Osteomyelitis
advertisement
Osteomyelitis
Osteomyelitis
Inflammation of bone and marrow
Types
Pyogenic osteomyelitis
Tuberculous osteomyelitis
Pyogenic
Osteomyelitis
Pyogenic osteomyelitis
Always caused by bacteria
Routes of infection
Hematogenous spread
Extension from a contiguous site
Direct implantation
Causes
Staphylococcus aureus in 80% to 90% of cases
E.coli, Pseudomonas, and Klebsiella in patients with
genitourinary tract infections and IV drug abusers.
In neonates: Hemophilus influenza and group B
streptococci
In patients with sickle cell disease –Salmonella
infection
Morphology
Acute
Subacute
Chronic
Organisms once localized in bone
Bacteria proliferate and induce inflammatory reaction and cause cell
death.
Bone undergoes necrosis within first 48 hours
Bacteria and inflammation spread within the shaft of the bone and
may percolate throughout the haversian systems and reach the
periosteum
Subperiosteal abscess
Segmental bone necrosis sequestrum (dead piece of bone)
Rupture of periosteum leads to an abscess in the surrounding soft
tissue and the formation of draining sinus.
Over time, host response develops
After first week of infection chronic inflammatory cells
become more numerous
Cytokines from leukocytes stimulates osteoclastic bone
resorption ingrowth of fibrous tissue deposition
of reactive bone in the periphery
Reactive woven or lamellar bone which forms sleeve of
living tissue surrounding dead bone is called as
involucrum.
Brodie abscess: is a small intraosseous abscess
that frequently involves the cortex and is walled
off by reactive bone
Sclerosing osteomyelitis of Garre: typically
develops in jaw and is associated with extensive
new bone formation
PATHOLOGY
Acute Infiltration of PMNs
Congested or thrombosed vessels
Chronic Necrotic bone
Absence of living osteocyte
Mixed inflmmatory cells
predominate
Granulation & fibrous tissue
Osteomyelitis-gross & microscopy
Sequestrum (necrotic bone)
Involucrum (new bone)
Osteomyelitis of the tibia of a
young child. Numerous
abscesses in the bone show
as radiolucency.
HEMATOGENOUS OSTEOMYELITIS
Clinical manifestation
Classic presentation: Sudden onset
High fever, Night sweats
Fatigue, Anorexia, Weight loss
Restriction of movement
Local edema, Erythema, & Tenderrness
Clenched fist
osteomyelitis
HEMATOGENOUS OSTEOMYELITIS
Diagnosis & work-up
Lab study:
WBC May be elevated, Usually normal
{
C-Reactive Protein (CRP)
Erythrocyte Sedimentation Rate
(Usually is elevated at presentation
Falls with successful therapy)
Blood culture
( Acute osteomyelitis + ve > 50% )
HEMATOGENOUS OSTEOMYELITIS
Diagnosis & work-up
Imaging
Radiology:
Normal
Soft tissue swelling
Periosteal elevation
Lytic change
Sclerotic change
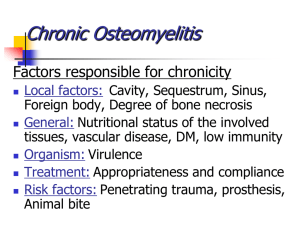
Complications of chronic osteomyelitis:
1)
2)
3)
4)
5)
6)
7)
Deformities of bones:
Pathological fractures.
Systemic effects such as chronic fever & fatigue.
Amyloidosis of the AA type (secondary
amyloidosis).This can get further deposited in the
kidney, liver & blood vessels.
Squamous cell carcinoma of the skin: The skin at
the edges of the draining sinus tracts may undergo
malignant transformation over time.
Sepsis
Rarely sarcoma in the infected bone
Specific forms of chronic osteomyelitis
Forms of chronic osteomyelitis include:
Brodie abscess,
Tuberculous osteomyelitis,
Osteomyelitis of congenital syphilis, and
Osteomyelitis of acquired syphilis.
TB osteomyelitis:
Dissemination of tuberculosis outside the lungs
can lead to the appearance of skeletal TB:
Skeletal Tuberculosis:
Tuberculous osteomyelitis involves mainly the
thoracic and lumbar vertebrae (known as Pott
disease) followed by knee and hip.
There is extensive necrosis and bony destruction
with compressed fractures (with kyphosis) and
extension to soft tissues, including psoas "cold"
•
abscess.
Tuberculous osteomyelitis of the bone is secondary
hematogenous spread from a primary source in the
lung or GI tract.
It most commonly occurs in the vertebrae (body) and
long bones.
Once established, the bacilli provoke a chronic
inflammatory reaction.
Small patches of caseous necrosis occur, and these
coalesce to form larger abscesses.
The infection spreads across the epiphysis into the
joints.
The infection may track along soft tissue to appear as a
cold abscess at a distant site (eg: psoas abscess in case
of spinal tuberculosis).
Spinal tuberculosis. Magnetic resonance imaging of the spine
revealing osteomyelitis involving T10 and T11 vertebral bodies
and disc space (A; arrow) and an adjacent multiloculated
paravertebral abscess (B; arrow).
Psoas abscess: Computed tomographic scan of the
abdomen showing a left iliopsoas abscess (arrow) that
likely originated from tuberculous osteomyelitis involving
the T12, L1, and L2 vertebrae.
Syphilitic osteomyelitis:
The transplacental spread of spirochetes from mother
to the fetus results in congenital syphilis.
Long bones, such as the tibia, are mainly affected.
Congenital syphilis has 2 forms:
Periosteitis and osteochonditis.
Regarding acquired syphilis, bone lesions are manifestations of
tertiary syphilis.
Gummatous lesions appear as discrete punched-out radiolucent
lesions in medulla or destructive lesions within the cortex.
The surrounding bone is sclerotic, and no discharge is present.
Bones frequently affected are those of nose, palate, skull and
extremities, especially the long tubular bones such as tibia.
Histology : edematous granulation tissue containing numerous
plasma cells and necrotic bone.
“Sabre” tibia