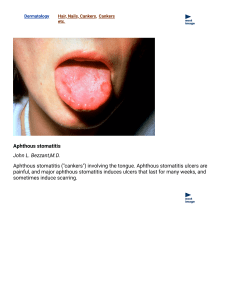
Apthous Ulcer - UCLA Oral Medicine
advertisement

Oral Medicine Block Presentation: Aphthous Ulcers Submitted by Rita Chen Diana Craft Sujain Dissanayake Neil Patel Asha Sethu Madhavan Aphthous Ulcers Pathogenesis • Recurrent aphthous stomatitis (RAS) is a chronic inflammatory disease with evidence of an inappropriate innate immune response. The stages in which it progresses: *Preulcerative stage T-lymphocytic infiltrate into epithilium. Cytokines involved: TNF-a, IL-2,IL-10. *Papular swelling with erythematous halo Localized keratinocyte vacuolization with surrounding vasculitis. Pathogenesis *Ulceration Papular ulceration, covered by a fibrinous exudate. *Healing with epithelial regeneration. Although the exact cause for the exaggerated immune response Is not known, there are a few known predisposing/precipitating factors. Pathogenesis: Predisposing/Precipitating Factors *Heredity -42% of patients have +ve family history. -90 of likelihood of developing lesions when both parents affected. *Psychologic factors Stress and anxiety been implicated in development of aphthous ulcers. *Mechanical trauma Pathogenesis *Endocrine Association of RAS with the menstrual cycle, pregnancy, use of oral contraceptives - suggest a possible relation to hormonal imbalance. *Systemic Conditions -Behçet syndrome -Crohn disease -Immune disturbances (HIV, cyclic neutropenia), Viral infection (HSV1) -Drug exposure (NSAIDs, alendronate, nicorandil) Pathogenesis *Dietary deficiencies Iron, folate or vit B12 deficiency in patients increases chances of developing aphthae (replacement therapy often improves the condition). *Allergy Patients with known allergy could benefit from avoiding the allergen. -Common kinds of foods that are potential allergens: milk, cheese, nuts, flour, tomatoes, citrus fruits, shellfish. -Cinnamic aldehyde: artificial cinnamon flavoring -Sodium lauryl sulfate present in toothpaste. Aphthous Ulcers Clinical Presentation – Painful open sores inside the mouth caused by a break in the mucuous membrane – Typically white color / erythematous around lesion. Clinical Presentation 4 Types: • Recurrent Aphthous Stomatitis (aka Sutton’s Disease) • Minor aphthous ulcerations – most common / least severe • Major aphthous ulcerations – greater than 10mm in size • Herpetiform aphthous ulcerations – most severe form Clinical Presentation • Minor Aphthous Ulcers – Occur in childhood / adolescence – Exclusively on non-keratinized mucosa (floor of mouth, buccal mucosa, soft palate) – Usually yellow-grey in color with erythematous halo less than 10 mm around it • Herpetiform aphthous ulcerations – Occurs frequently in females – Onset usually in adulthood – Small numerous lesions of 1 – 3 mm in clusters Clinical Presentation • Major Aphthous Ulcers – Typically up to 10 mm in size – Painful and typically leave a scar – Take up to 1 month to heal • Recurrent Aphthous Stomatitis – Typically occurs in 10% of the population Aphthous Ulcers Diagnostic Tests Diagnosis of aphthous ulcers is usually based on clinical signs and symptoms. There are tests which may be ordered to rule out other ulcer etiologies: r/o nutritional deficiency of vit B12, folate, iron r/o herpetic stomatitis with cytology smear (-) for cytopathic effects, (-) viral culture/ immunofluoresence r/o HIV for large, slow-healing ulcers Diagnostic Tests • r/o cancer for non-healing ulcer with biopsy • r/o Crohn disease with biopsy (+) for characteristic granulomatous inflammation • r/o Behçet syndrome- presence of anogenital or ocular lesions, arthralgia, skin, vascular or neurological involvement • r/o cyclic neutropenia with CBC • r/o possible drug reaction due to cytopathic drug therapies Aphthous Ulcers Histologic Appearance • Aphthous Minor – Fibrinopurulent exudate overlying granulation tissue consisting of many neutrophils, macrophages, and plasma cells. Mast cells and eosinophils are few. • Aphthous Major – Same as aphthous minor, plus perivascular lymphocyte infiltration. Inflammation goes deep into underlying connective tissue (CT). CT destruction heavy scar tissue formed upon healing. • Herpetiform Ulcers – Identical to Aphthous Minor, shallow little CT destruction no scarring. • Behçet Syndrome – Similar to aphthous minor, plus severe vasculitis: destruction of blood vessel walls due to inflammatory cell infiltrates. Histologic Appearance: Aphthous ulcer biopsy *Inflammation accompanies ulceration: an area of epithelial degeneration. *A diagnosis of aphthous ulcer cannot be based on histological findings alone. *The dark line on right traces the basement membrane outlining intact epithelium. Differential Diagnosis of Aphthous Ulcers • Infection: HSV, CMV, HIV, Coxsackie virus, syphilis, histoplasmosis • Autoimmune: Behcet’s disease, SLE, Crohn’s disease, bullous pemphigoid, pemphigous vulgaris, cicatricial pemphigoid, erythema multiforme. • Neoplasms: squamous cell carcinoma. • Medications: methotrexate, chemotherapy. • Poor nutrition: including vitamin deficiencies. Treatment of Aphthous Ulcers 1. Early treatment/avoidance of triggers: • • • Data support that early treatment promotes more rapid healing.1 Topical anesthetics including triamcinolone in orabase, fluocinonide gel in orabase. Identify and avoid triggers (physical trauma, emotional stress, food hypersensitivity like chocolate, sodium lauryl sulfate, menstrual cycle association). 1. Oral Lesions Goldstein, Beth MD. UpToDate.com Treatment of Aphthous Ulcers cont’d 2 2. Supportive Care • Symptomatic relief – Anesthetics – • • OTC Benzocaine Compound anesthetics • Viscous lidocaine Covering agents/Compound agents • • • Kaolin and Pectin 5% amlexanox 1:1:1 solution of Milk of Magnesia + Benadryl + Viscous lidocaine OTC Treatment of Aphthous Ulcers • Herbal remedies -Example: rock rose, 1:1 sage + chamomile mouthwash, echinacea. • Cleansing agents -Example: hydrogen peroxide • Toothpaste without sodium lauryl sulfate • Vitamins/dietary supplements: vitamin B, vitamin C, zinc lozenges, L-lysine tablets. 2. Dr. Younai’s lecture on Immunosurpressive therapeutics. Treatment of Aphthous Ulcers in Autoimmune Disease (Behcet’s, Crohn’s disease) • Local treatment: same as for other conditions with focus on symptom relief. Topical tetracycline mouthwash may be of benefit in patient’s with Behcet’s disease, although this may cause staining of teeth. • Systemic treatment: includes steroids, and immune modulators including cyclophosphamide, azathioprine, thalidomide, and cyclosporine. Treatment of Aphthous Major • Emphasize on the combined use of short-term systemic drugs and topical steroids – Systemic: thalidomide (200 mg daily x4 weeks) has been studied in HIV positive patients who have severe recurrent aphthous stomatitis and has been shown to improve the chance of healing4. However, recurrence of ulcers is common after stopping treatment. – Topical steroids: • Ex: Triamcinolone. • Antimicrobial rinses to reduce secondary infection. -- Ex: Chlorhexidine gluconate • Anti-inflammatory agents including 5% amlexanox. • Topical anesthetic to allow for eating3. 3. Contemporary oral and maxillofacial pathology 4. N. Engl. J. Med 1997; 336: 1487 . 2nd Editon J. Philip Sapp References • www.med.ucla.edu/modules/wfsection/article.php (UCLA Dept. of Medicine 2004) • Sapp J, Eversole L., Wysocki G. Contemporary Oral and Maxillofacial Pathology. Mosby Inc. 2004. 2nd edition. • Burket's Oral Medicine,Diagnosis and Treatment • Shafer's Textbook of Oral Pathology • Wikipedia.org • Young, Stephen K. Canker Sores & Cold Sores: What's the Difference. Continuing Education. University of Oklahoma College of Dentistry. Retrieved on 2006 August 22. • Goldstein, Beth MD. “Oral Lesions” UpToDate.com • Dr. Younai’s lecture on Immunosupressive Therapeutics • http://www.dentistry.ubc.ca/research/priddy/HTMLS/MIC1RAU.HTM QUESTIONS • Which test can provide a specific diagnosis of aphthous ulcer? a. immunofluorescence b. acid/base test c. brush biopsy d. there is no specific diagnostic test for aphthous ulcer • What is the most common form of aphthous ulcers? a. Recurrent Aphthous Stomatitis (aka Sutton’s Disease) b. Minor aphthous ulcerations c. Major aphthous ulcerations d. Herpetiform aphthous ulcerations