GAMETOGENESIS
OVARIAN & UTERINE CYCLES
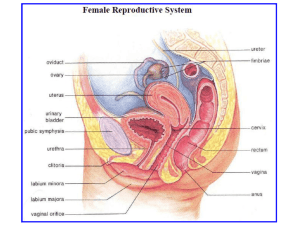
ANATOMY
DEPARTMENT
OBJECTIVES
• At the end of the lecture, the students should
be able to :
•
•
•
•
•
•
•
Describe the process of gametogenesis.
List the importance of meiosis.
List the stages of spermatogenesis.
List stages of oogenesis.
Compare between the 2 gametes.
Describe the ovarian cycle.
Describe the uterine cycle.
PROCESS OF GAMETOGENESIS
• It is the process of
conversion of immature germ
cells (spermatogonium or
oogonium), into mature
gametes (sperm or oocyte).
• This maturation is called
spermatogenesis in males
and oogenesis in females.
• During gametogenesis, a
special type of cell division
(meiosis) occurs, in which the
number of chromosomes is
reduced from diploid to
haploid number.
• It prepares gametes for
fertilization.
MEIOSIS
• It is the cell division that
takes place in the germ
cells only to produce male
and female gametes.
• It consists of two cell
divisions :
• meiosis I during which the
chromosome number of the
germ cells is reduced to half
(23), the Haploid number
(with double chromatid
chromosoes).
• Meiosis II during which the
haploid number (23) is
retained (with single
chromatid chromosome).
Segregation of
chromosomes
• (1) Reduces the chromosome
number from the Diploid to
Haploid.
• (2)Allows random movement
of maternal and paternal
chromosomes between the
gametes (Segregation)
• (3)Allows Crossing Over of
chromosome segments.
• (4)It enhances genetic
variability through cross over
and segregation (separation or
disjunction of paired
homologous chromosomes).
Spermatogenesis
• It is a conversion of
primitive germ cell
spermatogonium into
mature germ cell sperm.
• It begins at puberty and
continues into old age.
• It occurs in the
seminiferous tubules of
testes.
• After several mitotic
divisions, spermatogonia
increase in number and
grow into primary
spermatocytes
(46 chromosomes).
Spermatogenesis
• Each primary spermatocyte
undergoes a reduction
division- 1st meiotic
division to form 2 haploid
secondary spermatocytes.
• Secondary spermatocytes
undergo 2nd meiotic
division to form 4 haploid
spermatids (half size).
• Spermatids are
transformed into 4 mature
sperms by a process called
spermiogenesis.
Spermiogenesis
• It is the last phase of
spermatogenesis.
• The rounded spermatid is
transformed into elongated
sperm.
• Note the loss of cytoplasm,
development of the tail,
and formation of
acrosome, which is derived
from Golgi region of
spermatid.
• Acrosome contains
enzymes that are released at
the biginning of fertilization to
help sperm in penetrating
corona radiata & zona
pellucida surrounding
secondary oocyte.
• Spermatogenesis
including
spermiogenesis requires
about 2 months for
completion.
• It takes place in the
Seminiferous Tubules.
• The sperms are stored
and become functionally
mature in the
Epiddidymis.
The mature sperm
Mature sperm
Secondary oocyte
(Mature female gamete)
• It is a free-swimming actively motile cell,
consisting of a head, neck and a tail.
• The head, composed mostly of haploid
nucleus.
• The nucleus is partly covered by a
caplike acrosome, an organelle
containing enzymes to help sperm in
penetrating corona radiata & zona
pellucida of secondary oocyte during
fertilization.
• The tail of sperm consists of
3 segments : middle, principal &
end pieces. it provides motility of sperm
to the site of fertilization.
• The middle piece of the tail contains
mitochondria, providing adenosine
triphosphate (ATP) necessary for
activity.
Oogenesis
• It is a maturation of the germ
cells (oogonia) into mature
secondary oocytes.
• It occurs in the ovary, which
contains a large number of
oogonia that differentiate
into primary oocytes.
• It begins before birth
(in early fetal life) and is
completed after puberty and
continues to menopause.
• No oogonia are found in
ovary after birth because
they differentiate into
primary oocytes before
birth.
Oogenesis : Prenatal maturation of
Oocytes
• During early fetal life :
Oogonia proliferate by
mitosis to form daughter
oogonia, they enlarge and
grow to form primary
oocytes before birth
(each contains 46 ch.).
• A Single layer of flattened
follicular epithelial cells
from the cotex of ovary
surrounds the primary
oocyte, forming primitive or
primordial ovarian follicles
containing primary oocytes
(A)
• At birth all primary oocyte
(46 ch) remain arrested
and do not finish their
1st meiotic division until
puberty.
Oogenesis
During puberty, follicular
epithelial cells become
cuboidal then columnar
and the primary oocyte
becomes surrounded by
zona pellucida (acellular
glycoprotein material)
forming growing follicle
(B).
Then, Primary oocyte
has several layers of
follicular cells +
Z.P.membrane, forming
the primary follicle (C).
Oogenesis
At puberty : cavities appear between
the follicular cells, then join together
forming a single large cavity called
(Antrum) filled with a watery fluid
(liquor folliculi).
The follicular cells differentiated into :
Stratum granulosum, forming the wall of
follicle.
Cumulus oophorus : cells surrounding
the ovum (primary oocyte).
Theca folliculi differentiated into :
Graafian Follicle
theca externa : outer fibrous &
theca interna : inner vascular and cellular
layer.
At this stage the growing primary
follicle changed into mature
secondary follicle or Graafian follicle.
• Shortly before ovulation :
Primary Oocyte completes
first meiotic division :
• the Secondary Oocyte
(23 ch) receives almost all
the cytoplasm.
• The First Polar Body
receives very little.
• It is small nonfunctional
cell and soon degenerates.
At puberty /Before
ovulation
At ovulation
• At ovulation : the
nucleus of the
secondary oocyte
begins the second
meiotic division,
leading to :
• The secondary oocyte (23)
• The 2nd polar body.
• If the secondary oocyte
is fertilized by a sperm,
the second meiotic
division is completed
otherwise it degenerates
24 hours after ovulation.
• Most of the cytoplasm is
retained by the Mature
Oocyte (Fertilized
Oocyte).
• The rest is in the 2nd
Polar Body which soon
degenerats.
• Has a covering of
a morphous
material (Zona
Pellucida) and a
layer of follicular
cells (Corona
Radiata).
Comparison of Gametes
•
•
•
•
Sperm
It is highly motile.
It contains little cytoplasm.
It is not surrounded by Z.P & C.R.
It has 2 kinds of sex
chromosomes : 23,x and 23,y /
so the difference in sex
chromosome complement of
sperms forms the basis of
primary sex determination.
Secondary oocyte
It is immotile.
It has an abundance of cytoplasm.
It is surrounded by Z.P and a layer
of follicular cells-the C.R.
It has only one kind of sex
chromosome : 23,x
Oogenesis: postnatal maturation of Oocytes
At puberty
At ovulation
• No primary oocytes form after birth in
females, in contrast to continuous
production of primary spermatocytes
in males.
• Primary oocytes are formed in the
ovaries in early fetal life and remain
dormant in ovarian follicles until
puberty.
• At puberty,as a follicle matures, each
primary oocyte divides by 1st meiotic
division into one large secondary
oocyte (contains haploid chr.) and
one small non-functional cell- first
polar body (degenerates ,contains
haploid chr.).
• At ovulation, secondary oocyte
begins 2nd meiotic division, which is
completed after fertilization, giving
one ovum or fertilized oocyte + one
small nonfuctional cell- second polar
body , each one having haploid chr.
Female reproductive cycles
• Commencing at puberty and normally continuing
throughout the reproductive years.
• Involving activity of :
• Hypothalamus.
• Hypophysis.
• Ovaries.
• Uterus.
• Uterine tubes.
• Vagina.
• Mammary glands.
Female reproductive cycles
• Gonadotropine releasing hormone by hypothalamus
(GnRH) stimulates the release of :
• Follicle stimulating hormone (FSH);
• Stimulates development of ovarian follicles.
• Production of estrogen by follicular cells.
• Lutinizing hormone (LH);
• Trigger for ovulation (secondary oocyte)
• Stimulate production of progesterone by follicular cells
and corpus luteum.
• These hormones induce growth of endometrium.
Ovarian
cycle
•FSH and LH produce cyclic changes in the ovaries-the ovarian cycle
(development of follicles, ovulation, and corpus luteum formation).
Ovarian
cycle
changes in the ovaries.
• (FSH) and (LH) produce cyclic
• Follicular development, with the
resulting growth and proliferation of
follicular cells, formation of zona pellucida,
and development of theca folliculi.
• Subsequent estrogen production,
necessary for reproductive organs
development and function.
• Ovulation; occurs at mid menstrual cycle,
stimulated by increase of (LH) production,
and high estrogen level.
• Expulsion of the secondary oocyte,
surrounded by zona pellucida, and corona
radiata,
• Corpus luteum; the wall of ovarian follicle
after expulsion of the secondary oocyte
and develop under influence of (LH).
• It is of two types : corpus luteum of
pregnancy and corpus luteum of
menstruation (corpus albicans).
Ovarian cycle
Ovarian cycle
• Monthly series of events associated with the
maturation of an egg.
• Follicular phase – period of follicle growth (days
1–14).
• Ovulation occurs midcycle.
• Luteal phase – period of corpus luteum activity
(days 14–28).
Menstrual cycle
• It is the cyclic changes in the endometrium
(every 28 days) under fluctuating effect of
gonadotropic, ovarian follicle and corpus
luteum hormones (estrogen and
progesterone).
• It is the peroid during which the oocyte
matures, ovulated, and enters the
uterine tube.
Menstrual cycle
• Phases of the menstrual cycle :
• Menstrual phase; the functional layer of
the uterine wall is sloughed, discarded
with the menstrual flow, it lasts about 4-5
days.
• The endometrium is thin.
Menstrual cycle
• Proliferative phase :(follicular estrogenic),
coincides with growth of the ovarian follicle
and controlled by estrogen.
• It lasts about 9 days.
• Increase thickness of endometrium.
Menstrual cycle
• Luteal phase; (secretory progesterone),
coincides with formation, function, and growth of
corpus luteum,
• It lasts about 13 days.
• increase endometrial thickness under influence
of progesterone and estrogen of corpus luteum.
Menstrual cycle
• If fertilization occurs;
• corpus luteum under influence of hCG
continues to secrets estrogen and progesterone,
the luteal phase persists and
menstruation does not occur.
• The endometrium passes into the pregnancy
phase.
• If fertilization dose not occur; corpus
luteum degenerates, with fall of estrogen and
progesterone level, menstruation occurs.
Menstrual cycle
• Ischemic phase; due to hormonal
withdrawal as a result of non fertilization of
the oocyte,
• Shrinkage of the endometrium, with
patchy ischemic necrosis, resulting in
bleeding in the uterine cavity.
• The cycle is repeated.
THANK YOU