Care Management Protocols, Disease Registries, and Other
advertisement

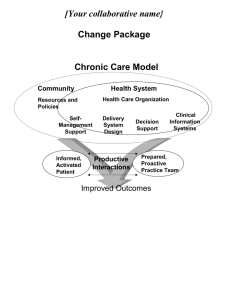
Systems Support: Care Management Protocols, Disease Registries, and Other Tools Amy M. Kilbourne, PhD, MPH VA Ann Arbor Serious Mental Illness Treatment Research and Evaluation Center Department of Psychiatry, University of Michigan SMITREC Mental Health Services Research Group Chronic Care Model- chronic mental illness Quality improvement interventions to improve medication adherence Mental health performance measures Primary Care – Mental Health Integration Program Substance abuse in primary care Predictors of suicide Aging and preventable mortality National VA Psychosis Registry National VA Registry for Depression Implementation Care Management Guidelines Patient Registries Other Tools Wagner Chronic Care Model Community Resources and Policies Health System Health Care Organization SelfManagement Support Informed, Activated Patient Delivery System Design Productive Interactions Decision Support Clinical Information Systems Prepared, Proactive Practice Team Functional and Clinical Outcomes CCM: Core Clinical Elements Leadership Vision Resources Practice Design Care management Protocols- coordinated care Clinical Information Systems Clinical information tracking Feedback to clinicians CCM: Core Clinical Elements Decision Support Guidelines Expert/specialist consultation Self-management Patient preferences Information on treatment Support Community Resources Information on and for consumers, groups, etc. Access to non-provider sources of care Care Manager Role General Medical (Chronic care, Prevention, Follow-up) Care Manager Self-management Liaison: PCP, MH Crisis intervention Behavioral Health (crisis referral for ICM, etc.) Care Manager: Skills Tracks depressive symptoms and treatment response (PHQ-9) Consults with team psychiatrist Collaborates closely with patient’s primary care provider (PCP) Provides follow-up and recommendations to PCP who prescribes antidepressants Facilitates referrals to specialty, community Prepares for relapse prevention Care Manager: Skills Familiar with commonly used antidepressant medications, doses Patient education about antidepressants Support antidepressant medication adherence Know when treatment is ‘not working’ CM: Self-management Eliciting concerns/barriers Problem-solving Providing information Clarifying preferences Encouraging informed decision-making Teaching skills Monitoring progress Reinforcing self-management Community resources CM: Self-Management Tools Medication lists Pillboxes Appointment reminders Healthy behaviors Pleasure activities list CM: Therapeutic Alliance Cultural competence Role of families Role of religion/spirituality Competing needs CM: Liaison Relay concerns/progress Refills Symptoms and side effects Urgent, emergent protocols Medical record documentation Cue providers if no improvement Supplement, not replace providers CM: Liaison Help patients and providers ID Potentially inadequate doses Ineffective treatment (e.g., persistent depression after Adequate duration of antidepressant trial) Side effects Facilitate patient-provider (e.g., PCP) communication about antidepressant medications Consult about medication questions Examples of CM-Provider Contact Medication toxicity, cross-reactivity Notifying provider of patient concerns, follow-up Fatigue, physical symptoms CM prompted provider to call pt. after missed appt Managing multiple medications, depression, diabetes, and HT (medication lists, pillboxes) Alcohol use and grief management Kilbourne AM. Bipolar disorders, in press 2008 Kilbourne AM. Psychiatric services, under review, 2008 Provider Communication Tips Obtain preferred mode of communication Emphasize as a supplemental service Focus on providing information on changes in treatment response, side effects, etc to inform decisions Baseline, Current PHQ Length of time on medications Problematic symptoms/side effects Adequate contact, but don’t overdo it CM: Crisis Intervention Suicidal ideation- coordinate with clinic Protocols On-call numbers Missed appointments Immediate follow-up CM: Suicidal Ideation If the patient articulates thoughts death/suicide: Where are you now? What is your phone number at the location? Are you alone or with someone? Do you have a plan of how you would do this? Do you have these things available (guns, pills)? Have you actually rehearsed or practiced how you would do this? Have you attempted suicide in the past? Do you have voices telling you to harm or kill yourself? Care Manager Registry Registries are . . . Simple tools to track patient progress (K.I.S.S.) NOT EMRs Best if “home-grown” Facilitate structured patient contacts Types of registries, pros and cons Excel file Web-based Developing Registries Things to Know Know your stakeholders and get their input (purchasers, payers) Know your population- case mix, location Know your key data sources What is in the administrative datasets? Do they capture utilization? Know what information technologies are available and whether they can be tailored Web-based patient health risk assessments Developing Registries Things to Know (cont.) Know your end users (e.g., care managers, clinic staff, providers), including their work flow, and ensure they can work with the registry on a day-today basis Know what stakeholders want in terms of outcomes: What quality and cost measures are they interested in, and use registry to enhance performance measures Registry: Sample Fields General information (update at each contact): Patient contact info, including emergency contact Providers Best time to call/OK to leave message? Plan to keep then safe/calm Contact (Encounter)-specific information: Contact or visit date Current Mood, Speech, Comorbidities Current medications/OTCs, refills needed? Medications not taking and reason Symptoms and side effects Health behaviors (sleeping, drug use, smoking ,exercise) Job/personal problems Education provided Access/barriers, provider engagement Next appt Registry Examples SMAHRT IMPACT Care Manager Toolbox Self-management materials Antidepressant medication list Registry file Provider contact sheet Preferences Crisis intervention Operations manual Care Manager Initial Visit Rapport- providers Patient initial intake Contact preferences Crisis and urgent care protocols Assessment Discuss treatment options / plans Coordinate care with PCP Start initial treatment plan Arrange follow-up contact Document initial visit Care Manager Subsequent Visit Upcoming appointments Registry- ongoing tracking