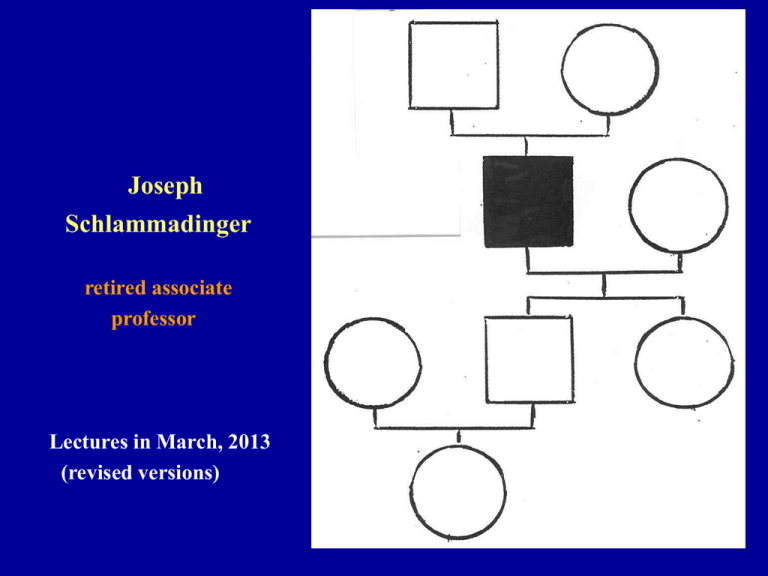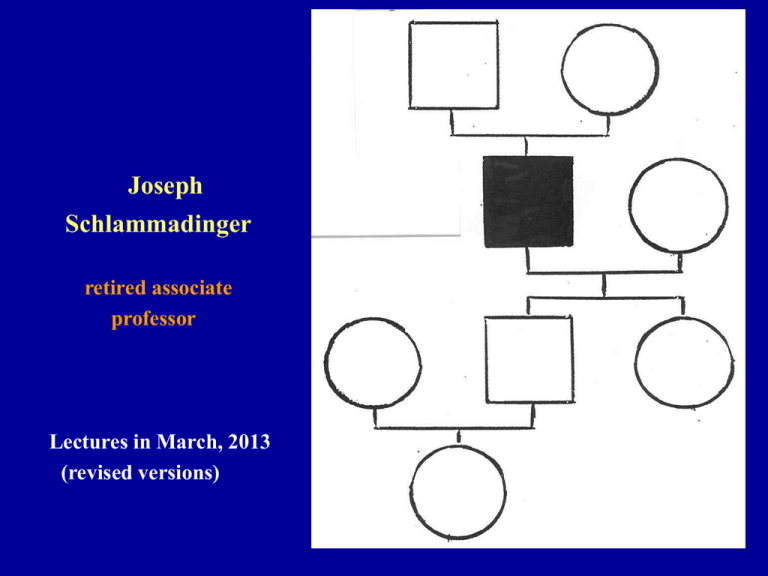
Joseph
Schlammadinger
retired associate
professor
Lectures in March, 2013
(revised versions)
Note and don’t forget, please
• Facts, their description, organization and
interpretation within one chapter of a given
science–in our case: Genetics–may be different as
taught by different lecturers, or seen in different
sources (e.g. textbook vs. lecture, and so on). The
essence, however, is the same even if different terms,
words, expressions are actually used, provided the
students understand and use them correctly.
• This formula is true to exam questions, too.
CYTOGENETICS
2013
Morphologically (microscopically) identifiable
chromosomes are seen only in eukaryotic organisms
Cytogenetics is the science of chromosomes, elements of genetics which can
be analyzed cytologically. (Better in LM than in EM.)
ONE CHROMOSOME = ONE DNA MOLECULE
The linear DNA molecule runs form one end of the chromosome (telomere)
to the other end. It is organized into chromatin (with histones and other
proteins), in a form of multiple coils. The physical length of a metaphase
chromosome is approximately 1/10,000 of the total length of the DNA
making that very chromosome.
The sequence of the genes within one DNA molecule, i.e. within a given
chromosome is determined, and is characteristic and specific to species.
(See details in genetics: linkage, linkage groups, etc., and the results of the
Human Genome Program.)
(G0)
Phases of the cell cycle:
G1, S and G2 = interphas
G1
Chromosomes are not visible
individually*.
M
S
G2
M = mitosis.
Individual chromosomes are
visible, the best in the metaphase.
* Novel methods, however, may show
(and even identify) the individual
chromosomes or part(s) of them in
interphase, too. (See FISH and next
slide.)
Arrangement
of
chromosomes
in an
interphase
nucleus.
(Computer
reconstruction in
false colours.)
MITOSIS (first half)
Metaphase
MITOSIS (second half cytokinesis)
Metaphase chromosome as seen in the electron microscope
THE NUMBER*,
SHAPE,
relative SIZE,
BANDING PATTERN
and GENE SEQUENCE (= order of loci**)
of CHROMOSOMES
is a characteristic standard for each species.
Morphological (light microscopic) features
of chromosomes of each species are
summarized in the IDEOGRAM,
most conveniently in diagrammatic
representation.
The chromosomes of a given individual
are evaluated by comparing them
to the ideogram
of the very species concerned.
Variable
stained
*Higher order eukaryotes are typically diploid organisms.
The normal (diploid) human chromosme number
is 2n = 46.
** Locus (latin) = place, location (plural: loci). In genetics:
the location of a gene in question within a specified
chromosome.
LIGHT MICROSCOPIC INVESTIGATION OF
HUMAN METAPAHSE CHROMOSOMES
I. TRADITIONAL PROCEDURE
1/ Dividing cells (predominantly: in vitro cell culture, e.g. PHA
[phytohemagglutinin] stimulated T lymphocytes).
2/ Accumulation in the metaphase: aided by colchicine treatment.
3/ Swelling in hypotonic solution (0.075 M KCl).
4/ Fixing.
5/ Spreading on specimen slides.
6/ Staining: Giemsa’s solution.
7/ Light microscope: metaphase plate.
8/ Photography.
9/ Print. Cut out images of individual chromosomes and arrange them
according to the principles of the ideogram (Denver nomenclature).
10/ The result is an ordered (arranged) karyogram. Evaluate and
11/ establish karyotype.
Some comments on terminology
English (mainly USA)
(printed photo of a) metaphase spread
European
not ordered karyogram
karyotype (in photographic presentation)
ordered karyogram
karyotype (symbols)
karyotype (symbols)
SHAPES OF CHROMOSOMES, I
A: metacentric, B: submetacentric, C: acrocentric.
1: sister chromatids, 2: centromere, 3: short arm,
4: long arm, 5: satellite, 6: secondary constriction.
A (not ordered) karyogram
Shapes of chromosomes, II
(for instance in mouse)
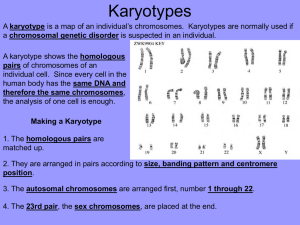
PRINCIPLES OF KARYOGRAM
ARRANGEMENTS
(diploid human cells)
The Denver system.
Order the chromosome images according size: the biggest is the first.
In the case of same size pairs the more metacentric comes first.
The homologous pairs, which are identical in both sexes,
are numbered from 1 to 22. These are called autosomes.
Sex chromosomes are denoted with X and Y. They are not homologs,
contain different genes, but in meiosis of the male
they behave as homologs in the reduction division.
Chromosomes also have been grouped: A (1-3) = big metacentrics,
B (4-5) = big submetacentrics, C (6-12) = medium size submetacentrics,
D (13-15) = big acro-centrics, E (16-18) = small submetacentrics,
F (19-20) = small metacentrics, G (21-22) = small acrocentrics.
On that basis X belongs to group C, Y to group G.
ARRANGED KARYOGRAMS
FEMALE
MALE
Description of karyotypes
with conventional symbols:
46,XX = altogether 46 chromosomes, among them two X, normal
female karyotype.
46,XY = altogether 46 chromosomes, among them one X and one
Y, normal male karyotype.
In English speaking countries (and in general: in English
publications) usually the image of a–representative, characteristic–
ordered karyogram is given as a karyotype. (The use of the term
karyogram is only occasional.)
(See further details below.)
LIGHT MICROSCOPIC INVESTIGATION OF
HUMAN METAPAHSE CHROMOSOMES
II. BANDING TECHNIQUES
1/ Dividing cells (predominantly: in vitro cell culture, e.g. T cells).
2/ Accumulation in the metaphase: aided by colchicine treatment.
3/ Swelling in hypotonic solution (0.075 M KCl).
4/ Fixing.
5/ Spreading on specimen slides. (Pretreatment for banding.)
6/ Staining: Giemsa’s solution or quinacrine (a fluorescent dye). These
give G bands and Q bands, respectively. (There are also other bands,
like C, R and T, developed by special staining procedures.)
7/ Conventional light or fluorescent microscope.
8/ Photography.
9/ Print. Cut out images of individual chromosomes and arrange them
according to the principles of the banded ideogram (Paris nomenclature).
10/ The result is an ordered (arranged) karyogram. Evaluate and
11/ describe karyotype.
Q-bands and G bands on
chromosomes,
and (Paris) ideogram
There are other banding procedures, too,
resulting in C, R and T bands, respectively.
Today the Giemsa (G) banding technique is
mostly used (G+ = dark staining, G– = light
staining). Chromosome arms are divided in
regions and these are numbered 1, 2, 3, and so
on in both p and q directions, starting from the
centromere. The bands within the regions are
numbered according to the same rule.
In quinacrine (Q) banding Q+ = intense
fluorescence, Q– = faint fluorescence. Q+ = G+,
Q– = G – .
A number of new high resolution banding
techniques have also been developed which
allow better longitudinal resolution within a
chromosome.
Human chromosome #1, standard (left) and
results of two high resolution bandings.
NUMERICAL ABERRATIONS
OF HUMAN CHROMOSOMES
NUMERICAL ABERRATIONS,
POLYPLOIDIES
triploidy (3n = 69)
tetraploidy (4n = 92)
Human numerical chromosome aberrations,
POLYPLOIDIES
All these are mentioned as euploidy, the actual chromosome numbers are
exact multiples of n, i.e. of the haploid set.
Please note. Triploidy as well as tetraploidy are lethal conditions in
humans, they result in spontaneous abortion rather than in stillbirth.
The traditional nomenclature defines these conditions, however, as
euploidy: they are exact multiples of n. (The haploid chromosome set
is represented by n. In Homo sapiens n = 23. Triploidy = 3n,
tetraploidy = 4n.) “Eu” as first syllable in some compound words
means “real”, “right”, “good”, “regular”, “self evident”, and so on.
In plants polyploidy may contribute to the development of desirable
traits in agriculture (higher yield, better resistance, and so on). The
majority of wheat (corn) sorts in production are hexaploid (6n = 42).
In that case we speak about allopolyploidy, where the three originally
diploid chromosome sets come from three different (closely related)
ancestors.
In the animal world, in vertebrates polyploidy is compatible with life–if
at all–in salamanders (amphibian); in higher order animals that is
lethal, like in humans.
Human numerical autosome aberrations
(anomalies),
aneuploidies
(Euploidy: see earlier. “an-” = privative prefix. Aneuploid = non-euploid.
The chromosome number is not exact multiple of n.)
CAUSES OF ANEUPLOIDIES
1) Nondisjunction. Homologous chromosomes or sister-chromatids fail
to separate from each other. It results in hyper- or hypohaploid
gamete, or in hyper- and/or hypodiploid somatic cells.
Occurs either in
a/ meiosis, when all the cells of the offspring are aneuploid,
or in
b/ mitosis, where it creates chromosome mosaicism, that is, in one
individual two (or more) cell types (cell lines) can be ascertained with
different chromosome numbers. (For instance 46,XX / 47,XX,+21.)
The extent and severity of the symptoms depend on the ratio of
normal / aneuploid cells, on one hand, on the other, on the tissues
(organs) involved.
2)
Delay (late arrival) of a chromosome. In the telophase of the cell
division a chromosome cannot reach the newly forming nucleus,
remains in the cytoplasm, where it will be destroyed. This
phenomenon creates monosomy, i.e. hypodiploidy. May occur in
mitosis and in meiosis as well.
>2n = hyperdiploid, <2n = hypodiploid. The latter is rare because of the
low viability of monosomic cells.
NONDISJUNCTION…
…of X chromosomes in
the first (left) or in the
second (right) female
meiotic division.
Please observe. If the first
meiotic division is
abnormal, the resulting
oocyte (mature egg cell)
contains the two X homologs. If a nondisjunction
occurs in the second
meiotic division, sister
chromatids remain
together, which results in
the presence of two
identical X chromosomes
in the egg cell (apart from
the effects of crossing
over).
MITOTIC NONDISJUNCTION
The monosomic cell is non-viable,
at least in the majority of the cases.
MOSAICISM
An individual organism (from one zygote) is composed of two (or more)
genetically different types of cells.
In this case: chromosome mosaicism, e.g. 46,XY/47,XY,+21.
CHIMERISM
An individual organism contains genetically different cells which derive from
two zygotes.
In our example: chromosomal chimerism, e.g. 46,XX/46,XY.
Possible sources of chimeras
Two egg cells fertilized by two sperm cells, and
the two zygotes form one preembryo.
Essentially the same, one cell, however, is a fertilized polocyte (fed by the fertilized egg cell).
Blue = nucleus
Dizygotic twins may exchange cells (e.g. bone
marrow stem cells) via their common placenta. Green signal = X chromosome.
Organ transplantation: 46,XY ► 46,XX.
Red signal = Y chromosome.
DOWN SYNDROME, I
What is a syndrome?
A group of symptoms and signs, which, when considered
together, characterize a disease or lesion.
It is not necessary to see all diagnostic signs in one patient,
some 3-4 very typical leading symptoms may already define a syndrome.
In this cytogenetics lecture you will see:
Down syndrome,
Pätau syndrome,
Edwards syndrome,
Turner syndrome,
Klinefelter syndrome, and
Cri du chat syndrome (cat cry disease).
You need not to learn the symptoms and signs of the syndromes listed above
(those are dealt with in detail by Clinical Genetics), but you are supposed to
mention the most important characteristic(s), one or two, in order to show that
you know what you are speaking/writing about.
Down syndrome, II
Down syndrome as trisomy 21
Karyotype: 47,XX,+21 or
47,XY,+21, that is
trisomy 21.
If the supernumerary chromosome #21
is present in all the cells of a Down
syndromic individual, we deal with
a form of meiotic origin. (See the
characteristic symptoms and signs
in the next figure.)
In the case of mosaicism (which is very
rare), the symptoms are strikingly
variable and diverse, e.g. no mental
retardation in the presence of well
visible facial signs (or vice versa),
and so on.
Symptoms and signs in Down syndrome
Increased liability to
leukemia
Increased liability to
infections
Incidence of
meiotic trisomy
21 in relation to
maternal age at
birth.
Pregnant women
above 35 are at
increased risk to
have a Down
syndromic baby,
they should be
offered a prenatal diagnosis.
(The risk of
other aneuploidies is also
higher.)
Don’t forget: the
majority (about
80%) of Down
syndromic children are born to
mothers <35
years.
Down syndrome and maternal age
Maternal age and risk of Down syndromic birth
(international statistical data)
Maternal
age
Risk of
Down
syndr.
Maternal
age
Risk of
Down
syndr.
Maternal
age
Risk of
Down
syndr.
<25
1:1500
33
1:570
42
1:65
25
1:1350
34
1:470
43
1:50
26
1:1300
35
1:380
44
1:35
27
1:1200
36
1:310
45
1:30
28
1:1100
37
1:240
46
1:20
29
1:1000
38
1:190
47
1:15
30
1:910
39
1:150
48
1:11
31
1:800
40
1:110
49
1:8
32
1:680
41
1:85
50
1:6
Do we have any means to prevent birth of Down syndromic
babies?
Yes, termination of pregnancy with a 21 trisomic embryo/fetus. Not legal in all
countries. Where permitted on the basis of medical indication, one needs
well established diagnosis.
How can a reliable diagnosis be made? By karyotyping only. Sampling for
that, however, is an invasive method.
Based on the statistical data cited above, is the maternal age >35 yr the only
indication of a prenatal diagnostics? And why 35?
The latter is a compromise. Risk of “spontaneous” abortion after sampling vs.
risk of birth of Down syndromic child. Above 35 the latter is higher.
Are there some non-invasive methods at hand indicative of Down syndromic
pregnancy, if present, in maternal age groups <35 yr?
First: in utero ultrasound investigation of the embryo.
Second: determination of biochemical markers in maternal blood, which
might be different in normal vs. Down syndromic pregnancies.
If these investigations disclose some elevated risk of the birth of a Down syndromic child, chromosome diagnosis has to be made.
Down syndrome diagnosis and screening
Assesment of risk in utero
Praenatal chromosome analysis – reliable diagnosis
(1) Chorionic villus sampling (CVS) / (2) Amniocentesis
Screening in (early) pregnancy
Ultrasound. Determination of the size of nuchal translucency (NT).
Biochemical marker investigations in maternal blood. They are non-invasive
methods (taking venous blood is generally assumed harmless). The evaluation is
statistical, if more markers are investigated, they can be indicative of the eventual
presence of a Down syndromic embryo/fetus in the maternal womb. A combination and comparison of the first and second trimester findings are evaluated.
Main biochemical markers used in screening protocols:
Alpha-fetoprotein (AFP)*
Non conjugated (unconjugated) oestriol (uE3)
Inhibin A (INH-A), a peptide hormone (of two subunits), inhibits FSH** excretion.
Pregnancy-associated plasma protein (PAPP-A)
Free and/or total human choriogonadotrophin (hCG)
* Very important in prenatal diagnostics of neural tube defects (NTD), see there.
** Follicle stimulating hormone.
◄ Sketch of amniocentesis
Fetal cells in the amniotic fluid are
obtained. (These cells as well as the
amniotic fluid are/can be subjects of
different analyses.) Traditional prenatal karyotyping only after in vitro
culture of the cells. Amniocentesis
earliest in week 16 of the pregnancy.
Plus 2-3-4 weeks in culture. Too late.
Prefer interphase cytogenetics.
Chorionic villus sampling,
sketch of CVS ►
Can be performed on week 9-10.
Delivers trophoblast cells (instead
of embryonic), they come from the
same zygote, but
higher risk of diagnostic error.
In utero ultrasound investigation:
determination of nuchal translucency
A vizsgála-tot a 10-12. (másutt: a 1113.) terhességi héten vég-zik.
Ha 3 mm- nél vasta-gabbat mérnek, az
Down szindróma gyanúját alapozza
meg, külö-nösen, ha az orrcsont
hiányával társul.
▼
▲
During
week 10-12
(other authors prefer
11-13) of the
pregnancy,
if the indicated distance >3
mm, that
speaks for
risk of
trisomy 21,
especially if
the nasal
bone cannot
be seen.
Distribution of some relevant biochemical markers
Some selected
combinations are
informative.
Down syndromic
pregnancies
= red curve.
MoM = multiple of the
median.
Cross-trimester marker ratios in prenatal screening (2007)
Mehod
Detection rate %
False-positive
First trimester
rate %
{NT, PAPP-A, free beta-hCG}
83,7
5,1
Second trimester
{AFP, uE3, total beta-hCG, INH-A}
84,4
6,6
Cross trimester ratios
{NT, PAPP-A, free beta-hCG} +
{AFP, uE3, total beta-hCG, INH-A}
90,8
3,1
Cross trimester ratios (another survey)
{NT, PAPP-A, free beta-hCG} +
{AFP, uE3, total beta-hCG, INH-A}
90,2
3,9
Some comments. The results of these investigations may be indicative of
other chromosomal anomalies as well as malformations, too. E.g. AFP is
elevated in the case of an open neural tube (and also in the case of twins).
Detection rate % = retrospective analysis.
CT =
cross trimester.
Integrated =
NT
result
included.
Serum
integrated =
serum
values
only.
What can we learn from this figure?: (1) Screening without
karyotyping does not give reliable diagnosis.
(2) Results of second trimester included ► rather late arrival.
(includes NT)
Cost per Down syndromic
pregnancy diagnosed
At 95% detection rate the cost can
vary between GBP 16,500 and
31,400. (British data, 2007.)
###
Financing national health care
If a bigger population is investigated, the cost of screening 100,000
pregnant women can vary between
GBP 3,540,000 and 6,740,000, depending on the extent of biochemical markers involved.
(Average = GBP 51.4 per case.)
PÄTAU SYNDROME
Patau* syndrome: trisomy 13
Multiple
developmental
anomalies, very
limited lifetime.
Trisomy 13 newborns
usually die before
age of 12 months.
* Remember: there is
no umlaut in the
English, thus no ä
for Klaus Pätau of a
German immigrant
ancestry.
Trisomy 13, symptoms and signs
EDWARDS SYNDROME: trisomy 18
Multiple
developmental
anomalies, very
limited lifetime.
Trisomy 18 newborns
usually die before
age of 12 months.
Trisomy 18, symptoms and signs
NUMBERS of GENES IDENTIFIED ON HUMAN
CHROMOSOMES by the HUMAN GENOME
PROJECT (HGP), as by February, 2007*
# 1 = 2782 2610
# 9 = 1148 1076
# 17 = 1469 1394
# 2 = 1888 1748
# 10 = 1106 983
# 18 = 432 368
# 3 = 1469 1381
# 11 = 1848 1692
# 19 = 1695 1592
# 4 = 1154 1024
# 12 = 1370 1268 # 20 = 737 710
# 5 = 1268 1190
# 13 = 551 496
# 21 = 352 337
# 6 = 1505 1394
# 14 = 1275 1173
# 22 = 742 701
# 7 = 1452 1378
# 15 = 945 906
X = 1336 1141
# 8 = 984 927
# 16 = 1109 1032
Y = 307 255
Σ human genes (in this table) = 28,924
Remember: a gene here = a given protein coding sequence of the DNA.
Small characters: data from January, 2006.
* The figures are the same in January, 2008.
SEXUAL DIMORPHISM IN HUMANS
Is there any relationship between the dimorphism of sex chromosomes
and the sex determination and sex development (resulting in the well
known human sexual dimorphism)? – Yes.
Is it possible to compensate for the gene dosis differences (XX vs. XY) of
females and males in the phenotype? (X = 1336, Y = 307 genes.) – Yes.
See M. Lyon’s hypothesis of X inactivation.
SEX DETERMINATION IN HUMANS
a genetic / chromosomal approach
Sexual development and some aspects
of its determination
1) Chromosomal sex
XX vs. XY karyotype, SRY gene on the short arm of Y.
2) Gonadal sex
Testosterone (androgene hormone) production by the fetal testes.
Hormone receptor for testosterone encoded in the X chromosome
(female development is automatic, this is suppressed in the case
of the presence and action of Y chromosome and testosterone).
3) Genital sex
Legal sex (as registered at birth).
4) Secondary sexual characteristics (developing mainly after
puberty).
5) Psychosomatic sex (also determined
by environmental effects).
Fate of the
indifferent
gonadal anlage
In the presence of Y
chromosome, and especially by the activity
of SRY gene in it =
development of testes.
In the absence of SRY
effect, the ovary
development is
automatic.
Important early steps in sexual differentiation
(see precise details in embryology)
MALE: XY, SRY (sex determining region of the Y chromosome) activity. ►
Indifferent genital ridge ► testes ► testosterone. ► Wolffian duct further
develops (gives rise to prostate, ductus epidydimidis, vesicula seminalis
etc.) ► while Müllerian duct disappears. ► Sinus urogenitalis closes. ►
Tuberculum genitale develops into penis. ► Genital ridges close to form
scrotum.
FEMALE: XX automatism. No SRY effect, ► no testes, ► no testosterone
effect, ► no development of Wolffian duct. ► Müllerian duct further
develops and gives rise to tuba uterina, uterus, and vagina. ► Sinus
urogenitalis remains open (labia minora, vestibulum vaginae). ► Tuberculum genitale develops into clitoris. ► Genital ridges do not close, form
labia maiora.
Genes on the Y and X chromosomes
Y
Pseudoautosomal region (PSAR)*.
SRY = sex determining region of the Y chromosome (previously: TDF =
testis determining factor, this term is still in use today).
Localization: Yp11.3.
ZFY = zinc finger protein Y (Yp11.32), a transcription regulator**.
X
Pseudoautosomal region (PSAR)*.
TFM = gene of the androgene (dihydrotestosterone) receptor.
ZFX = zinc finger protein X (Xp22.3-p21), a transcription regulator,
and so on…
99 other genes (including **), which code for proteins expressed in the
testes (or in tumors).
* PSAR on the short arm. Those in the Y and X are homologs to each
other. (There are some pseudoautosomal genes in other locations, too.)
** There is a number of other transcription regulators.
SRY on the Y chromosome
TFM on the X chromosome
The gene codes for a transription regulator protein. Mutation ►46,XY female.
Translocation ► 46,XX male (Klinefelter syndrome).
Gene for dihydrotestosterone receptor (Xq11-q12). ║
TFM = testicular feminisation, ║
Other name: AIS = androgen insensitivity syndrome. ║
Complete form: Morris syndrome, ║
incomplete form: Reifenstein syndrome. ║
Karyotype: 46,XY. Testes in the abdominal cavity. ║
No ovaries, no uterus. ║
Genes on autosomes
AMH, gene coding for anti-mullerian hormone. (Other name: Mullerian
Inhibiting Factor, MIF, or MIS) Responsible for the physiological degeneration of the Müller duct (which gives rise to internal female
organs).
Location: 19p13.3-p13.2. Expression: the encoded protein (560 amino
acids) is produced in the testis, in the Sertoli cells. (In the same gonad
the Leydig cells produce the testosterone, which is involved in the
differentiation of the Wolff duct into prostate, seminal vesicle,
spermatic duct, respectively. The Amh gene becomes silent after
puberty.
AMHR = gene coding for the receptor of AMH (MIF) protein.
PMDS = persistent Mullerian duct syndrome. (For instance uterus in
male, etc.)
Type I: defective Amh.
Type II: defective Amhr.
GENE DOSAGE COMPENSATION
Although there is a number of characteristic phenotypic differences, there
is no phenotypic sign of the more genes in females than in males.
Hypothesis of Mary Lyon: one out of the two X xchromosomes becomes
inactive. (It forms a heterochromatic Barr-body attached to the
internal surface of the nuclear envelope. If there are more than two X
chromosomes, one remains active and all the others become
inactivated: dosage compensation.)
X-inactivation is random, takes place in the 3rd embyonic week. If an X
chromosome–by chance, either of paternal or maternal origin–, has
been inactivated in a cell, in all descendants of that very cell the same
X will be inactivated and forms Barr-body. This can be expressed as
“inactivation is imprinted”.
Because of that random inactivation females are functional mosaics.
Normally there is no preference which X to remain active. We have quite
a big number of data indicating the validity of the random type
inactivation resulting in a closely fifty – fifty ratio. This is, however, a
statistical value, which is a subject of considerable deviations, too.
One, two, and four Barr bodies, respectively, in nuclei of
buccal epithelial cells. Barr body in polymorphonuclear
granulocyte nucleus (drumstick)
SEX CHROMOSOMAL ANEUPLOIDIES
in HUMANS
KARYOTYPES and CONSEQUENCES
X MONOSOMY
Turner syndrome: 45,X.
No Barr body.
Leading symptoms:
Sexual infantilism = immaturity of
secondray sexual characteristics.
Short stature.
Cubitus valgus, pterygium colli, and so
on.
Sterility (infertility) = No maturation and
production of egg cells. Instead of
ovarian tissue so called gonadal streak,
which is made of connective tissue. Not
only germ cells are not produced, neither
estrogen, nor progesterone hormones.
Consequently the level of gonadotropin is
high.
Main symptoms and signs of Turner syndrome
Turner syndrome
pterygium colli
No Grafian follicles, no meiotic divisions are
seen in the histological picture.
No maturation of egg cells. No production of
ovarial hormones.
gonadal streak
and its histology
Turner syndrome
lymphatic edema on the neck
Karyotype: 45,X
and on the feet
Symptoms of Turner syndrome can be partially prevented
Early diagnosis (verified in the neonatal period), including immediate
chromosome analysis (e.g. already from cord blood).
Hormonal treatment: (i) growth hormone, (ii) estorgen and progesterone.
Psychical/psychological support to the parents as well as to the Turner
syndromic patient herself.
X chromosomal hyperdiploidies
47,XXX
trisomy X
49,XXXXX
X pentasomy
X chromosomal hyperdiploidies
47,XXX (trisomy X) is not considered a syndrome: there are no
characteristic signs and symptoms of this aneuploidy, the phenotype is–in the majority of cases–normal*. It can result, however, in the birth of a 47,XXY (Klinefelter syndromic) baby.
(Theoretically the chance would be 1/4; 1/4 XX, 1/4 XXX, 1/4
XY, and 1/4 XXY. In fact the real risk is much lower.) In the
case of triplo-X, prenatal chromosome analysis is strongly recommended.
X tetrasomy (48,XXXX) is characterized by mental retardation;
X pentasomy (49,XXXXX) patients show severe mental and
corporal retardation in all cases, although in these aneuploidies
only one X remains active, all others form Barr bodies.
* See table of spontaneous abortions and chromosome anomalies.
Sex chromosomal hyperdiploidies
Klinefelter sydrome: sex
chromosome trisomy =
47,XXY.
Barr body is present in cell
nuclei.
Leading symptoms:
eunuchoid type tall
stature, gynecomastia, no
body hairs or very sparse,
no beard, small testes
with no Leydig and
Sertoli cell functions.
Sterility (infertility): no
spermiogenesis.
High gonadotrope hormone
level in blood.
Klinefelter syndrome (47,XXY)
Symptoms and signs in Klinefelter syndrome
Klinefelter syndrome variants (48,XXXY, 49,XXXXY,
48,XXYY)
In the case of 47,XXY Klinefelter syndrome
mental abilities are of average in majority of patients.
If more than one extra X chromosome is present in the karyotype
(48,XXXY, 49,XXXXY) mental retardation or even severe mental
retardation is one of the leading symptoms, although only one X
chromosome remains active, all the others form Barr body.
47,XYY
No symptoms,
therefore this is
not a syndrome.
Risk: 47,XXY
karyotype
offspring.
Prenatal diagnosis
stongly
recommended.
STRUCTURAL ABERRATIONS OF
HUMAN CHROMOSOMES
One should not forget the fact:
there are a number of genes in one–light microscopically visible–band. Any
deletion, duplication or rearrangement involves minimum 50 genes. (In high
resolution banding approximately 25.)
AUTOMATED INVESTIGATION OF HUMAN
METAPAHSE CHROMOSOMES
1/ Dividing cells (predominantly: in vitro cell culture, e.g. T cells).
2/ Accumulation in the metaphase: aided by colchicine treatment.
3/ Swelling in hypotonic solution (0.075 M KCl).
4/ Fixing.
5/ Spreading on specimen slides. (Pretreatment for banding.)
6/ Staining: Giemsa’s solution or quinacrine (a fluorescent dye).
7/ Conventional light or fluorescent microscope. TV/CCD camera on its
exit port.
8/ Images to computer which has been programmed for automatic
chromosome analysis. Arranged karyogram on the monitor.
9/ The operator is allowed to correct the arrangement offered by the
computer.
10/ The result is an ordered (arranged) karyogram. Evaluate and
11/ establish karyotype. Save as a karyotype file.
STRUCTURAL CHROMOSOME ABERRATIONS
– Deletion
Ring chromosome formation
Microdeletion
– Duplication
Microduplication (visible within the chromosome), microchromosome
– Isochromosome (deletion and duplication simultaneously)
– Translocation
Unidirectional traslocation
Reciproc translocation
Robertsonian translocation (centric fusion)
– Inversion
Pericentric
Paracentric
– Break and gap
– and some other forms (e.g. homogeneously staining region, double
minutes)
Deletion
any chromosome fragment without a centromere will be lost
Ring chromosome
the two telomeric fragments are lost
Cri du chat syndrome (cat cry disease): 46,XX,5p–
Isochromosome formation
Instead of the regular
separation of sister
chromatids, the long and
short arms, respectively,
remain together, because of
misdivision of the
centromere. Consequently,
in one daughter cell the
short arm, in the other the
long arm will be present in
duplicated (trisomic) form,
while the long arm and the
short arm, respectively, will
be monosomic in that very
cell.
X long arm isochromosome has
been described in Turner
syndrome. Do not miss the
point: that is X short arm
monosomy at the same time.
Robertsonian translocation = centric fusion:
46,XX,–14,t(14;21), Down syndrome
The Robertsonian translocation = centric fusion…
…may be the result of a new
chromosomal abnormality
= de novo mutation, but
also can be inherited from
a balanced carrier parent:
45,XX,–14,–21,t(14;21). ►
Very important. A careful
chromosomal diagnosis has
to be established in any
case of Down syndromic
birth, and if translocation
is discovered, the parents
have to be investigated, too.
Eventually some other
balanced carrier(s) might
be present in the family of
the affected.
Theoretical gametic combinations in balanced t(14;21)
translocation carriers
The theoretical risk in a family where one parent is a balanced carrier
of a Robertsonian 14/21 translocation is calculated as follows:
1/3 normal,
1/3 balanced translocation carrier, and
1/3 unbalanced translocation, i.e. Down syndrome.
The empirical statistical risk is, however, somewhat better:
1/10 for Down syndrome if the mother, and
1/20 if the father is balanced carrier.
Even if we calculate with this latter figures, that is high enough to
indicate: a prenatal chromosome diagnostics is a must. “Must”
means: anyone in the health profession must be aware of the
enhanced risk (like in the case of a pregnant woman ≥35), and is
obliged to inform the parents of that risk. It is the parents’
decision, however, whether they accept the information obtained at
the genetic counseling or not. Please note: no suggestion, no
persuasion, no obligation, just information.
Other types of Robertsonian translocations
t 21/22 Down syndrome
Pätau syndrome
46,XX,–14,t(13;14)
Pätau syndrome
45,XY,–13,–14,t(13,14)
balaced carrier parent
Reciprocal (non Robertsonian) translocation
Enhanced
risk for
incorrect
separation
after meiotic pairing,
resulting in
severe
gametic
(and
zygotic)
chromosomal aberrations. (See
also
considerations on
inversions
below.)
Inversions
Like in the case of balanced
translocations, inversions do not
necessarily involve gene loss or
gene duplication, i.e. the visible
phenotype can be normal,
without any indication of the
presence of some chromosomal
aberration in a balanced carrier.
If, however, during meiosis of a
balanced carrier
recombination(s) cause severe
rearrangements, these latter may
result in an unbalanced genome
in the offspring, which at one end
may be incompatible with life
(e.g. infertility, or serial
spontaneous abortions), on the
other end may result in serious
malformations.
Consequences of inversion and recombination in meiosis…
… and gamete formation after crossing over
and so on...
Familiar mental retardation (FMR)…
… fragile X (fraX, FRAXA) syndrome
1)
Not a real break on the X chromosome, it can be evoked and made
visible by certain cell culture technique (inhibition of DNA
synthesis).
2)
This abnormality can be made responsible for the fact, that mental
retardation is more frequent among males than females
(hemizygosity), although also heterozygous females may express the
symptoms. The fragile site at Xq27.3 is associated with the fmr gene,
i.e. patients with fragile X syndrome do not express the FMR1 gene.
3)
More details in chapter on dynamic (expansive) mutations.
Fragile-X and familial mental retardation
CHROMOSOMAL ABNORMALITIES and
SPONTANEOUS ABORTIONS (in 100,000 pregnancies)
Karyotype Sp. abortion
Normal
7,500
Trisomy 1
0
2
159
3
53
4
95
5
0
6 - 12
561
13
128
14
275
15
318
16
1,229
17
10
18
223
19 - 20
52
21
350
22
424
–(13, 18 and 21) 3,176
Livebirth
84,450
0
0
0
0
0
0
17
0
0
0
0
13
0
11 3
0
0
Karyotype Sp. abortion
47,XYY
4
47,XXY
4
45,X
1,350
47,XXX
21
Livebirth
46
44
8
44
Translocations,
balanced 14
unbalanced 225
164
52
Triploidy
Tetraploidy
1,275
450
0
0
280
49
Σ chromosomal
aberrations 7,500
Altogether
15,000
550
85,000
Others
SISTER CHROMATID EXCHANGE (SCE)
Up to a limited number (approximately 5-10/metaphase) this phenomenon
is considered normal. In certain hereditary diseases the frequency is,
however, elevated, and that is indicative of the presence of e.g. Bloom
syndrome, Fanconi anemia, xeroderma pigmentosum (all these are one
or other kind of DNA repair defects).
SCE frequency is increased e.g. in radiation injury as well as in the
presence of some chemical mutagens.
CHROMOSOME ABERRATIONS and CANCER, I
Philadelphia
chromosome in
CML (chronic
myelogeneous
leukemia).
Reciproc
translocation
►►►
A fusion of ABL
(proto-oncogene)
and BCR gene.
Chromosome aberrations and cancer, II
t(8;14) in B-cell lymphoma
IGH = immunoglobulin heavy chain gene. MYC = protooncogene, which is
activated to oncogene because of translocation.
Advantages of the FISH technique in general,
and in the detection of minor chromosome
abnormalities
FISH = fluorescent in situ hybridization.
You know a given DNA sequence (e.g., from the results of the
HGP). Synthesize a complementary single standed oligonucleotid probe. Label the latter with a fluorochrome.
Separate the two strands of the original double helix (e.g. by
moderate heating), in situ, in the chromatin material.
Add probe. Let it anneal (hybridize) to the complementary
strand (only to that, nowhere else), e.g., by slow cooling.
There are chromosome-specific (region-specific, band
specific, etc.) probes as well as gene specific probes, and the
like.
UP-TO-DATE DEVELOPMENTS of CYTOGENETICS
1/ Dividing cells are not inevitably necessary,
2/ interphase cell nuclei can also be investigated in some cases.
3/ Fluorescent in situ hybridization = FISH, with complementary single
stranded DNA probes (most commonly labeled oligonucleotides).
4/ These probes are: gene-specific, gene segment-specific, chromosomespecific, chromosome segment-specific and so on,
5/ i.e. extremely high resolution can be achieved.
6/ Probes are mostly labeled with a fluorochrome, and the preps are
7/ investigated in fluorescence or in laser confocal microscope.
8/ CCD / TV camera ► computer, programmed for karyotypic and
metaphase chromosome analysis, or a number of other evaluations.
9/ The investigator has a chance to reconsider and correct the result.
10/ The goal of the investigation can be karyotyping, analysis of individual
chromosomes. Even one gene can be identified. And so on.
11/ Another objective: CGH (comparative genomic hybridization) with
quantitative evaluation.
FURTHER DEVELOPMENTS in
CYTOGENETICS
In situ PCR (polymerase chain reaction, amplification of a well
defined, given sequence of a DNA molecule).
Qualitative and quantitative DNA analysis
by PCR (with or without DNA sequenation),
with DNA chips,
and many other recently developed methods.
For instance: one identifies a representative segment on the long
arm of chromosome 21 at the DNA level and determines if it is
present in 1× dose (normal), or in 1.5× doses (trisomy 21) in
isolated DNA of the patient. Cheaper and faster method than
traditional karyotyping.
Note, however. This diagnosis does not tell t(14;21) Robertsonian translocation
Down syndrome from trisomy 21 “classical” Down syndrome. One has to
investigate the presence or absence of 21p, too.
CHROMOSOME PAINTING
with chromosome-specific fluorescent DNA probes
( 46,XY / 47,XY,+8 )
Trisomy 8 might be viable in the
chromosome mosaic form, if only
few cells are trisomic.
FISH, a way to the interphase cytogenetics
Left: DiGeorge syndrome,
del(22q11.21-q11.23), microdeletion.
Right: Williams–Beuron syndrome, del(7q11.2), microdeletion.
Detection of a marker (mar) microchromosome
MCB = multi color banding
UNIPARENTAL DISOMY (UPD)
Some conceptuses have a normal 46,XX or 46,XY karyotype, but have inherited
two copies of the same chromosome from just one of the two parents. This may
result in abnormal phenotypes which are different according to parental origin
of the relevant chromosome.
Isodisomy. Both homologs of the affected are identical.
Heterodisomy. Both homologs of one parent are present in the individual
affected.
UPD is probably a result of an eventual correction of hyperdiploidy. The conceptus
may be trisomic, but the zygote finds a way to get rid of the supernumerary
chromosome (in order to remain viable). For example:
15mat 1 + 15mat 2 + 15pat after correction 15mat 1 + l5pat, or
15mat 2 + 15pat, or
15mat 1 + 15mat 2 = UPD.
The first two versions will not be detected.
Prader–Willi and Angelman syndromes
46,XX or 46,XY individuals who inherit both copies of their chromosome
#15 from their father, develop Angelman syndrome; if both copies of #15
are maternally inherited, Prader–Willi syndrome is seen.
Explanation. In non-UPD patients with Prader–Willi syndrome 15q12 is
deleted from the paternal #15 chromosome, in Angelman syndrome the
maternal #15 suffered a microdeletion of 15q12. If there is no paternal
#15 in the karyotype, it means also the absence of the indicated region.
This abnormality shows itself in the Prader–Willi syndrome.
The basic concept is found in the phenomenon of genomic imprinting. Some
genes are active only on the maternal or only in the paternal
chromosome. If the maternal region should be active, but that is missing,
the situation is equivalent with the occurrence of a loss of function
mutation. Prader–Willi and Angelam syndromes were identified
originally as recessively transmitted human malformations.