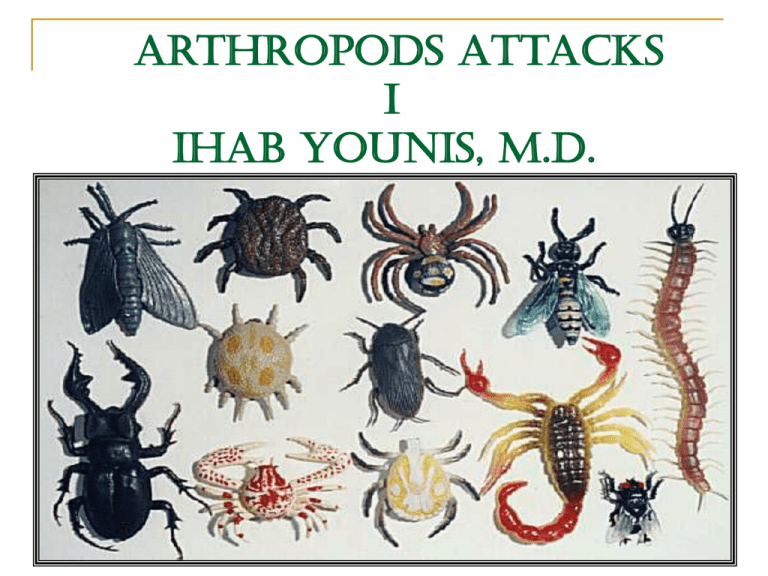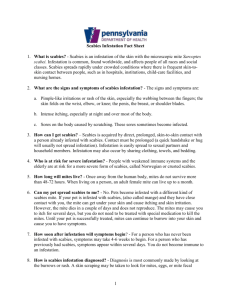
Arthropods Attacks
I
IHAB YOUNIS, M.D.
Scabies
Etymology: L. [scabo,] to scratch
History
" The seven year itch" was first used with
reference to persistent,undiagnosed
infestationswith scabies
Scabies has been reported for more than
2500 years
Aristotle discussed “lice in the flesh”
Celsus recommended sulfur mixed with liquid
pitch as a remedy for the disease
The disease was first ascribed to the mite by
Bonomo in 1687
It was the first human disease recognized to
be caused by a specific pathogen
Etiology
About 300 million cases occur annually
Prevalence is higher in children and sexually
active individuals
It affects persons of all ages, races, and
socioeconomic groups
Causative agent
The Female Gravid
Sarcoptes scabiei mite,
var hominis
G: sarx (the flesh) and
koptein (to cut)
Life cycle
The entire life cycle of the mite lasts 30 days
and is spent within the human epidermis
After copulation, the male mite dies and the
female mite burrows into the superficial skin
layers and lays a total of 60-90 eggs
The ova require 10 days to progress through
larval and nymph stages to become mature
adult mites
Mites can survive up to 3 days away from
human skin, so fomites such as infested
bedding or clothing are an alternate but
infrequent source of transmission
Mites move through the top layers of skin by
secreting proteases that degrade the stratum
corneum creating burrows
They feed on dissolved tissue but do not
ingest blood
An affected individual harbors a variable number
of living mites (10-15(
In immunocompromised hosts the number of
mites can exceed 1 million (crusted scabies)
Symptoms appear 2-6 weeks after infection as
delayed-type IV hypersensitivity reaction to the
mites, eggs, and scybala (packet of feces)
occurs
In reinfestation, the sensitized individual may
develop a reaction within hours
Mode of transmission
Epidemics or pandemics may occur in 30-year
cycles
Transmission is predominantly through direct
skin-to-skin contact(10 minutes)
Indirect contact through fomites such as
infested bedding or clothing is possible,
although not usual
Clinically
The history is very important
Intractable pruritus that is worse at night
Similar symptoms in close contacts
History of itching for a short time. On the other
hand, the infestation can persist indefinitely
Occurs more commonly in fall and winter
A short (2-3 mm), elevated, serpiginous , gray
brown track in the superficial epidermis,
known as a burrow, is pathognomonic
Occasionally, the mite
is visible to the naked
eye as a small white dot
A small vesicle or papule
may appear at the end of the burrow
Distribution
Any pruritic papule on
the penis or female
areola of breast
or palms & sole
of foot in an
infant is scabies
until proved
otherwise
Scabies in infants tends to be more
disseminated affecting head and face
Geriatric scabies demonstrates a propensity
for the back, often appearing as excoriations
One- to 3-mm erythematous papules and
vesicles are seen in typical distributions in
adults and most likely represent a
hypersensitivity reaction
In very young children and infants, a
widespread eczematous eruption primarily on
the trunk is common
Histopathology
If a burrow is excised,
mites, larvae, ova, and
feces may be identified
within the keratin
A superficial and deep
dermal infiltrate composed
of lymphocytes,
histiocytes, mast cells,
and eosinophils
Spongiosis and vesicle
formation with exocytosis
of eosinophils
Crusted scabies demonstrates massive
hyperkeratosis of the stratum corneum with
innumerable mites in all stages of
development
Psoriasiform hyperplasia of the underlying
epidermis with spongiotic foci and occasional
epidermal microabscesses is present
Types
1-Crusted Scabies (Norwegian):
First described in 1848 by Danielssen and
Boeck, who considered the disease to be a
form of leprosy endemic to Norway
May occur in almost any area of the body
including the scalp
Occurs in immunocompromised persons and
in weak patients who can not scratch
Extensive, widespread, crusted lesions
appear with thick, hyperkeratotic scales over
the elbows, knees, palms, and soles
Itching is minimal
Serum IgE and IgG
levels are extremely
high
2-Animal scabies
is characterized by absence of burrows since
the animal mites cannot adapt themselves to
human skin
It is not transmitted from one human being to
another
3-Scabies in the clean
The disease is easily misdiagnosed because
lesions are sparse and burrows are difficult to
find
4-Scabies incognito
Topical or systemic steroids may mask
symptomsand signs of scabies, although the
infestation remains freely transmissible
This often results in unusual clinical
presentations such as atypical and wide
distribution
5-Nodular scabies
Reddish-brown,
pruritic nodules on
covered parts
(most frequently the
male genitalia, groin,
and axillary regions)
Probably represents
a hypersensitivity
reaction to retained
mite parts or antigens
6-Bullous scabies
May mimic bullous pemphigoid clinically,
pathologically, and immunopathologically
Most patients are over 65 years of age. The
duration of the scabies from onset until
diagnosis is weeks to months, thereby
exposing a number of individuals to the
disease
Burrows are present in most cases
complications
Secondary bacterial infection may occur
Nephritogenic
streptococcal
strains may
colonize
scabietic lesions,
leading to acute
glomerulonephritis
Eczema, particularly in atopics, may be
prominent in the active scabies and may
continue as eczema after the scabies has
cleared
Acarophobia
Immunology
Delayed:T-lymphocytes in inflammatory
lesions
High IgG, IgM and IgA returning to normal
after treatment
IgM and C3 deposits at the DE junction in
burrows
Lab tests
Skin scraping: Place a drop of mineral oil on
a glass slide, touch a No. 15 blade or a 7-mm
curette to the oil, and scrape infested skin
sites, preferably primary lesions such as
vesicles, juicy papules, and burrows
cover with a coverslip, and examine under a
light microscope at 40X magnification
Multiple scrapings may be required to identify
mites or their products. Persistence is key to
accurate diagnosis
Crusted scabies: Add 10% potassium
hydroxide (KOH) to the skin scraping. This
dissolves excess keratin and permits
adequate microscopic examination
Treatment
Permethrin cream 5% (Ectomethrine)
Causes respiratory paralysis of parasite
Recommended by CDC as first-line therapy
Apply from chin to toes and shower off 10-12 h
later; repeat in 1 wk
Not recommended for children <2 mo
C - Safety for use during pregnancy has not
been established
More effective than a single dose of oral
ivermectin, although it has equivalent efficacy
when 2 doses of ivermectin are used at time
zero and 2 weeks later
Lindane (Scabene)
Stimulates nervous system of parasite, causing
respiratory paralysis
Second-line treatment if other agents fail or are
not tolerated
Not very safe in children as transcutaneous
absorption leading to neurotoxicity
Apply thin layer from chin to toes; use on dry
skin and shower off 10 h later; repeat in 1 wk
Infants and children: Apply as adults but leave
on 6-8 h before washing off and do not exceed
30 g/application
Oil-based hairdressings may increase toxicity
Safety in pregnancy:B - Usually safe but
benefits must outweigh the risks
Sulfur in petrolatum (2 -10%, with 6%
)preferred
May be used safely without fear of toxicity in
very small children and in pregnant women
It is malodorous, stains clothes & requires
repeat applications, thus reducing compliance. It
can cause a dermatitis in hot and humid
climates
Apply to entire body below head on 3
successive nights and bathe 24 h after each
application
Crotamiton (Eurax)
Mechanism of action is unknown
Apply thin layer onto skin of entire body from
neck to toes; repeat in 24 h; take a cleansing
bath 48 h after last application
Do not apply to face, urethral meatus, eyes,
mucous membranes, or swollen skin; can
cause seizures
Benzyl benzoate(Benzanil)
Neurotoxic to mites
Use 25% emulsion; apply below neck 3 times
within 24 h without an intervening bath
Safety in pregnancy:X - Contraindicated in
pregnancy
May cause stinging, if so reduce
concentration
Ivermectin (Ivactin 6 mg tab)
Binds selectively with glutamate-gated
chloride ion channels in invertebrate nerve
and muscle cells, causing cell death
2 mg/10kg/d PO as single dose
May cause nausea, vomiting, and mild CNS
depression; may cause drowsiness
Pediculosis
Etymology: L. [pediculus] louse +
G. [-osis] condition
Types
Pediculosis capitis
Pediculosis corboris
Pediculosis pubis
Pediculosis capitis
Etiology
The disease is spread from person to person
by close physical contact or through fomites
(eg, combs, clothes, hats, linens)
Overcrowding encourages the spread of lice
Head lice are very rare among negros due to
the twisted nature of the hair shaft
Causative agent
Pediculus humanus capitis (head louse)
Lice are ectoparasites that feed on human
blood several times daily
They have claws on their legs that are
adapted for feeding and clinging to hair or
clothing
They move quickly(up to 23 cm/min) , which
explains their ease of transmission
A fertilized female louse lays about 10 eggs a
day for up to a month until it dies
The eggs (nits) are attached to the hair shaft,
close to the skin surface, where the
temperature is optimal for incubation
Nits are cemented to the hair shaft with chitin
and are very difficult to remove. Nits can
survive for up to 10 days away from the
human host
The eggs hatch in about 6-10 days
Lice develop into adults
in 19 to 25 days from the time the egg is laid
Live nits are fluorescent white when
illuminated with
a Wood’s lamp; empty
nits are fluorescent gray
Clinically
Itching is the most common symptom
Erythema and scaling may be present, as
well as pruritic papules on the posterior neck
There may be linear excoriations at the
periphery of the hair area which frequently
lead to pyoderma
Cervical lymphadenopathy and febrile
episodes are not uncommon
Pediculosis corporis
Etiology
Infestations of body lice are found mainly in
those with low income and poor hygiene, and
homeless persons and refugees living in
crowded conditions
The infestation is transmitted chiefly by
contaminated clothing or bedding
Causative agent
Pediculus humanus corporis (body louse)
It is similar to the head louse but a little larger
Body lice and their eggs are predominantly
found on clothing and should be looked for in
the seams of clothes
Early lesions consist of macules or papules at
the site where the louse punctures the skin to
obtain blood
The characteristic eruption consists of
numerous vertical excoriations, especially on
the trunk and neck, caused by intense itching
Crusts and at times pus or serum may stain
the underclothing
Transitory wheals and bacterial infections
may complicate the process
Postinflammatory pigmentation is common
Few or no adult organisms are seen except in
heavily infested persons
Nnumerous nits are found in clothing seams,
particularly in contact with the crotch, armpits,
belt line, and collar
Pediculosis pubis
Etiology
It is typically transmitted sexually, frequently
coexisting with other sexually transmitted
diseases
Pubic lice were found in 1.7% of men and
1.1% of women in an STDs clinic
Causative agent
Pthirus pubis (pubic or crab louse)
It is much shorter than other lice, being
almost as wide as it is long
Lice have three pairs of legs. In the crab
louse, the first set of legs terminates in a
slender claw, while the second and third pairs
have well-developed claws perfectly adapted
for grasping the coarse, widely spaced hairs
of the pubis
It is sluggish,
travelling a maximum
of 10 cm/day
Clinically
Pubic hair is the most common site
The crab louse is found firmly attached to
the base of the pubic hair. Nits may also
be found
Pubic lice may spread to hair around the
anus, abdomen, axillae, chest, and
eyelashes
Bluish grey macules, or maculae cerulea,
may be seen on the abdomen or thighs
and are secondary
Diseases transmitted by lice
Typhus: Caused by Rickettsia prowazekii
high fever, petechial rash,CNS involvement
Trench fever: Caued by Bartonella quintana
fever similar to typhus, infective endocarditis
Relapsing fever: Caused by the spirochete
Borrelia recurrentis
relapsing fever,rash
Treatment
General measures
Nits are best removed with a very fine comb
Soaking the hair in a solution of equal parts
water and white vinegar and then wrapping
the wet scalp in a towel for at least 15
minutes may facilitate removal
Treat all family members
Discard infested clothing or wash in very hot
water
Shaving of the scalp or body hair eradicates
lice; if cosmetically acceptable by the patient
Wet combing or application of diluted vinegar
or commercial preparations of 8% formic acid
may help in the removal of nits or at least
make the combing easier. Plastic or the
sturdier metal nit combs may be used
Multiple lice suffocation agents have been
advocated, but most have not been
scientifically evaluated. These include
Vaseline; petroleum jelly; oils; mayonnaise
Drug therapy
Treatment should be repeated in 7-10 days
(the time needed for the eggs to hatch)
because nits are less effectively killed than
adults
All contacts should be treated simultaneously
Resistance to pediculicides has increased
over recent years. Therapeutic agents can be
rotated to slow the emergence
Same drugs as for scabies but:
Permethrin 5% :leave 5-10 min, then rinse
Lindane 1% shampoo: Apply to dry head or
pubic hair and surrounding areas; allow to set
for 4 min, then lather for 4 min and rinse;
repeat in 7 d prn
Malathion (Prioderm) : Irreversible
cholinesterase inhibitor that is hydrolyzed
and, therefore, detoxified rapidly by mammals
but not by insects causing respiratory
paralysis
Ovicidal and pediculicidal. Binds to hair and
provides some residual protection after
therapy
Available as 0.5% and 1% lotion
Apply lotion to dry hair; leave on 8-12 h,
rinse; repeat in 7 d prn(as needed)
Contains flammable alcohol; do not expose
lotion or wet hair to open flame or electric
heat, eg, hair dryers (allow hair to dry
naturally and uncovered following
application); avoid contact with eyes (flush
eyes immediately with water if contact)
Trimethoprim-sulfamethoxazole
The mechanism of action is postulated to be
ingestion of the antibiotic by the louse as it
takes its blood meal; subsequently the
antibiotic kills the gut flora of the louse, with
death ensuing from a deficiency of B vitamins
The combination of permethrin and
trimethoprim-sulfamethoxazole was more
effective than either agent alone
Mercuric oxide Ointment (1%) is treatment of
choice for Phthirus palpebrarum
Inspect eyelids and remove nits mechanically
Apply to eyelashes qid for 14 d
Kerosene has shown pediculicidal activity in
vitro, but safety and efficacy remain to be
evaluated
DDT was the first pediculicide widely
available. It was the main agent used in the
treatment of body lice infestations during
World War II. It was banned in the 1970s but
about to be reintroduced as pesticide
Treatment failures
Drug resistance
Improper dilution or duration of
application
Reinfestation from untreated contacts
It may be best to assume that no product
is reliably ovicidal and that patients will
not comply fully with instructions.
Retreatment in 1 week to 10 days is
advisable to kill recently hatched nymphs
Drugs are often applied to wet hair, which
dilutes the product and protects lice as
they reflexively close their respiratory
spiracles when exposed to water
Hair conditioners may coat the hair
shafts and prevent pediculicides from
binding adequately to the hairs
Lice have been in
existence for thousands
of years. Their extinction
seems no more likely
than our own