Mechanism of Thyroid Hormones
advertisement

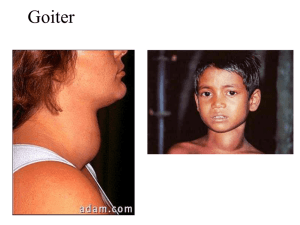
HPT axis Review of HPA Hypothalamus receives multiple signals from various regions of the brain Hypothalamus can directly release hormones into bloodstream in posterior pituitary via neurons or; Secrete hormones via portal system (blood vessels) to anterior pituitary that regulate hormone secretion from anterior pituitary HPT axis Hypothalamic-pituitary-thyroid axis Thyrotropin releasinng hormone (TRH) is released from paraventricular nucleus of hypothalamus TRH stimulates cells in the anterior pituitary, called thyrotropes, to release thyroid stimulating hormone (TSH) TSH stimulates the thyroid gland to synthesize the thyroid hormones (T3 and T4) Anatomy of thyroid gland Thyroid gland is an unpaired endocrine gland surrounding anterolateral (front and sides) surface of trachea in the neck Consists of two lateral lobes with a connecting isthmus (narrow strip) Histology and Composition •Composed of spherical follicles •Follicles are surrounded by a single layer of epithelial cells called follicular cells •Inner space is called follicular lumen and is filled with a colloid rich in thyroglobulin protein •Parafollicular cells, or “C-cells”, can be found scattered among follicular cells or in spaces between follicles •TSH receptors are found on the surface of follicular cells Colloid Thyroglobulin Follicular cell Parafollicul ar cell “Ccell” Capillary TSH receptor Thyroid hormone synthesis Thyroglobulin (Tg) is made in the follicular cells and released into the follicular lumen Tg has a number of exposed tyrosine residues An enzyme called thyroperoxidase (TPO) oxidizes an iodide (I-) to I+ and adds it to the tyrosine rings of Tg to get MIT and can do it a second time and form DIT TPO can fuse a DIT and an MIT to form T3 or DIT and a DIT to get T4 Thyroid hormone synthesis Tg, along with the attached T3, T4, DIT, and MIT, is engulfed by the follicular cell Tg is broken down and the T3 and T4 are released into the bloodstream Iodide in thyroid hormone synthesis Iodide is essential to the synthesis of TH On the external (non-lumenal) surface of follicular cells are iodide pumps that actively transport iodide into cell at concentrations 20-50 times of that outside the cell Effect of TSH Has multiple roles in increasing TH release Increases activity of iodide pump such that the ratio of [I]IC:[I-]EC is 500:1 Affects DNA to increases production of the iodide pump Activates TPO Stimulates breakdown of Tg and release of T3 and T4 Where are thyroid hormones stored? Thyroid hormones are stored in the colloid inside the follicle Stored in the form of iodinated thyroglobulin Thyroid gland can store enough hormones to serve the body for 2 – 3 months Thyroglobulin Glycoprotein (10% carbohydrate) 660 kDa, dimeric protein produced by and used only within the thyroid gland Produced by the follicular cells of the thyroid During storage, T3 and T4 are attached to thyroglobulin When thyroglobulin is endocytosed hormones are released Hydrolysis releases thyroid hormones Release of Thyroid Hormones 1.When TSH is released, thyroglobulin molecules form colloid droplets and are taken back up into follicular cells by endocytosis 2.Colloid droplets fuse with lysosomes hydrolysis of Tg T3 and T4 are released 3.About 10% T4 converted to T3 before secretion 4.T4 and T3 containing vesicles are excreted out to blood stream Delivery of Thyroid Hormones to Tissues T3 and T4 are water-insoluble Need to bind to a transport protein in the serum to be transported to tissues Thyroid Binding Globulin (TBG) = produced by the liver Transthyretin (TTR) = also secreted by liver Albumin = main protein in blood http://www.anaesthetist.com/icu/organs/endocr/th yroid/images/t3t4.gif Thyroid Binding Plasma Proteins Protein Binding strength Plasma concentration Thyroid Binding Globulin (TBG) highest lowest transthyretin (TTR) lower higher Albumin poorest much higher http://en.wikipedia.org/wiki/Transthyretin •In cerebrospinal fluid, TTR is the primary carrier Thyroid Proteins in Plasma Type Percent bound to Thyroxin Binding Globulin (TBG) 70% bound to transthyretin (TTR) 10-15% Albumin 15-20% unbound T4 (fT4) 0.03% unbound T3 (fT3) 0.3% http://en.wikipedia.org/wiki/Thyroid_hormone Conversion of T4 to T3 All T4 is converted to T3 in peripheral tissues More T4 is secreted by thyroid But T3 works better than T4 This conversion is done by Iodothyronine Deiodinase http://www.anaesthetist.com/icu/organs/endocr/th yroid/images/t3t4.gif Mechanism of Thyroid Hormones Thyroid hormones are hydrophobic readily cross lipid bilayer Bind to receptor in cytoplasm Enter nucleus Bind to DNA in the nucleus Change DNA expressions change specific mRNA level change protein level Physiologic Effects of Thyroid Hormones Almost all cells in the body are targets for thyroid hormones Important for development, growth and metabolism Deficiency and excess state lead to abnormal health state Thyroid Hormone and Metabolism Stimulate metabolic activities in most tissues → lead to increase in BMR (Basal metabolic rate) BMR = the amount of energy a person expends daily while at rest Thyroxine increases the number and activity of mitochondria in cells → increased body heat production → increased oxygen consumption and rates of ATP hydrolysis Effects on Lipid and Carbohydrate Metabolism Carbohydrate metabolism Low amounts glycogen synthesis (enhance insulin dependent entry of glucose into cells) High amounts glycogenolysis and gluconeogenesis to generate free glucose Lipid metabolism Deficient serum cholesterol levels increase High amount → fat mobilization and oxidation of fatty acids in tissues → serum cholesterol levels decrease Effects on Growth and Development Thyroid hormones are needed for normal growth in children and young animals Thyroid deficiency → growth-retardation Tadpoles deprived of thyroid hormone → unable to undergo metamorphosis into frogs Normal levels of thyroid hormones are essential for proper development and growth of fetus and neonatal brain Other Effects Cardiovascular system Thyroid hormones → increase heart rate, cardiac output, and vasodilation → more blood flow to organs Increase transcription of myosin protein genes in cardiac muscle → increased cardiac contractility Central Nervous System Too little → mentally sluggish Too much → anxiety and nervousness Reproductive System Too little → infertility Dysregulation - Hyperthyroidism Too much = HyPERthyroidism = increased thyroid hormones in blood Non-functional negative feedback system Graves Disease = autoimmune disease → antibodies bind to and activate the thyroid-stimulating hormone receptor → continuous stimulation of thyroid hormone synthesis Common symptoms: Nervousness, high heart rate, anxiety, weight loss but increased food ingestion Treatment: anti-thyroid drugs → suppress synthesis of thyroid hormones by blocking thyroid peroxidase Dysregulation - Hypothyroidism Too little = HyPOthyroidism Primary: Problem with the thyroid → part of the thyroid is destroyed (95% cases) = Hashimoto's thyroiditis Secondary: problem with pituitary → decreased TSH secretion → decreased production of T3 and T4 Tertiary: problem with hypothalamus → decreased TRH hormone Iodine deficiency → not enough thyroid hormones are made Common symptoms: Lethargy, fatigue, weakness, cold intolerance, reproductive failure, weight gain but appetite decrease Treatment = synthetic thyroid hormone