Best Practice for Pressure Ulcers
advertisement

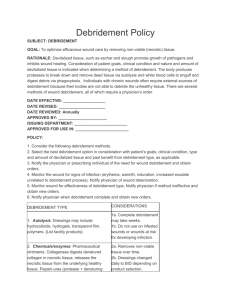
Best Practices for Pressure Ulcers to Promote Uncomplicated Healing Introduction Pressure ulcers are major health problems in the U.S. Affects approximately 1.3 to 3 million adults yearly. Over 11 billion dollars is use to treat ulcers per year. Introduction (cont.) Increased awareness is important in the health care setting to prevent ulcers. It is imperative to find the best research to prevent and treat the occurrences of ulcers in the healthcare setting. Sources We found 2 sources that were ranked high on level of evidence that had comprehensive information. The first source is a Retrospective cohort study with convenience sampling. Sources (cont.) There were 4 themes that were examined in this study: The relevance of nutrition to wound healing. Pressure ulcers cleaned with saline or soap compared to those cleaned with other cleansers such as antiseptic, antibiotic, or commercial cleansers. The therapeutic effectiveness of debridement on the wound bed. Evaluating whether dry or moist dressings is more advantageous to healing. Sources (cont.) Our second source is a clinical guideline. We used this article to support the evidence found in our other source. This clinical guideline identified the best practices for pressure ulcer management from 41 studies and articles related to pressure ulcer treatments. Nutrition Nutrition is considered a significant factor in both the prevention and treatment of pressure ulcers. Protein, carbohydrates, vitamins, minerals, and trace elements are required for wound healing. Nutrition A nutritional assessment should be performed on all newly admitted patients and whenever there is a change in a patient condition. Nutritional support should be given only to patients with identified nutritional deficiencies, and only when not contraindicated. Infection Pressure ulcers need to be assessed and reassessed for signs of infection. Infection complicates the healing process of pressure ulcers. Early recognition along with prompt and effective interventions is needed to address the infection. Assessment of the wound must be done to evaluate the healing and the treatment of the wound. Infection (cont.) Necrotic tissue must be removed and present infection must be treated for healing to occur. The necrotic tissue may be removed by different types of debridement. Debridement Why is it needed for pressure ulcers? To promote healing To allow the healing process to occur To protect against bacteria To remove dead tissue Types of Debridement Enzymatic Surgical Autolytic Mechanical Debridement (cont.) Enzymatic debridement Use of exogenous proteolytic enzymes to removed dead tissue. Used in wounds with large amount of debris. Advantages Minimal damage to healthy tissue Bleeding disorders Very effective in most patients Disadvantages Expensive Topical agents Needs to be softened Debridement (cont.) Surgical debridement Removal of layers of necrotic tissue using a laser, scissors forceps, or curette using sterile technique. Sharp debridement can be done by nurses with training. Advantages Best used for larger wounds and infected pressure ulcers. Disadvantages Painful EMLA cream as a local anesthetic Costly Contraindicated in patient receiving anticoagulants, and clotting disorders, lack of experience, sepsis Debridement (cont.) Autolytic debridement Stimulation of natural enzymatic activity by the use of the endogenous enzymes used to digest the dead tissue. Used for larger pressure ulcers and deep wounds. Semi-occlusive or occlusive dressing using transparent films, hydrocolloids, hydrogels Advantage Selective Painless Disadvantages Time Risk for infection Debridement (cont.) Mechanical debridement The removal of slough or necrotic tissue by use of wet-to-dry dressing or whirlpool treatment. Used in wounds with a great amount of necrotic tissue. Advantages Cost Disadvantages Painful Takes off healthy tissue Trauma to wound Infection (whirlpool) Least recommended Dressings Select the appropriate dressing for the wound Consider the wound’s characteristics: location, phase of healing, infection, frequency of dressing changes, product availability, cost. The choice of the dressing should change as the wound heals. Moist wound dressings Advantages Keeps the wound bed moist. Eliminates dead space. Controls the exudates. Dressings (cont.) Nondraining Wounds Use transparent film, hydrocolloid, or hydrogel dressings. Draining Wounds Use foam, alginate, or collagen dressings. Dressings (cont.) Hydrocolloid dressings Shown to have a lesser risk of infection than gauze dressings. Should not be used on infected wounds or wounds with undermining, tunneling, or sinus tracts. Hydrocolloid dressings have a greater affect on wound healing than saline gauze or paraffin gauze. Infected wounds Do not use occlusive dressings when an anaerobic bacterial infection is present or suspected. Positive correlation between gauze dressings and rates of infection, because they lower wound temperature and impede fluid evaporation.