Hematology Physiology Erythropoiesis
advertisement

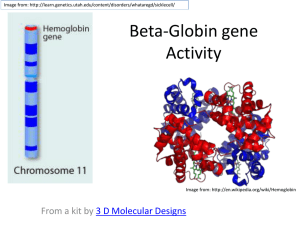
Hematology Physiology 1 Erythropoiesis Brenda Beckett, PA-C Terms to Understand Hematopoiesis Erythropoiesis Pluripotent hematopoietic stem cell (PHSC) Committed stem cell (progenitor cell) Differentiation Maturation Self-renewal Proliferation Reticulocyte Polychromasia Normocyte Erythropoietin Adult hemoglobin Fetal hemoglobin Apotransferrin Transferrin Apoferritin Terms, continued Ferritin Hemosiderin Serum iron Total iron binding capacity -thalassemia -thalassemia Hemoglobinopathy Anemia Porphyria A,B,O,Rh blood types Red Blood Cell Transports hemoglobin Carries oxygen from lungs to tissues Carries CO2 back to lungs Biconcave disc – Able to change shape – Has excess membrane Red Blood Cell Mature RBC has no nucleus 5,200,000 (males), 4,700,000 (females) per cubic milliliter Lifespan of 100-120 days Derived from pleuripotent hematopoietic stem cells (PHSC) PHSC Retained in bone marrow Reproduction controlled by growth inducers Differentiation controlled by differentiation inducers – Will become committed stem cell (progenitor cell) Erythropoiesis Decreased O2 in tissues causes increased production of erythropoietin – Hormone – Formed in kidney (80-90%) and liver Occurs in fetal liver and spleen, then shifts to fetal bone marrow Occurs in axial skeleton and proximal end of long bones in adults Reticulocytes Final cell produced in marrow before release Basophilic remnants of endoplasmic reticulum remain, becomes mature RBC (normocyte) within one day Normally ~1% of total RBCs Reticulocyte Count Can differentiate between anemias due to decreased production and those of increased destruction Will see polychromasia on Wright’s stain, need to order separate test for reticulocyte count Hemoglobin Formation Begins at proerythroblast stage, continues until reticulocyte (before leaving bone marrow) Heme molecule combines with globin (long peptide chain) to form hemoglobin chain. 4 chains bind together to form hemoglobin molecule. Hemoglobin Binds loosely and reversibly with O2 Oxygen atom binds loosely with iron atom in hemoglobin Bound as O2, released as dissolved O2 Iron Metabolism Iron important part of hemoglobin, myoglobin and other structures – ~65% of total iron in hemoglobin – 4% myoglobin – 1% various heme compounds – 0.1% in plasma combined with transferrin – 15-30% stored in liver as ferritin Iron Transportation & Storage Absorbed in small intestine Binds with apotransferrin (globulin) to form transferrin – loosely bound Excess deposited in liver and bone marrow In liver, combines with apoferritin to form ferritin. Also stored as insoluble hemosiderin – iron overload Iron Usage If plasma iron low, iron removed from ferritin, transported as transferrin in plasma Transferrin binds strongly with cell membranes on erythroblasts in marrow Ingested, delivered to mitochondria Heme synthesized Globin chains 4 globin chains combine with heme to make hemoglobin molecule 95-97% of adult hgb has 2 -chains and 2 -chains (22) aka Hgb A Fetal hgb (Hgb F) has 22. High O2 affinity, mostly changes to HgbA by birth Hgb A2 (22), 3-5% of adult Abnormal Hemoglobins Hemoglobinopathies: hemoglobin chains are abnormal Thalassemias: hemoglobin chains normal in structure but decreased or absent. Named for which chain is affected. Genes are on chromosomes 11 & 16 Anemia Qualitative or quantitative deficiency of hemoglobin – Significant blood loss • Plasma replaced in 1-3 days • RBCs replaced in 3-4 weeks – Hemolysis – Deficient RBC production Vitamin B12/Folate Important for final maturation of RBCs Essential to synthesize DNA Decrease in either leads to failure of nuclear maturation and division RBCs also become larger, irregular shape, flimsy membrane Carry O2 normally, have short lifespan Vitamin B12/Folate Deficiency Macrocytic or megaloblastic anemia Pernicious anemia: inability to absorb Vitamin B12 from GI tract Gastric mucosa secretes Intrinsic Factor (IF), combines with B12, available for absorption B12 stored in liver and bone marrow Iron deficiency When iron stores are depleted, stored iron is mobilized When iron stores drop, hemoglobin synthesis is affected – iron deficient erythropoiesis. (hypochromic) More severe, leads to decreased erythropoiesis, smaller cells (microcytic) Iron Deficiency Anemia Low iron stores = low Ferritin Low circulating iron (transferrin) = low Serum Iron Leads to increased Total Iron Binding Capacity (TIBC) Hypochromic, microcytic anemia Anemia of Chronic Disease Most likely due to inflammation Iron stores aren’t released Decreased erythropoiesis Upregulation of WBC production causes decreased erythropoiesis Normocytic or microcytic Hemolytic anemias RBCs are fragile, shorter lifespan Rupture as pass through capillaries and spleen Hereditary or acquired (immune mediated) Increased destruction leads to increased bilirubin (jaundice) Hemolytic anemias Hereditary spherocytosis (and others) – Cells are spherical, can’t withstand compression – easily ruptured Sickle cell anemia – Abnormal Hgb S (on chain) – Exposed to low O2, forms crystals, elongates cell – “sickle” – Sickle trait – protective against malaria Thalassemias Autosomal recessive, Mediterranean Reduced synthesis of one globin chain, leads to microcytic anemia or chain affected Can coexist with hemoglobinopathies Carrier state can be protective against malaria G6PD Deficiency Hereditary Low levels of G6PD (enzyme) Certain triggers lead to hemolysis, anemia, jaundice Foods, medications, infection Protective against malaria Polycythemia Increased number of RBCs – primary or secondary High altitude – physiologic polycythemia Cardiac failure, smoking, tumors Polycythemia vera: blast cells continue to produce RBCs even though there are too many in circulation. Viscous blood. Treatment: phlebotomy Porphyria Inherited or acquired Disorder of enzymes in heme pathway 7 different types Different combos of elevated porphyrins (heme precursors) in tissues – Excreted in urine and stool Sx: photosensitivity, abd pain, port wine urine, muscle weakness, behavior changes RBC/Hemoglobin destruction Changes to plasma membranes as cell ages Recognized by phagocytes Phagocytosis in spleen Heme broken down into iron & biliverdin – Biliverdin converted to bilirubin – Iron bound to transferrin Effects of anemia Lack of oxygen in tissues Symptoms can be vague – Weakness, fatigue, malaise – Dyspnea – Pallor Increased cardiac output: plapitations, heart failure Blood Groups ABO A&B antigens: “agglutinogens” on RBC Anti-A &/or Anti-B develop in absence of antigens Will agglutinate RBCs, lyse, leads to renal failure, death Rh Typing Other antigens can be present on RBCs Antibodies develop if exposed to antigen D (Rh), d, C, c, E, e Erythroblastosis fetalis WBC The overall concentration of white blood cells of all types in the blood, expressed as thousands of cells per cubic millimeter (mm3) of blood. The terms used to describe a decreased and an increased WBC are leukopenia and leukocytosis, respectively. RBC The concentration of erythrocytes in the blood, most commonly expressed as millions of cells per cubic millimeter (mm3). The terms describing a decreased and an increased RBC are erythrocytopenia and erythrocytosis, respectively, or, more commonly, anemia and polycythemia. HGB/HCT The overall concentration of hemoglobin in the blood, expressed as grams of hemoglobin per 100 milliliters of blood. The hematocrit, the percentage of the blood volume consisting of red cells, expressed as a percent (%). MCV mean corpuscular volume, the average volume of individual erythrocytes in a blood sample, expressed as femtoliters (fl) per cell. One femtoliter is the equivalent of 10-15 liters. The terms used to describe an erythrocyte with a normal, decreased, or increased cell volume are normocyte, microcyte, and macrocyte, respectively. MCHC mean cell hemoglobin concentration, the average concentration of hemoglobin within erythrocytes, expressed as grams of hemoglobin per dL of cells. Because the intracellular hemoglobin concentration determines the density of color (suffix chromia) of erythrocytes on a stained blood smear, the morphological descriptions associated with a normal, increased or decreased MCHC are normochromia, hyperchromia and hypochromia, respectively. MCH mean cell hemoglobin, the average quantity of hemoglobin in individual erythrocytes, expressed as picograms (pg) per cell. One picogram is the equivalent of 10-12 grams. RDW red cell distribution width, expressed as the coefficient of variation around the mean cell volume (MCV). The larger the value for RDW, the greater the variability in size within the erythrocyte population. The morphological correlate of an increased RDW is variation in the diameters of individual erythrocytes seen on the peripheral smear, or anisocytosis. PLT/MPV the concentration of platelets in the peripheral blood, expressed as thousands of platelets per cubic millimeter (mm3) of blood. mean platelet volume, the average volume of individual platelets, expressed as cubic microns per platelet or as femtoliters per platelet. RETIC the reticulocyte percentage, or the percentage of immature erythrocytes in a peripheral blood sample. These immature cells usually constitute from 0.5 to 1.5% of the circulating red blood cell population. An absolute reticulocyte count, expressed as millions of cells per cubic millimeter (mm3), can be obtained by multiplying the RBC by the reticulocyte percentage.