How to manage high risk myeloma — Dr Matthew Jenner
advertisement
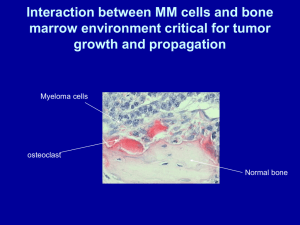
How to Manage High Risk Myeloma UK Myeloma Forum Autumn Day 12 November 2014 Dr Matthew Jenner Consultant Haematologist Southampton General Hospital Introduction Why define high risk myeloma? • Patient expectations o Outcomes vary widely between different patients o Myeloma very heterogenous disease • Aim for a risk stratified approach – one size may not fit all o Maximise treatment for those that need it o Minimise treatment and toxicities for those who may not o Acute leukaemia and lymphoma models • Better define high risk disease o Subgroup analysis may lead to identification of common clinical and biological features leading to more individualised treatments 3 Variables that impact prognosis in any malignancy including myeloma • • Patient factors o Age o Performance status (activity levels) o Co-morbidities o Medication o Kidney function Tumour stage o in myeloma, markers of disease bulk o ISS based on albumin and beta 2 microglobulin • Tumour biology o Isotype o Extramedullary myeloma and plasma cell leukaemia o Genetic lesions detected by cytogenetics, gene expression or mutation analysis o Response to treatment High risk myeloma Defining high risk myeloma Individual drug therapies Autologous transplantation Clinical trials and future strategies Smouldering myeloma Smouldering myeloma Classifiers of high risk status • Degree of bone marrow infiltration o IMWG criteria • Imaging o PET-CT o Whole body CT o Whole body DW MRI • Immunophenotyping o Aberrant vs normal plasma cells • 7 ?Cytogenetics Smouldering myeloma Role of high risk cytogenetics • Data for cytogenetics in symptomatic myeloma is clear cut • Adverse IgH translocations and copy number abnormalities well recognised o t(4;14), t(14;16), t(14;20), del1p, del17p, gain 1q • Same abnormalities found in MGUS and smouldering myeloma • Case series of stable MGUS and SMM with apparent high risk abnormalities • IgH translocations initiating events • Copy number abnormalities ?progression events 8 MGUS and smouldering myeloma cytogenetics: Wessex myeloma database IgH translocations • • • MGUS SMM MM t(4;14) 6/193 (3%) 19/148 (13%) 198/1830 (11%) t(14;16) 6/193 (3%) 4/148 (3%) 55/1830 (3%) t(14;20) 9/192 (5%) 1/149 (<1%) 27/1830 (1.5%) Different patterns of progression from MGUS and SMM to myeloma t(14;20) stable disease MGUS o • SMM o o 9 t(4;14) 1/5 progressed and t(14;16) 2/6 progressed at median f/u of 17-120 months from diagnosis of MGUS t(4;14) 12/19 progressed and t(14;16) 2//4 progressed at median f/u of 33 to 78months from diagnosis of SMM Evolving and non-evolving pattern of progression FM Ross, L Chiecchio et al, Haematologica 2010 Smouldering myeloma • • • No evidence to recommend treatment based on HR cytogenetics alone Use standard CRAB criteria for commencing treatment +/- novel imaging Close monitoring including imaging • Rationale: o Potential role for homeostasis between sub clones • Need for further studies to evaluate in face of new agents o Require OS as well as PFS data 10 Case 1 Case 1 60 year old female • 1996 o • 2005 o o • Generalised bone pain, weight loss IgG kappa paraprotein 15g/L Free KLC 551 mg/L BMA: 15% PC FISH: t(14;16), del17p, del1p, gain 1q ISS 2 SS: lytic lesions skull, humeri, collapse L2 and T12 July 2013 o o 12 DCIS left breast with bilateral mastectomies and Arimidex No evidence of relapse on follow-up May 2013 o o o o o o o • Right breast carcinoma treated with WLE and RT Local RT L2 8Gy single fraction Myeloma XI: CTD Case 1 • CTD x6 achieving VGPR: o o • • • BM: MRD positive 0.1% abnormal PC HDM(200) ASCT 9/12/13 D100 11/3/14 o o o o • • Paraprotein 1.6 g/L FKLC 127 mg/L BM: no excess PC MRD pos 0.1% abnormal PC April 2014 Randomised to lenalidomide and vorinostat maintenance June 2014 progressive flank pain: o o 13 paraprotein 0.7 g/L FKLC 140 mg/L Renal tract USS neg July 2014 PET-CT Case 1 PET-CT Case 1 July 2014 • PET-CT o o • Widespread FDG avid lesions multiple vertebrae, sternum, ribs, pelvis Left paravertebral mass MRI o T7 to T11/12 soft tissue mass with early cord compromise • • • Bone marrow approx 10% PC Paraprotein 3.5 g/L Free kappa light chains 77 mg/L • Treatment: o o o o • 15 RT to paraspinal mass VRD-PACE VRD VRD-PACE Awaiting follow-up imaging Case 1 Observations • • • • • Cytogenetically defined high risk myeloma (HRMM) Role of individual drugs cannot be ascertained from single case Achieved VGPR. MRD positive. Commenced maintenance at approx 4 months post ASCT Extramedullary relapse • Questions: o o o How important is depth of response in cytogenetically defined HRMM? Does high dose mephalan improve outcome or promote progression? What is the role of consolidation and maintenance and when should it start? o Does recovery period post ASCT enable myeloma plasma cell recovery? o o 16 What is more important dose intensity or dose density? What is the role of imaging? Genomic landscape of high risk myeloma Initiation and progression of myeloma Morgan, Walker & Davies, Nature Reviews Cancer 2012 Clonal dynamics in a patient with high-risk MM. The summarized results of 8 different FISH assays are shown to indicate the relative abundance of each clone defined by aCGH at the 5 time points studied. ©2012 by American Society of Hematology Keats J J et al. Blood 2012;120:1067-1076 HRMM: Thalidomide MRC Myeloma IX - Trial Design Intensive N = 1,960 RANDOMISATION Clodronate CVAD Zoledronic acid CVAD Clodronate C-TD Non-intensive RANDOMISATION Zoledronic acid C-TD Clodronate MP Zoledronic acid MP Clodronate C-TDa MEL-200 ASCT Max Response RANDOMISATION RANDOMISATION –Thal +Thal –Thal Zoledronic acid C-TDa +Thal Treatment continued until disease progression Primary endpoints: PFS, OS, ORR Secondary endpoints: Time to first SRE, SRE incidence, Safety, and QoL Zoledronic acid (4 mg IV q 3-4 wk); Clodronate (1,600 mg/d PO) ISRCTN68454111 21 Myeloma IX: Landmark analysis in patients with favourable and adverse iFISH Favourable iFISH Adverse iFISH B 100 100 80 80 60 Patients (%) Patients (%) A 40 CTDa MP P < .001 20 0 88 93 0 CTDa MP 88 93 12 60 40 CTDa MP P = .41 20 0 32 81 53 16 77 44 24 36 48 OS (months) 10 5 60 CTDa MP 72 60 55 0 60 55 12 43 44 24 23 17 36 8 8 48 3 6 60 OS (months) • In patients with favourable FISH there was a strong OS advantage for CTDa compared to MP. • This effect was not seen in patients with adverse cytogenetics: • t(4;14), t(14:16), +1q, del(17p) GJ Morgan, FE Davies et al, Blood 2011 Survival according to thalidomide maintenance therapy regimen (ITT population): (A) PFS; and (B) OS; (C) OS in patients with favorable iFISH profiles; (D) OS in patients with adverse iFISH profiles. Morgan G J et al. Clin Cancer Res 2013;19:6030-6038 ©2013 by American Association for Cancer Research HRMM: bortezomib IFM 2005-01 Bortezomib-Dex vs. VincristineAdriamicin-Dex (VAD) Newly diagnosed myeloma suitable for intensive chemotherapy and ASCT A: VAD Diagram of patient disposition and patient flow through protocol. Harousseau J et al. JCO 2010;28:4621-4629 ©2010 by American Society of Clinical Oncology B: Vel Dex IFM 2005-01: (A) Event-free survival (EFS) and (B) overall survival (OS) in patients with t(4;14) treated with bortezomib-dexamethasone (Vel/Dex) induction (n = 106) or vincristine, doxorubicin, and dexamethasone (VAD) induction (n = 98; EFS and OS in years; P < .001 for EFS and OS Avet-Loiseau H et al. JCO 2010;28:4630-4634 ©2010 by American Society of Clinical Oncology CONSORT diagram of 827 adult patients with multiple myeloma (MM) in the Dutch-Belgian Hemato-Oncology Group 65/German Multicenter Myeloma Group HD4 (HOVON-65/GMMG-HD4) A: VADthalidomide Sonneveld P et al. JCO 2012;30:2946-2955 ©2012 by American Society of Clinical Oncology B: PADbortezomib HOVON Phase III Trial of PAD and bortezomib maintenance vs. VAD and thalidomide in Myeloma: Survival Cumulative % Progression Free 100 HR: 0.79 (95% CI: 0.66-0.95; P = .01) 75 PAD 50 25 VAD PAD 0 n 373 371 0 12 VAD F 243 215 24 Mos 36 48 Survival Outcome HR 95% CI P Value PFS Overall From last HDM 0.79 0.82 0.66-0.95 0.66-1.02 .01 .08 OS 0.73 0.56-0.96 .02 Sonneveld P, et al. ASH 2010. Abstract 40. Kaplan-Meier survival curves of progression-free survival (PFS) and overall survival (OS) according to treatment arm within subgroups according to del(17p). Arm A VAD/thal Arm B PAD/bort Bortezomib appears to overcome adverse effect of del(17p) Perhaps related to adverse impact of thalidomide on del(17p) myeloma? Sonneveld P et al. JCO 2012;30:2946-2955 ©2012 by American Society of Clinical Oncology Bortezomib-Based Versus Nonbortezomib-Based Induction Treatment Before Autologous Stem-Cell Transplantation in Patients With Previously Untreated Multiple Myeloma: A Meta-Analysis of Phase III Randomized, Controlled Trials (A) Kaplan-Meier distribution curve (intent-to-treat analysis) for the key efficacy end point of progression-free survival. (B) Forest plot of hazard ratios for progression-free survival, for the individual studies and the integrated analysis Sonneveld P et al. JCO 2013;31:3279-3287 ©2013 by American Society of Clinical Oncology HRMM: Total therapy Total Therapy 3 Developed at MIRT, Arkansas Multidrug sequential treatment (V-DT-PACE) Intensive chemotherapy Tandem autologous transplantation Consolidation Maintenance High risk myeloma defined by gene expression profiling TT2 no bortezomib TT3 with bortezomib 32 TP53 deletion is not an adverse feature in multiple myeloma treated with total therapy 3 GEP low risk GEP high risk OS British Journal of Haematology Volume 147, Issue 3, pages 347-351, 21 AUG 2009 DOI: 10.1111/j.1365-2141.2009.07864.x http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2141.2009.07864.x/full#f1 EFS Identification of novel agents that improve the survival of patients with high-risk MM. xy plot of percent OS for the 2 arms of randomized controlled clinical trials for patients with different genetic lesions. Bergsagel P L et al. Blood 2013;121:884-892 ©2013 by American Society of Hematology HRMM: Novel agent combinations VRD consolidation Nooka et al Leukaemia 2014 • High-risk myeloma defined by o o o o • • • • 45 patients Induction not specified, majority VTD or VRD ASCT Maintenance therapy o o o o 36 the presence of deletion of p53 (locus 17p13) deletion of 1p (t(4;14) or t(14;16) by fluorescence in situ hybridization or by metaphase cytogenetics presentation as PCL (20% circulating plasma cells in peripheral blood) lenalidomide (10 mg/day orally) on days 1–21 of a 28-day cycle bortezomib (1.3 mg/m2 per week subcutaneously/intravenously) low-dose dexamethasone (40 mg per week orally) for up to 3 years, followed by single-agent lenalidomide maintenance thereafter RVD consolidation Overall median PFS 32/12, 3 year OS 93% 37 ASCT and maintenance 39 PFS Mel 200 x2 vs. MPR Len maint vs. not Therapy of high risk myeloma Potential conclusions • • • • Thalidomide minimal benefit during induction Thalidomide adverse as maintenance Bortezomib partially overcomes adverse risk associated with t(4;14) myeloma Bortezomib may overcome adverse risk associated with del17p myeloma Impact on GEP defined high risk myeloma unclear Tandem autologous transplant superior to MPR consolidation in high risk myeloma Lenalidomide maintenance unclear in high risk myeloma • All needs formal randomised evaluation • • • 43 MUK9 Optimum study Introduction: • High risk myeloma accounts for 20-30% of presenting cases • This subset of patients do not benefit from current treatment approaches • • There is a need for this population to develop both Good diagnostic tools to identify these patients New treatment strategies The high risk trial is a specific trial geared towards fit newly diagnosed high risk patients Registration phase: identify high risk patients Treatment phase: investigate 2 new treatment approaches Evaluate alongside anticipated best treatment including maintenance Cytogenetic inter-relationship Adverse translocation (n=144) Deletion 1p(n=71) 135 Number gained Frequency 1p- 10% 1q+ 34% 17p 9% Adverse Translocation 21% GEP 20% Overall 25-35% 2 61 6 1 7 60 Deletion 17p (n=74) Gain 1q (n=264) EMC92 180 65 71 Adverse (n=144) 14 18 1 7 18 48 Deletion 17p (n=74) 20 Cytogenetics Myeloma IX data Diagnosing high risk myeloma Our current definition of high risk is based on: - a full blood-count to identify Plasma cell leukaemia - A PCR based expression assay to identify translocations - MLPA to identify copy number changes such as 1q+, 1p- and 17q - Gene expression profile for High risk profile (EMC92 score) Kuiper et al (2009) Kaiser et al (2013) Daratumumab Daratumumab is monoclonal antibody Targets CD38 and has multiple mechanisms of action against CD38+ MM cells including - ADCC (antibody dependant cytotoxicity) - ADCP (antibody dependant cell phagocytosis) - Apoptosis - Modulating the enzymatic activity of CD38 (Cell adhesion) Demonstrated activity in MM Enhances the potency of other MM drugs such as Lenalidomide offering an interesting alternative to chemotherapy in myeloma. MUK9 Optimum study concepts • Arm A: intensive, chemotherapy-rich, DNA damaging. Hit multiple sub-clones • Arm B: Alkylator light to minimise secondary genetic events. Multiagent non-DNA damaging agents • Arm C: standard arm Pre-Screening 1200 newly diagnosed myeloma patients 20-30% High risk 70% Standard risk 15-20% t(11;14) High risk trial 60 % Hyper diploidy Other trials Other 20-30% lost CTD CVD CRD VTD Induction X2 cycles Max Define high risk status Newly diagnosed patients Trial design To progression Split HDM-V HDM-V ASCT ASCT VRDdX6 VRdX12 Rd CVRDd HDM ASCT VRDdX6 VRdX12 Rd CRD HDM ASCT VDT-PACE X 2 Registration phase: 1200 newly diagnosed patients 8 week turnaround time Randomise 50 patients per arm Expand by another 35 patients in best arm vs. Control Aim to open early 2015 R Endpoints: Primary phase II: • PFS • Abilility to turn around risk-defining investigations within 8 weeks Secondary • Overall survival • Deliverability of treatment • Clinical benefit rate • Maximum overall response • Time to progression • Time to maximum response • Response at first relapse • Safety • Toxicity • Recruitment rate Exploratory: To evaluate the potential to reduce genome instability by altering treatment strategies avoiding excessive alkylating agent exposure. Follow-on from MUK9 Optimum study Phase 2/3 expansion National Phase 3 study: NCRI portfolio Pick a winner concept Define best arm to evaluate against standard arm Potential to establish a high risk “backbone” on to which newer agents can be added Added benefit of providing baseline risk-based classification that may feed in to other studies Acknowledgements • ICR/RMH o o o o • o Sarah Brown o Louise Flanagan Gareth Morgan Faith Davies Martin Kaiser Eileen Boyle • • Myeloma CTN o o o o o 54 Eric Low Heather MacKinnon Jennifer Fraser Gordon Cook Guy Pratt Leeds CTRU Wessex Regional Genetics Lab o Fiona Ross o Laura Chiecchio