Bayesian evidence synthesis in drug
development and comparative
effectiveness research
David Ohlssen (Novartis Pharmaceticals Corporation)
Introduction
Evidence synthesis in drug development
The ideas and principles behind evidence synthesis date
back to the work of Eddy et al; 1992
However, wide spread application has been driven by the
need for quantitative health technology assessment:
• cost effectiveness
• comparitive effectiveness
Ideas often closely linked with Bayesian principles and
methods:
• Good decision making should ideally be based on all relevant
information
• MCMC computation
Recent developments in comparative effectiveness
Health agencies have increasing
become interested in health
technology assessment and the
comparative effectiveness of
various treatment options
Statistical approaches include
extensions of standard metaanalysis models allowing
multiple treatments to be
compared
FDA Partnership in Applied
Comparative Effectiveness
Science (PACES) -including
projects on utilizing historical
data in clinical trials and
subgroup analysis
Aims of this talk
Evidence synthesis
Introduce some basic concepts
Illustration through a series of applications:
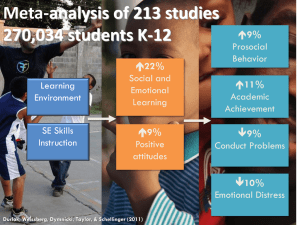
• Motivating public health example
• Meta-analysis and Network meta-analysis
• Using historical data in the design and analysis of clinical trials
• Extrapolation
• Subgroup analysis
Focus on principles and understanding of critical
assumptions rather than technical details
Basic concepts
Framework and Notation for evidence synthesis
Y1
Y2
YS
Y1,..,YS
Data from S sources
1,…, S
Source-specific
parameters/effects of interest
(e.g. a mean difference)
2
1
?
S
Question related to 1,…, S
(e.g. average effect,
or effect in a new study)
Strategies for HIV screening
Ades and Cliffe (2002)
HIV: synthesizing evidence from multiple sources
Aim to compare strategies for screening for HIV in prenatal clinics:
• Universal screening of all women,
• or targeted screening of current injecting drug users (IDU) or women
born in sub-Saharan Africa (SSA)
Use synthesis to determine the optimal policy
Key parameters
Ades and Cliffe (2002)
a- Proportion of women born in sub-Saharan Africa (SSA)
b Proportion of women who are intravenous drug users (IDU)
c HIV infection rate in SSA
d HIV infection rate in IDU
e HIV infection rate in non-SSA, non-IDU
f Proportion HIV already diagnosed in SSA
g Proportion HIV already diagnosed in IDU
h Proportion HIV already diagnosed in non-SSA, non-IDU
NO direct evidence concerning e and h!
A subset of some of the data used in the synthesis
Ades and Cliffe (2002)
HIV prevalence, women not born in SSA,1997-8
[db + e(1 − a − b)]/(1 − a)
74 / 136139
Overall HIV prevalence in pregnant women, 1999
ca + db + e(1 − a − b)
254 / 102287
Diagnosed HIV in SSA women as a proportion of all
diagnosed HIV, 1999
fca/[fca + gdb + he(1 − a − b)]
43 / 60
Implementation of the evidence synthesis
Ades and Cliffe (2002)
The evidence was synthesized by placing all data sources
within a single Bayesian model
Easy to code in WinBUGS
Key assumption – consistency of evidence across the
different data sources
Can be checked by comparing direct and indirect evidence
at various “nodes” in the graphical model (Conflict p-value)
Meta-analysis and network metaanalysis
Why use Bayesian statistics
for meta-analysis?
Natural approach for accumulating data / meta-analysis
Unified modelling and the ability to explore a wide range of modelling
structure
• Synthesis of evidence from multiple sources / multiple treatments
Formal incorporation of other sources of evidence by utilizing prior
distributions for modelling unknowns. e.g.
• Ability to incorporate prior information regarding background event
rates
• Ability to model between-study variability properly in random effects
models
Probability statements about true effects of treatment easier to
understand than confidence intervals and p-values
Bayesian random effects meta-analysis for summary data
Let yi denote the observed treatment effect in trial i and si2
be the corresponding estimated standard error
yi | i ~ N(i, si2)
i ~ N(m, t2)
Add prior distributions for unknowns:
m ~ N(?, ?)
• Heterogeneity
t ~ halfN(0, ?)
t ~ Unif(0, ?)
Carlin JB, Meta-analysis for 2x2 tables: a Bayesian approach. Statistics in Medicine 1992; 11: 141-58
Bayesian method - extending the basic model
Characterizing heterogeneity and prediction (See Higgins
et al; 2009)
• Heterogeneity: quantification – but not homogeneity test
• Mean effect: important, but incomplete summary
• Study effect: maybe of interest, if studies distinguishable
• Prediction: effect in new study most relevant and complete
summary (predictive distribution)
Flexibility
• Alternative scales and link function - see Warn et al (2002)
• Flexible random effects distributions – see Lee et al (2007) and
Muthukumarana (2012)
• Combining individual patient data with aggregate data - see Sutton
et al (2008)
• Subgroup analysis – see Jones et al (2011)
• Multiple treatments and network meta-analysis-
Motivation for Network Meta-Analysis
There are often many treatments for health conditions
Published systematic reviews and meta-analyses typically
focus on pair-wise comparisons
• More than 20 separate Cochrane reviews for adult smoking
cessation
• More than 20 separate Cochrane reviews for chronic asthma in
adults
An alternative approach would involve extending the
standard meta-analysis techniques to accommodate
multiple treatment
This emerging field has been described as both network
meta-analysis and mixed treatment comparisons
15
Bayesian Network Meta-Analysis
Systematic reviews are considered standard
practice to inform evidence-based decisionmaking regarding efficacy and safety
Bayesian network meta-analysis (mixed
treatment comparisons) have been presented
as an extension of traditional MA by including
multiple different pairwise comparisons across
a range of different interventions
Several Guidances/Technical Documents
recently published
Treatment comparison representation
A vs. B vs. C vs. D vs. P
A
P
B
P
A
P
B
P
A
P
B
P
A
P
B
C
A
D
B
C
A
D
B
D
17
Treatment comparison representation
A vs. B vs. C vs. D vs. P
A
P
B
P
A
P
B
P
A
P
B
P
A
P
B
C
A
D
B
C
A
D
B
D
18
P
A
C
B
D
Treatment comparison representation
A vs. B vs. C vs. D vs. P
A
P
B
P
A
P
B
P
A
P
B
P
A
P
B
C
A
D
B
C
A
D
B
D
P
A
C
B
D
Network Meta-Analysis
(NMA)
19
Treatment comparison representation
A vs. B vs. C vs. D vs. P
A
P
B
P
A
P
B
P
A
P
B
P
A
P
B
C
A
D
B
C
A
D
B
D
P
A
C
B
D
Direct comparison
Indirect comparison
Network Meta-Analysis
(NMA)
20
Network meta-analysis – key assumptions
Three key assumptions (Song et al., 2009):
Homogeneity assumption – Studies in the network MA
which compare the same treatments must be sufficiently
similar.
Similarity assumption – When comparing A and C
indirectly via B, the patient populations of the trial(s)
investigating A vs B and those investigating B vs C must
be sufficiently similar.
Consistency assumption – direct and indirect
comparisons, when done separately, must be roughly in
agreement.
Network meta-analysis
Trelle et al (2011) - Cardiovascular safety of non-steroidal anti-inflammatory
drugs:
Primary Endpoint was myocardial
infarction
Data synthesis 31 trials in 116 429
patients with more than 115 000
patient years of follow-up were
included.
A Network random effects metaanalysis were used in the analysis
Critical aspect – the assumptions
regarding the consistency of
evidence across the network
How reasonable is it to rank and
compare treatments with this
technique?
Trelle, Reichenbach, Wandel, Hildebrand, Tschannen, Villiger, Egger, and Juni. Cardiovascular safety of non-steroidal anti-inflammatory drugs
network meta-analysis. BMJ 2011; 342: c7086. Doi: 10.1136/bmj.c7086
Poisson network meta-analysis model
Based on the work of Lu and Ades (LA) (2006 & 2009)
b is the control treatment
associated with trial i
μj is the effect of the baseline treatment b in trial i and δibk is the trialspecific treatment effect of treatment k relative to treatment to b (the
baseline treatment associated with trial i)
Note baseline treatments can vary from trial to trial
Different choices for µ’s and ’s. They can be: common (over studies),
fixed (unconstrained), or “random”
Consistency assumptions required among the treatment effects
Prior distributions required to complete the model specification
Results from Trelle et al
Myocardial infarction analysis
Relative risk with 95% confidence interval compared to placebo
Treatment RR estimate
Celecoxib
1.35
Diclofenac
0.82
Etoricoxib
0.75
Ibuprofen
1.61
Lumiracoxib
2.00
Naproxen
0.82
Rofecoxib
2.12
lower limit
0.71
0.29
0.23
0.50
0.71
0.37
1.26
upper limit
2.72
2.20
2.39
5.77
6.21
1.67
3.56
Authors' conclusion:
Although uncertainty remains, little evidence exists to
suggest that any of the investigated drugs are safe in
cardiovascular terms. Naproxen seemed least harmful.
25
Comments on Trelle et al
Drug doses could not be considered (data not available).
Average duration of exposure was different for different
trials.
Therefore, ranking of treatments relies on the strong
assumption that the risk ratio is constant across time for all
treatments
The authors conducted extensive sensitivity analysis and
the results appeared to be robust
Two way layout via MAR assumption
An alternative way to parameterize proposed by Jones et al (2011) and Piephoetal et
al (2012) uses a classical two-way (TW) linear predictor with main effects for
treatment and trial.
Both papers focus on using the two-way model in the classical framework. By using
the MAR property a general approach to implementation in the Bayesian framework
can be formed
All studies can in principle contain every arm, but in practice many arms will be
missing. As the network meta-analysis model implicitly assume MAR (Lu and Ades;
2009) a common (though possibly missing) baseline treatment can be assumed for
every study (Hong and Carlin; 2012)
Comments on implementation and practical advantages
In WinBUGS include every treatment in every trial with
missing outcome cells for missing treatments
Utilize a set of conditional univariate normal distributions
to form the multivariate normal (this speeds up
convergence)
The parameterization has several advantages when
forming priors:
• In the Lu and Ades model, default “non-informative” priors must be
used as the trial baseline parameters are nuisance parameters with
no interpretation
• In the two-way model an informative prior for a single treatment
baseline treatment can be formed as each trial has the same
parameterization
• In the two way model there is much greater control over noninformative priors. This can be valuable when you have rare safety
events asymmetry in prior information can potentially lead to a bias
Full multivariate meta-analysis
Instead of associating a concurrent control
parameter with each study, an alternative
approach is to place random effects on every
treatment main effect
This creates a so called multivariate meta-analysis
29
MI and stroke results from Trelle et al
Comparing LA FE RE model with the TW RE model and MV RE
Discussion of full multivariate meta-analysis model
Allows borrowing of strength across baseline as
every treatment is considered random
Therefore, in rare event meta-analysis,
incorporates trials with zero total events through
the random effects
No consistency relations to deal with!
Priors on the variance components can be formed
using inverse Wishart or using Cholesky
decomposition
Breaks the concurrent control structure so
automatically will introduce some confounding
Future directions
Network meta-analysis with multiple outcomes
• Sampling model (multinomial?)
• Borrow strength across treatment effects
• Surrogate outcome meta-analysis combined with
a network meta-analysis
Network meta-analysis with subgroup analysis
Combining network meta-analysis; meta-analysis
of subgroups and multivariate meta-analysis
More work on informative priors for variance
components and baseline parameters
Use of Historical controls
Introduction
Objective and Problem Statement
Design a study with a control arm / treatment arm(s)
Use historical control data in design and analysis
Ideally: smaller trial comparable to a standard trial
Used in some of Novartis phase I and II trials
Design options
• Standard Design:
“n vs. n”
• New Design:
“n*+(n-n*) vs. n” with n* = “prior sample size”
How can the historical information be quantified?
How much is it worth?
The Meta-Analytic-Predictive Approach
Framework and Notation
Y1
Y2
Y1,..,YH
Historical control data from
H trials
YH
1,…, H
Control “effects” (unknown)
2
?
‘Relationship/Similarity’
(unknown)
no relation… same effects
1
?
*
H
*
Effect in new trial (unknown)
Design objective: [ * | Y1,…,YH ]
Y*
Y*
Data in new study
(yet to be observed)
Example – meta-analytic predictive approach to form priors
Application
Random-effect meta-analysis
prior information for control group
in new study, corresponding to
prior sample size n*
Bayesian setup-using historical control data
Meta Analysis of Historical Data
Study Analysis
Drug
Placebo
Observed Control Response
Rates
Prior
Distribution
of Control
Response
Rate
Historical
Trial 1
Observed
Control
data
Prior
Distribution
of drug
response
rate
Observed
Drug
data
Historical
Trial 2
Historical
Trial 3
Historical
Trial 4
Historical
Trial 5
MetaAnalysis
Predictive
Distribution
of Control
Response
Rate in a
New Study
Bayesian
Analysis
Posterior Distribution of
Control Response Rate
Posterior Distribution of
Drug Response Rate
Historical
Trial 6
Historical
Trial 7
Historical
Trial 8
Posterior Distribution of
Difference in Response
Utilization in a quick kill quick win PoC Design
... ≥ 70%
... ≥ 50%
... ≥ 50%
1st Interim
2nd Interim
Final analysis
Positive PoC if
P(d ≥ 0.2)...
Negative PoC if
P(d < 0.2)...
... ≥ 90%
... ≥ 90%
With N=60, 2:1 Active:Placebo, IA’s after 20 and 40 patients
First interim
Second interim
... > 50%
Final
Overall
power
Stop for
efficacy
Stop for
futility
Stop for
efficacy
Stop for
futility
Claim
efficacy
Fail
0
1.6%
49.0%
1.4%
26.0%
0.2%
21.9%
3.2%
d = 0.2
33.9%
5.1%
27.7%
3.0%
8.8%
21.6%
70.4%
d = 0.5
96.0%
0.0%
4.0%
0.0%
0.0%
0.0%
100.0%
Scenario
d=
With pPlacebo = 0.15, 10000 runs
R package available for design investigation
Extrapolation
Thanks to Roland Fisch
General Background: EMA Concept Paper on
Extrapolation
EMA produced a “Concept paper on extrapolation of efficacy
and safety in medicine development”:
A specific focus on Pediatric Investigation Plans :
‘Extrapolation from adults to children is a typical
example ...’
Bayesian methods mentioned:
• ‘could be supported by 'Bayesian' statistical approaches’
Alternative Approaches:
- No extrapolation: full development program in the target population.
- Partial extrapolation: reduced study program in target population
depending on magnitude of expected differences and certainty of
assumptions.
- Full extrapolation: some supportive data to validate the extrapolation concept.
Adult data Bayesian meta-analytic predictive approach
Model
Mixed effect logistic regression model
Yi ~ Binomial( Ni , πi )
logit( πi ) = μ + i + xi β
Study i, Yi = number of events, Ni = number of
patients, πi = event rate
• μ: intercept
• i ~ N(0, σ2): random study effect
• xi : design matrix (Study level covariates)
The Meta-Analytic-Predictive Approach
Framework and Notation
σ
n
*
μ
i
x*
yobs
Yrep
β
ni
YH
yi
xi
Subgroup analysis
Based on Jones, Ohlssen, Neuenschwander, Racine,
Branson (2011)
Introduction to Subgroup analysis
For biological reasons treatments may be more effective in
some populations of patients than others
• Risk factors
• Genetic factors
• Demographic factors
This motivates interest in statistical methods that can
explore and identify potential subgroups of interest
45
Challenges with exploratory subgroup analysis
random high bias - Fleming 2010
Effects of 5-Fluorouracil Plus Levamisole on Patient
Survival Presented Overall and Within Subgroups, by Sex and Age*
Hazard Ratio Risk of Mortality
Analysis
North Central
Intergroup
Group
Treatment
Study
Group Study
# 0035
(n = 162)
(n = 619)
All patients
0.72
0.67
Female
Male
0.57
0.91
0.85
0.50
Young
Old
0.60
0.87
0.77
0.59
Assumptions to deal with extremes
Jones et al (2011)
Similar methods to those used when combining historical
data
However, the focus is on the individual subgroup
parameters g1,......, gG rather than the prediction of a new
subgroup
1) Unrelated Parameters
g1,......, gG
(u)
Assumes a different treatment effect in each subgroup
2) Equal Parameters
g1=...= gG
(c)
Assumes the same treatment effect in each subgroup
3) Compromise.
Effects are similar/related to a certain degree
(r)
Comments on shrinkage estimation
This type of approach is sometimes called shrinkage
estimation
Shrinkage estimation attempts to adjust for random high
bias
When relating subgroups, it is often desirable and logical to
use structures that allow greater similarity between some
subgroups than others
A variety of possible subgroup structures can be examined
to assess robustness
Subgroup analysis– Extension to multiple studies
Data summary from several studies
• Subgroup analysis in a
meta-analytic context
• Efficacy comparison T
vs. C
• Data from 7 studies
• 8 subgroups
• defined by 3 binary baseline covariates A, B, C
• A, B, C high (+) or low (-)
• describing burden of
disease (BOD)
• Idea: patients with
higher BOD at baseline
might show better
efficacy
Graphical model
Subgroup analysis involving several studies
Y1
Y2
Y...
?
1
2
S
Study-specific parameters
1,…, S
• Parameters allow data to be
combined from multiple studies
Y1,..,YS
Data from S studies
YS
g2
g1
?
gG
Subgroup parameters
g1,…, gG
• Main parameters of interest
• Various modeling structures can be
examined
Extension to multiple studies
Example 3: sensitivity analyses across a range of subgroup structures
• 8 subgroups
• defined by 3 binary base-line covariates
A, B, C
• A, B, C high (+) or low (-)
• describing burden of disease (BOD)
51 | Evidence synthesis in drug development
Summary
Subgroup analysis
Important to distinguish between exploratory subgroup
analysis and confirmatory subgroup analysis
Exploratory subgroup analysis can be misleading due to
random high bias
Evidence synthesis techniques that account for similarity
among subgroups will help adjust for random high bias
Examine a range of subgroup models to assess the
robustness of any conclusions
Overall Conclusions
• There is general agreement that good decision making should be
based on all relevant information
• However, this is not easy to do in a formal/quantitative way
• Evidence synthesis
- offers fairly well-developed methodologies
- has many areas of application
- is particularly useful for company-internal decision making (we have used
and will increasingly use evidence synthesis in our phase I and II trials)
- has become an important tool when making public health policy decisions
References
Evidence Synthesis/Meta-Analysis
DerSimonian, Laird (1986). Meta-analysis in clinical trials. Controlled Clinical Trials, 7;
177-88
Gould (1991). Using prior findings to augment active-controlled trials and trials with
small placebo groups. Drug Information J. 25 369--380.
Normand (1999). Meta-analysis: formulating, evaluating, combining, and reporting
(Tutorial in Biostatistics). Statistics in Medicine 18: 321-359.
See also Letters to the Editor
by Carlin (2000) 19: 753-59, and Stijnen (2000) 19:759-761
Spiegelhalter et al. (2004); see main reference
Stangl, Berry (eds) (2000). Meta-analysis in Medicine in Health Policy. Marcel Dekker
Sutton, Abrams, Jones, Sheldon, Song (2000). Methods for Meta-analysis in Medical
Research. John Wiley & Sons
Trelle et al., “Cardiovascular safety of non-steroidal anti-inflammatory drugs: network
non-steroidal anti-inflammatory drugs: network meta-analysis,” BMJ 342 (January 11,
2011): c7086-c7086.
Meta-analysis and network meta-analysis
Carlin J. Meta-analysis for 2 2 tables: A Bayesian approach. Statistics in Medicine 1992; 11(2):141–158, doi:10.1002/sim.4780110202.
Smith TC, Spiegelhalter DJ, Thomas A. Bayesian approaches to random-effects meta-analysis: A comparative study. Statistics in Medicine 1995;
14(24):2685–2699, doi:10.1002/sim.4780142408.
Warn D, Thompson S, Spiegelhalter D. Bayesian random effects meta-analysis of trials with binary outcomes: methods for the absolute risk
difference and relative risk scales. Statistics in Medicine 2002; 21(11):1601–1623, doi:10.1002/sim.1189.
Lambert PC, Sutton AJ, Burton PR, Abrams KR, Jones DR. How vague is vague? a simulation study of the impact of the use of vague prior
distributions in MCMC using WinBUGS. Statistics in Medicine 2005; 24(15):2401–2428, doi:10.1002/sim.2112.
Turner RM, Davey J, Clarke MJ, Thompson SG, Higgins JP. Predicting the extent of heterogeneity in meta-analysis, using empirical data from the
Cochrane Database of Systematic Reviews. International journal of epidemiology 2012; 41(3):818–827.
Sutton A, Kendrick D, Coupland C. Meta-analysis of individual-and aggregate-level data. Statistics in Medicine 2008; 27(5):651–669,
doi:10.1002/sim.2916.
Turner R, Spiegelhalter D, Smith G, Thompson S. Bias modelling in evidence synthesis. Journal of the Royal Statistical Society: Series A(Statistics
in Society) 2009; 172:21–47.
Lee K, Thompson S. Flexible parametric models for random-effects distributions. Statistics in Medicine 2007; 27(3):418–434.
Muthukumarana S, Tiwari RC. Meta-analysis using Dirichlet process. Statistical Methods in Medical Research Jul 2012;
doi:10.1177/0962280212453891.
Jones HE, Ohlssen DI, Neuenschwander B, Racine A, Branson M. Bayesian models for subgroup analysis in clinical trials. Clinical Trials Apr 2011;
8(2):129–143, doi:10.1177/1740774510396933.
Turner RM, Davey J, Clarke MJ, Thompson SG, Higgins JP. Predicting the extent of heterogeneity meta-analysis, using empirical data from the
Cochrane Database of Systematic Reviews. Internationalj ournal of epidemiology 2012; 41(3):818–827.
56
Historical Controls
Ibrahim, Chen (2000). Power prior distributions for regression models.Statistical
Science, 15: 46-60
Neuenschwander, Branson, Spiegelhalter (2009). A note on the power prior.
Statistics in Medicine, 28: 3562-3566
Neuenschwander, Capkun-Niggli, Branson, Spiegelhalter. (2010). Summarizing
Historical Information on Controls in Clinical Trials. Clinical Trials, 7: 5-18
Pocock (1976). The combination of randomized and historical controls in
clinical trials. Journal of Chronic Diseases, 29: 175-88
Spiegelhalter et al. (2004); see main reference
Thall, Simon (1990). Incorporating historical control data in planning phase II
studies. Statistics in Medicine, 9: 215-28
Subgroup Analyses
Berry, Berry (2004). Accounting for multiplicities in assessing drug safety:
a three-level hierarchical mixture model. Biometrics, 60: 418-26
Davis, Leffingwell (1990). Empirical Bayes estimates of subgroup effects in clinical trial.
Controlled Clinical Trials, 11: 37-42
Dixon, Simon (1991). Bayesian subgroup analysis. Biometrics, 47: 871-81
Fleming (2010), “Clinical Trials: Discerning Hype From Substance,” Annals of Internal
Medicine 153:400 -406.
Hodges, Cui, Sargent, Carlin (2007). Smoothing balanced single-error terms Analysis of
Variance. Technometrics, 49: 12-25
Jones, Ohlssen, Neuenschwander, Racine, Branson (2011). Bayesian models for subgroup
analysis in clinical trials. Clinical Trials Clinical Trials 8 129 -143
Louis (1984). Estimating a population of parameter values using Bayes and empirical Bayes
methods. JASA, 79: 393-98
Pocock, Assman, Enos, Kasten (2002). Subgroup analysis, covariate adjustment and
baseline comparisons in clinical trial reporting: current practic eand problems. Statistics in
Medicine, 21: 2917–2930
Spiegelhalter et al. (2004); see main reference
Thall, Wathen, Bekele, Champlin, Baker, Benjamin (2003). Hierarchical
Bayesian approaches to phase II trials in diseases with multiple subtypes, Statistics in
Medicine, 22: 763-80
Acknowledgements
Stuart Bailey ,Björn Bornkamp, Roland Fisch, Beat
Neuenschwander, Heinz Schmidli, Min Wu, Andrew Wright