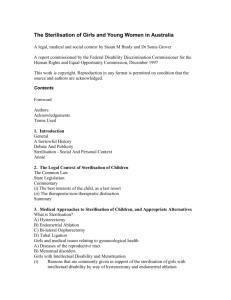
Cleaning, Disinfection, and Sterilisation
advertisement

Cleaning, Disinfection, and Sterilisation 1. Differentiate between disinfection and sterilisation. 2. Explain different types of sterilisation. 3. Outline the process for cleaning patient care items. December 1, 2013 Learning Objectives 2 • 90 minutes December 1, 2013 Time involved 3 • Cleaning, disinfection, and sterilisation are the backbone of infection prevention and control • Proper cleaning essential before any disinfection or sterilisation process • Failure to sterilise or disinfect reusable medical devices properly may spread infections • The type and level of device decontamination depends upon the nature of the item and its intended use December 1, 2013 Key points - 1 4 • Steam sterilisation effective only when preceded by • Thorough pre-cleaning, proper packaging/loading, and careful monitoring of autoclaves • Chemical disinfectants must be selected, used, and discarded to minimise harm • Those responsible for processing contaminated items must be fully trained and wear protective clothing when necessary • Clearly written policies and procedures must be available on-site for training personnel and for monitoring their performance December 1, 2013 Key points - 2 5 • A process of treatment that renders a medical device, instrument, or environmental surface safe to handle • Does not necessarily mean that the item is safe for patient reuse December 1, 2013 Decontamination 6 Everyone responsible for handling and reprocessing contaminated items must: • Receive adequate training and periodic retraining • Wear appropriate personal protective equipment (PPE) • Receive adequate prophylactic vaccinations December 1, 2013 Pre-Cleaning/Cleaning 7 Divided hospital instruments into general categories based on the risk of infection involved in their use • • • December 1, 2013 Spaulding Classification Critical items Semi critical item Non critical items 8 • Enter normally sterile tissues, the vascular system, or equipment through which blood flows • Items must be properly and safely pre-cleaned and sterilised before use December 1, 2013 Critical Items 9 • Implants • Prosthetic devices • Surgical instruments • Needles • Cardiac catheters • Urinary catheters • Biopsy forceps of endoscope December 1, 2013 Critical Items - Examples 10 • Contact mucous membranes but do not penetrate soft tissue or body surfaces • Meticulous physical cleaning followed by appropriate high-level disinfection December 1, 2013 Semi-critical Items 11 • Flexible fiberoptic endoscopes • Respiratory therapy equipment • Anaesthesia equipment • Endotracheal tubes • Bronchoscopes • Vaginal specula • Cystoscope • Hand-piece December 1, 2013 Semi-critical Item - Examples 12 • Direct contact with the patients intact skin (unbroken skin) • Little risk of pathogen transmission directly to patient • Clean and disinfect using a low to intermediate level disinfectant December 1, 2013 Non Critical Items 13 Items which are in contact with intact skin • • • • • • Bedpans Blood pressure cuffs Crutches Stethoscopes Face mask X-ray machine December 1, 2013 Examples of Non Critical Items 14 A process that eliminates many or all pathogenic microorganisms on inanimate objects, with the exception of bacterial spores December 1, 2013 Disinfection 15 • The complete elimination or destruction of all forms of microbial life • Includes large numbers of highly resistant bacterial spores December 1, 2013 Sterilisation - 1 16 • Store in clean, dry place • Protect wrapping • Inspect before use December 1, 2013 Sterilisation - 2 17 • Written and up-to-date policies and procedures must be available on-site for training/monitoring staff responsible for device reprocessing • Train staff fully and retrain as necessary; maintain written records • The staff must also be provided with: December 1, 2013 Staff Training and Protection • Personal protective equipment (PPE) • Prophylactic vaccinations 18 • Single-use items must be safely discarded after use • e.g., injection needles • No reprocessing before carefully considering the following: • • • • • Is device undamaged and functional? Can it be disassembled for reprocessing? Can its sterility be validated, if needed? Is the reprocessing cost-effective? Is an authorised person onsite willing to be responsible for any negative consequences? December 1, 2013 Single-Use Items 19 • Method to be used will depend on: • Device’s intended use • Risk of infection • Degree of soilage December 1, 2013 Choice of Method • Process must not damage the device 20 • Reduction in numbers of pathogens on inanimate surfaces/objects • For items that will contact intact skin or mucous membrane • Use physical or chemical agents or both December 1, 2013 Disinfection • Level of disinfection • High-level • Intermediate-level • Low-level 21 • Active against vegetative bacteria, viruses (including the non-enveloped ones), fungi, and mycobacteria • May have some activity against bacterial spores December 1, 2013 High-level Disinfectants - 1 • With extended contact times • HLDs are used to disinfect heat-sensitive and semi-critical devices • Such as flexible fibreoptic endoscopes 22 • HLDs typically require 10-45 minutes contact time • Depends on the temperature December 1, 2013 High-level disinfectants - 2 • After disinfection, items require thorough rinsing/flushing with sterile or filtered water to remove any chemical residues • They must then be dried with an alcohol rinse or by blowing clean, filtered air through the device’s channels prior to storage 23 • Active against vegetative bacteria, mycobacteria, fungi and most viruses • May fail to kill spores, even after prolonged exposure December 1, 2013 Intermediate-level Disinfectants 24 • Active against vegetative bacteria (except mycobacteria), some fungi, and only enveloped viruses • In many cases, washing with unmedicated soap and water would be sufficient in place of LLD December 1, 2013 Low-level Disinfectants 25 Agents Alcohols (60-90%) including ethanol and isopropanol Spectrum Uses Low- to intermediatelevel disinfectant. Used for decontaminating the outside of some semicritical and noncritical items, e.g., oral and rectal thermometers and stethoscopes. Also to disinfect small surfaces such as rubber stoppers of multi-dose vials. Alcohols with detergent are safe and effective for spot disinfection of countertops, floors, and other surfaces. Also common in handrubs. Advantages Fast acting. No residue. Non-staining. Low cost. Widely available in many countries for medicinal and research purposes. Disadvantages Volatile, flammable, and an irritant to mucous membranes. Inactivated by organic matter. May harden rubber, cause glue to deteriorate, or crack acrylate plastic. December 1, 2013 Chemical disinfectants in health care 26 Agents Chlorine and chlorine compounds: the most widely used is an aqueous solution of sodium hypochlorite 5.25-6.15% (domestic bleach) at a concentration of 1005000 ppm free chlorine Spectrum Low- to high-level disinfectant. Uses Used for disinfecting tonometers and for spot disinfection of countertops and floors. Can be used for decontaminating blood spills. Concentrated hypochlorite or chlorine gas is used for disinfection of large and small water distribution systems, such as dental appliances, hydrotherapy tanks, and water distribution systems in haemodialysis centres. Advantages Low cost, fast acting. Readily available in most settings. Available as liquid, tablets or powders. Disadvantages Corrosive to metals in high concentration (>500 ppm). Inactivated by organic material. Decolourises or bleaches fabrics. Releases toxic chlorine gas when mixed with ammonia. Irritant to skin and mucous membranes. Unstable if left uncovered, exposed to light, or diluted; store in opaque container. December 1, 2013 Chemical disinfectants in health care 27 Agents Aldehydes Glutaraldehyde: ≥2% alkaline or acidic solutions. Also formulated with phenol-sodiumphenate and alcohol. Spectrum High-level disinfectant. Uses Widely used as highlevel disinfectant for heat-sensitive semicritical items such as endoscopes. Advantages Good material compatibility. Disadvantages Allergenic and irritating to skin and respiratory tract. Must be monitored for continuing efficacy levels when reused. December 1, 2013 Chemical disinfectants in health care 28 Agents Orthophthalaldehyde (OPA) 0.55% Spectrum High-level disinfectant. Uses Advantages High-level disinfectant Excellent stability over for endoscopes. wide pH range. Superior mycobactericidal activity compared to glutaraldehyde. Does not require activation. Disadvantages Expensive. Stains skin and mucous membranes; may stain items not thoroughly cleaned. Eye irritation. Poor sporicide. Must be monitored for efficacy during reuse. Contraindicated for reprocessing certain urological instruments. December 1, 2013 Chemical disinfectants in health care 29 Agents Peracetic acid 0.20.35% and other stabilised organic acids. Spectrum Uses Advantages Disadvantages High-level disinfectant/sterilant. Used in automated endoscope reprocessors. Can be used for cold sterilisation of heatsensitive critical items, e.g., haemodialysers. Also suitable for manual instrument processing when properly formulated. Rapid sterilisation cycle time at low temperature (30-45 min. at 50-55oC). Active in presence of organic matter. Environmentallyfriendly by-products (oxygen, water, acetic acid). Corrosive to some metals. Unstable when activated. May be irritating to skin, conjunctivae and mucous membranes. December 1, 2013 Chemical disinfectants in health care 30 Agents Spectrum Hydrogen peroxide 7.5%. High-level disinfectant/sterilant. Hydrogen peroxide 7.5% and peracetic acid 0.23% High-level disinfectant/sterilant. Uses Can be used for cold sterilisation of heatsensitive critical items. Requires 30 minutes at 20oC. For disinfecting haemodialysers. Advantages No activation. No odour. Environmentallyfriendly by-products (oxygen, water). Fast-acting (high-level disinfection in 15 min.). No activation required. No odour. Disadvantages Not compatible with brass, copper, zinc, nickel/silver plating. December 1, 2013 Chemical disinfectants in health care Not compatible with brass, copper, zinc, and lead. Potential for eye and skin damage. 31 Agents Phenolics Spectrum Uses Low- to intermediatelevel disinfectant. Has been used for decontaminating environmental surfaces and noncritical items. Concerns with toxicity and narrow spectrum of microbicidal activity. Advantages Not inactivated by organic matter. Disadvantages Leaves residual film on surfaces. Harmful to the environment. No activity against viruses. Not recommended for use in nurseries and food contact surfaces. December 1, 2013 Chemical disinfectants in health care 32 Agents Iodophores (30-50 ppm free iodine) Quaternary ammonium compounds Spectrum Uses Low-level disinfectant. Used on some noncritical items, e.g., hydrotherapy tanks; however, main use is as an antiseptic. Low-level disinfectant Used mainly on unless combined with environmental other agents. surfaces. Can be used on skin. Advantages Relatively free of toxicity or irritancy. Stable with good detergent properties (cationic detergent). Usually non-irritating. Disadvantages Inactivated by organic matter. Adversely affects silicone tubing. May stain some fabrics. Relatively narrow microbicidal spectrum, but range of activity can be expanded when combined with other agents, e.g., alcohols. December 1, 2013 Chemical disinfectants in health care 33 • Develop a policy for chemical disinfection • Disinfectants may be supplied ready to use or may need to be diluted • Label bottles or containers with the name and concentration of disinfectant and, for diluted disinfectants, the date of dilution/preparation • Prepare dilutions with clean water • Prepare small amounts at a time to avoid wastage December 1, 2013 Practical Tips - 1 34 • Do not mix freshly made diluted solution with old solution • Wash and dry the container before filling with new solution • Clean, rinse and dry items thoroughly before disinfecting • After disinfection, rinse thoroughly with clean water to remove all chemical residues • Alcohol solutions can be allowed to dry without rinsing December 1, 2013 Practical Tips - 2 35 • Requires direct contact of an item with steam at a required temperature and pressure for a specified time • Most reliable • Non-toxic • Has broad-spectrum microbiocidal activity • Good penetrating ability • Cheap and easy to monitor for efficacy • 2 main types: gravity and pre-vacuum December 1, 2013 Steam Sterilisation 36 • Steam introduced to purge out air and build pressure • Raise temperature normally to 121°C at 15 pounds/square inch and maintain it for 15-45 minutes • For sterilising liquids and items in wraps that steam can penetrate December 1, 2013 Gravity Displacement Autoclaves 37 • Air is first vacuumed out and then steam introduced • Faster and better penetration throughout the load • Pressure and temperature higher; 134°C at about at 30 pounds/inch2 • Processing time about three minutes • Not suited for liquids due to need for vacuum December 1, 2013 High-Vacuum Autoclaves 38 • Proper loading must occur • All items in load must have contact with steam • Items in load must be free from grease and oil December 1, 2013 Factors Influencing Steam Sterilisation 39 • A wide range of sterilisers is available • Always sterilise items for the correct time using a clock or timer • Air in the steriliser and load results in inadequate steam penetration • Never sterilise single use items December 1, 2013 Practical Tips 40 • Mixture of steam (50-80°C) and formaldehyde vapour • To process heat-resistant or heatsensitive medical devices in specialised equipment • Devices pre-cleaned and wrapped in standard material and processed in a three-hour cycle • Cannot be used for liquids • Formaldehyde must be purged/ neutralised well December 1, 2013 Low-Temperature 41 • Only to process a critical surgical item: a) in an emergency b) when accidentally contaminated, or c) when other means of sterilisation unavailable December 1, 2013 Flash Sterilisation • Never to be used for implantable items or to compensate for shortage of key instruments 42 • Require hot-air ovens • For glassware, metallic items, powders and oil/grease • Time two hours at 160°C and one hour at 180°C • Plastics, rubber, paper and cloth cannot be placed in them due to fire risk December 1, 2013 Dry Heat Sterilisation - 1 43 Advantages • Can be used for powders, anhydrous oils • Inexpensive • No corrosive effect on instruments December 1, 2013 Dry Heat Sterilisation - 2 Disadvantages • High temperature damages some items • Penetration of heat slow, uneven 44 • Colourless, flammable, explosive and toxic gas • Processing cycles overnight or longer • Parametric release is not possible December 1, 2013 Ethylene Oxide (EO) • EO and relative humidity cannot readily be measured • Spores of Bacillus atrophaeus used as biological indicators to monitor process 45 • Used for heat or moisture sensitive items • Prevents normal cellular metabolism and replication December 1, 2013 Ethylene Oxide (EO) Gas Sterilisation 46 • • • • Advantages Items not damaged by heat or moisture Not corrosive, not damaging to delicate instruments, scopes Permeates porous materials Dissipates from material • • • • Disadvantages Cost Toxic properties of ethylene oxide Aeration required Longer process December 1, 2013 EO Sterilisation 47 • Highly reactive/charged particles from hydrogen peroxide generated under vacuum • Can be used to sterilise heat- and moisture-sensitive items December 1, 2013 Hydrogen Peroxide Gas Plasma • Some plastics, electrical/electronic devices, and corrosion-susceptible metal alloys • Not compatible with cellulose (linen, paper), devices with dead-end lumens, powders and liquids • Special wrapping required 48 • For rooms contaminated with some pathogens • Such as MRSA and Clostridium difficile • Release of hydrogen peroxide, chlorine dioxide gas or possibly ozone in sealed rooms • Spore strips (biological indicators) placed strategically to monitor process • Special equipment required • Risk of damage to sensitive items December 1, 2013 Fumigation 49 • Semi-critical items can be pasteurised • 65-77°C, 30 min • Example: respiratory therapy equipment December 1, 2013 Pasteurisation and Boiling • Must be retrieved carefully for safe transport and storage 50 • Removal of microbes from air or heat-sensitive liquids • Disinfectant-impregnated filters may inactivate trapped microorganisms • Example: High-efficiency particulate air (HEPA) filters • All filters must be checked for integrity and replaced as necessary December 1, 2013 Filtration 51 • Alternative to manual reprocessing of heat-sensitive devices • Minimise exposure of staff to pathogens and disinfectants • Require access to reliable electric and water supplies, specific chemicals, regular maintenance • Biofilm build-up must be avoided December 1, 2013 Automated Endoscope Reprocessors 52 • UV lamps useful for chemical-free disinfection of air and water and also possibly for decontamination of environmental surfaces • Broad-spectrum microbicidal action • Require regular cleaning and periodic replacement December 1, 2013 Ultraviolet (UV) Light 53 • Heating from rapid rotation of water molecules • Limited use except for disinfecting soft contact lenses and urinary catheters for intermittent selfcatheterisation • May be used in emergencies to treat water for drinking or to ‘disinfect’ small water-immersible plastic or glass items December 1, 2013 Microwaves 54 Recommended practices state that both biological and chemical indicators shall be used to monitor the sterilisation process December 1, 2013 Sterilisation Process Monitoring • Mechanical monitoring • Chemical monitoring • Biological monitoring 55 • External Chemical Indicator • process indicator - autoclave tape • distinguishes processed from unprocessed medical devices • secures pack • labels pack December 1, 2013 Chemical Indicators • Check external indicator to ensure it has changed color before using any package • If the indicator did not change, do not use 56 • Requires routine monitoring daily • Test must be dated and labeled • Once removed from the steriliser the test pack opened, BI labeled, crushed and incubated in the incubator • Records of time, date of incubation and staff initials is required and then time and date and initials of the staff reading the final BI result December 1, 2013 Biological Indicators 57 • Steam Geobacillus stearothermophilus • Dry heat B.atrophaeus (formerly B.subtilis) • EO B.atrophaeus • New low temperature sterilisation technologies December 1, 2013 Biological Monitoring • Plasma sterilisation (Sterrad) B.atrophaeus • Peracetic acid - Geobacillus stearothermophilus 58 • Development of reprocessing protocols for instruments and equipment based on generally recognised standards and manufacturer's recommendations • Use of clean water for cleaning items thoroughly • Maintenance, use, and monitoring of equipment, e.g., autoclaves • Discarding items that cannot be cleaned or reprocessed adequately • Storing reprocessed items away from potential sources of contamination December 1, 2013 Main IP&C priorities 59 • Guidelines for Environmental Infection Control in HealthCare Facilities. MMWR 2003; 52(RR10):1-42. http://www.cdc.gov/hicpac/pdf/guidelines/eic_in_HCF_0 3.pdf • Ontario Ministry of Health & Long-Term Care. Provincial Infectious Diseases Advisory Committee (PIDAC) Best Practices for Cleaning, Disinfection and Sterilization in All Health Care Settings, 2010. http://www.publichealthontario.ca/en/BrowseByTopic/In fectiousDiseases/PIDAC/Pages/PIDAC_Documents.aspx December 1, 2013 References - 1 60 • Rutala WA, Weber DJ. Guideline for Disinfection and Sterilization in Healthcare Facilities, 2008. Centers for Disease Control and Prevention, Atlanta, GA. http://www.cdc.gov/hicpac/pdf/guidelines/Disinfection_ Nov_2008.pdf • Snyder, OP. Calibrating thermometers in boiling water: Boiling Point / Atmospheric Pressure / Altitude Tables. http://www.hi-tm.com/Documents/Calib-boil.html • Sattar A. Allen Denver Russell Memorial Lecture, 2006. The use of microbicides in infection control: a critical look at safety, testing and applications. J Appl Microbiol 2006; 101:743-753. December 1, 2013 References - 2 61 1. Decontamination results in an item that is safe for patient reuse. True/False. 2. Disinfection: a. b. c. d. Is used for items that will contact intact skin Involves chemical agents Reduces the numbers of microorganisms All of the above December 1, 2013 Quiz 3. The most reliable means of sterilisation is: a. b. c. d. Ethylene oxide Steam Dry heat Plasma 62 • IFIC’s mission is to facilitate international networking in order to improve the prevention and control of healthcare associated infections worldwide. It is an umbrella organisation of societies and associations of healthcare professionals in infection control and related fields across the globe . • The goal of IFIC is to minimise the risk of infection within healthcare settings through development of a network of infection control organisations for communication, consensus building, education and sharing expertise. • For more information go to http://theific.org/ December 1, 2013 International Federation of Infection Control 63