Edematous states & Diuretics
advertisement

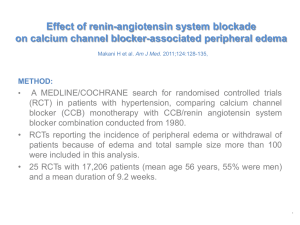
Edematous states & Diuretics • 2 basic steps in edema formation – – • • Alteration in capillary haemodynamics that favors the movement of fluid from the vascular space to the interstitium Dietary Na & water are retained by the kidney Major causes of edematous states Increased capillary hydrolic pressure – Increased plasma volume due to renal Na retention: • • heart failure Primary Na retention – – – – • • – Protein loss: nephrotic syndrome, protein losing enteropathyu Reduced albumin synthesis: liver disease, malnutrition Increased capillary permeability – • CCB, idiopathic edema Decreased oncotic pressure (alb<1.5-2mg/dl) – – • Hepatic venous obstruction, hepatic cirrhosis, Acute pulmonary edema, Local venous obstruction Decreased arteriolar resistance • • Pregnancy Idiopathic edema, when diuretic induced Venous obstruction • • – Renal ds incl. NS Drugs: minoxidil, CCB, diazoxide, NSAIDS, fludrocortisone, estrogen Refeeeding edema Early hepatic cirrhosis Idiopathic edema, burns, trauma, inflammation / sepsis, allergic reactions, ARDS, DM, IL2-therapy, malignant ascites Lymphatic obstruction / increased interstitial oncotic pressure – – Nodal enlargement due to malignancy Hypothyroidism, malignant ascites • Renal sodium retention – Inability to excrete the Na & water that has been ingested – patients with renal disease. – Appropriate compensatory response to effective circulating volume depletion, with urine [Na]<25 meq/L • The compensated state – Initial fluid retention has increased venous return to the heart, allowing systemic hemodynamics to be stabilized, and removing the stimulus for continued renin release – noremalization of BP, renin, aldosterone, urine [Na] secretion Intrarenal factors • Reflex activation of the sympathetic nervous system • Activation of RAAS and ADH • Resistance to the action of natriuretic peptides • Altered glomerular haemodynamics • Peritubular forces in PT General principles of treatment • When must edema be treated? – Pulmonary edema is life threatening and demands immediate treatment – Other edematous states, removal of fluid can proceed more slowly • What are the consequences of the removal of edema fluid? – Is the retention of Na & water a compensatory response or inappropriate primary Na retention? – If retention of edema fluid is compensatory then removal of this fluid with diuretics should diminish the effective circulating volume.- decrease in venous return to the heart, and cardiac filling pressures – fall in cardiac output – Leads to increased secretion of the hypovolemic hormones: renin, norepinephrine, ADH. – Most patients will benefit from the appropriate use of diuretics – Adequacy of tissue perfusion can be estimated by monitoring BUN & plasma [Cr] – as long as these parameters remain constant, it can be assumed that diuretic therapy has not led to a significant impairment in perfusion to the kidney or, therefore, to other organs. • How rapidly should edema fluid be removed? – Fluid that is lost initially comes from the plasma; restoration of plasma volume is by mobilization of edema luid into the vascular space – In patients with generalized edema due t heart failure, nephrotic syndrome, or primary Na retention, the edema fluid can be mobilized rapidly, since most capillary beds are involved – Important exception is hepatic cirrhosis with ascites but no peripheral edema – only 500-750 ml/d can only be removed safely. • Congestive heart failure Cardiac dysfunction Cardiac output Renal Na & water Retention Blood volume venous pressure EDEMA HEPATIC CIRRHOSIS & ASCITES HEPATIC DISEASE UNDERFILLING Hypoalbuminemia Peripheral vasodilatation sinusoidal pressure Splanchnic pooling ASCITES Effective Circ Volume Renal Na & Water retention FURTHER ASCITES OVERFLOW Renal Na & Water retention Plasma volume ASCITES Primary renal Na retention RENAL Na RETENTION Plasma volume Capillary hydraulic pressure EDEMA Pathogenesis of edema in primary renal Na retention, which is most often due to glomerular disease, advanced renal failure, Or the use of potent vasodilators in the treatment of hypertension. • Drugs; – direct vasodilators, minoxidil, diazoxide – CCB, dehydropyridines • Pregnancy; – normal pregnancy is associated with retention of 1000meq Na and 6-8L water • Refeeding edema – Insulin directly stimulates Na reabsorption in PT & perhaps in the loop of Henle & DT • Nephrotic syndrome • Idiopathic edema; – in young menstruating women – May represent a capillary leak syndrome – Dopamine deficiency & impaired hypothalamic function • Diuretic induced edema – Chronic use of diuretics activates Na retaining mechanisms DIURETICS Site of action Carrier/channel inhibited mechanism % filtered Na excreted Proximal Tubule Acetazolamide inhibits Enz. Carbonic Anhydrase prevent NaHCO3 reabsorption modest Loop of Henle Furosemide Bumetamide Ethacrinic acid Na – K - 2Cl carrier up to 25% Distal tubule & Connecting segment Thiazides Chlortalidon Metalazone Na – Cl Carrier up to 3 – 5% Cortical collecting tubule Spironolactone Amiloride Triamterene Na Channel up to 1 – 2% blocks aldosterone receptor in cytoplasm especially with thiazides Other effects • Loop diuretics – – – • Thiazide type diuretic – – – • Aldosterone sensitive Na – channel Can lead to hyperkalemia and metabolic acidosis Trimetoprim at very high doses Amiloride in the treatment of lithium induced nephrogenic DI Triamterene is a potential nephotoxin; crystalluria, cast formation, triamterene stones Acetazolamide – – • DT is major site of active Ca reabsorption, independent of Na transport Increase reabsorption of Ca, similar response occurs in the cortical collecting tubule with amiloride Useful in treatment of kidney stones due to hypercalciuria K-sparing diuretics – – – – – • Ca reabsorption in the loop of henle is primarily passive, driven by gradient created by NaCl transport Increase Ca excretion Treatment of hypercalcemia; NaCl solution & loop diuretic Net diuresis is modest; reclaimed in the more distal segments, diuretic action limited by the metabolic acidosis Major indication: as a diuretic in edematous patients with metabolic alkalosis Mannitol – – – Osmotic diuretic, inhibiting Na & water reabsorption in PT, loop of Henle Produces a relative water diuresis, water is lost > Na & K Can cause increase in plasma osmolality;- can lead to water deficit and hypernatremia, hypertonic mannitol may be retained in patients with renal failure Determinants of diuretic response • Site of action of the diuretic • Presence of counterbalancing antinatriuretic forces, AII, hypotension. • Rate of drug excretion – Most diuretics, particularly the loop diuretics, are highly protein bound – Are poorly filtered, and enter the urine primarily via the organic – anion/cation secretory pump in PT – Their ability to inhibit Na reabsorption is in part dose dependent • The natriuretic response tends to plateau at higher rates of diuretic secretion General guidelines • Use the minimum effective dose • Use for as short a period of time as necessary • Monitor regularly for adverse effects • Use only for appropriate conditions