Prototype drug - Nursing Pharmacology
advertisement

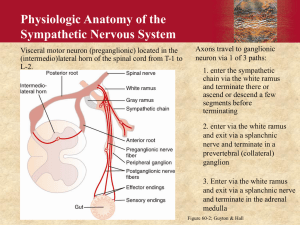
The Autonomic Nervous System (Ch 13) Two Major Divisions of the Nervous System Central Nervous System (CNS) Brain and spinal cord Peripheral Nervous System all nervous tissue outside the CNS, including sensory and motor neurons Basic Functions of the Nervous System Recognizing changes in Internal environment External environment Processing and integrating environmental changes Reacting to environmental changes by producing and action or response Figure 13.1 Functional divisions of the peripheral nervous system. Divisions of the Peripheral Nervous System Somatic nervous system Voluntary control over skeletal muscles Autonomic nervous system Involuntary control over smooth and cardiac muscle and glands Autonomic Nervous System: Sympathetic Nervous System Activated under stress Fight-or-flight response Ready the body for an immediate response to a potential threat Autonomic Nervous System: Parasympathetic Nervous System Activated under nonstressful conditions Rest-and-digest response Digestive processes promoted, heart rate and blood pressure decline Autonomic Nervous System: Sympathetic and Parasympathetic Divisions Branches produce mostly opposite effects Homeostasis – proper balance of the two branches achieved by changing one or both branches Branches do not always produce opposite effects Figure 13.2 Effects of the sympathetic and parasympathetic nervous systems. Source: Biology Guide to the Natural World, 2nd ed (p. 558) by David Krogh, 2002 Upper Saddle River, NJ, Prentice Hall. Reprinted by permission. Synaptic Transmission Synapse – juncture of neurons Connection of two neurons outside CNS – ganglionic synapse Preganglionic neuron Postganglionic neuron Many drugs affect autonomic function by altering neurotransmitter activity at the second synapse Five Mechanisms by Which Drugs Can Affect Synaptic Transmission 1. Affect the synthesis of the neurotransmitter in the presynaptic nerve 2. Prevent storage of the neurotransmitter in vesicles within the presynaptic nerve 3. Influence release of the neurotransmitter from the presynaptic nerve 4. Prevent the normal destruction or reuptake of the neurotransmitter 5. Bind to the receptor site on the postsynaptic target tissue Drugs Not Given to Correct Autonomic Nervous System System is relatively free of disease Drugs used to stimulate or inhibit target organs of the autonomic nervous system Figure 13.3 Basic structure of the autonomic pathway. Figure 13.4 Receptors in the autonomic nervous system: (a) sympathetic division; (b) parasympathetic division Primary Neurotransmitters of Autonomic Nervous System Norepinephrine (NE) Acetylcholine (Ach) Norepinephrine Released by most postganglionic nerves Class of agents called natural catecholamines, all involved in neurotransmission Adrenergic receptors - receptors at the ends of postganglionic sympathetic neurons Two Types of Adrenergic Receptors Alpha-receptors and Beta-receptors Hugely important to pharmacology Drugs are selective and activate only one type of adrenergic receptor, whereas others affect all receptor subtypes Alpha1-adrenergic Receptors In all sympathetic target organs except heart Response Constriction of blood vessels Dilation of pupils Alpha2-adrenergic Receptors At presynaptic adrenergic neuron terminals Activation inhibits release of norepinephrine Beta1-adrenergic Receptors In heart and kidneys Response Activation increases heart rate and force of contraction of heart. Increases release of renin Beta2-adrenergic Receptors In all sympathetic target organs except the heart Inhibit smooth muscle Prototype Drug: Phenylephrine (Neo-Synephrine) Prototype Drug: Phenylephrine (Neo-Synephrine) Norepinephrine (NE) is synthesized In the nerve terminal Requires the amino acids phenylalanine and tyrosine Conversion of dopamine to norepinephrine NE in nerve terminal may be returned to vesicles for future use, or destroyed enzymatically by monoamine oxidase Adrenal Medulla Anatomic and physiologic arrangement much different from rest of sympathetic branch Other types of adrenergic receptors Dopamine serves a larger role as a neurotransmitter Acetylcholine Released by cholinergic nerves Two types cholinergic receptors Muscarinic receptors Nicotinic receptors Nicotinic Receptors In sympathetic and parasympathetic divisions at the ganglionic synapse Response Stimulate smooth muscle Stimulate gland secretion Muscarinic Receptors In parasympathetic target organs except the heart Response Stimulate smooth muscle Stimulate gland secretion In heart: decreased heart rate and force of contraction Physiology of Acetylcholine Affords several mechanisms by which drugs may act Synthesized in presynaptic nerve terminal from choline and acetyl coenzyme A Ach in the synaptic cleft is rapidly destroyed by the enzyme acetylcholinesterase (AchE) Classification and Naming of Autonomic Drugs Based on four possible actions of sympathetic and parasympathetic nervous systems Stimulate sympathetic nervous system Adrenergic agents or sympathomimetics Inhibit sympathetic nervous system Adrenergic-blocking agents, adrenergic antagonists, or sympatholytics Classification and Naming of Autonomic Drugs (cont'd) Stimulate parasympathetic nervous system Cholinergic agents or parasympathomimetics Inhibit parasympathetic nervous system Cholinergic-blocking agents, anticholinergics, parasympatholytics, or muscarinic blockers One of Four Drug Classes is Most Important to Learn If the fight-or-flight actions of the sympathomimetics are learned, the other three groups can be deduced Mastering the actions and terminology of autonomic drugs early will pay dividends later Role of Nurse Monitor patient’s condition Provide education on drug therapy Note adverse effects of drug therapy Identify possible interactions Identify contraindications of drug therapy Sympathomimetic Monitor vital signs, urinary and cardiac output as appropriate Monitor breathing patterns Observe patient’s responsiveness to light Monitor for rhinorrhea and epistaxis Nursing Process Focus: Patients Receiving Adrenergic (Sympathomimetic Therapy) Nursing Process Focus: Patients Receiving Adrenergic (Sympathomimetic Therapy) Nursing Process Focus: Patients Receiving Adrenergic (Sympathomimetic Therapy) Nursing Process Focus: Patients Receiving Adrenergic (Sympathomimetic Therapy) Anticholinergics Monitor for signs of anticholinergic crisis Report changes in heart rate, blood pressure, or development of dysrhythmias Provide comfort measures for dry mouth Anticholinergic (cont'd) Minimize exposure to heat or cold or strenuous exercise Monitor intake and output Monitor patient for abdominal distension, and auscultate for bowel sounds Nursing Process Focus: Patients Receiving Anticholinergic Therapy Nursing Process Focus: Patients Receiving Anticholinergic Therapy Nursing Process Focus: Patients Receiving Anticholinergic Therapy Nursing Process Focus: Patients Receiving Anticholinergic Therapy Adrenergic Blockers Monitor urinary hesitancy, incomplete bladder emptying, interrupted urinary stream Monitor vital signs, level of consciousness, and mood Monitor for dizziness, drowsiness, or lightheadedness Observe for side effects Monitor cardiac output Nursing Process Focus: Patients Receiving Adrenergic-Blocker Therapy Nursing Process Focus: Patients Receiving Adrenergic-Blocker Therapy Nursing Process Focus: Patients Receiving Adrenergic-Blocker Therapy Nursing Process Focus: Patients Receiving Adrenergic-Blocker Therapy Parasympathomimetics Monitor for adverse effects Monitor liver enzymes Calculate and monitor doses Assess and monitor for appropriate self-care administration Direct Acting Monitor intake and output ratio Monitor for blurred vision Monitor for orthostatic hypotension Cholinesterase Inhibitors Monitor muscle strength and neuromuscular status Monitor ptosis, diplopia, and chewing Schedule medication around mealtimes Schedule activities to avoid fatigue Monitor for muscle weakness Nursing Process Focus: Patients Receiving Parasymptathomimetic Therapy Nursing Process Focus: Patients Receiving Parasymptathomimetic Therapy Nursing Process Focus: Patients Receiving Parasymptathomimetic Therapy Nursing Process Focus: Patients Receiving Parasymptathomimetic Therapy Nursing Process Focus: Patients Receiving Parasymptathomimetic Therapy Adrenergic Agents (Sympathomimetics) Prototype drug: phenylephrine (Neo- Synephrine) Mechanism of action: to stimulate the sympathetic nervous system directly/indirectly produce many of the same responses as the anticholinergics Adrenergic Agents (Sympathomimetics) (cont'd) Primary use: depends on receptors activated Alpha1-receptors: nasal congestion, hypotension, dilation of pupils for eye examination Alpha2-receptors: hypertension Beta1-receptors: cardiac arrest, heart failure, shock Beta2-receptors: asthma and premature-labor contractions Adrenergic Agents (Sympathomimetics) (cont'd) Adverse effects: tachycardia, hypertension, dysrhythmias, CNS excitation and seizures, dry mouth, nausea and vomiting, anorexia Adrenergic-Blocking Agents Prototype drug: prazosin (Minipress) Mechanism of action: to inhibit the sympathetic nervous system Primary use: hypertension, dysrhythmias, angina, heart failure, benign prostatic hypertrophy, narrow-angle glaucoma Adverse effects: dizziness, drowsiness, headache, loss of energy and strength, palpitations, dry mouth Prototype Drug: Prazosin (Minipress) Adrenergic-Blocking Agents Primary use of beta blockers is in the treatment of hypertension Beta-adrenergic antagonists have several other important therapeutic applications angina pectoris Migranes Heart failure Cholinergic Agents (Parasympathomimetic) Prototype drug: bethanechol (Urecholine) Mechanism of action: to activate the parasympathetic nervous system directly/indirectly, induce rest/digest response Uses: glaucoma, urinary retention, myasthenia gravis, Alzheimer’s disease Adverse effects: profuse salivation, sweating increased muscle tone, urinary frequency, bradycardia Prototype Drug: Bethanechol (Duvoid,Urecholine) Cholinergic Agents (Parasympathomimetic) Divided into two classes direct acting bind to cholinergic receptors to produce the rest-and-digest response indirect acting inhibit the action of AchE High potential for serious adverse effects Cholinergic-Blocking Agents Prototype drug: atropine (Atropair, Atropisol) Mechanism of action: to inhibit the parasympathetic nervous system Primary use: peptic ulcers, irritable bowel syndrome, mydriasis and cycloplegia during eye examination, bradycardia, preanesthetic, asthma Adverse effects: tachycardia, CNS stimulation, urinary retention, dry mouth, dry eyes, decreased sweating, photophobia Prototype Drug: Atropine (Atro-Pen, Atropair,Atropisol) Prototype Drug: Atropine (Atro-Pen, Atropair,Atropisol) Drugs Affecting the Autonomic Nervous System Assessment Potential nursing diagnoses Reason for drug Monitoring vital signs Doing complete health history Drugs Affecting the Autonomic Nervous System (cont'd) Cautions and contraindications for drug Allergies Drug history Possible drug interactions Evaluating lab findings Assess for therapeutics effect Watch for adverse effects Drugs Affecting the Autonomic Nervous System (cont'd) Nursing Diagnosis Knowledge deficient, related to drug therapy Risk for injury, related to side effect of drug therapy Disturbed sleep pattern Drugs Affecting the Autonomic Nervous System (cont'd) Planning Patient will exhibit therapeutic outcome based on specific drug Patient will demonstrate an understanding of drug’s activity Patient will accurately describe drug side effects and precautions Patient will demonstrate proper administration technique Drugs Affecting the Autonomic Nervous System (cont'd) Implementation Administration of drug Observing for adverse effects Patient education/discharge planning Providing additional information as needed to encourage compliance Doing home-health visits Drugs Affecting the Autonomic Nervous System (cont'd) Evaluation Evaluating effectiveness of drug therapy Confirming that patient goals and expected outcomes have been met NCLEX-RN Review Question 1 1. Following administration of an adrenergic (sympathomimetic) drug, the nurse would assess for which adverse drug effects? 1. 2. 3. 4. Insomnia, nervousness, and hypertension Nausea, vomiting, and hypotension Nervousness, drowsiness, and dyspnea Bronchial dilation, hypotension, and bradycardia NCLEX-RN Review Question 1 – Rationale Rationale: Adrenergic agonists stimulate the sympathetic nervous system and produce symptoms of the fight-or-flight response. Nausea, vomiting, nervousness, bronchial dilation, and hypertension are potential adverse reactions related to the use of adrenergic agonists. Hypotension is a potential adverse reaction related to the use of adrenergic antagonists. NCLEX-RN Review Question 2 2. Adrenergic-blocking (antagonist) drugs may include all of the following adverse reactions except: 1. 2. 3. 4. Bronchodilation Tachycardia Edema Heart failure NCLEX-RN Review Question 2 – Rationale Rationale: Potential adverse reactions associated with the use of adrenergic antagonists include tachycardia, edema, and heart failure. Bronchodilation is associated with the use of adrenergic agonists. Cognitive Level: Analysis Nursing Process: Assessment Patient Need: Physiological Integrity NCLEX-RN Review Question 3 3. Elderly patients taking bethanechol (Urecholine) need to be assessed more frequently because of which of the following side effects? 1. 2. 3. 4. Diaphoresis Hypertension Dizziness Urinary retention NCLEX-RN Review Question 3 – Rationale Rationale: The nurse should monitor elderly patients for episodes of dizziness caused by CNS stimulation from the parasympathomimetic. Diaphoresis and dizziness are potential side effects related to the use of bethanechol. Bethanechol is used to treat nonobstructive urinary retention. Cognitive Level: Application Nursing Process: Implementation Patient Need: Physiological Integrity NCLEX-RN Review Question 4 4. The patient taking benztropine (Cogentin) should be assessed for: 1. 2. 3. 4. Heartburn Constipation Hypothermia Increased gastric motility NCLEX-RN Review Question 4 – Rationale Rationale: Anticholinergic medications slow intestinal motility; therefore, constipation is a potential side effect. Heartburn and hypothermia are not associated with the use of benztropine. Cognitive Level: Application Nursing Process: Assessment Patient Need: Physiological Integrity NCLEX-RN Review Question 5 5. The patient taking tacrine (Cognex) should be observant for which of the following adverse effects that may signal a possible overdose has occurred? 1. 2. 3. 4. Excessive sweating, salivation, and drooling Extreme constipation Hypertension and tachycardia Excessively dry eyes and reddened sclera NCLEX-RN Review Question 5 – Rationale Rationale: Overdosage of parasympathomimetics (cholinesterase inhibitors) may produce excessive sweating, drooling, dyspnea, or excessive fatigue. These symptoms should be promptly reported. Cognitive Level: Comprehension Nursing Process: Assessment Patient Need: Physiological Integrity