Mammary Gland
Petek Korkusuz MD PhD
Learning Goals
• To learn the development, histology
and function of mammary glands
Development of Mammary Glands
•
Are a modified and highly
specialized type of apocrine
sweat glands.
•
Consist of parenchyma, which is
formed from ducts, and connective
tissue stroma.
Parenchyma derives embryonically
from surface ectoderm; stroma
arises from surrounding
mesenchyme.
•
•
•
Mammary buds begin to
develop during the sixth week
as solid downgrowths of the
epidermis into the underlying
mesenchyme
These changes occur in
response to an inductive
influence from the
mesenchyme.
Development of Mammary Glands
•
Mammary buds develop as
downgrowths from thickened mammary
crests, which are thickened strips of
ectoderm extending from the axillary to
the inguinal regions
•
The mammary crests (ridges)
appear during the fourth week but
normally persist in humans only in
the pectoral area, where the
breasts develop
Each primary bud gives rise to
several secondary mammary buds
that develop into lactiferous ducts
and their branches
Canalization of these buds is
induced by placental sex hormones
entering the fetal circulation. This
process continues until late
gestation, and by term, 15 to 19
lactiferous ducts are formed.
The fibrous connective tissue and
fat of the mammary gland develop
from the surrounding mesenchyme.
•
•
•
Development of Mammary Glands
•
A, Ventral view of an embryo of approximately 28 days showing the mammary
crests. B, Similar view at 6 weeks showing the remains of these crests. C,
Transverse section of a mammary crest at the site of a developing mammary
gland. D to F, Similar sections showing successive stages of breast development
between the 12th week and birth.
Development of Nipples and Areola
•
•
•
•
During the late fetal period, the epidermis at the site of origin of the
mammary gland becomes depressed, forming a shallow mammary pit
The nipples are poorly formed and depressed in newborn infants.
Soon after birth, the nipples usually rise from the mammary pits
because of proliferation of the surrounding connective tissue of the
areola, the circular area of skin around the nipple.
The smooth muscle fibers of the nipple and areola differentiate from
surrounding mesenchymal cells.
Postnatal Development of Female
Breast.
•
•
A, Newborn. B, Child. C, Early puberty. D, Late puberty. E, Young
adult. F, Pregnant female. Note that the nipple is inverted at birth
(A). Normally the nipple elevates during childhood. Failure of this
process to occur gives rise to an inverted nipple. At puberty (12-15
years), the breasts of females enlarge because of development of the
mammary glands and the increased deposition of fat.
Postnatal Development
•
•
•
•
•
•
The rudimentary mammary glands of newborn males and females
are identical and are often enlarged.
Some secretion, often called "witch's milk," may be produced caused
by maternal hormones passing through the placental membrane into
the fetal circulation.
Newborns breasts contain lactiferous ducts but no alveoli. Before
puberty, there is little branching of the ducts.
In females, the breasts enlarge rapidly during puberty, mainly because
of development of the mammary glands and the accumulation of the
fibrous stroma and fat associated with them
. Full development occurs at approximately 19-20 years
The lactiferous ducts of male breasts remain rudimentary throughout
life.
Gynecomastia
•
•
•
•
•
The rudimentary lactiferous ducts in
males normally undergo no
postnatal development.
Gynecomastia (Gr. gyne, woman +
mastos, breast) refers to the
development of the rudimentary
lactiferous ducts in the male
mammary tissue.
During midpuberty, approximately
two thirds of boys develop varying
degrees of hyperplasia of the
breasts. This subareolar hyperplasia
may persist for a few months to 2
years.
A decreased ratio of testosterone to
estradiol is found
80% of males with Klinefelter
syndrome (XXY) have
gynecomastia
Absence of Nipples (Athelia) or
Breasts (Amastia)
• Rare congenital anomalies
may occur bilaterally or
unilaterally.
• Result from failure of
development or
disappearance of the
mammary crests.
• May also result from failure
of mammary buds to form.
• More common is
hypoplasia of the breast,
often found in association
with gonadal agenesis and
Turner syndrome
Aplasia of Breast
• The breasts of a
postpubertal female often
differ in size. Marked
differences are regarded as
anomalies because both
glands are exposed to the
same hormones at puberty.
• In these cases, there is often
associated rudimentary
development of muscles of
the thoracic wall, usually the
pectoralis major
The thorax of an infant with congenital absence of the left pectoralis major
muscle. Note the absence of the anterior axillary fold on the left and the low
location of the left nipple. (From Behrman RE, Kliegman RM, Arvin AM [eds]: Nelson Textbook of Pediatrics,
15th ed. Philadelphia, WB Saunders, 1996.)
Supernumerary Breasts and Nipples
•
•
•
•
•
•
An extra breast (polymastia) or nipple
(polythelia) occurs in approximately 1% of
the female population as an inheritable
condition.
An extra breast or nipple usually develops
just inferior to the normal breast.
Supernumerary nipples are also relatively
common in males; often they are mistaken
for moles
Less commonly, supernumerary breasts
or nipples appear in the axillary or
abdominal regions of females developing
from extra mammary buds that develop
along the mammary crests. They become
more obvious in women when pregnancy
occurs.
Approximately one third of affected persons
have two extra nipples or breasts.
Supernumerary mammary tissue very
rarely occurs in a location other than along
the course of the mammary crests. It
probably develops from tissue that was
displaced from these crests.
A man and a female infant with extranipples (polythelia)
Inverted Nipples
• Nipples fail to elevate above the skin surface after birth,
remaining in their prenatal location (A)
• May make breast-feeding of an infant difficult;
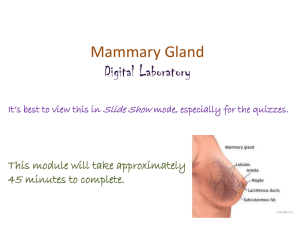
Mammary glands
• Compound tubuloalveolar glands
• Consist of 15 to 20 lobes
radiating out from the nipple
and are
• Separated from each other by
adipose and collagenous
connective tissue.
• Secrete milk, a fluid containing
proteins, lipids, and lactose as
well as lymphocytes and
monocytes, antibodies, minerals,
and fat-soluble vitamins
• Provide the proper nourishment
for the newborn.
•
•
•
•
Mammary Glands Development
Develop in the same manner and
are of the same structure in
both sexes until puberty,
At puberty changes in the
hormonal secretions in females
cause further development and
structural changes within the
glands.
Secretions of estrogen and
progesterone from the ovaries
(and later from the placenta)
and prolactin from the
acidophils of the anterior
pituitary gland initiate
development of lobules and
terminal ductules.
Full development of the ductal
portion of the breast requires
glucocorticoids and further
activation by somatotropin.
Mammary Glands Development
•
•
•
•
•
•
Concomittant with these events
is an increase in connective tissue
and adipose tissue within the
stroma, causing the gland to
enlarge.
Full development occurs at about
20 years of age
Minor cyclic changes occur during
each menstrual period,
Major changes occur during
pregnancy and in lactation.
After age 40 or so, the
secretory portions and some of
the ducts and connective tissue
elements of the breasts begin to
atrophy, and they continue this
process throughout menopause.
Gland Structure
• The glands within the breasts are
classified as compound
tubuloalveolar glands,
• Make 15 to 20 lobes radiating out
from the nipple and separated
from each other by adipose and
collagenous connective tissue.
• Each lobe is drained by its own
lactiferous duct leading directly
to the nipple, where it opens onto
its surface.
• Before reaching the nipple, each
of the ducts is dilated to form a
lactiferous sinus for milk storage
and then narrows before passing
through the nipple
Gland Structure
• Near the opening at the
nipple, lactiferous ducts are
lined by a stratified squamous
keratinized epithelium.
• The lactiferous sinus and
the lactiferous duct leading
to it are lined by stratified
cuboidal epithelium,
• Smaller ducts leading to the
lactiferous duct are lined by
a simple columnar epithelium.
• Stellate myoepithelial cells
located between the
epithelium and the basal
lamina wrap around the
developing alveoli and become
functional during pregnancy
r
o
u
s
s
i
n
u
s
a
n
d
t
h
e
l
a
c
t
i
f
e
r
o
u
s
d
u
c
t
l
e
a
d
i
n
g
t
o
i
t
a
r
e
l
Resting (Non secreting) Mammary
Gland
• Alveoli are not developed in nonpregnant
women
• nonpregnant women have the same basic
architecture as the lactating (active)
mammary gland, except that they are
smaller and without developed alveoli,
which occur only during pregnancy..
Lactating (Active) Mammary Glands
•
•
•
•
•
are activated by elevated surges of estrogen and progesterone
during pregnancy to become lactating glands to provide milk for
the newborn.
Terminal portions of the ducts branch and grow and the alveoli
develop and mature
As pregnancy progresses, the breasts enlarge as a result of
hypertrophy of the glandular parenchyma and engorgement with
colostrum,
Colostrum is a protein-rich fluid, in preparation for the newborn.
Within a few days after birth, when estrogen and progesterone
secretions have subsided, prolactin, secreted by acidophils of the
anterior pituitary gland, activates the secretion of milk, which
replaces the colostrum
Lactating (Active) Mammary
Glands
• During pregnancy, the
terminal portions of
the ducts branch and
grow and develop
secretory units known
as alveoli.
• Inset shows a
longitudinal section of
a gland and duct of
the active mammary
gland.
Alveoles and Alveolar Cells
•
•
•
Electron micrograph of an acinar cell
The alveoli are composed of
cuboidal cells partially
surrounded by a meshwork of
myoepithelial cells.
These secretory cells possess
abundant RER and mitochondria,
several Golgi complexes, many
lipid droplets, and numerous
vesicles containing caseins (milk
proteins) and lactose.
Not all regions of the alveolus
are in the same stage of
production, because different
acini display varying degrees of
preparation for synthesis of
milk substances
Milk Secretion from Alveolar Cells
• The secretions of the alveolar cells are of two kinds: lipids
and proteins.
• Stored as droplets within the cytoplasm.
• Released from the secretory cells by the apocrine mode of
exocytosis,
• Small droplets coalesce to form larger and larger droplets
that move to the periphery of the cell.
• Once there, they project as cytoplasmic blebs into the
lumen; eventually, the lipid droplets containing blebs are
pinched off and become part of the secretory product.
• Each bleb consists of a central lipid droplet surrounded by a
narrow rim of cytoplasm and enclosed by a plasmalemma.
• Proteins synthesized within these secretory cells are
liberated from the cells by the merocrine mode of
exocytosis in much the same manner as would be expected
of other cells that synthesize and release proteins into the
extracellular space
Areola and Nipple
•
•
•
•
•
The circular, heavily pigmented
skin in the center of the breast is
the areola.
Areola contains sweat glands and
sebaceous glands at its margin as
well as areolar glands (of
Montgomery) that resemble both
sweat and mammary glands.
In the center of the areola is the
nipple, a protuberance covered by
stratified squamous epithelium
containing the terminal openings of
the lactiferous ducts.
In fair-skinned individuals, a
pinkish color is imparted to the
nipple as a result of the color of
blood in the rich vascular supply
within the long dermal papillae that
extend near its surface.
During pregnancy, the color
becomes darker because of
increased pigmentation of the
areola and the nipple.
Areola and Nipple
•
•
•
•
•
The core of the nipple is
composed of dense collagenous
connective tissue with abundant
elastic fibers connected to the
surrounding skin or interlaced
within the connective tissue and a
rich component of smooth muscle
cells.
The wrinkling of the skin on the
nipple results from the
attachments of the elastic
fibers.
The abundant smooth muscle
fibers are arranged in two ways:
circularly around the nipple and
radiating longitudinally along the
long axis of the nipple.
The contraction of these muscle
fibers is responsible for erection
of the nipple.
Most of the sebaceous glands
located around the lactiferous
ducts open onto the surface or
sides of the nipple, although some
open into the lactiferous ducts
just before those ducts open
onto the surface.
Mammary Gland Secretion: Milk
Production
•
•
•
•
•
•
•
•
Prolactin is responsible for the production of milk
Oxytocin is responsible for the milk ejection reflex.
Although the mammary gland is prepared to secrete milk even before birth, certain
hormones prohibit this.
When the placenta is detached in the adult female, prolactin from the anterior
pituitary stimulates the production of milk, which reaches full capacity in a few days.
Before that, for the first 2 or 3 days after birth, a protein-rich thick fluid called
colostrum is secreted.
Colostrumis a high-protein secretion, rich in vitamin A, sodium, and chloride, also
contains lymphocytes and monocytes, minerals, lactalbumin, and antibodies
(immunoglobulin A) to provide nutrition and passive immunity to the newborn.
Milk, usually produced by the 4th day after parturition, is a fluid that contains
minerals, electrolytes, carbohydrates (including lactose), immunoglobulins (mostly
immunoglobulin A), proteins (including caseins), and lipids.
Production of milk results from the stimuli of sight, touch, handling of the newborn,
and anticipation of nursing, events that create a surge in prolactin release.
Mammary Gland Secretion: Milk
Production
• Once initiated, milk production is continuous, with the milk
being stored within the duct system.
• Concomitant with the production of prolactin, oxytocin is
released from the posterior lobe of the pituitary.
• Oxytocin initiates the milk ejection reflex by inducing
contractions of the myoepithelial cells around the alveoli
and the ducts, thus expelling the milk.
• Mothers who cannot breast-feed their infants on a regular
feeding schedule are inclined to suffer from poor lactation.
This may motivate a decision to discontinue nursing
altogether, with the result that the infant is deprived of
the passive immunity conferred by ingesting antibodies
from the mother.
Breast cancer
•
•
•
•
•
•
•
Seen second to lung cancer as one of the major causes of cancerrelated death in women,
may be of two different types: ductal carcinoma of the ductal
cells and lobular carcinoma of the terminal ductules.
Detection must be early, or the prognosis is poor because the
carcinoma may metastasize to the axillary lymph nodes and from
there to the lungs, bone, and brain.
At the recommendation of the medical profession, early detection
through self-examination and mammography has helped to reduce
breast cancer mortality rates.
In 2005, approximately 270,000 women and 1700 men were
diagnosed with breast cancer in the United States and
approximately 40,000 women and 500 men died of breast cancer.
There is an inverse relationship between the age of the woman and
her risk of contracting the disease, in that in 2005 1 out of 2200
women less than 30 years of age contracted breast cancer,
whereas 1 out 54 and 1 out of 23 women less than 50 and 60 years
of age, respectively, contracted breast cancer.
Although breast cancer is more likely to occur at an older age,
younger women tend to have more aggressive breast cancers
Summary: Mammary Glands
•
Modified and highly specialized type of apocrine sweat glands
•
Consist of parenchyma, which is formed from ducts, and connective tissue
stroma.
Parenchyma derives embryonically from surface ectoderm; stroma arises from
surrounding mesenchyme (inductive interactions).
The 6-week embryo has two ventral ridge-like thickenings of epidermis, the
mammary (milk) lines, extending from axillae to the inguinal area.
The major part of each ridge disappears almost immediately, but one pair
remains in the pectoral area and penetrates the mesenchyme.
Then, 15-25 solid epithelial cords develop from each and are later canalized to
form future lactiferous ducts.
Mesenchyme gives rise to loose connective tissue around each duct. Denser
connective tissue forms septa between them to divide the gland into lobes.
Childhood gland structure is rudimentary and alike in both sexes.
At puberty, glands in girls grow and undergo structural changes directly
influenced by ovarian hormones (estrogen and progesterone).
They are not fully formed and functional, however, until pregnancy and lactation.
In pregnancy, terminal ends of ducts develop into hollow, sac-like secretory
alveoli, which are lined by simple cuboidal epithelium.
Women who give birth have highly specialized exocrine glands that synthesize
and secrete milk. Prolactin, human placental lactogen, estrogen, and
progesterone in the presence of prolactin from the anterior pituitary result in milk
production; oxytocin from the posterior pituitary induces milk release.
•
•
•
•
•
•
•
•
•
•