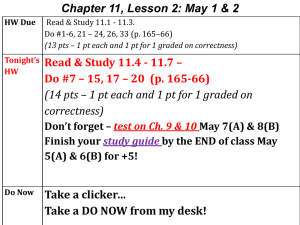
Microbiology_Classification_Review
advertisement

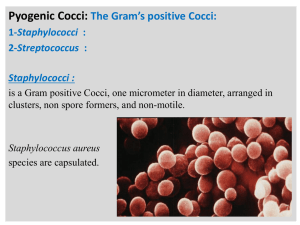
Gram Positive (purple/blue) Cocci Catalse (+) STAPH Coagulase (+) S. AUREUS Catalse (-) STREP Rods (bacilli) CLOSTRIDIUM (anaerobe) LISTERIA BACILLUS CORYNEBACTERIUM α Coagulase (-) Hemolysis Novobiocin (+) S. EPIDERMIDIS Capsule S. PNEUMONIA No Capsule VIRIDANS STREP β Group A S. PYOGENES Group B S. AGALACTAIE γ ENTEROCOCCUS PEPTOSTREPTOCOCCUS Novobiocin (-) S. PNEUMONIAE Gram Negative (pink) Cocci Maltose Fermenter Non Fermenter NEISSERIA MENINGITIDIS NEISSERIA GONORRHOEAE Rods “Coccoid” Rods H. FLU PASTURELLA BRUCELLA BORDETELLA PERTUSSIS Fast lactose Fermenter KLEBSIELLA E. COLI ENTEROBACTER Slow Fermenter CITROBACTER SERRATIA Oxidase Negative SHIGELLA SALMONELLA PROTEUS Lactose Nonfermenter Oxidase Positive PSEUDOMONAS Gram positive Gram negative 2 envelope layers: 3 envelope layers: 1) cytoplasmic membrane 2) thick peptidoglycan layer 1) cytoplasmic membrane 2 )thin peptidoglycan layer 3) phospholipid/LPS Low lipid content No endotoxin No periplasmic space High lipid content Endotoxin Periplasmic space Teichoic Acid O Specific Side chain Metabolic Characteristics • Obligate aerobes •Love oxygen •Need it to grow •Have all 3 enzymes •Like oxygen /doesn’t require it • Facultative anaerobes •Can use anaerobic fermentation •Catalase and Superoxide Dismutase • Microaerophilic bacteria • Obligate Anaerobes •Like small amounts of oxygen •Aerotolerent anaerobes •Superoxide Dismutase •Don’t like oxygen •No enzymes to counter act Gram Positive Pathogens • Cocci – Staphylococci – Streptococci • Rods (bacilli) – Spore formers • Bacillus • Clostridium – Nonspore formers • Nonfilamentous – Corynebacterium – Listeria – [Mycobacterium-kind of] • Filamentous – Actinomyces – Nocardia Gram Positive Pathogens Cocci-catalase test Streptococcus Streptococci-negative Staphylococci-positive Staphylococcus Genus: Staphylococci • Gram Positive Cocci in groups and clusters • Catalase positive • Coagulase Test for differentiation – S. Aureus-positive – S. Epidermidis-negative – S. Saprophyticus-negative Virulence factors •Surface protein A binds to Fc portion of IgG (prevents opsonization) •Enterotoxin and TSST-1 toxins Staphylococcus Aureus Direct infection Impetigo MRSA Staphylococcus Aureus diseases due to toxins TSST-1 Enterotoxin Very stable Scalded Skin Syndrome Genus: Staphylococcus Staph Epidermidis Genus: Streptococcus Catalase Negative Gram Positive Cocci in pairs and chains Genus: Streptococcus • • • • S. pyogenes S. agalactiae S. pneumoniae Enterococcus Genus: Streptococcus • Lancefield Antigens – Lancefield antigens denote cell wall carbohydrates – The presence of Lancefield antigens defines the pyogenic streptococci – Groups A through T • A,B, C and D are most important – Some Streptococcus are not assigned (they do not possess) Lancefield antigens Genus: Streptococcus • Hemolysis on BAP • The hemolysis is defined as alpha, beta and gamma No Complete Partial Genus: Streptococcus • Strep Pyogenes – Group A Beta Strep – Strep throat, scarlet fever, rheumatic fever, acute glomerulonephritis, impetigo • Strep Agalactactiae – Group B Beta Strep – Perinatal sepsis, meningitis and/or pneumonia • Strep Pneumoniae – Pneumococcus – Optichin Sensitive – Otitis media, pneumonia, meningitis • Enterococcus – Group D – UTI Genus: Streptococcus Lancefield Antigen Hemolysis on BAP Strawberry tongue • Group A Beta Strep – S. pyogenes • • • • • Strep Throat Scarlet Fever Rheumatic Fever Post Streptococcal Glomerulonephritis Impetigo Chromatographic Immunoassay Pharyngitis Genus: Streptococcus • Strep Agalactactiae – Group B Beta Strep – Perinatal sepsis, meningitis and/or pneumonia • Early Sepsis within one week of birth • Late Sepsis from 7days to 3 months of birth Genus: Streptococcus • • • • Alpha hemolysis Optichin Sensitive Gram positive Lancet Shaped Diplococci Strep Pneumoniae Significant sequalae – Pneumococcus (nickname) – Otitis media, pneumonia, meningitis Right lower lobe pneumonia encapsulated Genus: Streptococcus • Enterococcus – Group D – Virulence Factors • • • • • Abx resistant due to PBP Acquired Resistance Enzymes Adherence factors Biofilm formation – UTI, catheter related infections Gram Positive Spore Forming Rods • Bacillus (Fac. Anaerobe) • Clostridium (Strict Anaerobe) Genus: Bacillus • Fac. Anaerobe • G + Spore Forming Rod • Bacillus – B. Anthracis • Cutaneous • Respiratory • Intestinal Respiratory B. Anthracis BAP Genus: Clostridium • Anaerobic G + Rod • Spore formers • Clostridium – C. Perfringens – C Tetni – C. Botulinum – C. Difficile Myonecrosis/ gas gangrene Target hemolysis on BAP ~ two zones due to production of 2 toxins Genus: Clostridium • Anaerobic G + Rod • Spore formers • Clostridium – C. Perfringens – C Tetni – C. Botulinum – C. Difficile Neurotoxin binds to presynaptic terminals in prevents transmission of inhibitory neurotransmitters Terminal Spore DTP and DTaP Tennis Racket Genus: Clostridium • Anaerobic G + Rod • Spore formers • Clostridium Toxin ingestion (usual) – C. Perfringens – C Tetni – C. Botulinum – C. Difficile Infantile Botulism caused by spore ingestion with endogenous toxin production Spores Genus: Clostridium • Anaerobic G + Rod Endoscopic view of Psuedomembranous colitis • Spore formers • Clostridium – – – – C. Perfringens C Tetni C. Botulinum C. Difficile Plain film of abdomen showing bowel wall thickening, loss of haustral markings (thin arrow) and dilation of the ascending and transverse colon (thick arrow) Gram Positive Nonspore Forming Rods • Nonfilamentous – Corynebacterium – Listeria – [Mycobacterium-kind of] Genus: Corynebacterium • • • • • Gram Positive Nonspore Forming Rods Immobile Nonencapsulated Nonfilamentous Corynebacterium – C. Diphtheriae Pseudomembrane of throat and/or nasal cavity DTP and DTaP Pallisades/ Chinese Letter Arrangements Barred appearance (metachromatic granules) Genus: Listeria • Gram Positive Nonspore Forming Coccobacilus • Tumbling motility at 25 degrees Celsius • Nonfilamentous – Listeria • L. Monocytogenes Transplacental and birth canal transmission Raw milk, soft cheeses, ice cream, raw vegetables, raw or cooked poultry, raw meat, raw or smoked fish Beta hemolysis Genus: Mycobacterium • • • • • Gram Positive Nonfilamentous Nonspore Forming Rods Strict aerobe Very slow growing Weakly gram positive Acid Fast-waxy cell wall-mycolic acid – [Mycobacterium -kind of] • M. Tuberculosis • M.Leprae Divides every 15 to 20 hours Acid fast gram positive bacteria PPD Genus: Mycobacterium • • • • • Gram Positive Nonfilamentous Nonspore Forming Rods Waxy coating->acid fast Aerobic/ nonmotile Can not grow in artificial culture [Mycobacterium -kind of] – M. Tuberculosis – M.Leprae • Leprosy • Hanson’s Disease Nine banded Armadillo Incubation is 2-20 years • Gram Positive Filamentous Nonspore Forming Rods • Aerobic to Fac. Anaerobe • Opportunistic • Actinomyces – A. Israelii • Nocardia Genus: Actinomyces • Gram Positive Filamentous Nonspore Forming Rods • Aerobic to Fac. Anaerobe • Non acid fast • Opportunisitic • Actinomyces Lumpy Jaw – A. Israelii Actinomycoses infections are polymicrobial Primary source is soil Genus: Nocardia • • • • • • Colonies smell like wet dirt Gram Positive Filamentous Branching Weakly acid fast Strict aerobe Catalase positive Nonspore Forming Rods – Nocardia Low virulence opportunistic infection Now on to Gram Negatives Gram Negative Cocci • Neisseria – N. Meningitidis – N. Gonnorhea • Moraxella – Branhemella Cattorhalis • Gram Negative Cocci • Kidney bean shape • Ferments maltose and glucose like meningitis • Oxidase and catalase positive • Endotoxin production • Neisseria – N. Meningitidis • Meningiococcus (nickname) • Meningitis, septic shock – N. Gonnorhea Kidney bean shape Not B Nonblanching petechial rash Direct or from cultured specimen • Gram Negative Cocci • Kidney bean shaped • Neisseria – N. Gonorrhea • Gonorrhea • Ophthalmia Neonatorum Culture is the gold standard $$$ Nucleic Acid Amplification Tests Ophthalmia Neonatorum Otitis media • Gram Negative Cocci • Aerobic • Moraxella – Branhemella Catorrhalis • Otitis media, sinusitis sinusitis Gram Negative Spirochetes • Treponema – T. Pallidum • Borrelia – B. Burgdorfi – B. Recurrentis • Leptospira Gram Negative Spirochetes • • • • Too small for gram stain Can not be cultured from clinical specimen Dark field microscopy of clinical sample Treponema – T. Pallidum • Syphillus-acquired and congenital Electron Micrograph – Nontreponemal tests – Treponemal tests Secondary stage Gram Negative Spirochetes western black-legged tick (Ixodes) • Microaerophilic • Geimsa or Wright stain • Borrelia – B. Burgdorfi Erythema migrans Gram Negative Spirochete • • • • • • • • Aerobic Motile G –cell envelope Animal reservoirs Flexible spirochete Not seen on gram stain Dark field microscopy Leptospira – L. Interrigans Fine spirals with hooked ends Water transmission Petichial rash Many Many Gram Negative Bacilli • Respiratory – – – – Heamophilus Bordetella Legionella Gardnerella – – – – – Yersinia Franicisella Brucella Pasteurella Bartonella • Zoonotics • Enterics – Many many Respiratory Gram Negative Bacilli • • • • • • small pleomorphic, gram-negative coccobacillus. Nonmotile non–spore-forming fastidious facultative anaerobe Heamophilus – H. Influenzae – H. Ducryi Respiratory Gram Negative Bacilli • • • • • • Small pleomorphic, gram-negative coccobacillus. Nonmotile Otitis media non–spore-forming Fastidious-X &V factor facultative anaerobe Heamophilus Epiglottitis – H. Influenzae Insp. Stridor • HIb • Epiglottitis, otitis media, meningitis, pneumonia – H. Ducryi conjugated Satelliting around Staph. Respiratory Gram Negative Bacilli • small pleomorphic, gramnegative coccobacillus. • Nonmotile • non–spore-forming • Fastidious-X &V factor – Dies quickly outside of body • facultative anaerobe Heamophilus – H. Ducryi • “soft chancre” • Culture is difficult • chancroid Painful genital ulcer Respiratory Gram Negative Bacilli • Small aerobic G- Coccobacilllus • Singly and in pairs • Nicotinamide required for (slow) growth • Bordetella Bordet-Gengou – B. Pertussis medium – Whooping cough DTP & DTaP ELISA or PCR assays Paroxysmal cough with an inspiratory whoop Respiratory Gram Negative Bacilli • Nicotinamide required for (slow) growth • Bordetella – B. Pertussis – Whooping cough DTP & DTaP ELISA or PCR assays Virulence factors •Pili and surface protein for adhesion •Pertussis toxin •Enzyme that disrupts immune response •Peptidoglycan injury to ciliated trachea cells Bordet-Gengou medium Respiratory Gram Negative Bacilli • • • • • Poorly staining Facultative Intracellular parasite Compromised host Aerobic Legionella – L. Pneumophila • Legionnaires' disease – Pneumonia Paired serum sample Urinary antigen Sputum culture NONRespiratory Gram Negative Bacilli • Presumptive Identification – Clue Cells – KOH • Does not require X & V factors • Gardnerella – G. Vaginalis • Bacterial Vaginosis (BV), preterm labor Whiff Test Clue cells cervicitis Zoonotic Gram Negative Bacilli • Yersinia • Y. Pestis – Franicisella • F. Tulerensis – Brucella • • • • B. Suis B. Meltensis B. Abortus B. Canis – Pasteurella • P. Multicida – Bartonella • B. Henselae • B. Quintana Zoonotic Gram Negative Bacilli • Nonmotile • G- rod • Yersinia • Bubonic Plague bubo Y. Pestis Pneumonic Plague Zoonotic Gram Negative Bacilli •G- bacillus •Aerobic •Low infecting dose •Vector->tick or deer fly •Special media •Immunoflourescence •Serum Serology (>1:40) •Franicisella •F. Tularensis •Pneumonia •Glandular ulceroglandular pneumonia Zoonotic Gram Negative Bacilli • • • • • Nonmotile Non-acid fast Nonsporeforming Small G- coccobacillus Catalase, oxidase and urease positive • Brucella – Brucellosis Blood culture Recurrent flu-like symptoms with granulomas Zoonotic Gram Negative Bacilli • • • • • • • • Small G- coccobacillus Nonspore forming Oxidase positive Ferments CHO Nonmotile Grows on BAP PCN susceptible Bacteriophage encoded toxin Pasteurella – P. Multocida • Cellulitis associated with animal bites Bipolar staining Well demarcated cellulitis Zoonotic Gram Negative Bacilli • • • • • fastidious pleomorphic aerobic gram-negative bacillus Bartonella – B. Henselae • Cat Scratch Fever – B. Quintana • Trench fever • Urban Trench Fever Paired sera Pediculus humanus Cat scratch fever Family: Enterobacteriacea • • • • • • • • Escherichia Coli Shigella Salmonella Yersinia Klebsiella Proteus Enterobacter Serratia •Enterics live in the gut-> are members of the family of Enterobacteriacea •O antigen is lipopolysaccaride •K antigen is polysaccharide capsule •H-flagellar antigen Enterics • • • • • Facultative Anaerobe Large G- Rods Nonsporeformers Normal Flora Escherichia Coli – E. Coli (nickname) – E. Coli 0157:H7 or 0157 – UTI, Sepsis, Enteric E.Coli, Respiratory illness, multiple opportunistic infections Motile strains with peritrichous flagella UTI/ Pyelonephritis Enterics • Facultative Anaerobe • Large G- Rods • Nonsporeformers • Relatively inert • Shigella – S. Sonnei – S. Flexneri – S. Dysenteriae • Shigillosis The O antigens (LPS) define the four species of Shigella Enterics • • • • • • G- Rod Nonsporulating, Facultative anaerobe Ferment glucose Reduce nitrate Peritrichous flagella Eggs & Enteritidis when motile • Produce gas upon sugar fermentation Salmonella – S. Typhi • Typhoid Fever – S. Enteritidis • Gastroenteritis Carrier states Enterics • Nonmotile • G - rods • Prominent polysaccharide capsule • Multi Drug Resistant • Recently important in nosocomial infections • Normal flora • Klebsiella – K. Pneumoniae • Pneumonia in debilitated, UTI, etc etc. Encapsulated/ multi drug resistant Enterics • • • • • Gram Negative Rod Normal Flora Hydrolyzes Urea (struvite stone formation) Proteus – P. Mirabilis Opportunistic infections including UTI Highly motile Enterics • G-Rod • Multi drug resistance • Enterobacter – E. Aerogenes – E. Cloacae • UTI,Endocarditis, opportunistic infection Enterics • G-rods • Opportunistic infection Serratia – S. Marcescens Other Gram Negative Rods • • • • Vibrio Helicobacter Pseudomonas Bacteroides Other Gram Negative Rods • Vibrio – V. Cholerae Other Gram Negative Rods • Helicobacter – H. Pylori Other Gram Negative Rods • Helicobacter – Campylobacter Jejuni Other Gram Negative Rods • Pseudomonas – Ps. Aeruginosa Other Gram Negative Rods • Bacteroides – B. Fragilis Weird Bugs • • • • Chlamydia Rickettsia Coxiella Ehrlichia Weird Bugs • Chlamydia – C. Trachomatis Weird Bugs • Obligate intercellular gram negative coccobacilli • Vector – Dermacentor variabilis (dog tick) East US – Dermacentor andersoni Rocky Mountain region and Canada • Rickettsia – R. Ricketseii Peticheal rash Weird Bugs • Obligate intercellular gram negative coccobacilli • Coxiella Brunetti Weird Bugs • Ehrlichia – E. chaffeensis – E. ewingii Ehrlichea in white tail deer fawn Distribution of Amblyomma americanum Amblyomma americanum Nymph left ; adult right [Lone Star Tick] Genus: Mycoplasma • Pleomorphic • No cell wall • Mycoplasma – M. Pneumoniae • Atypical pneumonia The Inevitable Exceptions • Mycobacteria – Weakly gram positive – Better seen with acid fast stain • Spirochetes – Too small for light microscopy – Need Dark field microscopy • Mycoplasma – No cell wall – Neither G+ or G-