therefore, in this thesis we define FAs as those patients whose attendance rate
ranks in the top 10 centile per age and sex group in a GP-practice within a time
frame of one year, and persistent FAs as those patients who are FA during three
consecutive years. To calculate FAs we used all face-to-face consultations with
GPs (consultations in the surgery and house-calls) and the number of all enlisted
patients in a practice.
Selecting FAs by using age groups with a small range (for example a 10-year range)
is difficult and labour-intensive, especially in smaller populations like those of a
single practice. It may result in low numbers of patients in each age group. In the
UK, Howe advised using the following method to define FAs: group all men and
for women create two age groups and calculate the top 10% attenders in each of
these three groups.13 To establish which method would be most appropriate and
feasible to use in the Netherlands, we tested different methods of selecting FAs in
an average general (group) practice (Chapter 2).
CHAPTER 1
9
How to understand and interpret frequent attendance?
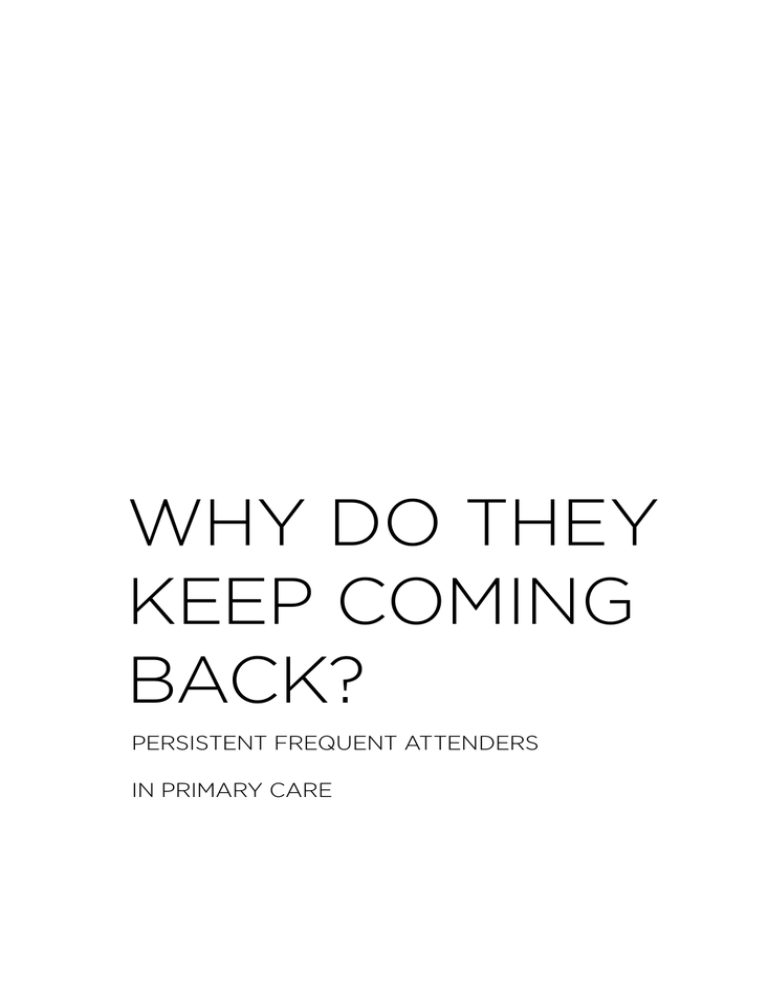
To structure our research we hypothesized that within the context of a given
western GP-centred primary healthcare system, attendance rates may be
influenced by patient characteristics (including morbidity), by GP characteristics
(like work style, experience, personality and professional interests), and thirdly by
the interpersonal dynamics between patients and their physicians (see figure 1).
We restrict our scope to healthcare systems with a well-organized primary care in
which GPs provide continuity of care for enlisted patients and act as gatekeepers to
specialist care.
Patient characteristics
Most studies describing patient characteristics concern short-term frequent
attenders. The decision whether to consult a GP seems to depend on the patient’s
past experience with healthcare, the perception of the symptoms, the perception of
the GP’s role as well as the relationship with the GP.17-20 Other reported factors are
health anxiety (balancing fears), passivity, lack of control or mastery and mental
health problems.20 One study found that FAs are often not aware of their frequent
attendance. The interviewed patients regarded the GP as an appropriate figure to
solve their distinctive and multiple physical symptoms and, despite their trust in
the GP, some dissatisfaction with the (not) given treatment remained.21
FAs with medically unexplained symptoms (MUS) seem to persist in frequent
attendance because of high health anxiety and concern about a missed diagnosis,
often despite some level of insight in their condition.19 In the attachment theory
cognitive schemas based on earlier repeated experiences with caregivers are
considered to influence how individuals perceive and act within interpersonal
relationships. The ‘insecure attachment style’ was shown to be associated with
frequent attendance after adjusting for socio-demographic characteristics, presence
of chronic physical illness and baseline physical function. The ‘preoccupied
attachment style’ was associated with high primary care costs and utilization.22;23
These associations were particularly strong for those patients who believed that
a physical problem caused their unexplained symptoms. High consultation rates
may be conceptualized as pathological care-seeking behaviour linked to insecure
attachment.23 Understanding frequent attendance as driven by difficulties in
relating to care giving figures may help doctors to manage their frequently
attending patients in a different way. Other authors observed that attendance rates
depend on early child experiences and that families tend to be consistent in illness
and consultation patterns over the years and even over the generations.17;18;24;25
10
WHY DO THEY KEEP COMING BACK?
Figure 1. Theoretical model of possible aetiological explanations of persistence of
Frequent attendance
Life events
Financial
circumstances;
educational level
Somatic problems
Demographic issues
(work, living circumstances)
Psychiatric Problems
(axis I)
Consultation
frequency of the
patient
Family; Ethnicity
Personality
(axis II)
Coping style
(mastery)
Communication between the patient
and the GP; Somatic fixation?
General practitioner
Age /Sex
Number of enlisted
patients
Habits in registering
problems in the EMD
Experience as a GP
Corrected number
of consultations per
patient
Special interests
CHAPTER 1
11
GP determinants
It seems plausible that GPs also play a role in the attendance frequency of their
patients. Physicians differ significantly in their clinical decision-making. The mean
consultation frequency, but also the number of lab tests and referrals to secondary
care vary considerably between GPs and practices.26;27 However, little is known
about the impact of GP specific determinants on the frequency of consultation and
on persistent frequent attendance in some patients.28
A qualitative study described the emotions and thoughts of physicians at primary
healthcare centers in Spain during consultations with short-term frequent
attenders.29 Positive emotions regarding FAs were associated with young age of
the physician and presence of the thought “This patient really needs me”. Feelings
of lack of control were associated with working in rural centres and with negative
thoughts about FAs. Anxious thoughts of the GP were associated with greater
workload, more requests for tests, more requests to see the doctor outside regular
hours, and negative thoughts about FAs. Guilt feelings were associated with a lower
perceived ability to solve the patient’s problem, and with a poor physician-patient
relationship. Sadness of the GP was associated with more frequent referrals to
specialists.29
Interaction between patient and GP
In the 1980s, some authors postulated that inadequate interpersonal dynamics
between patients and their GP could cause more inappropriate and unnecessary
consultations, testing and treatments, a phenomenon then labelled as “somatic
fixation”.30-32 They emphasized the importance of adequate communication skills
of the GP to break the chain of this fixation. However, literature describing the
interaction between FAs and the GP is scarce.29
(Medical) problems of frequent attenders
Most literature on FAs originates from countries which organise primary
care through a system in which a primary care physician (e.g. a GP) serves a
fixed group of enlisted patients. Apparently, frequent attendance is considered
more of a problem in this healthcare system because payment of the GP is
(largely) per enlisted patient and less per consultation. Several reviews from
Scandinavian countries14, the United Kingdom33, Spain34 and Health Maintenance
Organizations(HMO) in the United States35;36 describe morbidity of FAs during
a one year period (1yFAs). In 1yFAs combinations of somatic and psychosocial
problems are often observed and high rates of both psychological distress and
psychiatric disorders are found.37-39 Rates of somatization among FAs vary between
16 and 45% .35;40;41 As far as we know there is only one study describing frequent
12
WHY DO THEY KEEP COMING BACK?
attendance in the Netherlands42 and only one study from a country with an open
access system for primary care (France). The latter found that, when adjusting
for confounders, among four psychiatric diagnoses investigated, only somatoform
disorders remained significantly associated with frequent attendance. Physical
health and chronic diseases were not associated with frequent attendance.43
Thus, 1yFAs suffer more often from chronic somatic diseases, medically
unexplained symptoms, psychiatric problems (e.g. depression, anxiety) and
social problems than non-FAs.8;14 Less is known about persistent FAs, but existing
evidence indicates that these patients not only suffer from more somatic, but, in
particular, from more psychiatric problems.44;45 FAs who are depressed are more
likely to continue to be high-utilizers than non-depressed FAs.46 Therefore, we
examined the somatic and psychosocial morbidity of (persistent) frequent attenders
(chapter 3).
Workload and costs of FAs in primary and specialist healthcare
FAs are more frequently referred by their GP to specialist care than non-frequent
attenders (non-FAs).5 However, little is known about the magnitude of the
differences in primary and specialist healthcare utilisation and costs between nonFAs and FAs, as well as between subgroups of FAs (short-term versus persistent
FAs). Differences in workload and healthcare costs may be explained by the specific
characteristics and morbidities of FAs, and by physician characteristics. If not,
detection and treatment of underlying, not yet detected, conditions in FAs may
result in less morbidity, a better quality of life and decrease in costs.
Therefore, we examined the workload caused by FAs in primary care and costs of
healthcare of (persistent) FAs in primary and specialist care and whether these
costs can be explained by patients’ morbidities and by GP characteristics (chapter 3
and 6).
Prediction of persistent frequent attendance
Development of effective interventions to prevent 1yFAs to become persistent or
repetitive FAs is only possible if knowledge is available about determinants that
predict which one-year FAs are likely to become persistent FAs. However, literature
about determinants that predict persistent frequent attendance is inconsistent
and its interpretation is hampered by methodological differences (e.g. aetiological
and causal versus predictive non-causal outlooks, or confusion of these two), and
by different definitions of frequent attendance (e.g. proportional versus fixed
cutoff). In prospective cohort studies, using a proportional definition (the upper
10%), low physical quality of life, low educational level12 and psychological distress
(Hopkins Symptom Check List and Whiteley-7)9 predicted persistence of frequent
CHAPTER 1
13
attendance over the next two consecutive years. Using a fixed cutoff definition of
FA, one prospective cohort study found that female gender, obesity, former frequent
attendance, fear of death, alcohol abstinence, low satisfaction, and irritable bowel
syndrome were risk factors for persistence of frequent attendance during at least
3 out of the four next years.47 Another prospective cohort study concluded that the
Ambulatory Diagnosis Groups “unstable chronic medical conditions”, “see and
reassure conditions”, “minor time-limited psychosocial conditions”, and “minor
signs and symptoms” predicted persistence of frequent primary care use the next
year.48
A prediction rule may help GPs to identify which 1yFA is at risk to become a
persistent FA using information from the electronic medical record. Such a rule,
in addition to being clinically important, may also support the selection of more
homogeneous patient groups in future randomized trials among (subgroups of)
persistent frequent attenders (chapter 4 and 5).
Attempts to support and help (persistent) FAs, and to lower attendance rates
Is it possible to reduce the morbidity and use of healthcare of FAs and to improve
their quality of life? Several RCTs evaluating interventions for FAs have been
published but a clear overview of the different kind of interventions, an assessment
of their quality and the results of the interventions is lacking.44;49-54 Therefore, we
reviewed the literature to determine possible positive interventions to improve the
morbidity and the quality of life and to lower attendance rate of FAs (chapter 7).
This PhD thesis aims to answer these questions based on studies conducted among
(persistent) frequent attenders in the Netherlands. Hereafter, the Persistent
Frequent Attenders Risk Factors and treatment options (PERFACTIO) study is
described and the structure of the thesis is outlined.
The PERFACTIO study
Part I: Mapping frequent attenders in primary care
The first objective of this thesis was to establish the best method for selecting
FAs in a normal practice setting in the Netherlands. Secondly, we wanted to study
morbidity and GP’s workload of FAs of different duration. Thirdly, we examined
whether it would be feasible, using information readily available in GPs’ electronic
medical records, to predict which 1yFAs continue to attend frequently and whether
this prediction (rule) could be validated in another setting and timeframe. Finally,
we examined the costs of healthcare utilization by FAs of different duration in
primary and specialist care and to explore whether these costs could be explained
by the excess morbidity these FAs have or the characteristics of the GP’s.
14
WHY DO THEY KEEP COMING BACK?
Research questions
1.
What is the most feasible method to select FAs in a normal GP practice setting
using the proportional definition?
To answer this question we analysed in chapter 2 the data of the second Dutch
National survey of General Practice. These data were collected over a oneyear period on health and healthcare-related behaviour from 375 899 persons,
registered within 104 practices. We compared the quality of different FA
selection methods in general practice in the Netherlands.
2.
Which somatic, psychological and social problems do (persistent) FAs have?
What are the differences between short-term and persistent FAs in this
respect? What is the workload of a GP caused by (persistent) FAs?
In chapter 3 we analysed the GP database of the Academic Medical Center,
University of Amsterdam (Hag-net-AMC) of three consecutive years crosssectionally. We compared the diagnoses as registered by the GPs on the
so-called Problem Lists of frequent attenders during none, one, two and three
years, respectively.
3.
Which readily available information noted by the GP in patients’ Electronic
Medical Record predicts persistence of frequent attendance?
In order to answer this question we performed in chapter 4 a historic threeyear cohort study (2003-2005). We analysed which readily available data of
1yFAs out of the Electronic Medical Record of the GPs predict persistence of
frequent attendance.
4.
Can the prediction rule developed in chapter 4 be validated in another time
frame in the same GP database and in another GP database?
In chapter 5 we performed a geographical and temporal validation of our prior
prediction rule with data of a GP network in Eindhoven, the Netherlands
(SMILE; geographical validation) and our own network (Hag-net-AMC) in
another time frame (2009-2011).
5.
Are FAs of primary care also high users of specialist care? What are the costs of
healthcare of FAs in primary and specialist care?
6.
Are the high costs in primary and specialist healthcare of FAs of different
duration associated with patient’s morbidities and GP characteristics?
In order to answer research question 5 and 6 we linked in chapter 6 clinical
data of primary care patients to financial reimbursement data of the main
health insurer of our region (healthcare expenditures in primary and specialist
care), and GP characteristics. In a multilevel regression model, we analysed
CHAPTER 1
15
the healthcare expenditures of FAs and whether these expenditures can be
explained by the morbidity of the patients and the characteristics of their GPs.
Part II: Review of the literature about interventions on frequent attenders in
primary care.
7.
Research question 7. To determine possible effective interventions to improve
quality of life and lower attendance rate of FAs we systematically reviewed the
literature about possible effective interventions in FAs in chapter 7.
Part III: A prospective study of frequent attenders
The objective of the prospective study was to better understand the causes of
persistence of frequent attendance. This may facilitate the rational selection
of diagnostic tests and (better) prevention strategies. Potentially effective
interventions should be based on these aetiological factors for persistence of
frequent attendance. Research question eight is:
8.
Which (in particular psychosocial) factors are associated with persistence of
frequent attendance in a prospective cohort of 1-year FAs? Is there a supraadditive effect of combinations of somatic, psychological and socials factors?
In order to answer these questions we conducted a prospective cohort study
of 1yFAs and collected data about their GPs in chapter 8. With a multilevel
regression analysis we evaluated which patient and GP characteristics are
associated with persistence of frequent attendance.
Screening and consecutive treatment of patients in primary care tends to have
disappointing results.55-58 Therefore, we extrapolated the findings from the
cohort study among FAs over a period of 5 years and combined this with potential
treatment effects using modelling techniques. Research question nine is:
9.
To evaluate whether systematic detection and treatment of depression and
anxiety after one or two years of frequent attendance may be cost-effective
compared to usual GP care.
Therefore we performed in chapter 9 a Cost Effectiveness Analysis (CEA) with
data of the cohort of chapter eight. With a Markov simulation we analysed
whether diagnosing and treating of depression and anxiety (as measured by the
Patient Health Questionnaire) in FAs might be cost effective after one or two
years of frequent attendance.
We end the thesis with chapter 10, which provides a general discussion and
conclusion of our research.
16
WHY DO THEY KEEP COMING BACK?
References
(1) Ward AM, Underwood P, Fatovich
B, Wood A. Stability of attendance
in general practice. Fam Pract 1994;
11(4):431-437.
(2) Botica MV, Kovacic L, Tiljak MK, Katic
M, Botica I, Rapic M et al. Frequent
attenders in family practice in Croatia:
Retrospective study. Croatian Medical
Journal 2004; 45(5):620-624.
(3) Carney TA, Guy S, Jeffrey G. Frequent
attenders in general practice: a
retrospective 20-year follow-up study. Br
J Gen Pract 2001; 51(468):567-569.
(4) Andersson S-O, Lynoe N, Hallgren
C-G, Nilsson M. Is frequent attendance
a persistent characteristic of a patient?
Repeat studies of attendance pattern
at the family practitioner. Scandinavian
Journal of Primary Health Care 2004;
22(2):91-94.
(5) Heywood PL, Blackie GC, Cameron
IH, Dowell AC. An assessment of the
attributes of frequent attenders to
general practice. Fam Pract 1998;
15(3):198-204.
(6) Neal RD, Heywood PL, Morley S,
Clayden AD, Dowell AC. Frequency
of patients’ consulting in general
practice and workload generated
by frequent attenders: comparisons
between practices. Br J Gen Pract 1998;
48(426):895-898.
(7) Tomenson B, McBeth J, Chew-Graham
CA, Macfarlane G, Davies I, Jackson J et
al. Somatization and health anxiety as
predictors of health care use. Psychosom
Med 2012; 2012(6):656-664.
(8) Vedsted P, Fink P, Sorensen HT, Olesen
F. Physical, mental and social factors
associated with frequent attendance in
Danish general practice. A populationbased cross-sectional study. Soc Sci Med
2004; 59(4):813-823.
(9) Vedsted P, Fink P, Olesen F, MunkJorgensen P. Psychological distress
as a predictor of frequent attendance
in family practice: a cohort study.
Psychosomatics 2001; 42(5):416-422.
(10) Vedsted P, Fink P, Sorensen HT, Olesen
F. Physical, mental and social factors
associated with frequent attendance in
Danish general practice. A populationbased cross-sectional study. Social
Science & Medicine 2004; 59(4):813-823.
(11) Little P, Somerville J, Williamson
I, Warner G, Moore M, Wiles R et al.
Psychosocial, lifestyle, and health status
variables in predicting high attendance
among adults. Br J Gen Pract 2001;
51(473):987-994.
(12) Rifel J, Svab I, Selic P, Rotar Pavlic
D, Nazareth I, Car J. Association of
Common Mental Disorders and Quality
of Life with the Frequency of Attendance
in Slovenian Family Medicine Practices:
Longitudinal Study. PLoS ONE 2013;
8(1):e54241.
(13) Howe A, Parry G, Pickvance D, Hockley
B. Defining frequent attendance:
evidence for routine age and sex
correction in studies from primary
care settings. Br J Gen Pract 2002;
52(480):561-562.
(14) Vedsted P, Christensen MB. Frequent
attenders in general practice care: a
literature review with special reference to
methodological considerations. Public
Health 2005; 119(2):118-137.
(15) Westert GP, Schellevis FG, De Bakker
DH, Groenewegen PP, Bensing JM, van
der ZJ. Monitoring health inequalities
through general practice: the Second
Dutch National Survey of General
Practice. Eur J Public Health 2005;
15(1):59-65.
(16) Howe A. Who is a frequent attender?
Br J Gen Pract 2000; 50(457):666.
(17) van den Bosch WJ, Huygen FJ, van
den Hoogen HJ, van Weel C. Morbidity
in early childhood: family patterns in
relation to sex, birth order, and social
class. Fam Med 1993; 1993(2):126-130.
(18) Huygen FJ. Family Medicine- The
medical life history of families. Assen,
The Netherlands: van Gorcum; 1978.
CHAPTER 1
17
(19) Dwamena FC, Lyles JS, Frankel RM,
Smith RC. In their own words: qualitative
study of high-utilising primary care
patients with medically unexplained
symptoms. BMC Fam Pract 2009;
10(1):67.
(30) McDaniel SH, Campbell T, Seaburn
D. Treating Somatic Fixation: A
Biopsychosocial Approach: When
patients express emotions with physical
symptoms. Can Fam Physician 1991:451456.
(20) Neal RD, Heywood PL, Morley S. ‘I
always seem to be there’--a qualitative
study of frequent attenders. Br J Gen
Pract 2000(458):716-723.
(31) Rosendal M, Fink P, Bro F, Olesen F.
Somatization, heartsink patients, or
functional somatic symptoms? Towards
a clinical useful classification in primary
health care. Scand J Prim Health Care
2005; 2005(1):3-10.
(21) Hodgson P, Smith P, Brown T, Dowrick
C. Stories from frequent attenders: a
qualitative study in primary care. Ann
Fam Med 2005; 3(4):318-323.
(22) Taylor RE, Marshall T, Mann A,
Goldberg DP. Insecure attachment and
frequent attendance in primary care: a
longitudinal cohort study of medically
unexplained symptom presentations in
ten UK general practices. Psychol Med
2011:1-10.
(23) Ciechanowski PS, Walker EA, Katon
WJ, Russo JE. Attachment theory:
a model for health care utilization
and somatization. Psychosom Med
2002(4):660-667.
(24) Campbell T.L. Family’simpact on
health: a critical review. Family Systems
Medicine 1986; 4:135-336.
(25) Cardol M, van den Bosch WJHM,
Spreeuwenberg P, Groenewegen PP, van
Dijk L, de Bakker DH. All in the Family:
Headaches and Abdominal Pain as
Indicators for Consultation Patterns in
Families. The Annals of Family Medicine
2006; 4(6):506-511.
(26) Wennberg JE. Practice variations: why
all the fuss? Internist 1985; 26(4):6-8.
(27) Wennberg JE. Dealing with medical
practice variations: a proposal for action.
Health Aff (Millwood ) 1984; 3(2):6-32.
(28) Neal RD, Heywood PL, Morley S.
Frequent attenders’ consulting patterns
with general practitioners. Br J Gen Pract
2000; 50(461):972-976.
(29) Bellon JA, Fernandez-Asensio
ME. Emotional profile of physicians
who interview frequent attenders.
Patient Education and Counseling /9;
48(1):33-41Record.
18
(32) Tielens VC. Consulten van huisartsen
Meppel: Krips Repro; 1987.
(33) Gill D, Sharpe M. Frequent consulters
in general practice: a systematic review
of studies of prevalence, associations
and outcome. J Psychosom Res 1999;
47(2):115-130.
(34) Luciano JV, Fernandez A, Pinto-Meza
A, Lujan L, Bellon JA, Garcia-Campayo
J et al. Frequent attendance in primary
care: comparison and implications of
different definitions. Br J Gen Pract 2010;
60(571):49-55.
(35) Katon W, Von KM, Lin E, Lipscomb
P, Russo J, Wagner E et al. Distressed
high utilizers of medical care. DSM-III-R
diagnoses and treatment needs. Gen
Hosp Psychiatry 1990; 12(6):355-362.
(36) Von Korff M, Ormel J, Katon W, Lin EH.
Disability and depression among high
utilizers of health care. A longitudinal
analysis. Arch Gen Psychiatry 1992;
49(2):91-100.
(37) Karlsson H, Lehtinen V, Joukamaa M.
Psychiatric morbidity among frequent
attender patients in primary care. Gen
Hosp Psychiatry 1995; 17(1):19-25.
(38) Heywood PL, Blackie GC, Cameron
IH, Dowell AC. An assessment of the
attributes of frequent attenders to
general practice. Family Practice 1998;
15(3):198-204.
(39) Jyvasjarvi S, Joukamaa M, Vaisanen
E, Larivaara P, Kivela S, KeinanenKiukaanniemi S. Somatizing frequent
attenders in primary health care. J
Psychosom Res 2001; 50(4):185-192.
(40) Karlsson H, Joukamaa M, Lahti I,
Lehtinen V, Kokki-Saarinen T. Frequent
attender profiles: different clinical
subgroups among frequent attender
patients in primary care. J Psychosom
Res 1997; 42(2):157-166.
WHY DO THEY KEEP COMING BACK?
(41) De Waal MWM, Arnold IA, Eekhof JAH,
van Hemert AM. Somatoform disorders
in general practice. Br J Psych 2004;
184:470-476.
(42) van der Ploeg HM. Persoonlijkheid
en medische consumptie: Een
onderzoek naar de relatie van
persoonlijkheidsfactoren en de
frequentie van huisartsbezoek. Swets
&Zeitlinger B.V.; 1980.
(43) Norton J, David M, de Roquefeuil
G, Boulenger JP, Car J, Ritchie K et al.
Frequent attendance in family practice
and common mental disorders in an
open access health care system. J
Psychosom Res 2012; 2012(6):413-418.
(44) Katzelnick DJ, Simon GE, Pearson
SD, Manning WG, Helstad CP, Henk HJ
et al. Randomized trial of a depression
management program in high utilizers
of medical care. Arch Fam Med 2000;
9(4):345-351.
(45) Pearson SD, Katzelnick DJ, Simon
GE, Manning WG, Helstad CP, Henk
HJ. Depression among high utilizers of
medical care. J Gen Intern Med 1999;
14(8):461-468.
(46) Henk HJ, Katzelnick DJ, Kobak KA,
Greist JH, Jefferson JW. Medical costs
attributed to depression among patients
with a history of high medical expenses
in a health maintenance organization.
Arch Gen Psychiatry 1996; 1996(10):899904.
(47) Koskela TH, Ryynanen OP, Soini EJ.
Risk factors for persistent frequent
use of the primary health care services
among frequent attenders: a Bayesian
approach. Scand J Prim Health Care
2010; 28(1):55-61.
(48) Naessens JM, Baird MA, Van
Houten HK, Vanness DJ, Campbell CR.
Predicting persistently high primary care
use. Ann Fam Med 2005(4):324-330.
(49) Simon GE, Manning WG, Katzelnick
DJ, Pearson SD, Henk HJ, Helstad
CS. Cost-effectiveness of systematic
depression treatment for high utilizers
of general medical care. Arch Gen
Psychiatry 2001; 58(2):181-187.
(51) Christensen MB, Christensen B,
Mortensen JT, Olesen F. Intervention
among frequent attenders of the outof-hours service: A stratified cluster
randomized controlled trial. Scandinavian
Journal of Primary Health Care 2004;
22(3):180-186.
(52) Katon W, Von KM, Lin E, Bush T, Russo
J, Lipscomb P et al. A randomized trial of
psychiatric consultation with distressed
high utilizers. Gen Hosp Psychiatry 1992;
14(2):86-98.
(53) Bellon JA, Rodriguez-Bayon A, de
Dios LJ, Torres-Gonzalez F. Successful
GP intervention with frequent attenders
in primary care: randomised controlled
trial. Br J Gen Pract 2008; 58(550):324330.
(54) Barsky AJ, Ahern DK, Bauer MR,
Nolido N, Orav EJ. A Randomized Trial of
Treatments for High-Utilizing Somatizing
Patients. J Gen Intern Med 2013; 2013.
(55) Baas KD, Wittkampf KA, van Weert
HC, Lucassen P, Huyser J, van den
Hoogen H et al. Screening for depression
in high-risk groups: prospective cohort
study in general practice. The British
Journal of Psychiatry 2009; 194(5):399403.
(56) Bosmans J, Schreuders B, van Marwijk
H, Smit J, van Oppen P, van Tulder M.
Cost-effectiveness of problem-solving
treatment in comparison with usual care
for primary care patients with mental
health problems: a randomized trial. BMC
Family Practice 2012; 13(1):98.
(57) Bosmans JE, van Schaik DJ, de Bruijne
MC, van Hout HP, van Marwijk HW, van
Tulder MW et al. Are psychological
treatments for depression in primary
care cost-effective? J Ment Health Policy
Econ 2008; 11(1):3-15.
(58) Thombs BD, Ziegelstein RC, Roseman
M, Kloda LA, Ioannidis JP. There are no
randomized controlled trials that support
the United States Preventive Services
Task Force guideline on screening for
depression in primary care: a systematic
review. BMC Med 2014:13-12.
(50) Adam P, Brandenburg DL, Bremer
KL, Nordstrom DL. Effects of team
care of frequent attenders on patients
and physicians. Fam Syst Health. 2010
Sep;28(3):247-57.
GENERAL INTRODUCTION
19
part I
MAPPING FREQUENT ATTENDERS
IN PRIMARY CARE
chapter 2
DEFINING FREQUENT ATTENDANCE
IN GENERAL PRACTICE
Frans Th. M. Smits, Jacob Mohrs,
Ellen E. Beem, Patrick J.E. Bindels,
Henk C.P.M. van Weert
BMC Family practice, 2008, 9:21.
ABSTRACT
Background
General practitioners (GPs) or researchers sometimes need to
identify frequent attenders (FAs) in order to screen them for
unidentified problems and to test specific interventions.
We wanted to assess different methods for selecting FAs to
identify the most feasible and effective one for use in a general
(group) practice.
Methods
In the second Dutch National Survey of General Practice,
data were collected on 375 899 persons registered with 104
practices. Frequent attendance is defined as the top 3% and
10% of enlisted patients in each one-year age-sex group
measured during the study year. We used these two selections
as our reference standard. We also selected the top 3% and 10%
FAs (90 and 97 percentile) based on four selection methods of
diminishing preciseness. We compared the test characteristics
of these four methods.
Results
Of all enlisted patients, 24 % did not consult the practice during
the study year. The mean number of contacts in the top 10%
FAs increased in men from 5.8 (age 15-24 years) to 17.5 (age 6475 years) and in women from 9.7 to 19.8. In the top 3% of FAs,
contacts increased in men from 9.2 to 24.5 and in women from
14 to 27.8.
The selection of FAs becomes more precise when smaller age
classes are used. All selection methods show acceptable results
(kappa 0.849 – 0.942) except the three group method.
Conclusion
To correctly identify frequent attenders in general practice, we
recommend dividing patients into at least three age groups per
sex.
22
WHY DO THEY KEEP COMING BACK?
Background
In primary care, the workload of General
Practitioners (GPs) is significantly related
to a minority of patients who consult
more frequently than their peers1. Studies
are consistent in confirming that these
frequent attenders (FAs) have high
rates of physical disease, psychiatric
illness, social difficulties and emotional
distress2-4. Because frequent attendance
can be related to undisclosed medical
problems, identifying FAs could help GPs
to select those patients who may need an
adjustment to the care they receive5. The
combination of large workload and high
rate of (chronic) disease make FAs an
important group for a GP not only to study
but also to treat. Exceptional attendance
is also considered as an indicator of
inappropriate consulting behaviour and
healthcare use6-11. Health services research
has therefore used frequent attendance for
identifying both inadequate health care
delivery and possible misuse of health care.
Trials on the effect of (mainly psychiatric)
interventions on the attendance rate and
morbidity of FAs showed conflicting
results12-15. In a review of interventions on
FAs we found indications that frequent
attendance might be a sign of as yet
undiagnosed major depressive disorder
(MDD) and that treatment of MDD might
improve the depressive symptoms and the
quality of life of depressed FAs. We found
no evidence that it is possible to influence
healthcare utilization12-15.
The interpretation of studies on frequent
attendance is hampered because of
differences in the organisation of health
care, the setting and the definition
of FAs. Age and sex have been shown
to be highly associated with the
frequency of attendance16. Selecting FAs
without adjusting for age and sex will
predominantly result in the selection
of older women3. Therefore, any study
of frequent attendance requires a clear
definition of these patients and a clear
description of the selection process. After
reviewing the literature on frequent
attendance, Vedsted suggested that
frequent attendance should be defined as
a proportional part (highest 10%) of all
attenders, stratified for age and sex17.
Selecting FAs by using age groups with
a small band (for instance ten-year
groupings) is difficult, especially in
smaller populations like those of a (group)
practice because of the resulting low
number of patients in each cell. Therefore,
Howe et al. developed an easy cohort
definition to identify those patients whose
attendance patterns are unusual for their
sex and age. She stated that, dividing
the male population into two different
age groups (15-44; 45-74 years), would
result in including 95% of the total male
patients identified as attending at or
above the 97th percentile compared with
the more complex procedure of ten-year
groupings. Further, she concluded that
no such division of the population was
needed for females, as their consultation
rates were considered fairly constant. She
advised further analysis on the validity
of this method in other populations to be
performed18.
In the Netherlands every citizen is enlisted
by one GP and Dutch inhabitants consult
their own GP for all medical complaints.
CHAPTER 2
23
The GP functions as a gatekeeper for
specialist care. GP-care in 2001 was
paid either by a social sick-fund or an
obligatory private insurance. We used
the large database of the second Dutch
National Survey of General Practice (2001)
as a unique possibility for comparing the
quality of different FA selection methods
in general practice in the Netherlands.
Our aim was to assess these methods and
to identify the most feasible and effective
one for use in an average general (group)
practice.
Method
In the second Dutch National survey of
General Practice, data were collected
over a one-year period on health and
healthcare-related behaviour from 375
899 persons, registered with 104 practices.
Eight practices were excluded because
of insufficient data (see flow diagram).
Population, practices and GPs were
representative for the Dutch population,
with a slight under-representation of
single-handed GPs. The study design,
methods, response and quality of the data
of this extensive second Dutch National
Survey have been published elsewhere
in more detail19-21. To correct for loss or
growth of the practices involved during
the study year, we used the data of patients
enlisted within each practice over the
complete one-year period (n= 263 148) as
the denominator. As most previous studies
on frequent attendance have excluded
children and the very old, we also only
used the data of patients between the ages
of 15 and 74 years.
Figure 1. Flow diagram
National Survey of General
Practice (NS2).
•
375 899 patients
•
104 general practices
NS2
•
N= 276 924 patients
•
96 general practices
Exclusion:
< 15 y; >75 y.
8 practices because of insufficient data.
Exclusion:
Not enlisted all year.
Minus 13 776
Study population:
•
N= 263 148 patients
Analyses
24
WHY DO THEY KEEP COMING BACK?
For all patients included, each contact
with the primary care team (consultations,
house calls and telephone calls) was
registered. We calculated the contact
frequencies of all patients between the
ages of 15-74 years for every combination
of age and sex. As in previous research,
the top 3% and the top 10% consulting
patients from this calculation were defined
as FAs. We also included patients with no
attendance. These two selections were
then used as our reference standard.
As index-selections, we selected the top 3%
and 10% of FAs of the same population by
dividing the genders into four different age
group clusters ranging from just one to as
many as six. We compared the sensitivity
and specificity of the selection criteria in
each of these four cluster groups:
1.
Per each 10-year age band: 6 classes
per sex category17;18.
2.
Per each 15-year age band: 4 classes
per sex category.
3.
According to the sex-age grouping,
used by the WONCA classification
committee, we tested an adjusted
selection method with 3 age classes
per sex category: 15-44 years, 45-64
years and 65-74 years22.
4.
Dividing males into two separate
cohorts (15-44 years; 45-74 years) and
all women in one cohort: the three
group method18.
By constructing four by four tables we
calculated the test characteristics (the
sensitivity, specificity, positive and
negative predictive value and kappa) of
these four clusters, using the one-year age
band method as reference standard. All
data were analysed using SPSS 14.0 for
windows.
The study was conducted according to
the Dutch legislation on data protection
(Ministry of Justice, the Netherlands)
Results
From the total number of enlisted patients,
63102 (24%) of which 21 090 female and 42
012 men did not consult their primary care
practice during the study year. Women
consulted more frequently than men and
older age correlated with a rising number
of contacts for both sexes (figure 1). The
mean number of contacts increased in
men from 1.62 (age 15-24 years) to 5.13 (age
65-74 years) and in women from 3.32 (age
14-24 years) to 6.27 (65-74 years). The mean
attendance by sex and age of the top 3%
and 10% attenders is presented in figure
1. The mean number of contacts in the top
10% FAs increased in men from 5.84 (age
15-24 years) to 17.46 (age 64-75 years) and
in women from 9.72 (age 15-24 years) to
19.83 (age 64-75 years). The mean number
of contacts in the top 3% of FAs increased
in men from 9.21 (age 15-24 years) to 24.52
(age 64-75 years) and in women from 14.02
(age 15-24 years) to 27.83 (age 64-75 years).
All test characteristics (sensitivity,
specificity, positive and negative predictive
value and kappa), are summarized in table
1. With 6 classes, the kappa is 0.942 (10
% FA) and 0.925 (3% FA) but with the 3
group-method the kappa is 0.818 (10% FA)
and 0.756 (3% FA). Test characteristics
improve with smaller age classes and
CHAPTER 2
25
logically sensitivity drops by using the
three group method, even more in females
than in males. The test characteristics
are slightly better when the top 10 % is
selected instead of the top 3% of FAs. All
methods show acceptable results (kappa
0.849 - 0.942) except the three group
method.
Discussion
The purpose of this study was to compare
different methods for selecting frequent
attenders in primary care and to identify
the most feasible method with acceptable
test characteristics in a general (group)
practice . We found specificity to be about
the same in all methods, but sensitivity
diminishes gradually when larger age
groupings are used and shows a drop in
the three group method. This means that
with the three group method (3% resp.10%
FA) 25% resp. 17 % of the FAs will not be
identified. For instance selecting the top
10% of FAs the three group method misses
5247 FAs (17%) of which 58% female and
47% in the age between 15 and 24.
This study is the first attempt to compare
different methods of identifying FAs. In
a large database like the Dutch National
Survey, the reference method (with one
year sex-age bands) is the most precise
method for identifying FAs. In smaller
databases however, such a method results
in very few patients within each age band
and is therefore not feasible. Our results
demonstrate that specificity and sensitivity
for identifying FAs increases when smaller
age groups are used, as could be expected.
On the level of a general (group) practice,
less precise methods can be used with
Figure 2. Mean attendance per sex, all attenders and the top 3%/10% attenders
30
mean attendance 3%
FA women
mean attendance 3%
FA men
25
mean attendance 10%
FA women
20
mean attendance 10%
FA men
number of contacts
15
10
mean attendance women
mean attendance men
5
0
15-24
25-34
35-44
45-54
10-year age group
26
WHY DO THEY KEEP COMING BACK?
55-64
65-74
Table 1. Overview of the test characteristics of the four selection methods,
6 cl, method
3%FA1
6 cl, method
10%FA 2
4 cl, method
3%FA3
4 cl, method
10%FA4
women men
women men
women men
women men
Sensitivity
94,2
89,4
94,0
93,1
89,4
93,6
94,7
91,5
Specificity
99,8
99,8
99,3
99,8
99,8
99,6
99,6
99,1
5
93,7
93,7
94,3
98,2
93,7
89,5
96,3
93,1
NPV6
99,8
99,6
99,2
99,0
99,6
99,8
99,3
98,8
Kappa
0,937
0,912
0,934
0,950
0,912
0,911
0,949
0,912
PPV
3 cl, method
3%FA7
6 cl, method
10%FA8
4 cl, method
3%FA9
4 cl, method
10%FA10
women men
women men
women men
women men
Sensitivity
89,0
84,8
96,0
85,5
76,1
73,6
79,3
86,5
Specificity
99,3
99,3
98,3
98,8
99,1
99,4
98,5
97,6
PPV
88,1
80,4
87,8
90,6
74,1
82,3
86,9
83,1
NPV
99,6
99,5
99,5
98,0
99,2
99,1
97,4
98,1
Kappa
0,881
0,819
0,906
0,864
0,742
0,770
0,809
0,826
Table 2. Men and women
6 cl, method
4 cl, method
3 cl, method
3 group-method
3% FA
10% FA
3% FA
10% FA
3% FA
10% FA
3% FA
10% FA
Sensitivity
91,8
93,5
90,9
93,0
86,9
90,6
74,8
83,0
Specificity
99,8
99,5
99,7
99,3
99,4
98,5
99,3
98,0
PPV
93,7
96,3
91,4
94,6
84,1
89,1
78,0
84,8
NPV
99,7
99,1
99,7
99,1
99,5
98,7
99,1
97,7
kappa
0,925
0,942
0,912
0,930
0,849
0,885
0,756
0,818
1.
2.
3.
4.
5.
6.
7.
8.
9.
6 cl. method: selection FAs per 10 years of age.
Idem
4 cl. method: selection of FAs per 15 years of age
Idem
positive predictive value
negative predictive value
3 cl. method: selection of FAs in 3 age groups (15-44; 45-64; 65-74).
Idem
3 group method: selection of male FAs in two age groups (15-44; 45-74)
and women in one group.
10. Idem
CHAPTER 2
27
acceptable results: for instance, by dividing
all patients into at least 3 age cohorts per
sex. For studies on larger patient groups,
it is best to use the smallest possible age
groupings, mainly for reasons of positive
predictive value. Standardisation of
methods for selecting FAs is needed in
order to allow comparisons between
studies to take place.
The purpose for which FAs need to be
selected, as well as the limitations of
the database, can determine the degree
of the desired precision. For example,
if a GP wants to use frequent attending
as a red flag pointing at unidentified
medical problems, it would not be too big
a problem to incorrectly select a patient
(false positive). Not selecting an FA (false
negative) seems to be a bigger problem, but
the negative predictive value is high in all
methods. However researchers have to use
the smallest age band possible to correctly
select FAs.
Conclusion
We conclude that in order to identify
exceptional users of health care, sex and
age have to be taken into account. The best
method for identifying frequent attenders
is to use small age and sex groups. If this
is not possible or needed, for instance
in a single general (group) practice, we
recommend that GPs divide their patients
into at least 3 age groups per sex category
in order to identify their exceptional
attenders.
28
References
(1) Neal RD, Heywood PL, Morley S,
Clayden AD, Dowell AC. Frequency
of patients’ consulting in general
practice and workload generated
by frequent attenders: comparisons
between practices. Br J Gen Pract 1998;
48(426):895-898.
(2) Gill D, Sharpe M. Frequent consulters
in general practice: a systematic review
of studies of prevalence, associations
and outcome. J Psychosom Res 1999;
47(2):115-130.
(3) Vedsted P, Christensen MB. Frequent
attenders in general practice care: a
literature review with special reference to
methodological considerations. Public
Health 2005; 119(2):118-137.
(4) de Waal MW, Arnold IA, Eekhof JA,
Assendelft WJ, van Hemert AM. Followup study on health care use of patients
with somatoform, anxiety and depressive
disorders in primary care. BMC Fam
Pract 2008; 9(1):5.
(5) Karlsson H, Joukamaa M, Lahti I,
Lehtinen V, Kokki-Saarinen T. Frequent
attender profiles: different clinical
subgroups among frequent attender
patients in primary care. J Psychosom
Res 1997; 42(2):157-166.
(6) Booth BM, Ludke RL, Wakefield DS,
Kern DC, du Mond CE. Relationship
between inappropriate admissions and
days of care: implications for utilization
management. Hosp Health Serv Adm
1991; 36(3):421-437.
(7) Brandon WR, Chambers R. Reducing
emergency department visits among
high-using patients. J Fam Pract 2003;
52(8):637-640.
(8) Hansagi H, Olsson M, Sjoberg S,
Tomson Y, Goransson S. Frequent use
of the hospital emergency department
is indicative of high use of other health
care services. Ann Emerg Med 2001;
37(6):561-567.
(9) Kapur K, Young AS, Murata D, Sullivan
G, Koegel P. The economic impact of
capitated care for high utilizers of public
mental health services: the Los Angeles
PARTNERS program experience. J
Behav Health Serv Res 1999; 26(4):416429.
WHY DO THEY KEEP COMING BACK?
(10) Reid S, Wessely S, Crayford T, Hotopf
M. Frequent attenders with medically
unexplained symptoms: Service use and
costs in secondary care. British Journal
of Psychiatry 2002; 180(3):248-253.
(11) Stewart P, O’Dowd T. Clinically
inexplicable frequent attenders in
general practice. Br J Gen Pract 2002;
52(485):1000-1001.
(12) Christensen MB, Christensen B,
Mortensen JT, Olesen F. Intervention
among frequent attenders of the outof-hours service: a stratified cluster
randomized controlled trial. Scand J Prim
Health Care 2004; 22(3):180-186.
(13) Simon GE, Manning WG, Katzelnick DJ,
Pearson SD, Henk HJ, Helstad CP. Costeffectiveness of systematic depression
treatment for high utilizers of general
medical care. Archives of General
Psychiatry /2; 58(2):181-187.
(19) Jones R, Schellevis F, Westert G.
The changing face of primary care: the
second Dutch national survey. Fam Pract
2004; 21(6):597-598.
(20) Schellevis FG, Westert GP, De Bakker
DH. [The actual role of general practice
in the dutch health-care system. Results
of the second dutch national survey of
general practice]. Med Klin (Munich)
2005; 100(10):656-661.
(21) Westert GP, Schellevis FG, De Bakker
DH, Groenewegen PP, Bensing JM, van
der ZJ. Monitoring health inequalities
through general practice: the Second
Dutch National Survey of General
Practice. Eur J Public Health 2005;
15(1):59-65.
(22) Lamberts H, Wood M e. International
classification of primary care. Oxford:
Oxford University Press; 1988.
(14) Katzelnick DJ, Simon GE, Pearson
SD, Manning WG, Helstad CP, Henk HJ
et al. Randomized trial of a depression
management program in high utilizers
of medical care. Arch Fam Med 2000;
9(4):345-351.
(15) Katon W, von Korff M, Lin E, Bush
T. A randomized trial of psychiatric
consultation with distressed high
utilizers. General Hospital Psychiatry /3;
14(2):86-98Record.
(16) Little P, Somerville J, Williamson
I, Warner G, Moore M, Wiles R et al.
Psychosocial, lifestyle, and health status
variables in predicting high attendance
among adults. Br J Gen Pract 2001;
51(473):987-994.
(17) Vedsted P, Christensen MB. Frequent
attenders in general practice care: a
literature review with special reference to
methodological considerations. Public
Health 2005; 119(2):118-137.
(18) Howe A, Parry G, Pickvance D, Hockley
B. Defining frequent attendance:
evidence for routine age and sex
correction in studies from primary
care settings. Br J Gen Pract 2002;
52(480):561-562.
CHAPTER 2
29
chapter 3
EPIDEMIOLOGY OF (PERSISTENT)
FREQUENT ATTENDERS
-A 3-YEAR HISTORIC COHORT
STUDY COMPARING ATTENDANCE,
MORBIDITY AND PRESCRIPTIONS
OF ONE-YEAR AND PERSISTENT
FREQUENT ATTENDERSFrans T. Smits, Henk J. Brouwer,
Gerben ter Riet, Henk C. van Weert
BMC Public Health 2009, 9:36
ABSTRACT
Background
Attendance rates for patients visiting a General Practitioner
(GP) vary. Patients who remain in the top 10 centile of the age
and sex adjusted attendance rate for at least 3 years are known
as persistent frequent attenders. GPs spend a disproportionate
amount of time on persistent Frequent Attenders. So far, trials
on the effect of (mostly psychiatric) interventions on frequent
attenders have shown negative results. However, these trials
were conducted in short-term (< 3year) Frequent Attenders. It
would be more reasonable and efficient to target diagnostic
assessment and intervention at persistent Frequent Attenders.
Typical characteristics of persistent Frequent Attenders, as
distinct from frequent attenders during one year and nonFrequent Attenders, may generate hypotheses with respect
to modifiable factors on which new randomized trials may be
designed.
Methods
We used the data of all 28,860 adult patients from 5 primary
healthcare centres, participating in a GP-based continuous
morbidity registration network. Frequent Attenders were
patients whose attendance rate ranked in the (age and sex
adjusted) top 10 percent during 1 year (1- year-Frequent
Attenders) or 3 years (persistent Frequent Attenders). All other
patients on the register over the 3 year period were referred
to as non-Frequent Attenders. The lists of current medical
problems as registered and coded by the GP using the
International Classification of Primary Care (ICPC) were used to
assess morbidity.
First, we determined which proportion of 1-year-Frequent
Attenders was still a frequent attender during the next two
consecutive years and calculated the GPs’ workload for these
patients. Second, we compared the morbidity and the number
of prescriptions for non-Frequent Attenders, 1-year-Frequent
Attenders and persistent Frequent Attenders known to the GP.
32
WHY DO THEY KEEP COMING BACK?
Results
Of all 1yFAs, 15.4 % became a pFA (1.6% of all patients). Of
the FAs, 3,045 (10.6%) were responsible for 39% of the faceto-face consultations; 470 patients who would become pFAs
(1.6%) were responsible for 8% of all consultations in 2003.
Compared to non-FAs and 1yFAs, considerable more social
problems, feelings of anxiety, addictive behaviour and medically
unexplained physical symptoms were seen in pFAs. FAs
differ less where the prevalence of chronic somatic diseases
- respiratory problems, cardiovascular problems and diabetes
mellitus- are concerned.
Conclusion
One out of every seven 1-year-frequent attenders (15.4%)
becomes a persistent Frequent Attender. Compared with nonFrequent Attenders, and 1-year-Frequent Attenders, persistent
Frequent Attends consume more health care and are diagnosed
not only with more somatic diseases but especially more social
problems, psychiatric problems and medically unexplained
physical symptoms.
CHAPTER 3
33
Background
General practitioners (GP) spend a large
part of their time on a small proportion of
their patients. It is estimated that about
80% of a GP’s clinical work is spent on 20%
of their patients1. In most studies, frequent
attendance is defined as an age and sexadjusted attendance rate ranking in the top
10 centile within a time frame of one year
(1-year-Frequent Attenders)2;3.
Systematic reviews show that these
1-year-Frequent Attenders are more likely
to suffer from physical and psychiatric
illness, social difficulties and emotional
distress 2;4;5. High attendance rates are
also found for patients with medically
unexplained somatic symptoms, health
anxiety and perceived poor health 5-7. In
addition, frequent attendance may be a sign
of inappropriate consultation behaviour 8-11.
At this point, we should ask the question
whether or not it is possible to treat
frequent attenders and reduce their
attendance rates? Trials on the effect of
(mainly psychiatric) interventions have
shown conflicting results 12;12. No study
has shown convincing evidence that any
intervention improves the quality of life
or morbidity of Frequent Attenders in
primary care, although there is some
evidence that an effect might exist in a
subgroup of Frequent Attenders – that of
depressed patients. There is no evidence to
suggest that the utilization of health care
by Frequent Attenders can be influenced.
The only trials that showed positive effects
were with patients who were Frequent
Attender over a period of two years; all
others used a time frame of one year 13;14.
34
This means that these studies may have
targeted the wrong group of transient
Frequent Attenders.
Until now most research on frequent
attendance has been cross-sectional and
used one-year attendance rates. The few
longitudinal studies conducted showed
regression of attendance to the mean in
the longer run, with only 20-30% of FAs
continuing to attend frequently in the
following year 15-17. However, these studies
on persistent frequent attendance used
different definitions of FAs and lacked the
power to detect differences in morbidity
between transient and persistent frequent
attenders.
This study presents the results of a
historic 3-year cohort study on 28,860
adult patients in a longitudinal primary
care database. Our first objective was
to study the natural course of frequent
attendance and to determine the
proportion of 1-year-Frequent Attenders
who remain a Frequent Attender during
two consecutive years and to calculate the
GP workload for non-Frequent Attenders,
1-year-Frequent Attenders, and persistent
Frequent Attenders. Secondly, we wanted
to determine whether and how persistent
Frequent Attenders differ from 1-yearFrequent Attenders and normal attenders.
Methods
Patient population
Five primary healthcare centres in
Amsterdam provided data for this study.
These centres participate in the GP-based
continuous morbidity registration network
of the Department of General Practice
WHY DO THEY KEEP COMING BACK?
at the Academic Medical Centre of the
University of Amsterdam. The studied
patients have a lower socio-economic
level and are of more non-western descent
than the average Dutch population. The
age distribution refers about the Dutch
population. In this network, electronic
medical record data are extracted for
research purposes. The participating
GPs use a problem oriented registration
method. For this study we used the
following data: the numbers of face-toface GP consultations, the lists of patients’
current medical problems as registered
and coded by the GPs using the ICPC, the
number of a selection of prescriptions for
all enlisted patients from 1 January 2003
through 31 December 2005.
Selection of 1yFAs, pFAs and non-FAs
Frequent Attenders were defined as those
patients whose attendance rate ranked
nearest to the top 10th centile of their sex
and age group (15-30 years; 31-45 years; 4660 years; 61 years+) 2 3. Frequent Attenders
were determined for each of the years
2003, 2004 and 2005. As starting point,
we took the one-year-frequent attenders
for the year 2003. We defined persistent
Frequent Attenders as those patients
who continued to be a frequent attender
over the three year period. Patients who
were never a Frequent Attender in the
three year study period (non-Frequent
Attenders) were used as a reference group.
We compared the three selections. Patients
younger than 15 years were excluded,
because their consultations often depend
on their parents. A multivariable analysis
was performed to check for selective loss
to follow up.
Attendance
Only face-to-face consultations with GPs
(consultations in the surgery and housecalls) were included. Consultations with
other practice staff were excluded because
these contacts are mostly initiated by the
GP and relate mostly to the monitoring of
chronic diseases. We determined the mean
number of consultations per age and sex
group for the three groups of patients.
Morbidity
In the problem oriented approach to
medical record keeping, patients can have a
list of current medical problems (“Problem
list”). Different from the definition used
in the UK, in the Netherlands a current
medical problem is defined by the GP as:
any medical problem (disease or complaint)
which needs continual medical attention
or monitoring; any complaint or disease
presented to the GP that has lasted more
than 6 months and/or any recurrent
medical problem (more than 4 complaints
per half year).Every problem on this list
was coded by the GPs using the ICPC 18.
Please see appendix 1 for a list of the ICPCcodes.
The data from these problem lists were
extracted at the end of 2003 and the end
of 2005. The numerator in the prevalence
calculations was the number of enlisted
patients with a certain current problem
at the end of the two periods. Thus the
prevalence of each medical problem was
calculated for 1-year Frequent Attenders at
the end of the first year, for persistent and
non-Frequent Attenders at the end of the
third year.
CHAPTER 3
35
Box 1. Approach to the multivariable analysis
Loss to follow-up
368 patients (12%) were lost at some point over the two years of follow-up. We argued
that, in theory, a potential frequent attender might move out of the practice due to
dissatisfaction with care. The resulting selection bias may attenuate associations
found between the selected indicators and frequent attendance. We tested our
hypothesis in a multivariable logistic regression analysis with an indicator variable
“1 = moved house” and “0 otherwise” as the dependent variable and 9 independent
indicators (see below). Our hypothesis was not confirmed. On the contrary, we
found some evidence that those with at least one chronic somatic illness were less
likely to have moved out of the practice(odds ratio 0.73 (95%CI from 0.54 to 0.99));
all other associations were neither strong nor significant. These results support the
view that important selection bias is unlikely. Sixty-eight patients (2.2%) had died
over the two year follow-up period, but since, by definition, these patients cannot
become 3-year frequent attenders, selection bias by death is impossible.
Variable selection
The
1.
2.
3.
4.
5.
6.
7.
8.
9.
9 candidate predictors, modelled as 11 variables, included:
age at baseline (continuous),
sex,
number of problems on the problem list (continuous),
any of the three chronic somatic illnesses just mentioned (yes/no),
any psychological/social problem (yes/no),
any medically unexplained physical problem (yes/no),
psychoactive medication (yes/no),
average monthly number of prescriptions for antibiotics (0 = reference
category; 1-2; >2),
average monthly number of prescriptions for analgesics (0 = reference
category; 1-4; >4).
Figure 1. Flow diagram: Persistence of Frequent Attendance
3045
Frequent Attenders in 2003
2609
Enlisted in 2003, 2004 and 2005
2004
1008
FAs
2005
407
FAs = pFAs
36
1601
Non-FAs
2139
Non-pFAs
WHY DO THEY KEEP COMING BACK?
436
lost to follow-up in 2004 and 2005
32
110
died
moved out of practice
39
255
died
moved out of practice
Prevalences were calculated for that subset
of morbidity in which, according to the
literature, frequent attenders differ most
of normal attenders: diabetes mellitus,
chronic cardiovascular disease, chronic
respiratory disease, feelings of anxiety,
feelings of depression, addictive behaviour,
other psychological/psychiatric codes, all
social problems and medically unexplained
physical symptoms (MUPS)
2;4
. MUPS were
defined according to Robbins et al. and
had to comply with the definition of the
Problem List 19.
We determined the total number of
registered medical problems as indicator
of overall morbidity for the one and three
year periods.
Prescribed medication
The yearly number of prescriptions
for each patient was calculated
for the following: antibiotics,
painkillers, anxiolytics, hypnotics, and
antidepressants. We present the average
number of prescriptions of these 5 groups
of medications in non-Frequent Attenders,
1-year-Frequent Attenders and persistent
Frequent Attenders.
Statistical analysis
SPSS 14.0 for windows was used for the
statistical analysis. Differences between
patients groups were analysed using
X2 test. Statistical significance was set
at P<0.05. After checks for errors and
consistency, we assessed the potential for
selection bias due to loss to follow-up and
death.
Box 1 provides a description of our
approach. Statistical analyses were
performed in Stata (version 9.2).
Results
1-year-Frequent Attenders, persistent Frequent Attenders and GP-workload
The number of Frequent Attenders found
were as follows: 2003, 3,045 (10.6%); 2004,
2,897 (10.2%); 2005, 2,499 (9.3%). Of all
Frequent Attenders in 2003, 436 were
lost to follow-up because they had died
(71) or moved out of the practice (365)
before December 31, 2005. A multivariable
analysis showed (virtually) no signs of
selective loss to follow up for moving out
of the practice or for death (see Box 1). Of
the 2,609 Frequent Attenders in 2003 who
could be followed for three years, 1,008
were also Frequent Attender in 2004,
while 470 continued to be a Frequent
Attender in 2004 and 2005 and were a
persistent Frequent Attender according to
our definition. These persistent Frequent
Attenders comprised 1.6% of all enlisted
patients of 15 years and older in 2003 and
15.4% of all 1-year-Frequent Attenders in
2003. (See Figure 1) Compared with 1-yearFrequent Attenders, persistent Frequent
Attenders are older (see diagram 1). The
percentage of patients over the age of 65
years changed from 12.5% to 15.3%, the
percentage of patients in the age group 4564 years changed from 26.6% to 34% and
the percentage at 15-44 years decreased
from 60.9% to 50.6%.
The number of yearly consultations
varied substantially according to age. In
2003, the mean number of consultations
CHAPTER 3
37
Table 1.Mean number of GP-consultations per age group for non-Frequent Attenders,
1-year Frequent Attenders and persistent Frequent Attenders in 2003.
Non-FAs1
1yFAs2
pFAs3
15-44
1.01
6.5
8.47
45-64
1.61
8.6
10.98
65+
2.85
12.4
14.3
All patients >15
1.4
7.8
10.22
1. Non-frequent attenders
2. 1-year frequent attenders
3. persistent frequent attenders
Table 2. Morbidity of non-Frequent Attenders, 1-year Frequent Attenders and persistent Frequent Attenders: prevalence and relative difference (non-Frequent attenders
100)
Non-FAs1
1yFAs2
pFAs3
19120
2609
470
Diabetes mellitus
5.5
13.7
(250)
23.2
(421)
Chron. Cardiovasc. disease
13.7
23.4
(170)
37.7
(275)
Chron. resp. disease
9.8
17.8
(181)
27.2
(277)
(feelings of) Anxiety
1.8
4.7
(261)
9.4
(522)
(feelings of) Depression
3.2
6.4
(200)
8.7
(271)
Addictive behaviour
1.2
2.9
(241)
4.9
(408)
MUPS
6.8
13.1
(192)
25.3
(370)
Social problems
1.3
2.0
(153)
7.9
(607)
Psychological/psychiatric problems
9.2
20.6
(223)
37.0
(402)
Number of medical problems
1.16
2.00
(172)
3.52
(303)
1. Non-frequent attenders
2. 1-year frequent attenders
3. persistent frequent attenders
38
WHY DO THEY KEEP COMING BACK?
of non-Frequent Attenders (n= 19,120),
1-year Frequent Attenders (n= 2,609) and
persistent Frequent Attenders (n= 470)
were 1.4, 7.8 and 10.2 respectively (see
Table 1).
persistent Frequent Attenders, feelings of
anxiety is more prevalent than feelings of
depression. In 1-year Frequent Attenders
feelings of depression is more prevalent.
(See Table 2)
In 2003, for patients of 15 years and older,
80% of all face-to-face consultations
were with 37% of the registered patients.
Another 37% of patients had not visited
their GP at all during that year. In 2003,
the 3,045 Frequent Attenders (10.6%) were
responsible for 39% of all face-to-face
consultations; the 470 persistent Frequent
Attenders (1.6%) were responsible for 8% of
all consultations.
Number of prescriptions
Morbidity
Table 2 shows the distribution of 9 medical
problems or diagnoses across the three
categories of non- and frequent attenders.
The most important findings are the
substantial differences in morbidity for
social and psychological/psychiatric
problems and the high percentage of
persistent Frequent Attenders with
cardiovascular disease (37.7 %) and MUPS
(25.3 %). Persistent Frequent Attenders
present with more medical problems (3.52)
than 1-year Frequent Attenders (2.0) and
non-Frequent Attenders (1.16). Age follows
the predictable pattern of the older the
patient, the more consultations and the
more medical problems.
Compared with both other groups we see
in persistent Frequent Attenders especially
more social problems, more feelings of
anxiety and more addictive behaviour.
These persistent Frequent Attenders
differ less as far as the prevalence of
chronic somatic diseases is concerned. In
Compared to non- and 1-year-Frequent
Attenders, persistent Frequent Attenders
received more prescriptions for painkillers
antibiotics, antidepressants, anxiolytics
and sleeping tablets. Especially the high
number of prescriptions for painkillers
and anxiolytics in Frequent Attenders is
remarkable. (See Table 3)
Discussion
Main findings
When analysing the consultations of all
enlisted adult patients from 5 primary
health centres during 3 consecutive
years, we found that frequent attending is
usually a self-limiting condition. One out
every seven (15.4%) of patients who were a
Frequent Attender in 2003 (or 18% of those
FAs who were enlisted for all three years)
remained a Frequent Attender during
two consecutive years. These persistent
Frequent Attenders make up 1.6% of all
enlisted patients of 15 years and older in
2003. GPs held about seven times more
consultations with persistent Frequent
Attenders compared with non-Frequent
Attenders. Compared with non- and 1-yearFrequent Attenders, persistent Frequent
Attenders presented more social problems,
more feelings of anxiety, more addictive
behaviour and MUPS and they received
more prescriptions for psychotropic
medication.
CHAPTER 3
39
Table 3. Mean number of prescriptions in non-Frequent attenders, 1-year-Frequent
Attenders and persistent Frequent Attenders and relative difference (non-Frequent
attenders 100)
Non-FAs1
1yFAs2
pFAs3
19.120
2.609
470
Antibiotics
0.18
0.7
(388)
0.88
(488)
Painkillers
0.51
2.3
(457)
2.91
(570)
Anxiolytics
0.20
0.9
(450)
1.3
(650)
Hypnotics
0.19
0.7
(368)
0.99
(521)
Antidepressants
0.22
0.9
(409)
1.15
(523)
1. Non-frequent attenders
2. 1-year frequent attenders
3. persistent frequent attenders
Strength and limitations
An important strength of our study is
the size and the longitudinal character
of the dataset and the experience of
the participating GPs. Most GPs have
participated in the registration network
for over 10 years and are used to accepting
regular feedback on their registration
activities. Prescriptions are extracted
from the GPs’ Electronic Medical Record
and the number of actual prescriptions
is therefore reliable although the amount
of prescribed drugs is not. Prescription
data in general practice are generally
considered to be of higher quality
than data on diagnoses 20. As we used
routinely collected data and did not plan
any intervention in the normal practice
40
routine, our data reflects the day-to-day
business of general practice. Furthermore,
the demographic data are accurate.
A limitation of our study, however, is
that the data are restricted to “what the
GP knows and registered”. In particular,
the problem lists could be inflated (if
resolved problems are not removed) or
subject to underreporting. Underreporting
could be the case for patients with a low
consultation frequency – thus inflating the
contrast between Frequent Attenders en
non-Frequent Attenders – and for patients
who are relatively new in the practice.
As the problem lists of all participating
GPs are subject to evaluation on a regular
basis we think this problem is being dealt
with as well as possible 21. These problem
WHY DO THEY KEEP COMING BACK?
lists therefore seem quite valid 22;23. Many
patients who suffer from an incurable
disease become frequent attenders in the
months prior to their death. Although our
results may include terminally ill patients,
only few persistent frequent attenders
were incurably sick and died soon after the
study period (see box 1). The GP practices
in this study are situated in an urban area.
This means that the results cannot be
generalized and compared with practices
in more rural areas. Unfortunately, SocioEconomic-level and ethnicity were not
registered.
Relevant literature
There is substantial literature about the
characteristics and morbidity of 1-year
Frequent Attenders. The few longitudinal
studies show regression of attendance rates
to the mean in the longer run 15;15;16;24;25.
However, studies on persistent frequent
attendance used different definitions
of Frequent Attendance and lacked the
power to detect differences in morbidity
and prescriptions. Several trials have
been conducted to test interventions for
changing consultation behaviour and/
or morbidity of Frequent Attenders 12.
Only one study consisting of 2 RCTs
used frequent attendance over a period
of 2 years 13;14. All others included 1-yearFrequent Attenders 26-28. Although no study
found evidence to support the possibility
that healthcare utilization of Frequent
Attenders can be influenced, the study
that included Frequent Attenders for two
years did find evidence that treatment of
major depressive disorder in a subgroup of
depressed Frequent Attenders improved
the patients’ symptoms and quality of life.
Implications for future research or clinical
practice.
Knowing that frequent attendance is
predominantly a temporary phenomenon
and because of the continuous high
workload, the high prevalence of diseases
and the considerable use of medication,
we think that only persistent Frequent
Attenders deserve further attention.
Regarding the important role of
psychological and psychiatric problems
(especially anxiety) and social problems
in persisting frequent attendance it
seems logical to focus on these problems
in Frequent Attenders in order to try to
improve their quality of life and to prevent
the continuation of frequent consulting
behaviour.
Conclusion
We conclude that, compared with normal
attenders, 1-year-Frequent Attenders have
many somatic and psychiatric problems,
are prescribed much medication, including
psychotropic medication, and that they
constitute a substantial part of the clinical
work of a GP. One out of every seven
1-year Frequent Attenders persists to
consult frequently during a period of two
consecutive years. Compared to 1-year
Frequent Attenders, persistent Frequent
Attenders have even more consultations
with their GP, suffer from more morbidity
(especially social, psychiatric and MUPS)
and are prescribed more medication
(especially psychotropic medication).
CHAPTER 3
41
References
(1) Neal RD, Heywood PL, Morley S,
Clayden AD, Dowell AC. Frequency
of patients’ consulting in general
practice and workload generated
by frequent attenders: comparisons
between practices. Br J Gen Pract 1998;
48(426):895-898.
(2) Vedsted P, Christensen MB. Frequent
attenders in general practice care: a
literature review with special reference to
methodological considerations. Public
Health 2005; 119(2):118-137.
(3) Smits FT, Mohrs J, Beem E, Bindels
PJ, van Weert HC. Defining frequent
attendance in general practice. BMC
Fam Pract 2008; 9(1):21.
(4) Gill D, Sharpe M. Frequent consulters
in general practice: a systematic review
of studies of prevalence, associations
and outcome. J Psychosom Res 1999;
47(2):115-130.
(5) de Waal MW, Arnold IA, Eekhof JA,
Assendelft WJ, van Hemert AM. Followup study on health care use of patients
with somatoform, anxiety and depressive
disorders in primary care. BMC Fam
Pract 2008; 9(1):5.
(6) Little P, Somerville J, Williamson
I, Warner G, Moore M, Wiles R et al.
Psychosocial, lifestyle, and health status
variables in predicting high attendance
among adults. Br J Gen Pract 2001;
51(473):987-994.
(10) Hansagi H, Olsson M, Sjoberg S,
Tomson Y, Goransson S. Frequent use
of the hospital emergency department
is indicative of high use of other health
care services. Ann Emerg Med 2001;
37(6):561-567.
(11) Reid S, Wessely S, Crayford T, Hotopf
M. Frequent attenders with medically
unexplained symptoms: Service use and
costs in secondary care. British Journal
of Psychiatry 2002; 180(3):248-253.
(12) Smits FTM, Wittkampf KA, Schene
A, Bindels PJE, van Weert HCP.
Interventions on frequent attenders in
primary care. A systematic literature
review. Scand J Prim Health Care 2008;
26(2):111.
(13) Katzelnick DJ, Simon GE, Pearson
SD, Manning WG, Helstad CP, Henk HJ
et al. Randomized trial of a depression
management program in high utilizers
of medical care. Arch Fam Med 2000;
9(4):345-351.
(14) Simon GE, Manning WG, Katzelnick DJ,
Pearson SD, Henk HJ, Helstad CS. Costeffectiveness of systematic depression
treatment for high utilizers of general
medical care. Arch Gen Psychiatry 2001;
58(2):181-187.
(15) Ward AM, Underwood P, Fatovich
B, Wood A. Stability of attendance
in general practice. Fam Pract 1994;
11(4):431-437.
(7) Verhaak PF, Meijer SA, Visser AP,
Wolters G. Persistent presentation of
medically unexplained symptoms in
general practice. Fam Pract 2006;
23(4):414-420.
(16) Botica MV, Kovacic L, Tiljak MK, Katic
M, Botica I, Rapic M et al. Frequent
attenders in family practice in Croatia:
Retrospective study. Croatian Medical
Journal 2004; 45(5):620-624.
(8) Booth BM, Ludke RL, Wakefield DS,
Kern DC, du Mond CE. Relationship
between inappropriate admissions and
days of care: implications for utilization
management. Hosp Health Serv Adm
1991; 36(3):421-437.
(17) Carney TA, Guy S, Jeffrey G. Frequent
attenders in general practice: a
retrospective 20-year follow-up study. Br
J Gen Pract 2001; 51(468):567-569.
(9) Brandon WR, Chambers R. Reducing
emergency department visits among
high-using patients. J Fam Pract 2003;
52(8):637-640.
42
(18) Lamberts H, Wood M e. International
classification of primary care. Oxford:
Oxford University Press; 1988.
(19) Robbins JM, Kirmayer LJ, Hemami
S. Latent variable models of functional
somatic distress. J Nerv Ment Dis 1997;
185(10):606-615.
WHY DO THEY KEEP COMING BACK?
(20) Thiru K, Hassey A, Sullivan F.
Systematic review of scope and quality
of electronic patient record data in
primary care. BMJ 2003; 326(7398):1070.
(21) De LS, Stephens PN, Adal N, Majeed
A. Does feedback improve the quality of
computerized medical records in primary
care? J Am Med Inform Assoc 2002;
9(4):395-401.
(22) Brouwer HJ, Bindels PJ, van Weert
HC. Data quality improvement in general
practice. Fam Pract 2006; 23(5):529536.
(23) Jordan K, Porcheret M, Croft P.
Quality of morbidity coding in general
practice computerized medical records:
a systematic review. Fam Pract 2004;
21(4):396-412.
(24) Carney TA, Guy S, Jeffrey G. Frequent
attenders in general practice: a
retrospective 20-year follow-up study. Br
J Gen Pract 2001; 51(468):567-569.
(25) Andersson S-O, Lynoe N, Hallgren
C-G, Nilsson M. Is frequent attendance
a persistent characteristic of a patient?
Repeat studies of attendance pattern
at the family practitioner. Scandinavian
Journal of Primary Health Care 2004;
22(2):91-94.
(26) Christensen MB, Christensen B,
Mortensen JT, Olesen F. Intervention
among frequent attenders of the outof-hours service: a stratified cluster
randomized controlled trial. Scand J Prim
Health Care 2004; 22(3):180-186.
(27) Katon W, von Korff M, Lin E, Bush
T. A randomized trial of psychiatric
consultation with distressed high
utilizers. General Hospital Psychiatry /3;
14(2):86-98Record.
(28) Olbrisch ME. Evaluation of a stress
management program for high utilizers
of a prepaid university health service.
Med Care 1981; 19(2):153-159.
(29) Hernan MA, Hernandez-Diaz S, Robins
JM. A structural approach to selection
bias. Epidemiology 2004; 15(5):615-625.
CHAPTER 3
43
chapter 4
PREDICTABILITY OF PERSISTENT
FREQUENT ATTENDANCE: A
HISTORIC 3-YEAR COHORT STUDY
Frans T. Smits, Henk J. Brouwer,
Henk C. van Weert, Aart H. Schene,
Gerben ter Riet
Br. J. Gen. Pract.
2009 Feb; 59(559): e44-50
ABSTRACT
Background
Few patients who attend frequently continue to do so. While
transient frequent attendance may be readily explicable,
persistent frequent attendance often is not. Besides chronic
morbidity persistent frequent attenders may have hidden
illness. They increase GPs’ workload while reducing work
satisfaction. It is neither reasonable, nor efficient to target
diagnostic assessment and intervention at transient frequent
attenders.
Aim
To develop a prediction rule for selecting persistent frequent
attenders using readily available information from GPs’
electronic medical records.
Design
A historic 3-year cohort study
Method
We used data on 28,860 adult patients from 2003 to 2005.
Frequent attenders were patients whose attendance rate
ranked in the (age and sex adjusted) top 10 percent during
1 year (1-year frequent attenders) or 3 years (persistent
frequent attenders). Using bootstrapped multivariable
logistic regression analysis, we determined which predictors
contained information on persistent frequent attendance.
Results
Out of 3045 1-year frequent attenders 470 (15.4%) became
persistent frequent attender. The prediction rule could update
this prior probability to 3.3% (lowest value) or 43.3% (highest
value). However, the 10th and 90th centile of the posterior
probability distribution were 7.4% and 26.3%, respectively,
indicating that the model performs modestly. The area under
the receiver operating characteristics curve was 0.67 (95%
confidence limits 0.64 and 0.69).
46
WHY DO THEY KEEP COMING BACK?
Conclusions
Among 1-year frequent attenders, six out of seven are transient
frequent attenders. With the present indicators our rule performs
modestly in selecting those at risk of becoming persistent
frequent attender. More information or complementary
diagnostic tests seem needed to construct a rule with sufficient
performance for efficient risk stratification in clinical trials.
CHAPTER 4
47
Introduction
It is estimated that about 80% of a GP’s
clinical work is spent on 20% of his/
her patients, and that one in every seven
consultations is with patients who rank
in the top 3% of the attendance rate.1
Frequent attendance is often defined as
an age and sex-adjusted attendance rate
ranking in the top 10 centile within a time
frame of one year.2;3
Although longitudinal studies on frequent
attenders are scarce, we know that most
frequent attenders frequently attend
their GP for a short period of time only.4-7
It is neither reasonable, nor efficient to
target extensive diagnostic assessment,
monitoring, and intervention at transient
1-year frequent attenders
Trials on the effect of (mainly psychiatric)
interventions on morbidity and attendance
rates showed conflicting results.8 No
study showed convincing evidence that
an intervention improves quality of life or
morbidity of frequent attending primary
care patients, although an effect might
exist in a subgroup of depressed frequent
attenders.9-11 For this subgroup one trial
concluded that, in the year following the
intervention, patients in the intervention
Box 1. Approach to the multivariable analysis
Loss to follow-up
368 patients (12%) were lost at some point over the two years of follow-up.
We argued that, in theory, a potential frequent attender might move out of
the practice due to dissatisfaction with care. The resulting selection bias may
attenuate associations found between the selected indicators and frequent
attendance. We tested our hypothesis in a multivariable logistic regression
analysis with an indicator variable “1 = moved house” and “0 otherwise” as the
dependent variable and 9 independent indicators (see below). Our hypothesis
was not confirmed. On the contrary, we found some evidence that those with
at least one chronic somatic illness were less likely to have moved out of the
practice(odds ratio 0.73 (95%CI from 0.54 to 0.99)); all other associations were
neither strong nor significant. These results support the view that important
selection bias is unlikely. Sixty-eight patients (2.2%) had died over the two year
follow-up period, but since, by definition, these patients cannot become 3-year
frequent attenders, selection bias by death is impossible.
Variable selection
Frequent attendance during all three years, coded as 1, and zero otherwise was
the dependent variable. Independent variables: Continuous variables (age and the
number of problems on the GP’s problem list) were assessed for linear association
with the dependent variable using a graphical method proposed by Harrell to
avoid model mis-specification1. Presence of diabetes mellitus and/or chronic
respiratory illness and/or chronic cardiovascular illness was coded as 1, absence of
any of the above as zero (52 had all three, 316 had two, 891 one, 1786 none.
48
WHY DO THEY KEEP COMING BACK?
Similarly, presence of psychological and/or social problems including (feelings
of) anxiety, (feelings of) depression, and/or substance abuse were combined
(0 had all five, 1 had four, 33 three, 371 two, 285 one, and 2355 none). The use
of antidepressants, anxiolytics, and/or hypnotics was similarly combined (118
patients used all three types of drugs, 290 two, 408 one, and 2107 none).
Thus, the 9 candidate predictors, modelled as 11 variables, included:
1.
age at baseline (continuous),
2. sex,
3. number of problems on the problem list (continuous),
4. any of the three chronic somatic illnesses just mentioned (yes/no),
5. any psychological/social problem (yes/no),
6. any medically unexplained physical problem (yes/no),
7. psychoactive medication (yes/no),
8. average monthly number of prescriptions for antibiotics (0 = reference
category; 1-2; >2),
9. average monthly number of prescriptions for analgesics (0 = reference
category; 1-4; >4).
A final model was selected using bootstrapped forward stepwise logistic
regression analysis which was performed 100 times2. The p-values for entry
of variables into and removal from the model were 0.10 and 0.15, respectively.
Candidate predictors had to be selected 70 times or more to be eligible for the
final model. The final model’s fit was tested using the Hosmer-Lemeshow test
(10 groups) and accounted for intracluster correlation within general practices
by using robust variance estimation according to Huber and White3. Adding
interaction terms to the final model, we assessed subgroup effects in the
following subgroups requiring a p-value < 0.10 for significance: coexistence of a
documented somatic and psychosocial problem; coexistence of a psychosocial
problem and prescription of pain medication; female sex and prescription of pain
medication. The regression coefficients of the final model were used to compute
the probabilities of being a three year FA. The final model’s area under the
receiver operating characteristics (AUCROC) curve was calculated as a summary
of predictive power. The final model was fitted 500 times using bootstrap
methodology and the corresponding ROC curves were used to construct a
more robust confidence interval (CI) around the area under the curve thus
counteracting the influence of observations unique to our data set.
Reference List
1.
Harrell F. Regression Modeling Strategies. 2001. New York, Springer.
Ref Type: Generic
2. Sauerbrei W, Schumacher M. A bootstrap resampling procedure for
model building: application to the Cox regression model. Stat Med 1992;
11(16):2093-2109.
3. Williams RL. A note on robust variance estimation for cluster-correlated
data. Biometrics 2000; 56(2):645-646.
CHAPTER 4
49
Figure 1. Flow diagram: Persistence of Frequent Attendance
3045
Frequent Attenders in 2003
436
lost to follow-up in 2004 and 2005
2609
Enlisted in 2003, 2004 and 2005
2004
1008
FAs
2005
407
FAs = pFAs
1601
Non-FAs
2139
Non-pFAs
group had, on average, 47 depression-free
days more (5% CI from 27 to 68).11 There is
no evidence that it is possible to influence
health care utilization of frequent
attenders. All trials except one included
patients that attended frequently during
one year.12
Using information readily available in
GPs’ electronic medical records, we set
out to develop a prediction rule to help
GPs to identify, among 1-year frequent
attenders, those at extremely low or high
risk of becoming persistent frequent
attender. Such a rule, in addition to being
clinically useful, may also support the
selection of more homogeneous patient
groups in future randomized trials
among (subgroups of) persistent frequent
attenders.
50
32
110
died
moved out of practice
39
255
died
moved out of practice
Methods
Patient population
Five primary health care centres in
Amsterdam provided data for this study.
These centres participate in the GP-based
continuous morbidity registration network
of the Department of General Practice,
Academic Medical Centre - University
of Amsterdam. In this network EMR
data are extracted for research purposes.
The studied patients have a lower socioeconomic level, are of more non-western
descent and are slightly younger than
the Dutch population. The participating
GPs use a problem-oriented registration
method. For this study we used the
numbers of face-to-face consultations
with the GPs, the lists of current medical
problems as registered and coded by the
WHY DO THEY KEEP COMING BACK?
GP using the International Classification
of Primary Care (ICPC) and the number of
a selection of prescriptions of all patients
from 1 January 2003 through 31 December
2005.
Selection of one-year frequent attenders
and persistent frequent attenders
Frequent attenders were defined as those
patients whose attendance rate ranked
nearest to the top 10th centile of their sex
and age group (15-30; 31-45; 46-60; 61+)
.2;3 Frequent attenders were determined
for each of the years 2003, 2004 and 2005.
We took as a starting point the selected
frequent attenders of 2003. We defined
persistent frequent attenders as those
patients who were both registered and a
frequent attender during all three years.
Only face-to-face consultations with GPs
(consultations in the office and house calls)
were included. Consultations with other
practice staff were excluded because these
contacts are mostly initiated by the GP or
his/her staff and are related to controlling
chronic diseases. We determined the
mean number of consultations per age
and sex group for frequent attenders and
non-frequent attenders. Patients younger
than 15 years were excluded, because
their consultations often depend on their
parents.
Definition and extraction of
predictor information
In the problem-oriented approach to
medical record keeping a patient may
have a list of current medical problems,
also called problem list. Different from
the definition used in the UK, in the
Netherlands a current medical problem is
defined by the GP as:
1.
Any medical problem (disease or
complaint) which needs continuing
medical attention or monitoring.
2.
Any complaint or disease present for
more than 6 months (excluding all
(minor) short episodes).
Every problem on this list was coded by the
GPs using the International Classification
of Primary Care.13
Problem lists were extracted at the end
of 2003 and 2005. The prevalence of each
medical problem was calculated for 1-year
frequent attenders at the end of the first
year, for persistent frequent attenders
at the end of the third year. From the
electronic medical record we extracted
those prescriptions and medical problems
in which, according to the literature,
frequent attenders and non-frequent
attenders differed most: Number of
prescriptions (for analgesics, tranquilizers,
antidepressants and antibiotics), diabetes
mellitus, chronic cardiovascular disease,
chronic respiratory disease, (feelings of)
anxiety, (feelings of) depression, addictive
behaviour, any psychological/psychiatric
problem, all social problems and medically
unexplained physical symptoms (MUPS).
3;14
MUPS were defined according to
Robbins et al and complied with the
definition of the Problem List. 15 (See
appendix 1 for the used ICPC-codes)
Statistical analysis
We applied a multivariable analysis
using all above-mentioned information
CHAPTER 4
51
Table 1. Univariate associations of candidate predictors with persistent frequent
attendance (pFA), the dependent variable*.
Predictor
(crude)
Odds ratio
95% confidence
interval limits
Age¶
1.01
1.00 – 1.017
Sex, female
1.46
1.14 – 1.87
Number of active problems¶
1.21
1.16 – 1.25
Any chronic somatic illness
1.97
1.67 – 2.33
Any psychological problem
2.18
1.73 – 2.76
Medically unexplained complaint
2.02
1.55 – 2.62
Any psychoactive medication
1.50
1.21 – 1.86
Mean montly number of analgesic
prescriptions: 0
1
Reference
category
1-4
1.83
1.48 – 2.25
>4
2.56
1.98 – 3.30
1
Reference
category
1-2
1.21
0.99 – 1.48
>2
1.46
0.98 – 2.18
Mean monthly number of antibiotic
prescriptions: 0
*
¶
Based on 3045 observations; 470 pFAs (dependent variable = 1);
modelled as a continuous variable; All other variables were modelled as
dummies.
as predictors for persistence of frequent
attendance (See box 1). After checks for
errors and consistency we assessed the
potential for selection bias due to loss to
follow-up and death and used bootstrapped
stepwise logistic regression to select the
variables for the final model.
Box 1 provides a detailed description of our
analytical approach. Statistical analyses
were performed in Stata (version 9.2).
52
Results
(Persistent) frequent attenders
Of the 2609 frequent attenders in 2003
who could be followed for three years,
1008 (38.6%) also frequently attended in
2004, while 470 (18.0%) continued to do
so in 2004 and 2005 and were persistent
frequent attender according to our
definition (See figure 1). These persistent
frequent attenders comprised 1.6% of all
registered patients of 15 years and older in
2003. We studied selection bias, but found
(virtually) none for moving out of practice
or for death (see box 1).
WHY DO THEY KEEP COMING BACK?
Table 2. Associations between the five predictors retained in the final model and
persistent frequent attendance (pFA), the dependent variable.*
*
¶
Predictor
(adjusted)
Odds ratio
95% confidence
interval limits
Age ¶
0.99
0.98 – 1.00
Number of active problems ¶
1.13
1.05 – 1.22
Any chronic somatic illness
1.55
1.25 – 1.93
Any psychological problem
1.72
1.30 – 2.27
Mean montly number of analgesic
prescriptions: 0
1
Reference
1-4
1.77
1.41 – 2.23
>4
2.06
1.59 – 2.66
Based on 3045 observations; 470 pFAs (dependent variable = 1);
modelled as a continuous variable; All other variables were modelled as
dummies.
Prediction of persistent frequent attendance
Table 1 shows the univariate associations
of all candidate predictors with the
dependent variable, persistent frequent
attendance. Five predictors were
retained in the final model: age, the
number of problems on the GP’s problem
list, presence of any of three chronic
somatic illnesses (diabetes mellitus,
cardiovascular illness, and respiratory
illness), presence of a psychological/social
problem, and the use of pain medication
(Table 2). None of the interaction effects
proved significant at the 10% level. The
prior probability of 15.4% (470/3045) of
persistent frequent attendance could be
updated, using the model, to at best 3.3 %
(lowest value) or 43.3% (highest value).
The 10th and 90th centile of the posterior
probability distribution were 7.4% and
26.3%, respectively, indicating that the
model performs neither very good to rule
out persistent frequent attendance nor
to rule it in. The Hosmer-Lemeshow test
showed a p-value of 0.254, thus indicating
no strong evidence against good model
fit. As a summary of the model’s overall
discrimination, the AUCROC was 0.67
(bootstrapped bias corrected 95%CI from
0.64 to 0.69).
Discussion
Summary of main findings
In a historic 3-year cohort study, we found
that 15.4 percent of all 1-year frequent
attenders persisted in this behavior during
two consecutive years. Persistent frequent
attenders constituted less than 2% of all
registered patients 15+ of age. It proved
difficult to predict which 1-year frequent
attender persists in frequent consulting
behaviour using present readily available
information from GPs’ electronic medical
records.
CHAPTER 4
53
Strength and limitations of this study
Comparison with existing literature
An important strength of our study is
the size and the longitudinal character
of the dataset and the experience of
the participating GPs in recording and
coding the problem lists. Most GPs have
participated in the registration network
for over 10 years and are used to feedback
on their registration activity. The problem
lists have been monitored over the years
and differences between doctors have
been regularly discussed.16 Prescriptions
There is substantial literature about the
characteristics and morbidity of frequent
attenders.3;14 It is striking that almost
are extracted from the electronic medical
record and reflect the number of actual
prescriptions. Prescription data in general
practice may be generally considered to be
of higher quality than diagnosis-oriented
data.17 Our study was based on routinely
collected data reflecting everyday general
practice in The Netherlands. As far as
we know our study is the first predicting
persistence of frequent attendance with
information readily available to GPs.
Routine data that are readily available
have their limitations. For example,
problem lists may be inflated (by not
removing resolved problems) or subject
to underreporting. Moving out of practice
was a reason for exclusion, as followup of these patients was not possible.
Unfortunately, ethnicity and socio
economic-level are not (sufficiently)
registered in the current electronic
medical record. This precluded an analysis
of the interaction between ethnicity and
several other predictors to explore the role
of ethnicity in more detail.
54
all descriptive literature about frequent
attendance is produced in countries
with some kind of list system: the United
Kingdom, the Scandinavian countries, and
Health Maintenance Organizations in the
US.3;14 Most research on frequent attenders
however is cross-sectional and uses oneyear attendance rates. In particular, 1-year
frequent attenders have been reported to
use more analgesics, more antibiotics and
more tranquilizers.18;19 High attendance
rates are also found for patients with
medically unexplained somatic symptoms,
health anxiety and perceived poor
health.20-22 The few longitudinal studies
show attendance rates to regress to the
mean in the longer run, with only 20-30%
of frequent attenders continuing to attend
frequently in the following year. 4-7 These
studies on persistent frequent attendance
however use different definitions of
frequent attenders and lack the power to
detect factors associated with transient
frequent attendance becoming persistent.
In one study psychological distress, as
measured with two psychometric scales,
was found to increase the risk of future
daytime frequent attendance of adult
patients in family practice.23 As frequent
attendance proves to be mostly a transient
problem, interventions in 1-year frequent
attenders do not seem worthwhile.
Several trials have been conducted to
test interventions to change consultation
behaviour and/or morbidity of frequent
attenders.8 Only one study used frequent
WHY DO THEY KEEP COMING BACK?
attendance during 2 years.10;11 All others
included 1-year frequent attenders.24-26
Although none of the studies found
evidence that it is possible to influence
health care utilization by frequent
attenders, the one that included frequent
attenders during two years did find
evidence that treatment of major
depressive disorder in a subgroup of
depressed frequent attenders improved
their symptoms and quality of life.10;11
Implications for future research or clinical
practice
From the viewpoint of delivering good
care GPs do not have the reason or the
instruments to look for unmet health-care
needs among one year frequent attenders.
Both psychological and somatic chronic
diseases and complaints predispose
modestly a one-year frequent attender to
become a persistent frequent attender. However, as the predictive power (for
inclusion as well as for exclusion) of our
rule proved to be small there might be
other reasons for persistence of frequent
attendance. Because our study was not
a prospective cohort-study, we cannot
exclude the existence of ‘hidden morbidity’
among persistent frequent attenders.
Further studies are needed to decide,
first, whether there exist undiscovered
morbidity among persistent frequent
attenders and, secondly, whether it is
possible and worthwhile to construct a
rule with sufficient performance for risk
stratification by using more information
about the patient or from diagnostic tests.
Conclusion
Among 1-year frequent attenders, about
six out of seven are transient frequent
attenders. Information from GPs’
electronic medical records may be used
to identify those at low and higher risk of
becoming persistent frequent attender.
With the present indicators, available in
the electronic medical record, our rule
performs modestly in selecting those
at risk of becoming persistent frequent
attender.
Ethics committee
According to the Medical Research
Involving Human Subjects Act (WMO),
formal approval for this research project
by a Medical Ethics Committee was not
necessary. The academic GP network
extracts data according to strict guidelines
for the privacy protection of patients and
GPs. In addition we sought and obtained
permission for this work from the board of
the network
Competing interests
None.
Acknowledgments
We thank the GPs involved in the Network
of General Practitioners of the Academic
Medical Centre/University of Amsterdam
(HAG-net-AMC) for their continuous
efforts to keep the electronic medical
records updated.
CHAPTER 4
55
References
(1) Neal RD, Heywood PL, Morley S,
Clayden AD, Dowell AC. Frequency
of patients’ consulting in general
practice and workload generated
by frequent attenders: comparisons
between practices. Br J Gen Pract 1998;
48(426):895-898.
(2) Smits FT, Mohrs JJ, Beem EE, Bindels
PJ, van Weert HC. Defining frequent
attendance in general practice. BMC
Fam Pract 2008; 9(1):21.
(3) Vedsted P, Christensen MB. Frequent
attenders in general practice care: a
literature review with special reference to
methodological considerations. Public
Health 2005; 119(2):118-137.
(4) Ward AM, Underwood P, Fatovich
B, Wood A. Stability of attendance
in general practice. Fam Pract 1994;
11(4):431-437.
(5) Botica MV, Kovacic L, Tiljak MK, Katic
M, Botica I, Rapic M et al. Frequent
attenders in family practice in Croatia:
Retrospective study. Croatian Medical
Journal 2004; 45(5):620-624.
(6) Carney TA, Guy S, Jeffrey G. Frequent
attenders in general practice: a
retrospective 20-year follow-up study. Br
J Gen Pract 2001; 51(468):567-569.
pattern at the family practitioner.
Scandinavian Journal of Primary Health
Care 2004; 22(2):91-94.
(7) Andersson S-O, Lynoe N, Hallgren
C-G, Nilsson M. Is frequent attendance
a persistent characteristic of a patient?
Repeat studies of attendanceUniversity
Press; 1988.
(8) Smits FT, Wittkampf KA, Schene AH,
Bindels PJ, van Weert HC. Interventions
on frequent attenders in primary care.
A systematic literature review. Scand J
Prim Health Care 2008; 26(2):111-116.
(9) Schreuders B, van MH, Smit J, Rijmen
F, Stalman W, van OP. Primary care
patients with mental health problems:
outcome of a randomised clinical trial. Br
J Gen Pract 2007; 57(544):886-891.
56
(10) Simon GE, Manning WG, Katzelnick DJ,
Pearson SD, Henk HJ, Helstad CS. Costeffectiveness of systematic depression
treatment for high utilizers of general
medical care. Arch Gen Psychiatry 2001;
58(2):181-187.
(11) Katzelnick DJ, Simon GE, Pearson
SD, Manning WG, Helstad CP, Henk HJ
et al. Randomized trial of a depression
management program in high utilizers
of medical care. Arch Fam Med 2000;
9(4):345-351.
(12) Smits FTM, Wittkampf KA, Schene
A, Bindels PJE, van Weert HCP.
Interventions on frequent attenders in
primary care. A systematic literature
review. Scand J Prim Health Care 2008;
26(2):111.
(13) Lamberts H, Wood M e. International
classification of primary care. Oxford:
Oxford
(14) Gill D, Sharpe M. Frequent consulters
in general practice: a systematic review
of studies of prevalence, associations
and outcome. J Psychosom Res 1999;
47(2):115-130.
(15) Robbins JM, Kirmayer LJ, Hemami
S. Latent variable models of functional
somatic distress. J Nerv Ment Dis 1997;
185(10):606-615.
(16) Brouwer HJ, Bindels PJ, Weert HC.
Data quality improvement in general
practice. Fam Pract 2006; 23(5):529536.
(17) Thiru K, Hassey A, Sullivan F.
Systematic review of scope and quality
of electronic patient record data in
primary care. BMJ 2003; 326(7398):1070.
(18) Bergh H, Marklund B. Characteristics of
frequent attenders in different age and
sex groups in primary health care. Scand
J Prim Health Care 2003; 21(3):171-177.
(19) Vedsted P, Sorensen HT, Mortensen
JT. Drug prescription for adult
frequent attenders in Danish general
practice: a population-based study.
Pharmacoepidemiol Drug Saf 2004;
13(10):717-724.
WHY DO THEY KEEP COMING BACK?
(20) Little P, Somerville J, Williamson
I, Warner G, Moore M, Wiles R et al.
Psychosocial, lifestyle, and health status
variables in predicting high attendance
among adults. Br J Gen Pract 2001;
51(473):987-994
(30) Williams RL. A note on robust
variance estimation for cluster-correlated
data. Biometrics 2000; 56(2):645-646.
(21) Verhaak PF, Meijer SA, Visser AP,
Wolters G. Persistent presentation of
medically unexplained symptoms in
general practice. Fam Pract 2006;
23(4):414-420.
(22) de Waal MW, Arnold IA, Eekhof JA,
Assendelft WJ, van Hemert AM. Followup study on health care use of patients
with somatoform, anxiety and depressive
disorders in primary care. BMC Fam
Pract 2008; 9(1):5.
(23) Vedsted P, Fink P, Olesen F, MunkJorgensen P. Psychological distress
as a predictor of frequent attendance
in family practice: a cohort study.
Psychosomatics 2001; 42(5):416-422.
(24) Christensen MB, Christensen B,
Mortensen JT, Olesen F. Intervention
among frequent attenders of the outof-hours service: a stratified cluster
randomized controlled trial. Scand J Prim
Health Care 2004; 22(3):180-186.
(25) Katon W, Von KM, Lin E, Bush T, Russo
J, Lipscomb P et al. A randomized trial of
psychiatric consultation with distressed
high utilizers. Gen Hosp Psychiatry 1992;
14(2):86-98.
(26) Olbrisch ME. Evaluation of a stress
management program for high utilizers
of a prepaid university health service.
Med Care 1981; 19(2):153-159.
(27) Hernan MA, Hernandez-Diaz S,
Robins JM. A structural approach to
selection bias. Epidemiology
2004;
15(5):615-625.
(28) Harrell F. Regression Modeling
Strategies. 2001. New York, Springer.
Ref Type: Generic
(29) Sauerbrei W, Schumacher M. A
bootstrap resampling procedure for
model building: application to the
Cox regression model. Stat Med 1992;
11(16):2093-2109.
CHAPTER 4
57
chapter 5
PREDICTABILITY OF PERSISTENT
FREQUENT ATTENDANCE IN
PRIMARY CARE: A TEMPORAL
AND GEOGRAPHICAL VALIDATION
STUDY.
Frans T. Smits, Henk J. Brouwer,
Koos H. Zwinderman , Marjan van
den Akker, Ben van Steenkiste, Jacob
Mohrs, Aart H. Schene, Henk C. van
Weert, Gerben ter Riet
PLoS One. 2013 Sep 5;8(9):e73125.
ABSTRACT
Background
Frequent attenders are patients who visit their general
practitioner exceptionally frequently. Frequent attendance
is usually transitory, but some frequent attenders become
persistent. Clinically, prediction of persistent frequent
attendance is useful to target treatment at underlying diseases
or problems. Scientifically it is useful for the selection of highrisk populations for trials. We previously developed a model to
predict which frequent attenders become persistent.
Aim
To validate an existing prediction model for persistent
frequent attendance that uses information solely from General
Practitioners’ electronic medical records.
Method
We applied the existing model (N=3,045, 2003-2005) to
a later time frame (2009-2011) in the original derivation
network (N=4,032, temporal validation) and to patients of
another network (SMILE; 2007-2009, N=5,462, temporal and
geographical validation). Model improvement was studied
by adding three new predictors (presence of medically
unexplained problems, prescriptions of psychoactive drugs
and antibiotics). Finally, we derived a model on the three data
sets combined (N=12,539). We expressed discrimination using
histograms of the predicted values and the concordancestatistic (c-statistic) and calibration using the calibration slope
(1=ideal) and Hosmer-Lemeshow tests.
Results
The existing model (c-statistic 0.67) discriminated moderately
with predicted values between 7.5 and 50 percent and
c-statistics of 0.62 and 0.63, for validation in the original network
and SMILE network, respectively. Calibration (0.99 originally)
was better in SMILE than in the original network (slopes 0.84
and 0.65, respectively). Adding information on the three new
predictors did not importantly improve the model (c-statistics
0.64 and 0.63, respectively). Performance of the model based
on the combined data was similar (c-statistic 0.65).
60
WHY DO THEY KEEP COMING BACK?
Conclusion
This external validation study showed that persistent frequent
attenders can be prospectively identified moderately well
using data solely from patients’ electronic medical records.
CHAPTER 5
61
Introduction
Some patients visit their general
practitioner (GP) relatively often. This
frequent attendance is mostly defined
as an age- and sex-adjusted attendance
rate ranking in the top 10% within a time
frame of 1 year.1;2 Frequent attenders (FAs)
are responsible for 39% of all face-to-face
consultations of their GPs and persistent
frequent attenders (those 1.6 percent who
frequently attend during three consecutive
years or more; pFA) are responsible for
about 8% of face-to-face consultations.3
Frequent attenders and, in particular,
persistent frequent attenders have
relatively many somatic, psychiatric and
social problems.3
Although longitudinal studies on frequent
attenders are scarce, it is known that
most frequent attenders frequently
attend their GPs for a short period of time
only.3-7 It seems neither reasonable, nor
efficient to target extensive diagnostic
assessment, monitoring, and intervention
at transient 1-year frequent attenders.
However, patients who continue to
attend frequently may require special
attention, and potential effective
interventions should probably be targeted
at this group. Prediction of persistent
frequent attendance may therefore be
clinically useful if effective treatment of
underlying medical problem and (thereby)
prevention of this persistence is available.
Scientifically a prediction model for
pFAs may be useful to help select more
homogeneous high-risk populations
for future randomized trials or support
efficient subgroup analysis.8;9
62
A review on the effects of (mainly
psychiatric) interventions on morbidity
and attendance rates has shown conflicting
results.10 One out of a total of 5 trials
showed that a depression management
program improved quality of life and the
number of depression-free days of patients
frequently attending the GP during two
years.11;12 None of the included trials
showed an effect on healthcare utilization
of frequent attenders. All trials, except the
one mentioned above, included patients
that attended frequently during just one
year.12 Therefore, some negative findings
may have been due to strong regression
to the mean and spontaneous ‘recovery’,
making it difficult to detect any effects.
A more recent Spanish study in 1-year
FAs showed that a 15 hours’ training of
GPs, which incorporated biopsychosocial,
organizational, and relational approaches
resulted in a reduction of attendance rates
(mean number of annual contacts in the
intervention group 13.1 against 19.4 in the
usual care group).13
Using information that was readily
available in GPs’ electronic medical
records (EMR), we developed a prediction
rule to help GPs identify, among 1-year
frequent attenders, those at extremely
low or high risk of becoming persistent
frequent attenders (see table 1).14 With the
indicators available in the EMR presented
in our previous study, our rule was
modestly effective in selecting those at risk
of becoming persistent frequent attenders
(AUC 0.67; CI 0.64-0.69).
Since many diagnostic indices perform
worse in a different population, (external)
validation in a different primary care
WHY DO THEY KEEP COMING BACK?
Table 1. Original prediction rule14: Associations between five predictors and persistent
frequent attendance (pFA), the dependent variable.*
*
¶
Predictor
(adjusted)
Odds ratio
95% confidence
interval limits
Age¶
0,99
0,98 – 1,00
Number of active problems¶
1,13
1,05 – 1,22
Any chronic somatic illness
1,55
1,25 – 1,93
Any psychological problem
1,72
1,30 – 2,27
Mean montly number of analgesic
prescriptions: 0
1
Reference
1-4
1,77
1,41 – 2,23
>4
2,06
1,59 – 2,66
Based on 3045 observations; 470 pFAs (dependent variable = 1);
modeled as a continuous variable; All other variables were modeled as
dummies.
population is warranted before the use
in clinical practice is advocated.15 In
this study we temporally (another time
frame) and geographically (another area)
validated our previously derived prediction
model for pFA-ship using information
solely from GPs’ EMR and looked for
opportunities to improve it with extra
patient information.
Because they are more prevalent in
pFAs and theoretically likely to increase
persistence of frequent attendance, we
added 4 extra variables (sex, presence
of medically unexplained symptoms,
prescriptions of psychoactive drugs and
antibiotics) to the original model and
tested it for improvement on the 3 cohorts
(including original cohort).3;16;17
We also explored building a more robust
model based on the combined data of all
three datasets.
Methods
Ethics statement
The study was conducted according to
the Dutch legislation on data protection
(Ministry of Justice, the Netherlands).
Ethics approval was provided through
the Medical Ethics Review Committee
of the Academic Medical Center of the
University of Amsterdam (letter W
12_259#12.27.0295), stating that “the
Medical Research involving human
subjects Act (WMO) does not apply to this
study and that an official approval of this
study by our committee is not required”.
Patient population
To validate our prediction rule we used
two primary care cohorts:
1.
Temporal validation; Six primary
healthcare centres in Amsterdam and
Diemen provided data for the second
CHAPTER 5
63
cohort. These centers participate
in the GP-based continuous
morbidity registration network of
the Department of General Practice,
Academic Medical Center - University
of Amsterdam.14 This cohort was
an enlarged version of our original
cohort (4,032 vs. 3,045 adult patients)
in a more recent time frame (20092011). See our original article for more
details.14
2.
Geographical and temporal validation;
All primary healthcare centres of the
Eindhoven Corporation of Primary
Health Care Centres in Eindhoven
provided data for the first cohort.
These centers participate in the GPbased Study on Medical Information
and Lifestyles Eindhoven (SMILE) of
the Department of General Practice
of Maastricht University.18 The
patients studied were of average
socioeconomic level, of more western
descent, and slightly older than the
general Dutch population. This cohort
consisted of 5,462 patients who were
FA in 2007 and we followed them to
2009.
In both networks, EMR data are extracted
for research purposes. The participating
GPs use a problem-oriented registration
method. This study used the numbers of
face-to-face consultations with the GPs,
the lists of current medical problems
as registered and coded by the GPs
using the International Classification of
Primary Care (ICPC), and a selection of
prescriptions of all patients.19
Selection of one-year frequent attenders and
persistent frequent attenders
In all cohorts, frequent attenders were
defined as those adult patients whose
attendance rates ranked nearest to the
top 10th centile of their age group (15–30,
31–45, 46–60, 61 years) separate for
men and women.1;2 Persistent frequent
attenders were defined as those patients
who were both registered and frequently
attending during 3 consecutive years.
Figure 1. Flow chart of the 3 databases.
AMSTERDAM I
AMSTERDAM II
FAs1 in 2003
N= 3045
FAs in 2009
N= 4032
LFU2:436:
•
71 (died)
•
365 (moved house)
pFAs3
(2003-2005)
n= 470
64
WHY DO THEY KEEP COMING BACK?
LFU: 608
•
147 (died)
•
461 (moved house
pFAs
(2009-2011)
n= 629
Only face-to-face consultations with GPs
(consultations in the office and house calls)
were included. Consultations with other
practice staff were excluded because, in
the practices involved, such consultations
are mostly initiated and planned by GPs
or their staff and cover mainly chronic
disease programs.
Definition and extraction of predictor information
We considered potential predictors of
persistent frequent attendance which
were easily obtainable in all three cohorts
(see table 2). In the problem-oriented
approach to medical record keeping, a
patient may have a list of current medical
problems, also called a problem list. In the
Netherlands, a current medical problem is
defined as:
•
Any disease or complaint which,
according to the GP, needs continuing
medical attention or monitoring and/
or
SMILE
FAs in 2007
N= 5462
LFU: 1994
•
Any disease or complaint present for
more than 6 months and/or
•
Recurrent medical problems (more
than 4 episodes per half year).20
Every problem on this list was coded by
the GPs using the ICPC.19 The prevalence
of each medical problem was calculated at
the end of the year. Medically Unexplained
Symptoms (MUS) were defined according
to Robbins et al.21 See appendix 1 for a list
of the selected ICPC-codes.
Statistical analysis:Validation of model to
predict persistent frequent attendance
The prediction model, to be validated in
the present analysis, has been derived in
our previous study using (bootstrapped)
multivariable logistic regression analysis.
This model included the variables: age
(Odds ratio (OR) 0.99 per year), number
of active problems (OR 1.13 per additional
problem), presence of any chronic somatic
problems (OR 1.55), any psychological
problems (OR 1.72) and the monthly
1. FAs = frequent attenders during 1 year
2. LFU= Lost to follow up
3. pFAs= persistent frequent attenders;
frequent attender during 3
consecutive years
4. In the SMILE cohort patients who
changed GP within the same primary
care organisation were not properly
registered. Unfortunately no
distinction was made between moving
house or death.
pFAs
(2007-2009)
n= 1107
CHAPTER 5
65
Figure 2.
500
Amsterdam I
Histograms showing the predicted values
based on the model predictions for the
three cohorts: Amsterdam I (the original
(derivation) cohort) and the two external
validation cohorts, Amsterdam II and
SMILE.
400
300
200
The graphs illustrate the slight overoptimism of the original model and the
shrinkage of the distribution, that is,
the tails of the Amsterdam II and SMILE
cohort distributions are slightly closer to
the center and predicted values smaller
than 7 percent or greater than 54% no
longer occur on external validation. Y
-axes are frequencies.
100
0
0
500
1
2
3
4
5
6
Amsterdam II
400
300
200
100
0
0
500
1
2
3
4
5
6
SMILE
400
300
200
100
0
0
66
1
2
3
4
5
6
WHY DO THEY KEEP COMING BACK?
Figure 3.
4
In these Hosmer-Lemeshow
calibration plots, each circle
represents the observed mean
probability of becoming a persistent
frequent attender (pFA) within a
decile of patients after all patients
were ordered from lowest to highest
predicted probability.
Observer (proportion)
Amsterdam I
Hosmer Lemeshow plots: Observed
versus predicted risk for persistent
Frequent Attendance.
3
2
1
As usual, the Hosmer Lemeshow
calibration top plot shows a good
match between predicted and
observed risks in the derivation cohort
(Amsterdam I) as all circles are close
to the diagonal of perfect calibration.
0
0
1
2
3
4
4
On external validation in the
Amsterdam II cohort (middle graph),
eight out of ten predicted values were
higher than those observed and those
in deciles 5, 8 and 10 (extreme right
hand circle) in particular.
On external validation in the SMILE
cohort, predicted probabilities
matched the observed ones well,
except for the two highest deciles,
9 and 10. The small p-values are also
partly caused by the large sample size
so that small mismatches become
statistically significant. Note that
the vertical distance to the diagonal
represents the mismatch between
predicted and observed pF A
probabilities.
Amsterdam I to Amsterdam II
p < 0,001
3
2
1
0
0
1
2
Predicted (proportion)
Observer (proportion)
4
3
4
3
4
Amsterdam I to SMILE
p = 0,003
3
2
1
0
0
1
2
Predicted (proportion)
CHAPTER 5
67
Table 2. Comparison of the three databases
A’dam I #
A’dam II
SMILE
Time period
2003-2005 2009-2011
2007-2009
Patients n
28,680
40,320
54,620
Frequent attenders n
3,045
4,032
5,462
Number of Frequent Attenders n(%)
470 (15%)
629 (16%)
1,107 (20%)
Lost to follow up’ n(%)
436 (14.3)
608 (15.1)
199 (3.6)
Mean age (SD)
42.6 (18.2)
47.9 (18.5)
45.9 (18.8)
1,566 (51)
2,179 (54)
2,640 (48)
10.2
11.8
7.7
Active problems (Frequent Attenders),n(SD)
2.03 (2.16)
2.68 (2.70)
1.70 (1.55)
Any chronic somatic illness n(%)
1,259(41)
1,906(47)
2,768 (50)
Any psychological or social problem n(%)
690 (23)
1,028 (26)
2,781 (51)
Any Medically Unexplained Symptoms n(%)
391 (13)
610 (15)
98 (2)
Mean monthly number of analgesic
prescriptions: 0
1,484(49)
1,889 (49)
2,759 (51)
1-4
1,061 (35)
1,446 (36)
>4
500 (16)
597 (15)
2,703(50)
Any psychoactive medication n (%)
938 (31)
1,230 (31)
1,775 (33)
Mean monthly number of antibiotic
prescriptions: 0
1,976 (65)
2,374 (59)
3,120 (57)
1-2
814 (27)
1,172 (29)
>2
255 (8)
486 (12)
Females n(%)
*
Consultations of pFAs (mean n/year)
Problems on the problem list
n
SD
pFAs
#
*
68
2,342 (43)
indicates number
indicates standard deviation
indicates persistent Frequent attenders, frequent attenders during 3 years
Respectively in 2005 (A’dam I), 2011 (A’dam II) and 2009 (SMILE).
A’dam indicates the Amsterdam I cohort
Respectively in 2005 (A’dam I), 2011 (A’dam II) and 2009 (SMILE).
WHY DO THEY KEEP COMING BACK?
number of analgesic prescriptions (> 4: OR
2.06).14 See Table 1.
We first validated the original prediction
model through the assessment of its
discrimination (predictive values,
c-statistic and corresponding 95%
confidence intervals) and calibration
(slope and corresponding 95% confidence
intervals, and Hosmer Lemeshow plots and
tests comparing predicted versus observed
risk). A calibration slope of 1 indicates that
predicted probabilities match observed
risks perfectly (100%), a slope <1 indicates
over-prediction.22-24 We repeated this
analysis for an extended model with four
extra variables.
Recalculation of the prediction model in the
combined cohorts
Recalculation of the original model was
performed using all pooled subjects
from the three cohorts (update cohort,
n= 12,539). Regression coefficients were
obtained using logistic regression with
persistent frequent attendance as the
dependent variable and age, number of
active problems, any chronic somatic
problem, any psychological problem
and the monthly number of analgesic
prescriptions as predictors. Analyses
were performed using SPSS for windows,
version 20.
Results
Prediction of persistent frequent attenders
Table 2 and figure 1 show the general
characteristics of the three cohorts. The
persistent frequent attenders comprised
15-20% of all registered adult patients in all
cohorts. Compared with both Amsterdam
cohorts, patients in the SMILE cohort
were relatively more often pFAs, had less
loss to follow-up, fewer active problems,
more psychological problems and fewer
medically unexplained symptoms. In
SMILE the mean number of prescriptions
for analgesics and antibiotics was higher,
but lower for psychoactive medication.
In the SMILE cohort patients who
changed GP within the same primary care
organization were not registered as having
moved house. Unfortunately, no distinction
was made between moving house or death.
We corrected for loss to follow (LFU) up by
measuring the prognostic index with and
without correction for LFU. The results did
not materially change. See appendix 2.
Table 3 shows the results of the original
prediction rule in the Amsterdam II
cohort and the SMILE cohort. Using the
original regression weights with shrunken
coefficients the c-statistics were 0.67
(95% confidence interval (CI) 0.64-0.69)
in the original database, 0.62 (CI: 0.600.65) in the Amsterdam II cohort and
0.63 (CI: 0.61-0.65) in the SMILE cohort.
Re-estimation of the regression weights
did not change the results much (table 3).
As expected in low-prevalence settings,
negative predictive values were high, but
all other indices were of moderate size.
Figure 2 shows the predictive values
(predicted probabilities of becoming
pFA) based on the prediction model in
the three cohorts. Predictive values on
external validation (AMC II and SMILE)
lay between 7.5 percent and 54 percent,
slightly more conservative than those in
the original cohort (3.3 and 59%).
CHAPTER 5
69
Table 3. Discrimination and calibration on external validation of the original prognostic index to the Amsterdam II and SMILE cohorts.
number of FAs/ pFAsa
A’dam I
A’dam II
SMILE
3,045 / 470
4,032 / 629
5,462 / 1107
Using the original regression weights#
C-statistics (95% CI)b
0.67
Positive predictive value
Negative predictive value
0.64-0.69
0.62
0.60-0.65 0.63
0.27
0.22
0.27
0.90
0.89
0.86
0.61-0.65
Re-estimation of the regression weights
C-statistics (95% CI)
0.67
0.64-0.69
0.64
0.61-0.66
0.63
Positive predictive value
0.27
0.22
0.27
Negative predictive value
0.90
0.89
0.86
0.62-0.65
Adding 3 other predictor variablesc
C-statistics (95% CI)
0.67
0.65-0.70
0.65
0.62-0.67
0.65
Positive predictive value
0.26
0.23
0.26
Negative predictive value
0.90
0.89
0.88
0.656 0.07
0.83
0.63-0.66
Calibration of the original prognostic indexd
Slope (SE)
a
0.99
0.08
0.06
(p)FAs: (persistent) Frequent Attenders: frequently attending patients during 1
and 3 years, respectively.
Concordance statistics (95% confidence interval)
Any medically unexplained symptoms; any psychoactive
medication; mean monthly number of prescriptions of antibiotics
Ideally, the slope should be 1, which indicates perfect calibration of predicted
and observed risks. Values <1 indicate overoptimism (shrinkage), that is, high
risks are overestimated, while low risks are underestimated
using a model with shrunken coefficients of the original model (shrinkage
coefficient 0.993)Sensitivity, specificity, likelihood ratios and positive
and negative predictive values were calculated at the value where their sum
was maximal (Q-point of the ROC curve).
b
c
d
#
70
WHY DO THEY KEEP COMING BACK?
The effect of clustering on the health
center level was negligible with intraclass
correlations of 0.02-0.06 and almost no
change of the regression weights. See the
supporting file (Table S2).
Adding three predictors (any MUS, any
psychoactive medication and the mean
monthly number of antibiotic prescription)
hardly changed the performance
(c-statistics Amsterdam II 0.65; CI 0.620.67; SMILE 0.65; CI 0.63-0.66) (see table
3).
The Hosmer Lemeshow plots showed
modest calibration with underestimation
of the probability to become pFA (see
Figure 1, upper right circles which tend
to fall below the line y=x). This was
confirmed by the small p-values indicating
large discrepancies between predicted and
observed risks. (See figure 3)
Updated prediction model
We updated the prediction model using all
pooled patients of the three cohorts (12,539
patients). Pooling the three data sets and
fitting a new model did not materially lead
to important improvements (c-statistic
0.65; CI: 0.63-0.66).
Discussion
Summary of main findings
External validation in time and place of an
existing prediction model for persistent
frequent attendance in primary care
showed that its discrimination remained
stable while calibration was reduced for
the higher predictions in particular. Model
extension with three plausible predictors
not previously included hardly improved
model performance.
Strength and limitations of the study
Important strengths of this study are
the size and the longitudinal character
of the datasets and the experience of the
participating GPs in recording and coding
the problem lists.20 The SMILE cohort had
relatively little loss to follow-up (mostly
because fewer patients ‘moved house’
because of registration limitations) and
more pFAs. Knowing the way GPs and
practice staff cooperate in the Netherlands,
replacement of GP consultations by
practice staff consultation (off-utilization
bias) will be very limited.25 Prescriptions
are extracted from the electronic medical
record and reflect the number of actual
prescriptions. Prescription data in general
practice may generally be considered to be
of higher quality than diagnosis-oriented
data.26 The higher prescription rates of
analgesics and antibiotics and the lower
rates for psychoactive medication are
therefore difficult to understand and may
reflect the different patient populations in
both cities and/or different prescription
habits of the local GPs. Wennberg
showed that everyday clinical practice
is characterized by wide geographical
variations that cannot be explained by
illness severity or patient preference.27;28
The present retrospective study was based
on routinely collected data and therefore
reflects everyday general practice in the
Netherlands. Because we wanted to predict
patient behavior, we only used GP-patient
consultations and not planned monitoring
consultations for chronic diseases with
other primary care staff.
CHAPTER 5
71
However, there are also some limitations.
First, there are differences between the
Amsterdam and SMILE cohort which
may have influenced the predictive
performance of our rule. In general, within
a General Practice Research Network, one
distinguishes four categories of factors
to explain morbidity and prescription
differences: “healthcare system”,
“methodological characteristics of the
network”, “general practitioner”, and the
“patient”. These factors and sub-factors
are often interrelated.29 The differences
between the cohorts in Amsterdam and
Eindhoven may partly be explained by
methodological differences (the shorter
existence of SMILE (fewer active
problems) and coding agreements (fewer
MUS, but more psychological codes in
SMILE)), different populations of general
practitioners (shorter experience in coding
problems in SMILE) and patient factors
(more stable population; more females in
SMILE). However, socio-demographic
characteristics of populations cannot
explain the differences in morbidity
estimations among these cohorts.30
The problem lists may suffer from
overreporting (by not removing resolved
problems, for instance, depression) and
underreporting (for instance personality
disorder). This may have diminished the
predictive power of “any psychological
problem”. Moving out of practice was a
reason for exclusion, as follow-up of these
patients was not possible. Compared with
SMILE the loss to follow-up rate was
higher in Amsterdam, but in the original
study this did not result in selection bias.14
Finally, the presumed higher registration
72
quality in these academic networks
may diminish the generalizibility of a
prediction rule derived in these networks
to other practices.
Formal external validation of prediction
models while important is still scarce.
If the original prediction model had had
excellent performance, one may expect
worse performance on external validation.
External validation usually reveals the
so-called over-optimism of the original
model.31 Our original model performed
moderately well and its discrimination
performance remained largely intact,
although the predicted risks did not match
the observed risks very well for the more
extreme risk predictions. Using shrunken
coefficients of the original model had a
very limited effect and there was no sign
of selective loss to follow-up. Finally,
accounting for clustering within health
care center had little impact.
Comparison with existing literature
The few longitudinal studies about
frequent attendance showed that
attendance rates tend to regress to the
mean over time, with only 20–30% of
frequent attenders continuing to attend
frequently in the following year.4-6;32
However, these studies of persistent
frequent attendance used different
definitions of frequent attenders and
lacked the power to detect factors
associated with transient frequent
attendance becoming persistent. Vedsted
found that psychological distress, as
measured with two psychometric scales,
increased the risk of future daytime
frequent attendance of adult patients
WHY DO THEY KEEP COMING BACK?
in family practice.16 Another, small,
prospective study (85 primary healthcare
patients of working-age) detected as risk
factors for persistent frequent attendance
female sex, body mass index above 30,
former frequent attendance, fear of death,
alcohol abstinence, low patient satisfaction,
and irritable bowel syndrome.33 Smits et al
showed that with the indicators currently
present in Dutch electronic medical
records, a rule performed modestly in
selecting those more likely to become
persistent frequent attenders.14
beyond multiple univariable subgroup
analyses.9;35
Conclusion
Prediction of persistent frequent
attendance using data solely from EMRs
currently available in the Netherlands
may be moderately helpful in identifying
those patients at high (or low) risk of
becoming persistent frequent attenders.
Better predictors are needed to improve
prediction.
Implications for clinical practice
Acknowledgments
After validation and updating the existing
rule only predicts persistence of frequent
attendance moderately. For clinical use
this rule has some significance to predict
which 1yFAs have more risk to become a
persistent FA. We are currently prospectively following a cohort of 623 frequent attenders for three years and hope to be able
to improve predictions by incorporating
better and more patient-based information,
such as socioeconomic status, body mass
index, health anxiety/ illness behavior, depressive complaints and anxiety. This has
to be weighed against increased time and
costs to collect such information.
We thank the GPs involved in the Network
of General Practitioners of the Academic
Medical Centre/University of Amsterdam
(HAG-net-AMC) and of the Academic
Medical Centre/University Maastricht
(SMILE) for their continuous efforts
to keep the electronic medical records
updated and their support.
Implications for future research
The model may be useful to select
populations for RCTs with a higher
likelihood of becoming pFA. In addition,
prediction models can be used in RCTs to
characterize the trial arms at baseline in
a multivariable way, thus enhancing the
assessment of baseline comparability.9;34
Finally, subgroup analyses using the scores
from prediction models may serve to move
CHAPTER 5
73
References
1. Vedsted P, Christensen MB (2005)
Frequent attenders in general
practice care: a literature review with
special reference to methodological
considerations. Public Health 119: 118-137.
11. Katzelnick DJ, Simon GE, Pearson SD,
Manning WG, Helstad CP et al (2000)
Randomized trial of a depression
management program in high utilizers of
medical care. Arch Fam Med 9: 345-351.
2. Smits FT, Mohrs J, Beem E, Bindels PJ,
van Weert HC (2008) Defining frequent
attendance in general practice. BMC
Fam Pract 9: 21.
12. Simon GE, Manning WG, Katzelnick DJ,
Pearson SD, Henk HJ et al (2001) Costeffectiveness of systematic depression
treatment for high utilizers of general
medical care. Arch Gen Psychiatry 58:
181-187.
3. Smits FT, Brouwer HJ, ter Riet G, van
Weert HC (2009) Epidemiology of
frequent attenders: a 3-year historic
cohort study comparing attendance,
morbidity and prescriptions of one-year
and persistent frequent attenders. BMC
Public Health 9: 36.
4. Ward AM, Underwood P, Fatovich B,
Wood A (1994) Stability of attendance in
general practice. Fam Pract 11: 431-437.
5. Botica MV, Kovacic L, Tiljak MK, Katic
M, Botica I et al (2004) Frequent
attenders in family practice in Croatia:
Retrospective study. Croatian Medical
Journal 45: 620-624.
6. Carney TA, Guy S, Jeffrey G (2001)
Frequent attenders in general practice: a
retrospective 20-year follow-up study. Br
J Gen Pract 51: 567-569.
7. Andersson SO, Lynoe N, Hallgren CG,
Nilsson M (2004) Is frequent attendance
a persistent characteristic of a patient?
Repeat studies of attendance pattern
at the family practitioner. Scand J Prim
Health Care: 91-94.
8. Wagner M, Balk EM, Kent DM, Kasiske
BL, Ekberg H et al (2009) Subgroup
analyses in randomized controlled trials:
the need for risk stratification in kidney
transplantation. Am J Transplant: 22172222.
9. Kent DM, Hayward RA (2007)
Limitations of applying summary results
of clinical trials to individual patients: the
need for risk stratification. JAMA: 12091212.
10. Smits FT, Wittkampf KA, Schene AH,
Bindels PJE, Van Weert HCPM (2008)
Interventions on frequent attenders in
primary care. Scandinavian Journal of
Primary Health Care Vol 26 (2), -116.
74
13. Bellon JA, Rodriguez-Bayon A, de Dios
LJ, Torres-Gonzalez F (2008) Successful
GP intervention with frequent attenders
in primary care: randomised controlled
trial. Br J Gen Pract 58: 324-330.
14. Smits FTM, Brouwer H.J., ter Riet G,
van Weert HC (2009) Predictability
of persistent frequent attendance. A
historic 3-year cohort study. Br J Gen
Pract 2-2009: 114-119.
15. Steyerberg EW, Vickers AJ, Cook NR,
Gerds T, Gonen M et al (2010) Assessing
the performance of prediction models:
a framework for traditional and novel
measures. Epidemiology 128-138.
16. Vedsted P, Fink P, Olesen F, MunkJorgensen P (2001) Psychological
distress as a predictor of frequent
attendance in family practice: a cohort
study. Psychosomatics 42: 416-422.
17. Jyvasjarvi S, Joukamaa M, Vaisanen
E, Larivaara P, Kivela S et al (2001)
Somatizing frequent attenders in primary
health care. J Psychosom Res 50: 185192.
18. van den Akker M, Spigt MG, De Raeve
L, van Steenkiste B, Metsemakers JF
et al (2008) The SMILE study: a study
of medical information and lifestyles in
Eindhoven, the rationale and contents
of a large prospective dynamic cohort
study. BMC Public Health: 19-20696755.
19. Lamberts H and Wood M, eds (1988)
International classification of primary
care. Oxford: Oxford University Press.
20. Brouwer HJ, Bindels PJ, van Weert HC
(2006) Data quality improvement in
general practice. Fam Pract 23: 529-536.
WHY DO THEY KEEP COMING BACK?
21. Robbins JM, Kirmayer LJ, Hemami
S (1997) Latent variable models of
functional somatic distress. J Nerv Ment
Dis 185: 606-615.
22. Hosmer, D. W., Lemeshow, S.,
Sturdivant, R. X. (2013) Applied logistic
regression, 3 rd edition. New York: John
Wiley & Sons.
23. Lemeshow S, Hosmer DW, Jr. (1982)
A review of goodness of fit statistics
for use in the development of logistic
regression models. Am J Epidemiol: 92106.
32. Andersson S-O, Lynoe N, Hallgren C-G,
Nilsson M (2004) Is frequent attendance
a persistent characteristic of a patient?
Repeat studies of attendance pattern
at the family practitioner. Scandinavian
Journal of Primary Health Care 22: 91-94.
33. Koskela TH, Ryynanen OP, Soini
EJ (2010) Risk factors for persistent
frequent use of the primary health care
services among frequent attenders: a
Bayesian approach. Scand J Prim Health
Care 28: 55-61.
24. Paul P, Pennell ML, Lemeshow S (2012)
Standardizing the power of the HosmerLemeshow goodness of fit test in large
data sets. Stat Med 2012: Jul.
34. Hayward RA, Kent DM, Vijan S, Hofer
TP (2006) Multivariable risk prediction
can greatly enhance the statistical power
of clinical trial subgroup analysis. BMC
Med Res Methodol: 18.
25. Bellon JA, Delgado-Sanchez A, de
Dios LJ, Lardelli-Claret P (2007) Patient
psychosocial factors and primary care
consultation: a cohort study. Fam Pract
24: 562-569.
35. Kent DM, Lindenauer PK (2010)
Aggregating and disaggregating
patients in clinical trials and their
subgroup analyses. Ann Intern Med
2010: 51-52.
26. Thiru K, Hassey A, Sullivan F (2003)
Systematic review of scope and quality
of electronic patient record data in
primary care. BMJ 326: 1070.
27. Wennberg JE (1987) The paradox of
appropriate care. JAMA 258: 2568-2569.
28. Wennberg JE (1985) Practice
variations: why all the fuss? Internist 26:
6-8.
29. van den Dungen C, Hoeymans N,
Gijsen R, van den Akker M, Boesten J
et al (2008) What factors explain the
differences in morbidity estimations
among general practice registration
networks in the Netherlands? A first
analysis. The influence of population
characteristics on variation in general
practice based morbidity estimations.
BMC Public Health;14: 53-62.
30. van den Dungen C, Hoeymans N,
Boshuizen HC, van den Akker M,
Biermans MC et al (2011) The influence
of population characteristics on variation
in general practice based morbidity
estimations. BMC Public Health 2011: 887.
31. Altman DG, Royston P (2000) What
do we mean by validating a prognostic
model? Stat Med 2000: 453-473.
CHAPTER 5
75
chapter 6
MORBIDITY AND DOCTOR
CHARACTERISTICS ONLY PARTLY
EXPLAIN THE SUBSTANTIAL
HEALTHCARE EXPENDITURES OF
FREQUENT ATTENDERS: A RECORD
LINKAGE STUDY BETWEEN PATIENT
DATA AND REIMBURSEMENTS DATA
Frans T. Smits, Henk J. Brouwer,
Aeilko H. Zwinderman, Jacob Mohrs,
Hugo M. Smeets, Judith E. Bosmans,
Aart H. Schene, Henk C. van Weert,
Gerben ter Riet
BMC Fam. Pract. 2013, 14:138
ABSTRACT
Background
Frequently attending patients to primary care (FA) are likely to
cost more in primary care than their non-frequently attending
counterparts. But how much is spent on specialist care of
FAs? We describe the healthcare expenditures of frequently
attending patients during 1, 2 or 3 years and test the hypothesis
that additional costs can be explained by FAs’ combined
morbidity and primary care physicians’ characteristics.
Method
Record linkage study. Pseudonymised clinical data from the
medical records of 16 531 patients from 39 general practices
were linked to healthcare insurer’s reimbursements data. Main
outcome measures were all reimbursed primary and specialist
healthcare costs between 2007 and 2009. Multilevel linear
regression analysis was used to quantify the effects of the
different durations of frequent attendance on three-year total
healthcare expenditures in primary and specialist care, while
adjusting for age, sex, morbidities and for primary care physicians
characteristics. Primary care physicians’ characteristics were
collected through administrative data and a questionnaire.
Results
Unadjusted mean 3-year expenditures were 5044 and 15 824
Euros for non-FAs and three-year-FAs, respectively. After
adjustment for all other included confounders, costs both
in primary and specialist care remained substantially higher
and increased with longer duration of frequent attendance.
As compared to non-FAs, adjusted mean expenditures were
1723 and 5293 Euros higher for one-year and three-year FAs,
respectively.
Conclusion
FAs of primary care give rise to substantial costs not only in
primary, but also in specialist care that cannot be explained
by their multimorbidity. Primary care physicians’ working styles
appear not to explain these excess costs. The mechanisms
behind this excess expenditure remain to be elucidated.
78
WHY DO THEY KEEP COMING BACK?
Background
Primary care physicians (PCP) spend a
disproportionate amount of their time on
a relatively small proportion of patients
who frequently attend their practice1,2. In
most studies these frequent attenders (FAs)
are defined as the upper 10% of the most
frequently consulting patients per sex and
age group3-5.
Of all FAs during one year, 15.4% continues
to be a frequent attender during 3 years
(1.6% of all enlisted patients)2,6. All FAs
during one year (10% of all enlisted
patients by definition) were responsible
for 39% of all consultations while the 1.6%
FAs during 3 consecutive years (persistent
FAs; pFAs) were responsible for 8% of all
consultations 2.
FAs, and pFAs in particular, usually have
multiple (chronic) somatic diseases,
psychiatric disorders and social problems
2,7,8
. FAs are more frequently referred to
specialist care than non-frequent attenders
(non-FAs)9. However, little is known
about the magnitude of the differences in
healthcare utilisation and costs between
non-FAs and FAs and between subgroups
of FAs in specialist care. Possibly these
differences in healthcare costs can be
explained by specific characteristics
and morbidities of FAs, and by PCP
characteristics. If not, detection and
treatment of underlying, not yet detected,
conditions in FAs may result in a better
quality of life of FAs and decrease in costs.
The aim of this paper is to describe
primary and specialist care costs of FAs
in primary care using a combination of
clinical and healthcare insurer’s data
and to examine associations between
healthcare expenditures of FAs of different
duration in primary care and patient’s
morbidities and PCP characteristics.
Methods
Design and data collection
In a historic three-year cohort study seven
primary healthcare centres in Amsterdam,
The Netherlands, provided data. These
centres participate in the PCP-based
continuous morbidity registration network
of the Department of General Practice
at the Academic Medical Centre of the
University of Amsterdam (HAG-net-AMC).
Of all patients, 45% were insured by one
health insurer: AGIS10. Only these data
were used. Reimbursement claims of all
insured people are electronically verified
and saved at the patient level in the
AGIS Health Database. This registration
provides data of treatments by PCPs,
specialists, other health professionals and
prescriptions.
Linking of both databases
The two databases were linked using a
number that uniquely identifies single
Dutch citizens, the so-called “burger
[citizen] service nummer [number]” or BSN
in Dutch. Through a certified trusted third
party that specializes in record linkage
through irreversible pseudonymisation
(ZorgTTP, Houten, The Netherlands),
the PCP database (clinical data) and the
insurer database (financial reimbursement
data) were encrypted. Next, both
encrypted databases were linked. This
CHAPTER 6
79
resulted in a database in which individual
patients could not be identified.
Study population
All patients of 18 years and older registered
at the participating PCPs in 2009 were
eligible for this study. Patients were
classified according to their frequent
attendance status. FAs were defined as
those patients whose attendance rate
ranked in the top 10th centile of four
age groups (18–30 years; 31–45 years;
46–60 years; 61 years+) for men and
women separately3. Frequent attendance
was determined for each of the years
2007, 2008 and 2009. FAs during one
year (1yFAs) were classified as patients
who attended frequently during one of
those years, FAs during 2 years (2yFAs)
as patients who attended frequently in
two of these years and FAs during three
years (3yFAs; pFAs) as those who attended
frequently during all three years. Patients
who were not a frequent attender in any of
these years (non frequent attenders; nonFAs) were used as a reference group.
Ethics approval
The study was conducted according to
the Dutch legislation on data protection
(Ministry of Justice, the Netherlands).
Ethics approval was waived by the Medical
Ethics Committee of the Academic Medical
Center of the University of Amsterdam.
Variables
Costs
In the Netherlands, health insurance
covers a broad range of healthcare
costs including PCP care, prescription
80
medication, specialist care in and outside
hospitals and emergency care. Only over
the counter medication such as simple
painkillers and antihistamines are
excluded. EU citizens who work and live
in the Netherlands usually have Dutch
healthcare insurance and were included
in our study if they were AGIS insured.
All Dutch citizens are required by law to
have a healthcare insurance. Total costs
of all reimbursed primary and specialist
care costs in the years 2007–2009 were
used as the dependent variable. Costs
were retrieved from the insurer’s database
and covered all care reimbursed to their
clients during these years. By taking the
sum of all three years we tried to account
for fluctuating costs because of temporary
diseases.
We divided primary care costs in somatic
costs (e.g. PCP) and psychological costs
(psychologists). Costs of specialist care
consist of all specialist remuneration (in
and outside hospitals) and costs of hospital
admissions. Mental health prescriptions
have an Anatomical Therapeutic Chemical
(ATC) Classification System code and
are included as mental health costs, both
in primary and specialist care. Costs of
homecare, district nurses and nursing
homes were not included.
Attendance
Patients were classified based on the
number of face-to-face consultations with
the PCP. Because we wanted to study
consultation behaviour consultations with
other practice staff were excluded because
these contacts are almost always initiated
by the PCP or his staff and concern
planned control of chronic diseases.
WHY DO THEY KEEP COMING BACK?
Morbidity
The presence of morbidity was assessed using PCPs’ registration of medical problems.
A medical problem is defined as: any medical problem which needs long-term medical attention or monitoring lasting or likely
to last for more than 6 months was added
to the PCPs’ electronic medical record and
coded according to the ICPC system11,12.
These EMR data were extracted for the
purpose of this study. The validity and reliability of coding of the problem list in our
PCP network has been shown to be good in
previous studies4;5. The problem lists were
extracted at the end of 2009.
We selected a set of conditions that
according to the literature are associated
with frequent attendance and may also
be associated with costs (confounding):
diabetes mellitus, cardiovascular
disease, respiratory disease, cancers,
locomotor problems, skin problems and
digestive problems (feelings of) anxiety,
(feelings of) depression, addictions, other
psychological/psychiatric problems, all
social problems and medically unexplained
symptoms (MUS)2,4,13,14. MUS were
defined according to Robbins et al. and
covered several locomotor problems 15. See
appendix 1.
PCPs’ characteristics and practice style
PCPs’ characteristics and practice style
were measured using a questionnaire
(Appendix 3), the mean number of
registered medical problems and
consultations per listed patient (adjusted
for age and sex differences between the
practices) and the PCP practice size (4
categories: <1000 patients; 1001–1250
patients; 1251–1500 patients; >1500
patients).
Ethnicity
Ethnicity of the most prevalent groups in
Amsterdam (Dutch, Surinamese, Ghanese,
Morrocan and Turkish) was determined
in the insurer’s database using automated
name recognition algorithms manually
checked by employees of ethnic descent.
Statistical analysis
We compared primary and specialist care
costs between 1yFAs, 2yFAs, pFAs and
non-FAs. Associations between costs and
patient characteristics were estimated
using multilevel linear regression analysis
with PCP as random intercept. Differences
between patient groups for categorical
variables were analysed using generalized
linear mixed models. Statistical
significance was set at P < 0.05. SPSS 20.0
for windows was used for the statistical
analysis. A linear model for the actual costs
implied that we modelled the mean costs.
This facilitated the easy interpretation
of the regression parameters, namely the
cost difference associated with one unit
change of the characteristic. Mean costs
are also relevant for policy-makers and
health insurance management because of
the close relationship between average and
total costs. Because the cost-distribution
is highly skewed, we provided the median
costs as the statistic that is better suited
for individual patients. We also considered
several transformations to normalize the
costs distributions using the Box-Cox
family of transformations, and found that
a power close to zero yielded the best
CHAPTER 6
81
transformation (that is, the logarithmic
transformation) both for the primary
and the specialist care costs16-18. The
distributions of the transformed costs
were however not much better than
those of the untransformed costs. The
results of the regression analyses were
qualitatively similar for transformed and
untransformed costs. Multivariate analysis
was applied to determine independent
predictors of costs. To determine whether
PCP characteristics were associated with
costs, we extended the mixed-effects
models with PCP characteristics.
Results
Linkage
Of the eligible PCP patients 2% could not
be linked to the insurers’ database by
missing numbers in the files of the PCPs or
administrative failures.
Frequent attenders
In 2009 data were available on 16 531
patients. Of these patients 1208 were not
enlisted in 2008 and/or 2007. Of all 16 531
patients in 2009, 2540 were classified as
1yFAs, 843 as 2yFAs, and 334 as 3yFAs,
and 12 814 were non-FAs. Characteristics
and medical complaints are summarized
in Table 1. FAs were older and more
often female than non-FAs. A non-Dutch
ethnic background was slightly more
prevalent among FAs. The number of all
medical complaints, both somatic and
psychological, was higher among FAs (in
particular among pFAs) than among nonFAs.
82
Healthcare costs
Median and mean costs of both primary
and specialist care were significantly
and substantially higher in all FA groups
than in non-FAs (p < 0.001). Summed over
the three years the mean primary care
costs of 1yFAs, 2yFAs, 3yFAs and non-FAs
were 2650, 3872, 4674 and 1645 Euros
respectively. Specialist care costs showed
a similar pattern: 5866, 6911, 11 150 and
3399 Euros, respectively (all differences p
< 0.001). Costs that could be attributed to
psychosocial complaints were much lower
than costs attributed to somatic complaints
in all groups but showed a similar trend
over the four patient groups (p < 0.001). See
Table 2.
Patient-related determinants of healthcare
costs
Univariate associations between patient
characteristics and healthcare costs and
multivariate adjustment are summarized
in Appendix 4 and Appendix 5. Differences
between PCPs were negligible. The
intraclass correlation (PCP-variance as
part of the total variance) was smaller than
0.001 for both primary and specialist care.
After multivariate adjustment for all
patient and PCP characteristics large
and significant cost differences remained
between the different FA categories not
only in primary care, but even more in
specialist care with extra expenditures for
pFAs of 1264 and 3934 Euros respectively.
PCP-related determinants of healthcare costs
Thirty-nine PCPs of seven primary
healthcare centres participated in this
study. The average practice size was 1312
WHY DO THEY KEEP COMING BACK?
Table 1. Description of the study population in 2009 (by Frequent Attender-status)
Non-FA1
1yFA1
2yFA1
3yFA1
Number of patients
12 814
2540
843
334
Mean age2
46 (18)
47 (18)
49 (19)
53 (17)
Females, n(%)
7371 (58)
1410(56)
508 (60)
215 (64)
Dutch, n(%)
9798 (77)
1872 (74)
603 (72)
235 (70)
Moroccan, n(%)
465 (4)
120 (5)
49 (6)
17 (6)
Turkish, n(%)
280 (2)
66 (3)
24 (3)
12 (4)
Surinamese, n(%)
2262 (18)
480 (19)
167 (20)
70 (21)
3.39 (2.82)
4.50 (3.34)
Ethnicity
Mean number of entries on the problem list in 2009 (SD)3
All problems
1.58 (2.02)
2.43 (2.54)
Social
0.02 (0.16)
0.04 (0.20) 0.06 (0.26) 0.07 (0.26)
Psychological
0.14 (0.40)
0.24 (0.50) 0.35 (0.61)
0.56 (0.76)
Depression
0.03 (0.18)
0.06 (0.23) 0.10 (0.30)
0.13 (0.34)
Anxiety
0.02 (0.14)
0.03 (0.18)
Medically unexplained symptoms
0.09 (0.33) 0.17 (0.45)
0.26 (0.54) 0.36 (0.66)
Diabetes mellitus
0.09 (0.29) 0.14 (0.35)
0.18 (0.39)
0.19 (0.40)
Respiratory diseases
0.13 (0.36)
0.16 (0.40)
0.25 (.47)
0.30 (0.51)
Cardiovascular diseases
0.27 (0.63)
0.42 (0.74)
0.59 (.92)
0.66 (0.88)
1.
2.
3.
0.05 (0.23) 0.10 (0.32)
Different frequent attender groups: Patients who never frequently attended during
3 years (non-FAs); patients who attended frequently during 1 year (1yFA), 2 years
(2yFA), or 3 years (3yFA)
Numbers in brackets are standard deviations, unless indicated otherwise
Mean number of entries per patient on the problem list. Patient could have more
than one (social, cardiovascular, etc.) problem. SD means Standard Deviation
CHAPTER 6
83
patients (range, 312–2714) and 82% of
PCPs participated in medical education or
research.
After correction for patient characteristics,
intraclass correlations between healthcare
costs of individual patients in the same
general practice were small: 0.011 for
primary care costs, 0.006 for secondary
care costs. See table 4.
Discussion
Summary
In this population of 16,531 Dutch
primary care patients costs for FAs, and
in particular pFAs, were considerably
higher than for non-FAs throughout
the healthcare. After multivariable
correction for thirteen demographic
and medical confounding factors at the
patient and physician level, frequent
attendance remained associated with
higher expenditures both in primary and
specialist care.
Strength of this study
As far as we know this study is the first
to combine clinical primary care data
and PCP characteristics with cost data in
both primary and specialist care in this
particular type of patients. Second, as
most PCPs participated in the registration
network for over 15 years and received
regular feedback on their registration,
we think these data are of good quality,
especially for somatic and psychiatric
(DSM-IV axis 1) problems 11. However,
registration of e.g. personality disorders
is expected to be less complete. Third, the
cost data were collected from an insurance
84
company and are a valid reflection of
the healthcare costs of the selected
patients [10]. The population covered by
this healthcare insurer represents the
urbanized area very well10. Fourth, we used
a proven method of encrypting of both
databases performed by an independent
third party. Of all patients only 2% could
not be linked. Some of these patients may
have been illegal and not insured.
The distributions of patient characteristics
of key interest and of the confounders
guaranteed ample analytical contrast 19.
For example, age varied between 18 and
101, 58% were female, and 20 percent were
of Surinam origin. This resulted in enough
power to robustly estimate the effect of
these factors on costs.
Limitations of this study
Registration and coding of medical
problems in primary care has limitations.
In general, within a General Practice
Research Network, one can distinguish
several factors to explain morbidity and
prescription differences: “healthcare
system”, “methodological characteristics
of the network”, “general practitioner”,
and the “patient”. These factors and
sub-factors are often interrelated
and explain the different prevalence
figures20,21. Because PCPs register medical
problems mostly during consultations,
the number of registered problems
could be underreported in non-FAs (few
contacts) or overreported (if resolved
problems are not removed) in FAs (many
contacts). Overreporting may also occur
in recurrent or temporary diseases and
may lead to overestimation of prevalence
WHY DO THEY KEEP COMING BACK?
Table 2. Median and mean 3-year costs in Euro per patient in primary and specialist
care (by frequent attender status) #
FA status:
non
1 year
2 years
3 years
Characteristics
Median Mean
(SD)
Median Mean
(SD)
Median Mean
(SD)
Median Mean
(SD)
Primary care
physician
(PCP)
283
338
(197)
444
525
(300)
613
722
(402)
810
1005
(664)
Emergency
care by the
PCP
-
20
(164)
0
51
(114)
0
83
(156)
63
156
(334)
Physical
therapy1
0
41
(379)
0
77
(558)
0
99
(624)
0
181
(931)
Complementary medicine1
0
16
(98)
0
24
(122)
0
37
(142)
0
43
(160)
Laboratory
costs
0
19
(49)
0
42
(69)
40
65
(89)
52
86
(101)
psychotropic
medication
0
86
(719)
0
134
(760)
0
156
(670)
16
233
(672)
Antibiotics
0
15
(182)
11
28
(72)
19
40
(79)
33
63
(108)
Painkillers
0
19
(165)
0
52
(358)
0
50
(305)
16
99
(296)
Other
medication
135
1091
(4019)
401
1717
(4724)
756
2621
(6745)
1262
2808
(4542)
Somatic
primary care
costs
511
1553
(4212)
1049
2501
(5052)
1696
3696
(7035)
2626
4421
(5316)
Psychological
primary care
costs
0
92
(721)
0
48
(764)
0
176
(677)
20
253
(679)
All primary
care costs
540
1645
(4284)
1137
2650
(5145)
1839
3872
2746
(7056)
4674
(5583)
All specialist
care costs
379
3399
1753
(14124)
5866
3023
(16752)
6911
5393
(12877)
11 150
(18
582)
Medication:
#
1
All differences between means (and medians) were statistically significant at
the <0.001 level.
Only the costs reimbursed by the insurer.
CHAPTER 6
85
Table 3. The effects of Frequent Attender status on mean costs in primary and
specialist care adjusted for all patient characteristics and morbidities (in Euros)
additional costs#
Primary care
Specialist care
Non-Frequently Attending
Patients (reference)a
0
0
1-year Frequent Attenders
481 (44)
1242 (117)
2-year Frequent Attenders
800 (73)
1897 (192)
3-year Frequent Attenders
1268 (115)
4025 (302)
#
All effects were statistically significant at the <0.001 level.
Adjusted for sex, ethnicity, age, number of active problems, diabetes,
respiratory, cardiovascular, social, psychological and medically unexplained
problems, cancer, locomotor, skin and digestive problems.
Mean costs for non-FAs:1645 Euros (all primary care) and 3399 Euros
(all specialist care).
a
and underestimation of the effect on costs.
As in our registry, the problem lists are
subject to regular evaluation, we think
that the errors caused by this are likely to
be small. Second, the variation in PCPs’
characteristics was modest and this
reduced the data-analytic contrast at the
PCP level. For example, eighty-two percent
of the PCPs were involved in education or
research and all practices were relatively
small (mean 1,312 patients; average Dutch
practice: 2,150 patients). In addition, PCPs
might have tended to answer in a socially
desirable way to the questions on their
special interests. This may have led to a
seemingly homogeneous group of PCPs
and to underestimation of the effects of
special interests on costs. Third, there may
be undocumented determinants of costs
(residual confounding). By incorporating
an extensive set of possible confounders
in the analysis we tried to diminish this
bias. However, we had no data on severity
of diseases, perceived health status,
quality of life, illness attitude, life events
86
and socio-economic level. The resulting
residual confounding may have led to
overestimation of the association of (p)
FA-ship and costs. Fourth, because 7%
of the patients selected in 2009 were not
enlisted all 3 years we may have slightly
underestimated the number and the
effect of pFAs. Fifth, because insurers
compete on the basis of their premium,
the patient’s choice of the AGIS health
insurer could cause a some degree of selfselection. Finally, this study originates in
the specific Dutch healthcare system with
a well-organized primary care in which
PCPs provide continuity of care and act as
gatekeepers to specialist care. This may
restrict the generalisability of our results
to countries with a similar healthcare
system like the United Kingdom[8].
Comparison with existing literature
As most researchers we chose a
proportional definition of frequent
attendance that takes into account age and
sex3-5. Earlier research has shown that the
WHY DO THEY KEEP COMING BACK?
Table 4. Effect of Primary Care Physicians’ characteristics on 3-year mean costs
(in Euros) of primary and specialist healthcare
Primary care
Specialist care
difference in
costs (SE)
difference in
costs (SE)
Male sex of PCP ¶, n(%)
15 (38) a
-10 (20) a
-100 (66)
Involvement in education of
medical students and/or
vocational PCP training, n(%)
32 (82)
-5 (36)
59 (91)
2.4 (1.1)
-23 (9)
-35 (32)
17 (9)
-1 (1.1)
-0.2 (4)
Mean number of active
problems per patient on
problem list
1.7 (0.5)
-73 (17)
-289 (51)
Mean number of contacts
(adjusted for age and sex of
the patient)
2.8 (0.3)
13 (39)
-80 (131)
Mean percentage of
all problems that was
psychological or social
12 (3)
-1 (93)
2 (11)
3.2 (0.7)
0 (16)
24 (52)
COPD /Asthma
3.1 (0.7)
-23 (14)
-50 (45)
Cardiovascular disease
3.0 (0.5)
-20 (18)
-146 (58)
Anxiety
2.9 (0.8)
-11 (13)
-80 (41)
Depression
3.0 (0.7)
-15 (14)
-68 (46)
Medically Unexplained
Symptoms
4.0 (0.7)
10 (14)
33 (47)
a
General characteristicsb
Practice sizec
Experience (years)
d
Special interest in managinge
Diabetes mellitus
f
¶
a
b
c
d
e
f
PCP indicates primary care physician
Numbers in brackets are standard errors, unless indicated otherwise
In Euros per unit of the scale of the characteristic
Divided in 4 classes: class 1:0–1000 patients; class 2:1001–1250 patients; class
3:1251–1500 patients; class 4:>1500 patients. Range 312–2,714 patients.
Per (additional) year experience
Five levels of interest (from 1 (no special interest) to 5 (very much interest)) and
5 levels of percentage of patients treated by the GP (0%-100%).
See appendix 3.
Chronic Obstructive Pulmonary Disease
CHAPTER 6
87
number of health problems is consistently
and positively associated with utilisation of
primary and specialist care8,22. Our study
confirms these findings and evaluates
the influence of clinical and physician
characteristics on the relationship between
frequent attender status and healthcare
costs.
The mechanism behind the interaction
between FAs and PCP prompting the
performance of additional diagnostic
and therapeutic actions is not fully
understood. Earlier theories emphasized
a negative interaction between some
patients and their PCP in maintaining
“somatic fixation” resulting in unnecessary
consultations, tests and treatments 2325
. In patients with MUS explanations
for ‘somatisation’ should be sought in
doctor-patient interaction rather than in
patients’ psychopathology26-28. However,
the adjusted differences in costs between
the PCPs participating in this study
were small. This suggests that patient
determinants may be more important in
explaining extra expenditures by FAs than
PCP characteristics, although a larger
and more diverse group of PCPs may be
needed to corroborate this. The nestor of
Dutch general practice, Frans Huygen,
already demonstrated that families tend to
be consistent in illness and consultations
patterns29-31. This may imply that frequent
attending also could be understood as a
kind of learned behaviour or trait.
Implications for research and/or practice
This study shows that FAs of the PCP
are also heavy users of all clinical
services. As most somatic problems in
88
this patient group are already dealt with
in chronic care models, most advantages
are likely to be gained by diagnosing
and treating undetected psychiatric and
social problems. Adequate diagnosis and
treatment of such problems in primary care
and optimal PCP-patient-communication
may prevent referral of patients to
specialist care and may strengthen the
gate keeping role of PCPs32-36. The assumed
trait character of frequent attendance may
impede the effects of any treatment.
Future research should focus on the
aetiology of (the persistence of) frequent
attendance 36,37. Personality factors, life
events, social support and socio-economic
level should be investigated more to assess
how they affect attendance and costs.
Moreover, we need to clarify how and
why patients prompt their physicians to
do more than strictly indicated. Armed
with more knowledge about these causes
of frequent attendance future randomised
trials may target those interventions aimed
at modifying these causes and reduce
illness, attendance and costs.
Conclusions
Frequent attenders of primary care
contribute substantially to costs not only
in primary care but also in specialist
care. Morbidity, social problems and
PCP characteristics appear to only partly
explain these expenditures. Frequent
attendance may therefore be considered
as an independent, yet incompletely
understood contributing determinant of
healthcare utilisation and costs in primary
and specialist care.
WHY DO THEY KEEP COMING BACK?
References
1. Neal RD, Heywood PL, Morley S,
Clayden AD, Dowell AC: Frequency of
patients’ consulting in general practice
and workload generated by frequent
attenders: comparisons between
practices. Br J Gen Pract 1998, 48:895–
898.
2. Smits FT, Brouwer HJ, Ter Riet G, Van
Weert HC: Epidemiology of frequent
attenders: a 3-year historic cohort study
comparing attendance, morbidity and
prescriptions of one-year and persistent
frequent attenders. BMC Publ Health
2009, 9:36.
3. Smits FT, Mohrs J, Beem E, Bindels
PJ, Van Weert HC: Defining frequent
attendance in general practice. BMC
Fam Pract 2008, 9:21.
4. Vedsted P, Christensen MB: Frequent
attenders in general practice care: a
literature review with special reference to
methodological considerations. Public
Health 2005, 119:118–137.
5. Luciano JV, Fernandez A, Pinto-Meza
A, Lujan L, Bellon JA, Garcia-Campayo
J, et al: Frequent attendance in primary
care: comparison and implications of
different definitions. Br J Gen Pract 2010,
60:49–55.
6. Smits FTM, Brouwer HJ, Ter Riet G, Van
Weert HC: Predictability of persistent
frequent attendance. A historic 3-year
cohort study. Br J Gen Pract 2009 2009,
2:114–119.
7. Vedsted P, Fink P, Sorensen HT, Olesen
F: Physical, mental and social factors
associated with frequent attendance in
Danish general practice. A populationbased cross-sectional study. Soc Sci Med
2004, 59:813–823.
8. Dunlop S, Coyte PC, McIsaac W: Socioeconomic status and the utilisation of
physicians’ services: results from the
Canadian National Population Health
Survey. Soc Sci Med 2000, 51:123–133.
9. Heywood PL, Blackie GC, Cameron
IH, Dowell AC: An assessment of the
attributes of frequent attenders to
general practice. Fam Pract 1998,
15:198–204.
10. Smeets HM, De Wit NJ, Hoes AW:
Routine health insurance data for
scientific research: potential and
limitations of the Agis Health Database. J
Clin Epidemiol 2011, 64:424–430.
11. Brouwer HJ, Bindels PJ, Van Weert HC:
Data quality improvement in general
practice. Fam Pract 2006, 23:529–536.
12. Lamberts H: Wood M e: International
classification of primary care. Oxford:
Oxford University Press; 1988.
13. Gill D, Sharpe M: Frequent consulters
in general practice: a systematic review
of studies of prevalence, associations
and outcome. J Psychosom Res 1999,
47:115–130.
14. Ferrari S, Galeazzi GM, Mackinnon A,
Rigatelli M: Frequent attenders in primary
care: impact of medical, psychiatric and
psychosomatic diagnoses. Psychother
Psychosom 2008, 77:306–314.
15. Robbins JM, Kirmayer LJ, Hemami S:
Latent variable models of functional
somatic distress. J Nerv Ment Dis 1997,
185:606–615.
16. Box GEP, Cox DR: An Analysis of
Transformations. Journal of the Royal
Statistical Societ 1964, 26(2):211–256.
17. Manning WG, Mullahy J, Basu A:
Estimating log models: to transform or
not to transform? J Health Econ 2001,
20:461–494.
18. Manning WG, Basu A, Mullahy J:
Generalized modeling approaches to risk
adjustment of skewed outcomes data. J
Health Econ 2005, 24:465–488.
19. Miettinen OS: Theoretical Epidemiology:
principles of occurrence research in
medicine. New York: Wiley; 1985.
20. Van den Dungen C, Hoeymans N,
Gijsen R, van den Akker M, Boesten J,
Brouwer H: What factors explain the
differences in morbidity estimations
among general practice registration
networks in the Netherlands? A first
analysis. Eur J Gen Pract. 2008;14 Suppl
1:53-62.
CHAPTER 6
89
21. van den Dungen C, Hoeymans N,
Boshuizen HC, van den Akker M,
Biermans MC, Van BK: The influence of
population characteristics on variation
in general practice based morbidity
estimations. BMC Publ Health 2011,
201(1):887.
22. Wouterse B, Meijboom BR, Polder JJ:
The relationship between baseline health
and longitudinal costs of hospital use.
Health Econ 2011, 20(8):985–1008.
23. Van Eijk J, Grol R, Huygen F, Mesker
P, Mesker-Niesten J: [Somatic fixation.
Prevention by the general practitioner].
Soc Sci Med 1982,58:717–725.
24. Rosendal M, Fink P, Bro F, Olesen F,
Rosendal M, Fink P, et al: Somatization,
heartsink patients, or functional somatic
symptoms? Towards a clinical useful
classification in primary health care.
Scand J Prim Health Care 2005, 2005:3–
10.
25. McDaniel SH, Campbell T, Seaburn
D: Treating Somatic Fixation: A
Biopsychosocial Approach: When
patients express emotions with physical
symptoms. Can Fam Physician 1991, 37:
451-456.
26. Salmon P, Humphris GM, Ring A, Davies
JC, Dowrick CF, Salmon P: Primary
care consultations about medically
unexplained symptoms: how do patients
indicate what they want? Psychosom
Med 2006, 24:570–577.
27. Ring A, Dowrick CF, Humphris GM,
Davies J, Salmon P, Ring A: Doctors’
responses to patients with medically
unexplained symptoms who seek
emotional support: criticism or
confrontation? Soc Sci Med 2005,
29:1505–1515.
28. Ring A, Dowrick CF, Humphris G,
Salmon P: What do general practice
patients want when they present their
medically unexplained symptoms, and
why do their general practitioners feel
pressurized? J Psychosom Res 2005,
59:255–260.
30. van den Bosch WJ, Huygen FJ, van
den Hoogen HJ, Van Weel C: Morbidity
in early childhood: family patterns in
relation to sex, birth order, and social
class. Fam Med 1993, 1993:126–130.
31. Cardol M, van den Bosch WJHM,
Spreeuwenberg P, Groenewegen PP, Van
Dijk L, De Bakker DH: All in the Family:
Headaches and Abdominal Pain as
Indicators for Consultation Patterns in
Families. The Annals of Family Medicine
2006, 4:506–511.
32. Cuijpers P, Van Straten A, Schuurmans
J, Van Oppen P, Hollon S, Cuijpers
P: Psychotherapy for chronic major
depression and dysthymia: A metaanalysis. Clin Psychol Rev 2010, 30:
51-62.
33. Cuijpers P, Van Straten A, Warmerdam
L: Problem solving therapies for
depression: A meta-analysis. European
Psychiatry 2007, 22:9–15.
34. Reger MA, Gahm GA: A meta-analysis
of the effects of Internet- and computerbased cognitive-behavioral treatments
for anxiety. J Clin Psychol 2009,
65(1):53–75.
35. van der Feltz-Cornelis CM, Van Os TW,
Van Marwijk HW, Leentjens AF.: Effect
of psychiatric consultation models in
primary care. A systematic review and
meta-analysis of randomized clinical
trials. J Psychosom Res 2010, 68:521-33.
36. Morriss R, Kai J, Atha C, Avery A,
Bayes S, Franklin M: Persistent frequent
attenders in primary care: costs, reasons
for attendance, organisation of care
and potential for cognitive behavioural
therapeutic intervention. BMC Fam Pract
2012, 13:39.
37. Rifel J, Svab I, Selic P, Rotar PD,
Nazareth I, Car J: Association of
Common Mental Disorders and Quality
of Life with the Frequency of Attendance
in Slovenian Family Medicine Practices:
Longitudinal Study. PLoS One 2013,
8:e54241.
29. Huygen FJ: Family Medicine- The
medical life history of families. Assen,
The Netherlands: van Gorcum; 1978.
90
WHY DO THEY KEEP COMING BACK?
CHAPTER 6
91
part II
REVIEW OF THE LITERATURE
ABOUT INTERVENTIONS ON
FREQUENT ATTENDERS IN PRIMARY
CARE
chapter 7
INTERVENTIONS ON FREQUENT
ATTENDERS IN PRIMARY CARE. A
SYSTEMATIC LITERATURE REVIEW
Frans T. Smits, Karin A. Wittkampf,
Aart H. Schene, Patrick J. Bindels,
Henk C. van Weert
Scand. J. Prim. Health Care. 2008;
26(2): 111-6.
ABSTRACT
Purpose
To analyze which interventions are effective in influencing
morbidity, quality of life and healthcare utilization of frequently
attending patients (FAs) in primary care.
Method
We performed a systematic literature search for articles
describing interventions on FAs in primary care (Medline,
Embase and PsycINFO). Outcomes were morbidity, quality of
life and use of health care. Two independent assessors selected
all randomized clinical trials (RCT) and assessed the quality of
the selected RCTs.
Results
Three RCTs used frequent attendance to select patients at
risk for distress, major depression and anxiety disorders. These
RCTs applied psychological and psychiatric interventions and
focused on as yet undiagnosed psychiatric morbidity of FAs.
Two of them found more depression-free days and a better
quality of life after treating Major Depressive Disorder (MDD)
in FAs. No other RCT found any positive effect on morbidity or
quality of life. Two RCTs studied an intervention which focused
on reducing frequent attendance. No intervention significantly
lowered attendance. Due to the difference in study settings and
the variation in methods of selecting patients, meta-analysis of
the results was not possible.
Conclusion
We did find indications that frequent attendance might be a
sign of as yet undiagnosed MDD and that treatment of MDD
might improve the depressive symptoms and the quality of life
of depressed FAs. We found no evidence that it is possible to
influence healthcare utilization. Future studies should focus on
well-defined subgroups of FAs.
94
WHY DO THEY KEEP COMING BACK?
Introduction
Primary care physicians (PCP) spend about
80% of their time on 20% of their patients:
about one in every seven consultations
concerns the top 3% of attenders.1 Two
systematic literature reviews confirm
that these frequent attenders (FAs) have
high rates of physical disease, emotional
distress, psychiatric illness and social
difficulties.2;3
Frequent attenders are a heterogeneous
group of patients. Karlsson’s analysis of
FAs suggests dividing them into five subgroups: patients with purely somatic illness
(28%), patients with clear psychiatric
illness (21%), patients in temporary crisis
(10%), chronically somatizing patients
(21%) and those with multiple problems
(20%).4 In most cases somatic and
psychiatric illnesses are accepted reasons
for frequent consultation, crises pass and
are a reason for frequent consultation for a
short time. However frequent attendance
by multi-problem or somatizing patients
with related but undetected psychiatric
morbidity is thought to lead to unnecessary
consultations and therefore to ineffective
health care.5 Detecting, diagnosing and
treating the psychiatric disorders of these
FAs should improve their quality of life
as well as lower the impact of frequent
attending on the healthcare system.6
The combination of large workload and
high rate of (chronic) disease make FAs
an important group for a PCP not only to
study but also to treat.
The objective of this study is to analyze
which interventions might be helpful in
reducing morbidity and improving the
quality of life of FAs and might reduce
their healthcare utilization. We therefore
performed a systematic review of
interventions on FAs aimed at answering
two questions: (1) which interventions
have been studied, and at which group of
FAs were they targeted, and (2) what was
the effectiveness of these interventions
in terms of morbidity, quality of life and
frequency of attendance?
Methods
Literature search:
We searched the databases Medline,
Embase and PsycINFO (1980- 2006-11).
To obtain optimal sensitivity we used
the MESH-headings: ‘health services/
utilization’, ‘health services misuse’ and
‘health care utilization’, as well as the
following truncations as text words:
‘frequent attend*’, ‘frequent consult*’, ‘high
utiliz*’, ‘high consultation frequency’,’ high
consultation rate’. In addition we checked
the references of all included articles
for other relevant but not yet retrieved
articles.
Selection of articles: On title and abstract,
we selected articles which described
interventions in FAs in primary care
aged between 18 and 70 years, and were
written in the English, French, Dutch
or German language. We included all
possible FA-definitions, also definitions
based on specific (sub) groups of primary
care patients. When there was any doubt
about the setting or the kind of included
patients we assessed the full paper. An
overview of the FA definitions used in the
final selection of articles for this review is
presented in table 1.
CHAPTER 7
95
All articles that met the inclusion
criteria were read in detail to select only
randomized controlled trials (RCT) and
to re-check the inclusion and exclusion
criteria. Two assessors (FS; KW)
performed these procedures independently
and the final selection was discussed in a
consensus meeting with a third assessor
(HW).
Quality assessment: Two reviewers (FS and
KW) appraised each RCT independently
with the quality criteria for assessment of
experimental studies of Khalid Khan et
al.7 This checklist consists of nine items
on methodological quality. All items were
scored as yes, no or uncertain. Points of
disagreement were discussed with a third
senior assessor (HW) for a final decision.
Because of the differing study settings
and the variation in studied populations,
pooling of the results was not possible.
Results
Literature search:
Our literature search resulted in 4357
articles. After the first selection, 28 articles
were retrieved for detailed reading. (Figure
1) The second selection resulted in the
identification of five RCTs. Table 1 presents
an overview of their characteristics.
Included studies:
Setting, definition of FAs, kind of counted
contacts and the population of the included
studies are summarized in table 1.
Simon et al. and Katzelnick et al. refer to
the same research program. 8; 9 Their main
goal was the evaluation of a depression
management program among depressed
96
FAs. They excluded patients who had
received active treatment for depression
during the previous three months and for
whom the treatment program would be
inappropriate (i.e. bipolar or psychotic
disorder, substance abuse or terminal
illness). The selected patients (n=7203)
were screened by telephone using the
depression module of the Structured
Clinical Interview for DSM-IV (SCID).
Those currently suffering from major
depression or those reporting an
episode of major depression within the
previous two years but now in partial
remission (n=1475) were eligible for a
second assessment using the Hamilton
Depression Rating Scale (HDRS).
Finally, a total of 407 patients with a
HDRS score of 15 or more consented to
enrolment: 218 patients were randomized
to a Depression Management Program
(DMP) and 189 patients received usual
care (UC). Intervention: The depression
management program included a two hour
physician training program, an evaluation
visit with their PCP immediately after
enrolment, antidepressant medication
(AD) if appropriate, written and
videotaped educational materials and
treatment coordination. Results: in the
year following the intervention patients in
the intervention group had a mean of 47
more depression-free days (c.i. 26.6-68.2 ),
more prescriptions for AD (69.3% of DMP
patients and 18.5% of UC patients had filled
at least three antidepressant prescriptions
for the six-month period after enrolment ;
P<0.001), more improvement on the HDRS
(change in HDRS in 12 months for DMP
patients 9.2 and for UC patients 5.6; P<
0.001), more improvement on the SF-
WHY DO THEY KEEP COMING BACK?
Figure 1. Flow diagram selection of articles
Articles about frequent attending:
N= 4357
(Pubmed, Embase, PsycINFO)
Articles about interventions on frequent attenders:
N= 28
Exclusion criteria (N= 4329):
•
not about interventions
on FAs(N= 4329)
•
paediatric- or
geriatric-care (n= 0)
Exclusion criterion (N= 23):
•
no RCT.
Final list of RCT’s on frequent attenders:
N= 5
Analyses
20-scores for social functioning, mental
health, and general health perceptions
(P<0.05), and DMP patients had 3.2 more
contacts with the healthcare system (c.i.
0.70-5.80) as well as more costs ($51.84 per
additional depression-free day ; c.i. 17.37108.47).
Katon et al. evaluated a psychiatric
consultation-liaison program among
distressed FAs. 8 They selected 1790 FAs
(235 patients were excluded for various
reasons). From this group distressed FAs
were selected by using the Symptoms
Checklist Revised (SCL-R); sum score
1 standard deviation above population
mean. Of the 339 identified distressed FAs,
251 gave consent for randomization, 124
patients were assigned to the intervention
group and 127 to the control group. The
intervention consisted of a psychiatric
diagnostic interview by a psychiatrist
using the Diagnostic Interview Schedule
(DIS) with the family physician present,
a jointly formulated treatment plan and
a mutually accepted course of action (i.e.
medication adjustment, referral, fixedinterval visits etc.). The outcome measures
were rates of anxiety and depression
(SCL-90-R), use of antidepressants and
use of health care. Results: Katon found
no significant difference in improvement
of psychopathology, more prescribed
antidepressants (+ 38%; p<0.01.) in the
intervention group after one year and no
consistently significant differences in any
utilization measure between intervention
and control groups (primary care, p=
0.097; medical specialty visits, p=0.111;
radiography, p= 0.61; lab testing, p=0.072;
admission to inpatient care, p=0.16). .
CHAPTER 7
97
Table 1. Overview of the selected Randomized Clinical Trials
Setting
Definition FAs/
Kind of counted
contacts
Population
Identification
Number of
interventions /
contr. patients
Simon 8*
Primary care clinic,
3 prepaid health
plans in Midwest,
Northwest and New
England,
(USA)
• Top 15% attenders
during 2 consecutive years
• outpatient medical
visits
Age:
23-63
• Electronic data
• SCID : Pos MDD or MDD
pos. last 2 yrs (=1475
pat)
• HDRS>14, 163 General
practices:
• Usual care: 81
• Intervention: 82
Intervention:
218
Usual care:
189
• Top15% attenders
during 2 consecutive years
• outpatient medical
visits
Age:
25-63
• Electronic data
• SCID : Pos MDD or MDD
pos last 2 yrs (=1475 pat)
• HDRS>14 ,163 General
practices:
• Usual care: 81
• Intervention: 82
Intervention
218
Usual care
189
• Top 10% attenders
in 1 year for sex and
age.
• ambulatory health
care visits.
Age: 18-75
• >2 Years in practice
• Selection from electronic data
• SCL-R one standard
deviation above mean ->
339 patients.
• 251 Accepted randomisation
Intervention
124
Control
127
Intervention
34
Control
40
No contact
30
Katzelnick 9
Primary care clinic,
3 prepaid health
plans in Midwest,
Northwest and New
England,
(USA)
Katon 10
Primary care clinics
of HMO, Washington State,
(USA)
18 GP’s out
HMO
300.000
Patients.
Olbrisch 11
Primary health care
for students:
Florida State University,
(USA)
• > 4 face-to-face
contacts in first
quarter of study
year
• outpatient medical
visits
Freshmen,
sophomores
and juniors:
students
university
health
centre
•
•
•
•
•
400 Students
300 got letter
129 agreed
112 randomized
Plus “no contact”-group.
• > 4 Out-of-hours
contacts one year
before inclusion.
• consultations, home
visits and telephone
calls
No age
restriction.
• Consecutive patients
• Randomizat. per practice.
Christensen12
Primary care outof-hours service,
County of Northern
Jutland,
(Denmark)
SCID
MDD
HDRS
SF
98
Structured Clinical Interview DSM
Major Depressive Disorder
Hamilton Depression Rating Scale
Social Functioning
WHY DO THEY KEEP COMING BACK?
Intervention
practices:
83 GP’s; 3500
patients
Control practices:
93 GP’s
4635 patients
Intervention
Follow up
Outcomes
Results
• Depression management
program(DMP):
• 2 h training
• evaluation contact
• antidepressant medication
• information material
• treatment coordinator
1 Year after
randomization.
• Depression free
days
• Costs
• More depression free days (229>182)
• More costs (+$51.84 per additional depression free day)
• Depression management
program(DMP):
• 2 h training
• evaluation contact
• antidepressant medication
• information material
• treatment coordinator
1 Year after
randomization.
• HDRS
• SF-20 score
• Use of antidepressant medication
• Attendance
• Improvement HDRS (13,6-> 9,9
at 1 year)
• More use of AD (69.3% of DMPpatients and 18.5% of usual-carepatients with at least 3 prescriptions in 0, 5 year).
• Better SF-20 scores for social
funct, mental health, gen. health
perceptions
• More attendance in year after
inclusion (+3, 2 )
• DIS by psychiatrist
• Interview by the psychiatrist with the GP present
• Jointly formulated treatment plan
• Written protocol of treatment for GP
1 Year after
randomization
• Use of antidepressant med (AD).
• Rate of anxiety/
depression
• Use (psych) health
care
• More AD (+38%)
• No better psych state
• No lower use of health care and
costs
Brief educational program
(group of 3-8 students)
1 Year after
intervention
• Number of contacts primary care
• Use of other health
care
• Lower use of primary care on
short term.
• Convergence towards same utilization during follow-up
• No differences on number of visits to other health care providers
• Status consultation by GP
• Education of participating GP’s
• Questionnaire patients
• Economic incentives GP
1 Year after
the intervention
• Number of contacts with the outof-hours-service.
• Daytime contacts with the
GP;hospital admissions; visits to hospital outpatients
clinics
• No convincing effect.
SCL-R
DIS
*
Symptom Checklist Revisited
Diagnostic Interview schedule
The numbers in superscript refer to the reference list
CHAPTER 7
99
Table 2. Quality assessment selected RCTs
Quality criteria (7*)
Simon Katzelnick
(8)
(9)
Katon Olbrisch Christensen
(5)
(12)
(13)
Assignment to the treatment
groups really random?
+
+
+
?
+
Treatment allocation concealed?
+
+
?
?
-
Groups similar at baseline in
terms of prognostic factors?
+
+a
+
+
?
Were the eligibility criteria
specified?
+
+
+
+
+
Outcome assessors blinded to
the treatment allocation?
+
+
+
-
n.a.
Was the care provider blinded?
-
-
-
-
-
Was the patient blinded?
-
-
-
-
-
Points estimates and measure
of variability presented for the
primary outcome measure?
+
+
+
-
-
Analyses included an intention to
treat analysis?
+a
+
-
-
-
a
*
Not mentioned in this article. Katzelnick does mention the criteria.
Numbers between brackets refer to the reference list
Olbrisch refers to an intervention among
frequent attending students. 9;10 Her
purpose was to evaluate the effectiveness
of a brief health education intervention
aimed at making students aware of the
psychological and social factors that
make people prone to illness and to
inappropriate use of health care resources.
Three-hundred randomly-selected and
eligible students were sent a letter inviting
them to participate, 129 agreed and
112, who kept appointments scheduled
for them, were randomized to the
intervention group (n=34) or the control
group (n=40). Olbrisch also selected a
matched group with no contacts (n=30).
The exact routing of all study participants
100
is not clearly described. Her intervention
consisted of a brief educational group
program (presentations, discussion and
a demonstration or audiotape of deep
muscle relaxation). The outcome measure
was use of health care facilities. Results:
the intervention group showed reduced
utilization of the university health center
for a short period of time (not adequately
specified), with this effect dissipating over
time and no significant differences on
the number of visits to other health care
providers (F(2.85)=1.7 ; p=0.19).
In the only RCT outside of the USA,
Christensen et al studied an out-of-hours
primary care service in Denmark.11
WHY DO THEY KEEP COMING BACK?
They tested whether a combination of
intervention strategies reduced health
care utilization by FA’s.. In a cluster
randomization, family physician practices
were randomized to intervention practices
(83 practices; 3500 patients) and control
practices (93 practices; 4635 patients).
The intervention consisted of (1)a patient
questionnaire and an invitation for the
FAs to contact their family physician
for a status consultation, (2)information
about the project and FAs for the
PCP,(3) physician group education on
frequent attending (29% of all physicians
representing 40% of all practices
participated) and (4)economic incentives
for the PCP to perform the status
consultation. Outcome measures were (1)
the number and kind of contacts with the
out-of-hours-service (2) daytime contacts
with PCP, hospital admissions, and visits to
hospital outpatient clinics and emergency
departments. Results: They found no
significant difference in the primary and
secondary outcome measures. Quality assessment
The quality assessment of the included
RCTs is summarized in Table 2. None of
the RCTs fully complied with all quality
criteria. In none of the RCTs were the
patient and the care provider sufficiently
blinded. Blinding of patients and
physicians was not possible in the studies
of Simon, Katzelnick, Olbrish and Katon
because psychological treatments do not
allow concealment. Katon, Olbrisch and
Christensen did not include an intentionto-treat-analysis. Olbrisch did not describe
whether the outcome assessors were
blinded to the treatment allocation and
did not give point estimates and measures
of variability. Christensen did not go
into detail about point estimates and
measures of variability. All articles, except
Christensen’s, refer to various subgroups
of FAs. Therefore it was not possible to
generalize the results of these studies to
all FAs.
Discussion
Main findings
After an extensive search for all relevant
literature we were able to identify five
randomized controlled trials that studied
interventions on FAs. Our aim was to learn
more about the included FA population,
about the type of intervention program and
its effectiveness in improving morbidity
and quality of life and in lowering
attendance.
The outcome of these interventions was
disappointing. We found just 5 primary
care based trials. The populations
under study as well as the outcomes of
studies differed. Two RCTs found more
depression-free days and reported a better
quality of life after treating MDD in a
subgroup of depressed FAs.12;13 Although
on an individual basis the gain was quite
impressive (a mean of 47 depression
free days) the net gain on a group level
was disappointing: for every SCID 2.6
depression free day could be achieved.
One other RCT found no positive effect
on morbidity.8 Only two RCTs included
clear measures of quality of life.12;13 Finally,
all RCTs concluded that the studied
interventions did not significantly lower
attendance during one year of follow-up.
CHAPTER 7
101
Two RCTs describing an intervention in
depressed FAs found even more contacts,
more prescriptions for AD and more costs
in the intervention group within one year
of follow-up. 12;13 One RCT found more
prescription of AD and no significant
difference in health utilization.8 Two RCTs
did not measure costs.9;11
Strength and limitations
An important limitation was the
differences in study settings and the
variation in methods of selecting patients.
Four studies were carried out in the USA
(3 HMO; 1 university healthcare), one in
Denmark (out-of-hours-service). We also
found that frequent attendance is not
a clearly-defined concept. Two studies
selected patients who were FA for two
consecutive years (Simon, Katzelnick).
Other studies selected patients who were
FA for three months (Olbrisch) or one
year (Katon, Christensen).Three studies
selected a percentile of most attending
patients; two used a certain number of
consultations as a selecting criterion. In
three studies, frequent attendance was
used to select a group of patients at risk for
distress, major depression and/or anxiety
disorders.8;12;13 The other two made no
further selection and intervened in all
FAs.9;11 Also the interventions used were
different: in three studies, which focused
on as yet undiagnosed psychological
problems and psychiatric morbidity of
FAs, interventions consisted of a screening
and depression management program and
a treatment plan and intervention by a
psychiatrist. 8;12;13 One used an educational
group program.9 In only one study the
intervention (mainly a status consultation
102
and incentives for the PCP) was carried
out by a PCP and focused on diminishing
attendance.11 Due to the low number of
PCP’s trained in this study, it is likely
that the success of this intervention was
underestimated. Because of all these
differences we cannot generalize results to
other (sub) group of FAs.
A possible explanation for the lack of
generalisibility could be that frequent
attendance is the result of many diseaseand personality-linked factors which make
frequent attenders a heterogeneous group
of patients.4 Intervening on a specific
aspect of frequent attendance, for instance
depression, dilutes the outcome of a RCT
which studies all FAs. Moreover, frequent
attendance is not a consistent personality
trait, but often a transitory characteristic.
Some studies show that up to 60-70% of
frequently attending patients change their
health-seeking behavior within 2-3 years.
14-17
Using healthcare utilization as an
outcome measure therefore does not seem
adequate in studying FAs, defined on a one
year basis. Studies that did find an effect
used consultation patterns on a two year
basis.12;12 When an intervention is planned
the net effect on healthcare utilization
in the short term logically is upwards
and a follow-up of longer than one year is
needed.
Our study is the first that reviews
interventions on FAs. The strength of
this study is the sensitive search with
both Mesh-headings and text words. We
therefore expect not to have missed any
RCT describing an intervention in FAs.
WHY DO THEY KEEP COMING BACK?
Comparison with relevant literature
There is an extensive literature about the
characteristics of (sub) groups of FAs.
There are little studies (n= 28) which try to
influence morbidity, quality of life and use
of healthcare of FAs. Only five are RCT’s.
Definitions of FAs differed considerably.
We propose to follow the advice of Vedsted
et al.to define FAs as the top 10% of all
enlisted patients.2
Conclusion
We found a small number of studies that
evaluated interventions on FAs. There is
no evidence that it is possible to influence
healthcare utilization by frequent
attenders. Treatment of (not yet diagnosed)
major depressive disorder might improve
the symptoms and the quality of life of
depressed FAs, but will not reduce their
consultation rate within one year of followup.
References
(1) Neal RD, Heywood PL, Morley S,
Clayden AD, Dowell AC. Frequency
of patients’ consulting in general
practice and workload generated
by frequent attenders: comparisons
between practices. Br J Gen Pract 1998;
48(426):895-898.
(2) Vedsted P, Christensen MB. Frequent
attenders in general practice care: a
literature review with special reference to
methodological considerations. Public
Health 2005; 119(2):118-137.
(3) Gill D, Sharpe M. Frequent consulters
in general practice: a systematic review
of studies of prevalence, associations
and outcome. J Psychosom Res 1999;
47(2):115-130.
(4) Karlsson H, Joukamaa M, Lahti I,
Lehtinen V, Kokki-Saarinen T. Frequent
attender profiles: different clinical
subgroups among frequent attender
patients in primary care. J Psychosom
Res 1997; 42(2):157-166.
(5) Katon W, von Korff M, Lin E, Lipscomb
P. Distressed high utilizers of medical
care: DSM-III--R diagnoses and
treatment needs. General Hospital
Psychiatry /11; 12(6):355-362Record.
(6) Dowrick CF, Bellon JA, Gomez MJ.
GP frequent attendance in Liverpool
and Granada: the impact of depressive
symptoms. Br J Gen Pract 2000;
50(454):361-365.
(7) Khan KS, ter Riet G, Popay J, Nixon J,
Kleijnen J. Study quality assessment.
In Undertaking Systematic Reviews
of Research on Effectiveness CRD’s
Guidance for Carrying Out or
Commissioning Reviews.2 . 2001.
York: NHS Centre for Reviews and
Dissemination (CRD), University of York.
Ref Type: Generic
(8) Katon W, von Korff M, Lin E, Bush
T. A randomized trial of psychiatric
consultation with distressed high
utilizers. General Hospital Psychiatry /3;
14(2):86-98Record.
CHAPTER 7
103
(9) Olbrisch ME. Evaluation of a stress
management program for high utilizers
of a prepaid university health service.
Dissertation Abstracts International /5;
39(11-B):5573Record-1982.
(10) Olbrisch ME. Evaluation of a stress
management program for high utilizers
of a prepaid university health service.
Med Care 1981; 19(2):153-159.
(11) Christensen MB, Christensen B,
Mortensen JT, Olesen F. Intervention
among frequent attenders of the outof-hours service: a stratified cluster
randomized controlled trial. Scand J Prim
Health Care 2004; 22(3):180-186.
(12) Katzelnick DJ, Simon GE, Pearson
SD, Manning WG, Helstad CP, Henk HJ
et al. Randomized trial of a depression
management program in high utilizers
of medical care. Arch Fam Med 2000;
9(4):345-351.
(13) Simon GE, Manning WG, Katzelnick DJ,
Pearson SD, Henk HJ, Helstad CP. Costeffectiveness of systematic depression
treatment for high utilizers of general
medical care. Archives of General
Psychiatry /2; 58(2):181-187.
(14) Ward AM, Underwood P, Fatovich
B, Wood A. Stability of attendance
in general practice. Fam Pract 1994;
11(4):431-437.
(15) Andersson S-O, Lynoe N, Hallgren
C-G, Nilsson M. Is frequent attendance
a persistent characteristic of a patient?
Repeat studies of attendance pattern
at the family practitioner. Scandinavian
Journal of Primary Health Care 2004;
22(2):91-94.
(16) Carney TA, Guy S, Jeffrey G. Frequent
attenders in general practice: a
retrospective 20-year follow-up study. Br
J Gen Pract 2001; 51(468):567-569.
(17) Botica MV, Kovacic L, Tiljak MK, Katic
M, Botica I, Rapic M et al. Frequent
attenders in family practice in Croatia:
Retrospective study. Croatian Medical
Journal 2004; 45(5):620-624.
104
WHY DO THEY KEEP COMING BACK?
CHAPTER 7
105
part III
A PROSPECTIVE STUDY OF
FREQUENT ATTENDERS
chapter 8
WHY DO THEY KEEP COMING
BACK? PSYCHOSOCIAL AETIOLOGY
OF PERSISTENCE OF FREQUENT
ATTENDANCE IN PRIMARY CARE: A
PROSPECTIVE COHORT STUDY
Frans T. Smits, Henk J. Brouwer,
Aeilko H . Zwinderman, Jacob Mohrs,
Aart H. Schene, Henk C.P.M. van
Weert, Gerben ter Riet
Accepted by the Journal of
Psychosomatic Research
ABSTRACT
Background
Patients who visit their General Practitioner (GP) very frequently
over extended periods of time often have multi-morbidity and
are costly in primary and specialist healthcare. We investigated
the impact of patient-level psychosocial and GP-level factors
on the persistence of frequent attendance (FA) in primary care.
Method
Two-year prospective cohort study in 623 incident adult
frequent attenders (>90th attendance centile; age and
sex-adjusted) in 2009. Information was collected through
questionnaires (patients, GPs) and GPs’ patient data. We used
multilevel, ordinal logistic regression analysis, controlling for
somatic illness and demographic factors with FA in 2010 and/
or 2011 as the outcome.
Results
Other anxiety (odds ratio (OR) 2.00; 95% confidence interval
from 1.29-3.10) over 3 years and the number of life events in
3 years (OR 1.06; 1.01-1.10 per event; range of 0 to 12) and, at
baseline, panic disorder (OR 5.40; 1.67-17.48), other anxiety
(OR 2.78; 1.04-7.46), illness behaviour (OR 1.13; 1.05-1.20 per
point; 28-point scale) and lack of mastery (OR 1.08; 1.01-1.15
per point; 28-point scale) were associated with persistence of
FA. We found no evidence of synergistic effects of somatic,
psychological and social problems. We found no strong
evidence of effects of GP characteristics.
Conclusion
Panic disorder, other anxiety, negative life events, illness
behaviour and poor mastery are independently associated with
persistence of frequent attendance. Effective intervention at
these factors, apart from their intrinsic benefits to these patients,
may reduce attendance rates, and healthcare expenditures in
primary and specialist care.
108
WHY DO THEY KEEP COMING BACK?
Introduction
Some patients have exceptionally high
consultation rates with their General
Practitioner (GP), sometimes over many
years.1-5 These persistent frequent
attenders (FAs) often have multi-morbidity
and are costly in both primary and
specialist healthcare.6
Anyone may have short periods in her/
his lives in which frequent help from
a GP is sought or needed. However,
when such periods exceed two or more
consecutive years, more structural
psychosocial problems are often present.1;7;8
Thus, persistent frequent attendance
could be seen as an easily detectable
marker for underlying, often undetected
and unmet, psychosocial problems or
diseases. Previous work has shown that
psychological distress, low physical quality
of life and low educational level were
associated with persistence of frequent
attendance (when frequent attendance
is proportional defined).9;10 Using a fixed
cutoff, persistence of frequent attendance
has been found to be associated with such
diverse factors as female gender, obesity,
former frequent attendance, fear of death,
alcohol abstinence, low satisfaction, and
irritable bowel syndrome.11 Because high
attendance is strongly related to age and
sex, we think it makes sense to define
frequent attendance as an age and sexadjusted attendance rate ranking in the top
10 centile in a GP-practice within a time
frame of one year.12;13 Such a proportional
threshold definition selects the
exceptionally high utilizers within each
age and sex group and allows meaningful
comparison between practices, periods,
and countries.
However, the literature on the
precise aetiology of persistence of
frequent attendance is equivocal.7;11;14-18
Theoretically, within a specific healthcare
setting attendance may be influenced by
patient characteristics including morbidity,
by GP characteristics like work style,
experience, personality and professional
interests and thirdly by the interpersonal
dynamics between patients and their
physician .19;8;16 Previous work indicates
that the considerable costs in primary as
well as in specialist care associated with
(persistent) frequent attendance may
not simply be explained by the excess
morbidity these patients have.20 Therefore,
even fully effective treatment, of clearcut multi-morbidity, if available, cannot
be expected to reduce to normal the high
attendance rates and associated referral
rates to specialist care.
The incomplete understanding of the
aetiology of persistence of frequent
attendance hampers the thoughtful design
of preventive strategies for this persistence
and risks any trials to be well-intentioned
shots in the dark. Therefore we followed
over 2 years a cohort of frequent attenders
during one year to investigate which and
to what extent psychological and social
factors, and GP characteristics play a role
in the aetiology of persistence of frequent
attendance.
Methods
Design
In a prospective cohort study, we followed
incident FAs for two consecutive years.
CHAPTER 8
109
Box. Key variables and confounding variables (continued on right page)
Scale
Structure
Range*
Illness Attitude Scale
27 questions; 5 point scale
0-108
Health anxiety
11 questions; 5 point scale
0-44
Illness behaviour
6 questions; 5 point scale
0-24
Mastery
Pearlin-Schooler
Mastery Scale
7 questions; 5 point scale
0-28
Life events last
12 months
numeric
Number of life events
0-15 #
Depression
Patient Health
Questionnaire
9 items of the DSM IV (algorithm)1 y/n
Variable
Key variables
Somatoform
problems
Severity score 2
0-27
y/n
y/n
Panic disorder
Patient Health
Questionnaire
First screening question positive
and >2 positive scores on the
second panic question3
Other anxiety
Patient Health
Questionnaire
First screening question positive
and >4 positive scores on the
second anxiety question4
Confounding variables
Somatic
morbidity5
Diabetes
y/n
Any chronic respiratory disease
y/n
Any chronic cardiovascular disease
y/n
Any cancer problem
y/n
Any locomotor problem
y/n
Any skin problem
y/n
Any digestive problem
y/n
Social problems5
Any social problem
y/n
Psychological
problems5
Any psychological problem
y/n
Medically
Unexplained
Symptoms5
Any medically
unexplained symptom
(according to Robbins6)
y/n
Demographic
patient data
Age
Linear
Sex
Male; female
Education
7 levels of education
1-7
Ethnicity
Dutch
y/n
Surinamese
y/n
Other
y/n
Living situation
Living alone (with small children)
y/n
Employment
Paid work or study
y/n
Body Mass Index
110
18- 93 #
Weight (kg)/ height (m)
WHY DO THEY KEEP COMING BACK?
2
16-48 #
Structure
Range*
Practice size
<1000; 1001-1250; 1251-1500;
>1500 patients
1-4
Special knowledge of/interest in a
specific part of general practice
Yes or no
y/n
Variable
Scale
GP characteristics
Paediatric medicine
y/n
Geriatric medicine
y/n
Minor surgical procedures
y/n
Management of the practice
y/n
Financial management
y/n
Professional organizations
y/n
Special knowledge of/interest in
(the treatment of):
2
3
4
5
6
7
8
1-5
Diabetes mellitus
1-5
Astma and/or COPD
1-5
Cardiovascular diseaeses
1-5
Please indicate what percentage of
patients with … disorders you manage
yourself:
*
#
1
5 point scale7
5 point scale 8
1-5
Anxiety
1-5
Depressive symptoms
1-5
Medically unexplained symptoms
1-5
Theoretical range unless stated otherwise.
Range observed.
The Algorithm method) scores the first 8 items as positive if the answers
are: (‘more than half the days’ or ‘nearly every day’) and as or negative if
the answers are (‘“not at all’ or ‘several days’). The ninth item is scored as
positive if the answer is (‘several days’ or ‘more than half of the days’ or ‘nearly
every day’) and is scored negative if the answer is (‘not at all’). Five or more
positive items is counted as presence of depression.
The “Severity score” scores all items with 0 (‘not at all’), 1 (‘several days’),
2 (‘more than half of the days’) or 3 (‘nearly every days’).
The range is from 0 to 27.
To score panic we assessed the two first panic questions of the PHQ. Panic was
deemed present if the first screening question was positive and 2 or more items
(out of 3 items) of the second panic question were positive. We did not use the
third question.
To score ‘other anxiety’ we assessed the two anxiety questions of the PHQ.
A patient scores positive for ‘other anxiety’ with a positive answer on the
screening question (Over the last 4 weeks, how often have you been bothered
by any of the following problems: feeling nervous, anxious, on edge, or
worrying a lot about different things?) and 4 or more (out of six) positive
answers (‘several days’ or ‘more than half of the days’) on the second question.
Problems on GPs’ problem list coded with the international classification of
primary care. See appendix B.
Robbins JM, Kirmayer LJ, Hemami S. Latent variable models of functional
somatic distress. J Nerv Ment Dis 1997; 185(10):606-615.
5 point scale: no special interest: little interest; normal interest; more than
normal interest; very much interest.
5 point scale: 0%; 25%; 50%; 75%; 100%
CHAPTER 8
111
Setting
Data were collected in 41 practices of GPs,
participants in the GP-based continuous
morbidity registration network of the
Department of General Practice at the
Academic Medical Center of the University
of Amsterdam. The practices are located
in health centres in a suburban part of
Amsterdam (39 practices) and in two
single-handed practices in a nearby
rural area. In the GP network, electronic
medical record data are routinely extracted
for research purposes.
Study population
All patients of 18 years or older enlisted
with the GPs between January 1, 2008 and
January 1, 2010, were potentially eligible
for this study. Patients were classified
based on the number of consultations with
the GP (consultations in the surgery and
house calls). Consultations with other
practice staff were excluded because these
contacts are mostly initiated by the GP
or his/her staff and very often involve
planned monitoring of chronic diseases.
Patients who according to their GP were
unable to participate because of severe
mental disease, mental retardation
or illiteracy (literate in neither Dutch
nor English) were excluded. Frequent
attenders were defined as those patients
whose attendance rate ranked in the top
10th centile of four age groups (18-30; 3145; 46-60; 61+ years), separately for men
and women.12;13 Frequent attendance was
determined for the years 2008 through
2011. Incident FA during one year (1yFAs)
was defined as attendance in the top
10th centile during 2009, but not in 2008.
112
Frequent attendance was defined as 2yFA
if 1yFAs were FA in one of the consecutive
years (2010 or 2011) or as persistent FAs
(pFAs) if 1yFAs were FA both in 2010 and
2011.
Follow-up procedure
From the list of eligible 1yFAs (FA in 2009,
but not in 2008), GPs excluded those
people who were unable to participate
because of severe mental disease, mental
retardation or illiteracy. Subsequently,
an invitation letter signed by their own
GP was sent to the selected patients. The
letter describing the study also contained
an informed consent form and the baseline
questionnaire. In case of no response
within two weeks, a reminder was sent.
All patients who returned the informed
consent were enrolled and received a
follow-up questionnaire after one and two
years.
Data quality
The patient questionnaires were
predesigned to enable scanning of the
results electronically (Saxion Market
Research; Post box 70.000, 7500 KB
Enschede, the Netherlands). Because
patients with missing data were telephoned
or emailed within 10 days to achieve
optimal completeness of data, we had
little missing data and saw no need to for
multiple imputation.
Outcome measure
Persistence of frequent attendance during
2010 or 2011 or both was the outcome.
WHY DO THEY KEEP COMING BACK?
Figure 1. Flow diagram
Selection in 41 general practices:
Total number of enlisted patients
•
total Na = 44,700
•
> 17 year: 34,899
Eligible Frequent Attenders
•
N = 2,311 (FAb in 2009, not
in 2008)
Exclusion by the GPc
N = 132
Invited for participation
N= 2,179
No response = 1,433
Response
N = 746
Refusal = 123
Participants T0
N = 623 d
•
•
Death = 6
Moved house = 8
•
•
Death = 8
Moved house = 8
Participants T1
N = 609 ; response 526
Participants T2
N = 593 (623-30)
Response = 511
Patients analysede:
N= 497
a
b
c
d
e
Number
Frequent Attender
General Practitioner
All with written consent
Patients with known frequent attender status in all 3 years
CHAPTER 8
113
were measured using the Patient
Health Questionnaire (PHQ).31 The
Potential psychosocial aetiological factors
The following instruments were used to
capture the potential aetiological factors
for persistence of FA:
1.
2.
Somatoform determinants: The
Illness Attitude Scales (IAS) measures
fears, attitudes and beliefs associated
with health anxiety and illness
behaviour.21-26 The validated subscale
for ‘health anxiety’ consists of eleven
items on five-point scales.23;24 The
validated subscale ‘illness behaviour’
has six items on the use of healthcare
and the impact of physical complaints
on work, concentration and leisure.
The four steps of the scales are
labelled from ‘no’ to ‘most of the time’.
Because the IAS subscale ‘illness
behaviour’ also measures use of
healthcare, which is our outcome, we
reanalysed our data after omitting the
healthcare use-related questions from
the IAS to avoid circular reasoning.
Locus of control (“mastery”) was
assessed by the 7-item PaerlinSchooler Mastery Scale, adapted
version.21;27-29 This scale measures
the extent to which one feels to be in
control over changes in one’s own life
(locus of control). Items are answered
on a 5-point scale ranging from
‘strongly disagree’ to ‘strongly agree’.
3.
Life events were assessed via the
Life Event Questionnaire (LEQ) to
measure a patient’s total number of
negative life events in the previous 3
and 12 months.30
4.
Depression and anxiety disorders
114
PHQ has been validated in FAs.32-34
We used the algorithm score to assess
depression (assessing the 9 items of
the Diagnostic and Statistical Manual
of Mental Disorders IV text revision,
DSM-IV-TR). To assess panic disorder
we used the two panic questions and
to assess ‘other anxiety’ the two other
anxiety questions of the PHQ. See
appendix 6 for the above mentioned
instruments.
Other (confounding) factors
We considered a large set of potential
confounders:
•
Demographic factors
•
(Somatic) problems as registered
by the GP on the problem list in the
electronic medical record (See the
box). For the definition of a medical
problem we refer to our previous
work.1
•
And GP characteristics and work style
were measured using a questionnaire
(see appendix 3). See the box for more
details.
Statistical analysis
Multilevel ordinal multiple logistic
regression analysis with GPs as a random
intercept was performed with persistence
of frequent attendance during zero, one or
two of the following years as the ordinal
outcome variable. We used a proportional
odds model combining two analyses: 1yFA
versus (2yFA and 3yFA) and (1yFA and
2yFA) versus 3yFA to show the associations
WHY DO THEY KEEP COMING BACK?
Table 1. Characteristics of Frequent Attenders who gave Informed Consent and who
refused Participation.
a
b
c
Informed
consent
Refused
participation
p-value
Na
623
1556
Age (mean, SDb)
52 (17)
45 (18)
0.00
Female, %
52.7
51.4
0.00
N of contacts with GP in 2009
(mean, SD)
9.1 (3.6)
8.2 (3.7)
0.00
N of problems on problem list(mean, SD)
2.7 (2.7)
2.2 (2.3)
0.00
Psychological problemsc (%, SD)
7.7 (20)
8.1 (20)
0.68
N indicates number
SD indicates standard deviation
Psychological problems as percentage of all problems on the problem list
of General Practitioners’ characteristics
and persistence of frequent attendance
(Table 3) and the associations between
our main variables and persistence of
frequent attendance (Table 4).The ordinal
logistic model assumes that a predictor’s
effect on the probability of zero years
frequent attendance versus one or two
years is the same as that for zero and 1
year versus two years. Therefore, a single
odds ratio expresses the effect of each
predictor. We measured illness attitude
and lack of mastery only at baseline and all
other variables at baseline and after one
and two years. We estimated the effect
of psychosocial factors while controlling
for demographic factors, somatic diseases
and GP characteristics. We also applied
a simpler model, using only the baseline
values of the aetiological factors. We
tested the proportional odds assumption
using the parallel lines test. We assumed
for all covariables in the model that the
difference between the log odds of being
a 3yFA and a 2yFA, respectively is the
same as the difference of the log odds of
being a 2yFA and 1yFA, respectively. A
priori defined interaction terms between
somatic, psychological and social factors
were considered using a binary logistic
model with 2yFA (versus 0 and 1yFA) as the
dependent variable. SPSS 20.0 for windows
was used for the analyses. We report
odds ratios and their corresponding 95%
confidence intervals.
Ethics approval
The study was conducted according to
the Dutch legislation on data protection
(Ministry of Justice, the Netherlands).
Ethics approval was waived by the Medical
Ethics Committee of the Academic Medical
Center of the University of Amsterdam. All
participants gave their written informed
consent.
CHAPTER 8
115
Table 2. Characteristics of 1 year, 2 year and 3 year Frequent Attenders at Baseline
Frequent attender status#
1yFAs*
2yFAs*
3yFAs*
Number
307
155
35
Age (mean,SD)
52 (15)
54 (18)
55 (14)
0.78
Female
52
51
49
0.88
Education: none or low
20
24
31
0.30
p-value
Paid work or study
61
48
41
0.009
Living alone or with children
30
37
38
0.23
Ethnicity
0,85
- Dutch %
83
79
85
- Surinamese %
7
9
6
Class of working hours (mean,SD)
3.64 (1.04)
3.74 (1.02)
3.80 (1.15)
0.74
Body mass index (mean,SD)
26.4 (5.0)
27.3 (5.2)
28.7 (5.8)
0.41
Mastery score (mean,SD)
18.89(5.27)
16.99(5.54)
16.15(6.26) 0.33
- Health anxiety (mean,SD)
11.15(7.97)
12.49(8.17)
13.67 (9.12) 0.55
- Illness behaviour (mean,SD)
8.95(4.43)
10.83(4.69)
12.82(4.73) 0.032
Number of life eventsb (mean,SD)
2.30 (2.38)
2.68 (2.37)
2.60(2.48) 0.68
4.08 (4.71)
6.07 (5.83)
8.61(6.08)
0.017
5
10
18
<0.001
a
Illness attitude scale (IAS)b
Depression score PHQ
(mean,SD)
c; b
Depression (PHQ) c
Panic complaints (PHQ)
4
7
17
0.013
Other anxiety (PHQ)
7
14
17
0.017
- Total number of problems
(mean,SD)
1.57(1.54)
1.86(1.77)
2.34(1.97)
0.18
- Any cardiovascular disease
39
36
27
0.76
- Any cancer diagnosis
10
7
6
0.62
- Any respiratory disease
17
21
26
0.33
- Any addiction
6
4
0
0.34
- Any social problem
2
3
3
0.69
- Any medically unexplained
symptoms
9
13
26
0.012
- Any psychological problem
8
7
9
0.86
- Any digestive tract problem
13
15
26
0.15
- Any locomotor tract diagnosis
15
23
37
0.003
- Any skin disease
9
10
11
0.83
Problems on GP’s Problem listd
Legend on page 117
116
WHY DO THEY KEEP COMING BACK?
Legend of table two, on page 116
a
Number of working hours in 5 classes:1 (1 – 10 hours), 2 (11 – 20 hours),
3 (21 – 30 hours), 4 (31 – 40 hours) and 5 (more than 40 hours)
b
PHQ means Patient Health Questionnaire
c
We used the algorithm score to assess depression (assessing the 9 items of the
Diagnostic and Statistical Manual of Mental Disorders IV text revision,
DSM-IV-TR).
d
Problems registered by the General Practitioner in the electronic medical file
(definition of a problem in previous work 1)
#
1yFAs indicates frequent attenders (FAs) in 2009, but not in 2010 and 2011;
2yFAs indicates FAs in 2009 and 2010 or 2009 and 2011; 3yFAs indicates FAs in
2009, 2010 and 2011
*
Numbers are percentages unless stated otherwise
†
We used the Chi-square test or a one-way-Kruskal-Wallis ANOVA test
depending whether the variable was categorical or quantitative.
Results
General practitioners’ characteristics
The cohort of frequent attenders
The average practice size of the 41
participating GPs was 1,419 enlisted
patients (range, 849-2,792) and 82% of GPs
indicated their participation in academic
medical education or research. After
correction for patient characteristics,
intra-class correlations for general
practices were small indicating hardly
any clustering within GPs. The GP
characteristics significantly associated
with persistent frequent attendance were
special interest in diabetes mellitus (OR
1.40; 95%CI from 1.02 to 1.91; per point
on a 5-point Likert scale.) and interest in
performing minor surgical procedures
(yes/no; OR 1.48; 1.05 to 2.08). See Table 3.
Our sampling frame consisted of 44,700
patients who were enlisted with the
participating GPs of whom 34,899 were
18 years or older. Of these 2,311 patients
fulfilled the criteria for incident FA. GPs
excluded 132 patients for inclusion because
of illiteracy, severe mental health problems
or mental retardation. Of the 2,179 patients
eligible for participation, 746 (34%)
returned the questionnaire and of these
623 (29%) gave informed consent (figure 1).
Compared to non-consenters, consenting
individuals were older, more often female,
had contacted the GP more often in 2009
and had more problems on the problem list.
(See Table 1)
Characteristics of the cohort at baseline and
after one, and two years
Table 2 shows the characteristics of the
cohort at baseline. Persistent FAs were
less likely to be in paid work and scored
higher on illness behaviour, depression,
panic disorder and other anxiety. Finally
they had more medically unexplained
symptoms and locomotor problems on
their problem lists (GPs’ patients file).
Psychosocial aetiology of persistent frequent
attendance
We performed an ordinal logistic
regression with remaining a frequent
attender during zero, one or, two years
of follow-up as the outcome. See Table
4. Measured at baseline, panic disorder
(OR 5.40; 1.67 to 17.48), other anxiety
(OR 2.78; 1.04 to 7.46), illness behaviour
(per additional point on the scale; OR
1.13; 1.05 to 1.20) and lack of mastery (per
CHAPTER 8
117
Table 3. Associations of General Practitioners Characteristics and persistence of
frequent attendance*
95%-CIc
p-valued
1.03
0.75-1.41
0.87
50 (8)
1.00
0.98-1.02
0.84
17 (9)
1.00
0.98-1.02
0.69
Anxiety
2.85 (0.77)
1.07
0.84-1.37
0.56
Depression
3.05 (0.71)
1.18
0.89-1.54
0.24
Medically unexplained
symptoms
3.65 (0.70)
0.99
0.72-1.36
0.96
Diabetes
3.18 (0.64)
1.40
1.02-1.91
0.04
Respiratory diseases
3.13 (0.72)
1.04
0.82-1.33
0.72
Cardiovascular diseases
3.35 (0.53)
1.22
0.85-1.75
0.29
1.04-2.08
0.03
number/mean
(%/SDa)
OR
Female gender
23 (56%)
Age
Years of experience
b
Special interest in managinge
Special interest in a specific part of General Practice (yes/no) f
Minor surgical procedures, n/%.
a
b
c
d
e
16 (39)
1.48
SD: standard Deviation
Odds Ratio
95% confidence interval
probability value
Five levels of interest (from 1 (no special interest) to 5 (very much interest)) and
5 levels of percentage of patients treated by the GP (0%-100%).
Special interest (Y/N) in paedriatic medicine, geriatric medicine and
management/financial aspects of care were not significantly correlated.
Based on a multilevel ordinal regression analysis with two levels (GP and the pa
tient) with persistence of frequent attendance during 2010 or 2011 or both
as the outcome. The Akaike Information Criterion (AIC) of ordinary logistic
model was 1086.80, the AIC of ramdom effects logistic regression model
1084.03 (p-value 0.029).
f
*
additional point on the scale; OR 1.08; 1.01
to 1.15) increased persistence of frequent
attendance.
Measured over all 3 years, other anxiety
(OR 2.0; 1.29 to 3.10) and the number of
life events in 3 years (OR 1.06; 1.01-1.10
per event; range of 0 to 12), increased
the chance of persistence of frequent
attendance. The analysis showed a 5.6
percent increase in the odds of remaining
a frequent attender for every additional
negative life event (OR 1.06; 1.01 to 1.10).
118
This means that for a patient with for
example three negative life events in
3 years, the odds of repeated frequent
attendance was 18 percent higher than
for a similar person without negative life
events ((1.056)3). Psychosocial patient
variables of GPs’ electronic records were
not significantly related to repeated
frequent attendance.
We tested the parallel lines assumption
underlying the ordinal model and found
that for all variables, except the total
WHY DO THEY KEEP COMING BACK?
addictive problems summed over three
years, the p-values were > 0.52. Overall,
we interpreted this finding as supportive
for the more parsimonious model whose
parallel lines test p-value was 0.78.
Additional effect on persistence of frequent
attendance of (combinations of ) psychological, social and somatic problems
The probabilities of becoming a pFA were
0.16 (95%CI from 0.06 to 0.25), 0.12 (0.03
to 0.21) and 0.13 (0.06 to 0.19) for presence
of any somatic, any psychological and any
social problem, respectively. See figure
2. However, we found no evidence that
the effects (odds ratios) of combinations
of these factors were larger than those
predicted on the basis of multiplying the
odds ratios of separate effects (p-values for
interactions > 0.25; logistic models tests
interactions on a multiplicative scale).
Discussion
In a cohort of incident frequent attenders
prospectively followed during two
years, we found that presence of a panic
disorder, presence of other anxiety, the
occurrence of negative life events in the
previous year (all measured at baseline
and over all three years), illness behaviour
and lack of mastery (both measured at
baseline) were associated with persistent
frequent attendance during one or two
of the following two years. Presence of a
combination of chronic somatic disease
with social and/or psychological problems
gave no rise to effects over and above what
might be expected based on their separate
effects. We found no strong evidence of
effects of GP characteristics.
Strengths of this study
The prospective design with the clear
focus on psychosocial determinants
provides a good insight into aspects of the
psychosocial aetiology of persistence of
frequent attendance. The large variability
in FAs included in this study yielded ample
analytical contrast to robustly estimate
associations of many of the determinants
with persistence of frequent attendance.35
For example, the number of life events
varied between 0 and 12 and the mastery
scale from 5 to 26 (Table 2).36 The design
with three annual questionnaires and data
from GPs’ patient files provided us with a
rich database. The tests for psychological
problems have been specifically validated
in FAs. We also tested for an enhancing
effect of combinations of somatic,
psychological and social determinants but
found none.
We achieved good data quality without
imputation of missing data by automated
scanning of predesigned questionnaires
and a rigorous phoning and mailing
approach of patients in case of missing
data.
We also used morbidity prevalence data
of a GP database in which GPs register
medical problems over a long period
of time. As most GPs receive regular
feedback on their registration activities,
these registration data are of good quality,
especially for somatic and psychological
problems. 37;38 As GPs register these
problems during consultations, the
quality of this registration may be better
for frequent attenders who have many
consultations.
CHAPTER 8
119
Table 4. Results from a multilevel ordinal logistic regression model with 0, 1 or 2 years
as a frequent attender during follow-up1
Results of the Patient Questionnaire
OR*
95% CI*
P-value #
1.06
1.01-1.11
0.02
Total over 3 years2
Life events during last 12 months
Major depression
1.22
0.91-1.62
0.19
Other anxiety
2.00
1.29-3.10
0.002
Panic disorder
1.63
0.89-2.99
0.11
Life events during last 12 months3
1.09
0.95-1.24
0.21
3
1.08
1.01-1.15
0.02
Measured at baseline
Lack of mastery
Major depression
0.62
0.18-2.09
0.44
Other anxiety
2.78
1.04-7.46
0.04
5.40
1.67-17.48
0.01
Health anxiety
1.04
1.00-1.08
0.07
Illness behaviour3
1.13
1.05-1.20
<0.001
Illness behaviour without use of healthcare 4
1.14
1.03-1.26
0.01
Any addictive behaviour
0.68
0.37-1.23
0.20
Any social problem
1.25
0.53-2.97
0.61
Panic disorder
3
Results from the Electronic Medical Record
Total over 3 years
Any medically unexplained symptom
0.81
0.53-1.24
0.34
Any other psychological problem
0.89
0.59-1.36
0.60
Any addictive behaviour
0.17
0.02-1.79
0.14
Any social problem
1.84
0.21-16.08
0.58
Any medically unexplained symptom
0.93
0.26-3.33
0.91
Any other psychological problem
0.44
0.12-1.65
Measured at baseline
1.
2.
3.
4.
*
#
Based on a multilevel ordinal regression analysis with two levels (GP and the
patient). Persistence of frequent attendance during 2010 or 2011 or both was the
outcome. Each of the variables was modelled separately after correcting for the set
of confounders: age, gender, education, ethnicity, living situation, work, body mass
index, total number of problems, Chronic Obstructive Pulmonary Disease/asthma,
chronic vascular diseases, cancer, skin, locomotor tract disorders and digestive tract
disorders.
The sum or the mean of the values of a predictor across the three time points.
Per extra life event or extra point on the used scales.
Ilness behaviour without questions about use of healthcare but including questions
about impact on work, concentration and leisure.
OR indicates Odds Ratio; CI indicates Confidence Interval.
The p-values are Wald tests (estimated parameters / standard error).
120
WHY DO THEY KEEP COMING BACK?
proportion of pFA patients
Figure 2. The probability of persistence of frequent attendance in 2010 and 2011
(pFA) in primary care patients who attended frequently in 2009 (and not
in 2008) versus all other cohort patients depending on the presence of
any (combination of) chronic somatic, psychological or social problems at
baseline.1
0,35
0,30
0,25
0,20
0,15
00,10
0,05
P
P
at
ic
al
+
So
m
So
ci
So
og
ic
Ps
al
+
yc
h
ol
So
og
ci
ic
al
+
al
+
ic
at
m
So
al
ic
og
ol
Ps
yc
h
ol
Ps
yc
h
ci
al
ic
at
+
yc
h
So
m
So
ol
P
P
P
ci
ic
og
at
m
Ps
So
al
al
P
ic
P(
#)
no
P
0,00
1
2
3
4
#
Probability for pFA 2
95%CI3
SE4
Number of P #
0.06
0.00-0.12
0.03
Any somatic P
0.16
0.06-0.25
0.05
Any psychological P
0.12
0.03-0.21
0.05
Any social problem
0.13
0.06-0.19
0.03
somatic+psychological P
0.25
0.13-0.36
0.06
somatic+social P
0.20
0.12-0.29
0.04
psychological+social P
0.23
0.17-0.28
0.03
somatic+psychological+social P
0.29
0.25-0.34
0.02
The presence of problems was taken from the electronic medical records of
the general practitioners. Bars indicate proportions; antennas are standard
errors; pFA is persistent frequent attender.
pFA means persistent frequent attendance, frequent attendance during 20092011
CI mens Confidence Interval
SE means standard error
P means Problems; probability per extra problem
CHAPTER 8
121
Limitations of this study
We see the following limitations. First,
we used a proportional definition of FA.
Although in our opinion this definition
makes sense, its arbitrary cut-off of
90% has evident disadvantages as some
patients may drop just below the cut-off
(89th centile e.g.) the next year. However,
definitions based on some absolute
number of visits share this limitation.
Second, registration in GP practices has its
limitations.37-39 Some registered problems
could be overreported if resolved problems
are not removed, in recurrent (for instance
housing problem) or temporary diseases
(for instance a depressive episode). This
could lead to overestimation of their
prevalence and to bias in the estimations
of the effect of psychological and social
factors on persistence of frequent
attendance.40 Fourth, the participating
GPs appeared relatively similar on some
potential risk factors such as interest in
psychosocial diagnosis and treatment:
Eighty-two percent of the GPs were
involved in educating medical students,
vocational training of future GPs and/or
research activities. Also, GPs might have
tended to answer positively when asked
about their special interests in medical
issues and treatments. This may lead
to underestimation of the effects of GP
characteristics, if any. The association
of interest in surgical procedures and
diabetes with persistence of frequent
attendance may be explained by more
follow-up consultations in patients with
these problems. Fifth, although we
collected many patient characteristics
and clinical data, there may of course be
undocumented determinants of pFA. For
122
example, in this study we had no data on
perceived health status and quality of
life, which are both inversely associated
with persistence of frequent attendance.10
Sixth, this study originates in the Dutch
healthcare system with a strong and
well-organized primary care in which
most costs are covered by insurances and
GPs try to provide continuity of care and
integrated care (somatic and psychosocial
care). This specific context may restrict the
generalisability of our results to countries
with a comparable healthcare system such
as, for example, the United Kingdom or
Health Maintenance Organizations in the
United States.41 For reasons of feasibility,
we chose well known, validated, but easy
to use questionnaires and not diagnostic
interviews to assess depression, panic
disorder (PHQ) and somatoform disorders
(IAS). This may have resulted in some
misclassification of depression, anxiety
and somatoform disorders.23;32;34 Finally,
about two thirds of the eligible 1yFAs
refused to participate in our study. Because
we focus on aetiology and ample analytical
contrast, representativeness is not the issue
and we do not think this influenced our
results negatively.40 We analysed a cohort
of new FAs and our results are therefore
limited to frequent attendance during 3
years and we cannot determine whether
our results are applicable to frequent
attendance of longer duration.
Relevant literature
The literature about the causes of
persistent FA is inconsistent and its
straightforward interpretation is
hampered by methodological differences
(aetiological and causal versus predictive
WHY DO THEY KEEP COMING BACK?
noncausal outlooks or confusion about
these two) and different definitions of
frequent attendance (proportional versus
fixed cutoff point). In prospective cohort
studies, using a proportional definition,
low physical quality of life, low educational
level and psychological distress (Hopkins
Symptom Check List and Whiteley-7)
predicted persistence of frequent
attendance in the next two consecutive
years.7;10 Using a fixed cutoff definition of
FA, one study found that female gender,
obesity, former frequent attendance, fear of
death, alcohol abstinence, low satisfaction,
and irritable bowel syndrome were
risk factors for persistence of frequent
attendance during at least three out of the
four later years.42 Another study concluded
that the Ambulatory Diagnosis Groups
“unstable chronic medical conditions”,
“see and reassure conditions”, “minor
time-limited psychosocial conditions”, and
“minor signs and symptoms” predicted
persistence of frequent primary care
use the next year.15 We explicitly chose
a proportional definition of frequent
attendance per age and sex group.12;13;43
This hampers a comparison with the
results of studies that chose fixed numbers
of consultations to select FAs.15;42 We
confirmed the association of psychological
distress and pFA.7
In the Eighties some authors postulated
that inadequate interpersonal dynamics
between patients and their GP could cause
more, inappropriate and unnecessary
consultations, testing and treatments.
These authors also emphasized that
families tend to be consistent in illness
and consultation patterns over the years
and generations.16-18;44-46 However, in
our study we found little evidence of
associations between GP characteristics
and persistence of FA. This may suggest
that patient determinants are more
important in explaining persistence
of frequent attendance than GP
characteristics, although a larger and
more diverse group of GPs and more
detailed information about the GPs may be
needed to corroborate this. In our study
about healthcare expenditures of FAs we
hypothesized that the higher costs of FAs
in primary and secondary care could be
explained by not yet diagnosed medical
problems.20 The results of this prospective
cohort shows that undiagnosed anxiety
and somatoform disorders, life events
and poor mastery may partly explain this
frequent use of (primary) healthcare by
persistent FAs.
Clinical and public health implications
Frequent attenders of primary care
and persistent FAs in particular, have
more somatic, social and psychological
problems and incur higher costs than
non-FAs. 1;20 Our results imply that in
1yFAs, repeated FA is increased by anxiety,
illness behaviour (also after omission from
the IAS scale of the questions about use
of healthcare), negative life events and
low mastery and that, if our findings are
valid, a proportion of pFA is preventable
by eliminating these causes.47-51 Thus,
adequate detection and treatment of these
conditions in FAs may result in a better
quality of life of these patients and a
decrease in attendance and costs. As most
somatic problems in this patient group are
already dealt with relatively effectively
CHAPTER 8
123
in usual GP care, the largest effects are
likely to be gained by care (programmes)
which address psychological problems
(panic, other anxiety, depression) of
the involved patients and which try to
strengthen the self-efficacy of patients
(mastery).52 Although treatment of anxiety
and depression has been shown to be
effective 53-59, the effect of this treatment
in preventing persistence of FAs is
unclear and needs to be demonstrated in
research.60
anxiety disorders, illness behaviour,
negative life events and poor mastery
over one’s life were found to be associated
with persistence of frequent attendance
after adjustment for a large set of
confounders. GPs appeared to contribute
little to persistence of frequent attendance,
although participating GPs may have been
too similar to detect potential features of
importance.
In light of the budget problems in many
healthcare systems and the high costs
of (persisting) FAs not explained by
known morbidity, we think it might be
beneficial for these patients and might
reduce expenditures to develop and test
interventions to diminish persistence of
frequent attendance.6;60
We thank the GPs involved in the Network
of General Practitioners of the Academic
Medical Centre-University of Amsterdam
(HAG-net-AMC) for their continuous
efforts to keep the electronic medical
records updated and their support during
this study and Alice Karsten, Gerda
van Zoen and Nienke Buwalda for their
logistical support.
Acknowledgments
Implications for further research
More incident FAs, using psychiatric
interviews and measures of quality of life
are needed to provide more insight in
the difference between PHQ diagnoses
and diagnoses after a Structured Clinical
Interview for DSM Disorders (SCID
diagnosis) and the role of Quality of life
measures. Subsequently, randomised
trials may determine the extent to which
interventions aimed at modifying anxiety
disorders, illness behaviour and mastery
in this specific group of patients improve
quality of life and reduce attendance and
costs of (persistent) frequent attenders.
We’d like to give a special tribute for our
deceased colleague, Leo Beem, for his
helpful statistical work at the beginning of
this project.
Conflicts of interests:
The authors have no competing interests
to report.
Funding:
This study was financed by a grant from
the Netherlands Organisation for Health
Research and Development (ZonMw);
Alledaagse ziekten no. 42011002.
Conclusion
In patients who frequently attended their
general practitioners for one year, panic,
124
WHY DO THEY KEEP COMING BACK?
References
(1) Smits FT, Brouwer HJ, ter Riet G., van
Weert HC. Epidemiology of frequent
attenders: a 3-year historic cohort study
comparing attendance, morbidity and
prescriptions of one-year and persistent
frequent attenders. BMC Public Health
2009; 9(1):36.
(10) Rifel J, Svab I, Selic P, Rotar Pavlic
D, Nazareth I, Car J. Association of
Common Mental Disorders and Quality
of Life with the Frequency of Attendance
in Slovenian Family Medicine Practices:
Longitudinal Study. PLoS ONE 2013;
8(1):e54241.
(2) Ward AM, Underwood P, Fatovich
B, Wood A. Stability of attendance
in general practice. Fam Pract 1994;
11(4):431-437.
(11) Koskela TH, Ryynanen OP, Soini EJ.
Risk factors for persistent frequent
use of the primary health care services
among frequent attenders: a Bayesian
approach. Scand J Prim Health Care
2010; 28(1):55-61.
(3) Botica MV, Kovacic L, Tiljak MK, Katic
M, Botica I, Rapic M et al. Frequent
attenders in family practice in Croatia:
Retrospective study. Croatian Medical
Journal 2004; 45(5):620-624.
(4) Carney TA, Guy S, Jeffrey G. Frequent
attenders in general practice: a
retrospective 20-year follow-up study. Br
J Gen Pract 2001; 51(468):567-569.
(5) Andersson S-O, Lynoe N, Hallgren
C-G, Nilsson M. Is frequent attendance
a persistent characteristic of a patient?
Repeat studies of attendance pattern
at the family practitioner. Scandinavian
Journal of Primary Health Care 2004;
22(2):91-94.
(6) Smits FT, Brouwer HJ, Zwinderman AH,
Mohrs J, Smeets HM, Bosmans JE et al.
Morbidity and doctor characteristics only
partly explain the substantial healthcare
expenditures of frequent attenders: a
record linkage study between patient
data and reimbursements data. BMC
Fam Pract 2013; 2013(1):138.
(7) Vedsted P, Fink P, Olesen F, MunkJorgensen P. Psychological distress
as a predictor of frequent attendance
in family practice: a cohort study.
Psychosomatics 2001; 42(5):416-422.
(8) Tomenson B, McBeth J, Chew-Graham
CA, Macfarlane G, Davies I, Jackson J et
al. Somatization and health anxiety as
predictors of health care use. Psychosom
Med 2012; 2012(6):656-664.
(9) Vedsted P, Fink P, Olesen F, MunkJorgensen P. Psychological distress
as a predictor of frequent attendance
in family practice: A cohort study.
Psychosomatics: Journal of Consultation
Liaison Psychiatry /9; 42(5):416-422.
(12) Vedsted P, Christensen MB. Frequent
attenders in general practice care: a
literature review with special reference to
methodological considerations. Public
Health 2005; 119(2):118-137.
(13) Smits FT, Mohrs J, Beem E, Bindels
PJ, van Weert HC. Defining frequent
attendance in general practice. BMC
Fam Pract 2008; 9(1):21.
(14) McDaniel SH, Campbell T, Seaburn D,
van EJ, Grol R, Huygen F et al. Treating
Somatic Fixation: A Biopsychosocial
Approach: When patients express
emotions with physical symptoms. Soc
Sci Med 1982; 1982(13):717-725.
(15) Naessens JM, Baird MA, Van Houten
HK, Vanness DJ, Campbell CR.
Predicting persistently high primary care
use. Ann Fam Med 2005(4):324-330.
(16) Rosendal M, Fink P, Bro F, Olesen F.
Somatization, heartsink patients, or
functional somatic symptoms? Towards
a clinical useful classification in primary
health care. Scand J Prim Health Care
2005; 2005(1):3-10.
(17) Huygen FJ. Family Medicine- The
medical life history of families. Assen,
The Netherlands: van Gorcum; 1978.
(18) van den Bosch WJ, Huygen FJ, van
den Hoogen HJ, van Weel C. Morbidity
in early childhood: family patterns in
relation to sex, birth order, and social
class. Fam Med 1993; 1993(2):126-130.
(19) Tielens VC. Consulten van huisartsen.
Meppel: Krips Repro; 1987.
CHAPTER 8
125
(20) Smits FT, Brouwer HJ, Zwinderman
AH, Mohrs J, Smeets HM, Bosmans
JE et al. Morbidity and doctor
characteristics only partly explain the
substantial healthcare expenditures of
frequent attenders: a record linkage
study between patient data and
reimbursements data. BMC Fam Pract
2013(1):138.
(21) Sirri L, Grandi S, Fava GA. The Illness
Attitude Scales. A clinimetric index
for assessing hypochondriacal fears
and beliefs. Psychother Psychosom
2008;77(6):337-350.
(22) Kellner R, Abbott P, Winslow WW,
Pathak D. Fears, beliefs, and attitudes in
DSM-III hypochondriasis. J Nerv Ment
Dis 1987(1):20-25.
(23) Speckens AE, Spinhoven P, Sloekers
PP, Bolk JH, van Hemert AM. Illness
Attitudes Scale dimensions and their
associations with anxiety-related
constructs in a nonclinical sample. J
Psychosom Res 1996; 1996(1):95-104.
(24) Speckens AEM, Spinhoven P, Sloekers
PPA, Bolk JH, van Hemert AM. A
validation study of the Whitely Index,
the Illness Attitude Scales, and the
Somatosensory Amplification Scale in
general medical and general practice
patients. J Psychosom Res 1996;
40(1):95-104.
(31) Spitzer RL, Kroenke K, Williams JB.
Validation and utility of a self-report
version of PRIME-MD: the PHQ primary
care study. Primary Care Evaluation
of Mental Disorders. Patient Health
Questionnaire. JAMA 1999; 282(18):17371744.
(32) Wittkampf K, van RH, Baas K, van
de Hoogen H, Schene A, Bindels P
et al. The accuracy of Patient Health
Questionnaire-9 in detecting depression
and measuring depression severity in
high-risk groups in primary care. Gen
Hosp Psychiatry 2009; 31(5):451-459.
(33) Baas KD, Wittkampf KA, van Weert
HC, Lucassen P, Huyser J, van den
Hoogen H et al. Screening for depression
in high-risk groups: prospective cohort
study in general practice. The British
Journal of Psychiatry 2009; 194(5):399403.
(34) Wittkampf KA, Baas KD, van Weert
HC, Lucassen P, Schene AH. The
psychometric properties of the panic
disorder module of the Patient Health
Questionnaire (PHQ-PD) in high-risk
groups in primary care. J Affect Disord
2010:Nov.
(35) Miettinen O.S. Theoretical
Epidemiology: principles of occurrence
research in medicine. New York: Wiley;
1985.
(25) Kellner R. Hypochondriasis and
somatization. JAMA 1987; 1987(19):27182722.
(36) Rothman K, Greenland S. Modern
Epidemiology. Philadelphia: LippincottRaven Publishers; 1998.
(26) Sirri L, Fava GA, Sonino N. The
Unifying Concept of Illness Behavior.
2013.
(37) Brouwer HJ, Bindels PJ, van Weert
HC. Data quality improvement in general
practice. Fam Pract 2006; 23(5):529536.
(27) Pearlin LI, Schooler C. The structure of
coping. J Health Soc Behav 1978(1):2-21.
(28) Pearlin LI, Lieberman MA, Menaghan
EG, Mullan JT. The stress process. J
Health Soc Behav 1981(4):337-356.
(29) Moser DK, Dracup K. Psychosocial
recovery from a cardiac event: the
influence of perceived control. Heart
Lung 1995(4):273-280.
(30) Saxe LL, Abramson LY. The life events
scale, reliability an validity. Unpublished
manuscript.; 1987.
126
(38) van den Dungen CHN, Boshuizen
HC, van den Akker M, Biermans MC, van
Boven K., Brouwer HJ et al. What factors
explain the differences in morbidity
estimations among general practice
registration networks in the Netherlands?
A first analysis. Eur J Gen Pract. 2008;14
Suppl 1:53-62
(39) van den Dungen C, Hoeymans
N, Boshuizen HC, van den Akker M,
Biermans MC, van BK et al. The influence
of population characteristics on variation
in general practice based morbidity
estimations. BMC Public Health 2011;
11:887.
WHY DO THEY KEEP COMING BACK?
(40) Rothman K, Greenland S, Lash T.
Modern epidemiology. Philadelphia, PA
(USA): Lippincott Williams & Wilkins;
2008.
(41) Dunlop S, Coyte PC, McIsaac W. Socioeconomic status and the utilisation of
physicians’ services: results from the
Canadian National Population Health
Survey. Soc Sci Med 2000; 51(1):123-133.
(42) Koskela TH, Ryynanen OP, Soini EJ.
Risk factors for persistent frequent
use of the primary health care services
among frequent attenders: a Bayesian
approach. Scand J Prim Health Care
2010; 28(1):55-61.
(43) Luciano JV, Fernandez A, Pinto-Meza
A, Lujan L, Bellon JA, Garcia-Campayo
J et al. Frequent attendance in primary
care: comparison and implications of
different definitions. Br J Gen Pract 2010;
60(571):49-55.
(44) van Eijk J, Grol R, Huygen F, Mesker
P, Mesker-Niesten J, van MG et al.
[Somatic fixation. Prevention by the
general practitioner. Soc Sci Med 1982;
1982(13):717-725.
(45) McDaniel SH, Campbell T, Seaburn
D. Treating Somatic Fixation: A
Biopsychosocial Approach: When
patients express emotions with physical
symptoms. Can Fam Physician 1991:451456.
(46) Cardol M, van den Bosch WJHM,
Spreeuwenberg P, Groenewegen PP, van
Dijk L, de Bakker DH. All in the Family:
Headaches and Abdominal Pain as
Indicators for Consultation Patterns in
Families. The Annals of Family Medicine
2006; 4(6):506-511.
(47) Cuijpers P, van Straten A, Schuurmans
J, van Oppen P, Hollon S, Cuijpers
P. Psychotherapy for chronic major
depression and dysthymia: A metaanalysis. Clin Psychol Rev 2010 febr;
30(1):51-62
(48) Cuijpers P, van Straten A, Warmerdam
L. Problem solving therapies for
depression: A meta-analysis. European
Psychiatry 2007; 22(1):9-15.
(49) Reger MA, Gahm GA. A metaanalysis of the effects of Internet- and
computer-based cognitive-behavioral
treatments for anxiety. Journal of Clinical
Psychology 65[1], 53-75. 2009.
CHAPTER 8
127
(50) van der Feltz-Cornelis C, van der
Feltz-Cornelis C. Effect of psychiatric
consultation models in primary care. A
systematic review and meta-analysis
of randomized clinical trials. Journal of
Psychosomatic Research 2010;68(6).
(60) Smits FT, Wittkampf KA, Schene AH,
Bindels PJ, van Weert HC. Interventions
on frequent attenders in primary care. A
systematic literature review. Scand J Prim
Health Care 2008; 26(2):111-116.
(51) Morriss R, Kai J, Atha C, Avery A,
Bayes S, Franklin M et al. Persistent
frequent attenders in primary care: costs,
reasons for attendance, organisation
of care and potential for cognitive
behavioural therapeutic intervention.
BMC Fam Pract 2012:39.
(52) Samoocha D, Bruinvels DJ,
Elbers NA, Anema JR, van der Beek
AJ. Effectiveness of web-based
interventions on patient empowerment:
a systematic review and meta-analysis. J
Med Internet Res 2010(2):e23.
(53) Cuijpers P, van SA, van SA, Andersson
G. Psychological treatment of depression
in primary care: a meta-analysis. Br J Gen
Pract 2009; 59(559):51-60.
(54) Cuijpers P, van Straten A, Andersson
G, van Oppen P. Psychotherapy for
depression in adults: A meta-analysis of
comparative outcome studies. Journal
of Consulting and Clinical Psychology
2008; 76(6):909-922.
(55) Donker T, Griffiths KM, Cuijpers P,
Christensen H. Psychoeducation for
depression, anxiety and psychological
distress: a meta-analysis. BMC Med 2009
Dec 16;7:79
(56) Goldberg D. The “NICE Guideline”
on the treatment of depression.
Epidemiologia e Psichiatria Sociale Vol 15
(1), Jan -Mar 2006;-15.
(57) Kendall T, Cape J, Chan M, Taylor C,
Kendall T, Cape J et al.
Management of generalised anxiety
disorder in adults: summary of NICE
guidance. BMJ 2011(4):318-327.
(58) Pilling S, Mayo-Wilson E. Recognition,
assessment and treatment of social
anxiety disorder: summary of NICE
guidance. BMJ 2013; 346.
(59) National Collaborating Centre for
Mental Health. Generalised Anxiety
Disorder in Adults: Management in
Primary, Secondary and Community
Care. 2011.
128
WHY DO THEY KEEP COMING BACK?
CHAPTER 8
129
chapter 9
IS SYSTEMATIC DETECTION AND
TREATMENT OF DEPRESSION AND
ANXIETY IN FREQUENT ATTENDERS
COST-EFFECTIVE IN COMPARISON
WITH USUAL CARE BY GENERAL
PRACTITIONERS? A MODELLING
STUDY
Judith Bosmans, Frans Smits, Veerle
Coupé, Aart Schene, Henk van
Weert, Gerben ter Riet.
Article submitted
ABSTRACT
Background
Frequent attenders (FAs) are defined as patients with an age
and sex-adjusted attendance rate ranking in the top 10 centile
within a time frame of one year. Many FAs have underlying
psychiatric morbidity that may not always be detected and
treated by their General Practitioner (GP).
Objective
To evaluate if systematic detection and treatment of depression
and anxiety in FAs is cost-effective in comparison with usual
GP care and whether this should be initiated after 1 or 2 years
of frequent attendance.
Methods
A Markov model was developed to simulate the course of a
cohort of 10,000 one-year FAs (1yFAs) over a period of 5 years.
Main outcomes were years spent as non-FA without depression
or anxiety, and Quality-Adjusted Life-Years (QALYs). Several
treatment scenarios were simulated with treatment effects
expressed as risk reductions of 10%, 20%, and 40% compared
with usual care. Usual care consisted of the natural course of a
cohort of FAs in Dutch primary care around 2011. Uncertainty
was estimated using Monte Carlo simulation.
Results
Expected increases in years spent as non-FA without depression
or anxiety and QALYs were small in all treatment scenarios.
Treatment of 1yFAs resulted in larger health benefits and more
cost savings than treatment of 2yFAs. The 95% credibility
intervals around expected cost and effect differences were
wide and included no effect. Treatment was cost-effective or
dominant in comparison with usual care only if treatment was
assumed to result in a spillover effect on FA-ship.
Conclusion
Systematic detection and treatment of depression and anxiety
in FAs does not seem to be cost-effective.
132
WHY DO THEY KEEP COMING BACK?
Introduction
In primary care, patients who consult
more often than their peers have a
disproportionate effect on the workload
of General Practitioners (GPs).1, 2 Because
frequency of attendance is strongly
associated with age and sex, 3 it is
recommended to define frequent attenders
(FAs) as patients with an age and sexadjusted attendance rate ranking in the top
10 centile within a time frame of one year.4,
5
Such a proportional threshold allows for
meaningful comparison between practices,
periods, and countries. FAs in primary care
are not only frequent users of GP services,
but also of other healthcare services such
as emergency medical care services and
hospital services leading to high healthcare
costs.6-8
FAs tend to have lower education levels,
and more medical and psychiatric
morbidity than non-frequent attenders
(non-FAs).2, 6, 9 Between 80% and 90% of
the FAs frequently attend their GP for 1 or
2 years only10-13. Studies have shown that
patients who are a frequent attender for
2 or more consecutive years have more
chronic somatic diseases, social problems,
medically unexplained somatic symptoms
and psychiatric problems than one-year
frequent attenders.2, 14, 15 Moreover, they
have a lower quality of life and lower
education levels.16
Smits et al systematically reviewed
the evidence on the effectiveness of
interventions aimed at FAs in influencing
morbidity, quality of life and healthcare
utilization rates. The interventions
included in their review varied greatly
in content, and were not considered
effective.17 More recent studies showed
that more intensive interventions aimed at
healthcare providers or patients resulted
in reduced medical care utilization18-20,
although effects were generally small
(decrease in healthcare utilization 1.5 to 6
visits per year in comparison with usual
care).
Because many FAs have underlying
psychiatric morbidity that may not always
be detected or diagnosed by their GP, it has
been suggested that systematic detection
and treatment of underlying disorders
might improve quality of life and reduce
consultation rates.21, 22 We developed a
Markov model to assess whether such
an intervention may be cost-effective
compared to usual care and whether
the best moment to intervene is after 1
or 2 years of frequent attendance. To do
this we extrapolated the findings from a
cohort study among one-year FAs over a
period of 5 years and combined this with
potential treatment effects using modeling
techniques.
Methods
Design
We developed a Markov model in which
the course of a cohort of primary care
patients who frequently attended their GP
during one year (1yFAs) in Dutch primary
care (i.e. usual care) was extrapolated over
a period of 5 years and linked to cost data
from a large healthcare insurer in The
Netherlands. Transition probabilities for
the model were estimated using the 1 year
follow-up from the prospective cohort
study described below.
CHAPTER 9
133
Table 1. Model parameters used in the Markov model:costs, utility weights and
treatment effects.
Costs (¤) per year
Psychological treatment in primary care
¤500
nonFA
¤2400
FA duration
(years)
Depression
Anxiety
Unknown or
no morbidity
Successful
treatment
1
¤6300
¤13900
¤4500
--
2
¤12400
¤4200
¤4400
¤4400
>2
¤12000
¤6300
¤8100
¤8100
FA
NonFA
Depression
0.56 {Rifel}*
0.62 {Siskind 2010}{Paulden 2009}{Sado 2009}
{Siskind 2008}
Anxiety
0.55 {Rifel}*
0.66 {Konig 2009}
Unknown or no
morbidity
0.57{Rifel}*
0.85 {Sobocki 2008}{Burstrom 2001}{Johnson
2000}
Successful
treatment
0.65†
Utility weights
Treatment effects (Risk reduction)
Effect of
treatment on
disorder under
consideration
Spillover
Spillover effect
effect on other on FA status
disorder
Usual care scenario
0%
0%
0%
Alternative scenarios
10%
0%/10%
0%/10%
20%
0%/20%
0%/20%
40%
0%/40%
0%/40%
100%
100%
100%
Best case scenario
*
†
Based on unpublished data of Rifel et al[1].
Assumed that successful treatment of an underlying psychiatric disorder leads
to an increase in utility of 0.1.
134
WHY DO THEY KEEP COMING BACK?
Figure 2. Cost-effectiveness acceptability curves for scenarios involving a risk
reduction of 20% for depression and anxiety without spillover effects on FA
status.
1
scenario 3
0,9
scenario 6
0,8
scenario 8
0,7
probability cost-effective
0,6
0,5
0,4
0,3
0,2
0,1
0
0
5000
10000
15000
20000
25000
30000
25000
40000
45000
50000
threshold
Cohort study
A three-year prospective cohort study was
performed in seven primary healthcare
centres in Amsterdam, The Netherlands.8
All patients of 18 years and older registered
at the participating GPs in 2007, 2008,
2009 and 2010 were eligible for this cohort
study.
Patients were classified according to
their frequent attendance status based on
information in the GP’s electronic medical
record system. FAs were defined as those
patients whose attendance rate ranked
in the top 10th centile of four age groups
(18-30 years; 31-45 years; 46-60 years; 61
years+) for men and women separately.
Frequent attendance was determined for
each of the years 2007, 2008, 2009 en 2010.
Patients could frequently attend during
1 year (1-year frequent attenders, 1yFA),
2 years (2-year frequent attenders, 2yFA)
or 3 years or more (persistent frequent
attenders, pFA). Patients who were not
a frequent attender in any of these years
were classified as non-frequent attenders
(non-FAs).
Underlying morbidity
The presence of depression and anxiety
(panic disorder and other anxiety)
was assessed using the Patient Health
Questionnaire (PHQ) at the beginning
of 2010 and again after 1 year.23 We used
the algorithm score to assess depression
(assessing the 9 items of the DSM-IVTR). To assess panic disorder we used
the two panic questions and to assess
CHAPTER 9
135
‘other anxiety’ the other two anxiety
questions of the PHQ. Patients who were
both depressed and anxious according
to the PHQ were classified as being
depressed. Patients who were neither
depressed nor anxious according to the
PHQ were classified as having unknown
or no morbidity. Patients in this state may
have no morbidity or another underlying
different FA states.
disorder, such as a somatization disorder,
that might (partly) explain the FA status of
these patients, but whose exact nature was
unknown to us.
no or unknown morbidity.
Cost data
To obtain realistic data on costs of primary
and secondary care, and prescription
medication, data from the prospective
cohort study were linked to a database
with reimbursement claims from Achmea/
Agis, a large healthcare insurer in The
Netherlands.24 Linking was performed
using a unique and obligatory “citizen
service number” by a certified trusted
third party.8 Table 1 lists the cost estimates
per year for the different FA states.
Quality-adjusted life-years
Utility weights were estimated based
on available literature.16 Utility weights
express the relative desirability of a health
state on a scale of 0 (‘dead’) to 1 (‘perfect
quality of life’). For example, a utility
score of 0.56 indicates that a patient is
in a health state that is valued as 56% of
perfect health. Using these utility weights,
Quality-Adjusted Life-Years (QALYs) were
calculated by multiplying the utility weight
associated with a given FA state by the
number of person-years spent in that state.
Table 1 lists the utility weights for the
136
Model structure
In the Markov model, 1yFAs were classified
into three categories: depression, anxiety,
or no or unknown morbidity. Figure 1
shows a simplified model for 1yFAs with
depression. The full model contains
parallel chains for 1yFAs with anxiety and
After one year, a 1yFA may become a 2
year frequent attender (2yFA) or a nonfrequent attender (non-FA) either with
depression or anxiety, or no or unknown
morbidity. A 2yFA may remain a frequent
attender during the following year and,
thus, become a persistent frequent attender
(pFA) or go to a non-frequent attender state
either with depression, anxiety or no or
unknown morbidity. The model assumes
that people who go from a frequent
attender state to a non-frequent attender
state remain in that state indefinitely. If a
patient has been successfully treated for
depression or anxiety, the patient remains
1 year in a state reflecting this. It was
assumed that, after 1 year in this state, a
patient moves to the state of being a nonFA with no or unknown morbidity.
Treatment scenarios
The Markov model was used to evaluate
the cost-effectiveness of systematic
detection and treatment of depression and
anxiety in frequent attenders compared
to usual care. Treatment effects were
incorporated in the model as relative risk
reductions. Thus, the probability of moving
from a state with depression or anxiety to
any other state with depression or anxiety,
WHY DO THEY KEEP COMING BACK?
respectively, was reduced by 10, 20 or
40 percent points. For example, using a
treatment effect of 40% the probability of
going from the state 1yFA+depression to
2yFA+depression is reduced from 0.10 to
0.06.
Different treatment scenarios were
evaluated (see Table 1). Firstly, treatment
could be initiated in 1yFAs or 2yFAs.
Secondly, treatment could be aimed at
FAs with depression, FAs with anxiety,
or both at FAs with depression and FAs
with anxiety. Thirdly, spillover effects
on psychiatric morbidity and frequent
attender status were modeled. This allows
that, for example, a treatment aimed at
depression also decreases the probability
to become anxious or remain a frequent
attender. A best case scenario was also
modeled in which risk reductions of 100%
were assumed for depression, anxiety and
FA status.
In accordance with recent guidelines for
depression and anxiety, treatment was
assumed to consist of psychotherapy given
by a psychologist in primary care. Based
on Baas et al, we assumed that patients
receive on average 6.1 treatment sessions
25
that were valued using the standard
price for a psychologist (€80).26 This was
rounded up to €500 per patient treated.
Usual care
The reference scenario was the scenario
based on the transition probabilities
observed in the cohort study. This can be
considered the course under circumstances
of usual care received by frequent
attenders in general practice. Usual care in
this cohort was provided in a well-serviced
multi-ethnic setting in Amsterdam, The
Netherlands in the years between 2007 and
2010.
In the Netherlands, the GP has a gatekeeper function for care. Dutch primary
care guidelines for treatment of depression
recommend education and short-term
psychological therapy. Only in cases
of severe depression, referral and/
or antidepressants are recommended.
Dutch guidelines for anxiety recommend
education and short-term psychotherapy
if preferred. In persistent cases, cognitive
behavioural therapy or prescription of
antidepressants is recommended. Grol
et al showed that on average 61% of the
guideline recommendations is followed in
Dutch general practice.27
Cost-effectiveness analyses
The cost-effectiveness of the various
treatment scenarios as compared to usual
care was estimated by simulating the FA
trajectories of a cohort of 10,000 1yFAs
over a period of 5 years with a cycle length
of 1 year. For each treatment scenario, the
number of years in a non-FA state with
unknown or no morbidity, QALYs and costs
were estimated. Costs were discounted
at 4% and effects at 1.5% annually
as recommended by Dutch costing
guidelines.26 We calculated Incremental
Cost-Effectiveness Ratios (ICERs) for each
scenario in comparison with the reference
scenario by dividing the difference
in discounted costs between the two
scenarios by the difference in discounted
effects.
CHAPTER 9
137
WHY DO THEY KEEP COMING BACK?
0.10 0.02 0.01 0
0.06 0.04 0.03 0
0.39 0.27 0.17
var
0
0
0
0
0.02 0.07 0.03 0*
0.12
2yFA +depression
2yFA +anxiety
2yFA +unknown
2yFA +Tx succes
pFA +depression
pFA +anxiety
pFA +unknown
pFA +Tx succes
nonFA +depression
nonFA +anxiety
nonFA +no morbidity 0.31
0
1yFA +unknown
0
0
0
0
0
0
0.15
var
0*
0*
var
0.39 0.31
0.11
0.06 0.15
0
0
0
0
0.04 0.11
0
0
0
0
0
0
0
2yFA+anxiety
n=13
0
0
0
0
0
0
0
0
2yFA+Tx succes
n=0
0
0.01 0
0.03 0
0
0.34 0
0.02 0
0.03 0
0
0
0
0
0
0
0
2yFA+unknown
n=104
0.42 0.72 0.33 0.38 0.58 1
0.18
0
0
0
0
var
0
0
0
0
0
1yFA +anxiety
0
0
1yFA +depression
1yFA+unknown
n=359
State T1
2yFA+depression
n=18
1yFA+depression
n=49
State T0
pFA+depression
n=14
0
0
0
0
0
0
0
pFA+anxiety
n=15
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0.27 0.07 0
0
0.07 0*
0
0
0
0.07 0.20 0.40 1
0.07 0.07 0.03 0
0.14
0
0.43 0.20 0.49 0
0.21
0.07 0.20 0.01 0
0
0
0
0
0
0
0
pFA+unknown
n=75
Table 2. Yearly transition probabilities in a cohort study among 1 year frequent
attenders. The probabilities presented in this table relate to one year frequent
attenders in a usual care setting.
pFA+Tx succes
n=0
138
1yFA+anxiety
n=45
State T0
State T1
1yFA
2yFA
pFA
nonFA
unknown
Tx success
*
= state at beginning of the model cycle;
= state at the end of the model cycle;
= 1 year frequent attender;
= 2 year frequent attender;
= persistent frequent attender;
= non-frequent attender;
= unknown morbidity other than depression or anxiety;
= state after successful treatment of either depression or anxiety
These transition probabilities are 0 due to the relatively small number
of patients in these states. In the probabilistic sensitivity analysis,
these probabilities are estimated based on a beta distribution.
nonFA+
depression, n=0
0
0
0
0
0
0
0
0
0
0
0
nonFA+anxiety
n=0
0.50 0
0
0
0
0
0
0
0
0
0
0
0
0
0.50 0.50 1
0*
0.50 0
0
0
0
0
0
0
0
0
0
0
0
nonFA+no
morbidity, n=0
Figure 1. Simplified flowchart of the Markov model for one year frequent attenders
(1yFAs) with depression. The full model contains parallel chains for
1yFAs with
anxiety or unknown morbidity.
1YFA
+depression
1yFA
2yFA
pFA
nonFA
unknown or no morbidity
Tx success
anxiety
2YFA
+depression
pFA
+depression
NonFA
+depression
2YFA
+anxiety
pFA
+anxiety
NonFA
+anxiety
2YFA
+ unknown
or no
morbidity
pFA
+ unknown
or no
morbidity
NonFA
+ unknown
or no
morbidity
2YFA
+Tx succes
pFA
+Tx succes
1 year frequent attender;
2 year frequent attender;
persistent frequent attender;
non-frequent attender;
unknown morbidity other than depression or anxiety, or no
morbidity;
state after successful treatment of either depression or
Probabilistic sensitivity analysis
Probabilistic sensitivity analysis was
performed by specifying beta distributions
for all transition probabilities to represent
uncertainty in their estimation. Next,
Monte Carlo simulation was employed
to randomly select values from those
distributions.28 Uncertainty estimates
were obtained by simulating 1000 times
the course of a cohort of 10,000 1yFAs.
Ninety-five percent credible intervals
(95% CIs) around costs and effects were
estimated based on the 2.5 and 97.5 centiles
of the 1000 simulation estimates for costs
and effects. Results were presented per
1,000 FAs. Cost-effectiveness acceptability
curves were estimated for the scenarios
involving risk reductions of 20% without
spillover effects on FA status using the netbenefit approach.29 These curves show the
probability that a scenario is cost-effective
in comparison with the other scenarios for
different thresholds for willingness-to-pay.
All analyses were performed using Excel
2010.
CHAPTER 9
139
Results
From the prospective cohort study, data
was available on frequent attender status
and psychiatric morbidity (depression
and anxiety) at two time points one year
apart for 692 FAs. Over 2009, there were
453 1yFAs, 135 2yFAs, and 104 pFAs. Of
the 1yFAs, 49 were depressed, 45 were
anxious and 359 were neither depressed
nor anxious, but could have unknown
morbidity or no morbidity. Of the 2yFAs, 18
were depressed, 13 were anxious and 104
had other, unknown or no morbidity. For
pFAs, these numbers were 14, 15 and 75 for
depression, anxiety and other, unknown or
no morbidity, respectively.
Reference scenario
The trajectories of FAs under the reference
scenario are represented by the transition
probabilities in Table 2 which were
based on the observed transitions in the
prospective cohort study. Zero indicates
that these transitions are theoretically
impossible, while starred zeroes indicate
transitions that are possible but that did
not occur in the prospective cohort. A
probability of 1 indicates that patients who
reach this FA state remain in this state
indefinitely. Table 2 shows that after 1
year 55% of the 1yFAs with depression had
become a 2yFA. For 1yFAs with anxiety
and 1yFAs with no or unknown morbidity
this was 33% and 21%, respectively. Of
the 2yFAs with depression, anxiety and
unknown morbidity, 56%, 61%, and 39%,
respectively, had become a pFA after a
year. Seventy-two percent, 66% and 57%
of the pFAs with depression, anxiety and
no or unknown morbidity, respectively,
140
had remained a pFA after a year. Thus, the
longer a person resided in a FA state, the
higher the probability that s/he remained
in a FA state.
Of the 1yFAs with depression and the 1yFAs
with anxiety, 70% and 69%, respectively,
did not have either of these disorders a year
later. For the 2yFAs with depression and
the 2yFAs with anxiety, these figures were
72% and 69%, respectively, and for the
pFAs with depression and the pFAs with
anxiety, 50% and 40%, respectively. Thus,
in about two-thirds of 1yFAs and 2yFAs
with depression or anxiety these disorders
had disappeared after 1 year. Persistent
FAs, however, were more likely to remain
depressed or anxious.
Model-based 5 year predictions for a
cohort of 1,000 1yFAs under the reference
scenario are shown in the first row of
Table 3. On average, 4,322 out of 5000
person-years (86% of time) were expected
to be spent as a non-frequent attender,
4,502 person years (90% of time) without
depression or anxiety, and 4,087 personyears (82% of time) as a non-frequent
attender without depression or anxiety.
The number of QALYs expected over 5
years per 1,000 1yFAs was 3,927.
Treatment of 1yFAs
Table 3 shows estimates of the expected
outcomes and costs per 1,000 1yFAs over
a period of 5 years by treatment scenario.
Overall, the expected effects of systematic
treatment of depression and/or anxiety
in 1yFAs were small and 95% credibility
intervals (CrI) were wide. Even in the
best case scenario that assumed that the
treatment was fully effective (100% risk
WHY DO THEY KEEP COMING BACK?
reduction for depression, anxiety and FA
status), the number of years of being a
non-frequent attender without morbidity
increased by only 4.5% (186 person-years,
95%CrI 38 to 334) and the number of
QALYs by 1.1% (44 QALYs, 95%CrI 5 to 78)
in comparison with the reference scenario.
A cost reduction of 2.5% (-€330,710,
95%CrI -970,077 to 311,325) was expected
under the best case scenario in comparison
with the reference scenario. In general,
differences in years without being a FA
and without morbidity, differences in
QALYs and cost differences between the
depression treatment scenarios and the
reference scenario were more positive than
between the anxiety treatment scenarios
and usual care.
Table 3 shows that using the commonly
accepted threshold of €20,000/QALY in
The Netherlands, depression treatment
scenarios with risk reductions of 10%
with spillover effects on anxiety and FA
status and of 20% with a spillover effect
on anxiety (scenarios 4 and 6) were
cost-effective in comparison with the
reference scenario. This also applied for
the anxiety treatment scenarios with risk
reductions of 20% with spillover effects
and with risk reductions of 40% (scenarios
15 to 19), and the depression and anxiety
treatment scenario with risk reductions
of 10% with spillover effects (scenario 21).
Depression treatment scenarios assuming a
treatment effect of 20% on depression and
spillover effects on anxiety and FA status,
and of 40% regardless of spillover effects
(scenarios 7 tot 10) dominated (i.e. lower
costs and larger effects) the reference
scenario just as treatment scenarios for
depression and anxiety with treatment
effects of at least 20% with spillover
effects.
Figure 2 shows the cost-effectiveness
acceptability curve for the scenarios 3, 6
and 8. This curve shows that when taking
statistical uncertainty into account,
scenario 3 is cost-effective in comparison
with scenarios 6 and 8 for thresholds until
5000 €/QALY and scenario 8 for higher
thresholds. However, the probabilities of
cost-effectiveness do not differ greatly
between scenarios.
Treatment of 2yFAs
Table 4 shows astimates of the expected
outcomes and costs per 1,000 1yFAs
after 2 years of frequent attendance by
treatment scenario. Effects of treatment
after 2 years of frequent attendance were
smaller than treatment of 1yFAs. In the
best case scenario, the expected increase
in the number of person-years in a nonFA state without anxiety or depression
was 1.2% (48, 95%CrI -103 to 192) and in
QALYs 0.33% (13, 95%CrI -30 to 50) as
compared with the reference scenario. In
this scenario, cost savings in comparison
with the reference scenario were 1.3%
(-€175,268, 95%CrI -803,271 to 536,320).
Expected cost savings and effects in
comparison with the reference scenario for
anxiety treatment scenarios were larger
than for depression treatment scenarios.
The incremental cost-effectiveness
ratios in the last two columns of Table
4 show that using a cost-effectiveness
threshold for QALYs of 20,000 €/QALY,
only treatment scenarios assuming a risk
reduction of 10% or 20% without spillover
CHAPTER 9
141
Table 3. Expected costs, outcomes differences in costs and outcomes and incremental
cost-effectiveness ratios in one year frequent attenders (1yFAs) per 1,000
1yFAs.
FA = frequent attender; QALY = Quality-Adjusted Life-Year; Tx = treatment.
1.
2.
3.
4.
142
Rifel J, Svab I, Selic P, Rotar Pavlic D, Nazareth I, Car J: Association of common
mental disorders and quality of life with the frequency of attendance in
Slovenian family medicine practices: longitudinal study.
PLoS One 2013, 8(1):e54241.
Siskind D, Araya R, Kim J: Cost-effectiveness of improved primary care
treatment of depression in women in Chile. Br J Psychiatry 2010, 197(4):291296.
Paulden M, Palmer S, Hewitt C, Gilbody S: Screening for postnatal depression in
primary care: cost effectiveness analysis. BMJ 2009, 339:b5203.
Sado M, Knapp M, Yamauchi K, Fujisawa D, So M, Nakagawa A,
Kikuchi T, Ono Y: Cost-effectiveness of combination therapy versus
antidepressant therapy for management of depression in Japan. Aust N Z J
Psychiatry 2009, 43(6):539-547.
WHY DO THEY KEEP COMING BACK?
5.
6.
7.
8.
9.
Siskind D, Baingana F, Kim J: Cost-effectiveness of group psychotherapy for
depression in Uganda. J Ment Health Policy Econ 2008, 11(3):127-133.
Konig HH, Born A, Heider D, Matschinger H, Heinrich S, Riedel-Heller SG, Surall
D, Angermeyer MC, Roick C: Cost-effectiveness of a primary care model for
anxiety disorders. Br J Psychiatry 2009, 195(4):308-317.
Sobocki P, Ekman M, Ovanfors A, Khandker R, Jonsson B: The cost-utility of
maintenance treatment with venlafaxine in patients with recurrent major
depressive disorder. Int J Clin Pract 2008, 62(4):623-632.
Burstrom K, Johannesson M, Diderichsen F: Swedish population health-related
quality of life results using the EQ-5D. Qual Life Res 2001, 10(7):621-635.
Johnson JA, Pickard AS: Comparison of the EQ-5D and SF-12 health surveys in
a general population survey in Alberta, Canada. Med Care 2000, 38(1):115-121.
CHAPTER 9
143
Table 4. Expected costs, outcomes, differences in costs and outcomes and incremental
cost-effectiveness ratios of treatment in two year frequent attenders (2yFAs)
per 1,000 1yFAs.
FA = frequent attender; QALY = Quality-Adjusted Life-Year; Tx = treatment.
144
WHY DO THEY KEEP COMING BACK?
CHAPTER 9
145
effects (scenarios 2, 3, 5 and 11) were not
cost-effective as compared to the reference
scenario. Using this threshold, all other
scenarios were either cost-effective in
comparison with the reference scenario
(scenarios 4, 6, 8, 12, 14, 17, 20 and 22)
or dominated the reference scenario
(scenarios 7, 9, 10, 13, 15, 16, 18, 19, 21 and 23
to 26).
Discussion
Summary of main findings
Using a Markov model, we evaluated the
cost-effectiveness of systematic detection
and treatment of depression and anxiety
after 1 or 2 years of frequent attendance
compared with usual care as provided in a
multi-ethnic setting in Amsterdam.
In all scenarios, 95%CrIs around expected
cost and effect differences were wide and
included the possibility of no difference.
Treatment of 1yFAs with depression or
anxiety led to larger cost savings and
health benefits than treatment of 2yFAs.
Assuming of spillover effects on FA status
and psychiatric morbidity had a substantial
influence on ICERs. Scenarios including
such spillover effects were more often
cost-effective compared to the reference
scenario (using a threshold of 20,000
€/QALY) and more often dominated
the reference scenario than scenarios
excluding these effects.
Comparison with existing literature
In the prospective cohort study our model
was based on, approximately two-thirds
of the FAs had recovered from anxiety
or depression after 1 year. This is high
146
in comparison with recovery rates of
50% under usual care reported in the
literature.30, 31 It may be that the frequent
attenders in the prospective cohort study
our model was based on already received
some form of care for their underlying
morbidity which may partly explain their
increased healthcare utilization rates.
Earlier studies showed no or only minimal
effects of psychological treatments aimed
at undiagnosed psychiatric morbidity
in frequent attenders.17 More recent
studies suggest that interventions aimed
at primary care providers or cognitive
interventions aimed at somatising patients
reduced medical care utilization, although
effects were generally small.18-20 Our model
shows that, against a background of a
well-serviced multi-ethnic setting, even
when treatments are considered to be fully
effective, the benefits in terms of costs and
effects are likely to be small.
It has been suggested that FAs have
unrecognized morbidity and that
treatment of this underlying morbidity
will resolve their FA-ship thereby reducing
healthcare costs of FAs.21, 22 However, our
model suggests that systematic detection
and treatment of depression and anxiety
after 1 or 2 years of frequent attendance
results in only limited cost savings (2.5%
at maximum) in comparison with the
reference scenario.
Baas et al showed that systematic
screening for depression in a high
risk population including FAs was not
effective, because of low rates of treatment
initiation.32 We assumed that uptake
of treatment was 100%, but in clinical
WHY DO THEY KEEP COMING BACK?
practice this will probably be much lower.
Therefore, the effects of systematic
detection and treatment of depression
and anxiety in frequent attenders were
probably overestimated in this study.
Assumptions in the model
Firstly, we assumed that people who
moved to a non-FA state remained in that
state indefinitely. The most important
reason for this choice was that we did
not have enough data to estimate the
transitions from a non-frequent attender
state to a 1-year frequent attender state
reliably. In addition, incorporation of this
transition would have greatly complicated
the model by further increasing the
number of possible transitions. We expect
that this assumption resulted in an
overestimation of the potential benefits
of systematic detection and treatment of
psychiatric morbidity in FAs. Secondly,
many frequent attenders stop being a
frequent attender after 1 year, because the
problem causing the frequent attendance
is resolved within this first year. However,
it may also be hypothesized that the longer
the duration of FA-ship, the greater the
chance that s/he will become a FA again.
However, we did not have data available to
include this effect. Therefore, we limited
the time horizon of the model to 5 years.
We expect that a longer time horizon
would have led to less favourable results.
Thirdly, we assumed that patients could
have only one disorder at a time to avoid
complicating the model further. However,
presence of depression and anxiety
simultaneously may negatively influence
the success rate of treatment, thus leading
to an overestimation of benefits in terms of
costs and effects (Alpert, J; 2001).
Strengths and weaknesses
We modeled fixed risk reductions of
treatment on psychiatric morbidity of 10%,
20% and 40%. This range is in line with
recovery rates of psychotherapy reported
in the literature.30 This can be considered
strength of this study, because it indicates
the boundaries of the effects that can be
potentially gained by systematic detection
and treatment of depression and anxiety
in frequent attenders. Another important
strength is that transition probabilities
were estimated using data from a
prospective cohort study among frequent
attenders. Although some transitions
were rare and could not be estimated
precisely, we nevertheless expect that this
study design feature greatly enhances the
generalizability of our results. However,
there are also a number of limitations to
our study. First, only healthcare costs
were included. However, absenteeism
costs may be an important contributor
to the total societal costs imposed by
frequent attenders. Thus, our estimates
may underestimate the potential cost
savings, since one might expect that
scenarios with larger health benefits also
result in lower costs due to absenteeism.
Second, diagnoses of depression and
anxiety were based on self-report using
the PHQ questionnaire and not on a
clinical diagnostic instrument. A recent
review, however, showed that the PHQ
performs well as a screening instrument
for depression in high risk groups such as
FAs.33 The performance of the PHQ in
diagnosing anxiety disorders, however,
is only moderate.34 Thus, we probably
missed some cases of depression and
anxiety, while we also misclassified some
CHAPTER 9
147
patients as being depressed or anxious.
However, since the PHQ is also likely to
be used in primary care when initiating
systematic detection, we expect that
our results are a good estimation of the
potential effects of systematic detection
and treatment of psychiatric morbidity
in FAs. Finally, following recent Dutch
primary care guidelines we assumed that
treatment of psychotherapy consisted of
short-lasting psychotherapy. Provision
of psychotherapy is more expensive
than prescription of antidepressants.
However, the effect of antidepressants
is probably overestimated in depression,
although people with anxiety disorders
probably respond better to antidepressant
treatment. Thus, modelling of treatment
with antidepressants would have resulted
in lower treatment costs, but this probably
has to be balanced against smaller effects.
carefully weighed whether the potential
benefits outweigh the efforts required
from GPs to implement such a programme.
Future research should indicate which
treatments are effective in treating
psychiatric morbidity in FAs, whether it is
reasonable to assume spillover effects of
such treatments on FA status and whether
there are specific subgroups, such as e.g.
FAs who express a need for treatment, in
whom treatment is more effective.
Conclusion and recommendations
In conclusion, systematic diagnostic
assessment and treatment of depression
and anxiety in FAs results in minimal cost
savings and health effects in comparison
with FAs receiving usual care in a wellserviced multi-ethnic primary care setting.
Moreover, uncertainty surrounding
the cost and effect estimates was large,
precluding strong conclusions. Based
on the results of this study, systematic
screening and treatment of psychiatric
morbidity does not seem indicated. Such
programmes can only be considered
cost-effective or dominant in comparison
with usual care if these treatments are
associated with a spillover effect on FAship. However, even then it should be
148
WHY DO THEY KEEP COMING BACK?
References
1. Neal, R.D., et al., Frequency of patients’
consulting in general practice and
workload generated by frequent
attenders: comparisons between
practices. Br.J Gen.Pract, 1998. 48(426):
p. 895-898.
2. Smits, F.T., et al., Epidemiology of
frequent attenders: a 3-year historic
cohort study comparing attendance,
morbidity and prescriptions of one-year
and persistent frequent attenders. BMC.
Public Health, 2009. 9: p. 36.
3. Little, P., et al., Psychosocial, lifestyle,
and health status variables in predicting
high attendance among adults. Br J Gen
Pract, 2001. 51(473): p. 987-94.
4. Smits, F.T., et al., Defining frequent
attendance in general practice. BMC.Fam
Pract, 2008. 9: p. 21.
5. Vedsted, P. and M.B. Christensen,
Frequent attenders in general
practice care: a literature review with
special reference to methodological
considerations. Public Health, 2005.
119(2): p. 118-137.
6. Kersnik, J., I. Svab, and M. Vegnuti,
Frequent attenders in general practice:
quality of life, patient satisfaction, use of
medical services and GP characteristics.
Scand J Prim Health Care, 2001. 19(3): p.
174-7.
11. Vrca, B.M., et al., Frequent attenders in
family practice in Croatia: retrospective
study. Croat.Med J, 2004. 45(5): p. 620624.
12.Carney, T.A., S. Guy, and G. Jeffrey,
Frequent attenders in general practice:
a retrospective 20-year follow-up study.
Br.J Gen.Pract, 2001. 51(468): p. 567-569.
13.Andersson, S.O., et al., Is frequent
attendance a persistent characteristic of
a patient? Repeat studies of attendance
pattern at the family practitioner. Scand.J
Prim.Health Care, 2004. 22(2): p. 91-94.
14.Koskela, T.H., O.P. Ryynanen, and E.J.
Soini, Risk factors for persistent frequent
use of the primary health care services
among frequent attenders: a Bayesian
approach. Scand J Prim Health Care,
2010. 28(1): p. 55-61.
15.Naessens, J.M., et al., Predicting
persistently high primary care use. Ann
Fam Med, 2005. 3(4): p. 324-30.
16.Rifel, J., et al., Association of common
mental disorders and quality of life with
the frequency of attendance in Slovenian
family medicine practices: longitudinal
study. PLoS One, 2013. 8(1): p. e54241.
17. Smits, F.T., et al., Interventions on
frequent attenders in primary care. A
systematic literature review. Scand.J
Prim.Health Care, 2008. 26(2): p. 111-116.
7. Svab, I. and L. Zaletel-Kragelj, Frequent
attenders in general practice: a study
from Slovenia. Scand J Prim Health Care,
1993. 11(1): p. 38-43.
18.Adam, P., et al., Effects of team care
of frequent attenders on patients and
physicians. Fam Syst Health, 2010. 28(3):
p. 247-57.
8. Smits, F.T., et al., Morbidity and doctor
characteristics only partly explain the
substantial healthcare expenditures of
frequent attenders: a record linkage
study between patient data and
reimbursements data. BMC Fam Pract,
2013. 14: p. 138.
19.Bellon, J.A., et al., Successful GP
intervention with frequent attenders in
primary care: randomised controlled trial.
Br.J.Gen.Pract., 2008. 58(550): p. 324330.
9. Ferrari, S., et al., Frequent attenders
in primary care: impact of medical,
psychiatric and psychosomatic
diagnoses. Psychother Psychosom,
2008. 77(5): p. 306-14.
10.Ward, A.M., et al., Stability of attendance
in general practice. Fam.Pract., 1994.
11(4): p. 431-437.
20.Barsky, A.J., et al., A Randomized Trial of
Treatments for High-Utilizing Somatizing
Patients. J Gen Intern Med, 2013.
21.Katon, W., et al., Distressed high utilizers
of medical care. DSM-III-R diagnoses and
treatment needs. Gen Hosp Psychiatry,
1990. 12(6): p. 355-62.
CHAPTER 9
149
22.Dowrick, C.F., J.A. Bellon, and M.J.
Gomez, GP frequent attendance in
Liverpool and Granada: the impact of
depressive symptoms. Br J Gen Pract,
2000. 50(454): p. 361-5.
23.Spitzer, R.L., K. Kroenke, and J.B.
Williams, Validation and utility of a
self-report version of PRIME-MD: the
PHQ primary care study. Primary Care
Evaluation of Mental Disorders. Patient
Health Questionnaire. JAMA, 1999.
282(18): p. 1737-1744.
24.Smeets, H.M., N.J. de Wit, and A.W.
Hoes, Routine health insurance data
for scientific research: potential and
limitations of the Agis Health Database. J
Clin Epidemiol, 2011. 64(4): p. 424-430.
25.Baas, K.D., et al., Brief cognitive
behavioral therapy compared to general
practitioners care for depression in
primary care: a randomized trial. Trials,
2010. 11: p. 96.
31.Gilchrist, G. and J. Gunn, Observational
studies of depression in primary care:
what do we know? BMC Fam Pract,
2007. 8: p. 28.
32.Baas, K.D., et al., Screening for
depression in high-risk groups:
prospective cohort study in general
practice. Br J Psychiatry, 2009. 194(5): p.
399-403.
33.Wittkampf, K.A., et al., The psychometric
properties of the panic disorder module
of the Patient Health Questionnaire
(PHQ-PD) in high-risk groups in primary
care. J Affect Disord, 2011. 130(1-2): p.
260-7.
34.Wittkampf, K., et al., The accuracy
of Patient Health Questionnaire-9 in
detecting depression and measuring
depression severity in high-risk groups
in primary care. Gen.Hosp.Psychiatry,
2009. 31(5): p. 451-459.
26.Hakkaart-van Roijen, L., S.S. Tan,
and C.A.M. Bouwmans, Handleiding
voor kostenonderzoek: Methoden en
standaard kostprijzen voor economische
evaluaties in de gezondheidszorg.
Geactualiseerde versie 2010. [Dutch
manual for costing in economic
evaluations]. 2011, College voor
zorgverzekeringen (CVZ): Diemen.
27.Grol, R., et al., Attributes of clinical
guidelines that influence use of
guidelines in general practice:
observational study. BMJ, 1998. 317(7162):
p. 858-861.
28.Briggs, A.H., et al., Probabilistic analysis
of cost-effectiveness models: choosing
between treatment strategies for
gastroesophageal reflux disease. Med
Decis.Making, 2002. 22(4): p. 290-308.
29.Stinnett, A.A. and J. Mullahy, Net
health benefits: a new framework for
the analysis of uncertainty in costeffectiveness analysis. Med Decis
Making, 1998. 18(2 Suppl): p. 68-80.
30.Cuijpers, P., et al., The effects of
psychotherapies for major depression
in adults on remission, recovery and
improvement: A meta-analysis. J Affect
Disord, 2014. 159C: p. 118-126.
150
WHY DO THEY KEEP COMING BACK?
CHAPTER 9
151
general
discussion
1. General discussion
The aim of this thesis was to provide more insight in frequent attenders (FAs) and
persistence of frequent attendance in Dutch General Practice. Our main objectives
were to define a method to select FAs in a normal practice situation, to study
morbidity of (persistent) FAs, to determine the workload and costs of healthcare use
of (persistent) FAs, to examine whether it would be possible to predict persistence
of frequent attending and to determine which in particular psychosocial factors
may explain this persistence. Finally we reviewed the literature on effective
treatments for FA and we evaluated whether detection and treatment of depression
and anxiety after one or two years of frequent attendance might be cost-effective
compared to usual GP care as provided in The Netherlands.
2. Results
Part 1. Mapping frequent attenders in primary care
The first research question addressed how to select FAs in a regular GP practice. FAs
are patients who consult their general practitioner (GP) much more often than their
peers. As consultation frequency is strongly dependent on sex and age, we used a
proportional definition and defined FAs as the top 10% of attenders per sex and age
group. Using such a definition also had the advantage of comparability with other
countries, regions and practices. To calculate attendance we used all face-to-face
contacts with the GP during one year (consultations in the office and house-calls)
and the attendance rates of all enlisted patients. We showed that, in a real life GP
practice situation, dividing the practice population into, at least, three age-bands
per gender is an acceptable method to select FAs, which can be used by practicing
GPs.1
152
WHY DO THEY KEEP COMING BACK?
For the second research question we investigated the somatic, psychological and
social problems of FAs. What are the differences between short-term and longterm FAs in this respect? What is the workload of a GP caused by (persisting) FAs?
A retrospective study in the Hag-net-AMC database showed that most frequent
attendance is temporary: Of all FAs during one year (1yFAs), 15.4 % persisted in
frequent attendance during two consecutive years (persistent FA), which equaled
1.6% of all enlisted patients. However, the influence of FAs on the GP’s workload
was substantial: Contacts of 1yFAs (by definition 10% of all enlisted patients)
accounted for 39% of all face-to-face consultations; the contacts of the 1.6% of
enlisted patients who became persistent FAs accounted for 8% of all consultations.
Persistent FAs suffered more from social problems, feelings of anxiety, addictive
behavior, and medically unexplained physical symptoms than 1yFAs and nonfrequently attending patients (non-FAs). They differed less from 1yFAs and non-FAs
where the prevalence of chronic somatic diseases is concerned.2
The third research question addressed which readily available information
noted in the patients’ Electronic Medical Record (EMD) predicts persistence of
frequent attendance during 3 consecutive years (pFA). We showed that out of
3045 1yFAs, 470 (15.4%) became pFA. We selected indicators that were associated
with becoming a pFA and constructed a prediction rule to predict which types of
patients become pFA. With this prediction rule it was possible to change the prior
probability of 15.4% to 3.3% (lowest value) or 43.3% (highest value), although the
10th and 90th centiles were 7.4 and 26.3%, respectively. The area under the receiver
operating characteristics curve was 0.67 (c-statistic; 95% confidence limits 0.64 and
0.69). Using general cut-offs, our rule only moderately predicted which short-term
FA continued to frequently attend in consecutive years.3
The fourth research question concerned a validation of this prediction rule in
another time frame in the same GP database and in another GP database in a
different part of the Netherlands.
Our validation study in a different part of the Netherlands (Eindhoven; the SMILE
database of general practice4) and in the same database but over a different
timeframe (2009-2011), confirmed the results of the original study. The existing
model (c-statistic 0.67) discriminated moderately with predicted values between 7.5
and 50%and c-statistics of 0.62 and 0.63, for validation in the original database and
SMILE database, respectively. Data taken from the GP’s electronic medical records
were only moderately indicative for which short-term FAs continued to frequently
attend in consecutive years.5
The fifth and sixth research questions addressed the costs of health care of FAs in
primary and specialist care. Can these costs be explained by the morbidities of
these FAs and/or by GP characteristics? Unadjusted mean 3-year expenditures
were 5044 and 15 824 Euros for non-FAs and pFAs, respectively. We showed that
after adjustment for all included confounders, costs both in primary and specialist
care remained substantially higher and increased with longer duration of frequent
GENERAL DISCUSSION
153
attendance. As compared to non-FAs, adjusted mean 3-year expenditures were 1723
and 5293 Euros higher for 1yFA and pFAs, respectively.
Thus, these extra costs could only partly be explained by the increased morbidity
of (p)FAs as registered by the GP. Our results suggested only little influence of
GP characteristics on costs of (persistent) frequent attenders. These increased
costs might be explained by inadequate patient-GP communication and (as yet)
undiagnosed psychosocial morbidity.6
Part 2. Review of the literature
The seventh research question was to identify effective interventions to improve
quality of life and lower attendance rate of FAs. This question was answered by a
review of the literature to determine possible effective interventions to improve
quality of life and lower attendance rate of FAs. Although we intended to perform
a meta-analysis we were not able to pool the results because of the heterogeneity
of the included studies. No study showed convincing evidence that an intervention
improved quality of life or morbidity of frequent attending primary care patients,
although a small effect might be possible in a subgroup of depressed frequent
attenders. No evidence was found that it is possible to influence healthcare
utilization of FAs.7 A intervention study, published after this review, which had a
broad scope (a group of GPs assessing the reasons as to why a patient is frequently
attending with subsequent targeted therapeutic measures) resulted in a significant
and relevant reduction in frequent-attender consultations.8
Part 3. A prospective study of frequent attenders
The eighth research question addressed which (in particular psychosocial) factors
are associated with persistence of frequent attendance in a prospective cohort
of incident1yFAs. Is there a supra-additive effect of combinations of somatic,
psychological and social factors? Epidemiological studies of FAs showed that
psychological problems (depression, anxiety, somatoform problems) are all more
prevalent in FAs compared to non-FAs.2;9;10 However, in prospective cohort studies,
using a proportional definition of FA (the upper 10%), only psychological distress,
low physical quality of life and a low educational level predicted persistence of
frequent attendance over the next two consecutive years.11;12 In our prospective
cohort of incident (new) frequent attenders, we confirmed the association of
persistence of frequent attendance with psychological distress. We showed that
psychological determinants (panic, other anxiety, negative life events, illness
behavior, and low mastery, but not depression) are associated with persistence
of frequent attendance. We found no evidence of synergistic effects of somatic,
psychological and social problems and no strong evidence of effects of GP
characteristics on persistence of frequent attendance.
The ninth research question evaluated whether systematic detection (as measured
154
WHY DO THEY KEEP COMING BACK?
by the Patient Health Questionnaire) and treatment of depression and anxiety after
one or two years of frequent attendance might be cost-effective compared to usual
GP care.
Based on a cost-effectiveness analysis with data of the prospective cohort of chapter
eight using a Markov simulation we concluded that systematic detection and
treatment of depressed and/or anxious one-year- and two-year-FAs are unlikely to
be cost-effective compared with usual GP care as provided in the Netherlands.
3. In summary
Patients with an age and sex-adjusted attendance rate ranking in the top 10 centile
within a time frame of one year have more and multiple, somatic, psychological and
social problems compared to their non-frequently attending peers. Somatic and
psychosocial morbidity increases with longer duration of frequent attendance. Most
frequent attendance is temporary and only about 2 % of the practice populations
visits frequently during 3 or more consecutive years.
Information from GPs’ electronic files is only a moderate indicator to identify which
short-term FAs continue to frequently attend in consecutive years.
Frequent attenders, and in particular persistent frequent attenders, make more
use of primary care services than non-FAs. Frequent attenders, and in particular
persistent frequent attenders, also have considerably above-average costs in
primary and specialist healthcare in comparison with non-FAs. Morbidity of
the patient and characteristics of the GP do not fully explain these extra costs.
Panic complaints, general anxiety, life events, illness behavior and low mastery
are associated with persistence of frequent attendance. These morbidities and
characteristics are not (always) registered by the GP and may, partly, explain these
extra costs. Also personality characteristics and patient-physician communication
may play a role. An extrapolation of the results from our cohort study using a
Markov simulation among 1yFAs showed that systematic detection and treatment of
depression and/or anxiety is unlikely to be cost-effective in comparison with usual
GP care.
4. Strengths of this thesis
In this section we discuss the overall strengths of the work brought together in this
thesis. For detailed information about a specific part of our research, please refer to
the specific chapter.
Despite many studies in other countries with a strong GP system, to our knowledge
this is the first attempt at studying characteristics of FAs in the Netherlands.
GENERAL DISCUSSION
155
Most research presented in this thesis was embedded in the longitudinal GP
database of the department of General Practice, AMC (Hag-net-AMC). In this
database, GPs register medical problems over a long period of time. This database
of GP-patients, combined with a prospective cohort, identified through this
database, and with a health insurers’ database (with detailed information about
healthcare expenditures), made it possible to answer research questions 2 to 6
(part I) and 8 and 9 (part III). As all GPs participating in the Hag-net-AMC receive
regular feedback on their registration activities and, nowadays, are helped by
automated computer algorithms, these registration data are of reasonable quality,
especially for somatic and psychological problems.13-15 It is less clear to what extent
GPs register social problems adequately. Since GPs register problems during
consultations, we expect the quality of this registration to be higher for FAs (who
have many consultations). However, differences in prevalence figures of diseases
between registration networks are considerable and limit generalisation.15 These
differences may be caused by differences between regions, or by registration and
coding differences between GPs or by artefacts.15;16
Being a long-time member of the steering committee of HAG-net-AMC and
personally knowing many of the participating GPs, helped to secure participation
and to optimise data quality. When convincing practices to participate in the
(continuation of) our study or to complete missing data, it was beneficial to have an
experienced, local GP to lead the study.
5. Limitations of this thesis
In this section we discuss the general limitations of the work laid down in this
thesis. For detailed descriptions, please refer to the specific chapter.
First, we used a proportional definition of FA which has certain disadvantages:
some patients may drop just below the cut-off (89th centile e.g.) the next year.
However, definitions based on some absolute number of visits share this limitation
(chapter 2). Second, we assumed that the so-called Problem List (a list of all
patients’ problems as registered and coded by the GP in the electronic medical
record) would give a comprehensive picture of the main morbidity of a patient.
However, some registered problems can be overreported if resolved problems are
not removed from this list or underreported if a prevalent problem is not registered
on the Problem List by the GP. This could lead to over- and underestimation of the
prevalence of these disorders and to information bias in the estimations of the effect
on persistence of frequent attendance.17 Also GP differences in registration- and
coding-discipline may be confounding factors.13;14 It is also unclear whether and to
what extent FAs visit primary care for minor, transient, problems not captured by
the Problem List.
156
WHY DO THEY KEEP COMING BACK?
Third, the participating GPs appeared to have relatively similar characteristics:
Being embedded in one academic region, eighty-two percent of the GPs were
involved in educating medical students, vocational training of future GPs and/or
research activities. This may lead to non-detection or underestimation of the effects
of GP characteristics.
Fourth, although we attempted to collect complete sets of patient characteristics
and clinical data, other undocumented determinants of (p)FA may have been
present. This is particularly true for the retrospective database studies, (part I) in
which we had no influence on what was documented.
Fifth, this study is situated in an urban part of the specific Dutch healthcare system
with more than average Surinamese and Ghanese patients. This may limit the
extent to which our results can be generalised to other regions and countries.
Sixth, in the prospective cohort study (part III), about two thirds of the eligible
1yFAs refused to participate. However, because we focused on aetiology and ample
analytical contrast within our sample, representativeness was not an issue like, for
instance, in a survey predicting some election and we do not think this influenced
our results negatively.17 Nonetheless, it was surprising how sensitive these patients
appear to being called a FA. From our personal contacts with participating FAs
we got the impression that they did not recognise themselves in the label ‘FA’. The
term may be seen as pejorative and blaming to the patient.18-20 Therefore, in a British
study a user panel preferred the term “regular attender”.21
Finally, we analysed a cohort of new (incident) FAs, and our results are limited
to frequent attendance over a period of 3 years. We cannot comment on frequent
attending of longer durations.
6. Relevant literature
Frequent attendance has interested GPs, mostly in countries which use (largely)
a capitation system for remuneration and where GPs use a list system. Over the
last thirty years, a continuous flow of mostly descriptive articles about FAs has
been published from the United Kingdom, Scandinavian countries, Spain and
from Health Maintenance Organisations in the United States. Surprisingly,
despite having largely a capitation payment system the Netherlands has been
an exception. The only Dutch study we know of is a thesis about the association
between personality and medical consumption (1980).22 That study indicated
that “personality” (defined as neuroticism, somatisation) only increased medical
consumption in the top 5% of attenders.
As expected, results in the literature differ depending on the definition of frequent
attendance used. When no correction for age and sex is used the resulting
GENERAL DISCUSSION
157
overrepresentation of elderly and female patients results in a high prevalence of
somatic (multi)morbidity. Using the proportional definition on the other hand,
results in a better representation of all ages and both sexes resulting in higher
prevalence of psychological and social problems than without correction for age
and sex.
In several studies, FAs are used to select a group of patients at high risk for
distress23, mental health problems24, major depressive disorder25-27 or somatoform
disorders/ medically unexplained symptoms28;29, but not for anxiety. Generally,
screening- and treatment programs using frequent attendance as a selection
criterion to diagnose a target disease had disappointing results in improvement
of this target disease, 7;25;30 partly because uptake and acceptance of screening and
treatment in screened patients are generally low.31-33 In our opinion, using FAs to
select a certain disease or problem disregards the strong multi-causal character
of frequent attendance. Detection and treatment of just one underlying aspect is
not likely to resolve the complex, multiple problems found in FAs. In this context,
it is noteworthy that there is a wide range of studies about comorbid depression in
somatic diseases, but that such knowledge is much less for anxiety as a comorbidity.
Reviewing the literature we found no evidence that specific interventions reduce
healthcare utilization or improve quality of life of FAs in comparison with usual GP
care.7 However, one more recent Spanish intervention study of good quality in 1yFAs
showed that a GP intervention reduced attendance in primary care in comparison
with usual care. Bellón et al. applied a “7 Hypothesis + Team intervention” after 3
GPs received a 15h training in executing the intervention. The GPs held meetings
to share analyses and reflections on their FAs and to make tailored plans for each
FA. GPs also received emotional support in these meetings and were helped to
generate strategies to deal with FAs. Numbers of consultations decreased by 5.08/
year (p<.001).8
7. Clinical and public health implications
This thesis distinguishes between short-term and persistent frequent attendance.
Our results imply that in short-term FAs, persistence of frequent attendance is
associated with anxiety, illness behavior, negative life events and low mastery.
Thus, a proportion of pFA may be preventable by developing interventions to
diminish or eliminate these causes.34-39 Adequate detection and treatment of
these conditions in FAs may result in a better quality of life of these patients,
less morbidity and a decrease in attendance and costs. Although treatment of
anxiety in primary care patients has been shown to be effective, the effect of this
treatment in preventing persistence of FAs is unclear and needs to be demonstrated
in research.7;34;40 In a first attempt to explore this issue, using a Markov model
158
WHY DO THEY KEEP COMING BACK?
extrapolating the results of the prospective cohort study, we showed that
systematic diagnostic assessment and treatment of depression and anxiety in FAs
will probably result in minimal cost savings and health effects in comparison with
FAs receiving usual care in primary care (chapter 9). However, knowing the high
costs of (persistent) FAs it might be beneficial for these patients and for the budget
problems in healthcare to test other interventions in (p)FAs. 7 GP interventions to
better the (medical) situation of FAs should target these patients broadly, at least
including interventions which address present panic and anxiety complaints and
low mastery. In addition, knowing the results of Bellon, interventions to diminish
consultations frequency of FAs may also need to be targeted at the GP .8
The Frequent attender: a typical GP patient
Currently, most research in general practice is focussed on individual, well defined,
mono-causal issues and diseases. From a methodological perspective this is
understandable. Diabetes, asthma or depression are easier research topics than
multi-morbidity, headaches, deprivation and ……frequent attendance.
Similarly, in clinical general practice, GPs often prefer to focus on clear diseases,
despite the sometimes low prevalence and/or lack of therapeutic options (e.g. in
the case of COPD). The traditional diagnostic, treating, and consoling role of the
life-long physician is more and more superseded by large-scale preventive and
intervention programs. Large amounts of funding and effort are spent on programs
reaching a relatively small number of patients, sometimes without much scientific
evidence.
We think these trends disregard the complicated reality of everyday general
practice. The 10% most frequently attending patients consume 40% of the GP’s
consultation time. These FAs are an important and, as shown in our study,
expensive group of patients in general practice. Often, these FAs have complicated
problems and suffer from a mix of interacting social, psychological and medical
problems, which often cannot be classified in somatic or psychiatric (DSM-IV)
diagnoses. Only a GP with a broad bio-psychosocial knowledge and approach
is able to unravel this mix of problems and propose suitable treatment and
guidance. Research has shown that even then, the proposed treatment has to
suit the perception, expectations and wishes of the patient to be effective.32;41 In
our opinion, such an integral approach is a better match for FAs than the preprogrammed approach of disease programs. Since in countries with a strong
primary care orientation, the system’s focus is on continuity of care, knowledge
about the (family) background of the patient and bio-psychosocial care, the
GP can best be the backbone of such an integral approach of FAs, if necessary
supported by a psychologist. In this regard, the new approach in mental health
care, where a formal DSM- diagnosis is needed before treatment by a psychologist
GENERAL DISCUSSION
159
or psychotherapist can start, can be seen as a, possibly counterproductive and costly
downfall.36
The results of our prospective cohort study also urge for more emphasis on anxiety
problems in everyday general practice. The role of lack of mastery in persistence of
frequent attendance calls for experiments to try to strengthen coping mechanisms of FAs.
Possibly social interventions in FAs (targeted at assertiveness, housing and debts problems)
may have better results than medical interventions.
Stepped care approach
We support the approach of a multifaceted diagnostic process and treatment for frequent
attending patients, as advocated by Bellon.8 Unlike his approach, we think such a program
may be preferably directed at frequent attenders of longer duration (e.g. 2yFAs). Such a
program must be tested first in a proper randomized clinical trial.
Until such results are available, we propose that General Practitioners identify their
FAs, give them some sort of ‘label ‘in the electronic medical record (“ruiter”), and try
to implement a broad diagnostic and therapeutic approach in their usual care of these
patients. A diagnostic interview, possibly supported by a psychiatric questionnaire
(PHQ, 4-DKL, HADS), can help the GP to unravel the somatic, psychological and social
background of the patient, and to formulate a targeted therapeutic approach.
8. Implications for research
We think further research should focus on the background of repeated or persistent
frequent attendance. Also the role of the Problem List as proxy for FA’s morbidity needs
more clarification. A cohort with more incident FAs, use of standardized psychiatric
interviews and measures of quality of life may provide more insight in the difference
between PHQ diagnoses and diagnoses after a Structured Clinical Interview for DSM
Disorders (SCID diagnosis) and the role of Quality of life measures. Subsequently,
randomised trials may determine the extent to which interventions aimed at modifying
anxiety disorders, illness behavior and mastery in this specific group of patients are
acceptable to patients and improve quality of life, and reduce attendance and costs of
(persistent) FAs.
Using a more diverse group of GPs (setting of the practice, age distribution, (non) training
practices, (non) academic practices) could shed more light on the influence of the GP on
(persistence of) frequent attendance.
Let’s face the frequent attender not as heart sink but as a challenge for GP care!
Frequent attenders deserve better care, not more care!
160
WHY DO THEY KEEP COMING BACK?
References
(1) Smits FT, Mohrs J, Beem E, Bindels
PJ, van Weert HC. Defining frequent
attendance in general practice. BMC
Fam Pract 2008; 9(1):21.
(2) Smits FT, Brouwer HJ, ter Riet G., van
Weert HC. Epidemiology of frequent
attenders: a 3-year historic cohort study
comparing attendance, morbidity and
prescriptions of one-year and persistent
frequent attenders. BMC Public Health
2009; 9(1):36.
(3) Smits FTM, Brouwer H.J., ter Riet G, van
Weert HC. Predictability of persistent
frequent attendance. A historic 3-year
cohort study. Br J Gen Pract 2009;
2-2009(59):114-119.
(4) van den Akker M, Spigt MG, De Raeve
L., van Steenkiste B., Metsemakers JF,
van Voorst EJ et al. The SMILE study:
a study of medical information and
lifestyles in Eindhoven, the rationale and
contents of a large prospective dynamic
cohort study. BMC Public Health 2008;
2008:19.
(5) Smits FT, Brouwer HJ, Zwinderman AH,
van den Akker M, van SB, Mohrs J et
al. Predictability of persistent frequent
attendance in primary care: a temporal
and geographical validation study. PLoS
One 2013(9):e73125.
(6) Smits FT, Brouwer HJ, Zwinderman AH,
Mohrs J, Smeets HM, Bosmans JE et al.
Morbidity and doctor characteristics only
partly explain the substantial healthcare
expenditures of frequent attenders: a
record linkage study between patient
data and reimbursements data. BMC
Fam Pract 2013; 2013(1):138.
(7) Smits FT, Wittkampf KA, Schene AH,
Bindels PJ, van Weert HC. Interventions
on frequent attenders in primary care. A
systematic literature review. Scand J Prim
Health Care 2008; 26(2):111-116.
(8) Bellon JA, Rodriguez-Bayon A, de Dios
LJ, Torres-Gonzalez F. Successful GP
intervention with frequent attenders in
primary care: randomised controlled trial.
Br J Gen Pract 2008; 58(550):324-330.
(9) Ferrari S, Galeazzi GM, Mackinnon A,
Rigatelli M. Frequent attenders in primary
care: impact of medical, psychiatric and
psychosomatic diagnoses. Psychother
Psychosom 2008; 77(5):306-314.
(10) Gili M, Luciano JV, Serrano MJ,
Jimenez R, Bauza N, Roca M. Mental
disorders among frequent attenders in
primary care: a comparison with routine
attenders. J Nerv Ment Dis 2011(10):744749.
(11) Rifel J, Svab I, Selic P, Rotar PD,
Nazareth I, Car J. Association of
Common Mental Disorders and Quality
of Life with the Frequency of Attendance
in Slovenian Family Medicine Practices:
Longitudinal Study. PLoS One 2013;
8(1):e54241.
(12) Vedsted P, Fink P, Olesen F, MunkJorgensen P. Psychological distress
as a predictor of frequent attendance
in family practice: A cohort study.
Psychosomatics: Journal of Consultation
Liaison Psychiatry /9; 42(5):416-422.
(13) Brouwer HJ, Bindels PJ, van Weert
HC. Data quality improvement in general
practice. Fam Pract 2006; 23(5):529536.
(14) van den Dungen C, Hoeymans
N, Boshuizen HC, van den Akker M,
Biermans MC, van BK et al. The influence
of population characteristics on variation
in general practice based morbidity
estimations. BMC Public Health 2011;
11:887.
(15) van den Dungen CHN, Boshuizen HC,
van den Akker M, Biermans MC, van
Boven K., Brouwer HJ et al. What factors
explain the differences in morbidity
estimations among general practice
registration networks in the Netherlands?
A first analysis. Eur J Gen Pract2008;14
Suppl 1:53-62
(16) Wennberg JE. Dealing with medical
practice variations: a proposal for action.
Health Aff (Millwood ) 1984; 3(2):6-32.
(17) Rothman K, Greenland S, Lash T.
Modern epidemiology. Philadelphia, PA
(USA): Lippincott Williams & Wilkins;
2008.
GENERAL DISCUSSION
161
(18) Neal RD, Heywood PL, Morley S. ‘I
always seem to be there’--a qualitative
study of frequent attenders. Br J Gen
Pract 2000(458):716-723.
(19) Hodgson P, Smith P, Brown T, Dowrick
C. Stories from frequent attenders: a
qualitative study in primary care. Ann
Fam Med 2005; 3(4):318-323.
(20) Dwamena FC, Lyles JS, Frankel RM,
Smith RC. In their own words: qualitative
study of high-utilising primary care
patients with medically unexplained
symptoms. BMC Fam Pract 2009;
10(1):67.
(21) Morriss R, Kai J, Atha C, Avery A,
Bayes S. Persistent frequent attenders
in primary care: costs, reasons for
attendance, organisation of care and
potential for cognitive behavioural
therapeutic intervention. BMC Fam Pract
2012; 13:39.
(22) van der Ploeg HM. Persoonlijkheid
en medische consumptie: Een
onderzoek naar de relatie van
persoonlijkheidsfactoren en de
frequentie van huisartsbezoek. Swets
&Zeitlinger B.V.; 1980.
(23) Katon W, Von KM, Lin E, Bush T, Russo
J, Lipscomb P et al. A randomized trial of
psychiatric consultation with distressed
high utilizers. Gen Hosp Psychiatry 1992;
14(2):86-98.
(24) Schreuders B, van Marwijk H, Smit
J, Rijmen F, Stalman W, van Oppen P.
Primary care patients with mental health
problems: outcome of a randomised
clinical trial. Br J Gen Pract 2007;
57(544):886-891.
(25) Katzelnick DJ, Simon GE, Pearson
SD, Manning WG, Helstad CP, Henk HJ
et al. Randomized trial of a depression
management program in high utilizers
of medical care. Arch Fam Med 2000;
9(4):345-351.
(26) Baas KD, Wittkampf KA, van Weert
HC, Lucassen P, Huyser J, van den
Hoogen H et al. Screening for depression
in high-risk groups: prospective cohort
study in general practice. The British
Journal of Psychiatry 2009; 194(5):399403.
162
(27) Berghofer A, Roll S, Bauer M, Willich
SN, Pfennig A. Screening for Depression
and High Utilization of Health Care
Resources Among Patients in Primary
Care. Community Ment Health J
2014:Jan.
(28) Barsky AJ, Ahern DK, Bauer MR,
Nolido N, Orav EJ. A Randomized Trial of
Treatments for High-Utilizing Somatizing
Patients. J Gen Intern Med 2013:Mar.
(29) Smith RC, Gardiner JC, Armatti S,
Johnson M, Lyles JS, Given CW et al.
Screening for high utilizing somatizing
patients using a prediction rule derived
from the management information
system of an HMO: a preliminary study.
Med Care 2001; 39(9):968-978.
(30) Schreuders B, van Oppen P, van
Marwijk HW, Smit JH, Stalman WA.
Frequent attenders in general practice:
problem solving treatment provided by
nurses. BMC
(31) Vink JM, Willemsen G, Stubbe JH,
Middeldorp CM, Ligthart RS, Baas KD et
al. Screening for depression in high-risk
groups: prospective cohort study in
general practice. Eur J Epidemiol 2004;
2004;19(7):623-630.
(32) Wittkampf KA, van Zwieten M, Smits
FT, Schene AH, Huyser J, van Weert
HC. Patients’ view on screening for
depression in general practice. Fam
Pract 2008; 25(6):438-444.
(33) Thombs BD, Ziegelstein RC, Roseman
M, Kloda LA, Ioannidis JP. There are no
randomized controlled trials that support
the United States Preventive Services
Task Force guideline on screening for
depression in primary care: a systematic
review. BMC Med 2014:13-12.
(34) Kendall T, Cape J, Chan M, Taylor C.
Management of generalised anxiety
disorder in adults: summary of NICE
guidance. BMJ 2011; 2011(4):318-327.
(35) Pilling S, Mayo-Wilson E. Recognition,
assessment and treatment of social
anxiety disorder: summary of NICE
guidance. BMJ 2013; 346.
(36) Feltz-Cornelis CM, Van Oppen P, Ader
H, Van Dyck R. Randomised controlled
trial of a collaborative care model with
psychiatric consultation for persistent
medically unexplained symptoms in
general practice. Psychother Psychosom
2006; 75:282-289.
WHY DO THEY KEEP COMING BACK?
(37) van der Feltz-Cornelis C, Van Os
TWDP, Van Marwijk HWJ, Leentjens
AFG. Effect of psychiatric consultation
models in primary care. A systematic
review and meta-analysis of randomized
clinical trials. Journal of Psychosomatic
Research 68[6], 521-533. 2010.
(38) Reger MA, Gahm GA. A metaanalysis of the effects of Internet- and
computer-based cognitive-behavioral
treatments for anxiety. Journal of Clinical
Psychology 2009; 65(1):53-75.
(39) Donker T, Griffiths KM, Cuijpers P,
Christensen H. Psychoeducation for
depression, anxiety and psychological
distress: a meta-analysis. BMC Med
2009; 7:79.:79.
(40) Goldberg D. The “NICE Guideline”
on the treatment of depression.
Epidemiologia e Psichiatria Sociale Vol 15
(1), Jan -Mar 2006;-15.
(41) Arroll B, Goodyear-Smith F, Kerse
N, Fishman T, Gunn J. Effect of the
addition of a “help” question to two
screening questions on specificity for
diagnosis of depression in general
practice: diagnostic validity study. BMJ
2005(7521):884.Fam Pract 2005; 6:42.
GENERAL DISCUSSION
163
chapter 11
appendices
Appendix 1. Selected problems and diseases with ICPC-code1
ICPC code
Problem
Diabetes
T90
Diabetes mellitus type 1 and 2
Chronic Cardiovascular disease
K74
Angina pectoris
K75
Acute myocardial infarction
K76
Other and chronic ischemic heart disease
K77
Heart failure
K78
Atrial fibrillation/flutter
K82
Pulmonary heart disease
K83
Heart valve disease, non-rheumatic2
K86
Hypertension, uncomplicated
K87
Hypertension with involvement of target organs
K89
Transient cerebral ischemia
K90
Cerebrovascular accident; stroke
K91
Atherosclerosis excluding heart and brain
K92
Other arterial obstructive/ peripheral vascular disease
Chronic respiratory problems
R70
Tuberculosis of respiratory organs
R91
Chronic bronchitis/ bronchiectasis
R95
Emphysema/Chronic Obstructive Pulmonary Disease
R96
Asthma
R97
Allergic rhinitis; hay fever
164
WHY DO THEY KEEP COMING BACK?
Psychological / Psychiatric problems
All P
All P-codes
Sub-category 1: Anxious feelings
P01
Feeling anxious/nervous/tense
P74
Anxiety disorder/anxiety state
P09
Concern sexual preference
A-Y27
Fear of other disease of various tracts
A-D26
Fear of cancer of various tracts
L26
Fear of death
N26
Fear of AIDS
R-Y26
Fear of heart attack
A25
Fear of hypertension
B25
Fear of venereal disease
K24
Fear of sexual dysfunction
K25
Fear of genital cancer
X23/Y25
Fear of venereal disease
X24/Y24
Fear of sexual dysfunction
X25
Fear of genital cancer
Sub-category 2: Depressed feelings
P03
Feeling depressed
P76
Depressive disorder
Sub-category 3: Addictive behaviour
P15
Chronic alcohol abuse
P16
Acute alcohol abuse
P17
Tobacco abuse
P18
Abuse of medicines
P19
Drug abuse
Continued on page 166
APPENDICES
165
Social problems
All Z
All socio-economic problems
Medically unexplained physical problems (MUPS)
L01
Neck symptoms /complaints (excluding headache)
L02
Back symptoms/complaints
L03
Low back complaints without radiation
L04
Chest symptoms/complaints
L18
Muscle pain/ fibromyalgia
N01
Headache
N02
Tension headache
A04
General weakness/tiredness/chronic fatigue
P06
Disturbance of sleep/insomnia
P20
Disturbance of memory, concentration
T03
Loss of appetite
T07
Weight gain
T08
Weight loss
P04
Feeling/behaving irritably
R02
Shortness of breath, dyspnea
K04
Palpitations/ aware of heartbeat
N17
Vertigo/Dizziness
R21
Symptoms / complaints of the throat
N06
Other sensitive disturbance /abnormal involuntary movements
D09
Nausea
D11
Diarrhea / Loose bowels
D08
Flatulence/gas pain/belching
D12
Constipation
D01
Generalized abdominal pain/cramps
D93
Irritable bowel syndrome
166
WHY DO THEY KEEP COMING BACK?
Cancer
A79
Cancer of unknown location
B72-B74
Cancer of hematological tract
D74-D77
Cancer of stomach, colon, pancreas
K72
Cancer of the vascular tract
L71
Cancer of the locomotor tract
N74
Cancer of the nervous system
S77
Cancer of the skin
T71,T73
Cancer of the thyroid, endocrine tract
U75-U77
Cancer of the kidney, bladder, urine tract
W72
Cancer related to pregnancy
X75-X77
Cancer of the female organs
Y77-Y78
Cancer of the male organs
All D
All digestive tract problems/diseases
All L
All locomotor tract problems/diseases
All S
All skin problems/diseases
1:
2:
International classification of primary care
Not otherwise specified
Appendix 2. Effect of loss to follow-up and clustering on the health centre level on the
prognostic index.
Amsterdam
I
Amsterdam II SMILE
Deviance of the normal Logistic Regression model
2476
3046
5320
Ln(OR)1 of the prognostic index (SE)
0.993
(0.084)
0.663
(0.071)
0.835
(0.062)
Ln(OR) of the prognostic index corrected
for Loss to follow-up (SE)
1.028
(0.080)
0.694
(0.067)
0.848
(0.062)
Deviance of the multilevel model
2467
3029
5198
Ln(OR) of the prognostic index multilevel
model (SE)
0.994
(0.085)
0.707
(0.073)
0.909
(0.064)
variance practice effect
0.072
0.102
0.222
Intraclass correlation coëfficiënt
0.0214
0.0301
0.0632
1
2
2
Indicates natural logarithm of the odds ratio
SE indicates Standard Error
APPENDICES
167
Appendix 3. Primary care physicians’ questionnaire
The interaction between patient and physician factors may determine the number of
visits of a patient. With this questionnaire we are trying to determine primary care physicians’ characteristics which may influence patients’ attendance.
Filling out this survey will take about 10 minutes of your time. Please answer all questions. After entering, your data will, of course, be anonymized.
Thank you very much for your effort!
1. In which year did you graduate from
medical school?
2. At what university did you graduate as
a doctor?
3. Please note the number of years you
work as a physician: …
4. I am currently working
•
part-time
•
full-time
5. If part-time, what percentage of a full
contract do you work?: …
6. Do you have special knowledge of/
interest in a specific part of general practice?
•
Yes
•
No
If so, in which specific field are you interested? (Several options are possible)
•
paediatric medicine
•
geriatric medicine
•
small surgical procedures
•
management of the practice
•
financial management
•
professional organizations
7. Do you have special knowledge of/
interest in (the treatment of) diabetes
mellitus?
•
no special interest
•
little interest
•
normal interest
•
more than normal interest
•
very much interest
8. Do you have special knowledge of/
interest in (the treatment of) asthma and/
or COPD?
•
no special interest
•
little interest
•
normal interest
•
more than normal interest
•
very much interest
168
9. Do you have special knowledge of/
interest in (the treatment of) cardiovascular diseases?
•
no special interest
•
little interest
•
normal interest
•
more than normal interest
•
very much interest
10. Are you a member of a guideline committee of the Dutch College of General
Practitioners (NHG)?
•
Yes
•
No
11. If “Yes”: Please give the title of the
guideline(s)
•
NHG-standard:
•
NHG-standard:
•
NHG-standard:
12. Are you involved in the organization of
continuous medical education/post academic training of primary care physicians?
•
Yes
•
No
13. Do you treat patients with anxiety
disorders?
Please indicate what percentage of patients with anxiety disorders you manage
yourself.
•
0%
•
25%
•
50%
•
75%
•
100%
14. Do you treat patients with depressive
symptoms or depression?
Please indicate what percentage of
patients with depressive symptoms you
manage yourself.
•
0%
•
25%
•
50%
•
75%
•
100%
WHY DO THEY KEEP COMING BACK?
15. Do you treat patients with medically
unexplained somatic complaints? (Think
for instance of unexplained pain)
Please indicate what percentage of patients with unexplained symptoms you
manage yourself.
•
0%
•
25%
•
50%
•
75%
•
100%
16. Are you a primary care physician vocational trainer?
•
Yes
•
No
17. Do you regularly give (vocational)
training to medical students ?
•
Yes
•
No
23. How do you organize your office
schedule? Check on the checkboxes (multiple options).
•
Only after appointment
•
An open schedule
•
Telephone consultation
•
E-mail consultation
•
Appointments via the Internet
24. My age is:
25. I am:
•
Man
•
Woman
Thank you very much for completing this
questionnaire!
18. Are you also working at a university
and/or the Dutch College of General
Practitioners (NHG)? Multiple options are
possible.
•
Yes, university
•
Yes, NHG
•
No
19. Do you cooperate with other primary
care physicians (PCPs)?
•
Group practice (only PCPs)
•
Health centre
•
PCPs with one electronic
medical file
•
I am a solo PCP
20. Do you work with a trained practice
nurse?
•
Yes
•
No
21. If so, how many days support these
practice nurses your practice? _ _ days
22. Do you work with another discipline?
Please check the appropriate checkbox
(multiple options).
•
Nurse
•
Social psychiatric nurse
•
General social worker
•
Primary care psychologist
•
Other: …..
APPENDICES
169
Appendix 4. Univariate associations between patient characteristics and 3-year costs in
primary and specialist care
Primary care
Age1
Specialists care
Mean
(range)
Difference
(SE)
P-value
Difference
(SE)
P-value
47 (18-98)
59 (2)
< 0.001
101 (6)
< 0.001
Male (reference)
0
Female
343 (74)
0
< 0.001
155 (231)
0.50
Ethnicity:
Dutch (reference)
0
0
Moroccan
-409 (186)
Turkish
-369 (244)
0.001
-709 (764)
0.17
Surinamese
-318 (96)
0.001
-190 (300)
0.17
< 0.001
1466 (50)
< 0.001
< 0.001
0.001
-1212 (590) 0.17
Problems on the problem list2
Number of problems
2.43 (0-18) 743 (15)
Diabetes
0.14 (0-1)
3146 (116)
< 0.001
4003
(369)
COPD/Asthma
0.16 (0-2)
1132 (96)
< 0.001
929 (302)
0.002
Cardiovascular
0.42 (0-5)
1684 (52)
< 0.001
4210 (165)
< 0.001
Social
0.04 (0-2)
244 (212)
0.25
660 (649)
0.32
Psychological
0.24 (0-3)
1183 (81)
< 0.001
4506 (254) < 0.001
Depression
0.06 (0-1)
1292 (179)
< 0.001
2602 (559) < 0.001
Anxiety
0.03 (0-1)
886 (231)
< 0.001
1423 (723)
0.049
Addiction
0.05 (0-2)
1235 (186)
< 0.001
5617 (582)
< 0.001
Other
psychological
0.10 (0-2)
1404 (128)
< 0.001
6711 (400)
< 0.001
Medically Unexplained Symptoms
0.17 (0-5)
947 (96)
< 0.001
1791 (300)
< 0.001
Frequent attender during:
Non-FAs (reference)
0
1 year
1005 (109)
<0.001
2467 (355) <0.001
2 years
2227
(246)
<0.001
3512 (461)
3 years
3029
(308)
<0.001
7751 (1024) <0.001
1:
2:
170
0
<0.001
Costs per additional year of age
Binary variables were modeled using a dummy; all other variables were
modelled linearly
WHY DO THEY KEEP COMING BACK?
Appendix 5. The multivariate effects of patient characteristics on mean costs (by healthcare level#)
Age1
Primary care
Specialists care
Mean
(range) 4
difference
(SE)
P-value
difference
(SE)
P-value
47(18-98)
8.1 (1.1)
< 0.001
-4.5 (3.0)
0.13
Male (reference)
0
Female
119 (33)
0
< 0.001
259 (86)
0.002
Ethnicity
Dutch (reference)
0
Moroccan
171 (131)
0
0.087
7 (343)
Turkish
-41 (11)
194 (290)
Surinamese
-36 (106)
38 (277)
0.54
Problems on the problem list ¶
Total Number
2.43 (0-18) 451 (17)
< 0.001
802 (44)
< 0.001
Diabetes mellitus
0.14 (0-1)
1330 (59)
< 0.001
-268 (155)
0.083
COPD2/Asthma
0.16 (0-2)
161 (46)
0.001
-660 (121)
< 0.001
Cardiovascular
0.42 (0-5)
263 (36)
< 0.001
659 (94)
< 0.001
Social
0.04 (0-2)
-512 (95)
< 0.001
-582 (249) 0.019
Psychological
0.24 (0-3)
365 (282)
0.196
1074 (740) 0.15
Depression
0.06 (0-1)
-401 (292)
0.17
-433 (767) 0.57
Anxiety
0.03 (0-1)
-472 (263) 0.072
-588 (689) 0.39
Addiction
0.05 (0-2)
-344 (295) 0.24
-329 (775)
0.67
Other psychological
0.10 (0-2)
191 (289)
0.51
428 (758)
0.57
Medically Unexplained
Symptoms
0.17 (0-5)
-279 (50)
< 0.001
-801 (131)
< 0.001
Cancer
0.04 (0-1)
635 (82)
< 0.001
4195 (217)
< 0.001
Locomotor
0.16 (0-1)
-81 (57)
0.15
290 (148)
0.05
Skin
0.09 (0-1)
-289 (61)
< 0.001
-1124(159)
< 0.001
Digestive
0.11 (0-1)
113 (60)
0.059
492 (156)
0.002
Intraclass correlation
(PCP level 3)
#:
¶:
1:
2:
3:
4:
0.0097
0.0041
Based on the same regression analysis as presented in Table 4
All variables were linear, unless indicated otherwise
Costs in Euros per unit increase (for instance per extra year of age)
Chronic obstructive pulmonary disease
Variance between primary care physicians (PCPs) as part of the total variance
(residual variance + PCP variance).
Frequent attenders during 1 year in 2009 .
APPENDICES
171
Appendix 6. instruments used to capture the potential psychosocial aetiological factors for
persistence of frequent attendance.
1. Do you worry about your health?
2. Are you worried that you may get a serious illness in the future?
3. Does the thought of a serious illness scare
you?
4. If you have pain, do you worry you might
have a serious illness?
5. If a pain lasts for a week or more do you
see a physician?
6. If a pain lasts a week or more, do you
believe you have a serious illness?
7. Do you avoid habits which may be harmful
to you, such as smoking?
8. Do you avoid foods which may not be
healthy?
9. Do you examine your body to see if there
is something wrong?
10. Do you think that you have a illness but
doctors have not diagnosed it?
11. When your doctor says you have no illness, do you refuse to believe it?
12. When your doctor tells you what was
found, do you believe you have it?
13. Are you afraid of news which makes you
think of death?
14. Does the thought of death scare you?
15. Are you afraid that you may die soon?
16. Are you afraid that you may have cancer?
17. Are you afraid that you may have heart
disease?
18. Are you afraid that you may have another
serious illness?
19. When you read or hear about an illness,
do you get similar symptoms?
172
WHY DO THEY KEEP COMING BACK?
Most of the
time
Often
Sometimes
Seldom
No
Illness attitude scale:
Don’t think too long before answering the next questions: Just ask yourself does it happen and if it happens how often?
20. When you notice a sensation in your
body, do you find it difficult to think of
something different?
21. When you feel something in your body,
do you worry about it?
23. Has your physician told you that you are currently suffering from a disease?
Yes
No
*24. How often do you see a doctor?
Almost never
Seldom
About 4 times a year
About once a month
About once a week
*25. How many different caregivers (doctors, homoeopaths etc) have you seen in the
past year?
None
1
2 or 3
4 or 5
6 and more
*26. How often have you been treated in the past year?
Not at all
Once
2 or 3 times
4 or 5 times
6 times or more
27. In the next three questions we ask you about your physical symptoms (for instance pain, tensions in your body, breathing problem, tiredness)
1. Do your bodily symptoms stop you from
working?
2. Do your bodily symptoms stop you from
concentrating?
3. Do your bodily symptoms stop you from
enjoying yourself?
*
Question which counts for the health anxiety score
Question which score for the illness behaviour score
Questions which score for the illness behaviour score, omitted from the IAS to avoid
circular reasoning
APPENDICES
173
Stronglt
disagree
disagree
Don’t agree/
don’t
disagree
Agree
Strongly
agree
Mastery questionnaire
How strongly do you agree or disagree with the following statements?
1. I have little control over the things that
happen to me.
2. There is really no way I can solve some of
the problems I have.
3. There is little I can do to change many of
the important things in my life.
4. I often feel helpless in dealing with the
problems of life.
5. Sometimes I feel that I’m being pushed
around in life.
6. What happens to me in the future mostly
depends on me.
7. I can do just about anything I really set my
mind to do.
Negative life events
If you have never or not in the last 12 months experienced a certain event, please fill
in the square below “Not applicable”. If you did experienced a certain event last year,
please fill in the square below the time at which the event took place. If an event took
place over several time periods, please fill in this event for all these time periods.
1. Divorce:
a. close family member
b. yourself
c. significant other/s
2. New relationship of yourself
3. Moving house (yourself)
174
WHY DO THEY KEEP COMING BACK?
Yes, 3 to 12
months ago
Past year’s events: If Yes, when?
(More than one answer possible)
Yes, during
the last 3
months
1. Close family members can be: parents, foster parents, brothers,
sisters and children.
2. Significant others can be: friends, other family members, a trusted
person, pastor, vicar or other people that are close to you
Not
applicable
Please note:
4. Long-term and/or severe physical illness:
a. close family member or partner
b. yourself
c. significant other/s
5. Death of:
a. a close family member or partner
f. significant other/s
6. Severe mental illness:
a. close family member or partner
b. yourself
c. significant other/s
7. Attempted suicide:
a. close family member or partner
b. yourself
c. significant other/s
8. Violence within your family or relationship
9. Alcohol or drug abuse within your family or relationship
10. Been a victim of a crime
11 Been a victim of a serious accident
12. Been a victim of sexual abuse
13. Been a victim of physical abuse
14. Had an unwanted pregnancy or have made someone
pregnant who did not want to be
15. Problems concerning your work:
a. conflicts/arguments
b. dismissal
16. Financial troubles of yourself
a. worries about managing your finances
b. debts
APPENDICES
175
Patient Health Questionnaire
Nearly every
day
More than
half the days
Several days
Not at all
Depression: Over the last 2 weeks, how often have you been bothered by any of the
following problems?
Little interest or pleasure in doing things
Feeling down, depressed, or hopeless
Trouble falling asleep, staying asleep, or sleeping too
much
Feeling tired or having little energy
Poor appetite or overeating
Feeling bad about yourself, feeling that you are a
failure, or feeling that you have let yourself or your
family down
Trouble concentrating on things such as reading the
newspaper or watching television
Moving or speaking so slowly that other people may
have noticed. Or being so fidgety or restless that
you have been moving around a lot more than usual
Thinking that you would be better off dead or that
you want to hurt yourself in some way
Axiety:
In the last 4 weeks, have you had an anxiety attack (a sudden feeling of fear or panic)?
•
•
No (Go to question 14.3)
Yes
a. Has this ever happened before?
b. Do some of these attacks come suddenly out of the blue that is, in
situations where you don’t expect to be nervous or uncomfortable?
c. Do these attacks bother you a lot or are you worried about having
another attack?
176
WHY DO THEY KEEP COMING BACK?
No
Yes
If you answered “Yes”:
No
Yes
While answering the following questions, think about your last bad anxiety attack!
a. Were you short of breath?
b. Did your heart race, pound, or skip?
c. Did you have chest pain or feel pressure?
d. Did you sweat?
e. Did you feel as if you were choking?
f. Did you have hot flushes or chills?
g. Did you have nausea or an upset stomach, or the feeling that you
were going to have diarrhoea?
h. Did you feel dizzy, unsteady, or faint?
i. Did you have tingling or numbness in parts of your body?
j. Did you tremble or shake?
k. Were you afraid you were dying?
Over the last 4 weeks, how often have you been bothered by any of the
following problems?
feeling nervous, anxious, on edge, or worrying a lot about different things.
•
•
•
Not at all (Go to next question)
Several days
More than half the days
Nearly every
day
More than
half the days
Several days
Over the last 4 weeks,
how often have you been bothered by:
Not at all
If you answered Several days or More than half the days:
Feeling restless so that it is hard to sit still.
Getting tired very easily.
Muscle tension, aches, or soreness.
Trouble falling asleep or staying asleep.
Trouble concentrating on things, such as reading a
book or watching TV.
Becoming easily annoyed or irritable.
APPENDICES
177
summary
Why does someone, sometimes during several years, frequently visit
the general practitioner? Often, of course, because of medical problems,
but sometimes the background of these frequent consultations remains
unclear and the general practitioner wonders how to change this behavior.
Therefore, this thesis studies (the background of) frequent attenders of
the general practitioner and examines which factors lead to (long-term)
frequent attendance, the relationship with the (medical) problems of the
patient, the possible therapeutically approaches of frequent attenders and
the impact on the workload of the general practitioner and the cost of health
care.
This thesis consists of three parts:
1.
2.
3.
Retrospective database research on (persistent) frequent attenders;
Review of the literature about interventions on frequent attenders in
primary care;
Prospective research of a cohort of incident frequent attenders.
In chapter 1 we describe the background of this research. Anyone may have
periods in their lives during which frequent help from a general practitioner
(GP) is sought or needed because of a medical problem. However, when such
periods exceed two or more consecutive years, not only chronic physical,
but also psychosocial problems are often present. Most research on frequent
attendance is cross-sectional and focusses on patients who were frequent
attender during 1 year. Longitudinal studies show that only 20–30% of
frequent attenders (FAs) continue to attend frequently in the consecutive
year. FAs not only frequently attend their GP, but make also more use of
178
WHY DO THEY KEEP COMING BACK?
other primary care and of secondary care. It is unclear whether this high use of
health care may be explained by the excess morbidity these patients have. Thus,
persistent frequent attendance could be seen as an easily detectable marker for
underlying, often undetected, (psychosocial and psychiatric) problems.
However, there are insufficient data about (the aetiology of) persistent frequent
attendance, the costs of healthcare of (persistent) FAs, about effective interventions
of FAs and about the influence of the GP and GP-patient communication on
(persistence of) frequent attendance.
It is unknown whether it would be feasible to develop a prediction rule for selecting
persistent FAs using readily available information from GPs’ electronic medical
records. Finally, we wanted to evaluate, using the data of a prospective cohort,
whether detection and treatment of depression and anxiety of Fas could be costeffective.
Because frequent attendance is mostly temporary and relates to clear and
intercurrent medical problems and most somatic problems in this patient group
are already dealt with in (chronic) care programs, we concentrated this thesis on
persistent or repeated frequent attendance and on the specific role of psychological
and social factors and GP characteristics in the aetiology of (persistence of)
frequent attendance.
Part 1. Retrospective database research
Chapter 2. What is the best method to select FAs in a normal general practice? After
considering various options, we chose a proportional definition of FAs by age and
gender. Because consultation frequency depends on the age and the gender of the
patient and differs between physicians, countries and regions only such a definition
makes it possible to compare FAs. Using a large database of NIVEL (Netherlands
institute for health services research; the first national study), we found that
dividing the practice population in at least 3 age and sex groups is sufficient to
reliably determine the top 10% FAs.
In chapter 3 we describe the morbidity of short-term and persisting FAs and the
workload of GP’s, caused by FAs using the database of the department of General
Practice of the Academic Medical Center (HAG-net-AMC) This database contains
data of 28.860 adult patients of 5 health centres. We found that of all Fas during one
year (1yFAs), 15.4 % continued to frequently attend during 3 consecutive years (1.6%
of all enlisted patients). GP’s spend 4 times more consultations on FAs and 5 times
more on persistent FAs (pFAs, FAs during 3 years). Compared with non-FAs, FAs,
and in particular pFAs, consume more health care and are diagnosed not only with
more somatic diseases but especially more social problems, psychiatric problems
and medically unexplained physical symptoms. Prevalence rates of chronic somatic
illnesses vary less than psychosocial problems between non-FAs and (persistent)
FAs.
SUMMARY
179
Chapter 4. Besides already known morbidity (persistent) FAs may have hidden
disorders. Also Fas, and in particular persistent Fas, increase GPs’ workload
considerably. Therefore, it seems reasonable and efficient to target diagnostic
assessment and intervention at patients with a high probability of becoming a
persistent FA. But is it possible to predict which FAs are likely to continue to
frequently visit the GP? Therefore, in a historic 3-year cohort study, we aimed
to develop a prediction rule for selecting persistent FAs using readily available
information from GPs’ electronic medical records. We used data on 28,860 adult
patients from 2003 to 2005.
Out of 3045 1-year FAs 470 (15.4%) became pFA. With the present indicators our
rule performs modestly in selecting those at risk of becoming pFAs (area under
the receiver operating characteristics curve was 0.67; 95% confidence limits 0.64
and 0.69). More information or complementary diagnostic tests seem needed to
construct a rule with sufficient performance for efficient risk stratification in
clinical trials.
In chapter 5 we validated the prediction rule developed in chapter 4 in another
region and period. We applied the existing model to a later time frame (2009-2011)
in the original derivation network (temporal validation) and to patients of another
network (SMILE Eindhoven; 2007-2009, temporal and geographical validation).
Model improvement was studied by adding three new predictors. Finally, we
developed a prediction model on the three data sets combined (N=12,539).
We concluded that external validation confirmed that persistent frequent attenders
can be identified moderately well using data solely from patients’ electronic medical
records.
FAs to primary care are likely to cost more in primary care than their nonfrequently attending counterparts. But how much is spent on specialist care of FAs?
In chapter 6 we describe the healthcare expenditures of (persistent) FAs and test
the hypothesis that additional costs can be explained by FAs’ combined morbidity
and primary care physicians’ characteristics. We linked the pseudonymised
clinical data of 16,531 patients from 39 general practices to healthcare insurer’s
reimbursements data. Main outcome measures were all reimbursed primary and
specialist healthcare costs between 2007 and 2009. Primary care physicians’
characteristics were collected through administrative data and a questionnaire.
We concluded that FAs of primary care give rise to substantial costs not only in
primary, but also in specialist care that cannot be explained by their (known)
multimorbidity. Primary care physicians’ working styles appear not to explain
these excess costs. The mechanisms behind this excess expenditure remain to be
elucidated.
180
WHY DO THEY KEEP COMING BACK?
Part II. Review of the literature about interventions on frequent attenders in
primary care
In Chapter 7 we analyzed which interventions are effective in influencing
morbidity, quality of life and healthcare utilization of FAs in primary care. We
performed a systematic literature search for articles describing interventions on
FAs in primary care. Outcomes were morbidity, quality of life and use of health
care.
We identified 5 RCT’s of good quality. Three RCTs used frequent attendance to
select patients at risk for distress, major depression and anxiety disorders and
applied psychological and psychiatric interventions. Two of them found more
depression-free days and a better quality of life after treating depression in FAs.
No other RCT found any positive effect on morbidity or quality of life. Two RCTs
studied an intervention which focused on reducing frequent attendance. No
intervention significantly lowered attendance. Due to the difference in study
settings and the variation in methods of selecting patients, meta-analysis of the
results was not possible.
Concluding we did find indications that frequent attendance might be a sign of as
yet undiagnosed depression and that treatment of this depression might improve
the symptoms and the quality of life of depressed FAs. We found no evidence that it
is possible to influence healthcare utilization.
Part III. Prospective cohort research
Chapter 8. Persistent FAs frequently suffer from multimorbidity and often have
many (undiscovered) psychosocial problems. Assuming that somatic problems are
treated appropriately, profit could be achieved in the detection and treatment of
psychosocial disorders. Better understanding of the aetiology of persistent frequent
attendance could help to develop more targeted prevention. However, it is unknown
what the influence of psychosocial factors and general practitioner characteristics
is on persistence of frequent attendance.
In a prospective cohort study with a follow-up of 2 years in 623 incident FAs in
2009, we used multilevel ordinal logistic regression analysis with 0, 1 or 2 years
FB as the dependent variable and demographic, somatic, and general practitioner
factors as confounders.
We concluded that panic, generalized anxiety, life events, illness behavior and lack
of ‘mastery’ is independently associated with persistence of frequent attendance.
Prevention should focus on effective treatment of these factors.
In chapter 9 we evaluated whether systematic detection and treatment of depression
and anxiety after 1 and 2 years of frequent attendance might be cost-effective in
comparison with usual care. We applied a Markov model to simulate the course
SUMMARY
181
of a cohort of 10,000 1yFAs over a period of 5 years. Main outcomes were years
of not being a FA without depression or anxiety, and Quality-Adjusted Life-Years
(QALYs). We simulated 25 treatment scenarios with treatment effects expressed
as risk reductions of 10%-40%. In some scenario’s spillover effects on psychiatric
morbidity and frequent attender status were modeled. Uncertainty was estimated
using Monte Carlo simulation (1,000 simulations).
We concluded that systematic diagnostic assessment and treatment of depression
and anxiety in FAs is not cost-effective in comparison with usual care, unless large
spillover effects are assumed.
In chapter 10 we summarize our results. First we elaborate on the strengths and
limitations of our research. Secondly, we describe the literature on this topic. It is
striking that, although FAs are mainly studied in countries with a similar health
care system (enlisted patients), frequent attendance has only once previously been
studied in a scientific study in the Netherlands. Screening and treatment programs
that use frequent attendance as a ‘fishing pond’ for other illnesses (depression,
somatoform disorders , but not anxiety) often have disappointing results, probably
because this study design denies the multi-causal causes of frequent attendance.
In the literature we found only one RCT of good quality that reduces the use of
health care by FAs. In this (Spanish) research GPs analyzed FAs together and
determined a targeted individual approach for each FA.
Based on the results of the aetiological study (Chapter 8), we might possibly prevent
some of the persistent frequent visits and costs of health care by diagnosing and
treating anxiety (panic and generalized anxiety) and inadequate coping style of
FAs. As long as it is not clear whether a systematic care program for FAs might be
(cost) effective, we propose to identify FAs in the electronic medical file (flags) and
treat them individually.
This thesis advocates giving less attention to care programs focused on one single
disorder (often of low prevalence) and to focus on patients, such as (persistent) FAs
that can benefit optimally from the personal, continuous and comprehensive care of
the GP. As described in this thesis the GP spends almost 40% of his time on FAs!
Further research should focus on the background of persistent frequent attendance,
to the significance of the problem list as a proxy for FA’s morbidity and to the
influence of the GP on the frequency of patient consultation. A Randomized Clinical
Trial will have to decide whether and which intervention might be (cost) effective
in improving the quality of life and reduce health care consumption of FAs.
Let’s face the frequent attender not as heart sink but as a challenge for GP care!
Frequent attenders deserve better care, not more care!
182
WHY DO THEY KEEP COMING BACK?
SUMMARY
183
samenvatting
Waarom gaat iemand, soms meerdere jaren achtereen, vaak naar de
huisarts? Meestal natuurlijk vanwege medische problemen, maar soms is de
achtergrond van het frequente bezoek onduidelijk en weet de huisarts niet
goed hoe hierop te reageren. Dit proefschrift beschrijft (de achtergronden
van) frequent bezoek aan de huisarts, onderzoekt welke factoren leiden
tot langdurig frequent bezoek, de relatie met (medisch) aandoeningen, de
mogelijke aanpak van (onbegrepen) frequent bezoek en de gevolgen voor de
werkbelasting van de huisarts en de kosten van de zorg.
Dit proefschrift bestaat uit drie delen:
1.
2.
3.
Retrospectief onderzoek met behulp van gegevens van huisartsen
databases;
Evaluatie van de literatuur over interventies bij frequente bezoekers in
de eerste lijn;
Prospectief onderzoek in een cohort incidente frequente bezoekers.
In hoofdstuk 1 beschrijven we de achtergrond van dit onderzoek. Bijna
iedereen kent periodes waarin, vanwege een (tijdelijk) medisch probleem,
vaker contact met een huisarts nodig is. Wanneer een dergelijke periode
langer aanhoudt, spelen vaak niet alleen chronische lichamelijke, maar ook
psychosociale problemen een rol. Het meeste onderzoek naar frequente
bezoekers (FB’s) betreft dwarsdoorsnede-onderzoek en onderzoekt frequent
bezoek (FB) gedurende één jaar. Langer lopende studies tonen aan dat
slechts 20-30 % van de FB’s gedurende 1 jaar vaak blijven komen in het
daarop volgende jaar. FB’s bezoeken niet alleen hun huisarts vaak, maar
maken ook meer gebruik van andere eerste- en tweedelijns zorg. Het is
184
WHY DO THEY KEEP COMING BACK?
echter onduidelijk in hoeverre dit meer gebruik van de gezondheidszorg door FB’s
verklaard kan worden door ziekten en aandoeningen die zij nu eenmaal hebben
of dat hier sprake is van overgebruik. Langdurig FB is mogelijk een marker voor
onderliggende, nog onopgemerkte, psychosociale problematiek.
Kennis ontbreekt over (de etiologie van) langdurig FB, de kosten die (langdurige)
FB’s maken in de eerste, maar ook in de tweede lijn, en over mogelijke effectieve
behandelingen. Ook wilden we onderzoeken of de huisarts met gegevens,
beschikbaar in het patiëntendossier, zou kunnen voorspellen welke FB’s vaak zullen
blijven komen en wat de invloed is van huisarts kenmerken en huisarts - patiënt
communicatie op (langdurig) FB. Tot slot wilden we met behulp van de gegevens
van een prospectief cohort van FB’s evalueren of opsporen en behandelen van
depressie en angst bij FB’s kosten-effectief zou kunnen zijn.
Omdat FB meestal van tijdelijke aard is en omdat de meeste somatische problemen
al behandeld worden in (chronische) zorgprogramma’s, concentreerden we dit
proefschrift op langdurig frequent bezoek en met name op de specifieke rol van
psychologische en sociale factoren en huisartskenmerken in de etiologie van
(aanhoudend) frequent bezoek.
Deel 1. Retrospectief onderzoek met behulp van gegevens van huisartsen
databases
Hoe kun je FB’s in een normale huisartsenpraktijk het best selecteren? Na
bestudering van de verschillende mogelijkheden, kiezen we in hoofdstuk 2 voor
een proportionele definitie van (langdurige) FB’s per leeftijd en geslacht. Omdat
de bezoekfrequentie afhangt van de leeftijd en geslacht van de patiënt en verschilt
per arts, land en regio, maakt alleen een proportionele definitie het mogelijk
om FB’s (inter)nationaal te vergelijken. Met behulp van een database van het
NIVEL (Nederlands instituut voor onderzoek van de gezondheidszorg; de tweede
nationale studie) stelden we vast dat het voldoet om het patiëntenbestand van een
huisartspraktijk in 3 leeftijdsgroepen per geslacht te verdelen om betrouwbaar de
top 10 % FB’s te kunnen bepalen.
In hoofdstuk 3 beschrijven we de aandoeningen van kortdurende en langdurige FB’s
en de werkbelasting van de huisartsen door FB’s met behulp van de database van de
afdeling huisartsgeneeskunde van het AMC (Hag-net-AMC). Deze database bevat
gegevens van 28.860 volwassen patiënten van 5 gezondheidscentra. We vonden
dat van alle FB’s gedurende 1 jaar (1jFB’s), 15,4 % frequent bleef komen gedurende
3 opeenvolgende jaren (1,6 % van alle ingeschreven patiënten). FB’s “kostten”
de huisarts 4 keer zoveel consulten als zijn niet frequent komende patiënten. De
langdurige FB’s (FB’s gedurende 3 jaar) gebruikten 5 maal zoveel consulten. In
vergelijking met niet frequent komende patiënten hebben FB’s en vooral langdurige
FB’s aanzienlijk meer sociale problemen, gevoelens van angst, verslavingsgedrag
SAMENVATTING
185
en medisch onverklaarde lichamelijke klachten. FB’s hebben ook meer chronische
somatische ziekten dan niet frequent komende patiënten, maar deze verschillen
tussen FB’s en niet-FB’s zijn kleiner dan bij psychosociale aandoeningen.
Hoofdstuk 4. Naast al bekende aandoeningen hebben (langdurige) FB’s mogelijk nog
andere, onbekende (medische) problemen. Ook verhogen FB’s de werkbelasting van
hun huisarts aanzienlijk. Het lijkt daarom verstandig en efficiënt om diagnostiek en
preventie te richten op patiënten met een hoge kans op langdurig frequent bezoek.
Maar kun je voorspellen welke patiënten vaak zullen blijven komen? Om dit te
onderzoeken probeerden we, in een historische cohortstudie, vast te stellen welke
informatie uit het elektronische medische dossier (EMD) voorspelt wie langdurig
frequent zal blijven komen. We gebruikten de gegevens van 28.860 volwassen
patiënten in de jaren 2003-2005.
Van de 3.045 1jFB’s werden er 470 (15.4 % ) een langdurige frequente bezoeker.
Met de huidige EMD gegevens selecteerde ons predictiemodel de patiënten
die het risico lopen om langdurige frequente bezoeker te worden slechts matig
(oppervlakte onder de curve 0,67; 95% betrouwbaarheidsinterval 0,64-0,69). Meer
patiëntinformatie of aanvullende diagnostische tests lijken nodig om voldoende
betrouwbaar langdurig frequent bezoek te kunnen voorspellen.
In hoofdstuk 5 hebben we het predictiemodel, zoals beschreven in hoofdstuk 4,
gevalideerd in een andere regio en periode. We pasten het bestaande model toe in
een later tijdvak (2009-2011) in het oorspronkelijke netwerk (temporele validatie)
en bij patiënten van een ander huisartsbestand (SMILE Eindhoven; 2007-2009,
temporele en geografische validatie). We bestudeerden tevens of het toevoegen van
drie nieuwe voorspellers mogelijk ons predictiemodel zou kunnen verbeteren. Tot
slot, bouwden we een nieuw model op basis van de drie gecombineerde datasets (N
= 12.539 ).
Externe validatie bevestigde dat met de huidige gegevens uit het elektronische
medische dossier langdurige FB’s slechts matig kunnen worden geïdentificeerd.
FB’s maken waarschijnlijk meer kosten in de eerste lijn dan niet-FB’s. Maar hoeveel
geld wordt besteed aan specialistische zorg van FB’s? In hoofdstuk 6 beschrijven
we de uitgaven aan gezondheidszorg door FB’s en testen we de hypothese dat deze
extra kosten kunnen worden verklaard door aandoeningen van deze FB’s en door
kenmerken van hun huisarts. Wij koppelden de gepseudonimiseerde klinische
gegevens van 16.531 patiënten aan de declaratiegegevens van een zorgverzekeraar.
Belangrijkste uitkomstmaten waren alle vergoede kosten voor de 1e en 2e
lijnsgezondheidszorg tussen 2007 en 2009. Kenmerken van de huisartsen werden
verzameld door middel van administratieve gegevens en een vragenlijst.
We concludeerden dat FB’s aanzienlijke kosten maken, niet alleen in de eerste, maar
186
WHY DO THEY KEEP COMING BACK?
ook in de tweede lijn, die niet kunnen worden verklaard door, al bekende, medische
problematiek. Ook werkstijl en kenmerken van de huisartsen lijken deze extra
kosten niet te verklaren. De mechanismen achter deze extra uitgaven moeten nog
worden opgehelderd.
Deel II: Evaluatie van de literatuur over interventies bij frequente bezoekers in
de eerste lijn
In hoofdstuk 7 analyseerden we welke interventies de morbiditeit, de kwaliteit
van leven en het gezondheidszorggebruik van FB’s beïnvloeden. We deden een
systematisch literatuuronderzoek naar artikelen die interventies beschrijven bij
FB’s in de eerste lijn. Uitkomstmaten waren morbiditeit, kwaliteit van leven en het
gebruik van de gezondheidszorg.
We identificeerden 5 RCTs van goede kwaliteit. Drie RCT’s gebruikten FB’s
om patiënten te selecteren met een verhoogd risico voor distress, depressie
en angststoornissen. Deze RCT’s pasten psychologische of psychiatrische
interventies toe. Van deze drie vonden twee RCT’s meer depressie-vrije dagen
en een betere kwaliteit van leven na behandeling van depressie van FB’s. Twee
RCT’s bestudeerden een interventie die gericht was op het verminderen van het
aantal consulten. Geen enkele interventie verlaagde dit aantal. Door verschillen
in de setting van de studies en de selectie van patiënten was meta-analyse van de
resultaten niet mogelijk.
Concluderend vonden we aanwijzingen dat FB’s vaak een nog niet
gediagnosticeerde depressieve stoornissen hebben en dat de behandeling van deze
klachten de depressieve symptomen en de kwaliteit van leven van depressieve FB’s
kan verbeteren. We vonden geen bewijs dat het mogelijk is om het gebruik van
gezondheidszorg te beïnvloeden.
Deel III Prospectief cohort onderzoek
Hoofdstuk 8. Langdurige FB’s lijden vaak aan multimorbiditeit en hebben veel
(onontdekte) psychosociale problematiek. Ervan uitgaande dat patiënten somatisch
adequaat worden behandeld, zou winst behaald kunnen worden in het opsporen
en behandelen van psychosociale aandoeningen. Beter begrip van de etiologie van
langdurig FB zou kunnen helpen bij het ontwikkelen van gerichtere preventie.
Wat is de invloed van psychosociale factoren en huisartskenmerken op langdurig
frequent huisartsbezoek?
In een prospectief cohort onderzoek met een follow-up van 2 jaar bij 623 incidente
FB’s in 2009 gebruikten we een multilevel ordinale logistische regressieanalyse
met 0, 1 of 2 jaar FB als afhankelijke variabele en demografische, somatische en
huisartsfactoren als confounders.
SAMENVATTING
187
We concludeerden dat paniek, gegeneraliseerde angst, levensgebeurtenissen,
ziektegedrag en geringe ‘mastery’ onafhankelijk zijn geassocieerd met persisterend
FB. Preventie van langdurig FB zou zich kunnen richten op effectieve behandeling
van deze factoren.
In hoofdstuk 9 onderzochten wij of systematische opsporing en behandeling van
depressie en angst na 1 en 2 jaar FB kosteneffectief zou kunnen zijn in vergelijking
met gebruikelijke zorg. We gebruikten een Markov model om de loop van een
cohort van 10.000 1jFB’s over een periode van 5 jaar te simuleren. Belangrijkste
uitkomstmaten waren jaren van niet frequent bezoek zonder depressie of angst
en Quality-Adjusted Life-Years (QALY’s). Wij simuleerden 25 verschillende
behandelscenario’s waarbij de effecten werden uitgedrukt als risicoreducties
van 10% - 40%. In sommige scenario’s werd verondersteld dat behandeling van
depressie effect zou hebben op angst en vice versa en op FB (spillover effecten).
Onzekerheid werd geschat met behulp van Monte Carlo simulatie (1000 simulaties
van 10.000 1jFB’s).
We concludeerden dat systematische diagnostiek en behandeling van depressie en
angst bij FB’s niet kosteneffectief is in vergelijking met gebruikelijke zorg tenzij
grote spillover effecten aanwezig zouden zijn.
In hoofdstuk 10 worden de resultaten van dit proefschrift samengevat en beschrijven
we allereerst de sterke punten en de beperkingen van ons onderzoek. Daarna
beschrijven we de literatuur over dit onderwerp. Hierbij valt op dat, hoewel FB’s
vooral bestudeerd zijn in landen met een vergelijkbaar zorgsysteem (inschrijving
op naam), FB in Nederland slechts een maal eerder onderwerp is geweest van een
wetenschappelijke studie. Screening- en behandelprogramma’s die FB gebruiken als
visvijver ter opsporing van andere klachten (depressie, somatoforme stoornissen,
maar niet angst) hebben vaak teleurstellend weinig resultaat, waarschijnlijk omdat
deze opzet de multicausale genese van FB miskent.
In de literatuur vonden we slechts één goed onderzoek dat het gebruik van zorg
door FB’s vermindert. In dit (Spaanse) onderzoek analyseerden huisartsen samen
FB’s waarna een individuele aanpak werd vast gesteld.
Gezien de resultaten van de etiologische studie (hoofdstuk 8), zou mogelijk
een deel van het langdurig frequent bezoek voorkomen kunnen worden en de
kosten verlaagd kunnen worden door bij FB’s diagnostiek te doen naar angst
(paniek en gegeneraliseerde angst) en matige coping stijl (mastery) en door de
aldus aangetoonde aandoeningen te behandelen. Zolang niet duidelijk is of een
systematisch zorgprogramma voor FB’s (kosten) effectief is, stellen wij voor FB’s te
‘ruiteren’ en individueel te behandelen.
188
WHY DO THEY KEEP COMING BACK?
Dit proefschrift pleit ervoor om minder aandacht te geven aan zorgprogramma’s
gericht op één enkele (vaak laag prevalente) aandoening en de huisartsenzorg meer
te richten op patiënten zoals (langdurige) FB’s die meer kunnen profiteren van
de persoonlijke, continue en integrale zorg van de huisarts. De huisarts besteedt
immers circa 40% van zijn consult tijd aan FB’s!
Verder onderzoek moet worden gedaan naar de achtergrond van langdurig frequent
bezoek, naar de betekenis van de Probleem Lijst als weergave van de aandoeningen
van de FB’s en naar de invloed van de huisarts op de bezoekfrequentie van FB’s. Een
Randomized Clinical Trial zal moeten vaststellen of en welke interventie (kosten)
effectief is in het verbeteren van de kwaliteit van leven en het verlagen van de
zorgconsumptie van FB’s.
De frequente bezoeker moet meer een uitdaging worden voor de huisarts. Hij of zij
heeft niet méér zorg nodig, maar bétere zorg!
SAMENVATTING
189
dankwoord
Dankwoorden in proefschriften zijn tricky things! Voor je het weet vergeet
je iemand en beschadig je een (lange en gewaardeerde) samenwerking. Dus
voor ik begin: Neem me niet kwalijk als ik iemand vergeten ben. Ik beroep
me nu al op mijn (oude) geheugen!
Laten we bij het begin beginnen. In 2003 was ik met good old Hans
Grundmeijer ergens aan de borrel (Desmet?). We spraken over wat het
(huisartsen) leven ons al had gebracht en wat we nog wilden doen. Na het
(mede)opzetten van een gezondheidscentrum (Reigersbos in Amsterdamzuidoost), een huis verbouwen, een goede echtgenoot proberen te zijn,
het (mede) opvoeden van kinderen, een huisarts zijn, mede managen van
een centrum en een overkoepelende organisatie, coassistenten en aio’s
begeleiden, onderzoek van andere mogelijk maken etc. , vond ik, enigszins
beneveld door de drank, dat het tijd was voor nieuwe uitdagingen! En
….Hans vond dit natuurlijk een prima idee!
Een nieuwe baan was geen optie (ik wilde huisarts blijven en waar vind je
een leuker centrum met zulke goede collega’s?). Dus werd het onderzoek
doen. We brainstormden over een goed onderwerp (“Wat puzzelt je in je
vak?”) en Hans daagde me uit om hierover door te denken. Nu onder genot
van koffie bleek aan zijn keukentafel dat mijn gekozen onderwerp (frequente
bezoekers van de huisarts) internationaal al veel was bestudeerd, maar dat
Nederlandse gegevens ontbraken. Niet zo geschikt dus, leek, in tijden dat
internationaal publiceren de norm is.
Hans, bedankt voor die eerste ferme en onmisbare stoot in deze richting!
190
WHY DO THEY KEEP COMING BACK?
Maar vervolgens vroeg Henk (van Weert) of ik mee wilde werken aan het Apollo-D
onderzoek dat hij met Aart Schene en Eric Ruhé had opgezet. Het betrof een groot
onderzoek, samen met Nijmegen, over het screenen van hoog risicogroepen op
depressie. Eén van de hoog risicogroepen betrof frequente bezoekers. Ik zou dat
onderdeel (mede) gaan trekken.
Hoewel ik veel heb geleerd in die tijd (van Jochanan Huijser, Aart Schene, Eric
Ruhé en Henk van Weert) en het ook een gezellige tijd was op het kamertje in het
oude psychiatrie gebouw (met Karin Wittkampf, Kim Baas en onderzoeksassistente
Judith Kosman) bleek na enige tijd dat de koek van Apollo-D gegeten zou worden
door de fulltime promovendi uit Amsterdam en Nijmegen.
Ik koppelde mijn 5e wiel aan de wagen noodgedwongen af. Een poging in 2005
om, samen met Aart, subsidie te krijgen van het Nationaal Fonds Geestelijke
Volksgezondheid voor een apart vervolg onderzoek mislukte helaas.
Karen, Kim en Judith, Henk, Aart, Eric en Jochanan bedankt voor die leerzame en
gezellige tijd!
Als langdurig lid van de stuurgroep HAG-net-AMC kende ik, buiten Henk van
Weert, al langer Gerben ter Riet, Henk Brouwer en Jacob Mohrs. Zij wilden me
gelukkig helpen om de ideeën die er lagen uit te werken. Zij waren als geen ander
thuis in de rijke, meerjarige bestanden van het HAG-net-AMC. Deze ‘mannengroep’
leidde, mede, tot 4 artikelen ( hoofdstuk 2, 3,4 en 7).
In 2008 heeft Gerben ter Riet het initiatief genomen om een aanvraag voor ZonMW,
programma alledaagse ziekten, te schrijven voor een vervolg onderzoek. Dit werd
gehonoreerd en ik kon nu voor één dag in de week aan de slag als onderzoeker in het
kader van het PERFACTIO project (acroniem voor: PERsistent Frequent Attenders
risk faCtors and Treatment optIOns). Officiële start 01 12 2008.
Onderzoek doen is teamwork!: Er werd een begeleidingsgroep geformeerd (Henk
van Weert, Aart Schene, Marcel Dijkgraaf, Gerben ter Riet) en een werkgroep
(Gerben ter Riet, Henk Brouwer, Jacob Mohrs en Diana Toll). Later hebben Marcel
en Diana ons verlaten en hebben we succesvol samenwerking gezocht met de
afdeling gezondheidswetenschappen van de VU (Judith Bosmans). Leo Beem
versterkte ons team statistisch.
Gerben, Henk B en Jacob bedankt voor jullie stimulans, hulp en kennis van de
hag-net bestanden en SPSS! Het waren stimulerende, gezellige en productieve
bijeenkomsten op jullie kamers.
De (secretariële en onderzoeks) ondersteuning was al die jaren in de prima handen
van Alice Karsten, Gerda van Zoen en Nienke Buwalda. Alice, Nienke en Gerda
DANKWOORD
191
enorm bedankt voor jullie vele hulp en spandiensten.
Ik wil een paar personen apart noemen.
Allereerst de ‘mannengroep’, het ‘dagelijks bestuur’ van Perfactio:
Gerben, jij was al deze jaren de stimulerende, onvermoeibare onderzoeksleider. Ik
ben je heel veel dank verschuldigd voor het in goede banen houden van Perfactio.
Je grote epidemiologische en onderzoekstechnische kennis waren onmisbaar. Maar
vooral ook de kameraadschap die ik al die jaren bij je gevoeld heb, zal ik niet snel
vergeten. We hebben het toch maar geflikt!
Henk B, zonder mijn fijne contacten met jou, al vanuit de “transitie”tijd, zou ik
waarschijnlijk niet met dit onderzoek zijn begonnen. De manier waarop jij mijn
(klinische) vragen uit de hag-net bestanden wist te toveren hebben mij vaak blij
verrast. Heel wat uren hebben we samen op je kamer aan extracties gewerkt met dit
kloeke boek als resultaat. Enorm bedankt!
Jacob Mohrs, jij was de onverstoorbare ‘diesel’ van Perfactio. Jij maakte bestanden,
bouwde een onderzoeksdatabase en onderhield de contacten met Saxion en de
drukker over de (scan bare) vragenlijsten. Ik kon altijd op je bouwen en bij je terecht
voor hulp of een gezellig praatje. Heel erg bedankt!
Leo Beem, helaas hebben we, door je overlijden, afscheid van je moeten nemen.
Je was onnavolgbaar met cijfers, maar je dikke pak output leverde altijd toch een
bruikbare tabel op. Het ga je goed daarboven!
Koos Zinderman, gelukkig was jij bereid om Leo’s taken over te nemen. Heel
veel bewondering heb ik voor de rustige manier waarop jij, tussen je drukke
werkzaamheden door, tijd vrij maakte voor ons onderzoek. Jij was als geen ander
thuis in onze database! En …ik snap nu iets meer van de wondere achtergronden van
genen en quality of life!
Maar ook het ‘algemeen bestuur’ van de grote begeleidingsgroep was groots:
Allereerst mijn (co)promotores: Henk vW, we kennen elkaar al lang als collega
huisarts en het was even wennen aan deze ‘change of position’. Dit heeft niet lang
geduurd en ik heb voluit geprofiteerd van je grote huisartsgeneeskundige kennis en
onderzoekservaring. Ik kon altijd bij je terecht voor een goed advies, maar ook om
even te bomen over de politiek, de gezondheidszorg, de GAZO en wat niet meer.
Aart, ik leerde je kennen tijdens Apollo en sindsdien ben je bereid geweest om je
grote psychiatrische expertise in te zetten voor de frequente bezoekers van de
huisarts. Heel erg bedankt voor deze langjarige interdisciplinaire inzet en hulp! Erg
bedankt ook voor je altijd snelle en zeer to-the-pointe commentaar op stukken en
concept artikelen.
Judith, jij was onze kenner van kosten en centen. Als VU’er en als enige vrouw had
je het soms moeilijk met de haantjes van het AMC, maar we hebben enorm kunnen
192
WHY DO THEY KEEP COMING BACK?
profiteren van je kennis op het gebied van kosten(effectiviteits)onderzoek. Bedankt
voor je inzet, het meedenken, je prima commentaar op concepten en het (mee)
schrijven!
Gerben heb ik al gememoreerd!
De andere leden van de leescommissie, prof. H. v.d. Horst, prof. T. Lagro, prof. K.
Stronks, prof. M. Maas, prof. J.de Haes en dr. Eric Ruhé, wil ik hartelijk danken
voor het lezen en beoordelen van mijn proefschrift en de bereidheid om tijd vrij te
maken voor de promotie.
Beste collega’s van het gezondheidscentrum Reigersbos, jullie zijn natuurlijk
onmisbaar geweest. Ten eerste hebben jullie mij mede de inspiratie gegeven voor
dit onderzoek, maar ook was onze samenwerking altijd de fijne, stabiele en gezellige
rots in de branding. Ik geloof niet dat jullie verder veel “last” hebben gehad van mijn
andere “baan”, misschien ook wel baten. Heel erg bedankt voor jullie collegialiteit
en vriendschap!
Zonder de medewerking van de huisartsen en patiënten van het Hag-Net-AMC was
dit alles niet mogelijk geweest. Heel erg bedankt voor jullie moeite!
Tot slot mijn thuisfront. Jullie waren, op de achtergrond, erg belangrijk voor het
slagen van dit project. Ik besef heel goed dat ik enigszins heb geparasiteerd op
jullie en dat ik jullie en onze vrienden heb verwaarloosd. Dat moet maar weer snel
veranderen, want zonder jullie was ik nergens en was dit proefschrift trouwens
nooit gelukt. Lieve vrienden en buren, dankzij jullie ging het leven gewoon door en
was er ook de zo nodige afleiding. Bedankt voor jullie vriendschap!
Lieve, lieve Chris, heel erg bedankt voor je liefde, je geduld, maar ook voor de
(psychiatrische) inspiratie die je me heel vaak hebt gegeven en de vele hulp bij deze
promotie. Er breken nu langzamerhand andere tijden voor ons aan! Ik hoop nog veel
gelukkige jaren samen met jou te beleven!
Lieve Laura en Thomas, paranimfen, maar vooral dochter en zoon, bedankt voor
het vormgeven van dit boekje (Laura) en het organiseren van de feestelijkheden
(Thomas), jullie vele hulp bij de promotie, maar vooral voor jullie inspirerende
liefde en gezelligheid.
Chris, Laura, Thomas en Clara, ik hoop nog lang veel pittige discussies met jullie
aan tafel te voeren!
En nu maar hopen dat ik zelf nooit een frequente bezoeker van de (huis)arts zal
worden!
DANKWOORD
193
curriculum
vitae
Frans T.M.Smits werd geboren op 21 december 1950 te Breukelen. Na het
behalen van zijn Gymnasium-bèta-diploma aan het Sint Bonifatius College
te Utrecht in 1969, studeerde hij geneeskunde aan de Radboud Universiteit
Nijmegen. Na het behalen van het artsexamen in 1977, werkte hij tot 1978
als arts-assistent in het psychiatrisch ziekenhuis, huize Padua, te Boekel.
Van 1978 tot 1979 volgde hij de specialisatie tot huisarts aan de Radboud
Universiteit Nijmegen. Van 1979 tot 1981 werkte hij als verpleeghuisarts in
verpleeghuis Dekkerswald te Groesbeek. Tevens bereidde bij in die jaren
mede de start voor van een nieuw gezondheidscentrum in Amsterdam.
In 1982 startte hij een huisartsenpraktijk in het Gezondheidscentrum
Reigersbos, te Amsterdam-zuidoost. Hij was en is bestuurlijk actief binnen
de stichting Gezondheidscentra zuidoost, de afdeling huisartsgeneeskunde
AMC en regionale/stedelijke organisaties. Hij was opleider van coassistenten
en is opleider van artsen die zich specialiseren tot huisarts.
In 1984 participeerde hij in het transitieproject, een registratie project, van
prof. Henk Lamberts. In 1994 maakte hij deel uit van de congrescommissie
van het jaarlijkse NHG-congres (”Huisarts en zinvol handelen- tussen
teveel en tekort doen”). Van 2005 tot 2007 participeerde hij in de
onderzoeksgroep van het Apollo-D project, een onderzoek van de afdelingen
huisartsgeneeskunde en psychiatrie van de universiteit van Amsterdam
en van de Radboud Universiteit Nijmegen naar een screeningsprogramma
van depressieve stoornissen bij hoog risicopatiënten in de huisartspraktijk.
Van 2007 tot 2009 deed hij aan de afdeling huisartsgeneeskunde
van het Academisch Medisch Centrum, universiteit van Amsterdam
194
WHY DO THEY KEEP COMING BACK?
onderzoek naar frequente bezoekers van de huisarts. Van 2009-2014 was hij als
huisartsonderzoeker verbonden aan het PERFACTIO project, een door ZonMw
gesteund onderzoek naar de risicofactoren voor en de behandelmogelijkheden van
(langdurig) frequent bezoekers aan de huisarts.
Frans is gehuwd met Chris E. Folkers en heeft twee kinderen, Laura (1985) en
Thomas (1988).
CURRICULUM VITAE
195
PhD portfolio
196
PhD period:
December 2008 - December 2013
PhD-supervisors:
Dr. Gerben ter Riet
Prof. Dr. H.C. van Weert
Prof. Dr. A.H.Schene
WHY DO THEY KEEP COMING BACK?
Overview of PhD related activties
PhD Training
Year
Workload(hrs)
Cursus ‘Doelmatigheids onderzoek: methodes en principes’
(VU)
2010
21
Presentation hag-net-amc meeting
2009
4
Presentation at the EGPRN conference, Bertinoro, Italy (European General Practice Research Network)
2009
20
Poster presentation at the NHG wetenschapsdag
2010
4
Presentation at the NHG wetenschapsdag
2012
10
Presentation for colleagues of the st. Gazo
2012
4
Presentation at the Achmea congress
2013
10
Presentation at the NHG wetenschapsdag
2014
10
WONCA Europe Regional Conference, Istanbul
2008
21
the EGPRN conference, Bertinoro, Italy
2009
20
NHG-wetenschapsdag
2010
6
NHG conference
2011
6
NHG-wetenschapsdag
2012
6
Achmea conference
2013
6
NHG wetenschapsdag
2014
6
focusgroup of the gezondheidsraad
2010
2
Commentary in Br J Gen Pract. 2010
Apr;60(573):293-4
2010
2
Review article ‘Journal of Affective Disorders’: Published as:
J Affect Disord. 2011 Jun;131(1-3):428-32 The mental health of
doctor-shoppers: experience from
a patient-led fee-for-service primary care setting)
2010
4
Review article Scandinavian Journal of Primary Health Care:
2013
4
Letter to the editor (NRC)
2013
2
Response to Des Spence (BMJ)
(https://cealu11fn98fef.sec.amc.nl/content/348/bmj.
g208?tab=responses)
2014
3
Presentations
(Inter) national conferences
Other activities
PHD PORTFOLIO
197
list of
publications
Publications
198
1.
Contributions to: Gezondheidszorg in Nederland. Sun, Nijmegen,
1973.
2.
Smits F.T: Etniciteit als contextuele factor; Huisarts en
Wetenschap 01/2002; 45(2) 813-813
3.
Smits F.T, Mohrs JJ, Beem EE, Bindels PJ, van Weert HC:
Defining frequent attendance in general practice. BMC Fam Pract
2008,9:21.
4.
Smits F.T, Wittkampf KA, Schene AH, Bindels PJ, van Weert HC.
Interventions on frequent attenders in primary care. A systematic
literature review. Scand.J Prim. Health Care 2008;26(2):111-6.
5.
Wittkampf KA, van ZM, Smits FT, Schene AH, Huyser J, van
Weert HC. Patients’ view on screening for depression in general
practice. Fam Pract 2008; 25(6):438-444.
6.
Wittkampf KA, Van Zwieten M, Smits FT, Schene AH, Huyser
J, Van Weert HC. Wat denken gescreende patiënten met een
depressie over hun diagnose? Huisarts Wet 2009;52(6):274-80.
7.
Smits FT, Brouwer HJ, Ter Riet G, van Weert HH. Epidemiology
of frequent attenders: a 3-year historic cohort study comparing
attendance, morbidity and prescriptions of one-year and
persistent frequent attenders. BMC. Public Health 2009;9:36.
WHY DO THEY KEEP COMING BACK?
8.
Smits FT, Brouwer HJ, van Weert HC, Schene AH, Ter Riet G.
Predictability of persistent frequent attendance: a historic 3-year cohort
study. Br.J Gen.Pract. 2009 Feb;59(559):e44-50.
9.
Smits F T , Brouwer H J, van Weert HC, Schene AH, ter Riet G.:
Langdurig frequent bezoek aan de huisarts moeilijk te voorspellen.
Huisarts en wetenschap. 2009:4:166-172
10. Frans Smits,, Henk Brouwer, Gerben ter Riet. Letter to the editor:
Persistent frequent attenders.Br J Gen Pract April 1, 2010 60:293-294
11. Smits FT, Brouwer HJ, Zwinderman AH, van den Akker M, van SB,
Mohrs J, Schene AH, van Weert HC, Ter RG: Predictability of persistent
frequent attendance in primary care: a temporal and geographical
validation study. PLoS One2013:e73125.
12. Smits FT, Brouwer HJ, Zwinderman AH, Mohrs J, Smeets HM,
Bosmans JE, Schene AH, van Weert HC, Ter RG: Morbidity and
doctor characteristics only partly explain the substantial healthcare
expenditures of frequent attenders: a record linkage study
between
patient data and reimbursements data. BMC Fam Pract 2013, 14:138
13. Smits FT, ter Riet G, Bosmans J, Haroun D: Better care for frequent
attenders is possible. Rapid response BMJ; http://www.bmj.com/
content/348/bmj.g208?tab=responses
14. Letter to the editor of NRC, 26 sept 2013: “Surinamers zijn helemaal niet
duurder in de zorg”
15. Frans T. Smits, Henk J. Brouwer, Aeilko H. Zwinderman, Jacob Mohrs,
Hugo M. Smeets, Judith E. Bosmans, Aart H. Schene, Henk C. van Weert
en Gerben ter Riet: Frequente bezoekers van de huisarts maken hoge
kosten in de eerste en tweede lijn. Ned Tijdschr Geneeskd. 2014;158:A7117
LIST OF PUBLICATIONS
199
200
WHY DO THEY KEEP COMING BACK?