Statistical Considerations in Research Study Designs
advertisement

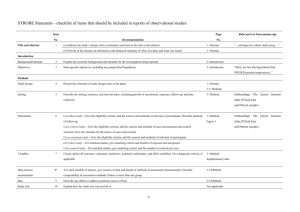
How to Design and Interpret Observational Outcomes Studies in Cardiovascular Disease Nathan D. Wong, PhD, FACC Professor and Director Heart Disease Prevention Program Division of Cardiology, UC Irvine Adjunct Professor of Epidemiology, UCLA and UC Irvine President, American Society for Preventive Cardiology Why are papers rejected for publication? (The Top 11 Reasons) 1. The study did not address an important scientific issue 2. The study was not original 3. The study did not actually test the authors’ hypothesis 4. A different type of study should have been done 5. Practical difficulties led the authors to compromise on the original study protocol (e.g., recruitment, procedures) Greenhalgh T, BMJ 1997; 15: 243-6 Reasons 6-11 for Paper Rejection 6. The sample size was too small 7. The study was uncontrolled or inadequately controlled 8. The statistical analysis was incorrect or inappropriate 9. The authors drew unjustified conclusions from the data 10. There is a significant conflict of interest among authors 11. The paper is so badly written that it is incomprehensible Critical Appraisal 1. Why was the study done, and what clinical question is being asked? (a brief background, review of the literature, and aim / hypothesis should be stated) 2. What type of study was done? (experiment, clinical trial, observational cohort or cross-sectional study, or survey) Critical Appraisal (cont.) 3. Was the design appropriate for the research? • Clinical trial preferred to test efficacy of treatments • Cross-sectional study preferred for testing validity of diagnostic/screening tests or risk factor associations • Longitudinal cohort study preferred for prognostic studies • Case-control study best to examine effects of a given agent in relation to occurrence of an illness, esp. rare illnesses (e.g., cancer) Outline • Elements of Designing a Research Protocol • Concepts of Study Design: Observational cross-sectional, case-control, cohort studies • Advantages and Disadvantages of Different Study Designs – which is right for you? • Analysis of Observational Studies Nine Key Elements of a Research Study Protocol • • • • • • • • • Background Hypotheses Clinical Relevance Specific Aims / Objectives Methodology Power / Sample Size Measures and Outcomes Data Management Statistical Methodology (UCI School of Medicine Scientific Review Committee) Background • A brief review of the problem to be studied and of related studies that generated the rationale and the central idea of the proposed study. Several pertinent references should be provided. Was the study original? • Few studies break entirely new ground • Many studies add to the evidence base of earlier studies which may have had other or more limitations • Meta-analyses depend on literature containing multiple studies addressing a question in a similar manner Features Distinguishing New vs. Previous Studies • • • • Sample size Length of follow-up More rigorous methodology Different population studied different from that of previous studies (ages, gender, ethnic groups)? • Does the new study address a clinical issue of sufficient importance? Greenhalgh T, BMJ 1997; 315: 305-8 Specific Aims / Objectives • What the study is intended to study or demonstrate; includes mention of predictor and outcome (or endpoint) variables. • For example: "The primary aim of the study is to examine whether treatment A is more effective than treatment B in reducing levels of C", or "in finding out whether X is associated with Y", etc. • There may both principal and secondary aims Elements of a Formulated Question • Patient or Population: Who is the question about? (e.g., pts with diabetes mellitus) • Intervention or Exposure: What is being done or what is happening to the patient/population? (e.g., tight control) • Outcome(s): How does the intervention affect the patient/population (mortality, CHD incidence) • Comparison(s): What could be done instead of the intervention? (e.g., standard management) Hypotheses • The problem/s stated in the Background may generate a primary hypothesis and possibly one or two secondary hypotheses. • A hypothesis is often stated in the null – e.g., "No difference between treatments A and B" is anticipated, or "No association between X and Y exists". • Alternatively, it can be stated according to what one expects e.g., “A will be more effective than B in reducing levels or symptoms of C", or “X will be associated with Y". Clinical / Community Relevance • In the case of clinical studies, the potential value in the understanding, diagnosis, or management of a clinical condition or pathological state should be stated. • Funding agencies often now require a statement of community relevance – e.g., how will the results be translated and disseminated to the target population or community. Methodology • Methodology should validate or not validate the hypothesis and specific aims using procedures consistent with sound scientific study design including: – the size and nature of the subjects studied – recruitment, screening, and enrollment procedures – inclusion and exclusion criteria – treatment schedules, and follow-up procedures, if applicable. A chart of the studies to be performed at each visit and the time of each visit and test is needed. Study Population Issues • How were the subjects recruited? Is there potential recruitment bias (e.g., from taking respondents of advertisements), or is survey done in a random (e.g., random digit-dialing) or consecutive sample? • Who was included? Many trials exclude those who have co-morbidities, do not speak English, or take other medications—may provide scientifically clean results, but may not be representative of disease in question. Study Population (cont.) • Who was excluded? Study may exclude those with more severe forms of disease, therefore limiting generalizibility • Were subjects studied in “real-life” circumstances? Is the consenting process describing the benefits/risks, access to study staff, equipment available, etc. be similar to that in an ordinary practice situation? Power / Sample Size • A power/sample size analysis should include an estimate of minimum effect or difference expected at a given level of power when the sample size is fixed, or a projection of the number of subjects needed to achieve a clinically important difference in what is being examined in the hypotheses and the specific aims. Measures and Outcomes • Includes both independent (predictor) and dependent (outcome) variables. • Outcomes include what the investigator is trying to predict, e.g., new or recurrent onset of a disease state, survival, or lowering of cholesterol. • The independent or predictor variables should always include treatment status (e.g., active vs. placebo) in the case of a clinical trial, or primary variables of interest (such as age, gender, levels of X at baseline) for other studies. • The measures and outcomes should expect to answer the proposed question and the importance of the knowledge expected from the research. Data Management • Data Management includes how data is captured for analysis and the tools that will be utilized while capturing the data. This includes: – Case report forms for clinical trials – Surveys, questionnaires, or interview instruments – Computerized spreadsheets or entry forms – Methods for data entry, error checking, and maintenance of study databases Statistical Methods of Analysis • Statistical analysis includes a description of the statistical tests planned to perform to examine the results obtained, e.g., – Student’s t-test will be used to compare levels of A and B between treatment and placebo groups – Multiple logistic regression analysis will be used to examine an independent treatment effect on the likelihood of recurrent disease. Hierarchy of Evidence (for making decisions about clinical interventions or proving causation) 1. Systematic reviews and meta-analyses 2. Randomized controlled trials with definitive and clinically significant effects 3. Randomized controlled trials with nondefinitive results 4. Cohort studies 5. Case-control studies 6. Cross-sectional surveys 7. Case reports Features Affecting Strength and Generalizability of Study • sample size • selection of comparison group (control or placebo) • selection of study sample (is it representative of population the study results are intended to apply to?) • length of time of follow-up • outcome assessed (e.g., hard vs. soft or surrogate endpoint) • Measurement and ability to control for potential confounders Case Reports and Series • Provides “anectdotal” evidence about a treatment or adverse reaction • Often with significant detail not available in other study designs • May generate hypotheses, help in designing a clinical trial. • Several reports forming a “case series” can help establish efficacy of a drug, or thru adverse reports, cause its demise (example: Cerivastatin fatal cases of rhabdomyolysis). Observational Studies • Cross-sectional, prospective, and casecontrol studies seldom can identify two groups of subjects (exposed vs. unexposed or cases vs. controls) that are similar (e.g., in demographic or other risk factors). • Much of the controlling for baseline and/or follow-up differences in subject characteristics occurs in the analysis stage (e.g., multivariable analysis as in Framingham) Observational Studies (cont.) • While statistical procedures may be done correctly, have we considered all possible confounders? • Some covariates may not have been measured as accurately as possible, and more often, may not be even known or measured. Observational, cross-sectional • Examines association between two factors (e.g, an exposure and a disease state) assessed at a single point in time, or when temporal relation is unknown • Example: Prevalence of a known condition, association of risk factors with prevalent disease. • Conclusions: Associations found may suggest hypotheses to be further tested, but are far from conclusive in proving Cross-Sectional Studies and Surveys • Examples: NHANES III, CHIS (telephone), chart-review studies • Surveys should include a representative, ideally randomly-chosen (rather than a small sample of approached subjects who actually agree to be surveyed) sample. • Data collected cannot assume any directionality in exposure / disease. • Can statistically adjust for confounders, but difficult to establish the temporal nature of exposure and disease. Prevalence of CHD by the Metabolic Syndrome and Diabetes in the NHANES Population Age 50+ CHD Prevalence 25% 19.2% 20% 13.9% 15% 10% 8.7% 7.5% 5% 0% No MS/No % of DM Population = 54.2% MS/No DM 28.7% DM/No MS 2.3% Alexander CM et al. Diabetes 2003;52:1210-1214.. DM/MS 14.8% Prospective (Cohort) Studies • Cohort studies begin with identification of a population, assessment of exposure (e.g., lipid or BP levels) • Follow-up to the occurrence of outcomes (CHD events)-- temporal sequence (e.g, follow-up time) to events is known Cohort Studies (cont.) • Difficult to ascertain effect of exposure because of many differences between exposed and unexposed groups (confounding factors). • Statistical adjustment for known risk factor differences can help, but unknown factors that may differ between exposed and unexposed groups will never be adjusted for. Duration of Follow-up • Is the planned follow-up reasonable and practical for the study question and sample size utilized? – effect of a new painkiller on degree of pain relief may only require 48 hours – effect of a cholesterol medication on mortality may require 5 years Prospective cohort studies • Examples: – Framingham Heart Study – Cardiovascular Health Study (CHS) – Multiethnic Study of Atherosclerosis (MESA) – Nurses Health Study • Advantages: – large sample size – ability to follow persons from healthy to diseased states – temporal relation between risk factor measures and development of disease Prospective Studies (cont.) • Disadvantages: – expensive due to large sample size often needed to accrue enough events – many years to development of disease – possible attrition – causal inference not definitive as difficult to consider all potential confounders Framingham Heart Study • Longest running study of cardiovascular disease in the world • Began in 1948 with original cohort of 5,209 subjects aged 30-62 at baseline • Biennial examinations, still ongoing, most of original cohort deceased • Offspring cohort of 5,124 of children of original cohort enrolled in 1971, and more recently and still being enrolled to better understand genetic components of CVD risk are up to 3,500 grandchildren of the original cohort. • Routine surveillance of cardiovascular disease events adjudicated by panel of physicians Framingham Most Significant Milestones • 1960 Cigarette smoking found to increase the risk of heart disease • 1961 Cholesterol level, blood pressure, and electrocardiogram abnormalities found to increase the risk of heart disease • 1967 Physical activity found to reduce the risk of heart disease and obesity to increase the risk of heart disease • 1970 High blood pressure found to increase the risk of stroke • 1976 Menopause found to increase the risk of heart disease • 1978 Psychosocial factors found to affect heart disease • 1988 High levels of HDL cholesterol found to reduce risk of death • 1994 Enlarged left ventricle (one of two lower chambers of the heart) shown to increase the risk of stroke • 1996 Progression from hypertension to heart failure described 14-y incidence rates (%) for CHD Low HDL-C Levels Increase CHD Risk Even When Total-C Is Normal (Framingham) 14 12 10 8 6 4 2 0 < 40 40–49 50–59 60 HDL-C (mg/dL) 260 230–259 200–229 < 200 Risk of CHD by HDL-C and Total-C levels; aged 48–83 y Castelli WP et al. JAMA 1986;256:2835–2838 Cardiovascular Health Study • 5,201 Medicare eligible individuals aged 65-102 at baseline enrolled beginning 1992 at six field centers. • Assessment of newer and older risk factors. • Ongoing follow-up of cardiovascular events and mortality • Subclinical disease measures included: – carotid B-mode ultrasound for carotid IMT at Year 2, Year 7, and Year 11 – m-mode echocardiographic measures of left ventricular mass and dimensions, left atrial dimension done at baseline (Year 2) (at UC Irvine) and follow-up (Year 7) examinations. – Ankle brachial index (ABI) for measurement of PAD – Pulmonary function (FVC and FEV1) Procedure BAS E Call B YR 3 Call 3 YR 4 Call 4 Tracking Update X X X X X X Stressful Life Events X X X X X X Depression Scale X X X Quality of Life X X X Social Support and Network X X X Medications - Prescription X X X Physical Function: ADL/IADL X X Cognitive Function MMSE X OTC 3MSE Digit Symbol Substitution X X X X X X X X X Benton Visual Retention Phlebotomy X Anthropometry - Weight X Standing Height X Waist Circumference X Hip Circumference X Arm Span X Cardiovascular Health Study: Combined intimal-medial thickness predicts total MI and stroke Cardiovascular Health Study (CHS) (aged 65+): MI or stroke rate 25% over 7 years in those at highest quintile of combined IMT (O’Leary et al. 1999) Case-control Studies • Most frequent type of epidemiologic study, can be carried out in a shorter time and require a smaller sample size, so are less expensive • Only practical approach for identifying risk factors for rare diseases (where follow-up of a large sample for occurrence of the condition would be impractical) • Selection of appropriately matched control group (e.g., hospital vs. healthy community controls) and consideration of possible confounders crucial • Relies on historical information to obtain exposure status (and information on confounders) Case-Control Studies (cont.) • Cannot determine for sure whether exposure preceded development of disease • Also difficult to identify all differences between cases and controls that can be statistically adjusted for Example of case-control study: Folate and B6 intake and risk of MI (Tavani et al. Eur J Clin Nutr 2004) • Cases were 507 patients with a first episode of nonfatal AMI, and controls were 478 patients admitted to hospital for acute conditions • Information was collected by intervieweradministered questionnaires • Compared to patients in the lowest tertile of intake, the ORs for those in the highest tertile were 0.56 (95% CI 0.35-0.88) for folate and 0.34 (95% CI 0.19-0.60) for vitamin B6. • Author conclusion: A high intake of folates, vitamin B6 and their combination is inversely associated with AMI risk Potential sources of bias and error in case control studies • Information on the potential risk factor or confounding variables may not be available from records or subjects’ memories • Cases may search for a cause of their disease and be more likely to report an exposure than controls (recall bias) • Uncertainty as to whether agent caused disease or whether occurrence of the disease caused the person to be exposed to the agent • Difficulty in assembling a case group representative of all cases, and/or assembling an appropriate control group Prospective, observational: nested case-control • In this design, one takes incident cases (e.g., incident CVD) and a matched set of controls to examine the association of a risk factor measured sometime before development of the outcome of interest • Less costly than a true prospective design where all subjects are included in analysis; may not provide equivalent estimates Prospective study of CRP and risk of future CVD events among apparently healthy women (Ridker et al., Circulation 1998) – a nested case control study • 122 female pts who suffered a first CVD event and 244 age and smoking-matched controls free of CVD • Logistic regression estimated relative risks and 95% CI’s, adjusted for BMI, diabetes, HTN, hypercholesterolemia, exercise, family hx, and trt • Those who developed CVD events had higher baseline CRP than controls; those in the highest quartile of CRP had a 4.8-fold (4.1 adjusted) increased risk of any vascular event. For MI or stroke, RR=7.3 (5.5 adjusted) hs-CRP Adds to Predictive Value of TC:HDL Ratio in Determining Risk of First MI Relative Risk 5.0 4.0 3.0 2.0 1.0 0.0 High Medium High Medium Low Total Cholesterol:HDL Ratio Ridker et al, Circulation. 1998;97:2007–2011. Low Examples where observational studies have taken us down the wrong path…… • Meta-analysis of observational studies have shown a 50% lower risk of CHD among estrogen users vs. non-users (which may have had many unknown differences that were not adjusted for), but recently randomized trials (HERS, WHI) show no benefit • Numerous prospective studies show a 25-50% lower risk of CHD among those taking vitamin E and other antoxidants vs. placebo– recent randomized trials (e.g., HOPE, HPS) show no benefit. Randomized Clinical Trial • Considered the gold standard in proving causation– e.g., by “reducing” putative risk factor of interest • Randomization “equalizes” known and unknown confounders/covariates so that results can be attributed to treatment with reasonable confidence • Inclusion and exclusion criteria can often be strict (to maximize success of trial) and may require screening numerous patients for each patient randomized Randomized Clinical Trials (2) • Expensive, labor intensive, attrition from loss to follow-up or poor compliance can jeopardize results, esp. if more than outcome difference between groups • Conditions are highly controlled and may not reflect clinical practice or the real world • Funding source of study and commercial interests of investigators can raise questions about conclusions of study Randomized Controlled Trials (3) • Randomized controlled trial eliminates systematic bias (in theory) by allocating treatments among participants in a random fashion • The allocation process eliminates selection bias in group characteristics (check comparability of baseline characteristics such as age, gender, severity of disease and covariate risk factors) (selection bias) Questions to Ask Regarding Statistical Analysis • Was there sufficient power/sample size? • Was the choice of statistical analysis appropriate? • Was the choice (and coding/classification) of outcome and treatment variables appropriate? • Is there an adequate description of magnitude and precision of effect? • Was there adjustment for potential confounders? • Have the results been correctly interpreted and not overstated? Statistical significance and power • Statistical significance is based on the Type I or Alpha error – the probability of rejecting the null hypothesis when it was true (saying there was a relationship when there isn’t one) – usually we accept being wrong <5% of the time, or alpha=0.05 • The Type II or Beta error is the probability of accepting the null when it was false (saying there is no relationship when there is one) • Power of a test is the probability of detecting a true result or difference (rejecting the null hypothesis of no difference when it is false), also 1-beta (80% conventional) Measures of Precision of Effect • The p-value, or alpha error most commonly indicates the precision of the result, with a low p-value corresponding to a precise result. • A t-statistic, F-statistic, Chi-square, or rsquare value gives the relative magnitude of a relation. • The higher the magnitude of the above statistics, the more precise or stronger is the relationship between the explanatory variable (s) and the outcome of interest. Precision of Effect: The Confidence Interval • The estimate of where the true value of a result lies is expressed within 95% confidence intervals, which will contain the true relative risk or odds ratio 95% of the time – corresponds to 2-tailed alpha=0.05 • 95% Confidence intervals are the RR + 1.96 X SE (since SE is SD/ sqrt(N), confidence intervals are smallest (precision greatest) with larger studies. Variable Classification • What is your outcome (Y) (dependent variable) of interest? – Categorical (binary, 3 or more categories) examples: survival, CHD incidence, achievement of BP control (yes vs. no) – Continuous: change in blood pressure • What is the main explanatory or independent variable (X) of interest? – Categorical (binary, 3 or more categories) examples: treatment status (active vs. placebo), JNC-7 blood pressure category (normal, pre-HTN, Stage 1 HTN, Stage 2 HTN) – Continuous: baseline systolic / diastolic blood pressure Covariates / Confounders • The relationship between X and Y may be partially or completely due to one or more covariates (C1, C2, C3, etc.) if these covariates are related to both X and Y • A comparison of baseline treatment group differences in all possible known covariates is often done and presented • Covariates / confounders normally equalized between groups only in randomized clinical trial designs Analyzing Effects of Confounders • The effect of confounders can be assessed by: – Stratifying your analysis by levels of these variables (e.g., examine relationship of X and Y separately among levels of covariates C) – Adjusting for covariates in a multivariable analysis – Considering interaction terms to test whether effect of one factor (e.g., treatment) on outcome varies by level of another factor (e.g., gender) Fallacies in Presenting Results: Statistically vs. Clinically Significant? • Having a large sample size can virtually assure statistically significant results, but often with a very low effect size or relative risk (e.g., a correlation of 0.10 is low but could be statistically significant when the sample is large) • Conversely, an insufficient sample size can hide (not significant) clinically important differences where the effect size or relative risk may be large. • Statistical significance is directly related to sample size and magnitude of effect or difference, and indirectly related to variance in measure. Assessing Accuracy of a Test TRUE DISEASE STATUS / TREATMENT DIFFERENCE TEST RESULT DISEASED / YES NONDISEASED TOTAL / NO POSITIVE / reject null a b a+b NEGATIVE / accept null c d c+d TOTAL a+c b+d a+b+c+ d SENSITIVITY = a / (a+c) SPECIFICITY = d / (b+d) Pos. Pred. Value = a / (a+b) Neg. Pred. Value = d/(c+d) False positive error (alpha, Type I) = b / (b+d) False negative error (beta, Type II) = c/ (a+c) Statistics and Statistical Procedures for Cross-Sectional and Case-Control Designs – When both independent and dependent variables are continuous: Pearson correlation or linear/polynomial regression – When dependent variable is continuous and independent variables are categorical (with or without continuous or categorical covariates) Analysis of variance (Analysis of covariance with covariates). Analysis for Cross-Sectional and Case Control Designs (cont.) – When both independent and dependent variables are categorical: Chi-square test of proportions- prevalence odds ratio for likelihood of factor Y in those with vs. w/o factor X. – When outcome is binary (e.g., survival) and explanatory variables are categorical and/or continuous: • Student-test or Chi-square for initial analysis • Logistic regression (multiple logistic regression for covariate adjustment) Odds of CVD Stratified by CRP Levels in U.S. Persons (Malik and Wong et al., Diabetes Care, 2005) 6 O d d s R a t i o *** 5 4 3 2 *** * * ** 1 0 High CRP No Metabolic disease Syndrome Low CRP Diabetes –*p<.05, **p<.01, **** p<.0001 compared to no disease, low CRP –CRP categories: >3 mg/l (High) and <3 mg/L (Low) –age, gender, and risk-factor adjusted logistic regression (n=6497) Metabolic Syndrome Independently Associated with Inducible Ischemia from SPECT (Wong ND et al., Diabetes Care 2005; 28: 1445-50 ) Predictor OR 95% CI P value Log coronary calcium (per SD) 4.11 2.60-6.51 <0.001 Chest Pain Symp 2.94 1.69-5.09 <0.001 1-2 MetS risk factors 2.99 0.70-12.8 0.14 3 MetS risk factors 4.80 1.01-22.9 0.049 4-5 MetS risk factors 10.93 2.09-57.2 0.005 Diabetes 4.55 0.98-21.1 0.053 *Estimates adjusted for age, gender, cholesterol and smoking. Odds of ischemia for metabolic abnormalities (yes vs. no) (separate model): 1.98 (1.20-3.98), p=0.008 Statistical Procedures for Prospective Cohort Studies • When outcome is continuous: Linear and/or polynomial regression • When outcome is binary: Relative risk (RR) for incidence of disease in those with vs. without risk factor of interest, adjusted for covariates and considering follow-up time to event--Cox proportional hazards regression: HR (t,zi) = HR0 (t) exp (α’zi) • If follow-up time is not known, use logistic regression: p (Y=1 | r1,r2,…) = 1/(1+ exp[-a-b1r1… b nr n) CHD, CVD, and Total Mortality: US Men and Women Ages 30-74 (age, gender, and risk-factor adjusted Cox regression) NHANES II Follow-Up (n=6255)(Malik and Wong, et al., Circulation 2004; 110: 12451250) 7 *** 6 *** 5 *** 4 *** *** *** 3 *** *** *** 2 * ** 1 0 CHD Mortality CVD Mortality Total Mortality * p<.05, ** p<.01, **** p<.0001 compared to none None MetS Diabetes CVD CVD+Diabetes CV Event-Free 8-year Survival Using Combined hs-CRP and LDL-C Measurements (n=27,939) 1.00 Median LDL 124 mg/dl Probability of Event-free Survival Median CRP 1.5mg/l Low CRP-low LDL 0.99 Low CRP-high LDL 0.98 High CRP-low LDL 0.97 0.96 High CRP-high LDL 0.00 0 2 4 6 Years of Follow-up Ridker et al, N Engl J Med. 2002;347:1157-1165. 8 Questions to ask regarding study results • How large is the treatment effect (or likelihood of outcome)? – Relative risk reduction (may obscure comparative absolute risks) – Absolute risk reduction: is this clinically significant? • How precise is the treatment effect (or likelihood of outcome)? – What are the confidence intervals? – Do they exclude the null value? (e.g., is the result statistically significant– magnitude of Chi-square or F-value) MRC/BHF Heart Protection Study (HPS): Eligibility • Age 40–80 years • Increased risk of CHD death due to prior disease – Myocardial infarction or other coronary heart disease – Occlusive disease of noncoronary arteries – Diabetes mellitus or treated hypertension • Total cholesterol > 3.5 mmol/L (> 135 mg/dL) • Statin or vitamins not considered clearly indicated or contraindicated by patient’s own doctors Heart Protection Study Group. Lancet. 2002;360:7-22. HPS: First Major Coronary Event StatinPlaceboType of Major Allocated Allocated Vascular Event (n = 10269) (n = 10267) Coronary events Nonfatal MI 357 (3.5%) 574 (5.6%) Coronary death 587 (5.7%) 707 (6.9%) Subtotal: MCE 898 (8.7%) 1212 (11.8%) Statin Better 0.73 (0.670.79) P < 0.0001 Revascularizations Coronary 513 (5.0%) 725 (7.1%) Noncoronary 450 (4.4%) 532 (5.2%) Subtotal: any RV 939 (9.1%) 1205 (11.7%) Any MVE 2033 (19.8%) Placebo Better 0.76 (0.700.83) P < 0.0001 0.76 (0.720.81) 2585 (25.2%) P < 0.0001 0.4 0.6 0.8 1.0 1.2 1.4 These results from the Heart Protection Study frequently present a relative risk reduction of 24% (or relative risk of 0.76), but an absolute risk reduction of only 5.5% associated with the simvastatin treatment. Heart Protection Study Collaborative Group. Lancet. 2002;360:722. Examining Magnitude of Effect: HPS Study Example of Vascular Event Reduction Event Yes Simvastatin/ a Event No Treatment 2042 b 8227 Placebo / Control c 2606 d 7661 Control event rate (CER) = c/c+d = 2606/10267=0.254 Experimental event rate (EER) = a/a+b = 2042/10269 = 0.199 Relative Risk (RR) = EER/CER = (.199)/(.254) = 0.78 Relative Risk Reduction (RRR) = CER-EER/CER=(0.254-0.199)/.254= 0.22 Absolute Risk Reduction (ARR) = CER-EER = 0.01 – 0.008 = 0.055, or 5.5% Number Needed to Treat = 1/ARR = 1/0.055 = 18.2 (or 56 events prevented per 1000 treated) Suggestions for Comparison of Models for Risk Prediction 1. Compare global model fit 2. Compare calibration and discrimination 3. Assess reclassification If global fit is better, but calibration/discrimination similar--- Is fit better among some individuals? (i.e. high risk) - Is the new risk category more accurate in those reclassified? 4. Would a higher or lower risk estimate change treatment for an individual patient? Cook N. Circulation 2007. ROC Curves and the c-Statistic • Measure of discrimination – Probability that the predicted risk is higher for a case than a non-case • A function of the sensitivity and specificity for each value of a measure or model – Perfect discrimination: c-statistic of 1 • Scores for all the cases are higher than scores for all noncases --- no overlap! – No discrimination: c-statistic of 0.5 (coin toss) • NOT the probability that an individual is classified correctly (people with high score will become a case) predictive value Comparison of ROC Areas for Prediction of Myocardial Ischemia 1.0 0.9 0.8 0.7 0.6 Age, gender, CRF, log(CCS+1) Area=80%, SE=.03 0.5 0.4 0.3 0.2 0.1 Age, gender, CRF Area=74%, SE=.03 All p<.001 Age, gender Area=66%, SE=.03 log(CCS+1) Area=76%, SE=.03 0.0 0.0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1.0 1-Specificity Berman and Wong et al., J Am Coll Cardiol 2004; 44: 923-930. Problems with C-statistic • If improvement in the c-statistic was used as the criterion for model selection: – Neither LDL, HDL, nor total cholesterol would have been included in Framingham score! Conclusion: Discrimination is only 1 aspect of model performance Reclassification • Can new markers accurately stratify individuals into higher or lower risk categories? • Important for clinical risk prediction! • Net Reclassification Index (NRI) • Integrated Discrimination Index Reclassification Table -Reclassified in desirable direction -Reclassified in undesirable direction Schnabel et abl. Circ 2010. Summary • Research protocols need to include key design elements such as hypotheses, background / aims, and methods, including subject selection/power analysis and statistical methods. • Different study designs have key advantages and disadvantages and levels of evidence for causation. • Evaluating results from studies requires an understanding of appropriate use of measures of effect and consideration of statistical vs. clinical significance. Thank you! For more information contact the UCI Heart Disease Prevention Program at: www.heart.uci.edu 949-824-5561