Update on ILCOR - Myra Wyckoff, MD, FAAP
advertisement

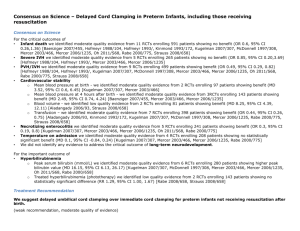
Session Title: NRP Current Issues Seminar Session Number: C0006 Myra H. Wyckoff, MD, FAAP UT Southwestern Medical Center at Dallas Update on the International Liaison Committee on Resuscitation (ILCOR) The 2015 Scientific Review is almost here! Faculty Disclosure Information In the past 12 months, I have no relevant financial relationships with the manufacturer(s) of any commercial product(s) and/or provider(s) of commercial services discussed in this CME activity. I do not intend to discuss an unapproved/investigative use of a commercial product/device in my presentation. Achieving Consensus on Resuscitation Science Australian Resuscitation Council Since 2000, the AAP with the American Heart Association, participates with the International Liaison Committee on Resuscitation (ILCOR) for a complete review of resuscitation science every 5 years. 32 new questions being reviewed for 2015 ILCOR 2010 Neonatal Working Group Guidelines for Neonatal Resuscitation Guidelines available online October 19, 2015 Printed Guidelines supplement will be published in Circulation, Resuscitation and likely Pediatrics Will be able to download at: www.heart.org/cpr NRP Guidelines are set by the AAP NRP Steering Committee Initial Assessment and Intervention CO2 detector, pulse oximetry O2 use during resuscitation O2 saturation targets Meconium stained amniotic fluid Umbilical Cord Clamping Prenatal prediction of respiratory compromise Supportive Therapy Warming Adjuncts Ventilation Strategies CPAP and IPPV LMA Comparing IPPV devices Ventilation parameters for neonates Monitoring During and After Intubation Bradycardia and CO2 monitoring CO2 detection Ventilation volume monitoring Teaching Resuscitation High fidelity training Impact of debriefing on team performance Circulatory Support Compression/Ventilation ratio 2 Thumb vs 2 Finger CPR Epinephrine dosing IO vs IV IV vs ETT drugs Naloxone Sodium Bicarbonate Volume Resuscitation Postresuscitation Management Hypothermia (induced) Maternal fever Supplemental glucose Withholding or Stopping Resuscitation Efforts Duration of CPR with asystole and outcome Futile resuscitation rules Initial Assessment and Intervention CO2 detector, pulse oximetry O2 use during CPR O2 saturation targets for preterms Meconium suctioning of the nonvigorous infants Umbilical Cord Clamping for nonvigorous infants Prenatal prediction of respiratory compromise Ventilation Strategies CPAP and IPPV LMA Comparing IPPV devices PEEP vs no PEEP Sustained Inflation Monitoring During and After Intubation Bradycardia and CO2 monitoring CO2 detection Ventilation volume monitoring Teaching Resuscitation Frequency of training Impact of debriefing on team performance Circulatory Support Compression/Vent ratios 2 Thumb vs 2 Finger CPR Epinephrine dosing IO vs IV IV vs ETT drugs Naloxone Sodium Bicarbonate Volume Resuscitation Supportive Therapy Warming Adjuncts Impact of Maternal Temp Impact of Hypothermia Impact of Hyperthermia Postresuscitation Management Hypothermia (induced) Maternal fever Supplemental glucose Withholding or Stopping Resuscitation Efforts Apgar score of 0 at 10 minutes Futile resuscitation Hot Topics in Neonatal Resuscitation Should cord clamping be delayed for neonates who are non-vigorous? How to best maintain euthermia of the neonate in the delivery room? Does intubation and suction benefit the nonvigorous meconium stained neonate? How should oxygen be used for premature neonates in the delivery room? How to deliver initial breaths to a premature neonate in the delivery room? Handling of the Cord In preterm neonates including those who require resuscitation does delayed cord clamping versus immediate cord clamping improve outcome? In very preterm infants does milking the cord versus immediate clamping improve outcomes? Temperature Management in the DR In non-asphyxiated babies at birth, does maintenance of normothermia (Core temp>=36.5 degrees and <=37.5 degrees centigrade) from delivery to admission, compared with hypothermia (< 36ºC) or hyperthermic (> 37.5ºC), change 77 F outcome. Among preterm neonates who are under radiant warmers in the hospital, does increased room temperature, thermal mattress, or another intervention, compared with plastic wraps alone, change outcome? Suctioning of the Non-vigorous Meconium Stained Infant Does suctioning of the trachea improve outcomes (prevent meconium aspiration syndrome, etc.) for non-vigorous meconium stained infants? Handling of the Cord In preterm neonates including those who require resuscitation does delayed cord clamping versus immediate cord clamping improve outcome? In very preterm infants does milking the cord versus immediate clamping improve outcomes? Delivery Room O2 Among preterm newborns (< 37 wks GA) who receive PPV in the delivery room, does low initial oxygen (21-30%) as opposed to high initial high oxygen (80-100%) decrease mortality, BPD, ROP, neurologic deficit, time to HR > 100 bpm How to Deliver Initial Breaths to a Preterm Infant in the DR In term/preterm newborn infants who do not establish spontaneous respiration at birth, does the administration of one or more pressure-limited sustained lung inflations lasting 15-30s as compared to intermittent positive pressure ventilation with short inspiratory times (< 1s) for 30-60s improve outcome? Great News! There is lots of new science to review and incorporate into the new ILCOR guidelines! Ackowledgments Thanks to the AAP for several of the photos used for illustration