File
advertisement

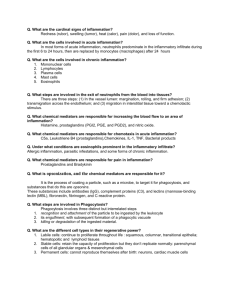
Case study 2 Inflammation, Tissue Repair, and Wound Healing Carlton, a 6-year-old boy, was playing on a sandy beach with his mother. He began to run along the shoreline when he stepped on the sharp edge of a shell, giving himself a deep cut on his foot. His mother washed his foot in the lake and put on his running shoe to take him home. One day later, Carlton’s foot looked worse. The gash was red and painful. The foot was warm to touch and appeared swollen. Carlton’s mom put some gauze over the wound and prepared to take him to the local community health clinic. 1. Describe the physiologic mechanism causing the wound to become red, hot, swollen, and painful. How is this different from the inflammatory response that might occur in an internal organ? Redness, swelling, pain, heat, and loss of function are all cardinal signs of inflammation. Acute inflammation lasts from a few minutes to several days, and is characterized by the exudation of fluid and plasma components and emigration of leukocytes, predominantly neutrophils, into the extravascular tissue. The physiologic mechanisms causing the wound changes are a result of the acute inflammatory response and the immediate vascular changes that occur, including vasodilation and increased capillary permeability; the influx of inflammatory cells such as neutrophils the effects of inflammatory mediators, which produce fever and other systemic signs and symptoms as seen in Carlton. Endothelial cells, platelets and neutrophils and Monocytes are the primary cells of inflammation. Endothelial cells produce antiplatelet and antithrombic agents that maintain vessel patency and vasodilators and vasoconstrictors that regulate blood flow. Activated platelets also release a number of potent inflammatory mediators, thereby increasing vascular permeability and altering the chemotactic, adhesive, and proteolytic properties of the endothelial cells (Porth, p. 378). Internal inflammation has systemic effects, lymph node involvement and can include inflammation of internal organs. Examples of the inflammatory responses in internal organs include inflammation of the heart (myocarditis), which may cause vague chest pain or fluid retention; inflammation of the kidneys (nephritis) may cause high blood pressure or kidney failure; inflammation of the large intestine (colitis) may cause cramps and diarrhea; inflammation of the eye (iritis or uveitis) may cause pain or decreased vision; inflammation of the muscles (polymyositis) may cause achiness or weakness; inflammation of the blood vessels (vasculitis) may cause rash, headaches, or internal organ damage; inflammation of the small tubes that transport air to the lungs (bronchiolitis) may cause shortness of breath similar to an asthma attack. (http://www.energeticnutrition.com/articles/inflammation.html) 2. Describe the immunologic events that are happening at the local level during Carlton’s acute inflammatory response. Consider the movement of leukocytes to the wound and the cells that would be particularly prevalent in this type of injury. The cells that would be particularly prevalent in this type of cell injury are the neutrophils. The neutrophils and macrophages are phagocytic leukocytes that are present in large numbers and are evident within hours at the site of inflammation. The neutrophil is the primary phagocyte that arrives early at the site of inflammation, usually within 90 minutes of injury, and is often referred to as PMN’s (polymorphonuclear neutrophils or segmented neutrophils (segs). The neutrophil count in the blood often increases greatly during an inflammatory process, especially with bacterial infections (Porth, p. 379). Neutrophils have a lifespan of only about 10 hours, and as a result, the circulating WBC count is increased, causing leukocytosis. With excessive demand for phagocytes, immature forms of neutrophils are released from the bone marrow. These immature cells are called bands. Within 24 hours, mononuclear cells arrive at the inflammatory site, and by 48 hours, monocytes and macrophages are the predominant cell types. 3. Nutrition plays an important factor in wound healing. Predict what stages of wound healing would be affected by a deficiency in vitamins A and C and explain your answers. All stages of wound healing could be affected by a deficiency in vitamins A and C. Although most vitamins are essential cofactors for the daily function of the body, vitamins A and C play an essential role in the healing process. Vitamin C is needed for collagen synthesis. In vitamin C deficiency, new wounds do not heal properly, and old wounds may fall apart. Administration of Vitamin C rapidly restores the healing process to normal. Vitamin A functions in stimulating and supporting epithelialization, capillary formation, and collagen synthesis. Vitamin A also has been shown to counteract the anti-inflammatory effects of corticosteroid drugs and can be used to reverse these effects in persons who are on chronic steroid therapy (Porth, p. 395).