Wound Care Interventions
advertisement

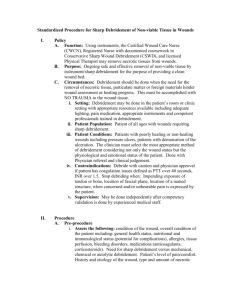
Wound Care Interventions Kate McKenney PT CWS June 4, 2013 Images • Images cannot be reused, reproduced or shared outside of the University of Michigan community. • Images can only be used for educational purposes. Contact Ultrasound – Slide 97 • Full thickness wounds – Ultrasound transmission gel to intact periwound and hydrogel to wound bed, then hydrogel sheet • Partial thickness wounds – Hydrogel sheet directly over the wound including 4-6 cm onto the periwound • Cleanse applicator with antibacterial agent • Ultrasound get on top of hydrogel sheet (Suspected) Deep Tissue Injury • DTI – Purple or maroon localized area of discoloration – Blood filled blister – May evolve rapidly into a very bad pressure ulcer, or may not evolve at all (Suspected) Deep Tissue Injury What we’ve covered • Cleansing the wound • Debridement – PLWS, Syringe Lavage, Whirlpool – Mechanical, Selective vs Non-Selective • • • • Topicals Dressings Contact Ultrasound Electrical Stimulation Contact Low Frequency Ultrasound • Ultrasound assisted wound therapy, ultrasound assisted debridement, Arobella, Qoustic Wound Therapy System • Low frequency 20-40 kHz (vs 1-3 MHz) • Non-thermal • Creates cavitation • Acoustic streaming Contact Low Frequency Ultrasound • Cavitation – Creation of miniscule gas bubbles in the tissue fluid and coupling medium – Bubbles expand/contract with variation in ultrasound field pressure levels – Bubbles implode; tiny shock waves – Necrotic tissue tensile strength < viable tissue – Shock waves liquefy necrotic tissue, biofilm Contact Low Frequency Ultrasound • Acoustic Streaming – Movement of fluids along the acoustic boundaries • Bubbles or cell membrane – Increases cell membrane permeability – Increases vascular wall permeability – Increase protein synthesis Cavitation and Acoustic Streaming • Believed to be responsible for stimulatory effects of cells. • Believed to modulate cell activity – Increase cellular proliferation – Increase collagen deposition* – Increase growth factor activity • Bottom line: – Good for healthy cells* – Bad for bacterial, senescent and devitalized cells Contact Low Frequency Ultrasound • http://www.youtube.com/watch?v=xl0tCZ5kD TY Contact Low Frequency Ultrasound • Indications: – All wounds that require debridement Contact Low Frequency Ultrasound • Benefits: – Immediate results- removal of slough – Selective – Less painful that sharp debridement??? • Considerations: – $$$$, no “extra” reimbursement – Can be painful – Be careful, used for “excisional” debridement • Debridement of living tissue • Physician only! (not in scope of practice of PT) • When performing this technique over living tissue, move the contact head more quickly so it doesn’t result in excisional debridement. – Aerosolization and PPE Contact Low Frequency Ultrasound • Contraindications: – All ultrasound contraindications • Malignancy, cardiac area in CHF, etc. – Untreated, advancing cellulitis – Signs of systemic infection – Metal components – Electrical device within treatment area – Uncontrolled pain: know what’s causing this! – DVT, emboli (can break up clot and cause a stroke) Non-Contact Low Frequency Ultrasound • MIST Therapy • Same principles as Contact Low Frequency Ultrasound • No contact = no pain – Reduces pain??? • Can be used for maintenance debridement – No harm to healthy tissue • Disposable; 3-5 minutes total • No aerosolization: mist does not come out at high enough PSI to create aerosolization – MUST wear PPE Non-Contact Low Frequency Ultrasound • http://www.youtube.com/watch?v=dhfGMW mBhhc • http://www.youtube.com/watch?v=Yi1hj7QC Oeo Non-Contact Low Frequency Ultrasound • Indications: – Suspected DTI (deep tissue injury that hasn’t opened up) – Plus any wound • Considerations: – $$$$ (18-25K) – CPT code coming January 1, 2014! (reimbursement to be determined still) Non-Contact Low Frequency Ultrasound • Contraindications – Same as Contact Low Frequency Ultrasound Debridement • Removal of tissue or foreign material – Conservative – removal of senescent, dead or devitalized tissue – Aggressive or excisional – removal of living tissue • Done by surgeon/physician in OR • Indications: – Any time there is something that needs to be removed! Debridement Benefits •Decrease bacterial load •Stimulates growth factors •Exposes cell receptors for growth factor interface •Remove senescent cells •Facilitate angiogenesis •Allow full determination of depth and character of wound bed (which will help with setting a prognosis) Debridement • Considerations – Pain – Anticoagulants/Bleeding disorder – Know your anatomy! • If you don’t know, don’t remove! – ABI? • Some texts say not to do on anyone with ABI less than 0.5 because there may not be enough blood flow to support debridement • Have to use good clinical judgment to determine whether to do this • Think about what you are doing to increase circulation IF choosing to do this on someone with a low ABI • If less than 0.7 send to see a vascular surgeon to see if they can get a stent, meds etc. Debridement • No – leave it alone! – Granulation tissue – Viable or potentially viable tissue – Stable eschar (see picture) – Dry gangrene – Pyoderma Gangrenosum – Muscle, tendon, ligament, capsule, fascia, nerves, blood vessels (things you need!) – Intact blisters Pyoderma Gangrenosum • Poorly understood skin condition • 1 in 100,000 (rare, but you will see in wound clinic) • Wound that will Rapidly enlarge with trauma and debridement of wound bed (ie: removing a dressing that is stuck to the wound bed, etc) • Unknown etiology – Associated with inflammatory conditions • (bowel disease, RA, immune disorders) – 50% of cases are idiopathic • Reoccurrence rate 30% Pyoderma Gangrenosum • Typically lower legs • Edges elevated with undermining • Violaceous borders – Looks similar to hemosiderin staining • Cribiform scarring – Criss cross scarring pattern • Diagnosis by exclusion – There is NOT test for this Pyoderma Gangrenosum • Treatment – If suspect, stop debridement and get to dermatologist ASAP! • Wound will appear worse after first treatment • Elevated edges will be worse – Oral steroids – Topical steroids, antibiotic and sometimes immunosuppressant • Months to years to heal – Because you cannot do debridement – Steroids=delayed healing Debridement • We’ve already covered some: – PLWS – Syringe lavage – Whirlpool – Irrigation – Selective vs Non-selective Debridement • Additional means: – Enzymatic Debridement – Autolytic Debridement – Biological Debridement – Sharp Debridement Debridement What are we trying to do? •Necrotic tissue •Eschar (firm, thick) •Slough (yellow, white, tan. Can be easy or hard to remove) •Debris (dressing residue) •Residual topicals •Foreign material •Callus DEFINITELY get rid of! •Biofilm/Bioburden? •Can’t see this but needs to be removed because it can cause Debridement Callus (yes) Blister (no) Debridement Granulation tissue (no) Debridement Slough (yes) Debridement Slough (yes) Debridement Stable eschar (no) Unstable eschar (yes) Debridement Tendon (no) Debridement Dry Gangrene (No)

![Jiye Jin-2014[1].3.17](http://s2.studylib.net/store/data/005485437_1-38483f116d2f44a767f9ba4fa894c894-300x300.png)