Microbiology
Cheng Zhang
Thurs 1 Dec 11
MM Tutorial
Gram staining
1.
2.
3.
4.
5.
Fixed film (heat kill bacteria etc...)
Methyl violet
STAIN 1: violet-blue
Lugol’s/gram’s iodine
Decolourise with acetone
Methyl red STAIN 2 (counter stain): pink-red colour
Gram staining
G+ve keeps stain 1 VIOLET/BLUE
G-ve recolourises with stain 2 PINK/RED
Organisms stain poorly with gram’s stain:
• Mycobacteria ‘Acid fast’ ZN stain instead
• Spiral bacteria Treponema, Leptospira,
Borrelia
• Mycoplasma Has no cell wall
• Rickettsia, Coxiella, Chlamydia obligate
intracellular
Nota bene
Bacterial pathogens can be...
• Extracellular
– Examples: Staphylococcus, Streptococcus
• Facultative intracellular = capable of living and
reproducing inside and outside a cell
– Examples: Listeria, Neisseria
• Obligate intracellular = cannot reproduce
outside host cell
Gram staining
• Peptidoglycan which is stained – most of cell
wall in G+ve but only about 10% in G-ve
• Acetone destroys outer lipopolysaccharide
membrane of G-ve washing away STAIN 1
• Peptidoglycan matrix retains STAIN 1
For your stage...
• Bacteria are either:
• G+ve or G-ve or other (as mentioned)
• Cocci (balls) or bacilli (rods) [or spirals]
• G+ve cocci: Streptococcus; Staphylococcus; Enterococcus
• G+ve bacilli: Clostridium, Listeria only ones you need
to know
• G-ve spirals: Helicobacter, Campylobacter
• G-ve cocci (HAN): Haemophilius , Acinetobacter,
Neisseria
For your stage...
• G-ve bacilli: Literally everything else you are
likely to be asked at this stage... you name it!
• Salmonella, Shigella, Proteus, ESBL i.e. E. Coli
and Klebsiella, Pseudomonas, Vibrio sp.,
Legionella...
For your stage...
• In summary...
• G+ve cocci... Staph + Strep + Enterococcus
• G+ve bacilli... Clostridium + Listeria
• G-ve cocci... NAH (What other N, A and H do
you know at this stage?)
• G-ve spirals: Helicobacter, Campylobacter
• G-ve bacilli... Everything else
Boring stuff
• Virulence, Infective dose, Virulence
determinants (genes), Pathogenicity islands
(clusters of genes)
• Factors in virulence?
– Tropism
– Replication (find nutrients)
– Immune evasion
– Toxic (exotoxins, endotoxins)
– Transmission
Routes of infection?
What organism causes what?
• Use your common sense...
• Don’t memorise the ridiculous list
Routes include:
–
–
–
–
–
Respiratory e.g. TB, pneumonia
Faecal-oral e.g. cholera, shigella
Direct contact e.g. UG: name any STI
or skin e.g. Staph
Vector borne (tick-borne) Lyme disease (Borrelia)
• Note: Erythema migrans
Familiarise yourself with names!
• The more you hear it, the more it’ll stick
• Most are aptly named e.g. Strep pneumoniae, Neisseria
meningitidis, Neisseria gonorrhoea, Mycobacterium
TB/leprae, Vibrio cholerae, Salmonella typhi
• Some can still be worked out e.g. Campylobacter
JEJUNI, Helicobacter PYLORI, Bacillus ANTHRACIS
• Some are confusingly named e.g. Haemophilius
influenzae, Rickettsia
• The rest you’ll have to learn... Enjoy!
• Large and small bowel: Gram negs, anaerobes, candida!
So, get to know what causes what!
• What are the bacterial causes of pneumonia?
• Diarrhoea?
• ETC...
• N.B. Single gram positive cause of pneumonia
is Streptococcus pneumoniae (pneumococcus)
“Pathogens to know....”
Gram negative
• Neisseria (meningitidis and
gonorrhoeae)
• Haemophilus influenzae
• E. coli (EPEC, EHEC, ETEC,
UPEC)
• Salmonella spp.
• Vibrio cholerae
• Shigella
Gram positive
• Staph aureus (PVL)
• Streptococcus
–
–
–
–
Group A = S. pyogenes
Group B = S. agalactiae (newborn)
Strep viridans = oral bacteria
Pneumococcus = S. pneumoniae
• Clostridium (difficile, tetani,
botulinum, perfringens)
• Listeria spp.
“Opportunistic bacterial pathogens”
Gram negatives
• Pseudomonas aeruginosa
UTI
• Acinetobacter baumanii
ITU infections, pneumonia
Gram positives
• Staphylococcus epidermidis
Commensal
• Enterococcus faecalis
Not VRE, common
A little bit of detail...
Vibrio cholerae (Genus species or G. species)
• Gram stain? Rod? Ball? You tell me...
• Extracellular, colonises small bowel
• Profuse watery diarrhoea (faecal-oral) – fluid replace
• 1A5B toxin co-regulated pilus (similar Shigella, E. coli)
• A = active, B = binding. Hence... 1A injected
intracellularly and ADP-ribosylates G-proteins
• The constantly active G protein stimulates adenylate
cyclase to increase cAMP to open apical ion channels
• Chloride and water leak out into the lumen
A little bit of detail...
Clostridium difficile
• Gram stain? Rod? Ball? You tell me...
• Hospital exposure to spores
• Opportunistic pathogen – antibiotics clear normal
flora
• Diarrhoea (symptomatic infection)
• If severe.. abdo pain, pseudomembranous colitis,
perforated colon leading to faecal peritonitis..
• Rx: Stop other ABx, use metronidazole,
vancomycin
A little bit of detail...
Neisseria meningitidis
• Gram? Rod? Ball?
• Vaccine for menC not menB
• Subepithelial colonisation in nasopharynx
• Septicaemia (10% fatality); non-blanching rash
• CSF neck stiffness, photophobia, vomitting
HAIs
Nosocomial = HAI >48h after admission
Immunocompromised; Immunosuppressed
WHY? Lines, catheters, intubation, chemo, prophylactic AB, prosthetics
UK BIG FIVE
• MRSA
• VRE (Enterococcis faecium)
• E. coli/Klebsiella (NDM-1) (ESBL enterobacteraciae)
• P. aeruginosa
• Acinetobacter baumannii
• Clostridium difficle
• Vancomycin-insensitive S. aureus (VISA)
• Stenotrophomonas maltophilia (what the!??!)
Antibiotics
Think of it in families:
• Inhibit cell wall synthesis
• Inhibit protein synthesis
• Inhibit DNA synthesis
• Metabolic targets
• Inhibit RNA synthesis (rifampicin)
• Metronidazole
Antibiotics
• Bacteriostatic/Bacteriocidal
• The ones in your slides:
–
–
–
–
–
Beta-lactams (inhibits transpeptidation enzyme)
Tetracycline (competes with tRNA for A site)
Chloramphenicol (bind to 50S subunit)
Quinolones (inhibits DNA synthesis)
Sulphonamides (competes for dihydropteroate)
• Co-trimoxazole for p. carinii
– Aminoglycosides (bind to 30S subunit)
• Gentamicin, streptomycin: many UWEs
– Macrolides (bind to 50S) e.g. erythromycin
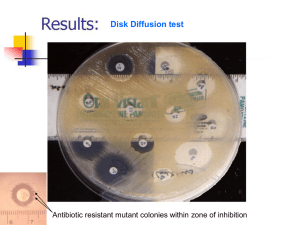
Antibiotic resistance
1.
2.
3.
4.
5.
6.
Decreased influx
Increased efflux e.g. Tetracycline
Drug inactivation e.g. Penicillin/ESBL
Target modification e.g. Penicillin/Quinolones
Target amplication e.g. Sulphonamides
Other: biofilms, spores, intracellular
Transfer of antibiotic resistance
1. Plasmids
2. Transposons – mobile genetic elements
integrate to chromosomal DNA
3. Integrons – gene cassettes in clusters, collect
resistance genes
Vaccination
• Active immunity – host response to antigen –
vaccination induces this
• Passive immunity – acquiring protection from
another immune individual through transfer
of antibody or activated T cells
• Herd immunity provides protection to
unvaccinated individuals. Ring vaccination.
Vaccine formulations
• Antigen(s) to stimulate an immune response
• Adjuvant to enhance and modulate the
immune response
– Delivery systems e.g. slow release depot
– Immune potentiators stimulate immune system
e.g. PAMPs such as TLRs
• Excipients e.g. buffer, salts, saccharides,
proteins to maintain pH, osmolarity, stability
Vaccine antigens
•
•
•
•
•
Live attenuated organisms e.g. BCG, Sabin (oral)
Killed organisms e.g. Cholera, Salk (IM)
Component vaccines e.g. Tetanus
DNA vaccines
Conjugate vaccines – saccharide linked to
protein carrier e.g. MenC
Fungal infections
• 3 major subclasses
• Allergies – over-exuberant immune response
to spores e.g. ABPA
– IgE blood test
• Mycotoxicoses – no immune component,
mycotoxin ingestion e.g. Aflatoxin, magic
mushrooms
– Rx: gastric lavage, charcoal, organ transplant,
supportive
Fungal infections
• Mycoses (fungal infections) – result of impaired
immunity
– Superficial (cosmetic of skin or hair shaft) e.g. Black
Piedra
– Cutaneous e.g. T. capitis, T. Pedis
– Subcutaneous e.g. Eumycetoma (often after traumatic
implantation of agent)
– Systemic (deep)/invasive e.g. Candida, IPA
• Dx: Gold standard is microscopy of sample e.g. BAL, skin,
sputum, vaginal smear, CSF...
• Also PCR, Ig/Ag-based assays
Fungal pathogens
• True or primary pathogens
– Endemic in well-defined areas
– You don’t need to be able to name any
• Opportunistic
– Ubiquitous
– Cryptococcus, Candida (1/4 carriers), Aspergillus
– N.B.
• C. albicans is a yeast at low temp and pH
• Nitrogen nutrient starvation: pseudohyphae (elongated cells
looking for nutrients)
• Serum pH: hyphae (cells divide)
Antifungal targets
1. Cell membrane (fungal ergosterol)
•
•
Polyene antibiotics e.g. Amphotericin B, Nystatin
Azole antifungals
2. DNA/RNA synthesis e.g. Flucytosine
3. Fungal cell wall (glucans, chitin)
•
Echinocandins e.g. Caspofungin acetate
Viruses
• 20-450nm obligate intracellular parasites
• Nucleic acid (DNA or RNA) + protein
(nucleocapsid – helical or icosahedral) +
sometimes lipid + sometimes CHO
• Many asymptomatic. Cause
epidemics/pandemics when viruses jump from
native species to unnatural host e.g. H1N1
(Spanish Flu) 1918/19 killed 40 million, SARS-CoV,
HIV
• Zoonosis
Viruses
1.
Binding to host cell – specificity
–
–
–
2.
Penetration
–
–
3.
Enveloped viruses fuse e.g. HIV, measles
Non-enveloped disrupt host cell membrane – genome crosses into
cytosol e.g. polio, bacteriophage T4
Eclipse phase (period of non-infectivity)
–
–
–
4.
5.
HIV gp120 to CD4
EBV gp340 to CD21
Influenza HA to sialic acid
Virus disassembled so no infectious particles present
Expression of viral proteins in highly regulated way
Nucleic acid... Protein coat... Proteins for cell lysis
Assembly of new particles
Release – cell lysis or budding (viruses with envelopes bleb)
Baltimore classification
• Based on how +ve sense mRNA is made! All
viruses must make mRNA.
• Single strand? double strand?
• +ve sense? –ve sense?
• Some degree of common sense can be applied
e.g. retroviruses
• ssDNA first copied to dsDNA
(host machinery)
• Retroviruses reverse
transcribed to DNA,
integrated with our DNA,
transcribed by our enzymes
• Viral genome ssRNA +ve =
same sense as mRNA
• dsRNA viruses have to
provide enzyme
• ssRNA –ve viruses must
provide enzyme to form
opposite strand polarity
Virus infection outcomes
• INFLUENCED BY...
– Virus dose, Route of entry (variolation), Age/sex/physiological state
(VZV, EBV asymptomatic in child, HBV > in neonates)
• CELL DEATH
– Polio (paralysis), rotavirus (diarrhoea), HIV (immunodeficiency), HBV
(hepatitis), rhabovirus (hydrophobia)
• PERSISTENT
– HBV (hepatitis), measles (subacute sclerosing panencephalitis)
• LATENT
– HSV-1 or 2 (cold sores, genital herpes), VZV (chickenpox, shingles)
• CELL TRANSFORMATION/CANCER
–
–
–
–
HBV (hepatocellular carcinoma)
HPV-6 and 11 (common warts)
HPV-16 and 18 (cervical/penile cancer)
EBV (Burkitt’s, nasopharyngeal carcinoma)
Viral routes of entry
• Respiratory: influenze, measles, mumps, variola,
VZV, rhinovirus
• Skin: HPV, HSV-1 and 2, rhabovirus, yellow fever
virus (mosquito)
• Blood products: HIV, HBV, HCV
• Genital tract: HIV, HSV-2, HPV-16 and 18
• GI: Polio, HAV, rotavirus
RELEASE
– Blood, Skin, Gut, Respiratory, Saliva, Semen, Breast
milk (HCMV), Placenta
Viruses evade the immune system by...
1. Antigenic variation
2. Hiding
3. Express inhibitory proteins
HIV (retrovirus env. +ve ssRNA)
•
•
•
•
>95% AIDS in developing country
Sexual, IVDU, mother-to-baby, blood products
Genome integrated into host DNA as provirus
Virus gp120 binds to CD4 + CCR5
(macrophage) or CXCR4 (T cell)
• HA (Highly Active) ART
HIV
1. Acute infection 2-3 months – active virus
replication, temporary reduction in CD4
2. CD8 HIV-specific CTL produced – virus titres
decrease and CD4 recovers. Patient may
become asymptomatic. Virus replication
continues in LNs – variation to escape
immune system
3. Virus variants escape control by CTL, titres
increase, CD4 drops and patient develops
AIDS
HIV drugs
1. Binding/entry binds CXCR4, CCR5 or gp41 (T-20)
2. Reverse transcription Nucleoside reversetranscriptase inhibitors e.g. AZT and NNRTI
(allosteric enzyme inhibition) e.g. EFV
3. Protease inhibitors (prevent cleavage of polyprotein
precursors) e.g. Ritonavir
4. Integrase inhibitors prevent integration with host
DNA e.g. Raltegravir
• Learn short names e.g. T-20 for Enfuvirtide, AZT for
Zidovudine
• If you’re hell bent on getting a ridiculously high
exam mark, learn the whole list.
Influenza
• -ve sense ssRNA enveloped
• Antigenic drift (AA mutations) and shift (e.g.
zoonosis e.g. human + avian co-infection)
• 100nm:
• HA (glycoprotein, binds sialic acid)
• NA (removes sialic acid to allow new viruses to
escape) – tamiflu
• M2 ion channel
Virus vaccines
• Smallpox, diphtheria, tetanus, yellow fever,
pertussis, MMR, poliomyelitis, HBsAg
• Smallpox eradicated because...
–
–
–
–
No animal reservoir
No latent/persistent infection
Easily recognisable disease
Vaccine effective against all strains, low cost,
abundant, potent (vaccinia vaccine and variola
envelope highly conserved)
– WHO co-ordinated a global effort
Questions?