Common drugs Eruption
advertisement

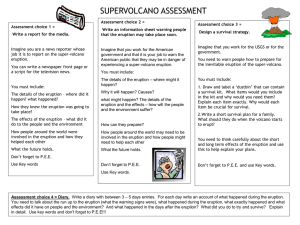
Professor Ihab Younis, M.D. Etiology • It occurs in approximately 2-5% of inpatients and in greater than 1% of outpatients • Most estimates of the incidence of drug eruptions are inaccurate, because many mild and transitory eruptions are not recorded, and because skin disorders are sometimes falsely attributed to drugs • Elderly patients have an increased prevalence of adverse drug reactions • It may be divided into immunologically and nonimmunologically mediated reactions A - Immunologically mediated reactions The 4 types of hypersensitivity occur: Type I (IgE-Dependant) • The drug or protein conjugates with two or more specific IgE molecules, then gets fixed to sensitized mast cells or circulating basophil. This triggers the cell to release a variety of chemical mediators e.g.histamine and cytokines • Clinically, this may produce pruritus, urticaria, bronchospasm, laryngeal edema and in severe cases anaphylactic shock with hypotension and possible death • Immediate reactions occur within minutes of drug administration; accelerated reactions may occur within hours or days, and are generally urticarial but may involve laryngeal oedema • Penicillins are the commonest cause of IgEdependent drug eruptions Type II (Antibody Mediated) • An immune complex is formed from: The drug + a cell + Ig G antibodies with subsequent complement fixation • Example:thrombocytopenic purpura that may result from antibodies to quinidine Type III (Immune Complex Reaction) • Soluble immune complexes are formed from Ig G class antibodies & a soluble antigen (not attached to the organ involved) • Example:Vasculitis induced by antibiotics results from deposition of immune complexes on vascular endothelium resulting in activation of the complement cascade Type IV (Delayed or cell-mediated) • First,sensitization to the drug occurs when Langerhans' cells take up and process antigen, and migrate to regional lymph nodes, where they activate T cells with the consequent production of memory T cells, which end up in the dermis. On consequent exposure to the drug T cells & keratinocytes release cytokines causing inflammation • Example:Contact dermatitis to neomycin B- Nonimmunologicallymediated reactions 1-Accumulation: e.g. argyria (blue-gray discoloration of skin and nails) observed with use of silver nitrate nasal sprays 2-Side effects: unwanted or toxic effects, which are not separable from the desired pharmacological action of the drug e.g. the drowsiness induced by antihistamines 3-Direct release : The direct release of mast cell mediators is a dose-dependent phenomenon that does not involve antibodies. For example, aspirin and other NSAIDs cause a shift in leukotriene production, which triggers the release of histamine and other mast-cell mediators 4-Idiosyncrasy: a response, not predictable from animal experiments, and its cause is often unknown, but genetic variation in metabolic pathways may be involved e.g. dapsone induced hemolysis due to glucose-6-phosphate dehydrogenase deficiency 5-Intolerance:The characteristic effects of the drug are produced to an exaggerated extent by an abnormally small dose. This may simply represent an extreme within normal biological variation or may occur in patients with altered metabolism. For example, individuals who are slow acetylators of the enzyme N-acetyltransferase are more likely than others to develop drug-induced lupus in response to procainamide 6-Imbalance of endogenous flora: may occur when antimicrobial agents preferentially suppress the growth of one species of microbe, allowing other species to grow vigorously. For example, candidiasis frequently occurs with antibiotic therapy 7-Overdosage: is an exaggerated response to an increased amount of a medication. For example, increased doses of anticoagulants may result in purpura 8-Jarisch-Herxheimer phenomenon: is a reaction due to bacterial endotoxins and microbial antigens that are liberated by the destruction of microorganisms. The reaction is characterized by fever, tender lymphadenopathy, arthralgias, transient macular or urticarial eruptions, and exacerbation of preexisting cutaneous lesions. The reaction is not an indication to stop treatment because symptoms resolve with continued therapy. This reaction can be seen with penicillin therapy for syphilis, griseofulvin or ketoconazole therapy for dermatophyte infections 9-Metabolic effects: Drugs may induce cutaneous changes by their effects on metabolism e.g. isotretinoin may cause xanthomas by increasing lipoproteins 10-Teratogenicity and other effects on the fetus:Thalidomide, retinoids and cytotoxic drugs are proven teratogens and tetracyclines are deposited in developing bones and cause discoloration and enamel hypoplasia of teeth 11-Effects on spermatogenesis: A number of drugs cause oligospermia e.g. estrogens, androgens, cyproterone acetate, colchicine, most monoamine oxidase inhibitors, ketoconazole. Conception should also be avoided after griseofulvin for 3 months as it potentially can damage sperm Clinically • They usually begin 7-20 days after the medication is started • They may involve blood or tissue eosinophilia • They may recur if drugs chemically related to the causative agent are administered • • • • During history taking note and detail the following: All prescription and over-the-counter drugs, including topical agents, vitamins, herbal, laxatives, oral contraceptives, vaccines, homeopathic medicines, etc. as these may not be volunteered as medications The interval between the introduction of a drug and onset of eruption Route, dose, duration, and frequency of drug administration Any improvement after drug withdrawal and any reaction with readministration • Determining the morphology of drug eruptions can help the clinician determine the causative medication : Eruption Common drugs 1- Morbilliform (exanthematous(: •It is the most common pattern •Lesions are symmetric, with confluent erythematous macules and papules that spare the palms and soles •It typically develops within 2 weeks after the onset of therapy Ampicillin,penicillin, phenylbutazone,sulphonamides, gold, gentamycin, cephalosporins, barbiturates, thiazides Eruption Common drugs 2- Urticaria: •It is the 2 nd most common eruption •Occurs as small wheals that may coalesce or have cyclical or gyrate forms •Lesions appear within 36h of intake and resolve rapidly when the drug is withdrawn ACEI ,aspirin/NSAIDs,blood products,cephalosporins, cetirizine, dextran, infliximab, inhaled steroids, opiates, penicillin, radiologic contrast material, ranitidine, tetracycline, vaccines, zidovudine Eruption 3- Purpura: •Can occur alone or as a component of vasculitis Common drugs Aspirin, cephalosporins, cytotoxics,heparin Eruption Common drugs 4- Pityriasis rosea-like: •Eruption is similar to PR •Itching is severe not responding to antihistamines •There is no tendency of spontaneous remission Gold,ACE inhibitors, thiazides, bismuth, barbiturates, griseofulvine, metronidazole Eruption Common drugs 5-Erythroderma:It is a scaling erythematous dermatitis involving 90% or more of the cutaneous surface Allopurinol,sulphonamides,anticonvulsants, aspirin, barbiturates, captopril, cefoxitin, chloroquine, chlorpromazine, cimetidine, griseofulvin, lithium, nitrofurantoin Eruption 6- Serum sickness: •Cutaneous signs begin with erythema on the sides of the fingers, hands, and toes and progress to a widespread eruption (most often morbilliform or urticarial) • Viscera may be involved, and fever, arthralgia, and arthritis are common Common drugs Antithymocyte globulin for bone marrow failure, human rabies vaccine, penicillin and vaccines containing horse serum, aspirin Eruption Common drugs 7- Erythema multiforme minor: It is characterized by target lesions distributed predominantly on the extremities. Mucous membrane involvement may occur but is not severe. Patients with EM minor recover fully, but relapses are common Sulphonamides,cephalosporins,penicillins,tetracyclines, phenytoin, barbiturates, aspirin, NSAID,thiazides Eruption Common drugs 8-Stevens Johnson synd. As EM •Bloody bullae, eroded, bloody or crusted lips, stomatitis and genitals mucosal ulceration •Conjunctivitis •Extensive EM on limbs •Sloughing of >10% of skin • Constitutional symptoms •Lymphadenopathy Eruption Common drugs 9-Toxic epidermal necrolysis: As EM •Starts with a burning morbilliform eruption accompanied by systemic flu-like symptoms •This is quickly followed by rapid, widespread, fullthickness skin sloughing affecting 30% or more the total body surface area Eruption 10- Fixed drug eruptions: • Lesions recur in the same area ½ -8 h after the drug is reused •Circular, violaceous, edematous plaques that resolve with macular hyperpigmentation •Hands, feet&genitalia are the most common sites but perioral and periorbital lesions may occur Common drugs Sulfonamides,penicillin, tetracyclines, aspirin/NSAID, barbiturates, cetirizine, ciprofloxacin, dapsone, fluconazole, hydroxyzine, loratadine, metronidazole, oral contraceptives, phenytoin, vancomycin Eruption 11- Lichenoid: •May develop weeks or months after initiation of therapy •Lesions are more extensive, more itchy and psoriasi-form than in idiopathic lichen •Oral lesions are rare •Resolution may take 14 months or more Common drugs Antimalarials, gold, diuretics,antihypertensives, hypoglycaemicagents, NSAI,antituberculous,tetracyclines, allopurinol, phenytoin Eruption 12- Phototoxic dermatitis •Min. to h. after sun exposure •Exaggerated sunburn •Vesicles& bullae in severe cases •Burning is the main symptom •Limited to sun-exposed skin Photoallergic dermatitis •1-3 days after sun exposure •Lesions are eczematous •Pruritus is the main symptom •May spread to non-exposed area Common drugs Chlorpromazine, psoralens,sulphonamides,tetracyclines, NSAI, thiazides Eruption 13- Acneiform: •Characterized by inflammatory papules or pustules that have a follicular pattern •Localized primarily on the upper body •In contrast to acne vulgaris, comedones are absent Common drugs Corticosteroid, anabolic steroids, oral contraceptives,halogens, isoniazid, lithium, phenytoin Eruption Common drugs 14- Pseudoporphyria: •Blistering and skin fragility that is clinically and pathologically identical to that of porphyria cutanea tarda, but hypertrichosis and sclerodermoid changes are absent and urine and serum porphyrin levels are normal Frusemide, cyclosporine, dapsone, etretinate, 5-fluorouracil,thiazides,isotretinoin, NSAIDs, oral contraceptives, tetracyclines Eruption 15 - Bullous pemphigoid: •Patients tend to be younger •Tissue-bound and circulating antibasement-membrane zone IgG antibodies may be absent Common drugs Frusemide, penicillamine, penicillins, sulphasalazine, PUVA Eruption 16- Pemphigus: •Pemphigus folliacius &erythematosus may occur but pemphigus vulgaris is rare •Most patients have tissue and serum autoantibodies as in idiopathic pemphigus Common drugs Captopril, D-penicillamine, captopril, gold, penicillins Eruption 17- Leukocytoclastic vasculitis: •It is the most common severe drug eruption •There are blanching erythematous macules quickly followed by palpable purpura • Fever, myalgias, arthritis, abdominal pain may occur • It appears 7-21 days after the onset of therapy Common drugs Sulphonamides, frusemide, aspirin /NSAIDs, cimetidine, gold, hydralazine,minocycline, penicillins, phenytoin, quinolones, sulfonamide, tetracycline, thiazides Eruption Common drugs 18- Erythema nodosum: •Tender, red, subcutaneous nodules •Appear on the anterior aspect of the legs •Lesions do not suppurate or become ulcerated Oral contraceptives (most common), halogens, penicillin, sulfonamides, tetracyclines Eruption Common drugs 19- Sweet syndrome (acute febr. neutrophilic dermatosis): •Tender erythematous papules and plaques occur most often on the face, neck, upper trunk, and extremities •The surface of the lesions may become vesicular or pustular •Systemic findings are common and include fever, arthritis, conjunctivitis, oral ulcers Retinoic acid, nitrofurantoin, oral contraceptives, tetracyclines,trimethoprimsulfamethoxazole Eruption Common drugs 20- Acral erythema: Cytotoxic •It is a relatively common drugs reaction to chemotherapy •There is symmetric tenderness, edema, and erythema of the palms and soles thought to be a direct toxic effect on skin •It resolves 2-4 weeks after chemotherapy withdrawal Eruption Common drugs 21- Acute generalized Beta-lactam antibiotics, macrolides, and mercury exanthematous pustulosis : Acute-onset fever and generalized scarlatiniform erythema occur with many small, sterile, nonfollicular pustules. The clinical presentation is similar to pustular psoriasis Eruption 22- Hair loss: Common drugs Cytotoxic drugs, anticoagulants, anticonvulsants, levodopa, antithyroids Eruption 23 - Hypertichosis: Common drugs Androgens, corticosteroids, minoxidil, phenytoin, penicillamine, cyclosporin, psoralens ,streptomycin Nail changes Silver : lunula discoloration D-penicillamine: Yellow nail Cytotoxics: Beau’s lines Minocycline: blue nails Rates of reactions to commonly used drugs • • • • • • • • • Amoxicillin - 5.1% Trimethoprim sulfamethoxazole - 4.7% Ampicillin - 4.2% Semisynthetic penicillin - 2.9% Blood (whole human) - 2.8% Penicillin G - 1.6% Cephalosporins - 1.3% Quinidine - 1.2% Gentamicin sulfate - 1% Drugs that commonly cause serious reactions • • • • • • • • • Allopurinol Anticonvulsants NSAIDs Sulfa drugs Bumetanide Captopril Furosemide Penicillamine Thiazide diuretics Drugs unlikely to cause skin reactions •Digoxin •Acetaminophen •Diphenhydramine •Aspirin •Aminophylline •Prochlorperazine •Ferrous sulfate •Prednisone •Codeine •Tetracycline •Morphine •Regular insulin •Warfarin •Folic acid •Methyldopa •Chlorpromazine •Serotonin-specific reuptake inhibitors Investigations • If history and physical examination are not sufficient for diagnosis, the following investigations may help: – Biopsy e.g. by showing eosinophils in morbilliform eruptions or numerous neutrophils without vasculitis in persons with Sweet syndrome – CBC count with differential may show leukopenia, thrombocytopenia, and eosinophilia in patients with serious drug eruptions – Special attention should be paid to the electrolyte balance and renal and/or hepatic function indices in patients with severe reactions such as SJS, TEN, or vasculitis – Urinalysis, stool guaiac tests (for occult blood), and chest radiography are important for patients with vasculitis – Drug reactions, apart from fixed drug eruption, have non-specific clinical features, and it is often impossible to identify the offending chemical with certainty, especially when a patient with a suspected reaction is receiving many drugs simultaneously Treatment • Once the offending drug has been identified, it should be promptly stopped. Failure of a rash to subside on drug withdrawal does not necessarily exonerate it, since traces of the drug may persist for long periods, and some reactions, once initiated, continue for many days without reexposure to the drug • Patients with morbilliform eruptions can continue medication even in presence of rash as the eruption often resolves, especially if the individual is being treated for a serious disease • Treatment of a drug eruption depends on the specific type of reaction -Therapy for exanthematous drug eruptions is supportive in nature. First-generation antihistamines are used with mild topical steroids (e.g. hydrocortisone( and moisturizing lotions, especially during the late desquamative phase • Oral antihistamines • A drying antipruritic lotion (calamine with or without 0.25% menthol and/or 1% phenol) or lubricating antipruritic emollients will help relieve the pruritus. Lotions with phenol should not be given to pregnant women • Topical steroids may provide some relief • If signs and symptoms are severe, a 2-week course of systemic corticosteroids (prednisone, starting at 60 mg) will usually stop the symptoms and prevent further progression of the eruption within 48 hours of the onset of therapy • Treatment of erythroderma : maintenance of body temperature and fluid and electrolyte balance, treatment of cardiac failure by use of digitalization and diuretics and administration of intravenous albumin for hypoalbuminaemia • The management of TEN is perhaps best carried out on an intensive care or burns unit Management of anaphlyaxis • Stop drug administration • Give i.m. 0.5-1ml 1:1000 adrenaline immediately • Check airway and give oxygen • Antihistamines:Chlorpheniramine maleate 1020 mg i.v. • Corticosteroids:Hydrocortisone 250mg i.v. and 100mg 6 hourly + Prednisolone 40mg/day for 3 d • I.V. Saline or glucose 5% • Monitor BP and pulse • For bronchospasm:aminophylline 250mg i.v. over 5 mins and 250mg in 500ml saline over 6 h.