The Chronic Lymphocytic Leukemia (CLL)
advertisement

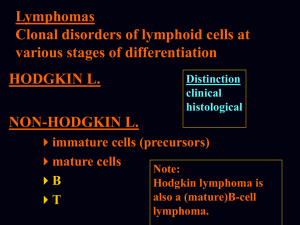
The Chronic Lymphocytic Leukemia (CLL) The Chronic Lymphocytic Leukemias (1) • The group of clonal diseases characterized by proliferation and accumulation of small, mature lymphocytes in blood, bone marrow and lymphoid tissues (lymph nodes, spleen) • Neoplastic lymphocytes belong most often to B-cell lines and they have the special for B-cell antigenes on their surface; exceptionally neoplastic lymphocytes belong to T-cell lines or NKcell • According to REAL (Revised European-American Lymphoma)/ /WHO classification CLLs belong to the group of: – lymphoproliferative diseases – lymphomas Lymphoproliferative diseases • Primary lymphatic system (central) – bone marrow – thymus • Secondary lymphatic system (peripheral ) – spleen – lymph nodes – MALT (The mucosaassociated lymphoid tissue = also called mucosaassociated lymphatic tissue) Clinical stages of lymphomas according to Ann Arbor’s classification I II III IV A: no general symptoms B: general symptoms such as fever, night sweats, weight loss Lister T, et al. J Clin Oncol 1989; 7:1630 • Ann Arbor’s classification is specific for all lymphomas • CLL is classified according to Rai and Binet classification WHO classification B-Cell neoplasms - Precursor B-cell neoplasm: B-lymphoblastic leukemia/lymphoma - Mature (peripheral) B-cell neoplasms: B-cell chronic lymphocytic leukemia/small lymphocytic lymphoma B-cell prolymphocytic leukemia Lympfioplasmacytic lymphoma Splenic marginal zone B-cell lymphoma (+ /- villous lymphocytes) Hairy cell leukemia Plasma cell myeloma/plasmacytoma Extranodal marginal zone B-cell lymphoma of MALT type Nodal marginal zone B-cell lymphoma (+/— monocytoid B cells) Follicular lymphoma Mantle-cell lymphoma Diffuse large B-cell lymphoma Mediastinal large B-cell lymphoma Primary effusion lymphoma Burkitts lymphoma/Burkitt cell leukemia T-cell and NK-cell neoplasms - Precursor T-cell neoplasm: T-lymphoblastic lymphoma/leukemia - Mature (peripheral) T-cell neoplasms: T-cell prolymphocytic leukemia T-cell granular lymphocytic leukemia Aggressive NK-cell leukemia Adult T-cell lymphoma/leukemia (HTLV1 +) Extranodal NK/T-cell lymphoma, nasal type Enteropathy-type T-cell lymphoma Hepatosplenic gamma-delta T-cell lymphoma Subcutaneous panniculitis-like T-cell lymphoma Mycosis fungoides/Sezary syndrome Anaplastic large-cell lymphoma, T/null cell, primary cutaneous type Peripheral T-cell lymphoma, not otherwise characterized Angioimmunoblastic T-cell lymphoma Anaplastic large-cell lymphoma, T/null cell, primary systemic type The Chronic Lymphocytic Leukemia (1) • Chronic lymphocytic leukemias are derived from: • B-cell line – B-cell chronic lymphocytic leukemia – B-cell chronic prolymphocytic leukemia – Hairy cell leukemia – Splenic marginal zone B-cell lymphoma ( + /- villous lymphocytes) • T-cell line – T-cell chronic lymphocytic leukemia – T-cell chronic prolymphocytic leukemia – T-cell granular lymphocytic leukemia • Chronic lymphocytic leukemias differ form each other in biology, morphology, antigen structure of the cell and in clinical course The B-CLL - definition • B-CLL is a neoplastic disease characterized by proliferation and accumulation of small, mature, long-living lymphocytes in blood, marrow and lymphoid tissues (lymph nodes, spleen) • This lymphocytosis leads to specific clinical and laboratory symptoms of B-CLL • The neoplastic lymphocytes have on their surface the special for Bcell line antigens – CD19, CD20 and also CD5, CD23, and a very weak expression of surface immunoglobulin B-CLL epidemiology • Most common adult leukemia in Europe and North America (in USA incidence of about 3/100.000 population) • predominantly, CLL is a disease of elderly (50-55 years) • 40% of leukemias in patients over 60 years old • Morbidity: – Men 2,2-3,69 / 100 000 / year – Women 0,9-1,59 / 100 000 / year /men affect twice as often as women; 2:1 ratio of male to female / • CLL morbidity rapidly increases with age (especially between 50 and 60 years of age) • in 98% of patients the leukemic cells are a monoclonal population of mature B lymphocytes with low-density surface immunoglobulin • death from infections, BM failure, high-grade transformation (Richter's syndrome), kachexia B-CLL etiology & pathogenesis (1) • the cause of CLL is unknown • there is increased incidence in farmers, rubber manufacturing workers and tire repair workers • genetics factors have been postulated to play a role in high incidence of CLL in some families B-CLL etiology & pathogenesis (2) • Cytogenetics - clonal chromosomal abnormalities are detected in approximately 50% of CLL patients • Immunoglobulin genes - monoclonal surface immunoglobulin is expressed by over 90% of patients (60% kappa and 40% lambda light chains) – nearly half of all cases have leukemia cells that express mutated immunoglobulin variable region genes (Ig VH genes) - associated with more indolent disease • Immunologic abnormalities – autoimmune disease (hemolytic anemia and thrombocytopenia, pure red cell aplasia) – hypogammaglobulinemia – cellular immune defects B-CLL clinical symptoms (1) • often none! - 25% of patients are asymptomatic and the diagnosis is typically accidental • unspecific: night sweats, fever, weakness (many patients have fatigue, reduced exercises tolerance or malaise, weight loss) • recurrent infections (bacterial, viral – Herpes Zoster, fungal) – they are the most common cause of death • bleeding and symptoms of anemia and thrombocytopenia • Lymphadenopathy (lymph node enlargement) – at diagnosis - nontender in 80% of patients – later - may become very large • splenomegaly - mild to moderate in 50% of patients • hepatomegaly • some organs infiltration (lungs, pleura, skin and soft tissue) Blood lymphocytosis does not cause symptoms! B-CLL clinical symptoms (2) Cervical and axillary limfadenopathy in 60-years old patient with B-CLL B-CLL clinical symptoms (2) Cervical and axillary limfadenopathy in 70-years old patient with B-CLL B-CLL clinical symptoms (3) Cervical limfadenopathy in patient with B-CLL B-CLL clinical symptoms (3) The CLL patient can have splenomegaly B-CLL clinical symptoms (3) The CLL patient has splenomegaly, which is visble B-CLL laboratory features (1) • Morphology: – Leucocytosis with monoclonal lymphocytosis of greater than 5.000/ul. – anemia • Because of „displacement ” • and/or autoimmunohemolic (10-20% of patients have a positive direct antiglobulin test; AIHA is commonly connected with the presence of warm auto- antibodies IgG class – rapidly increasing fatigue, skin getting yellow, anemia with enlarged reticulocytosis, higher level of bilirubin) • pure red cell aplasia is very rare (selective aplasia of red cell line in bone marrow) – thrombocytopenia • Because of „displacement ” • and/or immunologic (about 5% of B-CLL patients have antyplatelet antibodies) • protein electrophoresis – Hipogammaglobulinemia, monoclonal protein in 5% of patients B-CLL laboratory features (2) • Peripheral blood smear: – Lymphocytosis • small, mature, morphologically normal – Smudge cells – Neutropenia • Because of „displacement ” • and/or autoimmunologic B-CLL laboratory features (3) • Bone Marrow smear (cytological examination) – extensive replacement of marrow element by mature lymphocytes (more than 30%) B-CLL laboratory features (4) • Bone Marrow Biopsy (histological examination): Lymphocyte infiltration – nodular infiltration, – interstitial infiltration, – difussed infiltration – mixed infiltration Difussed infiltration (unfavourable prognostic factor) B-CLL laboratory features (5) • Bone Marrow Biopsy Interstitial infiltration B-CLL laboratory features (6) • lymph node finding (histopathological examination) - diffuse infiltration of small lymphocytes identical to low-grade, small lymphocytic lymphoma B-CLL laboratory features (7) • Immunophenotype: – CD5+/CD19+/CD23+/CD20+, – sometimes also CD38+, – low expression of CD22; – lack expression of CD 10-, CD 103-, – 90% of the patient have a very weak expression of surface immunoglobulin (kappa or lambda light chain, IgM, IgD) B-CLL features (8) • Radiological examinations (X-ray, ultrasonography, CT, ...) • Serological examinations (direct and indirect antiglobulin tests) • Biochemical examinations (lactate dehydrogenase, 2-microglobulin) B-CLL laboratory features (9) • Cytogenetic examinations - clonal chromosomal abnormalities are detected in approximately 50% of CLL patients – deletion 13 (13q14.3) – trisomy 12 – structural abnormalities of chromosomes 11 (11q-), 14, 17 Genomic aberrations found in approximately 50% of CLL Diagnosis of B-CLL Blood test lymphocytosis ≥ 5G/l (6 weeks) Morphology monoclonal population of small mature lymphocyte B-cell CLL phenotype clonal CD5+/CD19+ population of lymphocyte Markers of clonality κ/λ light chain restriction; cytogenetical abnormalities Bone marrow infiltration > 30% of nucleated cells on aspirate Lymph node diffuse infiltrate of small lymphocytes RAI’s CLINICAL STAGING SYSTEM Stage Clinical Features at Diagnosis Median Survival (years) 0 Low risk Blood lymphocytosis>5G/l, Bone marrow lymphocytosis>30% >12,5 I Intermediate risk Blood lymphocytosis>5G/l, Bone marrow lymphocytosis>30% and enlarged lymph nodes 8 II Intermediate risk Blood lymphocytosis>5G/l, Bone marrow lymphocytosis>30% and enlarged spleen and/or liver 6 III High risk Blood lymphocytosis>5G/l, Bone marrow lymphocytosis>30% and anemia (Hb < 11g/dl) 1,5-2 IV High risk Blood lymphocytosis>5G/l, Bone marrow lymphocytosis>30% and thrombocytopenia(< 100 000 /ul) 1,5-2 CLL – Rai stages BINET’s CLINICAL STAGING SYSTEM Stage Clinical Features at Diagnosis A Blood lymphocytosis>5G/l, Bone marrow lymphocytosis>30% and less than 3 areas of palpable lymphoid-tissue enlargement Without anemia (Hb >= 6,21 mmol/l, 10 g/dl) and thrombocytopenia > 120 month B Blood lymphocytosis>5G/l, Bone marrow lymphocytosis>30% and 3 and more areas of palpable lymphoid-tissue enlargement Without anemia (Hb >= 6,21 mmol/l, 10 g/dl) and thrombocytopenia 60 month C Blood lymphocytosis>5G/l, Bone marrow lymphocytosis>30% with anemia (Hgb <10g/dL) or thrombocytopenia (Plt <100.000/uL) 24 month An area: cervical, axillary left, axillary right, inquinofemoral left, inquinofemoral right lymph nodes, spleen, liver Median Survival (month) CLL – Binet’s stages New prognostic indicators in B-CLL (1) Prognostic factor Good prognosis Bad prognosis Clinical stage according to Binet Rai A 0 B, C I, II, III, IV Non-Difussed infiltration <=80% lymphocytes <= 50 x 109/l <= 10% Difussed infiltration > 80% lymphocytes > 50 x 109/l >10% > 12 months <= 12 months Bone marrow infiltration in - bone marrow biopsy - cytological examination Leucocytosis Prolymphocytes in peripheral blood Leukemia cell doubling time New prognostic indicators in B-CLL (2) Prognostic factor Good prognosis Bad prognosis Serum markers: - lactate dehydrogenase activity (LDH) - ß2-mikroglobulin activity - lymphocyte’s thymidine kinase activity - CD23 expression Normal range Clonal chromosomal abnormalities Normal karyotype Del (11q) isolated del (13q) Del (17p) CD 38 expression <= 30 % Elevated > 30% New prognostic indicators in B-CLL (3) Prognostic factor Good prognosis Bad prognosis The mutational status of mutated immunoglobulin variable region of heavy chain genes (IgvH) unmutated ZAP–70 expression low (< 20%) high ( > 20 %) Survivin absence presence New prognostic indicators in B-CLL (4) - summary • • • • • • • • • clinical stage bone marrow histology (diffuse replacement carries worst prognosis) leukemia cell doubling time (less than 1 year - worse prognosis) percentage of prolymphocyte high cell-surface expression of CD38 ZAP-70 expression serum level of: B2-microglobulin; thymidine kinaze, LDH, sCD23 IgVH mutational status genetic features - FISH cytogenetic – low-risk: normal kariotype; isolated del(13q) – high-risk: del(17p0, del(11q), trisomy 12 CLL : ZAP-70 ZAP70 is an intracellular protein which is strongly correlated with the VH status in CLL CLL – treatment (1) • We have to remember: – B-CLL – indolent lymphoma, but incurable – Elderly patients – risk of additional diseases – Course of the disease can be very long, indolent for many years, patient can die because of another reason which is not connected to BCLL. • Decision about treatment depends on clinical stage, prognostic factors and patient’s condition • Indications to treatment: • III/IV stage according to Rai’s classification • Progressive disease (rapidly increasing lymphadenopathy, infections, general symptoms) • leukemia cell doubling time <6 (12) months • rapidly increasing organomegaly • Secondary anemia, neutropenia, thrombocytopenia because of bone marrow infiltration • Richter’s syndrome CLL – treatment (2) • Watch and wait • Monotherapy – Glucocorticoids (autoimmunological complications) – alkylating agents (Chlorambucil, Cyclophosphamide) – purine analogues (Fludarabine, Cladribine, Pentostatin) • Combination chemotherapy – Chlorambucil/Cyclophosphamide + Prednisone – purine analog (Fludarabine) + Cyclophosphamide +/- Mitoxantrone – CVP, CHOP (Cyclophosphamide, Doxorubicin, Vincristin, Prednisone) • Monoclonal antibodies (monotherapy and in combination) – Alemtuzumab (anti-CD52) = CAMPATH – Rituximab (anti-CD20) = Mabthera – antiCD23 etc. – monoclonal antibodies conjugated with radionuclides = Ibritumomab tiuxetan = Zevalin • Splenectomy (hypersplenism) • Radiotherapy (massive lymphadenopathy) CLL – treatment (3) • Hematopoietic stem cell transplantation – autologous - still no cure with auto-SCT – allogenic with reduced intensity conditioning • Even RIC-SCT is still a risky procedure - indicated only in highrisk disease • Can allo-SCT cure CLL? - YES • New and novel agents – Oblimersen – bcl2-directed antisense oligonucleotide – Lenalidomide – Flavopiridol – Anti-CD23 – Anti-CD40 • Vaccine strategies • Supportive therapy (allopurinol, G-CSF, blood and platelet transfusion, immunoglobulins, antibiotics) Response criteria (NCI working group 1996) • Complete response (for at least 2 months) – clinical features – normal – morphology – normal (Hb>11 g/dl; Pt>100 000 /ul, lymphocytes <4000 G/l; neutrofiles >1500 G/l)) – bone marrow - lymphocytosis less than 30% • Partial response • Stable Disease • Progressive Disease Richter’s Syndrome • is always the transformation of CLL into an aggressive Lymphoma – diffuse large cell lymphoma (DLCL) or Hodgkin‘s lymphoma • usually evolves after a long indolent course • can occur as 1st manifestation of CLL: Primary Richter‘s - but still CLL • has a poor prognosis