Janssen - Endstage COPD nog naar de IC
advertisement
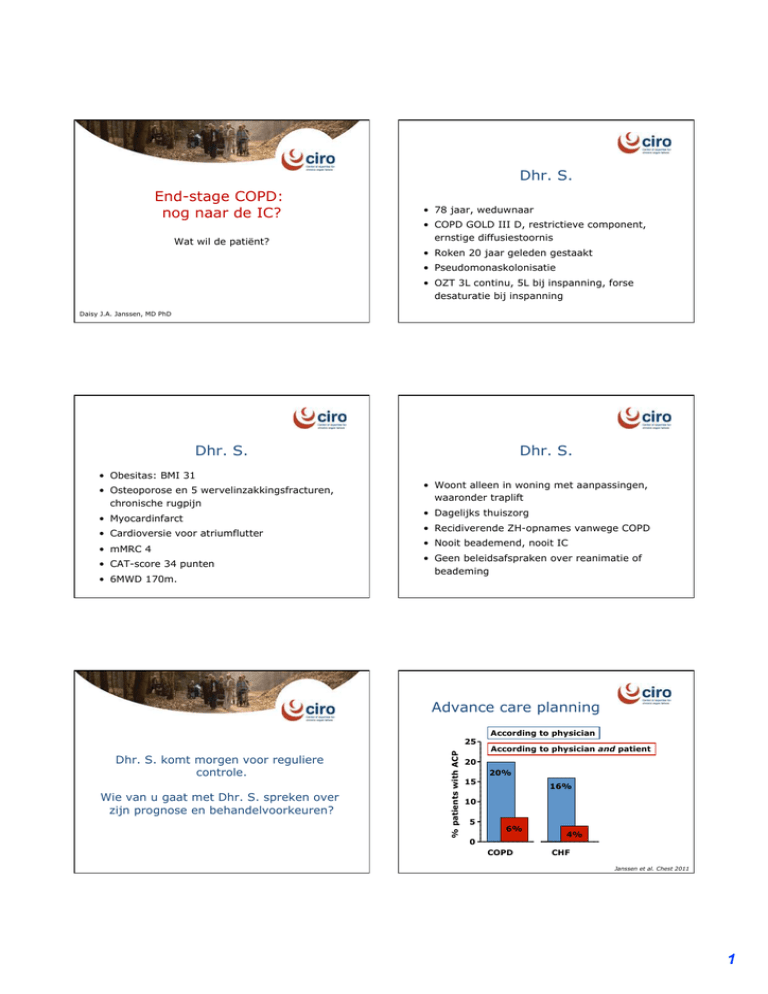
Dhr. S. End-stage COPD: nog naar de IC? Wat wil de patiënt? • 78 jaar, weduwnaar • COPD GOLD III D, restrictieve component, ernstige diffusiestoornis • Roken 20 jaar geleden gestaakt • Pseudomonaskolonisatie • OZT 3L continu, 5L bij inspanning, forse desaturatie bij inspanning Daisy J.A. Janssen, MD PhD Dhr. S. • Obesitas: BMI 31 • Osteoporose en 5 wervelinzakkingsfracturen, chronische rugpijn • Myocardinfarct • Cardioversie voor atriumflutter • mMRC 4 • CAT-score 34 punten • 6MWD 170m. Dhr. S. • Woont alleen in woning met aanpassingen, waaronder traplift • Dagelijks thuiszorg • Recidiverende ZH-opnames vanwege COPD • Nooit beademend, nooit IC • Geen beleidsafspraken over reanimatie of beademing Advance care planning Dhr. S. komt morgen voor reguliere controle. Wie van u gaat met Dhr. S. spreken over zijn prognose en behandelvoorkeuren? % patients with ACP 25 According to physician According to physician and patient 20 20% 15 16% 10 5 6% 0 COPD 4% CHF Janssen et al. Chest 2011 1 Advance care planning Planning for and about preference-sensitive decisions often arising at the end of life and implemented usually by means of effective patient–provider communication and education. • • • • • goals of care resuscitation and life support palliative care surrogate decision making living wills and medical directives Benefits ACP interventions • Increased completion of advance directives • Increased occurrence of end-of-life care discussions • Improved concordance between preferences for care and delivered care • May improve quality of communication Patel et al. Respirology 2011 Houben et al. JAMDA 2014 Dhr. S. • De volgende ochtend blijkt dhr. S. opgenomen met exacerbatie en toegenomen respiratoire insufficiëntie. • Arts-assistent heeft op SEH beleidsafspraken gemaakt: dhr. wenst volledig actief beleid Vindt u dat een wijs besluit? Welke informatie zou u meneer geven die hem kunnen helpen bij zijn besluitvorming? Preferences for mechanical ventilation Preferences for CPR 4% 2% 26% 28% yes yes 70% no 70% don't know n=105 Janssen et al. Chest. 2011 n=105 no don't know Janssen et al. Chest. 2011 2 Treatment preferences 1 week hospital Recovery 95% 1 month hospital Recovery 83% 1 week hospital 1 week hospital Bedbound 29% Memory loss 7% proportion choosing treatment (%) Treatment preferences 100 Low-burden, death 80 High-burden, death 60 Low-burden, functional impairment Low-burden, cognitive impairment 40 20 0 0 10 20 30 40 50 60 70 80 90 100 Likelihood of adverse outcome (%) Janssen et al. Chest 2011 Expectation patient survival inhospital CPR Janssen et al. Chest 2011 COPD patients discharged ICU n=126 COPD 46% first ICU admission Nava et al. Int J COPD 2008 12 months outcome ICU COPD 23% died in hospital Dhr. S. • Dhr. herstelt en wordt weer naar huis ontslagen 4791 patients LTOT 45% died in subsequent 12 months Schmidt et al. Crit Care Med 2014 67% readmitted within 12 months 40% of 3177 pts nursing home within 12 months • Tijdens een polibezoek wilt u nogmaals met meneer zijn behandelvoorkeuren bespreken, in aanwezigheid van zijn zoon. Hajizadeh et al. Thorax 2014 3 Patients’ wishes for ACP • • • • Little previous discussion with HCP about COPD. All aware of progressive and fatal nature. Consultations with HCP focused on the present. Most participants wanted more information about how their disease would progress, and more discussion about the future. • Difficult to raise these discussions themselves, despite wanting to. Hoe begint u dit gesprek? MacPherson et al. Palliat Med 2013 Understanding of Illness Advance care planning What do you think will happen Think about the last time your COPD got so bad that to you as a result of your COPD you had trouble breathing. in the future? If you were in this situation again, what would you hope for? What would you be most worried about? What are your biggest hopes? What are your greatest fears? Fried et al. JAMA 2012 Advance care planning Some patients say that if they became so sick that they could not recognize or talk to their loved ones, they would still want all possible treatments to prolong their life. Other patients say they would rather have care focused on comfort. Fried et al. JAMA 2012 Dhr. S. • Er wordt een NRNB-beleid afgesproken, wel bipap. • Meneer is een tijd stabiel • Wel achteruitgang mobiliteit • 6 maanden later polibezoek Which kind of person are you? Fried et al. JAMA 2012 4 Stability of preferences for CPR 13% Bespreekt u opnieuw behandelvoorkeuren? 11% no change decreased willingness 62% 14% increased willingness variable preference Janssen et al. Chest 2012 Dhr. S. Δ Δ Δ Δ Δ Health status Depression Anxiety Marital status Mobility • Enkele maanden later wordt meneer opnieuw opgenomen • Respiratoir insufficiënt • SEH, verlaagd bewustzijn, gesprek niet mogelijk • Zoon is erbij aanwezig Patients’ wishes for ACP Komt u met de zoon nog terug op de gemaakte beleidsafspraken? • Participants wanted to be involved in decisions about their treatment and to discuss treatment options. • Participants did not want HCP to make decisions based on previously stated preferences without reviewing those preferences with them and their family in the immediate circumstance those decisions apply to. MacPherson et al. Palliat Med 2013 5 ACP objective Take home messages To have patients make treatment decisions in advance so that clinicians can attempt to provide care consistent with their goals. • Advance care planning improves outcomes for The preparation of patients and surrogates to participate with clinicians in making the best possible in-the-moment medical decisions. patients and loved ones • Complexity of decision-making • Changes in preferences Sudore et al. Ann Intern Med 2010 6