The lacrimal apparatus
advertisement
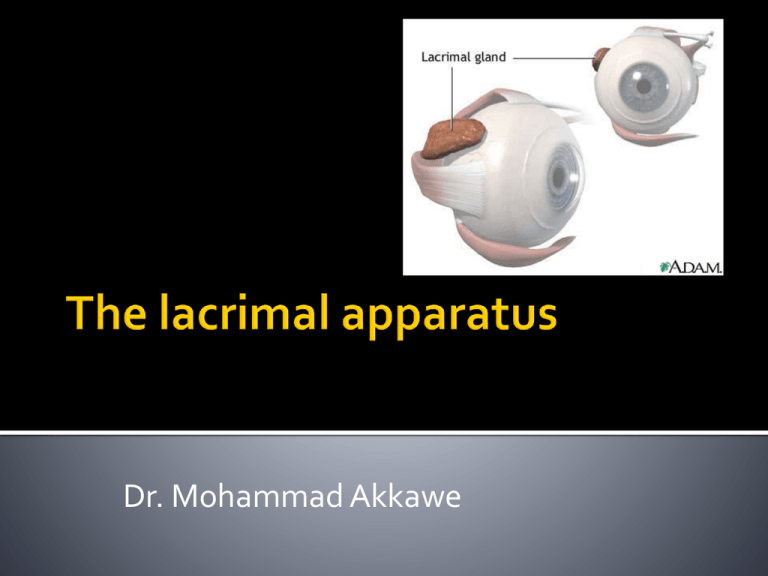
Dr. Mohammad Akkawe The lacrimal glands are paired almondshaped glands, one for each eye, that secrete the aqueous layer of the tear film. They are situated in the upper, outer portion of each orbit, in the lacrimal fossa of the orbit formed by the frontal bone. Anatomists divide the gland into two sections. The smaller palpebral portion, lies close to the eye, along the inner surface of the eyelid; if the upper eyelid is everted, the palpebral portion can be seen. The orbital portion contains fine interlobular ducts that unite to form 3 - 5 main excretory ducts, joining 5 - 7 ducts in the palpebral portion before the secreted fluid may enter on the surface of the eye. The lacrimal gland is tubuloacinar gland derived from surface ectoderm with ducts lined by a low columnar or cuboidal epithelium (often bilayered). The secretory cells in the acini have a predominance of dense granules, suggesting that most are of a serous nature However, some cells are mucus producing The lobules of the orbital portion of the lacrimal gland are near the orbital septum but lie under the levator muscle. The fornix of the upper eyelid lies immediately adjacent to the accessory lacrimal gland of Krause The glands of Krause are accessory lacrimal glands having the same structure as the main gland. They are placed deeply in the subconjunctival connective tissue (mainly) of the upper fornix between the tarsus and the inferior lacrimal gland, of which they are offshoots. There are some 42 in the upper and 6 to 8 in the lower fornix. Glands of Wolfring are also accessory lacrimal glands, but larger than the glands of Krause. There are 2 to 5 in the upper lid situated actually in the upper border of the tarsus about its middle between the extremities of the tarsal glands or just above the tarsus. The postganglionic secretomotor fibres (which arise from the pterygopalatine ganglion) “hitch-hike” on the zygomaticotemporal and lacrimal nerves to the gland The accessory lacrimal tissue found at various sites in the conjunctiva is histologically identical to the main lacrimal gland, as are the secretions it produces Tear secretion can be classified as basal secretion and reflex secretion the concept of “basal” tear production is a redundant one, as even minimal tear production in the undisturbed eye is thought to be secondary to light or temperature stimulation or both Reflex tearing is mediated via parasympathetic nerves that stimulate the myoepithelial cells lining lacrimal acini, causing them to contract These fibers originate in the superior salivatory nucleus and lesions in this region will reduce reflex tearing Sympathetic nerves may influence tear production by altering the blood flow to the lacrimal glands The underlying mechanism of psychogenic tearing is not clearly understood, but it is always bilateral The original model of the precorneal tear film described a trilayered film composed of: anterior lipid layer, middle aqueous layer an inner hydrophilic mucin layer produced by the goblet cells lipid Aqueous Mucoid Location Anterior Middle @ the corneal epithelium Thickness 0.1 µm 10 µm 30 µm Secreted by Meibomian glands, glands of Zeis Lacremal glands, accessory lacremal gland Conjunctiva Function Reduces evaporation. Prevents overflow from lid margin Contains nutrients. Uptakes O2 from cornea Allows the tear film to spread evenly on a hydrophopic corneal surface Until recently it was thought that the mucin layer is <o.o5µm, however it was discovered by modern imaging techniques that the actual thickness is 30µm and that the tear film is a mucus dominated gel hydrated by aqueous fluid Mucin secreting cells are found throughout the conjunctiva with a maximal concentration inferonasally The stability of the tear film is dependent on: the epithelial glycocalyx the antievaporative effects of the lipid layer the viscous properities of the tears imparted by the mucin layer The tear film break-up time is a crude measure of tear film stability, and is of the order of 10-30 seconds in normal eyes The maximum volume of the conjunctival sac is 20 µm but the normal tear volume is approximately 6-7 µm because of the effect of blinking This explains why only 20% of an average drop of medication (approximately 50 µm) is retained in the conjunctival sac, the rest being lost to overflow A tear turnover rate of 18% per minute compounds poor retention of medication, which means that after 5 min only 40% of the medication is present in the conjunctival sac A normal schrimer’s test would produce 1525 mm of “wetting” over a period of 5 mins The primary secretion from the acinar region of the lacrimal gland is essentially an ultrafiltrate of plasma; it is later modified by ductal secretion of potassium chloride This explains elevated potassium (15-30 mmol/l) concentrations, with respect to plasma Passive diffusion of electrolytes through the intercellular spaces of conjunctival or corneal surface epithelial cells is prevented by tight junctions The osmolarity of the aqueous layer is approximately that of normal saline and the PH is 7.4 The precorneal tear film and the limbal vessels supply the corneal epithelium with glucose; the glucose concentration in the aqueous layer is therefore lower than that of plasma The protein components of unstimulated tears is variable but is usually 7-10 mg/ml this falls to 3.9mg/ml with high flow rates The major protein constituents of the precorneal tear film comprise those produced by the acinar cells and those derived from other sources Production of the acinar derived proteins lysosyme and lactoferrin rises with increasing stimulation, and therefore their concentration in the tear film remains relatively constant Lysosyme and lactoferrin are antibacterial agents; the former breaks down bacterial cell walls and the latter inhibits the growth of irondependent bacteria and also scavenges free radicals The concentrations of both lactoferrin and lysosyme decrease with age The production of secretory IgA decreases with increased tear production Conversely, the levels of secretory IgA rises markedly at night, as aqueous tear production by the acinar cells declines IgG concentrations are very low (0.004g/l) in the normal tear film compared with those of secretory IgA levels (1.9 g/l),although IgG levels are elevated in inflamatory conditions as a result of leakage from conjunctival vessels Tear lipocalin ( formerly known as tear specific prealbumin) accounts for 20% of tear film production It has significant homology with members of the lipocalin family of proteins, which bind small hydrophobic molecules Tear lipocalin was thought to have a protective effect on the epithelium and has been shown to inhibit cysteine proteinase The tear film lipids are derived from the meibomian glands, these holocrine glands excrete a clear oil on to the lid margins in response to each blink Most tear film lipids is in the form wax esters 32% and sterol esters 27% free fatty acids accounting for only 2% of tear film lipids Other lipid components of the tear film include diesters, triacyl triglycerides and polar lipids The profile of free fatty acids and the proportion of lipid classes varies considerably between individuals, and may be a factor that predisposes to the development of chronic plepharitis The composition of lipid after realease is altered by the action of lipolytic lid margin bacteria and is invariably different from that of the lipid originally produced by the meiobian glands