Conservative Sharp Debridement
advertisement

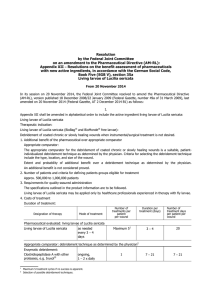
Conservative Sharp Debridement Nursing Care Responsibilities (Physical Therapy Too) Patricia Gill, MSN, RN, CWON, CHRN KNOW THE RULES OBTAIN A COPY OF YOUR LICENSING BOARD’S POSITION Written P& P in place All documents in employee file Written MD order for EVERY procedure New to ALL Facilities A written consent EVERY TIME A procedural checklist EVERY TIME A TIME OUT IMMEDIATELY PRIOR TO PROCEDURE EVERY TIME Dated and timed documentation with signatures of participating staff Conservative Sharp Debridement Differs from surgical debridement Definition Removal of loose, avascular tissue No pain No bleeding Topical anesthesia only (and only with a written order EVERY time) CONTRAINDICATIONS Unable to clearly identify viable from nonviable tissue Increased risk of bleeding (ASA, anticoagulation, disease process) Dry eschar, especially if on heel or suspect calciphalaxis Poor perfusion (arterial disease) Patient and Family Education (sometimes staff too) Dead tissue prevents healing Awareness that debridement may make the wound larger initially Frequent debridement will actually increase the rate of healing Develop the Goal of Treatment Healing vs Palliative Care Infection vs Colonization Comfort or Odor Control Include patient, family, staff, other treating MDs Other Types of Debridement Autolytic Mechanical Biologic Chemical Ultrasonic Surgical Know What You Are Cutting Out Dead tissue Tendon Muscle Fascia KNOW YOUR LIMITATIONS STOP Pain Bleeding You can’t see Structure visible Meet fascial plane The patient says “enough” YOU GET UNCOMFORTABLE Notify the Physician if: Sinus tracts or undermining Infection or cellulitis No improvement in 2 – 3 weeks Patient becomes febrile or develops other signs of systemic infection If There Is BLEEDING... APPLY PRESSURE Silver nitrate cauterization (need an order) Alginates (leave in place for 24 hours) Gelfoam or other stoppers Maybe hold VAC for 24 hours Post Debridement Procedures Saline dressing first 24 hours Sterile dressing 8 – 24 hours if there has been bleeding May need more frequent dressing changes Safe Practitioners... Know A & P Set goals of treatment Know when to stop Regularly update skills and competencies DOCUMENT DOCUMENT DOCUMENT